Abstract
Study Design
Controlled experimental study.
Objective
To evaluate the kinematical effects of X-Stop device on the spinal process at the operated and the adjacent segments before and after X-Stop surgeries during various weight-bearing postures in elderly patients with lumbar spine stenosis.
Summary of Background Data
The mechanism of interspinous process (ISP) devices is to directly distract the ISP of the implanted level to indirectly decompress the intervertebra foramen and spinal canal. Few studies have investigated the changes of ISP gap caused by X-Stop implantation using magnetic resonance imaging or radiography, but the effect of X-Stop surgery on the kinematics of spinous processes during functional activities is still unclear.
Methods
Eight patients were tested before and, on average, 7 months after surgical implantation of the X-Stop devices using a combined computed tomography/magnetic resonance imaging and dual fluoroscopic imaging system during weight-bearing standing, flexion-extension, left-right bending, and left-right twisting positions of the torso. The shortest distances of the ISPs at the operated and the adjacent levels were measured using iterative closest point method and was dissected into vertical (gap) and horizontal (lateral translation) components.
Results
At the operated levels, the shortest vertical ISP distances (gap) significantly (P <0.05) increased by 1.5mm during standing, 1.2mm during left twist, 1.3mm during extension, and 1.1mm during flexion, whereas they also increased yet not significantly (P>0.05) in right twist, left bend, and right bend after the X-Stop implantation. The lateral translations were not significantly affected. At both cephalad and caudad adjacent levels, the ISP distances (vertical and horizontal) were not significantly affected during all postures after X-Stop implantation.
Conclusion
The findings of this study indicate that implantation of the X-Stop devices can effectively distract the ISP space at the diseased level without causing apparent kinematic changes at the adjacent segments during the studied postures.
Keywords: in vivo, spinous process, kinematics, X-Stop, lumbar spine stenosis
Recently, interspinous process (ISP) devices such as the X-Stop have been used as an alternative solution to the conventional decompressive surgery for lumbar spinal stenosis (LSS) and have shown promising clinical outcomes. 1–7 Compared with decompressive procedures, ISP devices are less invasive and can be inserted between the ISPs at the symptomatic level to create a slightly local flexion.2,7–10 In vitro studies have suggested that the posterior elements at the implanted segments are significantly distracted during extension after the ISP device implantation.9,11–13 However, few in vivo studies have been performed to investigate the changes of the ISP kinematics at the adjacent segments.1,4,14 For example, using a dynamic MRI technique, Lee et al1 reported that the ISP distance of the implanted segment increased significantly in LSS patients, whereas Zucherman et al4 noticed different results using plane radiographic measurements. The effect of the ISP devices on the kinematics of spinous processes during weight-bearing functional activities is still unclear.
In a previous investigation of asymptomatic volunteers, Xia et al14 measured the ISP distance using a combined magnetic resonance imaging (MRI)/computed tomography (CT) and dual fluoroscopic imaging system during upright standing, flexion and extension, and found that changes in ISP distances were dependent on body postures and vertebral levels. To evaluate the influence of X-Stop implantation on the kinematics of the spinous processes at the implanted and adjacent segments, we measured the vertical (gap) and horizontal (lateral translation) shortest distances in the ISP at the implanted and adjacent segments during weight-bearing functional activities before and after X-Stop implantation using the combined MRI/CT and the dual fluoroscopic imaging system technique. We hypothesized that although the ISP vertical distances at the implanted segment will be significantly increased, the ISP distances at the adjacent segments will not be changed.
MATERIALS AND METHODS
Patient Characteristics
Ten LSS patients who suffered from neurogenic intermittent claudication and were indicated to undergo X-Stop surgeries were recruited. Approval of the experimental design by the authors’ institutional review board was obtained before the initiation of the study and a signed consent form was obtained from each subject. In addition, to meet the United States Food and Drugs Administration (FDA)-approved indications4,10 for the X-Stop implantation, the patients must be able to stand for at least 20 minutes (more than the duration of fluoroscopic imaging) without motor deficit of the torso. Of the 10 recruited patients, 2 failed to complete the study: 1 patient opted out of the surgery; 1 patient did not want to undergo the follow-up visit. The data of these 2 subjects were excluded from analysis. Eight patients completed the study (4 males and 4 females; mean age 78.8 y, range from 66 to 86 y old).
