Abstract
A noncommunicable disease (NCD) is a medical condition or disease that is by definition non-infectious and non-transmissible among people. Currently, NCDs are the leading causes of death and disease burden worldwide. The four main types of NCDs, including cardiovascular disease, cancer, chronic lung disease, and diabetes, result in more than 30 million deaths annually. To reduce the burden of NCDs on global health, current public health actions stress the importance of preventing, detecting, and correcting modifiable risk factors; controlling major modifiable risk factors has been shown to effectively reduce NCD mortality. The World Health Organization's World Health Report 2002 identified tobacco use, alcohol consumption, overweight, physical inactivity, high blood pressure, and high cholesterol as the most important risk factors for NCDs. Accordingly, the present report set out to review the prevalence and trends of these modifiable risk factors in the Korean population. Over the past few decades, we observed significant risk factor modifications of improved blood pressure control and decreased smoking rate. However, hypertension and cigarette smoking remained the most contributable factors of NCDs in the Korean population. Moreover, other major modifiable risk factors show no improvement or even worsened. The current status and trends in major modifiable risk factors reinforce the importance of prevention, detection, and treatment of risk factors in reducing the burden of NCDs on individuals and society.
Keywords: Noncommunicable disease, Risk factors, Prevalence, Trend, Korea
INTRODUCTION
A noncommunicable disease (NCD) is a medical condition or disease that is by definition non-infectious and non-transmissible among people. NCDs have long been the leading causes of death in developed countries, but are no longer health issues limited to high income countries [1,2] . The World Health Organization (WHO) reports and many international statistics indicate that NCDs are the global leading cause of death. According to the WHO's Global Health Observatory data, NCDs resulted in 36 million deaths (63% of 57 million deaths total) in 2008 [3]. Alarmingly, NCDs are now the leading causes of death in most low-income and middle-income countries. More seriously, NCD burden is increasing more rapidly in lower income countries and populations. In 2008, four fifths of NCD deaths occurred in low- and middle-income countries, and one third of these deaths killed people aged less than 60 years [4]. The four main types of NCDs are cardiovascular diseases, cancers, chronic lung diseases, and diabetes, leading to 17 million, 7.6 million, 4.2 million, and 1.3 million deaths, respectively, in 2008 [3]. Accordingly, most public health actions have targeted modifiable risk factors to reduce the burden of NCDs, as preventing or treating major modifiable risk factors has proven to be effective in reducing mortality from NCDs. The WHO's World Health Report 2002 identified tobacco use, alcohol consumption, overweight, physical inactivity, high blood pressure, and high cholesterol as important risk factors for NCDs [5]. In accordance therewith, the present report set out to review the prevalence and trends of these six modifiable risk factors in the Korean population.
TOBACCO USE
Cigarette smoking has long been the greatest cause of NCDs in Korea. Previously, the population attributable risks due to smoking were estimated as 73% for lung cancer mortality, 32% for stomach cancer mortality, 15% for liver cancer mortality and 24% for pancreas cancer mortality [6]. An additional study reported that smoking attributed to 41% of coronary heart diseases and 26% of strokes in Korean men [7]. Korean data indicate that cigarette smoking is a major modifiable risk factor for type 2 diabetes: smoking is associated with diabetes incidence and mortality [8], and smoking cessation has been shown to reduce the risk for developing diabetes among smokers [9]. Additionally, smoking is the most contributable factor in the development and progression of chronic lung disease [10-12].
