Abstract
Background
Tunnels created for reconstruction of a torn anterior cruciate ligament (ACL) are critical determinants of joint stability and clinical outcomes. There is limited objective evidence on the ability of transtibial (TT), anteromedial (AM) portal, and outside-in (OI) operative techniques in creating anatomic tunnels.
Hypothesis
(1) Tibial tunnel–independent techniques can create tunnels more accurately at the anatomic ACL footprint center than the TT technique, and (2) femoral tunnel exit location of the OI and TT techniques on the lateral cortex will be significantly further away from the lateral epicondyle than the femoral tunnel exit location of the AM portal technique.
Study Design
Controlled laboratory study.
Methods
Eight cadaveric knee specimens with a mean age of 56 years were used in this study. A digitizing system was used to record points along the outlines of the ACL insertion area and apertures of tunnels created by the TT, AM portal, and OI techniques. The following parameters were measured from the digitized points: (1) amount of ACL, anteromedial bundle, and posterolateral bundle coverage by the tunnels; (2) relationship between the centers of the ACL and the tunnels; and (3) distance between the center of the femoral tunnel exit and the lateral epicondyle. All the recorded parameters were analyzed in 3-dimensional solid modeling software.
Results
The percentage of ACL footprint coverage achieved by all 3 surgical techniques was not significantly different from one another. However, larger femoral posterolateral bundle coverage was observed in tunnels created by the AM portal and OI techniques than in the TT tunnel. In terms of anteromedial bundle coverage, no significant differences were observed between the 3 techniques. On average, 27.1% ± 17.4% of the TT tunnel was outside the ACL footprint. This was significantly larger compared with 13.6%± 15.7% with the AM portal technique (P = .01) and 10.8%± 10.8% in the OI technique (P = .01). Centers of femoral tunnels created by the TT, AM portal, and OI techniques were located at a distance of 3.0 ± 1.5 mm, 2.1 ± 0.9 mm, and 1.5 ± 1.2 mm, respectively, from the ACL footprint center. The femoral tunnel exit location of the AM portal technique on the lateral femoral cortex was closer to the lateral epicondyle than the femoral tunnel exit location of the OI and TT techniques.
Conclusion
Findings of this study indicate that a larger posterolateral bundle coverage is achieved by the AM portal and OI techniques than by the TT technique. Centers of the tunnels created by the AM portal and OI techniques were closer to the native ACL footprint center than the center of the TT technique tunnel. The incidence of a posterior femoral tunnel exit relative to the lateral epicondyle is higher in the AM portal technique than in the OI and TT techniques.
Clinical Relevance
For ACL reconstruction using soft tissue grafts, tibial tunnel–independent techniques can produce more anatomic tunnels than the TT technique.
Keywords: ACL reconstruction, transtibial technique, anteromedial portal technique, outside-in technique
Determinants of successful anterior cruciate ligament (ACL) reconstruction are multifactorial. One such factor known to critically influence the success of surgical reconstruction of a torn ligament is the position of tunnels created for graft fixation.11,16,19,22,23 There has been recent evidence emphasizing anatomic reconstruction to achieve better clinical outcomes after surgical intervention. 2,11,19,22,23 While creating the femoral tunnel through the tibial tunnel continues to be the most widely practiced technique,17 it has been shown to result in a higher percentage of nonanatomic femoral tunnel position primarily because of its dependency on the tibial tunnel.6,13,14,26 However, some authors have proposed modifications to the traditional transtibial (TT) technique and have demonstrated that an anatomic femoral tunnel can be created by adopting these modifications.10,20,21 Alternatively, anteromedial (AM) portal and outside-in (OI) techniques are being used to circumvent the dependency on the tibial tunnel to create a femoral tunnel.1,25 Although these techniques have several advantages, various risks and limitations have been identified.7–9,18
Despite the evidence of 2 functional ACL bundles, the majority of ACL reconstructions are performed by using a single femoral and tibial tunnel created by the AM portal, OI, or TT technique.4,12 Therefore, it is imperative that this single tunnel captures both the functional bundles of the ACL. However, a comprehensive understanding of the relationship between the ACL, anteromedial bundle (AMB), and posterolateral bundle (PLB) footprints and the single tunnel created for soft tissue grafts remains unclear. It is important to establish objective evidence on the efficacy of the 3 surgical techniques in creating anatomic tunnels. Further, there is a theoretical risk for iatrogenic injury to the lateral soft tissue structures such as the lateral gastrocnemius tendon, popliteus tendon, lateral collateral ligament, common peroneal nerve, and biceps femoris tendon when creating the femoral tunnel through an AM portal. Therefore, the relationship between femoral tunnel exit on the lateral femoral cortex and the lateral epicondyle is critical to elucidate the potential risk for iatrogenic injury to the femoral attachments of the lateral gastrocnemius tendon, popliteus tendon, and lateral collateral ligament by each of these techniques.
