Abstract
Background
The function of the anteromedial (AM) and posterolateral (PL) bundles of the anterior cruciate ligament (ACL) during gait has not been reported.
Hypothesis
The AM and PL bundles have distinct functional behavior during the stance phase of treadmill gait.
Study Design
Descriptive laboratory study.
Methods
Three-dimensional models of the knee were created by magnetic resonance images from 8 healthy subjects. The contour of the 2 bundle attachments were constructed on each model. Each bundle was represented by a straight line connecting its tibial and femoral attachment centroids. Next, the knee kinematics during the stance phase of gait was determined with a dual fluoroscopic imaging system. The relative elongation, sagittal plane elevation, coronal plane elevation, and transverse plane deviation of the 2 bundles were measured directly from heel strike to toe-off.
Results
At heel strike, the AM and PL bundles had first peak elongation of 9% ± 7% and 9% ± 13%, respectively. At 50% progress of the stance phase, both bundles were maximally elongated, 12% ± 7% for the AM bundle and 13% ± 15% for the PL bundle. No significant difference was found for each bundle between 40% and 60% of the stance phase (P > .05). With increasing knee flexion, the sagittal plane and coronal plane elevations of the 2 bundles decreased, whereas the deviation angles increased.
Conclusion
Both bundles are anisometric and function in a similar manner during the stance phase of gait. They were maximally elongated throughout the midstance where they were stretched maximally to resist anterior tibial translation.
Clinical relevance
This information can be useful for further improving anatomical ACL reconstructions to better reproduce the 2 bundle functions. It may also be useful for designing postoperative rehabilitation regimens to prevent overstretch of the grafts.
Keywords: in vivo knee kinematics, gait, anterior cruciate ligament (ACL), ACL bundles
Numerous studies have investigated the ACL biomechanics under various loading conditions.1,17,18,28,40 Early in vitro studies using cadaveric knees have found that the anteromedial (AM) bundle of the ACL functions more in high flexion angles while the posterolateral (PL) bundle is stressed more at low flexion angles during passive knee flexion or under an anterior tibial load.1,17,18,40 However, under simulated muscle loads, the ACL was found to function mainly at low flexion angles.30,43,46 The ACL deformation during in vivo joint motion, either using surface strain measurements4,5,12,14,15 or apparent elongation patterns of the ACL bundles,21,26 was found to be higher at low flexion angles.
Most previous studies examined the ACL function during flexion-extension motion of the knee.1,17,18,21,30,31,34,37,40 However, little is known about the ACL function during other functional activities.9,12,13 No data have been reported on the ACL function during gait. Because gait is the most common daily activity of the knee, this knowledge is critical for designing ACL reconstruction techniques and postoperative rehabilitation regimens.
Recently, we used a combined dual fluoroscopic imaging system and MR technique to measure dynamic knee joint motion during gait on a treadmill.25,27,29 In this study, we constructed the attachment areas of the ACL on the femoral and tibial bony surfaces of the subjects recruited from a previous study25 and investigated the relative bundle elongation and the orientations of AM and PL bundles of the ACL during the stance phase of gait. Specifically, we examined the correlation between the ACL bundle elongation and the knee kinematics in 6 degrees of freedom.25 We hypothesized that during the stance phase of treadmill gait, the AM and PL bundles have distinct functional behavior.
MATERIAL AND METHODS
Six Degree of Freedom Knee Kinematics During Gait
Eight subjects (6 men and 2 women) with no history of knee injury, surgery, or systemic disease were recruited in a previous study under the institutional review board guidance.25 Each patient signed an institutional review board-approved consent form. One knee of each subject (3 right and 5 left) was scanned in extension using a 3-Tesla scanner (MAGNETOM Trio, Siemens, Erlangen, Germany) and a double-echo water excitation sequence. The MR images were placed in parallel planes separated by 1 mm in modeling software (Rhinoceros, Robert McNeel & Associates, Seattle, Washington), and the contours of the femur and tibia were manually digitized to construct the 3-dimensional (3D) computer models of the knee.21
Next, the dual fluoroscopic imaging system, previously validated for treadmill gait analysis,27,29 was used to determine knee kinematics during the stance phase of gait.25 The subject practiced the gait on the treadmill for 1 minute at a treadmill speed of 1.5 miles per hour (0.67 m/s). Two thin pressure sensors (Force Sensor Resistor, Interlink Electronics Specifications, Camarillo, California) were fixed to the bottom of each shoe to determine the moment between heel strike and toe-off of the stance phase during gait. The knee was imaged during 3 consecutive strides at a frame rate of 30 Hz. The stance phase was analyzed in 4 portions: loading response, 0% to 15%; midstance phase, 15% to 55%; terminal extension, 55% to 85%; and preswing phase, 85% to 100%.
After testing, the fluoroscopic images were imported into the modeling software and placed in a way so as to reproduce the geometry of the fluoroscopes during testing. The 3D MRI-based bone models of the knee were imported into the software and manipulated in 6 degrees of freedom until the projections of each model matched the outline of the knee on each fluoroscopic image, reproducing the position of the knee during gait. This process was repeated at each 10% progress of the stance phase from heel strike to toe-off.25
Determination of ACL Kinematics
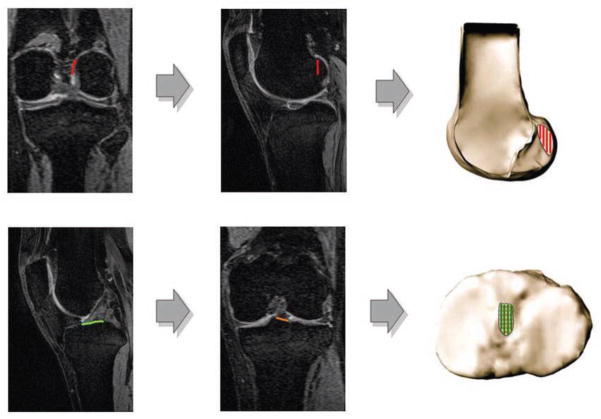
The femoral origin and tibial insertion site of the ACL were created using MR images of the knee in both sagittal and coronal planes (Figure 1). The method for construction of ACL attachments on the femur and tibia has been extensively used and validated in previous studies.11,24,26,42 The attachment areas were then divided into 2 functional bundles using an established protocol.19,21,26 Figure 2 shows a 3D anatomical model of the knee including ACL attachment areas.