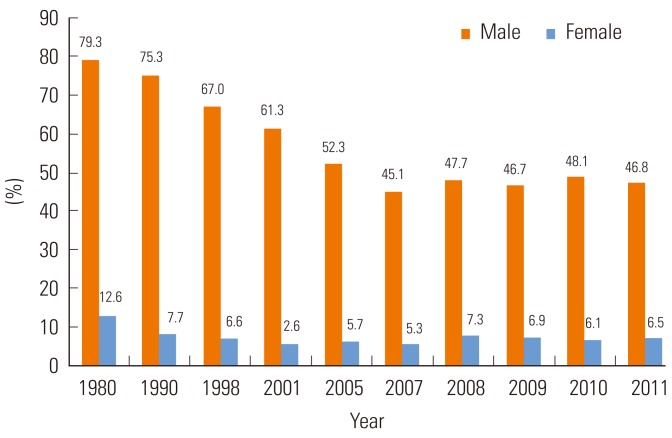
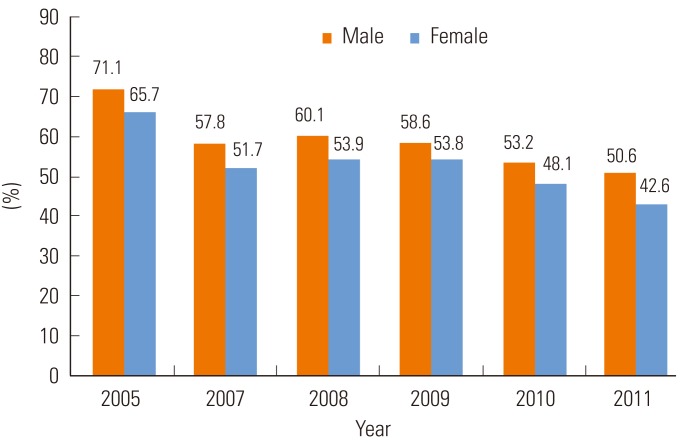
Among Korean adult males, smoking rates have decreased from 79% in 1980 to 67% in 1998 and 45% in 2007, but have not decreased any further since. Smoking rates in adult females have not seen much change (Figure 1). According to the latest Korea National Health and Nutrition Examination Surveys (KNHANES) report, the smoking rate was 47% in male adults and 6.5% in female adults [13]. However, in a 2008 survey, smoking rates verified by urinary cotinine level were much higher, at 50% for male and 14% for female adults [14]. Reports have also indicated that smoking rates differ by age and socio-economic status. Among men, smoking rates were highest in those in their 30s, while among women, smoking rates were highest in those in their 20s. Lower household income was also associated with a higher smoking rate in both men and women, but this association was stronger in women: smoking rate was 4% in women of the highest income quartile, but 11% in those of the lowest income quartile [13].
Figure 1.
Proportion of current smokers among Korean adults aged 19 years or older. Modified from Korea Centers for Disease Control and Prevention. Korea health statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2). Seoul: Ministry of Health and Welfare; 2012 [13].
ALCOHOL CONSUMPTION
Alcohol consumption is associated with increased risks of chronic liver disease, heart failure, and some types of malignancy [15-17]. Although moderate alcohol consumption has been shown to be associated with reduced cardiovascular incidence and mortality, excessive alcohol consumption is associated with elevated blood pressure and thus hemorrhagic types of stroke [18,19]. Moreover, increasing evidence supports that there is no threshold in the adverse effects of alcohol on the risk of cancer and other chronic diseases [20,21]. For these reasons, alcohol drinking of more than one drink per day is not recommended for the purpose of disease prevention.
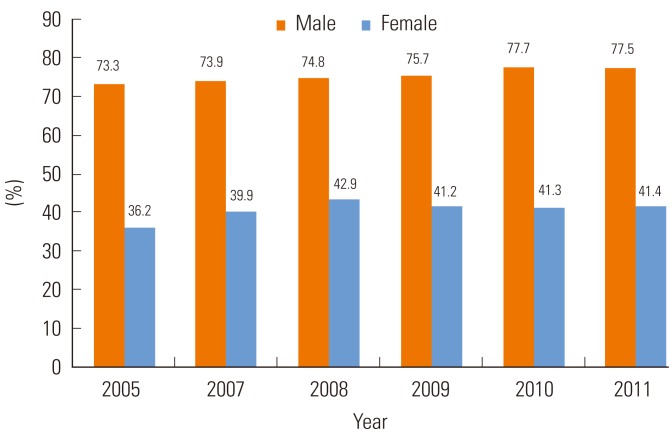
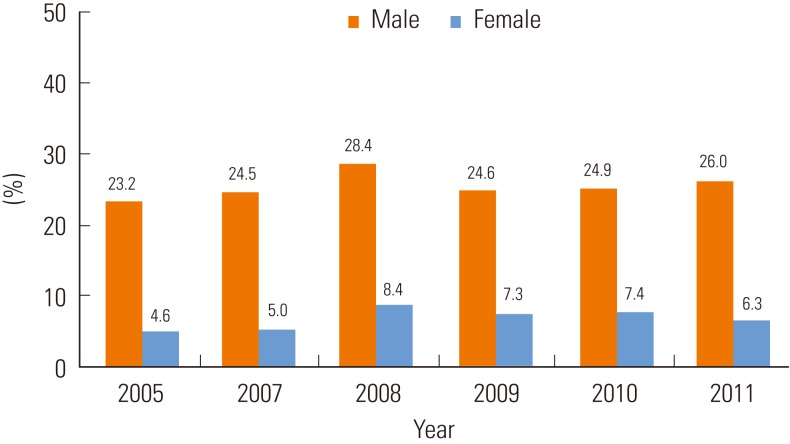
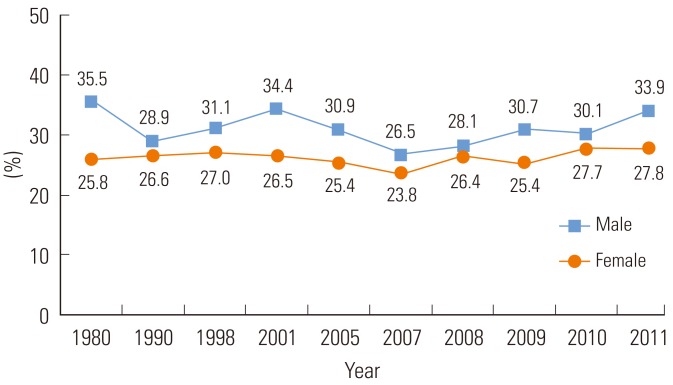
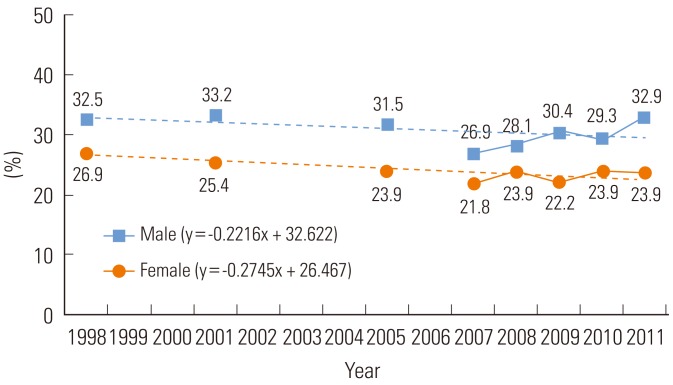
According to the 2011 KNHANES report, 78% of male and 41% of female adults aged 19 years or older drink alcohol at least once a month (Figure 2). At risk drinking is highly frequent among both male and female Korean adults: 26% of adult males intake 7 or more drinks at least twice a week and 6% of adult females intake 5 or more drinks at least twice a week, the prevalence of which showed a slightly increasing trend (Figure 3) [13]. Among alcoholic drinkers, 38% were classified into harmful categories based on Alcohol Use Disorders Identification Test: 24% for hazardous drinking, 7% for alcohol abuse, and 8% for alcohol dependence [13,22].
Figure 2.