The objectives of this study were to (1) establish a relationship between intra-articular femoral tunnel aperture and anatomic ACL footprint and (2) measure the distance between the extra-articular femoral tunnel exit location and lateral epicondyle for the tunnels created by the TT, AM portal, and OI techniques for soft tissue ACL grafts. We hypothesized that tibial tunnel–independent techniques can create tunnels more accurately at the anatomic ACL footprint center than the TT technique. We also hypothesized that the femoral tunnel exit location of the OI and TT techniques on the lateral cortex would be significantly further away from the lateral epicondyle than the femoral tunnel exit location of the AM portal technique.
MATERIALS AND METHODS
This study was conducted on 8 cadaveric knee specimens with a mean age of 56.4 years (range, 46–77 years). These fresh-frozen human cadaveric specimens were purchased from a tissue bank (MedCure Inc, Portland, Oregon) and were stored at −20°C at our institution. After the specimens were thawed for 24 hours at room temperature, all musculature surrounding the joint was removed. The diaphysis of the femur was potted in bone cement to secure it on a rigidly fixed pedestal.
With the tibia flexed to 90°, the AMB and PLB were carefully identified through a medial parapatellar arthrotomy. The identified AMB and PLB were transected using a No. 15 scalpel blade at the femoral attachment site. A surgical marking pen was then used to outline the femoral insertion area of the AMB and PLB. A 3-dimensional (3-D) digitizing system (MicroScribe G2LX, Immersion Corp, San Jose, California) with a manufacturer-reported accuracy of 0.3 mm was used to digitally record the ACL footprint, tunnel footprint, and anatomic landmarks. The AMB and PLB insertions were recorded as evenly spaced points along the previously outlined insertion areas in 3-D solid modeling software (Rhinoceros, Robert McNeel and Associates, Seattle, Washington) by the stylus of the digitizing system. After the ACL insertions were recorded, femoral tunnels were created by the TT technique, AM portal technique, and OI technique in each of the 8 specimens to implement a repeated-measures study design. After the tunnels were created by each surgical technique, the digitizing system and 3-D solid modeling software were used to digitally record evenly spaced circumferential points around the femoral tunnel intra-articular apertures.
The same specimens were used for 3 surgical techniques by filling the created femoral tunnels with bone cement. To minimize the bias in creating tunnels in bone cement, the sequence of the 3 techniques was varied among the 8 specimens. After the tunnels were filled with bone cement, the center of the anatomic ACL insertion was identified for subsequent surgical techniques by using the previously digitized ACL insertion. The motion of the stylus in space can be tracked in real time in 3-D solid modeling software. With the previously recorded ACL insertion in 3-D solid modeling software as the reference, the position of the stylus was manually maneuvered on the lateral intercondylar wall until the position of the tip of the stylus coincided with the virtual ACL insertion center (area centroid of ACL insertion) in 3-D solid modeling software. This position of the tip of the stylus was marked as the center of the ACL for subsequent tunnel creation. This procedure allowed us to accurately identify the ACL center repeatedly despite the use of bone cement.
In addition to the digitization of the outlines of ACL insertion and tunnel apertures for each technique, other anatomic structures digitized included medial and lateral epicondyles, inner and outer articular margins of the distal femur, and the Whiteside line and its extension to the anterior and posterior cortex of the femoral shaft. Further, before drilling the tunnels by each technique, we digitized the tip of the guide pin, when it was flush with the lateral femoral cortex, as a point to represent the center of the femoral tunnel exit.