X-Stop devices were implanted at a total of 10 segments in the 8 patients (7 at L4 to L5, 2 at L3 to L4, and 1 at L5 to S1). Six patients had a single-level implantation and 2 patients received implantation at 2 levels. In addition, 2 had mild degenerative scoliosis (Cobb angle 14 degrees and 18 degrees, respectively). The size of the X-Stop device was determined intraoperatively by measuring the distraction of the ISP space with a sizing distractor. At the mean final follow-up of 7.4 months (range: 3–12) postoperatively, there was no subject with ISP fracture or X-Stop device dislocation (Table 1).
TABLE 1.
Patients’ Demographics and Lumbar Spine Radiographic Characteristics
| No. | Sex | Age | Diagnosis | Implanted Level | Follow-up (mo) | Proximal Segment | Distal Segment | Scoliosis | X-Stop Related Complications |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 74 | LSS | L4/5 | 3 | L3/4 | L5/S1 | No | No |
| 2 | F | 86 | LSS | L4/5 | 5 | L3/4 | L5/S1 | No | No |
| 3 | M | 78 | LSS | L3/4, L4/5 | 13 | L2/3 | L5/S1 | No | No |
| 4 | M | 81 | LSS | L4/5 | 10 | L3/4 | L5/S1 | Yes (14°) | No |
| 5 | M | 66 | LSS | L4/5 L5/S1 | 8 | L3/4 | N/A | No | No |
| 6 | F | 84 | LSS | L4/5 | 2 | L3/4 | L5/S1 | No | No |
| 7 | M | 76 | LSS | L3/4 | 8 | L2/3 | L4/5 | Yes (18°) | No |
| 8 | F | 85 | LSS | L4/5 | 10 | L3/4 | L5/S1 | No | No |
Scoliosis diagnosis: Cobb angle >10 degrees.
Construction of 3-dimensional Anatomic Models of L2 to S1 Vertebrae
Lumbar segments of 7 subjects were CT scanned (Light-Speed Pro16, General Electric, Waukesha, WI) in a relaxed, supine position using high-resolution axial plane images. Images were obtained with a thickness of 0.625mm and a gap of 0.625 mm, and with a resolution of 512×512 pixels. Lumbar spine of 1 patient was MRI scanned using a 3 Tesla scanner (Siemens, Erlangen, Germany) with a spine surface coil and a T2-weighted fat-suppressed spoiled gradient recalled sequence. Parallel sagittal images were obtained with a thickness of 1mm without gap, and with a resolution of 512×512 pixels.
The CT and MRI images were imported into a solid modeling software (Rhinoceros version 4.0, Robert McNeel & Associates, Seattle, WA) to construct 3-dimensional anatomic vertebral models of L2, L3, L4, L5, and S1 using an established, validated protocol.15,16 Both the CT and MRI techniques yield accurate 3-dimensional vertebral models that can be used interchangeably.16
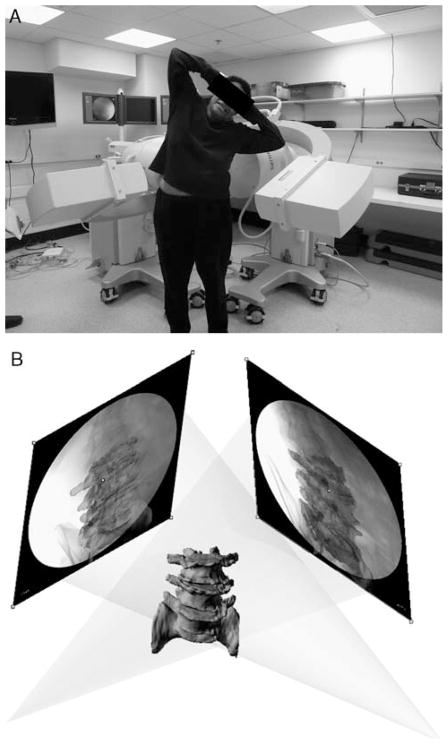
Virtual Reproduction of Vertebral Positions
Before the X-Stop implantation, the lumbar spines of the patients were imaged using a dual orthogonal fluoroscopic imaging system (BV Pulsera, Phillips, Bothell, WA) at 7 weight-bearing postures of the torso: upright standing, maximum extension, flexion, left-twist, right-twist, left-bend, and right-bend (Fig. 1A). Using an established protocol, the 3-dimensional models of the vertebrae were independently translated and rotated in 6-degrees of freedom until their projection outlines matched the osseous contours captured on the 2 fluoroscopic images (Fig. 1B).14,16,17 The in vivo positions of the lumbar vertebrae were therefore reproduced using the 3-dimensional models of the vertebrae and the dual fluoroscopic images in the solid modeling software.15,16
FIGURE 1.