Proportion of people who drink at least once a month among Korean adults aged 19 years or older. Modified from Korea Centers for Disease Control and Prevention. Korea health statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2). Seoul: Ministry of Health and Welfare; 2012 [13].
Figure 3.
Proportion of people who reported at risk drinking1 among Korean adults aged 19 years or older. 1At risk drinking: intake 7 or more drinks (5 or more in women) at least twice a week. Modified from Korea Centers for Disease Control and Prevention. Korea health statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2). Seoul: Ministry of Health and Welfare; 2012 [13].
OVERWEIGHT AND OBESITY
Being overweight or obese is an important risk factor for all four major NCDs including cardiovascular disease, cancer, diabetes, and chronic lung disease. Moreover, obesity is a well-known risk factor of diabetes and insulin resistance. The prevalences of obesity and diabetes are increasing concomitantly in Korea [23,24]. Presumably, the population attributable risk of obesity in cardiovascular disease is increasing, as obesity itself is on the rise and the major forms of cardiovascular disease have changed from hemorrhagic stroke to ischemic stroke and coronary heart disease in Korea. The impact of obesity is also garnering greater attention among cancer prevention efforts as well. Colorectal cancer and female breast cancer are increasing as two major causes of cancer death [25,26], and obesity is a major modifiable risk factor of these two malignancies. Additionally, there is increasing evidence that obesity and chronic lung disease are inter-related [27].
Currently, about one third of Korean adults have a body mass index (BMI) higher than 25.0 kg/m2. Between 1998 and 2011, the prevalence of a high BMI (≥25.0 kg/m2) increased from 29% to 34% among adults aged 30 years or older. During the same period, the prevalence of a high BMI increased from 15% to 22% among people aged 19 to 29 years old [13]. Similarly in many other developed countries, being overweight increased more steeply among low-income people than high-income people.
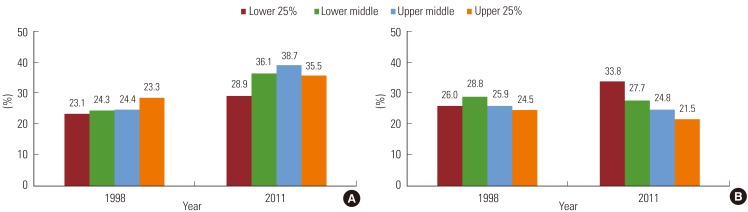
One unique feature in the trends of obesity in Korea is a discrepancy between men and women. Between 1998 and 2011, the age-standardized prevalence of high BMI increased by 1.1% per year in men, but decreased by 0.1% per year in women [13]. Interestingly, obesity trends were affected by household income in a different manner between men and women (Figure 4). Obesity increased in men of all income categories, although the increase was slightly greater in men of lower household income. On the contrary, the prevalence of a high BMI increased greatly from 26% to 34% in women of the lowest income quartile, but decreased from 25% to 22% in women of the highest income quartile [13].