Data Analysis
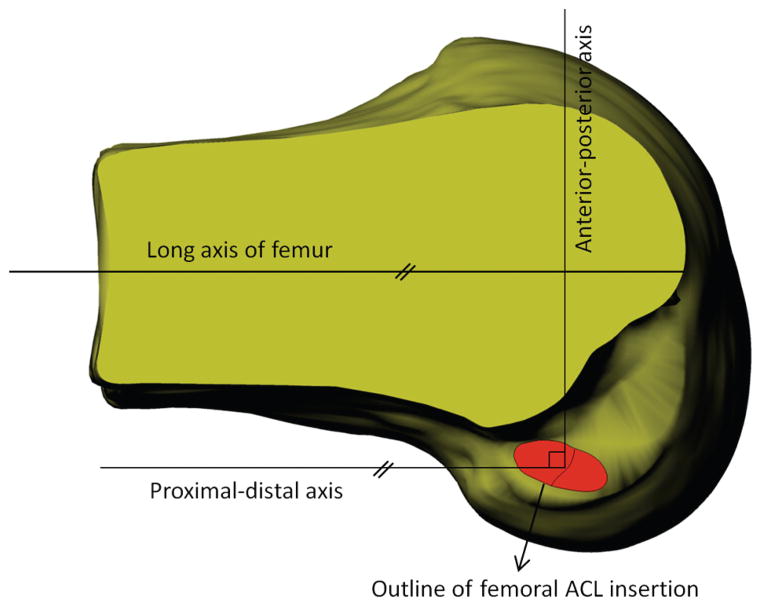
All the digitizations were performed at the same initial fixed position on the pedestal. The recorded points along the AMB and PLB insertions were connected by spline curves to form closed circumferential curves of the AMB and PLB footprints and hence the ACL footprint. A plane was then fitted to the ACL curve to form the femoral ACL plane. The proximal-distal axis of the femoral ACL plane was defined as a line parallel to the long axis of the femoral shaft, and the anterior-posterior axis was defined perpendicular to the proximal-distal axis in the femoral ACL plane (Figure 1). The recorded points along the intra-articular apertures of the femoral tunnels were also connected by spline curves to create closed circumferential curves of the tunnel footprints. Each spline curve was then projected onto the femoral ACL plane, and the areas and area centroids of these curves (ACL and tunnels created by TT, AM portal, and OI techniques) were evaluated using the built-in functions of the 3-D modeling software. The amount of ACL, AMB, and PLB coverage by each tunnel was evaluated by measuring the amount of overlapping area between the tunnel and the ACL, AMB, or PLB. The distance between the ACL center and each tunnel center was evaluated as the distance between their area centroids. Further, the proximodistal and anteroposterior relations of the tunnel centers with respect to the femoral ACL center were also evaluated. Distance between the center of the extra-articular femoral tunnel exit and lateral epicondyle was measured as the distance between the tip of the guide pin (previously digitized point) and a point at the lateral epicondyle in the 3-D modeling software.
Figure 1.
Position of the tunnel center relative to the femoral anterior cruciate ligament (ACL) center was evaluated by using a femoral ACL coordinate system. The proximal-distal axis was defined parallel to the long axis of the femur, and the anterior-posterior axis was defined perpendicular to the proximal-distal axis in the femoral ACL plane.
Surgical Techniques
TT Technique
The TT technique was performed with the tibia flexed to 90°. Intra-articularly, the tip of a 50° ACL tibial guide (DePuy Mitek, Raynham, Massachusetts) was positioned at the center of the posterolateral quadrant of the ACL footprint, and extra-articularly, the position of the sleeve ranged from a point lateral to the anterior margin of the medial collateral ligament (MCL) to the midpoint of the anterior margin of the MCL and medial border of the tibial tubercle. The tibial tunnel starting point in this study was located 20.8 ± 4.4 mm from the anterior margin of the MCL and 22.2 ± 4.5 mm from the edge of the medial tibial plateau, with a coronal angle of 60° with respect to the joint line. With these reference points, a guidewire was inserted into the tibia, and a tibial tunnel was then created by reaming over the inserted guidewire by an 8-mm cannulated drill bit (DePuy Mitek). To create the femoral tunnel, a 7.5-mm offset guide (DePuy Mitek) was inserted through the tibial tunnel and hooked at the “over-thetop” position. The offset guide was then laterally rotated so as to position the guidewire as close to the center of the femoral ACL footprint as possible. After the desired position of the guidewire was achieved, an 8-mm acornhead reamer was used to create a femoral tunnel.
AM Portal Technique
To create a femoral tunnel using the AM portal technique, a guidewire was inserted at the anatomic center of the ACL femoral footprint through the AM portal with the knee flexed to 120°. With the inserted guidewire as the reference, a femoral tunnel was then reamed to the lateral cortex of the distal femur using an 8-mm acorn-head reamer (DePuy Mitek).
