Abstract
Epithelial cell polarization and integration are essential to their function and loss of epithelial polarity and tissue architecture correlates with the development of aggressive tumors. Erbin is a basolateral membrane-associated protein. The roles of Erbin in establishing cell polarization and regulating cell adhesion have been suggested. Erbin is also a negative regulator in Ras-Raf-ERK (extracellular signal-regulated kinase) signaling pathway. However, the potential functions of Erbin in human cancer are basically unknown. In the present study, we show, for the first time, that loss of Erbin endows cervical cancer cells with resistance to anoikis both in vitro and in vivo and promotes the growth and metastasis of human cervical cancer xenografts in nude mice. We found that knockdown of Erbin induced the phosphorylation, nuclear translocation and transcriptional activities of signal transducer and activator of transcription factor 3 (STAT3) in cervical cancer cells. Overexpression of STAT3C or induction of endogenous STAT3 activation by interleukin (IL)-6 evidently inhibited anoikis of cervical cancer cells, whereas WP1066, a potent inhibitor of Janus-activated kinase 2 (Jak2)/STAT3, effectively blocked the effect of Erbin knockdown on cell survival under anchorage-independent conditions, indicating that loss of Erbin confers resistance of cervical cancer cells to anoikis in a STAT3-dependent manner. Interestingly, IL-6 induced STAT3 activation and Erbin expression simultaneously. Overexpression of STAT3C also significantly upregulated the level of Erbin, whereas the Jak2 inhibitor AG490 remarkably blocked not only STAT3 phosphorylation but also IL-6-induced Erbin expression. Knockdown of Erbin augmented the effects of IL-6 on STAT3 activation and anoikis resistance. In addition, by immunohistochemical analysis of Erbin expression, we demonstrate that the expression of Erbin is significantly decreased or even lost in cervical cancer tissues. These data reveal that Erbin is a novel negative regulator of STAT3, and the IL-6/STAT3/Erbin loop has a crucial role in cervical cancer progression and metastasis.
Keywords: Erbin, STAT3, IL-6, cervical cancer, anoikis, metastasis
Introduction
Erbin is the founding member of the leucine-rich repeat and PDZ (PSD-95/DLG/ZO-1) domain (LAP) protein family.1, 2 The known LAP protein family includes four mammalian proteins hScrib, Erbin, Densin-180 and Lano, one Drosophila melanogaster protein Scribble and one Caenorhabditis elegans protein LET-413.3, 4, 5, 6 LAP proteins are generally localized at the basolateral membrane or associated with lateral junctions in polarized epithelial cells of worms, flies and humans. The functions of LAP proteins in establishment of cell polarity and maintenance of epithelial cell integration have been discovered.5, 7, 8 Mutation of LET-413 results in the absence of adherens junctions and disruption of epithelial integrity.9 Similar characteristics are identified in Drosophila melanogaster Scribble mutant. Depletion of mammalian Scribble leads to the loss of intracellular adhesion and cell migratory directionality.10 Erbin, a human homologue of LET-413, is localized basolaterally and proposed as a mediator of basolateral trafficking. The binding partners of Erbin are mainly the components of adherens junctions and proteins involved in cell attachment to substrates, indicating that Erbin has an important role in cell polarization.11, 12
Numerous studies suggest that the LAP family may act as scaffolding molecules for organizing signal transduction proteins into complexes and orienting signaling molecules to physical or functional interfaces.13, 14, 15 Erbin interacts with scaffold protein Sur-8 and disrupts the Sur-8–Ras–Raf interaction, inhibiting the Ras-mediated activation of the mitogen-activated protein kinase.16, 17, 18 Our recent study also indicates that Erbin may be a double modulator in extracellular signal-regulated kinase (ERK) signaling pathway, because Erbin mediates catecholamine-induced β2-AR/Her2 complexation and promotes catecholamine-induced activation of ERK signaling in cardiomyocytes.19 The leucine-rich repeat domain of Erbin mediates the interaction of Erbin with Nod2 and inhibits Nod2-dependent activation of nuclear factor κB.20, 21 Erbin is also considered as a negative modulator of transforming growth factor-β signaling by blocking oligomerization of Smad2/Smad3 with Smad4.22, 23 During the past few years, the findings reveal that the regulatory roles of Erbin in signal transduction have become increasingly complex. The functions of Erbin in diverse signaling events are far from understood.
Apical/basal polarization and integration of epithelial cells are essential to their function and the loss of epithelial polarity and tissue architecture correlates with the development of aggressive tumors, raising the possibility that cell proliferation and polarity can be functionally coupled.24 Several members of LAP family have been considered as tumor suppressors.25, 26, 27 However, there is little information regarding the expression and distribution patterns of Erbin in human tumor tissues in the literatures. The potential functions of Erbin in human cancer are basically unknown.
In this study, we demonstrate that the expression of Erbin is significantly decreased or even lost in cervical cancer tissues. Loss of Erbin induces the phosphorylation of signal transducer and activator of transcription factor 3 (STAT3), endows cervical cancer cells with resistance to anoikis both in vitro and in vivo and promotes the growth and metastasis of human cervical cancer xenografts in nude mice. Our data suggest that Erbin may act as a key regulator of cancer progression by inhibiting STAT3 activation.
Results
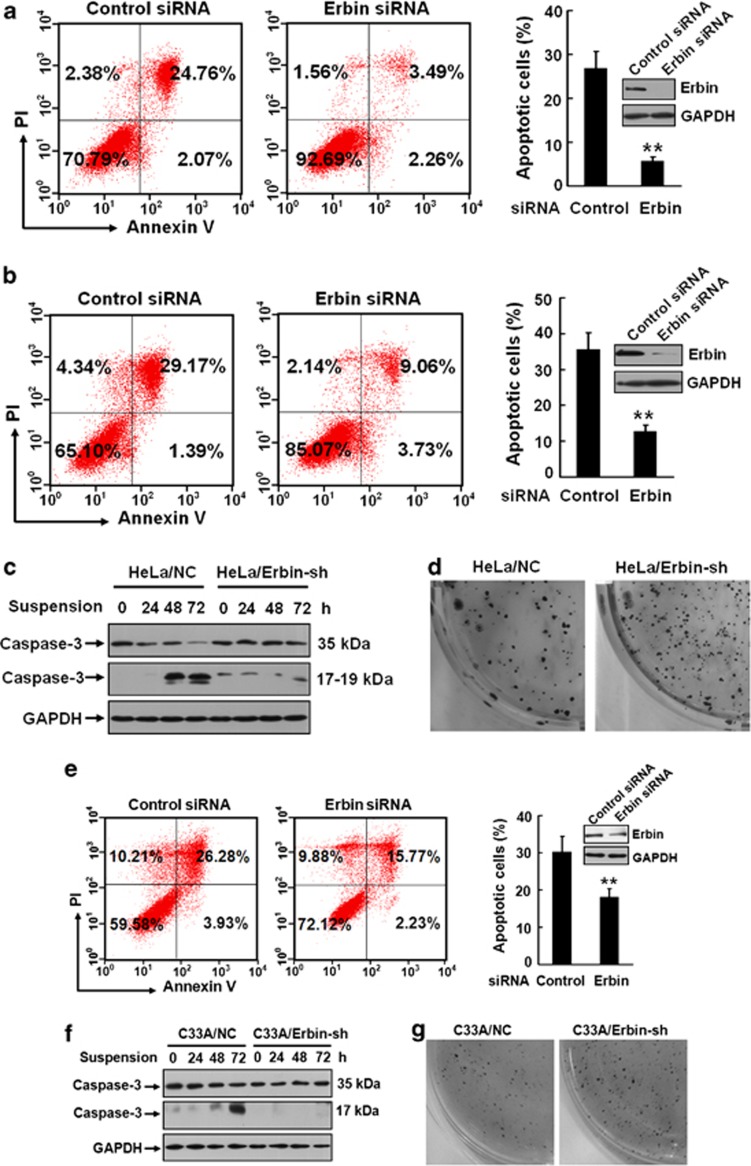
Loss of Erbin protects cervical cancer cells from cell-detachment-induced anoikis
The epithelial junctions are important in the regulation of cell polarity.24 Erbin is associated with the junctional membrane-associated proteins, such as the p120 catenin family proteins p0071 and δ-catenin, which are thought to interact with classic cadherins or desmosomal cadherins. Mutations of the junctional components disrupt cell polarity.12 Erbin also binds to β4-integrin and bullous pemphigoid antigen 1, which are involved in cell attachment to the extracellular matrix.28 Loss of cell adhesion triggers apoptosis, a process termed anoikis, in epithelial cells. Malignant tumor cells often develop resistant to anoikis, which enables their survival after detachment from the extracellular matrix.29, 30, 31, 32 When HeLa cells transfected with Erbin siRNA or control siRNA were cultured in the plates coated with PolyHEMA in the media containing 1% serum or no serum, they grew predominantly as a single-cell suspension and underwent anoikis after loss of detachment for 72 h, with the anoikis rates of 26.83% for the cells in low-serum (1%) media and 30.56% for the cells in serum-free media, respectively (Figures 1a and b). Interestingly, knockdown of Erbin resulted in a significant reduction in anoikis (∼5.75% for low serum and ∼12.79% for serum-free). To confirm the role of Erbin in anoikis, we established HeLa cells stably expressing Erbin-specific shRNA (HeLa/Erbin-sh) and control shRNA (HeLa/NC) by lentiviral transduction and analyzed the activation of caspase-3 in response to cell detachment by western blot. Cleavage of full-length caspase-3 was seen in suspension-cultured HeLa/NC cells (Figure 1c). However, the activation of caspase-3 was not remarkable in HeLa/Erbin-sh cells. Resistance to anoikis has been described in many types of human malignancies, including gastric, mammary, colon and lung cancers. To determine whether deficiency of Erbin affects anchorage-independent growth, we performed colony-formation assays. The data show that HeLa/Erbin-sh cells exhibited a higher capability of colony formation in soft agar (Figure 1d and Supplementary Figure S1A). Similar data were obtained in C33A (Figures 1e–g and Supplementary Figure S1B) and CaSki cells (Supplementary Figure S1C). These results demonstrate that loss of Erbin confers resistance of cervical cancer cells to cell-detachment-induced anoikis and promotes tumor cell survival.