Figure 4.
Age-adjusted prevalence of obesity by quartiles of household income. Male (A) and female (B) adults aged 19 years or older. Obesity is defined as body mass index ≥25 kg/m2. Modified from Korea Centers for Disease Control and Prevention. Korea health statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2). Seoul: Ministry of Health and Welfare; 2012 [13].
PHYSICAL INACTIVITY
Physical inactivity is the fourth leading risk factor for mortality [28], and it has been shown to be associated with cardiovascular [29,30] and cancer mortality [31], as well as all-cause mortality [32]. In addition, physical inactivity is a known risk factor for obesity, metabolic syndrome [33], and cardiovascular disease [34]. Korean data also suggests that increased levels of physical activity are significantly associated with a decreased risk of abnormal components of metabolic syndrome [35,36].
According to the KNHANES report, the percentage of Koreans who exercised at moderate-to-high intensity, including walking, significantly decreased in both Korean men (from 71.4 % in 2005 to 50.6 % in 2011) and women (from 65.7 % in 2005 to 42.6 % in 2011) (Figure 5) [13]. Physical inactivity also differed by age and sex. The highest amounts of physical activity were shown in both men and women in their 20s, while men in their 40s and women in their 70s or older showed the lowest amounts of physical activity [13].
Figure 5.
Proportion of people who exercise at moderate to high intensity (including walking) among Korean adults aged 19 years or older. Modified from Korea Centers for Disease Control and Prevention. Korea health statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2). Seoul: Ministry of Health and Welfare; 2012 [13].
HIGH BLOOD PRESSURE
High blood pressure is the most contributable risk factor of stroke, and one of the major risk factors of coronary heart disease [37-40]. Hypertension is closely associated with type 2 diabetes [41], even though it is unclear whether hypertension directly increases the risk of diabetes. There is some evidence, however, that supports that hypertension is associated with risk of certain types of cancer [42-44]. Prevention and control of hypertension may be the most urgent public health issue in Korea, as the prevalence of hypertension is relatively high and stroke is the leading cause of death among Koreans.
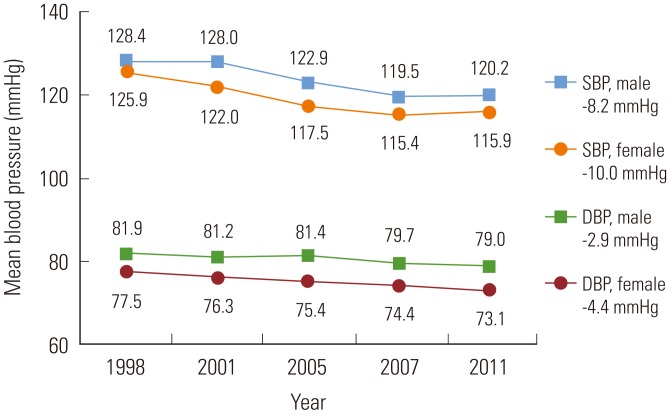
According to early nationwide blood pressure studies in 1980 and 1990 [45,46] and reports from the KNHANES since 1998 [13], the prevalence of hypertension in the Korean population did not change very much (Figure 6). Korea, however, is a rapidly aging society, in which the age-adjusted prevalence of hypertension actually shows a decreasing tendency. Analysis of data from the KNHANES 1998 through 2011 showed that the age-adjusted prevalence of hypertension decreased by 0.2 to 0.3 percent annually (Figure 7). More importantly, the population's mean blood pressure level has decreased continuously. Mean systolic blood pressure level decreased by 8 mmHg in men and by 10 mmHg in women, and mean diastolic blood pressure level by 3 mmHg in men and by 4 mmHg in women between 1998 and 2011 (Figure 8). This decrease in population blood pressure level was largely due to lowered blood pressure levels among patients with hypertension. Management of hypertension has been markedly improved in Korea during the past few decades. Among the patients with hypertension aged 30 years or older, awareness rates increased from 25% in 1990 to 67% in 2011, treatment rates increased from 16% in 1990 to 61% in 2011, and control rates increased from 1% in 1990 to 43% in 2011 [13].
Figure 6.