Figure 1.
Sagittal and coronal plane magnetic resonance images of the knee were digitized and used to create the femoral and tibial attachment areas of the ACL bundles.
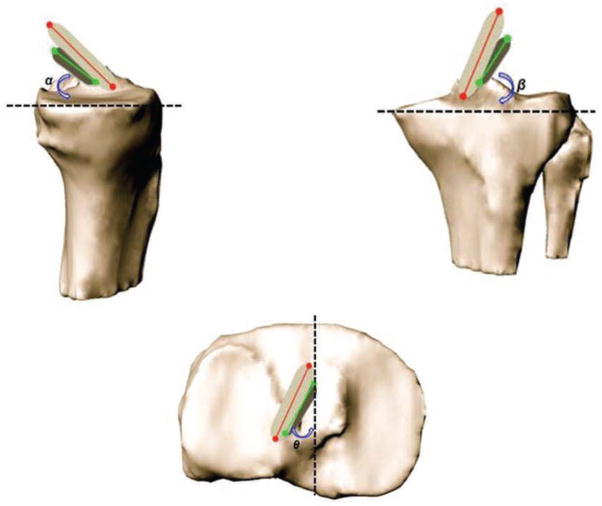
Figure 2.
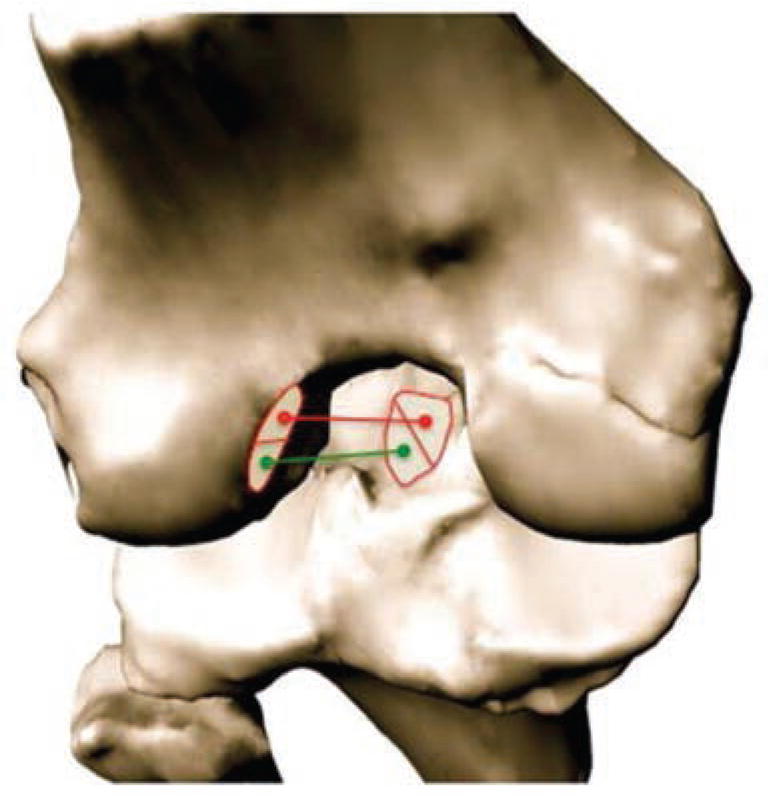
The 3-dimensional anatomical model of the knee including ACL attachment areas was created. The attachment areas were divided into 2 functional bundles using an established protocol.
We measured the length and orientation of each bundle to investigate the kinematics of the ACL throughout the stance phase of gait. Length was defined as the distance from the centroid of the femoral attachment to the centroid of the tibial attachment of each bundle at each time point of the stance phase. The lengths of the 2 bundles measured at the position during MRI scan were used as reference lengths to calculate the relative elongation of AM and PL bundles during gait. The length of each bundle normalized by its reference length was defined as the relative elongation. The orientation of each bundle was described using 3 angles: sagittal plane elevation, coronal plane elevation, and transverse plane deviation (Figure 3). The sagittal plane elevation angle (α) was defined as the angle between each bundle projected onto the sagittal plane of the tibia and the anteroposterior (AP) axis.21 The coronal plane elevation angle (β) was defined as the angle between the bundles projected onto the coronal plane of the tibia and the mediolateral axis of the coordinate system.37 The deviation angle (θ) was defined as the angle between the projection of each bundle on the tibial plateau and the AP axis.21
Figure 3.
The orientation of each bundle was described using 3 angles: sagittal plane elevation, coronal plane elevation, and transverse plane deviation. The sagittal plane elevation angle (α) was defined as the angle between each bundle projected onto the sagittal plane of the tibia and the anteroposterior axis. The coronal plane elevation angle (β) was defined as the angle between the bundles projected onto the coronal plane of the tibia and the mediolateral axis of the coordinate system. The deviation angle (θ) was defined as the angle between the projection of each bundle on the tibial plateau and the AP axis.