OI Technique
For the OI technique, a 70° ACL tibial guide (DePuy Mitek) was inserted through the central (transpatellar tendon) portal, and the tip of the guide was positioned at the anatomic center of the ACL footprint. The central portal was located at the level of the joint line through the patellar tendon. A longitudinal incision over the lateral thigh was made, and the iliotibial band was split; then, the lateral aspect of the distal femoral metaphysis was accessed by retracting the vastus lateralis muscle. Extra-articularly, the guide sleeve was placed proximal and anterior to the lateral epicondyle. A guidewire was first inserted with these references with the tibia flexed to 70°. A femoral tunnel was then established by an 8-mm cannulated drill bit (DePuy Mitek) over the inserted guidewire.
Statistical Analysis
Statistical analyses were performed by 1-way repeatedmeasures analysis of variance (ANOVA). If significant, post hoc comparisons between the 3 tunnel creation techniques were made by using the Newman-Keuls test. All statistical analyses were performed by using Statistica 6.1.478.0 (StatSoft Inc, Tulsa, Oklahoma). A P value of <.05 was considered statistically significant.
RESULTS
Area
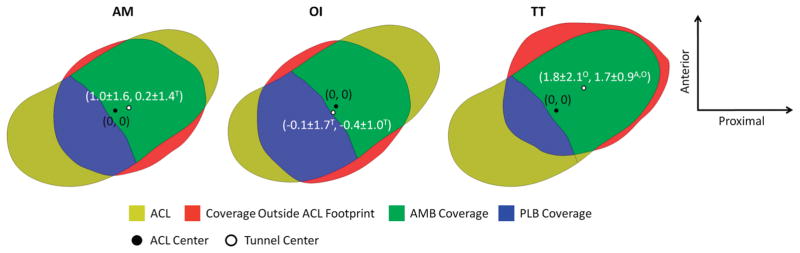
The areas of the ACL, AMB, and PLB footprints were 109.4 ± 12.7 mm2, 57.4 ± 7.6 mm2, and 52.0 ± 9.8 mm2, respectively. The cross-sectional areas at the aperture of the femoral tunnels created by the TT, AM portal, and OI techniques were 77.9 ± 23.8 mm2, 70.1 ± 18.9 mm2, and 70.1 ± 11.9 mm2, respectively. No significant difference was observed in the total ACL footprint coverage achieved by these 3 tunnels (Figure 2). Coverage of the PLB by the TT tunnel (26.4% ± 18.9%) was significantly lower than the coverage by the tunnels created by the OI (61.5% ± 27.0%) and AM portal (42.2% ± 29.4%) techniques (P < .05) (Figure 2). In terms of AMB coverage, no significant differences were observed between the 3 techniques. On average, 27.1% ± 17.4% of the TT tunnel was outside the ACL footprint. This was significantly larger than the 13.6% ± 15.7% with the AM portal technique (P = .01) and 10.8% ± 10.8% with the OI technique (P = .01). Also, no significant difference was observed in the percentage of tunnel outside the ACL footprint between the AM portal and OI techniques (P = .56).
Figure 2.

Percentage of the femoral anterior cruciate ligament (ACL) footprint covered by the 3 surgical technique tunnels (mean ± standard deviation). The figures in this table do not represent the average ACL and tunnel outlines; they are from a single specimen. A, statistically significant difference compared with the anteromedial portal technique; AMB, anteromedial bundle; O, statistically significant difference compared with the outside-in technique; PLB, posterolateral bundle; T, statistically significant difference compared with the transtibial technique; dashed line represents the tunnel outline.