Prevalence of hypertension among Korean adults. Modified from Korea Centers for Disease Control and Prevention. Korea health statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2). Seoul: Ministry of Health and Welfare; 2012 [13].
Figure 7.
Age-adjusted prevalence of hypertension among Korean adults. Modified from Korea Centers for Disease Control and Prevention. Korea health statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2). Seoul: Ministry of Health and Welfare; 2012 [13].
Figure 8.
Trends in mean blood pressure level (mmHg) among Korean adults. Modified from Korea Centers for Disease Control and Prevention. Korea health statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2). Seoul: Ministry of Health and Welfare; 2012 [13].
SBP, systolic blood pressure; DBP, diastolic blood pressure.
These improvements in hypertension indexes have led to a dramatic decrease in stroke mortality. However, stroke remains the number one cause of death in Koreans, and hypertension control is still the biggest challenge to reducing the burden of NCDs. Although hypertension management has improved much in general, greater attention is needed concerning subgroups. For example, awareness, treatment, and control rates are much lower in younger patients with hypertension than in older patients, while control rates within patients under treatment do not differ by age [13]. These imply that a lack of awareness is the main cause of uncontrolled hypertension among younger patients, and reinforce the importance of screening for elevated blood pressure earlier in life.
HIGH BLOOD CHOLESTEROL
High blood cholesterol level or hypercholesterolemia is a major risk factor of atherosclerotic cardiovascular diseases including coronary heart disease and ischemic stroke, as well as peripheral arterial disease [47]. High cholesterol level has been reported to be associated with certain types of malignancy including breast cancer, colon cancer, or prostate cancer [48-50], although the cholesterol-cancer relationship is still unclear. High blood cholesterol and diabetes are known to be correlated with each other, yet it is unclear whether hypercholesterolemia contributes to the development of diabetes. Increasing evidence, however, suggests that high triglyceride level and low high-density lipoprotein cholesterol level are associated with an increased risk of type 2 diabetes [51-54].
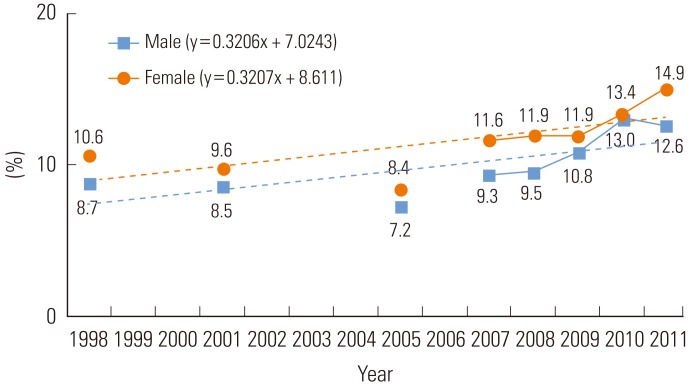
Until recently, high blood cholesterol level has garnered little attention in Korea, as its prevalence was relatively low, compared to that of other risk factors. However, reports of hypercholesterolemia are increasing (Figure 9); accordingly, coronary heart disease and cholesterol-related cancers are also increasing. According to the KNHANES reports, the prevalence of high total cholesterol level increased from 9.9% in 1998 to 14.5% in 2011. Nevertheless, while the prevalence of hypercholesterolemia is much lower than that of hypertension, the management of hypercholesterolemia is still poor. In the 2011 KNHANES, among adults with hypercholesterolemia, the awareness rate was 43%, the treatment rate was 33%, and the control rate was 26% [13].
Figure 9.
Age-adjusted prevalence of hypercholesterolemia among Korean adults. Modified from Korea Centers for Disease Control and Prevention. Korea health statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2). Seoul: Ministry of Health and Welfare; 2012 [13].
CONCLUSION
In order to reduce the burden of NCDs, comprehensive approaches across the entire disease spectrum are needed, from health promotion, primary prevention, screening of high-risk groups, and early diagnosis to better treatment and rehabilitation. An efficient and proven strategy to reducing NCD burden is risk factor modification. Major modifiable risk factors including high blood pressure, high blood cholesterol, tobacco use, alcohol consumption, and obesity are considered preventable or treatable, and exhibit great potential in reduce NCD burden.
The initial step for risk factor modification should be monitoring of prevalence and trends in risk factors. Recently, nationwide or community-based epidemiological studies have been accumulating descriptive data on NCDs and their risk factors. Over the past few decades, we observed some significant achievements in risk factor modifications among Koreans, such as improved blood pressure control and decreased smoking rate. Despite this success, hypertension and cigarette smoking still remained the most contributable factors of NCDs in the Korean population. Unfortunately, we did not observe any significant improvement in other major modifiable risk factors. Through this report, we discerned that greater attention is needed for indentifying and modifying such risk factors among subgroups of gender, age, and socioeconomic status.