A, Experiment setup of the dual fluoroscopic system for capturing lumbar spine positions in vivo (B) Virtual reproduction of the dual fluoroscopic system and the vertebral positions.
Patients were called back in average 7 months after surgery. The lumbar spine was imaged using the dual fluoroscopic system at the 7 weight-bearing postures. The corresponding postoperative vertebral positions were reproduced using the 3-dimensional vertebral models and the image matching method.
Measurement of the Shortest ISP Distance
To quantitatively evaluate the distraction of the ISP space after the X-Stop implantation, the shortest ISP distances of the ISP were measured before and after X-Stop implantation using the reproduced vertebrae positions at the 7 weight-bearing functional postures. The shortest distance between every pair of adjacent spinous processes (the shortest distance of the ISP) were automatically calculated using a software code based on iterative closest point method (Matlab v. 7.0, MathWorks, Natick, MA).16 Further, the distance was dissected into vertical and horizontal components to demonstrate the cranio-caudal gap and the lateral translation of the adjacent spinous processes (Fig. 2).
FIGURE 2.
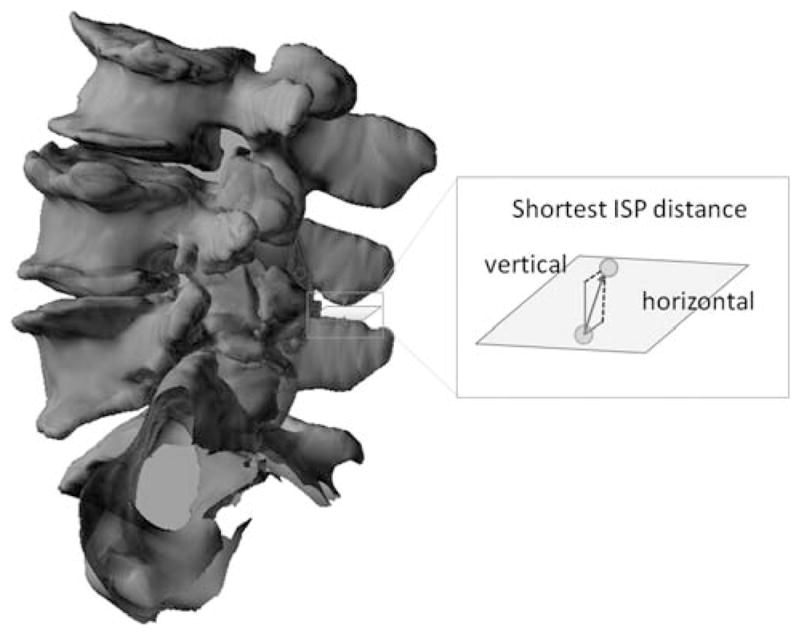
The shortest interspinous process (ISP) distance was decomposed into the cranio-caudal gap (vertical distance) and the lateral translation (horizontal distance).
Statistical Analysis
Two-way repeated analysis of variance was used to compare the shortest distances of the ISP at the operated and the adjacent vertebral segments during each of the functional activities. When a statistically significant difference was detected, the Newman-Keuls post hoc test was performed. Statistical significance was set at P<0.05. The statistical analysis was performed using Statistica 8.0 (Statsoft, Tulsa, OK).
RESULTS
Implanted Segments
At the operated levels, the postoperative shortest vertical ISP distances (gap) significantly increased by 1.5mm (P=0.004) during standing, 1.2mm (P=0.036) during left twist, 1.3mm (P=0.015) during extension, and 1.1mm (P=0.038) during flexion after X-Stop implantation, whereas increased yet not significantly during right twist (0.7 mm, P=0.281), bending left (1.0 mm, P=0.113), and during bending twist (1.1 mm, P=0.059) (Table 2). The horizontal ISP distance (lateral translations) at the implanted segment was not significantly (P value, from 0.420 to 0.989) affected by the X-Stop implantation in all the functional postures (Table 3).