Location of Tunnel Center Relative to ACL Footprint Center
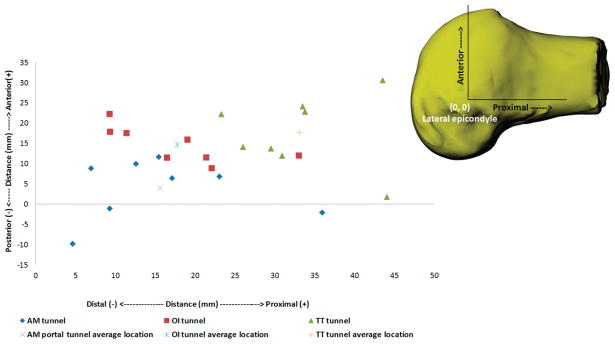
Among the 3 techniques, the tunnel center of the OI technique was the closest to the ACL center at 1.5 ± 1.2 mm, followed by the AM portal tunnel center at 2.1 ± 0.9 mm and TT technique tunnel center at 3.0 ± 1.5 mm. The center of the TT technique tunnel was significantly anterior compared with the centers of both the AM portal (P = .004) and OI (P = .001) tunnels (Figure 3). No significant difference was found in the location of the AM portal and OI tunnel centers in the anteroposterior direction (P = .25). The location of the TT technique tunnel center was significantly more proximal than the OI technique tunnel center (P = .03) (Figure 3). No significant difference was found in the location of the AM portal compared with both OI (P = .12) and TT (P = .25) tunnel centers in the proximodistal direction.
Figure 3.
Average femoral anterior cruciate ligament (ACL) and tunnel footprints. The white circle represents the location of the tunnel center relative to the femoral ACL center (mean ± standard deviation in mm). AM, anteromedial portal technique; OI, outside-in technique; TT, transtibial technique; A, statistically significant difference compared with the AM portal technique; O, statistically significant difference compared with the OI technique; T, statistically significant difference compared with the TT technique.
Location of Femoral Tunnel Exit Center Relative to Lateral Epicondyle
The TT tunnel exit was the farthest away from the lateral epicondyle at 42.3 ± 7.9 mm, followed by the OI tunnel exit at 27.4 ± 4.3 mm, and the AM portal tunnel exit was the closest to the lateral epicondyle at 20.8 ± 8.8 mm (Figure 4). The TT tunnel exit location was significantly different from the AM portal tunnel exit (P = .0002) and OI tunnel exit (P = .0008). No significant difference was observed between the AM portal and OI tunnel exits (P = .07). In terms of the anteroposterior component of the distance, the AM portal tunnel exit was significantly posterior compared with the OI tunnel exit (P = .006) and the TT tunnel exit (P = .003), and no significant difference was observed between the OI and TT tunnel exits in the anteroposterior direction (not significant) (Figure 4). In terms of the proximodistal component of the distance, the TT tunnel exit was significantly more proximal than the AM portal tunnel exit (P = .0007) and OI tunnel exit (P = .0008), and the locations of the AM portal and OI tunnel exits were not significantly different in the proximodistal direction (Figure 4).
Figure 4.
Anteroposterior and proximodistal location of the femoral tunnel exit relative to the lateral epicondyle. AM, anteromedial portal technique; OI, outside-in technique; TT, transtibial technique.
DISCUSSION
The results of this controlled laboratory study indicated that similar coverage of the femoral ACL footprint can be achieved by each of the tunnels created by the TT, AM portal, and OI operative techniques. However, the tibial tunnel–independent techniques were able to cover a larger portion of the femoral PLB footprint than the TT technique. The centers of the femoral tunnels created by the AM portal and OI techniques were closer to the anatomic ACL footprint center than the center of the TT tunnel. Further, the AM portal technique femoral tunnel exit location on the lateral femoral cortex was closer to the lateral epicondyle than the femoral tunnel exit location of the OI and TT techniques.
Evidence of improved clinical outcomes after anatomic ACL reconstruction has provided an impetus for the debate on the ability of currently practiced surgical techniques to achieve anatomic tunnel positions. The percentage of the ACL footprint covered by a tunnel is an important parameter, as it is directly related to the amount of collagen within the native footprints of the ACL. In this study, we found that with an 8-mm reamer the maximum femoral ACL footprint coverage was <57%. Although the maximum coverage was achieved by a tunnel created by the OI technique, no significant differences were observed among the 3 surgical techniques. Few studies have quantified the ACL footprint coverage by the TT technique tunnel, 20,26 and we are not aware of a study that measured the ACL footprint coverage by AM portal and OI technique tunnels. Strauss et al26 reported a 30.0% femoral ACL footprint coverage by the TT technique tunnel by using an 8-mm reamer. The larger femoral ACL footprint coverage that was observed in this study compared with the Strauss et al26 study (51.0% vs 30.0%) may be because of the larger offset guide used in this study (7.5 mm vs 6 mm), which allowed the tunnel to be placed closer to the ACL footprint center. Larger offset guides are required to accurately position the guidewire at the center of the ACL footprint.3,26
When the amount of ACL footprint coverage was divided into AMB and PLB footprint coverage, the tunnel by the TT technique achieved maximum (72%) AMB coverage and minimum (26%) PLB coverage compared with the tibial tunnel–independent techniques. Rue et al21 reported 50% coverage of the AMB and 51% coverage of the PLB by using a 10-mm reamer for the TT technique. The discrepancy between these 2 studies may be because of the difference in reamer sizes used in them. We are not aware of other studies that compared the amount of AMB and PLB coverage achieved by using the AM portal or OI techniques. While the amount of AMB and PLB footprint coverage may be more easily controlled by the AM portal and OI techniques, an increase in the PLB footprint coverage by the TT technique is a challenge because of the constraint imposed on the reamer by tibial tunnel location.