Finally, the current status and trends in major modifiable risk factors reinforce the importance of prevention, detection, and treatment of risk factors in reducing the burden of NCDs on individuals and society.
Footnotes
The authors have no conflicts of interest with the material presented in this paper.
References
- 1.Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, et al. Priority actions for the non-communicable disease crisis. Lancet. 2011;377(9775):1438–1447. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Preventing chronic diseases: a vital investment. [cited 2013 Jul 7]. Available from: http://www.who.int/chp/chronic_disease_report/en.
- 3.World Health Organization. Global Health Observatory (GHO): deaths from NCDs. [cited 2013 Jul 1]. Available from: http://www.who.int/gho/ncd/mortality_morbidity/ncd_total/en/index.html.
- 4.World Health Organization. Global Health Observatory (GHO): NCD mortality and morbidity. [cited 2013 Jul 17]. Available from: http://www.who.int/gho/ncd/mortality_morbidity/en/
- 5.World Health Organization. The world health report 2002: reducing risks, promoting healthy life. [cited 2013 Jul 1]. Available from: http://www.who.int/whr/2002/en/index.html. [DOI] [PubMed]
- 6.Jee SH, Samet JM, Ohrr H, Kim JH, Kim IS. Smoking and cancer risk in Korean men and women. Cancer Causes Control. 2004;15(4):341–348. doi: 10.1023/B:CACO.0000027481.48153.97. [DOI] [PubMed] [Google Scholar]
- 7.Jee SH, Suh I, Kim IS, Appel LJ. Smoking and atherosclerotic cardiovascular disease in men with low levels of serum cholesterol: the Korea Medical Insurance Corporation Study. JAMA. 1999;282(22):2149–2155. doi: 10.1001/jama.282.22.2149. [DOI] [PubMed] [Google Scholar]
- 8.Jee SH, Foong AW, Hur NW, Samet JM. Smoking and risk for diabetes incidence and mortality in Korean men and women. Diabetes Care. 2010;33(12):2567–2572. doi: 10.2337/dc10-0261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hur NW, Kim HC, Nam CM, Jee SH, Lee HC, Suh I. Smoking cessation and risk of type 2 diabetes mellitus: Korea Medical Insurance Corporation Study. Eur J Cardiovasc Prev Rehabil. 2007;14(2):244–249. doi: 10.1097/01.hjr.0000239474.41379.79. [DOI] [PubMed] [Google Scholar]
- 10.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Measuring the global burden of disease and risk factors, 1990-2001. In: Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ, editors. Global burden of disease and risk factors. Washington, DC: World Bank; 2006. pp. 1–13. [Google Scholar]
- 11.Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370(9589):765–773. doi: 10.1016/S0140-6736(07)61380-4. [DOI] [PubMed] [Google Scholar]
- 12.Rennard SI, Vestbo J. COPD: the dangerous underestimate of 15% Lancet. 2006;367(9518):1216–1219. doi: 10.1016/S0140-6736(06)68516-4. [DOI] [PubMed] [Google Scholar]
- 13.Korea Centers for Disease Control and Prevention. Korea health statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2) Seoul: Ministry of Health and Welfare; 2012. pp. 22–27.pp. 52–59. (Korean) [Google Scholar]
- 14.Jung-Choi KH, Khang YH, Cho HJ. Hidden female smokers in Asia: a comparison of self-reported with cotinine-verified smoking prevalence rates in representative national data from an Asian population. Tob Control. 2012;21(6):536–542. doi: 10.1136/tobaccocontrol-2011-050012. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention (CDC) Alcohol-attributable deaths and years of potential life lost--United States, 2001. MMWR Morb Mortal Wkly Rep. 2004;53(37):866–870. [PubMed] [Google Scholar]
- 16.O'Keefe JH, Bybee KA, Lavie CJ. Alcohol and cardiovascular health: the razor-sharp double-edged sword. J Am Coll Cardiol. 2007;50(11):1009–1014. doi: 10.1016/j.jacc.2007.04.089. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. Global status report on alcohol 2004. [cited 2013 Jul 1]. Available from: http://www.who.int/substance_abuse/publications/global_status_report_2004_overview.pdf.