TABLE 2.
Interspinous Process Vertical Distance Before and After X-Stop Implantation (mm)
| Operated Level
|
|||||||
|---|---|---|---|---|---|---|---|
| Stand | TL | TR | BL | BR | EXT | FLEX | |
| Pre-Op | 0.8 ± 1.1 | 1.3 ± 1.0 | 1.2 ± 1.1 | 1.6 ± 1.1 | 1.2 ± 0.9 | 0.8 ± 0.9 | 2.1 ± 0.8 |
| Post-Op | 2.4 ± 1.8 | 2.5 ± 2.5 | 1.9 ± 1.9 | 2.6 ± 2.2 | 2.3 ± 1.4 | 2.1 ± 1.4 | 3.2 ± 2.4 |
| Difference | 1.5 | 1.2 | 0.7 | 1.0 | 1.1 | 1.3 | 1.1 |
| P value | 0.004 | 0.036 | 0.281 | 0.113 | 0.059 | 0.015 | 0.038 |
| Proximal Level | |||||||
| Stand | TL | TR | BL | BR | EXT | FLEX | |
| Pre-Op | 2.8 ± 1.8 | 3.0 ± 2.1 | 3.0 ± 2.5 | 2.6 ± 3.3 | 2.7 ± 2.7 | 1.9 ± 2.2 | 3.3 ± 2.7 |
| Post-Op | 3.0 ± 2.2 | 3.0 ± 2.5 | 2.2 ± 2.3 | 2.7 ± 1.9 | 2.4 ± 2.0 | 2.2 ± 2.9 | 3.3 ± 1.4 |
| Difference | 0.2 | −0.0 | −0.8 | 0.0 | −0.3 | 0.2 | 0.0 |
| P value | 0.965 | 0.985 | 0.838 | 0.965 | 0.941 | 0.706 | 0.946 |
| Distal Level | |||||||
| Stand | TL | TR | BL | BR | EXT | FLEX | |
| Pre-Op | 3.2 ± 2.1 | 3.3 ± 2.9 | 2.1 ± 1.9 | 3.5 ± 3.3 | 3.2 ± 1.9 | 3.4 ± 2.7 | 2.9 ± 2.8 |
| Post-Op | 2.7 ± 1.9 | 3.2 ± 1.8 | 2.4 ± 1.5 | 2.7 ± 1.5 | 2.6 ± 2.8 | 2.7 ± 1.6 | 2.9 ± 1.8 |
| Difference | −0.5 | −0.1 | 0.2 | −0.9 | −0.6 | −0.7 | 0.0 |
| P value | 0.977 | 0.998 | 0.778 | 0.990 | 0.997 | 0.991 | 0.956 |
The values are mean ± standard deviation and 2-way repeated analysis of variance is used. Surgery and postures were 2 independent variables. Statistical significance is set at P < 0.05 and is indicated using bold and italic fonts.
BL indicates bend left, BR, bend right, EXT, extension, FLEX, flexion; Pre-Op, preoperative; Post-Op, postoperative; TL, twist left; TR, twist right.
TABLE 3.