Figure 1.
Loss of Erbin protects cervical cancer cells from cell-detachment-induced anoikis. (a, b) HeLa cells were transfected with control or Erbin siRNA. After transfection for 24 h, the cells were cultured in the medium containing 1% serum (a) or no serum (b) in the plates coated with PolyHEMA to avoid the adhesion of cells. After incubation for 72 h, the cells were harvested and the percentage of cellular apoptosis was analyzed by FACS using Annexin V-FITC detection kit. (c) HeLa cells stably expressing control shRNA (HeLa/NC) and Erbin shRNA (HeLa/Erbin-sh) were established by lentiviral transduction. Cleavage of full-length caspase-3 in response to cell detachment was analyzed in these cells by western blot. (d) In all, 3 × 103 HeLa/NC and HeLa/Erbin-sh cells were suspended in DMEM containing 10% FBS and 0.35% agar and plated on top of the bottom layer of 0.6% agarose in six-well plates. Anchorage-independent growth was determined by colony-formation assays. Colonies were stained with MTT, photographed and measured after 20 days. (e) C33A cells transfected with control or Erbin siRNA were cultured in the medium containing 1% serum in the plates coated with PolyHEMA. After incubation for 72 h, the anoikis rates were determined by FACS. (f, g) C33A cells stably expressing control shRNA (C33A/NC) or Erbin shRNA (C33A/Erbin-sh) were cultured in the medium containing 1% serum in the plates coated with PolyHEMA. The cleavage of full-length caspase-3 was analyzed by western blot (f). Anchorage-independent growth was determined by colony-formation assays (g). **P<0.01. PI, propidium iodide.
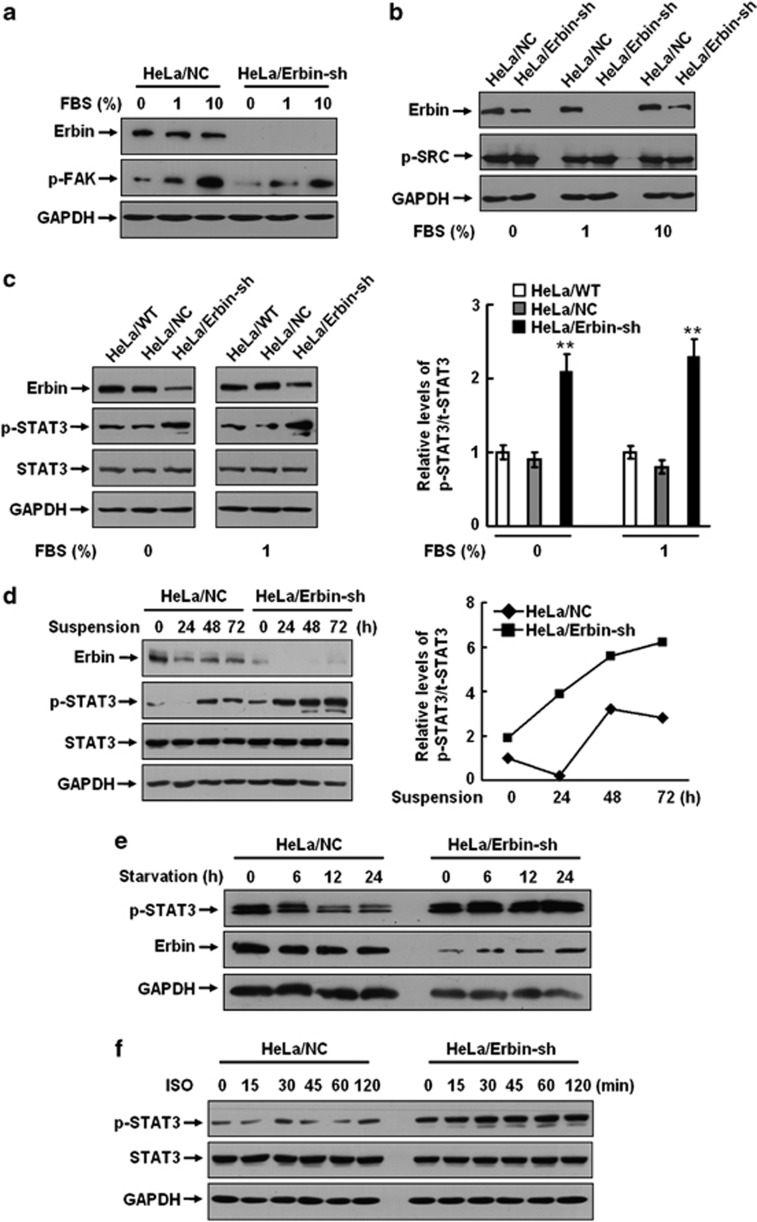
Loss of Erbin induces STAT3 activation in cervical cancer cells
Activation of focal adhesion kinase (FAK) and Src are known to participate in protecting cells from anoikis.29, 30 To dissect the signaling pathways involved in Erbin-deficiency-associated anoikis resistance, we examined the phosphorylations of FAK and Src in HeLa/NC and HeLa/Erbin-sh cells. Figure 2a shows that the phosphorylation level of FAK was significantly increased when the cells were cultured in media containing 10% fetal bovine serum (FBS). Knockdown of Erbin did not importantly influence FAK activation. No change in the phosphorylation of Src was observed in both HeLa/NC and HeLa/Erbin-sh cells (Figure 2b). These data suggest that the activity of FAK or Src is not influenced by Erbin.
Figure 2.
Loss of Erbin induces STAT3 activation in cervical cancer cells. (a, b) HeLa/NC and HeLa/Erbin-sh cells were cultured in the media containing 1% or 10% or no serum. The phosphorylations of FAK (a) and Src (b) were analyzed by western blot. (c) Parental HeLa (HeLa/WT), HeLa/NC and HeLa/Erbin-sh cells were cultured in the media containing 1% or no serum. The phosphorylation of STAT3 was analyzed by western blot. The relative STAT3 phosphorylation levels were determined by densitometry and normalized with protein levels. (d) HeLa/NC and HeLa/Erbin-sh cells were cultured in the media containing 1% serum in the plates coated with PolyHEMA. The phosphorylation of STAT3 was analyzed at the indicated time points. The relative STAT3 phosphorylation levels were determined by densitometry and normalized with protein levels. (e) HeLa/NC and HeLa/Erbin-sh cells were cultured in serum-free media. The phosphorylation of STAT3 was analyzed at the indicated time points. (f) HeLa/NC and HeLa/Erbin-sh cells were cultured in serum-free media overnight and then treated with 10 μℳ ISO. The phosphorylation of STAT3 was analyzed at the indicated time points. **P<0.01.
The recent studies reveal that the activation of STAT3 mediates anoikis resistance in esophageal squamous cell carcinoma and colon cancer.33, 34 We examined the phosphorylation of STAT3 at tyrosine residue 705. When the cells were cultured in the media containing 1% or no serum, increased phosphorylation of STAT3 was noticed only in HeLa/Erbin-sh cells but not in parental or HeLa/NC cells (Figure 2c). To further test whether STAT3 is activated in response to Erbin-knockdown-associated anoikis, STAT3 phosphorylation was analyzed in the cells cultured in suspension. Figure 2d shows that the phosphorylation of STAT3 was started at 48 h after loss of cell attachment in HeLa/NC cells. However, in HeLa/Erbin-sh cells a stronger STAT3 activation occurred significantly earlier (24 h), implicating that Erbin may be involved in modulating STAT3 activation. To confirm this, the cells were starved in serum-free media and then STAT3 phosphorylation was analyzed. In HeLa/NC cells, the phosphorylation level of STAT3 was decreased after starvation for 12 h. Conversely, a sustained elevation in STAT3 phosphorylation was clearly observed in HeLa/Erbin-sh cells (Figure 2e). The previous studies have demonstrated that catecholamine stimulation can induce STAT3 activation in ovarian and breast cancer cells.35, 36 The effect of catecholamine was verified in both HeLa/NC and HeLa/Erbin-sh cells by treating the cells with isoproterenol (ISO; Figure 2f). Interestingly, ISO stimulation induced a stronger activation of STAT3 in a time-dependent manner in HeLa/Erbin-sh cells, compared with HeLa/NC cells. The data suggest that Erbin negatively regulates the STAT3 activation.