- 18.Ariesen MJ, Claus SP, Rinkel GJ, Algra A. Risk factors for intracerebral hemorrhage in the general population: a systematic review. Stroke. 2003;34(8):2060–2065. doi: 10.1161/01.STR.0000080678.09344.8D. [DOI] [PubMed] [Google Scholar]
- 19.Sturgeon JD, Folsom AR, Longstreth WT, Jr, Shahar E, Rosamond WD, Cushman M. Risk factors for intracerebral hemorrhage in a pooled prospective study. Stroke. 2007;38(10):2718–2725. doi: 10.1161/STROKEAHA.107.487090. [DOI] [PubMed] [Google Scholar]
- 20.Bagnardi V, Blangiardo M, La Vecchia C, Corrao G. A meta-analysis of alcohol drinking and cancer risk. Br J Cancer. 2001;85(11):1700–1705. doi: 10.1054/bjoc.2001.2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Corrao G, Bagnardi V, Zambon A, La Vecchia C. A meta-analysis of alcohol consumption and the risk of 15 diseases. Prev Med. 2004;38(5):613–619. doi: 10.1016/j.ypmed.2003.11.027. [DOI] [PubMed] [Google Scholar]
- 22.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The alcohol use disorders identification test: guidelines for use in primary care 2001. [cited 2013 Jul 1]. Available from: http://whqlibdoc.who.int/hq/2001/who_msd_msb_01.6a.pdf.
- 23.Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368(9548):1681–1688. doi: 10.1016/S0140-6736(06)69703-1. [DOI] [PubMed] [Google Scholar]
- 24.Lim S, Shin H, Song JH, Kwak SH, Kang SM, Yoon JW, et al. Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and Nutrition Examination Survey for 1998-2007. Diabetes Care. 2011;34(6):1323–1328. doi: 10.2337/dc10-2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jung KW, Won YJ, Kong HJ, Oh CM, Seo HG, Lee JS. Cancer statistics in Korea: incidence, mortality, survival and prevalence in 2010. Cancer Res Treat. 2013;45(1):1–14. doi: 10.4143/crt.2013.45.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park JH, Lee KS, Choi KS. Burden of cancer in Korea during 2000-2020. Cancer Epidemiol. 2013;37(4):353–359. doi: 10.1016/j.canep.2013.03.015. [DOI] [PubMed] [Google Scholar]
- 27.Zammit C, Liddicoat H, Moonsie I, Makker H. Obesity and respiratory diseases. Int J Gen Med. 2010;3:335–343. doi: 10.2147/IJGM.S11926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization. Global strategy on diet, physical activity and health. [cited 2013 Jul 17]. Available from: http://www.who.int/dietphysicalactivity/factsheet_inactivity/en/index.html.
- 29.Sofi F, Capalbo A, Cesari F, Abbate R, Gensini GF. Physical activity during leisure time and primary prevention of coronary heart disease: an updated meta-analysis of cohort studies. Eur J Cardiovasc Prev Rehabil. 2008;15(3):247–257. doi: 10.1097/HJR.0b013e3282f232ac. [DOI] [PubMed] [Google Scholar]
- 30.Lee CD, Folsom AR, Blair SN. Physical activity and stroke risk: a meta-analysis. Stroke. 2003;34(10):2475–2481. doi: 10.1161/01.STR.0000091843.02517.9D. [DOI] [PubMed] [Google Scholar]
- 31.Thune I, Furberg AS. Physical activity and cancer risk: dose-response and cancer, all sites and site-specific. Med Sci Sports Exerc. 2001;33(6 Suppl):S530–S550. doi: 10.1097/00005768-200106001-00025. [DOI] [PubMed] [Google Scholar]
- 32.Lee IM, Skerrett PJ. Physical activity and all-cause mortality: what is the dose-response relation? Med Sci Sports Exerc. 2001;33(6 Suppl):S459–S471. doi: 10.1097/00005768-200106001-00016. [DOI] [PubMed] [Google Scholar]
- 33.Church T. Exercise in obesity, metabolic syndrome, and diabetes. Prog Cardiovasc Dis. 2011;53(6):412–418. doi: 10.1016/j.pcad.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 34.Oldridge NB. Economic burden of physical inactivity: healthcare costs associated with cardiovascular disease. Eur J Cardiovasc Prev Rehabil. 2008;15(2):130–139. doi: 10.1097/HJR.0b013e3282f19d42. [DOI] [PubMed] [Google Scholar]