A 2-way repeated-measures analysis of variance was used to compare the function between the AM and PL bundles and to detect whether each phase of the gait cycle had a statistically significant effect on the relative elongation, sagittal plane elevation, coronal plane elevation, and transverse plane deviation. The Student-Newman-Keuls test was used to detect the differences between means when significant differences were detected. Differences were considered statistically significant when P < .05. The relationship between the relative elongations (outcomes) of AM and PL bundles and the predictor variables (anterior-posterior and medial-lateral femoral translations and flexion-extension, internal-external and varus-valgus femoral rotations) were evaluated by a multiple regression analysis. The kinematics used in this analysis have been reported in a previous publication that investigated the tibiofemoral kinematics of the normal knee during the stance phase of treadmill gait.25
RESULTS
Relative Elongation of ACL Bundles
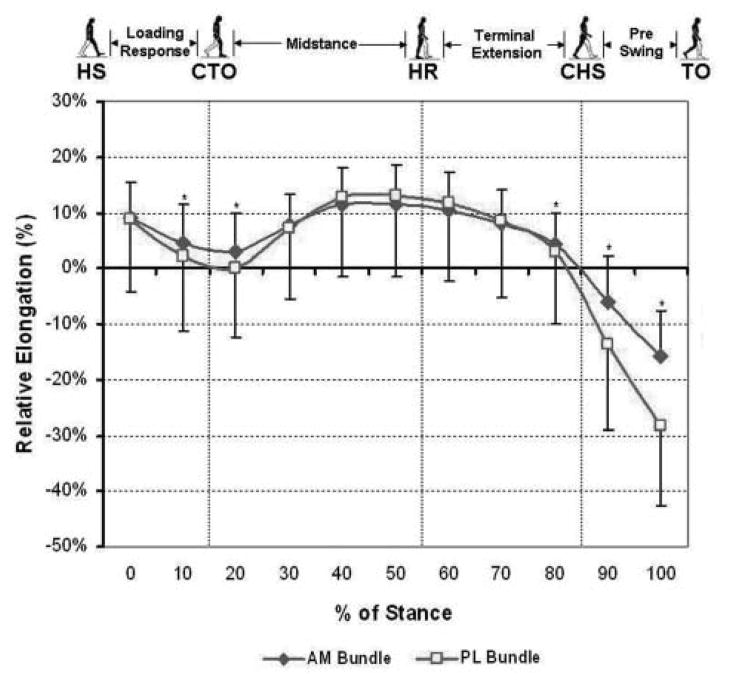
At heel strike, the AM bundle had a relative elongation of 9% ± 7% (Figure 4). That decreased to 3% ± 7% at 20% of the stance phase. Thereafter, the elongation increased gradually and reached the second peak of 12% ± 7% at 50% of the stance. The relative elongation between 40% and 60% of the stance was relatively constant (P > .05). Thereafter, the elongation decreased and the lowest elongation of −16% ± 8% was at toe-off.
Figure 4.
The relative elongation of the anteromedial and pos-terolateral bundles from heel strike to toe-off during the stance phase of gait. *, P < .05; HS, heel strike; CTO, contralateral toe-off; HR, heel rise; CHS, contralateral heel strike; TO, toe-off.
The trend of the relative elongation for the PL bundle followed the same pattern as the AM bundle (Figure 4). The first peak of the elongation of the PL bundle was 9% ± 13% at heel strike. The second peak of 13% ± 15% was found at late midstance. The lowest elongation of −28% ± 14% was at toe-off. No significant difference was also found between 40% and 60% of stance (P > .05).
Correlation Between the Relative Elongation of the ACL Bundles and the Knee Kinematics
Anteromedial Bundle
The regression analysis was performed by an entry method that resulted in a significant model. The included predictors explained 63.3% of the variance in the relative elongation of the AM bundle during the stance phase of gait (R2 = .633, P < .0001). Flexion-extension was the strongest predictor of the relative elongation of the AM bundle. The model demonstrated a negative correlation between knee flexion and relative elongation of the AM bundle; that is, as the knee flexed, the length of the AM bundle decreased and vice versa (Figure 5). A 58.0% variance in the relative elongation of the AM bundle was account for by flexion-extension alone (R2 = .580, P < .0001). A significant change in the value of R2 was observed when additional predictor variables (anterior-posterior and medial-lateral femoral translations and internal-external and varus-valgus femoral rotations) were added to the model (Δ R2 = .053, P < .025). The predictor variables that significantly contributed to the model were anterior-posterior translation and internal-external rotations (Table 1).
Figure 5.
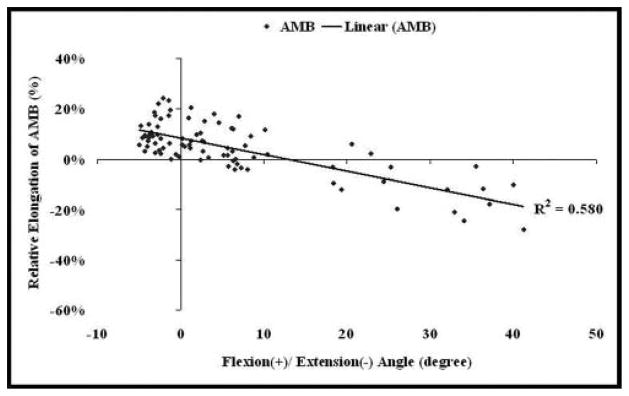
Relationship between relative elongation of the anteromedial bundle and the knee flexion angle during stance phase of gait. AMB, anteromedial bundle.
TABLE 1.