Another important parameter is the location of the tunnel center relative to the ACL footprint center, as this reflects the ability of a technique to position a tunnel at the anatomic center. The location of the TT tunnel center was farthest from the femoral ACL footprint center compared with the AM portal and OI tunnel centers. Further, the location of the TT tunnel center was anterior (high) and proximal (deep) compared with the femoral ACL footprint center. This observation is in agreement with several studies that have evaluated the location of the TT tunnel center with respect to the ACL footprint center.1,6,13,24,26 The tibial tunnel starting point in this study was located 20.8 ± 4.4 mm from the anterior margin of the MCL and 22.2 ± 4.5 mm from the edge of the medial tibial plateau, with a coronal angle of 60° with respect to the joint line. In addition to a medialized starting point used in this study, the offset guide was also laterally rotated as much as possible to place the guidewire as close to the ACL footprint center as possible. A more medial and proximal starting position than the one used in this study may potentially place the tunnel at the anatomic center of the ACL footprint. However, such a starting point is perilous, as it may cause iatrogenic damage to the MCL and may produce a tunnel too close to the medial tibial plateau.10,20
Theoretical risk for iatrogenic injury to the lateral gastrocnemius tendon, popliteus tendon, lateral collateral ligament, common peroneal nerve, and biceps femoris tendon is cited as a potential concern while preparing the femoral tunnel.5,18 The femoral attachment of the lateral collateral ligament is 1.4 mm proximal and 3.1 mm posterior to the lateral epicondyle, the femoral attachment of the lateral gastrocnemius tendon is located posterior and proximal to the lateral epicondyle at a distance of 17.2 mm, and the popliteus tendon attachment on the femur lies anterior to the lateral epicondyle at a distance of 15.8 mm.15 In this study, we observed minimal risk of injury to the femoral attachment of the lateral gastrocnemius tendon, popliteus tendon, and lateral collateral ligament in the OI and TT techniques, as all the tunnel exit locations were anterior and proximally located relative to the lateral epicondyle. Although, on average, the tunnel exits of the AM portal technique were also proximal and anterior relative to the lateral epicondyle, in 3 specimens, our AM portal tunnel exit was located posterior to the lateral epicondyle; such a location could potentially cause an injury to the lateral gastrocnemius tendon femoral attachment.
Our study has certain limitations. First, 3 different surgical techniques were tested in each specimen by filling the tunnels created with bone cement. A digitization system and 3-D modeling software were utilized to accurately reidentify the ACL center after the tunnels were filled with bone cement. Further, the sequence of surgical techniques was alternated to minimize the bias resulting from this limitation. Second, using different reamer sizes will alter the percentage of ACL coverage; however, we chose an 8-mm reamer to replicate a tunnel size commonly used for soft tissue grafts. Third, we did not use a retrograde reamer and a larger angled (>70°) femoral guide for the OI technique. The tunnel position of the OI technique may be improved by utilizing these instruments. Fourth, a different tibial flexion angle and tibial starting position may influence the tunnel characteristics of the TT technique. Evaluation of tunnel characteristics with such variation may be required to comprehensively realize the potential of the TT technique.
In conclusion, our findings indicated that, although equal percentage of femoral ACL coverage can be achieved by all 3 surgical techniques, more femoral PLB coverage could be achieved by our tibial tunnel–independent technique. Centers of the tunnels created by the AM and OI techniques were closer to those of the native ACL footprint center than the center of the TT technique tunnel. The incidence of a posterior femoral tunnel exit relative to the lateral epicondyle is higher in the AM portal technique than in the OI and TT techniques. The characteristics of tunnels created for ACL reconstruction are a function of several factors such as tunnel entry point, flexion angle, drilling angle, and so on. Therefore, our observations presented here must be interpreted within the framework of the technical details of each technique used in this study.
