Hemolytic-uremic syndrome (HUS) is a thrombotic microangiopathy, characterized by microangiopathic hemolytic anemia, acute renal failure, and thrombocytopenia.1 It is subdivided into D+HUS or D-HUS/atypical HUS (aHUS), depending on the presence or absence of a diarrheal prodrome.2 Research linked aHUS to genetic abnormalities in the complement system proteins like: factor H, factor I, membrane co-factor protein, factor CD46, factor B, and C3.3 Ocular manifestations are rare and include retinal, choroidal, and vitreal hemorrhages, retinal ischemic signs, and non-perfusion.1, 4
Case report
We first describe the outcome of eculizumab therapy in a 23-year-old female with aHUS complicated with bilateral serous retinal detachment (SRD). She first presented during the third trimester of pregnancy with preeclampsia and HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome, so she underwent cesarean section. Following delivery, thrombocytopenia persisted with elevated liver transaminases and progressive renal failure. Kidney biopsy was compatible with thrombotic microangiopathy. After ruling out all possible differential diagnosis, aHUS was strongly suggested as the subsequent diagnosis. Treatment with plasmapheresis, hemodialysis, and systemic steroids was conventionally initiated.
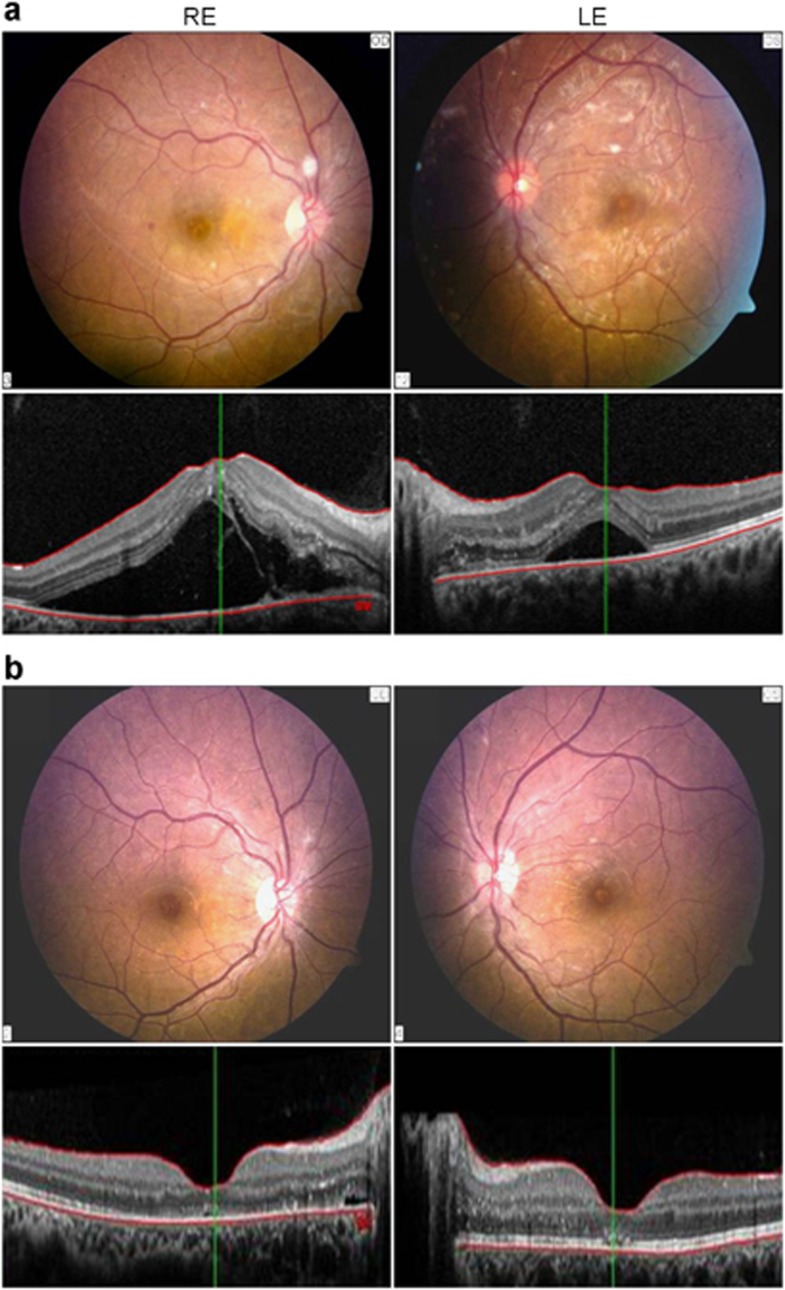
Subsequently, she complained of bilateral blurred vision. Best-corrected visual acuity (BCVA) was 6/60 RE and 6/10 LE. Funduscopy revealed bilateral SRD, small retinal hemorrhages, and cotton wool spots. Fluorescein angiography showed leakage mainly around optic discs. Optical coherence tomography showed bilateral SRD (Figure 1a).