Summary of the Multiple Regression Analysis Between Relative Elongation of Anteromedial Bundle and the Kinematic Variablesa
| Model | B | SE B | β | P |
|---|---|---|---|---|
| Constant (B0) | .084 | .008 | ||
| Flexion (+)/extension (−) | −.007 | .001 | −.761 | <.0001 |
| Constant (B0) | .202 | .056 | ||
| Flexion (+)/extension (−) | −.007 | .002 | −.785 | <.0001 |
| Anterior (+)/posterior (−) | .021 | .009 | .418 | .020 |
| External (+)/internal (−) | −.010 | .004 | −.285 | .018 |
SE, standard error; β, standardized coefficients.
Posterolateral Bundle
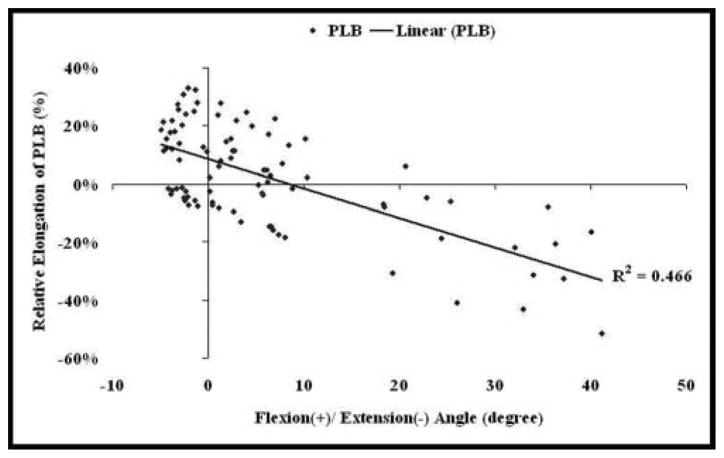
Similar to the AM bundle multiple regression analysis, an entry method was used in the multiple regression analysis to evaluate the relationship between the relative elongation of the PL bundle and the kinematic variables. The included predictors accounted for 51.2% of the variance in the relative elongation of the PL bundle during the stance phase of gait (R2 = .512, P < .0001). However, similar to the relative elongation of the AM bundle, the strongest predictor of the relative elongation of the PL bundle was again flexion-extension of the knee (Figure 6). Flexion-extension during the stance phase alone explained 46.6% of the variance in the relative elongation of the PL bundle (R2 = .466, P < .0001). Addition of the predictor variables (anterior-posterior and medial-lateral femoral translations and internal-external and varus-valgus femoral rotations) did not significantly change the R2 of the model that had flexion-extension as the only predictor (Δ R2 = .046, P < .109). Predictor variables with significant contributions to the model along with their beta values are reported in Table 2.
Figure 6.
Relationship between relative elongation of the posterolateral bundle and the knee flexion angle during stance phase of gait. PLB, posterolateral bundle.
TABLE 2.
Summary of the Multiple Regression Analysis Between Relative Elongation of Posterolateral Bundle and the Kinematic Variablesa
| Model | B | SE B | β | P |
|---|---|---|---|---|
| Constant (B0) | .085 | .016 | ||
| Flexion (+)/extension (−) | −.010 | .001 | −.682 | <.0001 |
| Constant (B0) | .388 | .111 | ||
| Flexion (+)/extension (−) | −.014 | .003 | −.920 | <.0001 |
| Anterior (+)/posterior (−) | .040 | .018 | .460 | .026 |
| Varus (+) valgus (−) | −.038 | .019 | −.248 | .044 |
SE, standard error; β, standardized coefficients.
Orientation of ACL Bundles
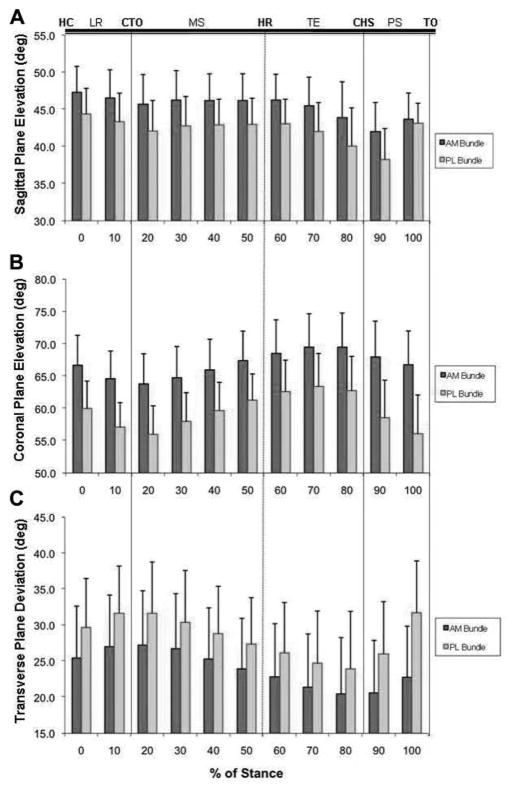
Sagittal Plane Elevation
The PL bundle was more oblique in the sagittal plane elevation than the AM bundle throughout the stance phase of gait (P < .05) (Figure 7A). At heel strike, the AM and PL bundles reached the maximal elevation (47.3° ± 3.5° and 44.3° ± 3.5°, respectively). The elevations of both bundles decreased until 20% progress of the stance phase (45.7° ± 4.0° and 42.1° ± 4.1°, respectively). The elevation had no significant changes for each bundle between 20% and 70% progress of the stance. Thereafter, the sagittal plane elevations of the AM and PL bundles reached minimum at 90% progress of the stance (42.0° ± 3.9° and 38.2° ± 4.2°, respectively) and increased again until toe-off.
Figure 7.
The sagittal plane elevation (A), coronal plane elevation (B), and transverse plane deviation (C) of the ante-romedial and posterolateral bundles from heel strike to toe-off during the stance phase of gait. *, P < .05.