Interspinous Process Horizontal Distance Before and After X-Stop Implantation (mm)
| Operated Level
|
|||||||
|---|---|---|---|---|---|---|---|
| Stand | TL | TR | BL | BR | EXT | FLEX | |
| Pre-Op | 1.0 ± 1.1 | 1.4 ± 1.3 | 0.7 ± 0.5 | 1.0 ± 0.8 | 1.0 ± 0.5 | 0.7 ± 0.4 | 1.3 ± 0.9 |
| Post-Op | 1.4 ± 0.7 | 1.4 ± 1.1 | 1.1 ± 1.2 | 1.0 ± 0.7 | 1.3 ± 0.9 | 0.9 ± 0.3 | 1.4 ± 0.8 |
| Difference | 0.4 | 0.1 | 0.4 | 0.1 | 0.3 | 0.2 | 0.1 |
| P value | 0.854 | 0.983 | 0.811 | 0.982 | 0.744 | 0.420 | 0.989 |
| Proximal Level | |||||||
| Stand | TL | TR | BL | BR | EXT | FLEX | |
| Pre-Op | 1.4 ± 0.8 | 1.3 ± 0.7 | 1.2 ± 0.8 | 1.3 ± 1.0 | 1.0 ± 1.1 | 0.8 ± 0.9 | 1.2 ± 1.0 |
| Post-Op | 1.5 ± 1.3 | 1.3 ± 0.8 | 1.2 ± 1.0 | 1.3 ± 1.0 | 1.2 ± 0.7 | 1.3 ± 1.0 | 1.5 ± 1.0 |
| Difference | 0.1 | −0.0 | −0.1 | 0.0 | 0.3 | 0.4 | 0.4 |
| P value | 0.826 | 0.948 | 0.961 | 0.999 | 0.890 | 0.885 | 0.985 |
| Distal Level | |||||||
| Stand | TL | TR | BL | BR | EXT | FLEX | |
| Pre-Op | 2.0 ± 1.6 | 2.6 ± 1.9 | 1.8 ± 1.9 | 2.3 ± 2.4 | 2.1 ± 1.3 | 2.3 ± 1.5 | 2.0 ± 2.0 |
| Post-Op | 2.4 ± 2.0 | 2.1 ± 1.5 | 2.2 ± 2.4 | 2.3 ± 1.8 | 2.6 ± 2.5 | 1.6 ± 1.3 | 2.2 ± 1.6 |
| Difference | 0.4 | −0.5 | 0.4 | −0.0 | 0.6 | −0.7 | 0.2 |
| P value | 0.999 | 0.988 | 0.988 | 0.990 | 0.992 | 0.959 | 0.984 |
The values are mean ± standard deviation and 2-way repeated analysis of variance is used. Surgery and postures were 2 independent variables. Statistical significance is set at P < 0.05 and is indicated using bold and italic fonts.
BL indicates bend left, BR, bend right, EXT, extension, FLEX, flexion; Pre-Op, preoperative; Post-Op, postoperative; TL, twist left; TR, twist right.
Adjacent Segments
The shortest vertical ISP distances at both cephalad and caudad adjacent segments were not significantly affected (P value, from 0.706 to 0.998) by the X-Stop implantation in all the functional postures (Table 2). The horizontal ISP distances at both cephalad and caudad adjacent segments were also not significantly affected (P value, from 0.826 to 0.999) by the X-Stop implantation during all studied postures (Table 3).
DISCUSSION
The rationale behind the ISP devices is to relieve pain in LSS patients by increasing the space available for neural elements, to decompress the stenotic segment by introducing local kyphosis similar to the effect of bending forward.2,18 We have measured the ISP distance during 7 weight-bearing postures in patients with LSS before and after implantation of the X-Stop device. The data confirmed our hypothesis by demonstrating that the vertical ISP distances increased during all the weight-bearing postures. Concurrently, the adjacent segments were not significantly affected in terms of the ISP space.
In a cadaveric study, Lindsey et al8 reported that implantation of X-Stop caused the implanted segment to increase 2 degrees of flexion in the unloaded position, consistent with our observations in living patients. Using a dynamic MRI technique, Lee et al1 reported that the shortest ISP distance increased significantly from 3.6 preoperatively to 9.0mm postoperatively in elderly LSS patients upon X-Stop implantation. The increments measured in their study were higher than the increments observed in this study. On the other hand, using coronal x-ray images Zucherman et al4 observed that the ISP distances were similar in the neutral or standing position before and after X-Stop implantation (51 and 52 mm, respectively) after 12 months in 100 LSS patients with an average age of 70 years.19 The differences among these studies might be due to different measurement methods and inclusion criteria: Elderly patients of our study had remarkable lumbar degeneration. On the other hand, the 2-dimensional image measurement technique employing plain radiograph might not be able to consistently locate the actual shortest distance of the ISP. Using the 3-dimensional modeling method, the shortest ISP distance can be precisely calculated to determine the effect of the surgeries without the interference of bone projection that overlay on 2-dimensional images. Our previous study16 validated the current image matching method and showed its mean accuracy to be below 0.2 mm. The average repeatability for determining the in vivo vertebral position and orientation are 0.16 mm/0.51 degrees and 0.23 mm/0.74 degrees for CT and MRI models, respectively.
