Abstract
Obesity during childhood is a dominant risk factor for noncommunicable diseases (NCDs), and is itself considered a disease that needs to be treated. Recently, the growth in childhood obesity in Korea has become stagnant; however, two in every ten children are still overweight. In addition, 60% or more of overweight children have at least one metabolic syndrome risk factor. Thus, childhood obesity should be controlled through lifestyle modification. This paper reviews studies of the modifiable risk factors of obesity in Korean children. According to the life-course approach, preschool-aged children (<5 years) are influenced by their parents rather than individual habits because they are under mostly parental care. Elementary school-aged children (6 to 11 years) are affected by overlapping individual and parental effects. This may mean that the establishment of individual behavior patterns begins during this period. The conditions of poor eating habits such as skipping meals, eating out, and high fat intake, along with low physical activity, facilitate increased obesity among adolescents (12 to 18 years). Notably, adolescent girls show high rates of both underweight and obesity, which may lead to the development of NCDs in their offspring. Therefore, the problem of NCDs is no longer limited to adults, but is also prevalent among children. In addition, early intervention offers cost-effective opportunities for preventing NCDs. Thus, children need primary consideration, adequate monitoring, diagnosis, and treatment to reduce the burden of NCDs later in adulthood.
Keywords: Adolescents, Children, Noncommunicable diseases, Metabolic syndrome, Obesity
INTRODUCTION
Obesity is caused by multiple factors, including genetic, socio-economic, behavioral, and environmental factors, and it is, in turn, the dominant risk factor for noncommunicable diseases (NCDs). It is accepted as a disease needing to be treated like any other [1,2]. Environmental pollution, physical inactivity, an unbalanced diet, and excessive intake, along with dramatic societal growth, have contributed to creating an obesogenic environment [3]. This promotes an increase in NCDs among children or adolescents, despite their common onset in adulthood [2,4]. In Korea, NCDs were responsible for 82% of all deaths in 2008 [5], and the economic cost due to obesity was estimated to be 2.2 trillion won in 2003 [6].
Increasing evidence suggests that the development of obesity in childhood can continue into adulthood, and over one quarter of childhood obesity co-exists with metabolic syndrome (MetS) [1]. Additionally, being overweight or obese during childhood has long-term adverse effects on health [7]. Consequently, controlling obesity as early as possible to reduce the economic burden of NCDs is now the highest priority in public health [7,8]. To date, many studies internationally have reported several modifiable risk factors, but obesogenic environments differ by country. Thus, we review here the available literature on the prevalence estimation and modifiable risk factors for obesity or MetS, focusing on Korean children and adolescents.
SUBJECTS
Definition of Obesity and Metabolic Syndrome
Generally, obesity can be assessed using the body mass index (BMI) or percentage of the ideal body weight. Because children and adolescents are growing and developing, unlike adults, no fixed value of BMI is used to determine obesity. To establish the standard growth charts of Korean children and adolescents, surveys were conducted in 1997 and 2005 by the Korea Centers for Disease Control and Prevention and the Korean Pediatric Society (KPS). Currently, many studies use the 2007 Korean Children and Adolescents Growth Standard surveyed in 2005 to define obesity [9]. Although the terminology for different levels of weight or BMI varies, generally, a statistical definition of overweight and obesity is based on the 85th to 95th and greater than 95th percentile of age- and gender-specific BMI values for children aged 2 to 18 years, respectively [1,10]. As a percentage of ideal body weight, the KPS classified overweight as 10% to 20% of the ideal body weight, and obesity as 20% or greater, along with some additional subdivisions [1,10]. The BMI-based definition is used commonly due to its ease of estimation, but it has a limitation in terms of expression of body fat composition, so the meaning of obesity in such studies should be interpreted with caution.
A survey of the secular trend of body size allows the evaluation of socioeconomic changes. According to a 2005 survey, the BMI corresponding to the 85th and 95th percentiles increased by 1.5 kg/m2 and 1.9 kg/m2 in males, and 0.7 kg/m2 and 1.0 kg/m2 in females, respectively, compared to 1997 values. Overall, the average BMI also increased markedly among adolescents [8]. Moon [11] reported that the height and weight of children and adolescents in Korea had changed substantially during the last few decades. In children aged 7 years, the mean weight difference between 1965 and 1985 was 3.2 kg in males (19.1 kg in 1965, 22.3 kg in 1985) and 2.1 kg in females (19.1 kg in 1965, 21.2 kg in 1985). Over the next two decades, the mean weight increased by 4.5 kg in males (26.8 kg in 2005) and 4.3 kg in females (25.5 kg in 2005), respectively. In the short-term, this may have been influenced by the rapid economic growth and urbanization. Moreover, the trend towards a sedentary lifestyle and a westernized diet has increased. As young individuals continue to adopt these obesogenic environments, the risks of obesity starting from early life may contribute to earlier NCD onset.
MetS is commonly determined as the clustering of three or more of the following five cardiovascular disease (CVD) risk factors: abdominal obesity, hypertension, elevated fasting glucose, reduced high-density lipoprotein cholesterol (HDL-C) level, and hypertriglyceridemia [1]. However, pediatric MetS has not been well characterized because determining the cut-off pediatric percentile corresponding to the adult risk level is difficult. Consequently, various definitions of pediatric MetS have been used. Currently, the pediatric MetS definitions by Cook et al. [12] or de Ferranti et al. [13] based on the National Cholesterol Education Program Adult Treatment Panel III have been used widely, along with the definition by the International Diabetes Federation published in 2007 [14] (Table 1).
Table 1.