Coronal Plane Elevation
The coronal plane elevation of the PL bundle showed a similar trend as the AM bundle. The obliquity in the AM bundle was less than that of the PL bundle during the stance phase (P < .05) (Figure 7B). The AM and PL bundle reached the first peak of the coronal plane elevation (66.6° ± 4.7° and 60.0° ± 4.2°, respectively) at heel strike, and then significantly decreased until 20% of the stance (63.7° ± 4.7° and 56.0° ± 4.5°, respectively). Afterward, the coronal elevation began to increase until late terminal extension. The maximal coronal elevations were at 80% progress of the stance phase (69.5° ± 5.3° and 62.7° ± 5.4°, for AM and PL bundles, respectively) and there was no significant difference for each bundle between 60% and 80% progress of stance. Thereafter, the coronal plane elevation decreased until toe-off.
Transverse Plane Deviation
The pattern of the PL bundle in transverse plane deviation also followed that of the AM bundle, whereas the PL bundle deviated more laterally than the AM bundle (P <.05) through the stance phase of gait and shown in Figure 7C. At heel strike, the AM and PL bundles deviated laterally and peaked by 27.2° ± 7.6° and 31.6° ± 7.2°, respectively, at 20% progress of the stance. Thereafter, the deviation decreased significantly until the 80% of the stance (20.4° ± 7.8° for AM bundle vs 23.9°± 8.0° for PL bundle, respectively). It increased again toward toe-off.
DISCUSSION
This study investigated the kinematics of the 2 bundles of the ACL during the stance phase of gait. The data showed that the AM and PL bundles functioned in a similar manner and had peak elongation at 0% and 50% of the stance phase where the knee motion on the sagittal plane was found to be at full extension and hyperextension.25 The relative elongation of the 2 bundles was significantly correlated with knee flexion. The sagittal and coronal elevation decreased with increasing flexion, whereas the transverse plane deviation increased with flexion. The in vivo kinematics of the ACL bundles during walking demonstrate unique characteristics and are different from those measured during weightbearing knee flexion.21
Jordan et al21 used the dual fluoroscopic imaging system technique to measure the in vivo kinematics of the 2 bundles during the full range of weightbearing flexion (from 0° to 135° of flexion) and demonstrated that the AM bundle does not significantly change its length between 0° and 60° of flexion, whereas the length of PL bundle decreased with increasing flexion. Recently, several in vitro studies using either dial caliper or navigation system also showed similar results and indicated that the strain of the AM bundle was relatively constant but that of the PL bundle decreased with increasing flexion during passive flexion-extension motion tested.21,34,37,38 In the present study, the relative elongation of the 2 bundles during the stance phase decreased similarly with increasing flexion. However, we did not find the relative constant elongation pattern of the AM bundle with flexion throughout the stance phase, which is different from what was found during single-legged lunge by Jordan et al.21 This again indicated that the ACL function is activity-dependent or loading-dependent.
Our multiple regression analysis demonstrated a negative correlation between the relative elongation of both the bundles and knee flexion. Furthermore, it was found that knee flexion-extension was the most significant predictor of the relative elongation. Several studies have examined the in vivo strain behavior of the ACL during various activities such as active range of motion, passive range of motion, and squatting.3,5,6 These studies have reported a maximum ACL strain (2.8% to 3.8%) close to extension (5° to 10°) and found ACL strain to decrease with knee flexion during active range of motion. However, measurement of ACL strain at knee extension less than 5° to 10° was not feasible in these studies because of the potential impingement of strain transducers against the femoral intercondylar notch. Although we could not directly compare the ACL strain values between these studies because of the variations in the activities, we found a similar trend of increased ACL strain with knee extension and decreased strain with knee flexion. However, the transition from strained ACL to unstrained ACL occurred between 80% and 90% of stance phase where the knee flexion was 4.1° ± 1.6° and 21.9° ± 3.1°, respectively. On the contrary, this transition is reported to occur between a mean flexion angle from 35° to 48° during active range of motion.3,5,6 Although there is no clear explanation on the discrepancy between these studies, it could be partly explained by the differences in the activities used to measure ACL strain among the studies.
It is of note that at 50% of the stance, both bundles were maximally elongated, 12% for the AM bundle and 13% for the PL bundle. At this stage of the stance phase, the knee was in a slightly hyperextended position (average, 3.5°) and the leg was under full body weight, coupled with maximal anterior tibial translation (average, 4.0 mm), valgus rotation (average, 3.0°), and minimal internal rotation (average, 0.3°).25 Markolf et al33 showed that ACL tensile forces reach the peak as the knee approaches hyperextension. The relative elongation for each bundle between 40% and 60% progress of the stance also showed no significant differences (P > .05). These data implied that the ACL bundles were maximally loaded and elongated throughout the midstance, which differs with that reported by Shelbourne et al.41 They pointed out that the ACL was maximally loaded at the contralateral toe-off using multi-body mathematical modeling.
The previous biomechanical studies have shown that the AM and PL bundles have reciprocal functions in providing stability of the knee.17,18,40 The reciprocal function between the 2 bundles has been a rationale for tensioning strategies of grafts in double-bundle ACL reconstructions.10,45 However, some recent studies could not confirm the reciprocal function between the AM and PL bundles.21,35,43 Jordan et al21 found that the AM and PL bundles of ACL played a more important role in low flexion angles, with the 2 bundles reaching maximum length near extension and reducing length with flexion during weightbearing knee flexion. They concluded that the 2 bundles function in a complementary rather than reciprocal manner. Markolf et al35 implied that the AM bundle under different loading conditions was still loaded in a near-normal fashion after cutting the PL bundle. More recently, a biomechanical study using a robotic testing system to measure the in situ forces of the AM and PL bundles under various external loads indicated that the AM bundle carried the majority of the load at all flexion angles, whereas the PL bundle shared the load only at low flexion angles.43 Under simulated muscle loads, both bundles carried similar loads at all flexion angles.43 In the present study, no inversely proportional relative elongations between the 2 bundles were observed during gait. Therefore, these studies supported that both bundles supplement each other rather than function independently or reciprocally.