Few studies have investigated the effects of X-Stops on the ISP distances at the adjacent segments.1,4 We found that the ISP vertical distances of the adjacent segments were not significantly affected. Similarly, Lindsey et al8 and Park et al9 reported that although the ranges of flexion-extension at the implanted segments decreased significantly, those at the adjacent segments were not significantly affected. Siddiqui et al20 also reported that the sagittal plane kinematics of the adjacent segments was not significantly changed in LSS patients. Although, a direct comparison with our data is difficult because of different loading conditions applied in these studies, in general, these studies indicated that the X-Stop implantation does not significantly alter the biomechanics of the adjacent segments during the studied postures.
The X-Stop device has achieved promising short term clinical outcomes.2,4,6 However, in vitro studies have suggested that the interspinous implant (X-Stop) may transfer the loading pressures from the disc11 and facet joints13 posterior to the spinous processes. Thus, over-distraction can be a potential problem that may lead to a fracture during or after the X-Stop implantation in the elderly who usually have underlying osteoporosis21,22 or degenerative spondylolisthesis.23 For these reasons, long-term biomechanical and clinical evaluations are necessary.
There are several limitations in this study. First, the enrolled subjects had the ISP devices implanted at different levels. There were 2 subjects who underwent implantation at 2 adjacent levels. Second, the ISP device is most commonly used in the elderly patients with intermittent neurogenic claudication secondary to LSS.4 In this age range, patients will more or less have degeneration in lumbar spine. In the current study, the mean age of the enrolled patients was 78.75 (66–86) years old. Third, the sample size was relatively small (8 subjects in the current study), but, it is still sufficient to detect statistical significance.
In summary, from a biomechanical standpoint, implantation of the X-Stop device in patients with symptomatic LSS provides an effective distraction of the ISP space in vivo without causing significant kinematic disturbances at the adjacent segments. This study represented an average of 7-month postoperative observation and further long-term follow-up is necessary to determine if the device retains its biomechanical and clinical efficiency.
Acknowledgments
Supported by a research grant of Medtronic Inc and partially supported by NIH (R21AR057989) and China Scholarship Council (2009637094).
Footnotes
The authors declare no conflict of interest.
References
- 1.Lee J, Hida K, Seki T, et al. An interspinous process distractor (X STOP) for lumbar spinal stenosis in elderly patients: preliminary experiences in 10 consecutive cases. J Spinal Disord Tech. 2004;17:72–77. doi: 10.1097/00024720-200402000-00013. discussion 78. [DOI] [PubMed] [Google Scholar]
- 2.Bono CM, Vaccaro AR. Interspinous process devices in the lumbar spine. J Spinal Disord Tech. 2007;20:255–261. doi: 10.1097/BSD.0b013e3180331352. [DOI] [PubMed] [Google Scholar]
- 3.Anderson PA, Tribus CB, Kitchel SH. Treatment of neurogenic claudication by interspinous decompression: application of the X STOP device in patients with lumbar degenerative spondylolisthesis. J Neurosurg Spine. 2006;4:463–471. doi: 10.3171/spi.2006.4.6.463. [DOI] [PubMed] [Google Scholar]
- 4.Zucherman JF, Hsu KY, Hartjen CA, et al. A multicenter, prospective, randomized trial evaluating the X STOP interspinous process decompression system for the treatment of neurogenic intermittent claudication: two-year follow-up results. Spine. 2005;30:1351–1358. doi: 10.1097/01.brs.0000166618.42749.d1. [DOI] [PubMed] [Google Scholar]
- 5.Kondrashov DG, Hannibal M, Hsu KY, et al. Interspinous process decompression with the X-STOP device for lumbar spinal stenosis: a 4-year follow-up study. J Spinal Disord Tech. 2006;19:323–327. doi: 10.1097/01.bsd.0000211294.67508.3b. [DOI] [PubMed] [Google Scholar]