Metabolic syndrome criteria in children and adolescents
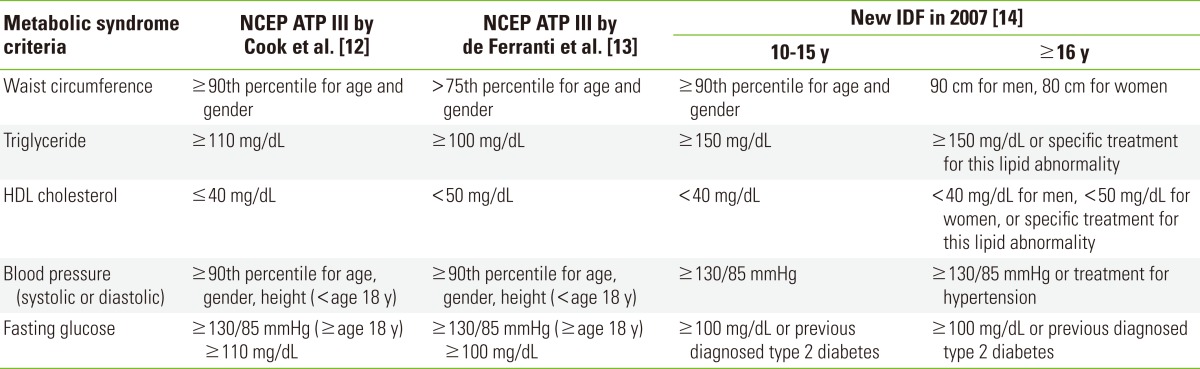
NCEP, National Cholesterol Education Program; ATP, Adult Treatment Panel; IDF, International Diabetes Federation; HDL, high-density lipoprotein.
Prevalence of Obesity and Metabolic Syndrome Among Overweight Children
Studies based on data from the Korean National Health and Nutrition Examination Survey showed that childhood obesity as defined by BMI almost doubled from 5.4% in 1998 to 11.4% in 2001, and then changed little from 2005 to 2011 (9.7% in 2005, 9.1% in 2007, and 9.7% in 2011) (Table 2). According to age group, the prevalence of obesity increased from 5.1% in 1997 to 6.3% in 2005 in preschool-aged children; school-aged children also showed a significant increase, particularly in middle and high school subjects (4.2% to 8.6% in children age 7 to 12 years, 7.3% to 14.8% in children aged 13 to 15 years, 8.9% to 17.5% in children aged 16 to 18 years, respectively). The increasing trend was most marked in males aged 13 to 18 years [8]. Although there were differences according to age group in the definition of pediatric MetS, the prevalence of MetS in children and adolescents across studies was in the range 2.3% to 9.2% (Table 3).
Table 2.
Prevalence of overweight and obesity among children aged 2 to 19 years in Korea
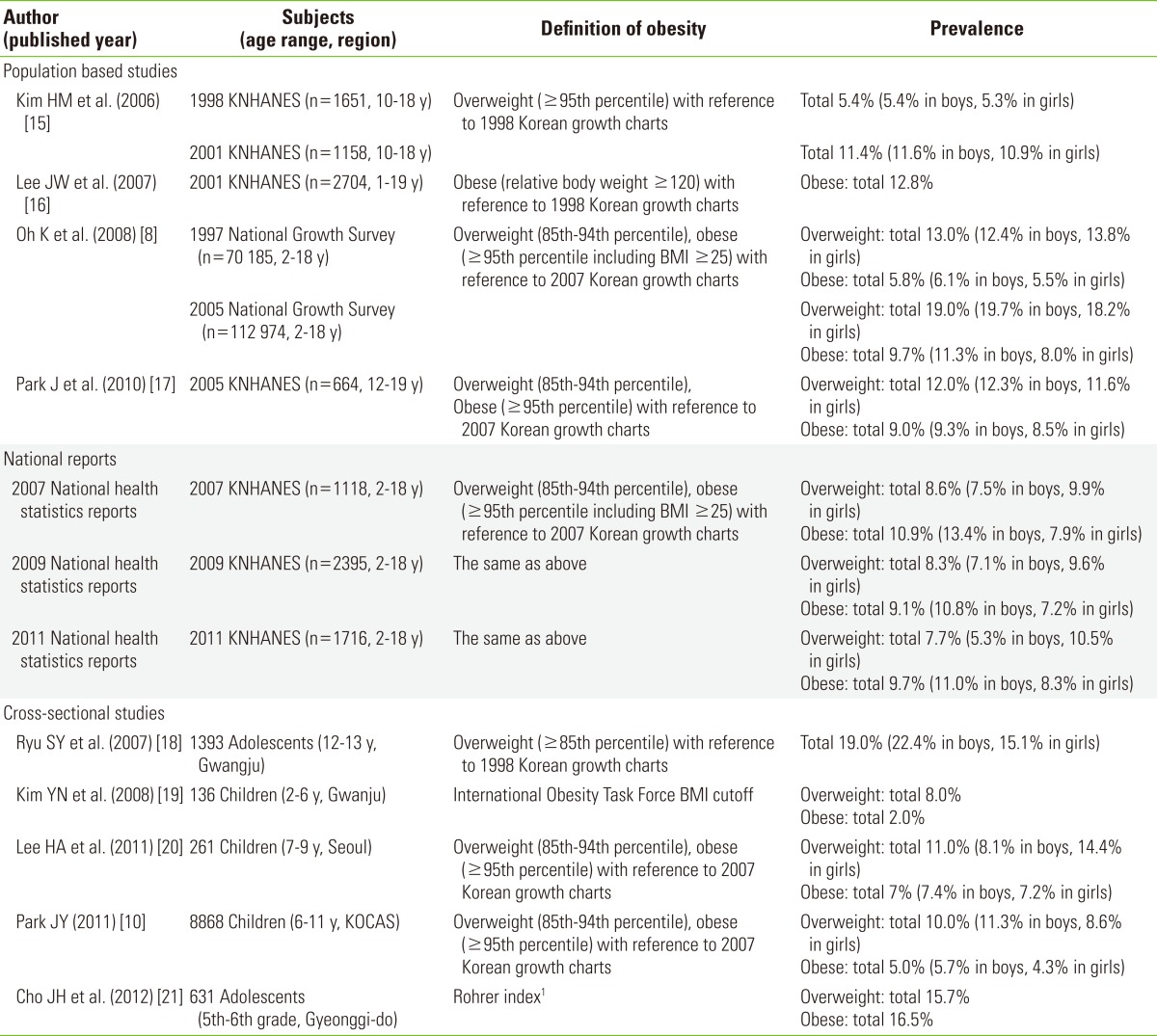
KNHANES, Korean National Health and Nutrition Examination Survey; BMI, body mass index; KoCAS, Korean Children and Adolescents Obesity Cohort Study.