Our data on the ACL bundle orientations showed that the 2 bundles were not parallel throughout the stance of gait. The AM bundle was less oblique in the sagittal and coronal planes than the PL bundle throughout the stance phase (P < .05), while the PL bundle had significantly more lateral deviation than the AM bundle (P < .05). With increasing knee flexion, the sagittal plane and coronal plane elevation of the 2 bundles decreased, whereas the deviation angle increased. From a biomechanical point of view, the more oblique line of action of the ACL bundles would make them behave more efficiently in resisting translation or rotational loading. A different trend in transverse plane deviation was observed in our study compared with a previous in vivo study during single-legged lunge.21 In that study, the deviation angle of the AM bundle decreased with increasing flexion less than 90°, whereas for the PL bundle it decreased only at low flexion angles (0° to 30°).21 This difference may be due to lateral pivoting of the knee joint during normal walking23,25 compared with the medial pivoting during nonambulatory activities.8,16,20
Several studies measured strains of the ACL bundles or grafts by measuring the distances between 2 insertion points on the bony surfaces.21,26,37,44 These studies indicated that the 2 bundles of the ACL should be fixed at or near full extension in ACL reconstruction because the bundle lengths were longest at low flexion angles. Our data on the ACL bundle elongation during gait also indicated that the elongation of both bundles increased with extension and implied that the 2 bundles should be fixed at full extension to prevent overtensioning of the grafts.2,22,36 Nevertheless, the tensioning protocol for double-bundle grafts under full extension still needs to be further investigated to reproduce the synergistic function of the 2 bundles.
The present study may also provide implications for ACL patients on the regimen for postoperative rehabilitation. Although the previous studies reported that no significant difference was found between nonaccelerated and accelerated postoperation rehabilitation programs,7,32,39 it is still important to pay attention to avoid hyperextended knee motion during gait without crutches, so as to avoid overstretching of the ACL grafts. The flexion motion of the knee during gait should be allowed postoperatively because the elongation of the AM and PL bundle grafts would not increase with increasing flexion.21,26,44
Several technical limitations of this study should be noted. We measured the 2-point distance between the femoral and tibial insertions of each bundle throughout the stance phase of gait. Because the zero-strain reference lengths of the actual AM and PL bundles were not known, measuring the length on resting MRI position as the reference was used. Thus, the actual strain of the bundles could not be directly obtained. Further, only treadmill gait was studied. Other physiological loading conditions such as running or landing condition should be further researched.
In summary, this study investigated the in vivo kinematics of the ACL bundles during gait on a treadmill. During the complex loading condition of gait, the AM and PL bundles of the ACL are not isometric and have similar functional behavior during the stance phase. The 2 bundles of ACL were maximally elongated throughout the midstance, where they played a major role to resist the anterior tibial translation. Overall, both bundles supplement each other rather than function reciprocally during gait. This information can be useful for further understanding the in vivo function of the ACL bundles and evaluation of the kinematics in ACL grafts after ACL reconstruction during gait.
Acknowledgments
The authors gratefully acknowledge the support of the National Institutes of Health grants AR 052408 and AR051078.
Footnotes
One or more authors has declared a potential conflict of interest:
References
- 1.Amis AA, Dawkins GP. Functional anatomy of the anterior cruciate ligament: fibre bundle actions related to ligament replacements and injuries. J Bone Joint Surg Br. 1991;73(2):260–267. doi: 10.1302/0301-620X.73B2.2005151. [DOI] [PubMed] [Google Scholar]
- 2.Asagumo H, Kimura M, Kobayashi Y, Taki M, Takagishi K. Anatomic reconstruction of the anterior cruciate ligament using double-bundle hamstring tendons: surgical techniques, clinical outcomes, and complications. Arthroscopy. 2007;23(6):602–609. doi: 10.1016/j.arthro.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 3.Beynnon B, Howe JG, Pope MH, Johnson RJ, Fleming BC. The measurement of anterior cruciate ligament strain in vivo. Int Orthop. 1992;16(1):1–12. doi: 10.1007/BF00182976. [DOI] [PubMed] [Google Scholar]
- 4.Beynnon BD, Fleming BC. Anterior cruciate ligament strain in-vivo: a review of previous work. J Biomech. 1998;31(6):519–525. doi: 10.1016/s0021-9290(98)00044-x. [DOI] [PubMed] [Google Scholar]
- 5.Beynnon BD, Fleming BC, Johnson RJ, et al. Anterior cruciate ligament strain behavior during rehabilitation exercises in vivo. Am J Sports Med. 1995;23(1):24–34. doi: 10.1177/036354659502300105. [DOI] [PubMed] [Google Scholar]