Figure 1.
(a) Color fundus photographs (upper) on presentation show shallow serous retinal detachment in the posterior poles with cotton wool spots and small retinal hemorrhages most obviously seen temporal to the right fovea. The optic discs and the retinal vessels looked normal. Optical coherence tomography of both eyes (lower) show subretinal fluid more in the right eye with small hyperreflective exudates in the left papillomacular bundle. (b) Color fundus photographs (upper) and optical coherence tomography (lower) show total resolution of serous retinal detachment 1 month later.
Treatment with plasmapheresis, hemodialysis, antihypertensive medications, and systemic steroids was reinstituted with partial systemic and ocular response. Thus, systemic weekly eculizumab was added resulting in prompt improvement of blood parameters, normalization of urine output together with complete resolution of SRD (Figure 1b). BCVA improved to 6/15 RE and 6/8 LE and the eyes remained stable in a follow-up period of 2 months.
Comment
Eculizumab is a humanized monoclonal antibody against complement protein C5a.3 Its beneficial effects have already been demonstrated in patients with paroxysmal nocturnal hemoglobinuria.5 Recently, it was also shown to be effective for aHUS as it inhibits activation of the terminal complement pathway.3
In conclusion, although ocular findings in HUS are rare, prompt ophthalmological examination must be performed in the presence of ocular complaints. Eculizumab seems to be a promising treatment for aHUS and its ocular complications.
The authors declare no conflict of interest.
References
- Eberhard OK, Labjuhn SO, Olbricht CJ. Ocular involvement in haemolytic uraemic syndrome—case report and review of the literature. Nephrol Dial Transplant. 1995;10:266–269. [PubMed] [Google Scholar]
- Sturm V, Menke MN, Landau K, Laube GF, Thomas JN. Ocular involvement in paediatric haemolytic uraemic syndrome. Acta Ophthalmol. 2010;88:804–807. doi: 10.1111/j.1755-3768.2009.01552.x. [DOI] [PubMed] [Google Scholar]
- Westra D, Wetzels JF, Volokhina EB, van den Heuvel LP, van den Kar NC. A new era in the diagnosis and treatment of atypical haemolytic uremic syndrome. Neth J Med. 2012;70:121–129. [PubMed] [Google Scholar]
- Larakeb A, Leroy S, Fremeaux-Bacchi V, Montchilova M, Pelosse B, Dunand O, et al. Ocular involvement in hemolytic uremic syndrome due to factor H deficiency—are there therapeutic consequences. Pediatr Nephrol. 2007;22:1967–1970. doi: 10.1007/s00467-007-0540-0. [DOI] [PubMed] [Google Scholar]
- Roth A, Hock C, Konik A, Christoph S, Duhrsen U. Chronic treatment of paroxysmal nocturnal hemoglobinuria patients with eculizumab: safety, efficacy, and unexpected laboratory phenomena. Int J Hematol. 2011;93:704–714. doi: 10.1007/s12185-011-0867-y. [DOI] [PubMed] [Google Scholar]