1Rohrer index=[weight (kg)/height (cm3)]×107 Rohrer index values <140, 141-156, and >157 were categorized as normal, overweight, and obese, respectively.
Table 3.
Prevalence of MS in Korean children and risk of MetS among overweight or obese children
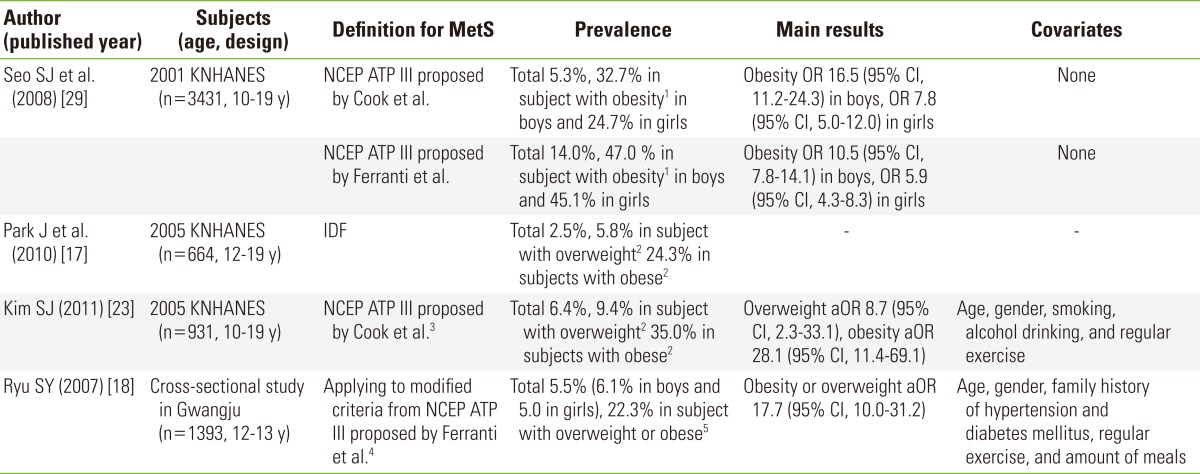
MetS, metabolic syndrome; KNHANES, Korean National Health and Nutrition Examination Survey; NCEP ATP III, National Cholesterol Education Program Adult Treatment Panel III; OR, odds ratio; CI, confidence interval; aOR, adjusted odds ratio; IDF, International Diabetes Federation.
1Obesity defined those who have a body weight of 20% or more over an individual's ideal body weight using 1998 Korean growth charts.
2Using 2007 Korean growth charts, those with a BMI ≥95th percentile for age and gender were classified as obese, and those with a BMI ≥85th but <95th percentile were classified as overweight.
3Blood pressure cut-off using National Heart, Lung, and Blood Institutes in the US.
4Of risk components, the criterion for abdominal obesity applied was waist circumference above the 70th percentile instead to waist circumference ≥75th percentile and the criteria applied for glucose was a glucose concentration of more than 110 instead of ≥100 mg/dL.
5Using 1998 Korean growth charts, overweight or obese was defined as a BMI≥85th percentile for age and gender.
Unlike adult obesity, childhood obesity is mediated by the number of fat cells and not simply an increase in their size [22]. Thus, obese children can regain weight easily after weight loss. Obesity in early life is associated with various CVD risk factors, including hypertension, dyslipidemia, and insulin resistance [15]. Among obese subjects, 24% to 35% of children had accompanying MetS [17,23] (Table 3), and 63.2% had at least one CVD risk factor [15]. Among the components of MetS, four risk components, the exception being hyperglycemia, are present more frequently in overweight than normal weight persons.
Other studies have also reported that BMI in early life may be associated with early menarche [24], deterioration of lung function, asthma [25], and CVD risk [26]. One longitudinal study showed that the risk of the highest carotid intima-media thickness at 25 years increased twofold per unit increase in BMI at 16 years of age in males (odds ratio [OR], 2.02; 95% confidence interval [CI], 1.21 to 3.35) [26], Thus, childhood obesity should be controlled, with particular emphasis on the need for intervention and management through lifestyle modification, rather than treatment with medication or surgery, due to the growth of the child.
Modifiable Risk Factors for Reducing Noncommunicable Disease in Children and Adolescents
Unhealthy diet and behaviors
Eating behavior is associated with the development of obesity. Secular trends in dietary intake indicated that the fat composition of calories has increased steadily since 1969 (7.2%), reaching 19.6% in a 2011 survey [27]. The 2011 National Health Statistic report showed that the rate of excessive intake based on the estimated energy requirement increased from 37.9% in 1998 to 42.3% in 2011, and this rate was noticeable in children aged 3 to 11 years. In contrast, the rate of excessive fat intake based on the acceptable macronutrient distribution range was higher in the adolescents than the other age groups (10.4% in children aged 3 to 5 years, 10.3% in children aged 6 to 11 years, and 17.9% in children aged 12 to 18 years, respectively) [27]. A study conducted in Gwangju by Kim et al. [19] reported similar results, while a study of the data from the 4th KNHANES showed that 32.7% of infants had a high carbohydrate intake [28]. The consumption of too much carbohydrate and fat causes obesity. The nutritional composition of a meal is important, but the individual variation in energy requirements is considerable; thus, there were some limitations to the research. Additionally, several recent studies have revealed that the intake of micronutrients such as vitamin D is associated with obesity; however, evidence supporting the causal relationship is insufficient.