- 6.Beynnon BD, Johnson RJ, Fleming BC, Stankewich CJ, Renstrom PA, Nichols CE. The strain behavior of the anterior cruciate ligament during squatting and active flexion-extension: a comparison of an open and a closed kinetic chain exercise. Am J Sports Med. 1997;25(6):823–829. doi: 10.1177/036354659702500616. [DOI] [PubMed] [Google Scholar]
- 7.Beynnon BD, Uh BS, Johnson RJ, et al. Rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind comparison of programs administered over 2 different time intervals. Am J Sports Med. 2005;33(3):347–359. doi: 10.1177/0363546504268406. [DOI] [PubMed] [Google Scholar]
- 8.Blaha JD, Mancinelli CA, Simons WH, Kish VL, Thyagarajan G. Kinematics of the human knee using an open chain cadaver model. Clin Orthop Relat Res. 2003;410:25–34. doi: 10.1097/01.blo.0000063564.90853.ed. [DOI] [PubMed] [Google Scholar]
- 9.Cerulli G, Benoit DL, Lamontagne M, Caraffa A, Liti A. In vivo anterior cruciate ligament strain behaviour during a rapid deceleration movement: case report. Knee Surg Sports Traumatol Arthrosc. 2003;11(5):307–311. doi: 10.1007/s00167-003-0403-6. [DOI] [PubMed] [Google Scholar]
- 10.Colombet P, Robinson J, Jambou S, Allard M, Bousquet V, Lavigne C. Two-bundle, four-tunnel anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14(7):629–636. doi: 10.1007/s00167-005-0002-9. [DOI] [PubMed] [Google Scholar]
- 11.Edwards A, Bull AM, Amis AA. The attachments of the anteromedial and posterolateral fibre bundles of the anterior cruciate ligament. Part 2: femoral attachment. Knee Surg Sports Traumatol Arthrosc. 2008;16(1):29–36. doi: 10.1007/s00167-007-0410-0. [DOI] [PubMed] [Google Scholar]
- 12.Fleming BC, Beynnon BD, Renstrom PA, et al. The strain behavior of the anterior cruciate ligament during stair climbing: an in vivo study. Arthroscopy. 1999;15(2):185–191. doi: 10.1053/ar.1999.v15.015018. [DOI] [PubMed] [Google Scholar]
- 13.Fleming BC, Beynnon BD, Renstrom PA, Peura GD, Nichols CE, Johnson RJ. The strain behavior of the anterior cruciate ligament during bicycling: an in vivo study. Am J Sports Med. 1998;26(1):109–118. doi: 10.1177/03635465980260010301. [DOI] [PubMed] [Google Scholar]
- 14.Fleming BC, Ohlen G, Renstrom PA, Peura GD, Beynnon BD, Badger GJ. The effects of compressive load and knee joint torque on peak anterior cruciate ligament strains. Am J Sports Med. 2003;31(5):701–707. doi: 10.1177/03635465030310051101. [DOI] [PubMed] [Google Scholar]
- 15.Fleming BC, Renstrom PA, Beynnon BD, et al. The effect of weight-bearing and external loading on anterior cruciate ligament strain. J Biomech. 2001;34(2):163–170. doi: 10.1016/s0021-9290(00)00154-8. [DOI] [PubMed] [Google Scholar]
- 16.Freeman MA, Pinskerova V. The movement of the normal tibio-femoral joint. J Biomech. 2005;38(2):197–208. doi: 10.1016/j.jbiomech.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 17.Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE. Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res. 2004;22(1):85–89. doi: 10.1016/S0736-0266(03)00133-5. [DOI] [PubMed] [Google Scholar]
- 18.Girgis FG, Marshall JL, Monajem A. The cruciate ligaments of the knee joint: anatomical, functional and experimental analysis. Clin Orthop Relat Res. 1975;106:216–231. doi: 10.1097/00003086-197501000-00033. [DOI] [PubMed] [Google Scholar]
- 19.Hosseini A, Gill TJ, Li G. In vivo anterior cruciate ligament elongation in response to axial tibial loads. J Orthop Sci. 2009;14(3):298–306. doi: 10.1007/s00776-009-1325-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br. 2000;82(8):1189–1195. doi: 10.1302/0301-620x.82b8.10717. [DOI] [PubMed] [Google Scholar]
- 21.Jordan SS, DeFrate LE, Nha KW, Papannagari R, Gill TJ, Li G. The in vivo kinematics of the anteromedial and posterolateral bundles of the anterior cruciate ligament during weightbearing knee flexion. Am J Sports Med. 2007;35(4):547–554. doi: 10.1177/0363546506295941. [DOI] [PubMed] [Google Scholar]
- 22.Kondo E, Yasuda K. Second-look arthroscopic evaluations of anatomic double-bundle anterior cruciate ligament reconstruction: relation with postoperative knee stability. Arthroscopy. 2007;23(11):1198–1209. doi: 10.1016/j.arthro.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 23.Koo S, Andriacchi TP. The knee joint center of rotation is predominantly on the lateral side during normal walking. J Biomech. 2008;41(6):1269–1273. doi: 10.1016/j.jbiomech.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kopf S, Musahl V, Tashman S, Szczodry M, Shen W, Fu FH. A systematic review of the femoral origin and tibial insertion morphology of the ACL. Knee Surg Sports Traumatol Arthrosc. 2009;17(3):213–219. doi: 10.1007/s00167-008-0709-5. [DOI] [PubMed] [Google Scholar]
- 25.Kozanek M, Hosseini A, Liu F, et al. Tibiofemoral kinematics and condylar motion during the stance phase of gait. J Biomech. 2009;42(12):1877–1884. doi: 10.1016/j.jbiomech.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li G, Defrate LE, Rubash HE, Gill TJ. In vivo kinematics of the ACL during weight-bearing knee flexion. J Orthop Res. 2005;23(2):340–344. doi: 10.1016/j.orthres.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 27.Li G, Kozanek M, Hosseini A, Liu F, Van de Velde SK, Rubash HE. New fluoroscopic imaging technique for investigation of 6 DOF knee kinematics during treadmill gait. J Orthop Surg Res. 2009;4:6. doi: 10.1186/1749-799X-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li G, Rudy TW, Sakane M, Kanamori A, Ma CB, Woo SL. The importance of quadriceps and hamstring muscle loading on knee kinematics and in-situ forces in the ACL. J Biomech. 1999;32(4):395–400. doi: 10.1016/s0021-9290(98)00181-x. [DOI] [PubMed] [Google Scholar]