A surprising finding is that the level of Erbin was significantly downregulated when HeLa/NC cells were cultured in suspension. Low level of Erbin was maintained in suspension-cultured HeLa/NC cells until 48–72 h (Figure 2d and Supplementary Figure S2A). There was no significant alteration in the Erbin expression at the transcription level (Supplementary Figure S2B), suggesting that the downregulation of Erbin expression may occur at a post-transcriptional level. Pretreatment of suspension-cultured HeLa and C33A cells with MG132, an established proteasome inhibitor that disrupts protein degradation (Supplementary Figures S2C and S2D), remarkably inhibited the reduction of the Erbin expression in response to cell detachment, implicating that loss of cell detachment resulted in degradation of Erbin. However, the molecular mechanisms of Erbin degradation in response to cell detachment remain to be further investigated.
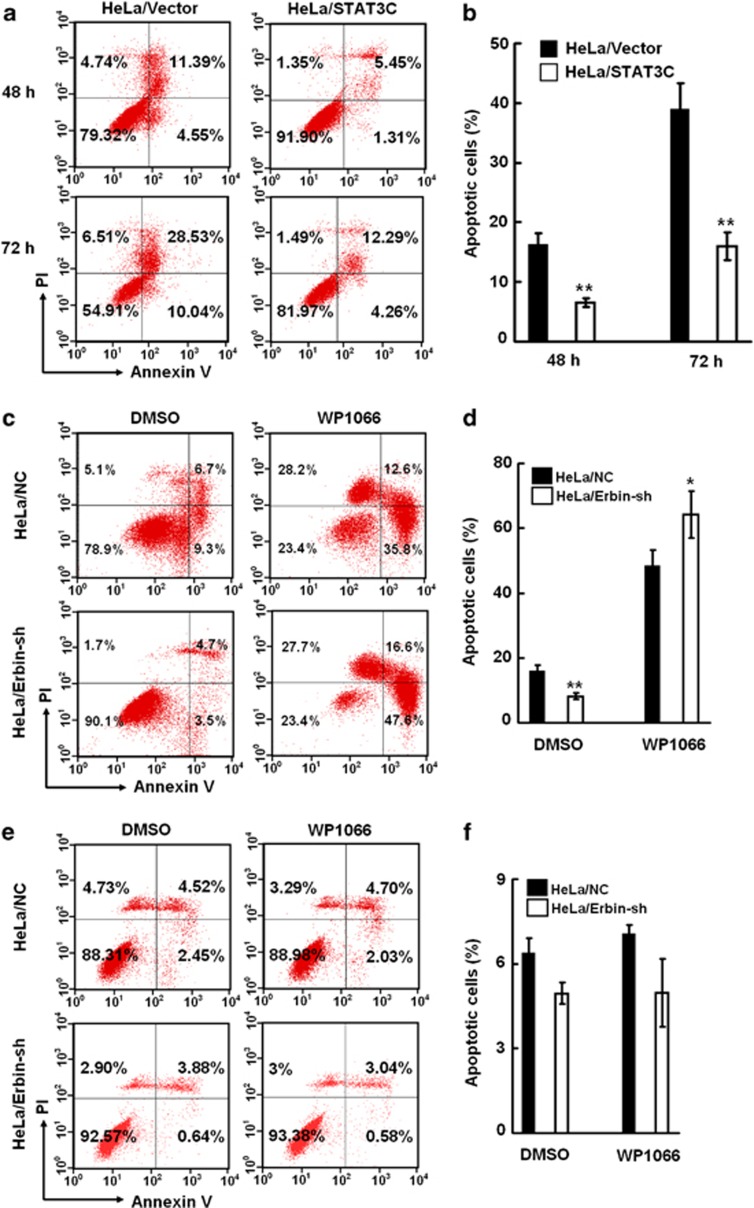
Loss of Erbin expression confers resistance of cervical cancer cells to anoikis in a STAT3-dependent manner
To address the potential role of STAT3 activation in Erbin-knockdown-induced anoikis resistance, we constructed HeLa cells stably expressing STAT3C, a constitutive active form of STAT3 (HeLa/STAT3C cells) and analyzed cellular apoptosis after suspension culture for 48 and 72 h. As shown in Figures 3a and b, the anoikis rates of the control cells, which were transfected with the empty plasmid (HeLa/Vector), were 15.94% for 48 h and 38.57% for 72 h. Overexpression of STAT3C remarkably suppressed cell apoptosis in response to cell detachment (6.76% for 48 h and 16.55% for 72 h). The treatment of the cells with WP1066, a potent inhibitor of Janus-activated kinase 2 (Jak2)/STAT3, effectively abrogated the effect of Erbin knockdown on cell survival under anchorage-independent conditions (Figures 3c and d), reconfirming the critical role of STAT3 activation in anoikis resistance associated with Erbin deficiency. Interestingly, no remarkable difference in cell apoptosis existed between HeLa/NC and HeLa/Erbin-sh cells under conventional culture conditions, and inhibition of STAT3 activation by WP1066 did not cause an increase in cell apoptosis (Figures 3e and f), indicating that the STAT3 signaling pathway modulated by Erbin has a distinct role in cell-detachment-induced anoikis. The previous studies demonstrate that Erbin inhibits Ras-Raf-ERK pathway,16, 17, 18 which also participates in regulation of anoikis.29, 37 We found that knockdown of Erbin triggered an enhanced ERK phosphorylation in cervical cancer cells (Supplementary Figure S3). To verify the specificity of STAT3 signaling pathway in cell-detachment-induced anoikis, we utilized the specific inhibitors of ERK signaling, U0126 and PD98059. As demonstrated in Figures 3g and h, the sensitivity of HeLa/Erbin-sh cells to anoikis was dramatically restored by WP1066 but not by U0126 and PD98059. These data indicate that loss of Erbin expression confers resistance of cervical cancer cells to anoikis in a STAT3-dependent manner.
Figure 3.
Loss of Erbin expression confers resistance of cervical cancer cells to anoikis in a STAT3-dependent manner. (a, b) HeLa cells were transfected with the plasmid expressing STAT3C (HeLa/STAT3C) or the empty vector (HeLa/Vector). The transfected cells were cultured in the medium containing 1% serum in the plates coated with PolyHEMA. After incubation for 48 and 72 h, the anoikis rates were determined by FACS. (c, d) HeLa/NC and HeLa/Erbin-sh cells cultured in suspension were treated with WP1066. The anoikis rates were determined by FACS. (e, f) HeLa/NC and HeLa/Erbin-sh cells under conventional culture were treated with WP1066. The apoptotic rates were determined by FACS. (g, h) HeLa/NC and HeLa/Erbin-sh cells were treated with WP1066, U0126 or PD98059. The anoikis rates were determined by FACS. **P<0.01. DMSO, dimethyl sulfoxide; PI, propidium iodide.
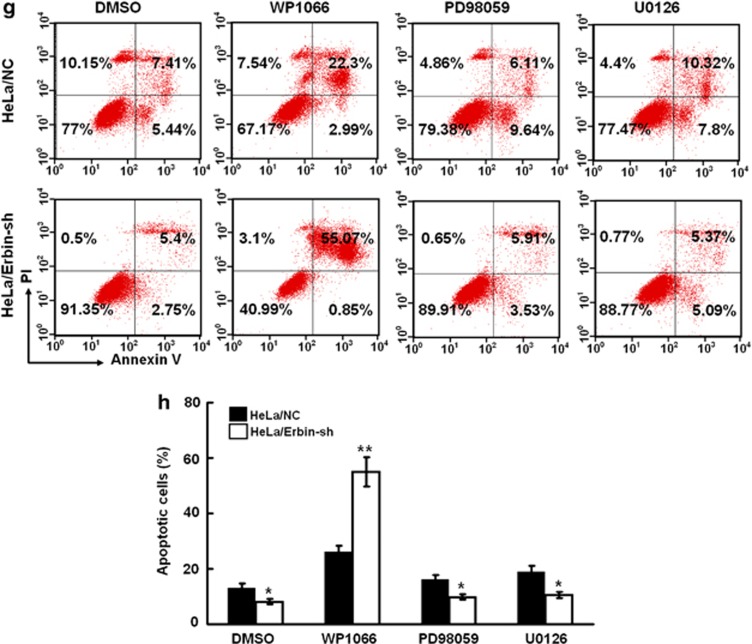
Erbin negatively regulates interleukin (IL)-6/STAT3 pathway and IL-6-induced anoikis resistance
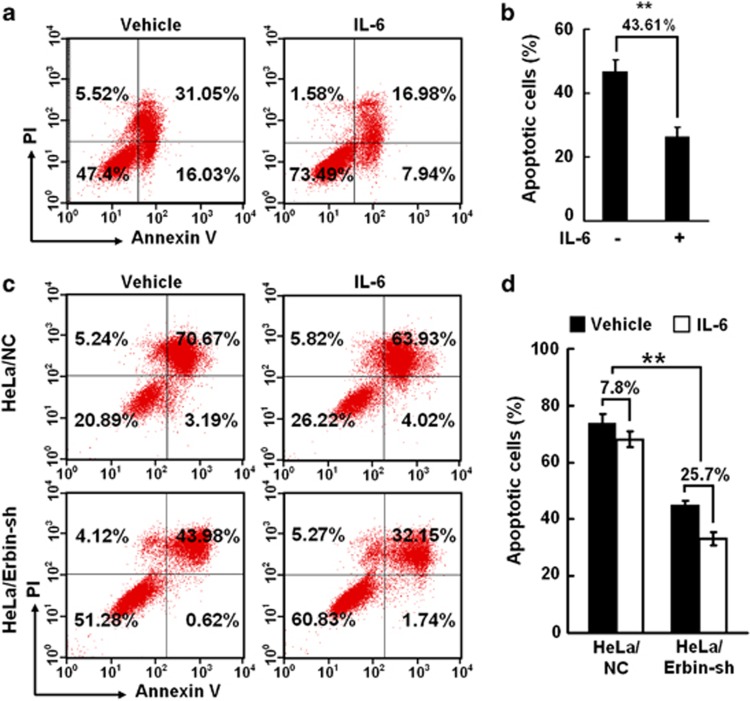
STAT3 is an important transcription factor in inflammatory pathways and has crucial roles in inflammation-mediated tumor promotion and metastasis.38, 39 IL-6 is a major STAT3 activator. Circulating level of IL-6 is frequently elevated in cancer patients. To determine whether IL-6 is involved in cell-detachment-induced anoikis resistance, we treated HeLa cells with IL-6 and analyzed cell apoptosis. Figures 4a and b show that 47.08% of HeLa cells underwent apoptosis after 72 h of suspension culture. Treatment with IL-6 significantly promoted cell survival (anoikis rate is 24.92%), and the inhibitory rate of anoikis by IL-6 ((apoptotic cells in control group−apoptotic cells in IL-6 treatment group)/apoptotic cells in control group × 100%) was 43.61%. However, the effect of IL-6 stimulation on anoikis was attenuated at 96 h, and the inhibitory rate of anoikis was 7.8% in HeLa/Nc cells. Under the same cultural condition, the inhibitory rate of anoikis by IL-6 stimulation was 25.8% in HeLa/Erbin-sh cells. These data suggest that Erbin knockdown augments the effect of IL-6 on anoikis resistance (Figures 4c and d).