The frequency of eating out and intake of precooked/frozen products is increasing in accordance with the growing number of women in the workforce and the expanding market of food products available. During the period of the 2008-2011 KNHANES, the proportion of those who ate out once or more daily increased from 24.2% to 28.2%; this was most pronounced in the high socio-economic subgroup. This proportion was also higher among teenagers compared to other age groups (eating out once or more, 40%; and twice or more, 19%) [27]. Eating out, overeating, rapid intake, and fewer family meals may be related to the total caloric intake. In a study of one elementary school, those who engaged in overeating more than twice per week, ate rapidly, and had fewer family meals had a greater risk of being overweight (OR, 3.1; 95% CI, 1.4 to 6.9; OR, 3.3; 95% CI, 1.7 to 6.4; and OR, 9.5; 95% CI, 1.2 to 74.8; respectively) [20] (Tables 4 and 5). As a part of that study, Kong et al. [34] reported that those who ate one or more precooked/frozen meals per day had an eightfold greater risk of clustering of MetS (Table 5). Both the preference for food and eating behavior establishment start at a much younger age, and can be maintained into adulthood. Moreover, parental behaviors influence the quantity and quality of their offspring's nutritional status [35]. Eating a meal with a parent increases the tendency to have a high quality meal and can also directly guide the eating behavior of the child.
Table 4.
Review of studies for modifiable risk factors of obesity focused on Korean children
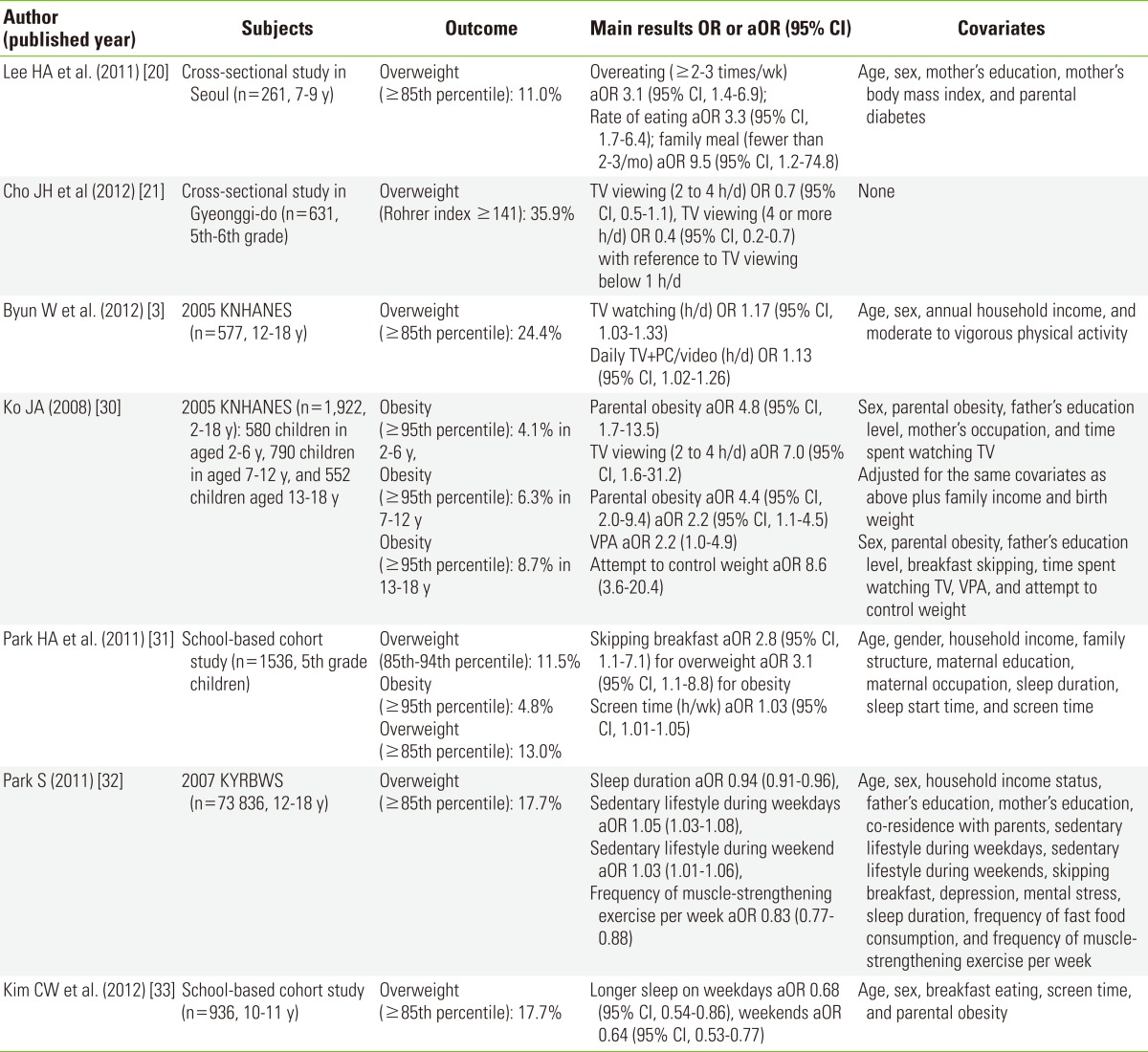
OR, odds ratio; aOR, adjusted odds ratio; CI, confidence interval; VPA, vigorous physical activity; KNHANES, Korean National Health and Nutrition Examination Survey; KYRBWS, Korea Youth Risk Behavior Web-based Survey.
Table 5.