- 6.Zucherman JF, Hsu KY, Hartjen CA, et al. A prospective randomized multi-center study for the treatment of lumbar spinal stenosis with the X STOP interspinous implant: 1-year results. Eur Spine J. 2004;13:22–31. doi: 10.1007/s00586-003-0581-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richards JC, Majumdar S, Lindsey DP, et al. The treatment mechanism of an interspinous process implant for lumbar neurogenic intermittent claudication. Spine. 2005;30:744–749. doi: 10.1097/01.brs.0000157483.28505.e3. [DOI] [PubMed] [Google Scholar]
- 8.Lindsey DP, Swanson KE, Fuchs P, et al. The effects of an interspinous implant on the kinematics of the instrumented and adjacent levels in the lumbar spine. Spine. 2003;28:2192–2197. doi: 10.1097/01.BRS.0000084877.88192.8E. [DOI] [PubMed] [Google Scholar]
- 9.Park SW, Lim TJ, Park J. A biomechanical study of the instrumented and adjacent lumbar levels after In-Space interspinous spacer insertion. J Neurosurg Spine. 2010;12:560–569. doi: 10.3171/2009.11.SPINE08668. [DOI] [PubMed] [Google Scholar]
- 10.Siddiqui M, Nicol M, Karadimas E, et al. The positional magnetic resonance imaging changes in the lumbar spine following insertion of a novel interspinous process distraction device. Spine. 2005;30:2677–2682. doi: 10.1097/01.brs.0000187878.79676.26. [DOI] [PubMed] [Google Scholar]
- 11.Swanson KE, Lindsey DP, Hsu KY, et al. The effects of an interspinous implant on intervertebral disc pressures. Spine. 2003;28:26–32. doi: 10.1097/00007632-200301010-00008. [DOI] [PubMed] [Google Scholar]
- 12.Wilke HJ, Drumm J, Haussler K, et al. Biomechanical effect of different lumbar interspinous implants on flexibility and intradiscal pressure. Eur Spine J. 2008;17:1049–1056. doi: 10.1007/s00586-008-0657-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wiseman CM, Lindsey DP, Fredrick AD, et al. The effect of an interspinous process implant on facet loading during extension. Spine. 2005;30:903–907. doi: 10.1097/01.brs.0000158876.51771.f8. [DOI] [PubMed] [Google Scholar]
- 14.Xia Q, Wang S, Passias PG, et al. In vivo range of motion of the lumbar spinous processes. Eur Spine J. 2009;18:1355–1362. doi: 10.1007/s00586-009-1068-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li G, DeFrate LE, Park SE, et al. In vivo articular cartilage contact kinematics of the knee: an investigation using dual-orthogonal fluoroscopy and magnetic resonance image-based computer models. Am J Sports Med. 2005;33:102–107. doi: 10.1177/0363546504265577. [DOI] [PubMed] [Google Scholar]
- 16.Wang S, Passias P, Li G, et al. Measurement of vertebral kinematics using noninvasive image matching method-validation and application. Spine. 2008;33:E355–E361. doi: 10.1097/BRS.0b013e3181715295. [DOI] [PubMed] [Google Scholar]
- 17.Li G, Wang S, Passias P, et al. Segmental in vivo vertebral motion during functional human lumbar spine activities. Eur Spine J. 2009;18:1013–1021. doi: 10.1007/s00586-009-0936-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Inufusa A, An HS, Lim TH, et al. Anatomic changes of the spinal canal and intervertebral foramen associated with flexion-extension movement. Spine. 1996;21:2412–2420. doi: 10.1097/00007632-199611010-00002. [DOI] [PubMed] [Google Scholar]
- 19.Neumann P, Wang Y, Karrholm J, et al. Determination of interspinous process distance in the lumbar spine. Evaluation of reference population to facilitate detection of severe trauma. Eur Spine J. 1999;8:272–278. doi: 10.1007/s005860050172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Siddiqui M, Karadimas E, Nicol M, et al. Effects of X-STOP device on sagittal lumbar spine kinematics in spinal stenosis. J Spinal Disord Tech. 2006;19:328–333. doi: 10.1097/01.bsd.0000211297.52260.d5. [DOI] [PubMed] [Google Scholar]
- 21.Bowers C, Amini A, Dailey AT, et al. Dynamic interspinous process stabilization: review of complications associated with the X-Stop device. Neurosurg Focus. 2010;28:E8. doi: 10.3171/2010.3.FOCUS1047. [DOI] [PubMed] [Google Scholar]
- 22.Idler C, Zucherman JF, Yerby S, et al. A novel technique of intraspinous process injection of PMMA to augment the strength of an inter-spinous process device such as the X STOP. Spine. 2008;33:452–456. doi: 10.1097/BRS.0b013e318163e06d. [DOI] [PubMed] [Google Scholar]
- 23.Denard PJ, Holton KF, Miller J, et al. Back pain, neurogenic symptoms, and physical function in relation to spondylolisthesis among elderly men. Spine J. 2010;10:865–873. doi: 10.1016/j.spinee.2010.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]