Figure 4.
Erbin negatively regulates IL-6-induced anoikis resistance. (a, b) HeLa cells were treated with or without IL-6, and the anoikis rates determined after 72 h of suspension culture. (c, d) HeLa/NC and HeLa/Erbin-sh cells cultured in suspension were treated with or without IL-6. The anoikis rates were determined by FACS after 96 h. **P<0.01. PI, propidium iodide.
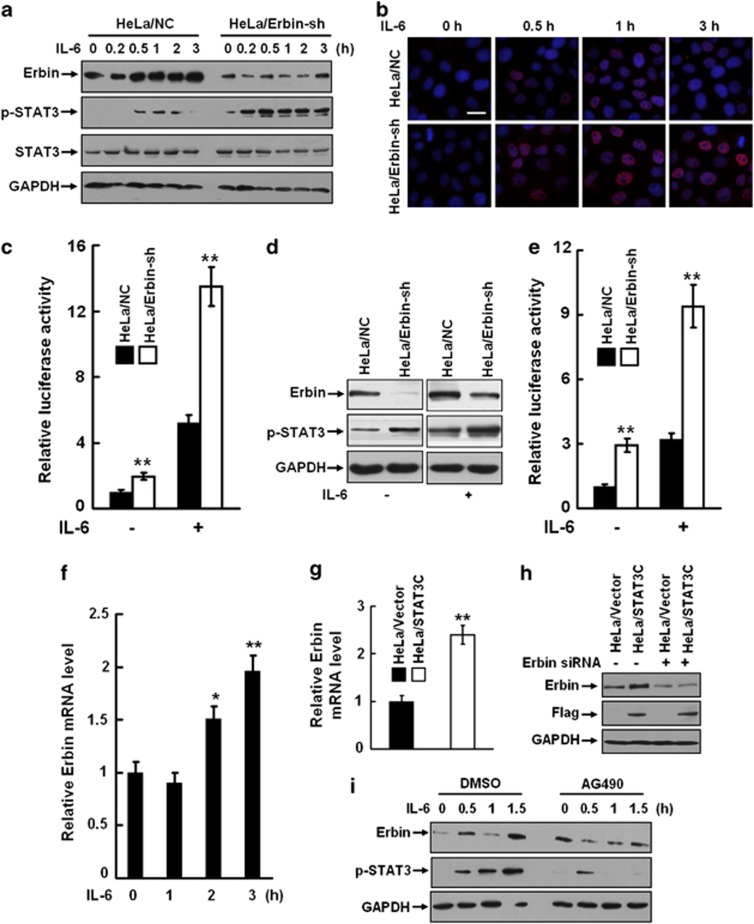
To interpret the relationship between IL-6, STAT3 and Erbin, we treated HeLa/NC and HeLa/Erbin-sh cells with IL-6 under conventional culture conditions. A transient activation of STAT3 was induced by IL-6 treatment in HeLa/NC cells. However, a stronger and more prolonged phosphorylation of STAT3 was noticed in HeLa/Erbin-sh cells (Figure 5a). Similar results were observed in CaSki and SiHa cells (Supplementary Figures S4A and S4B). Moreover, nuclear translocation of activated STAT3 was markedly increased in HeLa/Erbin-sh cells (Figure 5b). Knockdown of Erbin also significantly promoted the transcriptional activity of STAT3 either in the presence or absence of IL-6 stimulation as demonstrated by the reporter assays (Figure 5c). Similar results were also obtained in the suspension-cultured cells (Figures 5d and e).
Figure 5.
Erbin negatively regulates IL-6/STAT3 pathway. (a) HeLa/NC and HeLa/Erbin-sh cells under conventional culture were treated with 10 ng/ml IL-6. The activation of STAT3 was analyzed by western blot at the indicated time points. (b) HeLa/NC and HeLa/Erbin-sh cells were treated with 10 ng/ml IL-6 and then labeled with the anti-phoaphor-STAT3 antibody and Alexa fluor 549-labeled secondary antibody. Nuclei were stained with 1 μg/ml DAPI. Nuclear translocation of activated STAT3 was observed under a laser scanning confocal microscope. (c) HeLa/NC and HeLa/Erbin-sh cells grown in 24-well plates were transiently cotransfected by the STAT3 reporter and pRL-TK vectors. The transfected cells were treated with or without 10 ng/ml IL-6. The luciferase activities were measured using a dual luciferase assay kit. (d, e) HeLa/NC and HeLa/Erbin-sh cells were cultured in the media containing 1% serum in the plates coated with PolyHEMA for 24 h and treated with or without 10 ng/ml IL-6. The phosphorylation of STAT3 was analyzed (d) and the luciferase activities were measured (e). (f) HeLa cells were treated with or without IL-6, and the expression of Erbin mRNA was analyzed by real-time reverse transcriptase–PCR (RT-PCR). (g) HeLa cells were transfected with pRc/CMV-Stat3C-Flag (HeLa/STAT3C) or the empty vector (HeLa/Vector). The expression of Erbin mRNA was examined by real-time RT-PCR. (h) The HeLa/STAT3C and HeLa/Vector cells were transfected with Erbin siRNA or control siRNA. The expression of Erbin protein was examined by western blot. (i) HeLa cells were starved overnight and then treated with AG490. IL-6 was added into the cell culture after 1 h of the treatment. The phosphorylation of STAT3 was analyzed by western blot at the indicated time points. **P<0.01.
The previous studies indicate that negative regulators of STAT3, such as Socs3 and SHP-2, can be induced or activated by IL-6 stimulation.40, 41, 42, 43 Surprisingly, IL-6 stimulation also dramatically induced the expression of Erbin in a time-dependent manner (Figure 5a). By real-time reverse transcriptase–PCR, we demonstrate that the expression of Erbin was upregulated at the transcription level in response to IL-6 stimulation (Figure 5f). The upregulation of Erbin expression by IL-6 was also observed in human ovarian cancer cell line SKOV3 (Supplementary Figures S5A and S5B). Overexpression of STAT3C, a constitutive activated mutant STAT3, induced a dramatic upregulation in the Erbin expression at both transcription and protein levels (Figures 5g and h). As shown in Figure 5i, IL-6 induction simultaneously promoted the expression of Erbin and phosphorylation of STAT3 in a time-dependent manner, whereas the Jak2 inhibitor AG490 strongly repressed the effects of IL-6 on the Erbin expression and STAT3 activation. These data indicate that a negative feedback loop of STAT3/Erbin exists in response to IL-6 stimulation and that Erbin negatively regulates IL-6-induced STAT3 activation and IL-6-triggered anoikis resistance.