Summary of modifiable risk factors based on studies conducted in Korea for preventing the development of obesity or metabolic syndrome
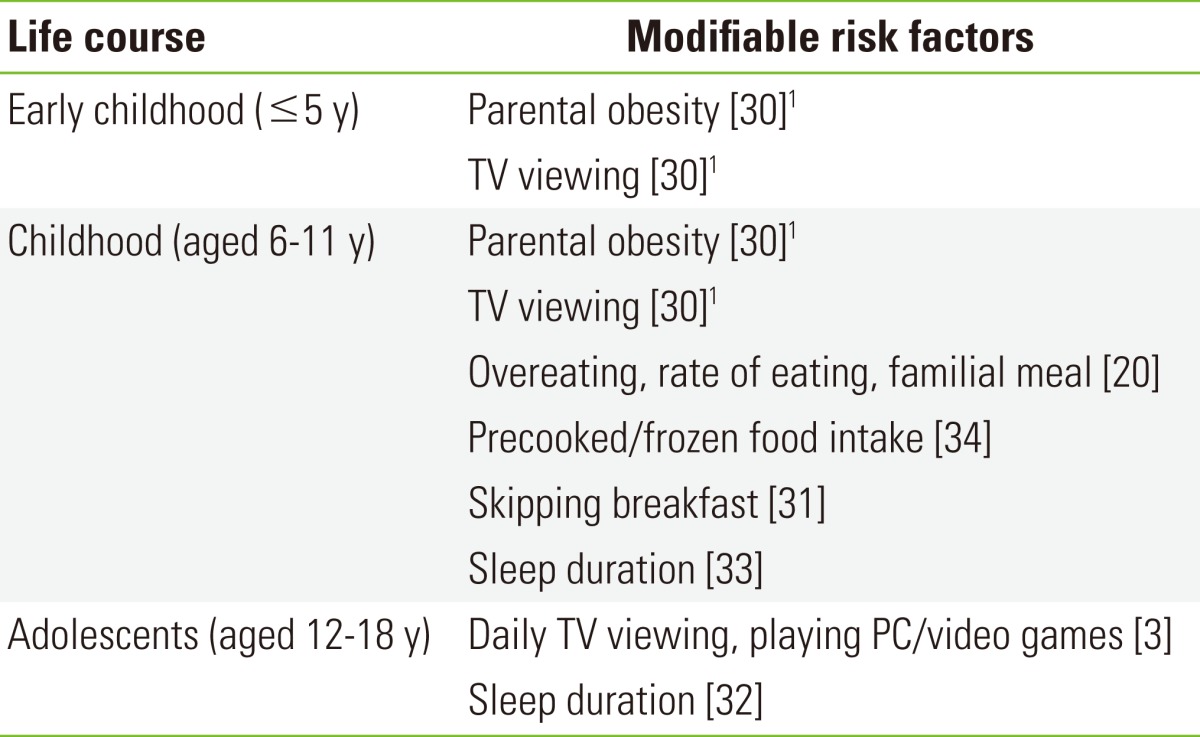
1The study conducted by Ko [30] classified subjects as follows: children aged 2 to 6 years, 7 to 12 years, and 13 to 18 years.
Currently, regular breakfast is becoming important for the prevention of obesity. Because skipping breakfast is related to the increased intake of snacks and calories in subsequent meals, the guidelines for children and adolescents published by the Ministry of Health and Welfare include a regular breakfast [36]. In a study of 1536 fifth-grade elementary school students, the prevalence of being overweight in the skip-breakfast group was 19.6%, which was significantly higher than the daily breakfast intake group (14.9%, p=0.01) [31] (Tables 4 and 5). However, breakfast is dependent on individual lifestyle and environment and is difficult to research due to the subjective definition of skipping breakfast [36].
Sedentary lifestyle and physical inactivity
Obesity is known to occur as a result of an imbalance between energy intake and energy expenditure. Environments with increased availability of energy-dense foods and fewer opportunities for physical activities contribute to increased obesity. Screen-based behaviors, such as watching TV and playing computer/video games, offer fewer opportunities for physical activity for energy expenditure, and prolonged TV watching may lead to eating more snacks or high calorie foods due to viewing commercial advertisements.
Data from 1033 Korean adolescents aged 12 to 18 years from the 2005 KNHANES were used to estimate the proportion of sedentary behaviors. The average time spent watching TV and playing PC/video games was 4.2 h/d for males and 4.0 h/d for females. The data indicated that Korean adolescents spent about 33% more time compared to their American counterparts, represented by American adolescents aged 12 to 19 years in the 99-04 NHANES (3.1 h/d in males and 2.3 h/d in females) [37]. A recent study of elementary school children in Seoul found that 58.7% spent more than 2 hours per day watching TV [38]. The American Academy of Pediatrics recommends that children and adolescents be limited to less than 2 hours per day of screen-based sedentary behaviors [39], but Korean adolescents spent an average of 4 or more hours per day on sedentary activity. Males spent more time playing games, while girls spent more time watching TV, which decreased with increasing age. Those who watched TV for an additional hour had a 17% risk of being overweight (95% CI, 1.0 to 1.3), and 27% risk of both abdominal obesity and low HDL-C (≤35 mg/dL) (95% CI, 1.0 to 1.5; 95% CI, 1.1 to 1.5; respectively). Moreover, an additional hour spent playing PC/video games was significantly associated with the risk of abdominal obesity (OR, 1.2; 95% CI, 1.0 to 1.4) [3] (Tables 4 and 5). However, among preadolescent children, some studies failed to detect a relationship between TV viewing and overweight [20] (Tables 4 and 5) or clustering of MetS components [34] (Table 5). Indeed, Cho et al. [21] reported an inverse association (Table 4). The increasing prevalence of smart phone ownership will likely contribute to prolonging the time spent on screen-based sedentary behaviors.
According to the 2011 KNHANES, the total proportion of regular moderate physical activities was 30.9% (43.1% in males, 16.6% in females), and this rate declined among high school adolescents [27]. It seems that Korean adolescents in high school spend a significant amount of time studying. The 2005 KNHANES showed that the time spent in weekly physical activity was higher for males than females, and the time spent in weekly vigorous physical activity was twofold higher in males than in females (936.5 vs. 484.5 min/wk, respectively, p<0.001) [3] (Tables 4 and 5). However, studies of physical inactivity have not shown consistent results. In this regard, one study suggested that physical inactivity appeared to be the result of obesity rather than its cause [40]. In addition, the measurement error has been challenged in related studies.
Sleep duration
Some recent studies have reported that both excessive and insufficient sleep duration are linked to the development of obesity. One potential mechanism is related to the regulation of appetite by the hypothalamus; thus inappropriate sleep seems to influence appetite and energy metabolism [41]. In Korea, the average sleep duration among adolescents is 7.2 hours; sleep duration in high school adolescents was 1 hour less than in middle school adolescents (7.8 hours for 12 to 14 years, 6.8 hours for 15 to 18 years) [27]. About 0.4% of middle school students and 18% of high school students reported sleeping less than 6 hour per night. One study using data from the 2007 Korea Youth Risk Behavior Web-based Survey (KYRBWS) revealed that the BMI tended to decrease with increasing sleep duration and showed a preventive effect against obesity (OR, 0.94; 95% CI, 0.91 to 0.96) [32] (Tables 4 and 5). Another school-based cohort study reported that longer sleep on weekdays and weekends showed about 30% reduction in the risk of being overweight in childhood (OR, 0.64; 95% CI, 0.53 to 0.77; OR, 0.68; 95% CI, 0.54 to 0.86; respectively) [33] (Tables 4 and 5). However, further studies are required to confirm the biological mechanism in children.