Acknowledgments
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was supported by the National Institutes of Health (R01AR055612).
References
- 1.Abebe ES, Moorman CT, 3rd, Dziedzic TS, et al. Femoral tunnel placement during anterior cruciate ligament reconstruction: an in vivo imaging analysis comparing transtibial and 2-incision tibial tunnel-independent techniques. Am J Sports Med. 2009;37(10):1904–1911. doi: 10.1177/0363546509340768. [DOI] [PubMed] [Google Scholar]
- 2.Alentorn-Geli E, Samitier G, Alvarez P, Steinbacher G, Cugat R. Anteromedial portal versus transtibial drilling techniques in ACL reconstruction: a blinded cross-sectional study at two- to five-year follow-up. Int Orthop. 2010;34(5):747–754. doi: 10.1007/s00264-010-1000-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Behrendt S, Richter J. Anterior cruciate ligament reconstruction: drilling a femoral posterolateral tunnel cannot be accomplished using an over-the-top step-off drill guide. Knee Surg Sports Traumatol Arthrosc. 2010;18(9):1252–1256. doi: 10.1007/s00167-010-1112-6. [DOI] [PubMed] [Google Scholar]
- 4.Duquin TR, Wind WM, Fineberg MS, Smolinski RJ, Buyea CM. Current trends in anterior cruciate ligament reconstruction. J Knee Surg. 2009;22(1):7–12. doi: 10.1055/s-0030-1247719. [DOI] [PubMed] [Google Scholar]
- 5.Farrow LD, Parker RD. The relationship of lateral anatomic structures to exiting guide pins during femoral tunnel preparation utilizing an accessory medial portal. Knee Surg Sports Traumatol Arthrosc. 2010;18(6):747–753. doi: 10.1007/s00167-009-0902-1. [DOI] [PubMed] [Google Scholar]
- 6.Gavriilidis I, Motsis EK, Pakos EE, Georgoulis AD, Mitsionis G, Xenakis TA. Transtibial versus anteromedial portal of the femoral tunnel in ACL reconstruction: a cadaveric study. Knee. 2008;15(5):364–367. doi: 10.1016/j.knee.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 7.George MS, Huston LJ, Spindler KP. Endoscopic versus rear-entry ACL reconstruction: a systematic review. Clin Orthop Relat Res. 2007;455:158–161. doi: 10.1097/BLO.0b013e31802eb45f. [DOI] [PubMed] [Google Scholar]
- 8.Hardin GT, Bach BR, Jr, Bush-Joseph CA, Farr J. Endoscopic singleincision anterior cruciate ligament reconstruction using patellar tendon autograft: surgical technique. 1992 [classical article] J Knee Surg. 2003;16(3):135–144. discussion 145–147. [PubMed] [Google Scholar]
- 9.Harner CD, Marks PH, Fu FH, Irrgang JJ, Silby MB, Mengato R. Anterior cruciate ligament reconstruction: endoscopic versus two-incision technique. Arthroscopy. 1994;10(5):502–512. doi: 10.1016/s0749-8063(05)80004-0. [DOI] [PubMed] [Google Scholar]
- 10.Heming JF, Rand J, Steiner ME. Anatomical limitations of transtibial drilling in anterior cruciate ligament reconstruction. Am J Sports Med. 2007;35(10):1708–1715. doi: 10.1177/0363546507304137. [DOI] [PubMed] [Google Scholar]
- 11.Jepsen CF, Lundberg-Jensen AK, Faunoe P. Does the position of the femoral tunnel affect the laxity or clinical outcome of the anterior cruciate ligament-reconstructed knee? A clinical, prospective, randomized, double-blind study. Arthroscopy. 2007;23(12):1326–1333. doi: 10.1016/j.arthro.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 12.Karlsson J, Irrgang JJ, van Eck CF, Samuelsson K, Mejia HA, Fu FH. Anatomic single- and double-bundle anterior cruciate ligament reconstruction, part 2: clinical application of surgical technique. Am J Sports Med. 2011;39(9):2016–2026. doi: 10.1177/0363546511402660. [DOI] [PubMed] [Google Scholar]