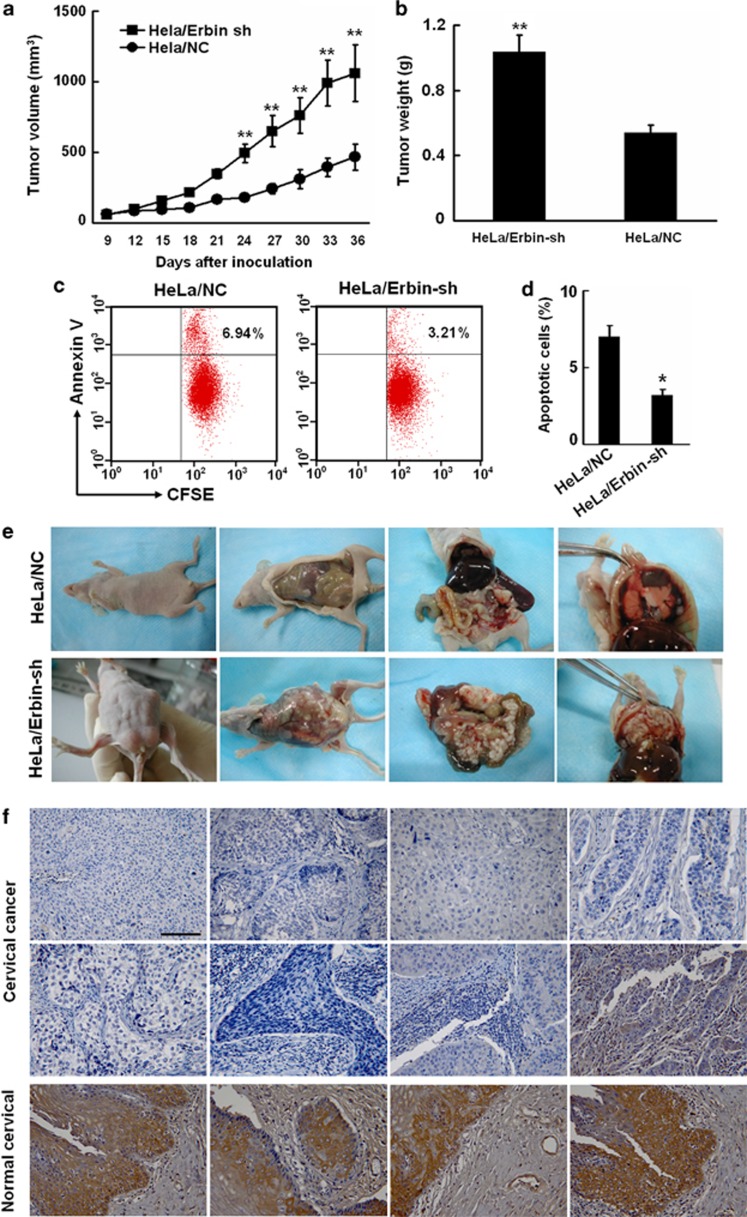
Knockdown of Erbin promotes proliferation and metastasis of cervical cancer cells in nude mice
To explore the role of Erbin in proliferation and metastasis of cervical cancer cells in vivo, we first injected HeLa/NC and HeLa/Erbin-sh cells subcutaneously into nude mice and monitored the tumor growth. As shown in Figures 6a and b, HeLa/Erbin-sh cells grew significantly faster than HeLa/NC cells in mice (P<0.01). To evaluate the effects of Erbin knockdown on in vivo anoikis, the cells were labeled with carboxyfluorescein succinimidyl ester (CFSE) and then implanted into the peritoneal cavity of nude mice. At 72 h after implantation, the apoptotic rates of the tumor cells from peritoneal cavity were determined by analyzing CFSE and Annexin V-phycoerythrin double-positive cells using FACS (fluorescence-activated cell sorter). HeLa/Erbin-sh cells exhibited a significantly lower apoptotic rate (3.21%) than HeLa/NC cells (6.94%), indicating that HeLa/Erbin-sh cells acquired anoikis resistance in vivo (Figures 6c and d). After implantation for 56 days, we dissected the tissues of the peritoneal cavity. As demonstrated in Figure 6e, HeLa/NC cells produced only a few tumor foci in the peritoneal cavity, but a large number of metastatic foci were observed in whole peritoneal cavity of the mice injected with HeLa/Erbin-sh cells, demonstrating that knockdown of Erbin promotes proliferation and metastasis of cervical cancer cells in nude mice. We examined the expression of Erbin in human cervical cancer tissues by immunohistochemistry using cervical cancer tissue microarray. The level of Erbin expression in normal cervical tissues was generally high. Surprisingly, the expression of Erbin was very low or even lost in most cervical cancer tissues, and decreased Erbin expression was noticed in 80% (32/42) of the tumor tissues examined (Figure 6f), suggesting that the reduction of the Erbin level was associated with cervical cancer.
Figure 6.
Knockdown of Erbin promotes proliferation and metastasis of cervical cancer cells in nude mice. (a, b) In all, 5 × 106 HeLa/NC and HeLa/Erbin-sh cells were subcutaneously injected into the right flanks of six-to-seven-week old female Balb/C athymic nude mice. The mice were monitored daily, and tumor volumes estimated according to the formula volume=length × width2/2. At the end of the experiments, the mice were killed. The primary tumors were dissected and weighted. (c, d) HeLa/NC and HeLa/Erbin-sh cells were labeled with CFSE and then implanted into the peritoneal cavity of nude mice. At 72 h after implantation, the apoptotic rates of the tumor cells from peritoneal cavity were determined by FACS analysis of CFSE and Annexin V-phycoerythrin double-positive cells. (e) In all, 5 × 106 HeLa/NC and HeLa/Erbin-sh cells were implanted into the peritoneal cavity of nude mice. After implantation for 56 days, the peritoneal cavities were dissected and photographed. (f) The expression of Erbin in human cervical cancer tissues was analyzed by immunohistochemistry with the antibody against Erbin using a tissue microarray containing cervical cancer and normal cervical tissues.
Discussion
It has been reported that the expression and phosphorylation of STAT3 are increased in cervical precancer and cancer lesions.44, 45 The level of STAT3 phosphorylation is significantly correlated with clinicopathological parameters such as lymph node metastasis or tumor size, which are considered as predictors of poor prognosis in cervical cancer.46 Exploration of the mechanisms underlying regulation of STAT3 activation and identification of key regulators of STAT3 are important for elucidation of cervical cancer pathogenesis and improvement of clinical outcomes. Activation of STAT3 can be triggered by multiple oncogenic and environmental signaling pathways.38 The activators of STAT3, such as growth factors/growth factor receptors,47, 48, 49 cytokines/cytokine receptors,39 catecholamines/adrenergic receptors35, 50 and nicotin/nicotinic receptors,51 have critical roles in malignant progression of cancer. However, how STAT3 is inactivated physiologically remains largely unknown. So far, very few STAT3 inhibitors have been identified.
An emerging role of STAT3-negative regulators in cancer progression has been recognized. A recent study shows that ablation of SHP-2, a STAT3 negative regulator, remarkably promotes diethylnitrosamine-induced hepatocellular carcinoma in mice, and the level of SHP-2 proteins is importantly decreased in human hepatocellular carcinoma tissues.52 Another study reveals that STAT3 activation is tightly regulated by the endogenous feedback inhibitor Socs3, which inhibits STAT3 signaling by binding to gp130. Homozygous deletion of Socs3 in the pancreas of mice accelerates progression of pancreatic intraepithelial neoplasias and development of pancreatic ductal adenocarcinoma.53 These studies imply that the negative regulators of STAT3 are also essential determinants in cancer progression.
In the present study, we show that loss of Erbin induces phosphorylation, nuclear translocation and transcriptional activities of STAT3 in cervical cancer cells. It has been reported that Socs3 and SHP-2 can be induced or activated by IL-6, a classical STAT3 stimulus.40, 41, 42, 43 We found that IL-6 induced STAT3 activation and Erbin expression simultaneously. Overexpression of STAT3C also significantly upregulated the level of Erbin, whereas the Jak2 inhibitor AG490 remarkably blocked not only STAT3 phosphorylation but also IL-6-induced Erbin expression. Our study reveals a novel negative regulator of STAT3 and a negative feedback loop of STAT3/Erbin in response to IL-6 stimulation, although the precise mechanism underlying the induction of Erbin by IL-6/STAT3 pathway is not fully understood.
Detachment of epithelial cells from the basement membrane results in anoikis, which is a self-defense strategy used by organisms to eliminate mislocated cells. Anoikis resistance is an important characteristic of tumor cells,31, 32 enabling tumor cells to invade adjacent tissues and to disseminate to distant organs. The molecular mechanisms of anoikis resistance are mostly unclear.29, 30 Constitutive activation of STAT3 signaling pathway promotes the proliferation and survival of cancer cells.38 The findings in several studies suggest that STAT3 activation may be involved in modulation of cell adhesion.54 Our current study reveals that STAT3 activation has a key role in the development of anoikis resistance in cervical cancer cells. Overexpression of STAT3C or induction of endogenous STAT3 activation by IL-6 evidently inhibited anoikis of cervical cancer cells, whereas inhibition of STAT3 activation by WP1066 greatly promoted anoikis, particularly in the cells with Erbin deficiency, indicating that the development of anoikis resistance is at least partially dependent upon STAT3 activation.