Other factors
Parental obesity has been suggested to be the dominant predictor of child obesity. Using the 3rd KNHANES, Ko [30] found that parental obesity was significantly associated with a 4.8-fold increased risk of obesity in children aged 2 to 6 years, and 4.4-fold increased risk in children aged 7 to 12 years (Tables 4 and 5). Parents' obesity can affect their offspring through not only genetic factors but also the environment created by parental behaviors; thus some studies have suggested the need for family-based intervention to control childhood obesity.
Since the hypothesis of fetal origin of adult disease was suggested by Barker, evidence from various countries has accumulated [42], revealing that small size at birth is associated with NCDs; moreover, some diseases exhibit a U-shaped relationship with birth weight. Inappropriate birth weight can be a result of an unhealthy intrauterine environment, and the after-birth growth rate in response to the environment is also a potential risk factor for NCDs. One study of 660 middle school students showed that those in the low-birth-weight groups had a high insulin concentration and the homeostasis model assessment index compared to others [43], but not all [44]. In addition, one cohort study reported that accelerated growth is associated with systolic blood pressure at 3 years of age [45]. However, the assessment of growth rate since birth is difficult without collection of data at regular follow-ups. For this reason, evidence regarding the relationships between birth data or growth status and NCDs is sparse.
National Efforts for Mediation
Interventions aimed at reducing the burden of NCDs can be useful and effective and can be applied at the level of policy and legislation, as well as in schools, families, and communities. In Korea, limiting the access of young people to tobacco, alcohol, and unhealthy food products around schools through legal and school-level health-promotion programs are in the development and testing stage. Although participation is optional, community-based physical activity programs under national certification are at present operating [46].
Since 2009, in accordance with the enforcement of the Special Act on Safety Management of Children's Dietary Life, stores around schools in Korea have been restricted in terms of the sale of high-calorie, low-nutrition food items, along with formation of a green food zone. In addition, as a part of a comprehensive plan for student health and promotion established by the Ministry of Education, Science and Technology, the restriction of soft-drink sales, labeling of nutritional information for school meals, and enhancement of regular physical activity participation are being carried out.
Recently, the Korean Food and Drug Administration developed an educational program for healthy eating and supported piloting of the program in select experimental schools beginning in 2011. Both nutrition knowledge and dietary behavior scores were significantly improved in all of the subjects [47]. Another study conducted an intervention, which comprised both nutrition education and physical activity and targeted fourth-grade children for 3 months, resulted in significant improvements in the density of micronutrients such as potassium, vitamin A, and niacin, and significant decreases in waist-hip ratio and body fat mass [48]. However, this study is still in the preliminary stage, and further studies are needed to support the efficacy of nutrition education.
Needs for Further Consideration
To prevent the development of obesity or related diseases, efforts toward weight control may be necessary for those who are overweight. However, unhealthy weight control behaviors, such as fasting and an unbalanced diet, may be harmful, particularly for females of childbearing age. In a survey performed in the 2011 KNHANES, the prevalence of underweight females aged 19 to 29 years was 21%, which was the highest of all age groups [27]. In a study derived from the 2nd KYRBWS, 26.5% of adolescents were found to be underweight and 26.6% of subjects responded that their body image was fat [49]. Extreme diets among adolescent girls can influence their reproductive health. Therefore, it seems necessary to mediate excessive weight control.
Obesity may also lead to the development of psychological problems, including low self-esteem, a sense of inferiority, and depression [21,22]. Due to a cultural preference for a slim body, dissatisfaction with body image leads to emotional instability. Mental health is becoming a critical issue among teenagers in Korea. Thus, the intervention program for weight regulation should include mental health counseling.
CONCLUSION
In the late 1990s and early 2000s, the prevalence of childhood obesity showed a dramatic increase, and then leveled off; however, two out of ten children are still overweight. In addition, 60% or more of overweight children have at least one factor of MetS. The primary NCD alliance [4] and the World Health Assembly and World Health Organization [50] insist that children need primary consideration in the context of NCDs, and that adequate monitoring, diagnosis, and treatment are essential for children [2]. Starting action in the early stage of life offers cost-effective opportunities for preventing NCDs, and children as peer educators are susceptible to change through intervention. Notably, adolescent girls showed high rates of both low weight and obesity. Maternal pre-pregnancy BMI is independently related to the development of NCDs in their offspring, and it may lead to a vicious circle. Thus, information that may enhance their child's future health should be provided to women of childbearing age.
Therefore, the problem of NCDs is no longer limited to adults. Strategies for preventing NCDs must also consider children, for several reasons. First, a wide range of NCDs and predisposing risk factors have been identified in children. Second, children are vulnerable to the same risk factors that affect adults. Finally, childhood offers opportunities for cost-effective prevention of NCDs.
Footnotes
The authors have no conflicts of interest with the material presented in this paper.
References
- 1.Chu MA, Choe BH. Obesity and metabolic syndrome among children and adolescents in Korea. J Korean Med Assoc. 2010;53(2):142–152. (Korean) [Google Scholar]
- 2.AstraZeneca Young Health Programme. Non-communicable diseases and adolescents: an opportunity for action. 2011. [cited 2013 Jul 10]. Available from: http://www.jhsph.edu/bin/g/q/noncommunicable.pdf.
- 3.Byun W, Dowda M, Pate RR. Associations between screen-based sedentary behavior and cardiovascular disease risk factors in Korean youth. J Korean Med Sci. 2012;27(4):388–394. doi: 10.3346/jkms.2012.27.4.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.NCD Alliance. A focus on children and non-communicable diseases (NCDs) 2011. [cited 2013 Jul 10]. Available from: http://ncdalliance.org/sites/default/files/resource_files/20110627_A_Focus_on_Children_&_NCDs_FINAL_2.pdf.