- 29.Li G, Van de Velde SK, Bingham JT. Validation of a non-invasive fluoroscopic imaging technique for the measurement of dynamic knee joint motion. J Biomech. 2008;41(7):1616–1622. doi: 10.1016/j.jbiomech.2008.01.034. [DOI] [PubMed] [Google Scholar]
- 30.Li G, Zayontz S, Most E, DeFrate LE, Suggs JF, Rubash HE. In situ forces of the anterior and posterior cruciate ligaments in high knee flexion: an in vitro investigation. J Orthop Res. 2004;22(2):293–297. doi: 10.1016/S0736-0266(03)00179-7. [DOI] [PubMed] [Google Scholar]
- 31.Lo J, Muller O, Wunschel M, Bauer S, Wulker N. Forces in anterior cruciate ligament during simulated weight-bearing flexion with anterior and internal rotational tibial load. J Biomech. 2008;41(9):1855–1861. doi: 10.1016/j.jbiomech.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 32.Majima T, Yasuda K, Tago H, Tanabe Y, Minami A. Rehabilitation after hamstring anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2002;397:370–380. doi: 10.1097/00003086-200204000-00043. [DOI] [PubMed] [Google Scholar]
- 33.Markolf KL, Gorek JF, Kabo JM, Shapiro MS. Direct measurement of resultant forces in the anterior cruciate ligament: an in vitro study performed with a new experimental technique. J Bone Joint Surg Am. 1990;72(4):557–567. [PubMed] [Google Scholar]
- 34.Markolf KL, Park S, Jackson SR, McAllister DR. Anterior-posterior and rotatory stability of single and double-bundle anterior cruciate ligament reconstructions. J Bone Joint Surg Am. 2009;91(1):107–118. doi: 10.2106/JBJS.G.01215. [DOI] [PubMed] [Google Scholar]
- 35.Markolf KL, Park S, Jackson SR, McAllister DR. Contributions of the posterolateral bundle of the anterior cruciate ligament to anterior-posterior knee laxity and ligament forces. Arthroscopy. 2008;24(7):805–809. doi: 10.1016/j.arthro.2008.02.012. [DOI] [PubMed] [Google Scholar]
- 36.Otsubo H, Shino K, Nakamura N, Nakata K, Nakagawa S, Koyanagi M. Arthroscopic evaluation of ACL grafts reconstructed with the anatomical two-bundle technique using hamstring tendon autograft. Knee Surg Sports Traumatol Arthrosc. 2007;15(6):720–728. doi: 10.1007/s00167-006-0274-8. [DOI] [PubMed] [Google Scholar]
- 37.Pearle AD, Shannon FJ, Granchi C, Wickiewicz TL, Warren RF. Comparison of 3-dimensional obliquity and anisometric characteristics of anterior cruciate ligament graft positions using surgical navigation. Am J Sports Med. 2008;36(8):1534–1541. doi: 10.1177/0363546508315536. [DOI] [PubMed] [Google Scholar]
- 38.Robinson J, Stanford FC, Kendoff D, Stuber V, Pearle AD. Replication of the range of native anterior cruciate ligament fiber length change behavior achieved by different grafts: measurement using computer-assisted navigation. Am J Sports Med. 2009;37:1406–1411. doi: 10.1177/0363546509331941. [DOI] [PubMed] [Google Scholar]
- 39.Rosen MA, Jackson DW, Atwell EA. The efficacy of continuous passive motion in the rehabilitation of anterior cruciate ligament reconstructions. Am J Sports Med. 1992;20(2):122–127. doi: 10.1177/036354659202000205. [DOI] [PubMed] [Google Scholar]
- 40.Sakane M, Fox RJ, Woo SL, Livesay GA, Li G, Fu FH. In situ forces in the anterior cruciate ligament and its bundles in response to anterior tibial loads. J Orthop Res. 1997;15(2):285–293. doi: 10.1002/jor.1100150219. [DOI] [PubMed] [Google Scholar]
- 41.Shelbourne KB, Pandy MG, Anderson FC, Torry MR. Pattern of anterior cruciate ligament force in normal walking. J Biomech. 2004;37(6):797–805. doi: 10.1016/j.jbiomech.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 42.Siebold R, Ellert T, Metz S, Metz J. Tibial insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: morphometry, arthroscopic landmarks, and orientation model for bone tunnel placement. Arthroscopy. 2008;24(2):154–161. doi: 10.1016/j.arthro.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 43.Wu J-L, Seon JK, Gadikota HR, et al. In-situ forces in the anteromedial and posterolateral bundles of the anterior cruciate ligament under simulated functional loading conditions. Am J Sports Med. 2010;38(3):558–563. doi: 10.1177/0363546509350110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yasuda K, Ichiyama H, Kondo E, Miyatake S, Inoue M, Tanabe Y. An in vivo biomechanical study on the tension-versus-knee flexion angle curves of 2 grafts in anatomic double-bundle anterior cruciate ligament reconstruction: effects of initial tension and internal tibial rotation. Arthroscopy. 2008;24(3):276–284. doi: 10.1016/j.arthro.2007.08.031. [DOI] [PubMed] [Google Scholar]
- 45.Yasuda K, Kondo E, Ichiyama H, et al. Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy. 2004;20(10):1015–1025. doi: 10.1016/j.arthro.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 46.Yoo JD, Papannagari R, Park SE, DeFrate LE, Gill TJ, Li G. The effect of anterior cruciate ligament reconstruction on knee joint kinematics under simulated muscle loads. Am J Sports Med. 2005;33(2):240–246. doi: 10.1177/0363546504267806. [DOI] [PubMed] [Google Scholar]