- 13.Kaseta MK, DeFrate LE, Charnock BL, Sullivan RT, Garrett WE., Jr Reconstruction technique affects femoral tunnel placement in ACL reconstruction. Clin Orthop Relat Res. 2008;466(6):1467–1474. doi: 10.1007/s11999-008-0238-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kopf S, Forsythe B, Wong AK, et al. Nonanatomic tunnel position in traditional transtibial single-bundle anterior cruciate ligament reconstruction evaluated by three-dimensional computed tomography. J Bone Joint Surg Am. 2010;92(6):1427–1431. doi: 10.2106/JBJS.I.00655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.LaPrade RF, Ly TV, Wentorf FA, Engebretsen L. The posterolateral attachments of the knee: a qualitative and quantitative morphologic analysis of the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and lateral gastrocnemius tendon. Am J Sports Med. 2003;31(6):854–860. doi: 10.1177/03635465030310062101. [DOI] [PubMed] [Google Scholar]
- 16.Loh JC, Fukuda Y, Tsuda E, Steadman RJ, Fu FH, Woo SL. Knee stability and graft function following anterior cruciate ligament reconstruction: comparison between 11 o’clock and 10 o’clock femoral tunnel placement. 2002 Richard O’Connor Award Paper. Arthroscopy. 2003;19(3):297–304. doi: 10.1053/jars.2003.50084. [DOI] [PubMed] [Google Scholar]
- 17.Lopez-Vidriero E, Hugh Johnson D. Evolving concepts in tunnel placement. Sports Med Arthrosc. 2009;17(4):210–216. doi: 10.1097/JSA.0b013e3181bf6668. [DOI] [PubMed] [Google Scholar]
- 18.Lubowitz JH. Anteromedial portal technique for the anterior cruciate ligament femoral socket: pitfalls and solutions. Arthroscopy. 2009;25(1):95–101. doi: 10.1016/j.arthro.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 19.Marchant BG, Noyes FR, Barber-Westin SD, Fleckenstein C. Prevalence of nonanatomical graft placement in a series of failed anterior cruciate ligament reconstructions. Am J Sports Med. 2010;38(10):1987–1996. doi: 10.1177/0363546510372797. [DOI] [PubMed] [Google Scholar]
- 20.Piasecki DP, Bach BR, Jr, Espinoza Orias AA, Verma NN. Anterior cruciate ligament reconstruction: can anatomic femoral placement be achieved with a transtibial technique? Am J Sports Med. 2011;39(6):1306–1315. doi: 10.1177/0363546510397170. [DOI] [PubMed] [Google Scholar]
- 21.Rue JP, Ghodadra N, Bach BR., Jr Femoral tunnel placement in single- bundle anterior cruciate ligament reconstruction: a cadaveric study relating transtibial lateralized femoral tunnel position to the anteromedial and posterolateral bundle femoral origins of the anterior cruciate ligament. Am J Sports Med. 2008;36(1):73–79. doi: 10.1177/0363546507311093. [DOI] [PubMed] [Google Scholar]
- 22.Sadoghi P, Kropfl A, Jansson V, Muller PE, Pietschmann MF, Fischmeister MF. Impact of tibial and femoral tunnel position on clinical results after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(3):355–364. doi: 10.1016/j.arthro.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 23.Scopp JM, Jasper LE, Belkoff SM, Moorman CT., 3rd The effect of oblique femoral tunnel placement on rotational constraint of the knee reconstructed using patellar tendon autografts. Arthroscopy. 2004;20(3):294–299. doi: 10.1016/j.arthro.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 24.Silva A, Sampaio R, Pinto E. Placement of femoral tunnel between the AM and PL bundles using a transtibial technique in single-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18(9):1245–1251. doi: 10.1007/s00167-010-1132-2. [DOI] [PubMed] [Google Scholar]
- 25.Steiner ME, Battaglia TC, Heming JF, Rand JD, Festa A, Baria M. Independent drilling outperforms conventional transtibial drilling in anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37(10):1912–1919. doi: 10.1177/0363546509340407. [DOI] [PubMed] [Google Scholar]
- 26.Strauss EJ, Barker JU, McGill K, Cole BJ, Bach BR, Jr, Verma NN. Can anatomic femoral tunnel placement be achieved using a transtibial technique for hamstring anterior cruciate ligament reconstruction? Am J Sports Med. 2011;39(6):1263–1269. doi: 10.1177/0363546510395488. [DOI] [PubMed] [Google Scholar]