- 5.World Health Organization. NCD country profiles: Republic of Korea. 2011. [cited 2013 Jul 10]. Available from: http://www.who.int/nmh/countries/kor_en.pdf.
- 6.Jung YH. Determinant of health in Korea. Seoul: Korea Institute for Health and Social Affairs; 2006. p. 19. (Korean) [Google Scholar]
- 7.Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360(9331):473–482. doi: 10.1016/S0140-6736(02)09678-2. [DOI] [PubMed] [Google Scholar]
- 8.Oh K, Jang MJ, Lee NY, Moon JS, Lee CG, Yoo MH, et al. Prevalence and trends in obesity among Korean children and adolescents in 1997 and 2005. Korean J Pediatr. 2008;51(9):950–955. [Google Scholar]
- 9.Korea Center for Disease Control and Prevention. 2007 Korean Children and Adolescents Growth Standard. Korean Pediatric Society; 2008. [cited 2013 Jul 10]. Available from: http://www.cdc.go.kr/CDC/notice/CdcKrInfo0301.jsp?menuIds=HOME001-MNU0004-MNU0036-MNU0037&cid=12103 (Korean) [Google Scholar]
- 10.Park JY. Prevalence of overweight and obesity in Korean children: the results of Korean children-adolescent cohort study, 2005-2010. Public Health Wkly Rep. 2011;4(47):857–862. (Korean) [Google Scholar]
- 11.Moon JS. Secular trends of body sizes in Korean children and adolescents: from 1965 to 2010. Korean J Pediatr. 2011;54(11):436–442. doi: 10.3345/kjp.2011.54.11.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 2003;157(8):821–827. doi: 10.1001/archpedi.157.8.821. [DOI] [PubMed] [Google Scholar]
- 13.De Ferranti SD, Gauvreau K, Ludwig DS, Neufeld EJ, Newburger JW, Rifai N. Prevalence of the metabolic syndrome in American adolescents: findings from the Third National Health and Nutrition Examination Survey. Circulation. 2004;110(16):2494–2497. doi: 10.1161/01.CIR.0000145117.40114.C7. [DOI] [PubMed] [Google Scholar]
- 14.Zimmet P, Alberti KG, Kaufman F, Tajima N, Silink M, Arslanian S, et al. The metabolic syndrome in children and adolescents: an IDF consensus report. Pediatr Diabetes. 2007;8(5):299–306. doi: 10.1111/j.1399-5448.2007.00271.x. [DOI] [PubMed] [Google Scholar]
- 15.Kim HM, Park J, Kim HS, Kim DH, Park SH. Obesity and cardiovascular risk factors in Korean children and adolescents aged 10-18 years from the Korean National Health and Nutrition Examination Survey, 1998 and 2001. Am J Epidemiol. 2006;164(8):787–793. doi: 10.1093/aje/kwj251. [DOI] [PubMed] [Google Scholar]
- 16.Lee JW, Hwang J, Cho HS. Dietary patterns of children and adolescents analyzed from 2001 Korea National Health and Nutrition Survey. Nutr Res Pract. 2007;1(2):84–88. doi: 10.4162/nrp.2007.1.2.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Park J, Hilmers DC, Mendoza JA, Stuff JE, Liu Y, Nicklas TA. Prevalence of metabolic syndrome and obesity in adolescents aged 12 to 19 years: comparison between the United States and Korea. J Korean Med Sci. 2010;25(1):75–82. doi: 10.3346/jkms.2010.25.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ryu SY, Kweon SS, Park HC, Shin JH, Rhee JA. Obesity and the metabolic syndrome in Korean adolescents. J Korean Med Sci. 2007;22(3):513–517. doi: 10.3346/jkms.2007.22.3.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim YN, Cho YO, Driskell JA. Anthropometric indices and selected nutrient intakes of young children in Kwangju, Korea. Nutr Res Pract. 2008;2(3):178–183. doi: 10.4162/nrp.2008.2.3.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee HA, Lee WK, Kong KA, Chang N, Ha EH, Hong YS, et al. The effect of eating behavior on being overweight or obese during preadolescence. J Prev Med Public Health. 2011;44(5):226–233. doi: 10.3961/jpmph.2011.44.5.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cho JH, Han SN, Kim JH, Lee HM. Body image distortion in fifth and sixth grade students may lead to stress, depression, and undesirable dieting behavior. Nutr Res Pract. 2012;6(2):175–181. doi: 10.4162/nrp.2012.6.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moon YI, Park HR, Koo HY, Kim HS. Effects of behavior modification on body image, depression and body fat in obese Korean elementary school children. Yonsei Med J. 2004;45(1):61–67. doi: 10.3349/ymj.2004.45.1.61. [DOI] [PubMed] [Google Scholar]
- 23.Kim SJ, Lee J, Nam CM, Lee SY. Impact of obesity on metabolic syndrome among adolescents as compared with adults in Korea. Yonsei Med J. 2011;52(5):746–752. doi: 10.3349/ymj.2011.52.5.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oh CM, Oh IH, Choi KS, Choe BK, Yoon TY, Choi JM. Relationship between body mass index and early menarche of adolescent girls in Seoul. J Prev Med Public Health. 2012;45(4):227–234. doi: 10.3961/jpmph.2012.45.4.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jeong Y, Jung-Choi K, Lee JH, Lee HY, Park EA, Kim YJ, et al. Body weight at birth and at age three and respiratory illness in preschool children. J Prev Med Public Health. 2010;43(5):369–376. doi: 10.3961/jpmph.2010.43.5.369. [DOI] [PubMed] [Google Scholar]
- 26.Lee YJ, Nam CM, Kim HC, Hur NW, Suh I. The association between obesity indices in adolescence and carotid intima-media thickness in young adults: Kangwha Study. J Prev Med Public Health. 2008;41(2):107–114. doi: 10.3961/jpmph.2008.41.2.107. (Korean) [DOI] [PubMed] [Google Scholar]
- 27.Ministry of Health and Welfare; Korea Center for Disease Control and Prevention. Korea health statistics 2011: Korea Health and Nutrition Examination Survey (KNHANES V-2) 2012. [cited 2013 Jul 10]. Available from: http://www.bokjiro.go.kr/cmm/fms/FileDown.do?atchFileId=5951033&fileSn=12872.0KB (Korean)