The LAP proteins such as Scribble and LET-413 have important roles in maintaining epithelial cell polarity in D. melanogaster and C. elegans. As membrane-bound adaptor proteins, LAP family members may provide a scaffold within the basolateral domain to assemble adherens junctions. Loss of function of let-413 and scribble genes disrupts epithelial organization and leads to abnormality in adherens junctions and cell polarity.55 Erbin interacts with cell adhesion proteins and is colocalized with p0071 at the cell–cell contacts and lateral membrane in polarized epithelial cells. Disruption of the interaction between Erbin and p0071 impairs integrity of epithelial cell monolayer, implicating a potential role of Erbin in cell adhesion and polarization formation.8 In our study, we demonstrate that Erbin deficiency in cervical cancer cells induces anoikis resistance both in vitro and in vivo, and knockdown of Erbin augments the effects of IL-6 on STAT3 activation and anoikis resistance. These data suggest that a IL-6/STAT3/Erbin loop exerts critical functions in protecting cells from anoikis and actively participates in cervical cancer progression and metastasis. However, reciprocal roles of Erbin and STAT3 in regulation of cell polarization and cell adhesion remain to be further investigated.
The previous studies showed that mutations in some genes encoding LAP proteins not only disrupted epithelial organization but also led to neoplastic overgrowth of tissues, revealing a close connection between cytoarchitecture and growth control.24, 55 Some members of LAP family have been proposed as tumor suppressors in Drosophila and human.26, 27 In our study, we present evidence indicating that loss of Erbin promotes the growth and metastasis of cervical cancer cells in nude mice. By immunohistochemical analysis of Erbin expression, we demonstrate that the expression of Erbin is significantly decreased or even lost in cervical cancer tissues, suggesting that loss of Erbin may contribute to malignant progression of human cervical cancer.
In summary, our study demonstrates for the first time that Erbin negatively modulates STAT3 activation in cervical cancer cells. Loss of Erbin magnifies IL-6-triggered STAT3 activation, endows cervical cancer cells with resistance to anoikis and facilitates malignant progression in human cervical cancer xenograft model.
Materials and methods
Cell culture and treatment
The human cervical cancer cell lines HeLa, SiHa, C33A, CaSki and human ovarian cancer cell line SKOV3 were obtained from the American Type Culture Collection (ATCC). All cell lines were cultured in Dulbecco's modified Eagle's medium (DMEM) (Invitrogen, Carlsbad, CA, USA) supplemented with 10% FBS (Hyclone, Logan, UT, USA). For treatment with IL-6 (Cell Signaling, Danvers, MA, USA) or ISO (Sigma, St Louis, MO, USA), the cells were incubated overnight in a serum-free medium and then treated with 10 ng/ml IL-6 or 10 μℳ ISO.
siRNA targeting Erbin
The siRNA specifically targeting Erbin (5′-CACACUGUUGUAUGAUCAACCAU-3′)15 was chemically synthesized by Invitrogen. Scramble siRNA (Invitrogen) was used as a control. HeLa, CaSki and SiHa cells were plated in 24-well plates at a density of 1.8 × 105/ml/well and cultured for 24 h. Then the cells were transfected with the Erbin siRNA or control siRNA (6 pmol/well) using Lipofectamine RNAiMAX (Invitrogen) when approximately 80% confluent.
Construction and transfection
The sequences, 5′-GCCACACTGTTGTATGATCAA-3′ and 5′-TTGATCATACAACAGTGTGGC-3′, in Erbin mRNA were selected through the siRNA Target Finder (http://www.ambion.com/techlib/misc/siRNA_finder.html, Ambion, Paisley, UK) as siRNA target sites. The synthetic double-strand oligonucleotides (Erbin shRNA, sense: 5′-TCGAGCCACACTGTTGTATGATCAAGGAATTCGTTGATCATACAACAGTGTGGCTTTTT-3' and anti-sense: 5'-CTAGAAAAAGCCACACTGTTGTATGATCAACGAATTCCTTGATCATACAACAGTGTGGC-3′ were inserted into the plasmid pSuppressorNeo (Imgenex, San Diego, CA, USA), according to the manufacturer's recommendation. Green fluorescent protein shRNA (sense: 5′-tcgagagagaccacatggtccttctggaattcgagaaggaccatgtggtctctcttttt-3′ and anti-sense: 5′-ctagaaaaagagagaccacatggtccttctcgaattccagaaggaccatgtggtctctc-3′) were used as a control. All constructs were verified by sequence analysis. The plasmid pRc/CMV-Stat3C-Flag (constitutive activated Stat3, Stat3C) is a generous gift from Dr Bromberg and Dr Darnell. The STAT3 reporter and pRL-TK reporter vectors were purchased from Promega (Madison, WI, USA). Transfection was carried out using Lipofectamine 2000 (Invitrogen) following the manufacturer's protocol.
Transduction
HeLa, C33A and CaSki cells were infected with the lentiviral vectors expressing Erbin shRNA or control shRNA (GeneChem, Shanghai, China).
Western blot
The following antibodies were employed for immunoblotting: the rabbit monoclonal antibodies against caspase-3 (Abcam, Cambridge, UK), phosphor-FAK (pY397, Abcam), phosphor-Src (Tyr416, Cell Signaling), phosphor-STAT3 (Tyr705, Cell Signaling) and glyceraldehyde-3-phosphate dehydrogenase (GAPDH, Sungene Biotech, Tianjin, China), the rabbit polyclonal antibody against STAT3 (Cell Signaling) and mouse polyclonal antibody against Erbin (produced in our laboratory).56 The experiments were repeated at least twice.
Quantitative reverse transcriptase–PCR
The total cellular RNA was isolated from HeLa cells using TRIzol reagent (Invitrogen). The cDNA was synthesized by reverse transcription kit (Fermentas, Glen Burnie, MD, USA) in accordance with the manufacturer's instructions. The specific primers (forward: 5′-TATTGTTAACCATGATGATGT-3′ and reverse: 5′-AGCGATTAGTTCTAATTGAGAAAA-3′) were used to detect the mRNA expression of Erbin in response to cell detachment. PCR was performed using SYBR Green Supermix (Agilent Technologies, Santa Clara, CA, USA) on Real-Time PCR Detection System (Agilent Technologies). The results were analyzed using the comparative threshold cycle method with β-actin (forward: 5′-gtggggcgccccaggcacca-3′, reverse: 5′-cttccttaatgtcacgcacgatttc-3′) as an internal control. The experiments were repeated at least twice.
Anoikis assays
Cells were cultured in the plates coated with PolyHEMA (Sigma) to avoid the adhesion of cells as described previously.33 To determine the roles of IL-6 and AKT in cell-detachment-induced anoikis, 10 ng/ml IL-6 or 2.5 μℳ WP1066 (Calbiochem, Millipore Corporation, Billerica, MA, USA) was added into the cell culture. After incubation for different time periods, the cells were harvested, and cell apoptosis was measured using Annexin V-FITC detection kit (Calbiochem). The experiments were repeated at least twice.
Colony-formation assays
Anchorage-independent growth was determined by soft agar colony-formation assays. HeLa, C33A and CaSki cells stably expressing Erbin shRNA or control shRNA were suspended in DMEM containing 10% FBS and 0.35% agar and plated on top of the bottom layer of 0.6% agarose. In all, 3 × 103 cells were plated in six-well plates and fed twice a week by adding 0.3 ml DMEM with 10% FBS. Colonies were stained with MTT (3-[4,5-dimethylthiazol-2-yl]-2,5 diphenyl tetrazolium bromide), photographed and measured after 20 days. The experiment was repeated in duplicate.
Luciferase assays
HeLa cells were co-transfected with the STAT3 reporter (Promega) and pRL-TK reporter plasmid using Lipofectamine 2000 (Invitrogen) according to the manufacturer's protocol. After transfection for 48 h, the cells under conventional culture or in suspension culture were incubated in serum-free medium for an additional 24 h and then stimulated with 10 ng/ml IL-6. For luciferase assays, cells were lysed in lysis buffer (Promega). Firefly and Renilla luciferase activities were measured with a dual luciferase assay kit (Promega) according to the manufacturer's instructions. All transfections were carried out in triplicate and repeated at least twice.
Immunofluorescence and confocal microscopy
The HeLa cells were treated with 10 ng/ml IL-6 for different time periods and then labeled with the rabbit monoclonal antibody against phosphor-STAT3 (Tyr705, Cell Signaling). Binding was detected by Alexa fluor 549-labeled (red) secondary antibody (Invitrogen). Nuclei were stained with 1 μg/ml DAPI (4,6-diamidino-2-phenylindole; Sigma). Fluorescence images were collected under a laser scanning confocal microscope (LSM 510 META, ZEISS, Oberkochen, Germany). This experiment was repeated in duplicate.
Tissue array and immunohistochemistry
A tissue microarray containing cores from 40 cervical cancer and normal cervical tissues was purchased from the US Biomax company (Rockville, MD, USA). Immunohistochemical staining was performed as described previously36, 57 by using the rabbit polyclonal antibody against Erbin (Santa Cruz, Dallas, TX, USA). Staining was assessed microscopically by two independent pathologists. Photomicrographs were taken with an Olympus microscope (Tokyo, Japan).
In vivo anoikis assays
HeLa cells stably expressing control shRNA (HeLa/NC) or Erbin shRNA (HeLa/Erbin-sh) were labeled by CFSE (Dojindo Laboratories, Dojindo, Kumamoto, Japan) according to the manufacturer's instruction. Subsequently, the labeled cells were implanted into the peritoneal cavity of nude mice. After 72 h, the mice were killed and peritoneal cells harvested by lavage of peritoneal cavity. Annexin V-phycoerythrin and CFSE dual-positive cells were analyzed by flow cytometry (FACS).