- 35.Lee DH, Kim YM, Jekal Y, Park S, Kim KC, Naruse M, et al. Low levels of physical activity are associated with increased metabolic syndrome risk factors in korean adults. Diabetes Metab J. 2013;37(2):132–139. doi: 10.4093/dmj.2013.37.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jekal Y, Lee MK, Park S, Lee SH, Kim JY, Kang JU, et al. Association between obesity and physical fitness, and hemoglobin A1c level and metabolic syndrome in Korean adults. Korean Diabetes J. 2010;34(3):182–190. doi: 10.4093/kdj.2010.34.3.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Neaton JD, Wentworth DN, Cutler J, Stamler J, Kuller L Multiple Risk Factor Intervention Trial Research Group. Risk factors for death from different types of stroke. Ann Epidemiol. 1993;3(5):493–499. doi: 10.1016/1047-2797(93)90103-b. [DOI] [PubMed] [Google Scholar]
- 38.Giroud M, Creisson E, Fayolle H, André N, Becker F, Martin D, et al. Risk factors for primary cerebral hemorrhage: a population-based study--the Stroke Registry of Dijon. Neuroepidemiology. 1995;14(1):20–26. doi: 10.1159/000109775. [DOI] [PubMed] [Google Scholar]
- 39.Kannel WB. Framingham study insights into hypertensive risk of cardiovascular disease. Hypertens Res. 1995;18(3):181–196. doi: 10.1291/hypres.18.181. [DOI] [PubMed] [Google Scholar]
- 40.O'Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376(9735):112–123. doi: 10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- 41.Epstein M, Sowers JR. Diabetes mellitus and hypertension. Hypertension. 1992;19(5):403–418. doi: 10.1161/01.hyp.19.5.403. [DOI] [PubMed] [Google Scholar]
- 42.Chow WH, Gridley G, Fraumeni JF, Jr, Järvholm B. Obesity, hypertension, and the risk of kidney cancer in men. N Engl J Med. 2000;343(18):1305–1311. doi: 10.1056/NEJM200011023431804. [DOI] [PubMed] [Google Scholar]
- 43.Choi MY, Jee SH, Sull JW, Nam CM. The effect of hypertension on the risk for kidney cancer in Korean men. Kidney Int. 2005;67(2):647–652. doi: 10.1111/j.1523-1755.2005.67137.x. [DOI] [PubMed] [Google Scholar]
- 44.Lee SY, Kim MT, Jee SH, Im JS. Does hypertension increase mortality risk from lung cancer? A prospective cohort study on smoking, hypertension and lung cancer risk among Korean men. J Hypertens. 2002;20(4):617–622. doi: 10.1097/00004872-200204000-00017. [DOI] [PubMed] [Google Scholar]
- 45.Kim JS, Jones DW, Kim SJ, Hong YP. Hypertension in Korea: a national survey. Am J Prev Med. 1994;10(4):200–204. [PubMed] [Google Scholar]
- 46.Kim IS, Lee YH, Suh I, Oh HC, Oh DK, Kim SJ, et al. Korean nationwide blood pressure study. Yonsei Med J. 1982;23(1):15–25. doi: 10.3349/ymj.1982.23.1.15. [DOI] [PubMed] [Google Scholar]
- 47.Kannel WB. Lipids, diabetes, and coronary heart disease: insights from the Framingham Study. Am Heart J. 1985;110(5):1100–1107. doi: 10.1016/0002-8703(85)90224-8. [DOI] [PubMed] [Google Scholar]
- 48.Kitahara CM, Berrington de González A, Freedman ND, Huxley R, Mok Y, Jee SH, et al. Total cholesterol and cancer risk in a large prospective study in Korea. J Clin Oncol. 2011;29(12):1592–1598. doi: 10.1200/JCO.2010.31.5200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Freeman MR, Solomon KR. Cholesterol and prostate cancer. J Cell Biochem. 2004;91(1):54–69. doi: 10.1002/jcb.10724. [DOI] [PubMed] [Google Scholar]
- 50.Ha M, Sung J, Song YM. Serum total cholesterol and the risk of breast cancer in postmenopausal Korean women. Cancer Causes Control. 2009;20(7):1055–1060. doi: 10.1007/s10552-009-9301-7. [DOI] [PubMed] [Google Scholar]
- 51.Experience of an international collaborative group. Circulating cholesterol level and risk of death from cancer in men aged 40 to 69 years. JAMA. 1982;248(21):2853–2859. doi: 10.1001/jama.1982.03330210035031. [DOI] [PubMed] [Google Scholar]
- 52.Nomura AM, Stemmermann GN, Chyou PH. Prospective study of serum cholesterol levels and large-bowel cancer. J Natl Cancer Inst. 1991;83(19):1403–1407. doi: 10.1093/jnci/83.19.1403. [DOI] [PubMed] [Google Scholar]
- 53.Sorlie PD, Feinleib M. The serum cholesterol-cancer relationship: an analysis of time trends in the Framingham Study. J Natl Cancer Inst. 1982;69(5):989–996. [PubMed] [Google Scholar]
- 54.Williams RR, Sorlie PD, Feinleib M, McNamara PM, Kannel WB, Dawber TR. Cancer incidence by levels of cholesterol. JAMA. 1981;245(3):247–252. [PubMed] [Google Scholar]