- 28.Kim YH, Lee SG, Kim SH, Song YJ, Chung JY, Park MJ. Nutritional status of Korean toddlers: from the Korean National Health and Nutrition Examination Survey 2007-2009. Korean J Pediatr Gastroenterol Nutr. 2011;14(2):161–170. (Korean) [Google Scholar]
- 29.Seo SJ, Lee HY, Lee SW. The prevalence of the metabolic syndrome in Korean children and adolescents: comparisons of the criteria of Cook et al., Cruz and Goran, and ferranti et al. Yonsei Med J. 2008;49(4):563–572. doi: 10.3349/ymj.2008.49.4.563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ko JA. Childhood obesity and familial environmental factor according to the developmental stages: the Korea NHANES Study. J Korean Acad Fam Med. 2008;29(12):939–947. [Google Scholar]
- 31.Park HA, Kang JH, Kim KW, Cho YG, Hur YI, Kim OH. Breakfast skipping, related factors, and nutrients intake of 5th grade students. Korean J Fam Med. 2011;32(1):11–20. (Korean) [Google Scholar]
- 32.Park S. Association between short sleep duration and obesity among South korean adolescents. West J Nurs Res. 2011;33(2):207–223. doi: 10.1177/0193945910371317. [DOI] [PubMed] [Google Scholar]
- 33.Kim CW, Choi MK, Im HJ, Kim OH, Lee HJ, Song J, et al. Weekend catch-up sleep is associated with decreased risk of being overweight among fifth-grade students with short sleep duration. J Sleep Res. 2012;21(5):546–551. doi: 10.1111/j.1365-2869.2012.01013.x. [DOI] [PubMed] [Google Scholar]
- 34.Kong KA, Park BH, Min JW, Hong J, Hong YS, Lee BE, et al. Clustering of metabolic risk factors and its related risk factors in young schoolchildren. J Prev Med Public Health. 2006;39(3):235–242. (Korean) [PubMed] [Google Scholar]
- 35.Park JS, Lee JH. Elementary school children's intake patterns of health functional foods and parent's requirements in Daejeon area. Korean J Community Nutr. 2008;13(4):463–475. (Korean) [Google Scholar]
- 36.Park KY. Breakfast and health in adolescents. Korean J Pediatr Gastroenterol Nutr. 2011;14(4):340–349. (Korean) [Google Scholar]
- 37.Mark AE, Janssen I. Relationship between screen time and metabolic syndrome in adolescents. J Public Health (Oxf) 2008;30(2):153–160. doi: 10.1093/pubmed/fdn022. [DOI] [PubMed] [Google Scholar]
- 38.Ha A. Obesity and its association with diets and sedentary life style among school children in Seoul, Korea: compliance with dietary references intakes for Koreans food guides. Nutr Res Pract. 2007;1(3):212–217. doi: 10.4162/nrp.2007.1.3.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.American Academy of Pediatrics; Committee on Public Education. American Academy of Pediatrics: children, adolescents, and television. Pediatrics. 2001;107(2):423–426. doi: 10.1542/peds.107.2.423. [DOI] [PubMed] [Google Scholar]
- 40.Metcalf BS, Hosking J, Jeffery AN, Voss LD, Henley W, Wilkin TJ. Fatness leads to inactivity, but inactivity does not lead to fatness: a longitudinal study in children (EarlyBird 45) Arch Dis Child. 2011;96(10):942–947. doi: 10.1136/adc.2009.175927. [DOI] [PubMed] [Google Scholar]
- 41.Prinz P. Sleep, appetite, and obesity: what is the link? PLoS Med. 2004;1(3):e61. doi: 10.1371/journal.pmed.0010061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Calkins K, Devaskar SU. Fetal origins of adult disease. Curr Probl Pediatr Adolesc Health Care. 2011;41(6):158–176. doi: 10.1016/j.cppeds.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim CS, Park JS, Park J, Nam JS, Kang ES, Ahn CW, et al. The relation between birth weight and insulin resistance in Korean adolescents. Yonsei Med J. 2006;47(1):85–92. doi: 10.3349/ymj.2006.47.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kong KA, Lee HA, Park BH, Seo JW, Oh JY, Chang N, et al. Relationships of birth weight and postnatal growth with metabolic risk factors in junior school children. Curr Hypertens Rev. 2011;7:153–159. [Google Scholar]
- 45.Min J, Kim YJ, Lee H, Park EA, Cho SJ, Hong YM, et al. Is the association between ACE genes and blood pressure mediated by postnatal growth during the first 3 years? Early Hum Dev. 2012;88(6):425–429. doi: 10.1016/j.earlhumdev.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 46.National Youth Policy Institute. 2009 A study on the obesity situation of youth and children and policy measures. [cited 2013 Jul 10]. Available from: http://lib.nypi.re.kr/pdfs/2009/14.pdf (Korean)
- 47.Ministry of Food and Drug Safety. Evaluation of a nutrition education program for elementary school children. 2013. [cited 2013 Jul 10]. Available from: http://www.mfds.go.kr/index.do?mid=56&cmd=v&seq=19569 (Korean)
- 48.Lee JW, Lee HS, Chang N, Kim JM. The Relationship between nutrition knowledge scores and dietary behavior, dietary intakes and anthropometric parameters among primary school children participating in a nutrition education program. Korean J Nutr. 2009;42(4):338–349. (Korean) [Google Scholar]
- 49.Park E. A comparative study of youth health risk behaviors by region: focused on metropolitan areas, medium sized and small city areas, and rural areas. J Korean Acad Nurs. 2010;40(1):14–23. doi: 10.4040/jkan.2010.40.1.14. (Korean) [DOI] [PubMed] [Google Scholar]
- 50.World Health Organization. Development of an updated action plan for the global strategy for the prevention and control noncommunicable diseases covering the period 2013 to 2020. Geneva: World Health Organization; 2012. p. 5.p. 21. [Google Scholar]