In vivo assays for tumor growth and metastasis
Six-to-seven-week old female Balb/C athymic nude mice were purchased from Beijing Vital River Laboratory Animal Technology Co. Ltd (Beijing, China). In all, 5 × 106 HeLa/NC or HeLa/Erbin-sh cells were subcutaneously injected into the right flanks of each mouse. Each group contains six mice. The mice were monitored daily and tumor volumes estimated according to the formula volume=length × width2/2. At the end of the experiments, the mice were killed. The primary tumors were dissected and weighted.
To evaluate the effects of Erbin knockdown on tumor metastasis in the peritoneal cavity of mice, 5 × 106 HeLa/NC or HeLa/Erbin-sh cells were injected into the peritoneal cavity of mice. At 56 days after implantation, the mice were killed. The peritoneal cavities were dissected, viewed and photographed.
Statistical analysis
Data were expressed as mean±s.d. Paired data were evaluated by Student's t-test. For comparisons between the multiple groups, two-way ANOVA tests were employed. P<0.05 was considered statistically significant.
Acknowledgments
We are grateful to Dr Bromberg and Dr Darnell for kindly providing us the plasmid pRc/CMV-Stat3C-Flag. This work is supported by National Basic Research Program of China (973 Program, 2010CB911904), National Natural Science Foundation of China (No. 31271440, 81272232 and 30800582) and Beijing National Natural Science Foundation (No. 7122124 and 7132163).
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on the Oncogenesis website (http://www.nature.com/oncsis).
Supplementary Material
References
- Bilder D, Birnbaum D, Borg JP, Bryant P, Huigbretse J, Jansen E, et al. Collective nomenclature for LAP proteins. Nat Cell Biol. 2000;2:E114. doi: 10.1038/35017119. [DOI] [PubMed] [Google Scholar]
- Bryant PJ, Huwe A. LAP proteins: what's up with epithelia. Nat Cell Biol. 2000;2:E141–E143. doi: 10.1038/35019616. [DOI] [PubMed] [Google Scholar]
- Apperson ML, Moon IS, Kennedy MB. Characterization of densin-180, a new brain-specific synaptic protein of the O-sialoglycoprotein family. J Neurosci. 1996;16:6839–6852. doi: 10.1523/JNEUROSCI.16-21-06839.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saito H, Santoni MJ, Arsanto JP, Jaulin-Bastard F, Le Bivic A, Marchetto S, et al. Lano, a novel LAP protein directly connected to MAGUK proteins in epithelial cells. J Biol Chem. 2001;276:32051–32055. doi: 10.1074/jbc.C100330200. [DOI] [PubMed] [Google Scholar]
- Borg JP, Marchetto S, Le Bivic A, Ollendorff V, Jaulin-Bastard F, Saito H, et al. ERBIN: a basolateral PDZ protein that interacts with the mammalian ERBB2/HER2 receptor. Nat Cell Biol. 2000;2:407–414. doi: 10.1038/35017038. [DOI] [PubMed] [Google Scholar]
- Huang YZ, Wang Q, Xiong WC, Mei L. Erbin is a protein concentrated at postsynaptic membranes that interacts with PSD-95. J Biol Chem. 2001;276:19318–19326. doi: 10.1074/jbc.M100494200. [DOI] [PubMed] [Google Scholar]
- Bilder D, Perrimon N. Localization of apical epithelial determinants by the basolateral PDZ protein Scribble. Nature. 2000;403:676–680. doi: 10.1038/35001108. [DOI] [PubMed] [Google Scholar]
- Izawa I, Nishizawa M, Tomono Y, Ohtakara K, Takahashi T, Inagaki M. ERBIN associates with p0071, an armadillo protein, at cell-cell junctions of epithelial cells. Genes Cells. 2002;7:475–485. doi: 10.1046/j.1365-2443.2002.00533.x. [DOI] [PubMed] [Google Scholar]
- Legouis R, Gansmuller A, Sookhareea S, Bosher JM, Baillie DL, Labouesse M. LET-413 is a basolateral protein required for the assembly of adherens junctions in Caenorhabditis elegans. Nat Cell Biol. 2000;2:415–422. doi: 10.1038/35017046. [DOI] [PubMed] [Google Scholar]
- Ellenbroek SI, Iden S, Collard JG. Cell polarity proteins and cancer. Semin Cancer Biol. 2012;22:208–215. doi: 10.1016/j.semcancer.2012.02.012. [DOI] [PubMed] [Google Scholar]
- Dan L, Shi M, Duan H, Han C, Guo N. Erbin, a negative regulator in diverse signal pathways. Curr Protein Pept Sci. 2010;11:759–764. doi: 10.2174/138920310794557673. [DOI] [PubMed] [Google Scholar]
- Jaulin-Bastard F, Arsanto JP, Le Bivic A, Navarro C, Vely F, Saito H, et al. Interaction between Erbin and a Catenin-related protein in epithelial cells. J Biol Chem. 2002;277:2869–2875. doi: 10.1074/jbc.M109652200. [DOI] [PubMed] [Google Scholar]
- Kobe B, Kajava AV. The leucine-rich repeat as a protein recognition motif. Curr Opin Struct Biol. 2001;11:725–732. doi: 10.1016/s0959-440x(01)00266-4. [DOI] [PubMed] [Google Scholar]
- Fan JS, Zhang M. Signaling complex organization by PDZ domain proteins. Neurosignals. 2002;11:315–321. doi: 10.1159/000068256. [DOI] [PubMed] [Google Scholar]
- Harmon RM, Simpson CL, Johnson JL, Koetsier JL, Dubash AD, Najor NA, et al. Desmoglein-1/Erbin interaction suppresses ERK activation to support epidermal differentiation. J Clin Invest. 2013;123:1556–1570. doi: 10.1172/JCI65220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai P, Xiong WC, Mei L. Erbin inhibits RAF activation by disrupting the sur-8-Ras-Raf complex. J Biol Chem. 2006;281:927–933. doi: 10.1074/jbc.M507360200. [DOI] [PubMed] [Google Scholar]
- Huang YZ, Zang M, Xiong WC, Luo Z, Mei L. Erbin suppresses the MAP kinase pathway. J Biol Chem. 2003;278:1108–1114. doi: 10.1074/jbc.M205413200. [DOI] [PubMed] [Google Scholar]
- Rangwala R, Banine F, Borg JP, Sherman LS. Erbin regulates mitogen-activated protein (MAP) kinase activation and MAP kinase-dependent interactions between Merlin and adherens junction protein complexes in Schwann cells. J Biol Chem. 2005;280:11790–11797. doi: 10.1074/jbc.M414154200. [DOI] [PubMed] [Google Scholar]
- Shi M, Zhao M, Hu M, Liu D, Cao H, Qian L, et al. β2-AR-induced Her2 transactivation mediated by Erbin confers protection from apoptosis in cardiomyocytes Int J Cardiol(e-pub ahead of print 5 May 2012). [DOI] [PubMed]
- McDonald C, Chen FF, Ollendorff V, Ogura Y, Marchetto S, Lecine P, et al. A role for Erbin in the regulation of Nod2-dependent NF-kappaB signaling. J Biol Chem. 2005;280:40301–40309. doi: 10.1074/jbc.M508538200. [DOI] [PubMed] [Google Scholar]
- Kufer TA, Kremmer E, Banks DJ, Philpott DJ. Role for erbin in bacterial activation of Nod2. Infect Immun. 2006;74:3115–3124. doi: 10.1128/IAI.00035-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner DR, Pisano MM, Roberts EA, Greene RM. Identification of three novel Smad binding proteins involved in cell polarity. FEBS Lett. 2003;539:167–173. doi: 10.1016/s0014-5793(03)00155-8. [DOI] [PubMed] [Google Scholar]
- Dai F, Chang C, Lin X, Dai P, Mei L, Feng XH. Erbin inhibits transforming growth factor beta signaling through a novel Smad-interacting domain. Mol Cell Biol. 2007;27:6183–6194. doi: 10.1128/MCB.00132-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin-Belmonte F, Perez-Moreno M. Epithelial cell polarity, stem cells and cancer. Nat Rev Cancer. 2012;12:23–38. doi: 10.1038/nrc3169. [DOI] [PubMed] [Google Scholar]
- Pearson HB, Perez-Mancera PA, Dow LE, Ryan A, Tennstedt P, Bogani D, et al. SCRIB expression is deregulated in human prostate cancer, and its deficiency in mice promotes prostate neoplasia. J Clin Invest. 2011;121:4257–4267. doi: 10.1172/JCI58509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu M, Pastor-Pareja JC, Xu T. Interaction between Ras(V12) and scribbled clones induces tumour growth and invasion. Nature. 2010;463:545–548. doi: 10.1038/nature08702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhan L, Rosenberg A, Bergami KC, Yu M, Xuan Z, Jaffe AB, et al. Deregulation of scribble promotes mammary tumorigenesis and reveals a role for cell polarity in carcinoma. Cell. 2008;135:865–878. doi: 10.1016/j.cell.2008.09.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Favre B, Fontao L, Koster J, Shafaatian R, Jaunin F, Saurat JH, et al. The hemidesmosomal protein bullous pemphigoid antigen 1 and the integrin beta 4 subunit bind to ERBIN. Molecular cloning of multiple alternative splice variants of ERBIN and analysis of their tissue expression. J Biol Chem. 2001;276:32427–32436. doi: 10.1074/jbc.M011005200. [DOI] [PubMed] [Google Scholar]
- Taddei ML, Giannoni E, Fiaschi T, Chiarugi P. Anoikis: an emerging hallmark in health and diseases. J Pathol. 2012;226:380–393. doi: 10.1002/path.3000. [DOI] [PubMed] [Google Scholar]
- Guadamillas MC, Cerezo A, Del Pozo MA. Overcoming anoikis--pathways to anchorage-independent growth in cancer. J Cell Sci. 2011;124:3189–3197. doi: 10.1242/jcs.072165. [DOI] [PubMed] [Google Scholar]
- Jenning S, Pham T, Ireland SK, Ruoslahti E, Biliran H. Bit1 in anoikis resistance and tumor metastasis. Cancer Lett. 2013;333:147–151. doi: 10.1016/j.canlet.2013.01.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson CD, Anyiwe K, Schimmer AD. Anoikis resistance and tumor metastasis. Cancer Lett. 2008;272:177–185. doi: 10.1016/j.canlet.2008.05.029. [DOI] [PubMed] [Google Scholar]
- Du XL, Yang H, Liu SG, Luo ML, Hao JJ, Zhang Y, et al. Calreticulin promotes cell motility and enhances resistance to anoikis through STAT3-CTTN-Akt pathway in esophageal squamous cell carcinoma. Oncogene. 2009;28:3714–3722. doi: 10.1038/onc.2009.237. [DOI] [PubMed] [Google Scholar]
- Fan Y, Zhang YL, Wu Y, Zhang W, Wang YH, Cheng ZM, et al. Inhibition of signal transducer and activator of transcription 3 expression by RNA interference suppresses invasion through inducing anoikis in human colon cancer cells. World J Gastroenterol. 2008;14:428–434. doi: 10.3748/wjg.14.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landen CN, Jr., Lin YG, Armaiz Pena GN, Das PD, Arevalo JM, Kamat AA, et al. Neuroendocrine modulation of signal transducer and activator of transcription-3 in ovarian cancer. Cancer Res. 2007;67:10389–10396. doi: 10.1158/0008-5472.CAN-07-0858. [DOI] [PubMed] [Google Scholar]
- Shi M, Liu D, Duan H, Qian L, Wang L, Niu L, et al. The beta2-adrenergic receptor and Her2 comprise a positive feedback loop in human breast cancer cells. Breast Cancer Res Treat. 2011;125:351–362. doi: 10.1007/s10549-010-0822-2. [DOI] [PubMed] [Google Scholar]
- Xiao Q, Qu K, Wang C, Kong Y, Liu C, Jiang D, et al. HDGF-related protein-3 is required for anchorage-independent survival and chemoresistance in hepatocellular carcinomas. Gut. 2012;62:440–451. doi: 10.1136/gutjnl-2011-300781. [DOI] [PubMed] [Google Scholar]
- Yu H, Pardoll D, Jove R. STATs in cancer inflammation and immunity: a leading role for STAT3. Nat Rev Cancer. 2009;9:798–809. doi: 10.1038/nrc2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu H, Kortylewski M, Pardoll D. Crosstalk between cancer and immune cells: role of STAT3 in the tumour microenvironment. Nat Rev Immunol. 2007;7:41–51. doi: 10.1038/nri1995. [DOI] [PubMed] [Google Scholar]
- Endo TA, Masuhara M, Yokouchi M, Suzuki R, Sakamoto H, Mitsui K, et al. A new protein containing an SH2 domain that inhibits JAK kinases. Nature. 1997;387:921–924. doi: 10.1038/43213. [DOI] [PubMed] [Google Scholar]
- Naka T, Narazaki M, Hirata M, Matsumoto T, Minamoto S, Aono A, et al. Structure and function of a new STAT-induced STAT inhibitor. Nature. 1997;387:924–929. doi: 10.1038/43219. [DOI] [PubMed] [Google Scholar]
- Starr R, Willson TA, Viney EM, Murray LJ, Rayner JR, Jenkins BJ, et al. A family of cytokine-inducible inhibitors of signalling. Nature. 1997;387:917–921. doi: 10.1038/43206. [DOI] [PubMed] [Google Scholar]
- Stahl N, Farruggella TJ, Boulton TG, Zhong Z, Darnell JE, Jr., Yancopoulos GD. Choice of STATs and other substrates specified by modular tyrosine-based motifs in cytokine receptors. Science. 1995;267:1349–1353. doi: 10.1126/science.7871433. [DOI] [PubMed] [Google Scholar]
- Shukla S, Shishodia G, Mahata S, Hedau S, Pandey A, Bhambhani S, et al. Aberrant expression and constitutive activation of STAT3 in cervical carcinogenesis: implications in high-risk human papillomavirus infection. Mol Cancer. 2010;9:282. doi: 10.1186/1476-4598-9-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CL, Hsieh FC, Lieblein JC, Brown J, Chan C, Wallace JA, et al. Stat3 activation in human endometrial and cervical cancers. Br J Cancer. 2007;96:591–599. doi: 10.1038/sj.bjc.6603597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takemoto S, Ushijima K, Kawano K, Yamaguchi T, Terada A, Fujiyoshi N, et al. Expression of activated signal transducer and activator of transcription-3 predicts poor prognosis in cervical squamous-cell carcinoma. Br J Cancer. 2009;101:967–972. doi: 10.1038/sj.bjc.6605212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong Z, Wen Z, Darnell JE., Jr. Stat3: a STAT family member activated by tyrosine phosphorylation in response to epidermal growth factor and interleukin-6. Science. 1994;264:95–98. doi: 10.1126/science.8140422. [DOI] [PubMed] [Google Scholar]
- Grandis JR, Drenning SD, Chakraborty A, Zhou MY, Zeng Q, Pitt AS, et al. Requirement of Stat3 but not Stat1 activation for epidermal growth factor receptor- mediated cell growth In vitro. J Clin Invest. 1998;102:1385–1392. doi: 10.1172/JCI3785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo HW, Hsu SC, Ali-Seyed M, Gunduz M, Xia W, Wei Y, et al. Nuclear interaction of EGFR and STAT3 in the activation of the iNOS/NO pathway. Cancer Cell. 2005;7:575–589. doi: 10.1016/j.ccr.2005.05.007. [DOI] [PubMed] [Google Scholar]
- Shi M, Liu D, Duan H, Han C, Wei B, Qian L, et al. Catecholamine up-regulates MMP-7 expression by activating AP-1 and STAT3 in gastric cancer. Mol Cancer. 2010;9:269. doi: 10.1186/1476-4598-9-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arredondo J, Chernyavsky AI, Jolkovsky DL, Pinkerton KE, Grando SA. Receptor-mediated tobacco toxicity: cooperation of the Ras/Raf-1/MEK1/ERK and JAK-2/STAT-3 pathways downstream of alpha7 nicotinic receptor in oral keratinocytes. FASEB J. 2006;20:2093–2101. doi: 10.1096/fj.06-6191com. [DOI] [PubMed] [Google Scholar]
- Bard-Chapeau EA, Li S, Ding J, Zhang SS, Zhu HH, Princen F, et al. Ptpn11/Shp2 acts as a tumor suppressor in hepatocellular carcinogenesis. Cancer Cell. 2011;19:629–639. doi: 10.1016/j.ccr.2011.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesina M, Kurkowski MU, Ludes K, Rose-John S, Treiber M, Kloppel G, et al. Stat3/Socs3 activation by IL-6 transsignaling promotes progression of pancreatic intraepithelial neoplasia and development of pancreatic cancer. Cancer Cell. 2011;19:456–469. doi: 10.1016/j.ccr.2011.03.009. [DOI] [PubMed] [Google Scholar]
- Vultur A, Cao J, Arulanandam R, Turkson J, Jove R, Greer P, et al. Cell-to-cell adhesion modulates Stat3 activity in normal and breast carcinoma cells. Oncogene. 2004;23:2600–2616. doi: 10.1038/sj.onc.1207378. [DOI] [PubMed] [Google Scholar]
- Elsum I, Yates L, Humbert PO, Richardson HE. The Scribble-Dlg-Lgl polarity module in development and cancer: from flies to man. Essays Biochem. 2012;53:141–168. doi: 10.1042/bse0530141. [DOI] [PubMed] [Google Scholar]
- Zhang H, Yu M, Hu M, Qian L, Chen L, Shi M, et al. Overexpression, refolding, purification of Erbin PDZ domain from Escherichia coli and preparation of its polyclonal antibody. Prep Biochem Biotechnol. 2008;38:282–293. doi: 10.1080/10826060802165105. [DOI] [PubMed] [Google Scholar]
- Zhou Q, Zeng R, Xu C, Liu L, Chen L, Kou P, et al. Erbin inhibits TGF-beta1-induced EMT in renal tubular epithelial cells through an ERK-dependent pathway. J Mol Med (Berl) 2012;90:563–574. doi: 10.1007/s00109-011-0833-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.