Abstract
Background
Patients with unilateral ligament deficiency are believed to have altered kinematics of the contralateral knee, increasing the risk of contralateral joint injury. Therefore, the contralateral knees might not be a reliable normal kinematic control.
Purpose
To compare the in vivo kinematics of the uninjured contralateral knees of patients with anterior or posterior cruciate ligament deficiency with knee kinematics of age-matched patients without joint injury.
Study Design
Controlled laboratory study.
Methods
Ten subjects with bilateral healthy knees, 10 patients with acute unilateral anterior cruciate ligament injury, and 10 with acute unilateral posterior cruciate ligament injury participated in this study. Kinematics were measured from 0° to 90° of flexion using imaging and 3-dimensional modeling.
Results
No significant differences were found across the groups in all rotations and translations during weightbearing flexion (P > .9).
Conclusion
Patients with unilateral cruciate ligament deficiency did not alter kinematics of the contralateral uninjured knee during weightbearing flexion. In addition, these findings suggest that the included patients with anterior cruciate ligament or posterior cruciate ligament deficiency did not have preexisting abnormal kinematics of the knee.
Clinical Relevance
As the contralateral joint kinematics of the injured patients were not affected by the ipsilateral ligament injury in the short term, physicians and researchers might use the contralateral knee as a reliable normal kinematic control.
Keywords: cruciate ligament, knee kinematics, contralateral knee, imaging
Much of the current knowledge about the in vivo knee kinematics in anterior cruciate ligament (ACL) or posterior cruciate ligament (PCL) deficiency is based on studies comparing the kinematics of the injured knee to that of the contralateral uninjured side.3,9,11,16,18 Both ACL and PCL deficiency have been shown to alter knee kinematics when compared with the intact contralateral side.3,11,16 However, it has been suggested in the literature that patients with unilateral cruciate ligament deficiency have altered kinematics of the contralateral knee.6 Therefore, the contralateral uninjured knee might not be a reliable normal kinematic control.6 In addition, it has been theorized that the altered kinematics might increase the risk of bilateral joint injury.6 To our knowledge, no data have been reported on the effect of acute unilateral deficiency of either ACL or PCL on the 6 degrees of freedom kinematics of the contralateral uninjured knee joint during in vivo weightbearing flexion.
The purpose of this study was to investigate the in vivo kinematics of the contralateral uninjured knees of patients with either ACL or PCL deficiency and to compare the kinematics with an age-matched group of subjects with bilateral healthy knees. Kinematics of the knee joint were measured during weightbearing flexion using a combined magnetic resonance imaging (MRI) and dual-orthogonal fluoroscopic technique.3,21 We hypothesized that abnormal kinematics are present in the uninjured contralateral knees of patients with a unilateral rupture.
MATERIALS AND METHODS
Patient Recruitment
Thirty subjects were recruited for this study (Table 1). Ten patients had unilateral ACL rupture and healthy contralateral knees, 10 patients had unilateral PCL rupture and healthy contralateral knees, and 10 subjects had no history of injury, surgery, or disease in both knees. The status of each ACL and PCL was verified on physical examination by an orthopaedic surgeon as well as on MRI examination performed as a part of this study. Additionally, the status of each injured ACL and PCL was confirmed during arthroscopy performed after the completion of this study. The purpose of the study was explained in detail to all participants at the time of recruitment. Each participant signed an institutional review board–approved consent form.
TABLE 1.
Basic Characteristics of 30 Included Subjectsa
| Healthy | Contralateral ACL Injury | Contralateral PCL Injury | |
|---|---|---|---|
| N per group | 10 | 10 | 10 |
| Side | 5 right, 5 left | 5 right, 5 left | 5 right, 5 left |
| Age, y | 30 ± 7 | 28 ± 7 | 39 ± 17 |
| Gender | 5 female, 5 male | 4 female, 6 male | 3 female, 7 male |
| Time from injury, mo | N/A | 2 ± 2.5 | 4 ± 2.1 |
| Height, cm | 174 ± 11 | 176 ± 6 | 175 ± 8 |
| Weight, kg | 79 ± 29 | 83 ± 13 | 78 ± 12 |
| BMI, kg/m2 | 23 ± 2 | 27 ± 4 | 25 ± 3 |
ACL, anterior cruciate ligament; PCL, posterior cruciate ligament; N/A, not applicable; BMI, body mass index.
Three-Dimensional Knee Model
The technique used in this study has been used extensively to study knee joint kinematics.3,4,9,16,21 The contralateral uninjured knees of patients in the ACL and PCL injury group were imaged as well as the knees of the healthy cohort using a 1.5-T MR scanner (Signa, General Electric, Fairfield, Connecticut); knees were scanned in a relaxed, extended position using a fat-suppressed 3-dimensional (3D) spoiled-gradient echo sequence. The MRI scans were used to generate sagittal plane images (512 × 512 pixels) with a field of view of 16 × 16 cm and 1 mm spacing. The MR images were imported into solid modeling software (Rhinoceros; Robert McNeel and Associates, Seattle, Washington) and manually digitized to outline the contours of the femur and tibia. Afterward, these outlines were used to reconstruct 3D geometric models of the knee.3
Dual-Orthogonal Fluoroscopic System Setup
Next, each patient was imaged with a dual-orthogonal fluoroscopic system. The patient performed a quasistatic lunge while standing within the C-arms of the 2 fluoroscopes (OEC 9800; General Electric) positioned in orthogonal planes to simultaneously capture images of the knee.9–11,16 Each patient placed his or her target knee within the field of view of the 2 fluoroscopes and remained still while images (1000 × 1000 pixels) were captured simultaneously from 2 orthogonal directions at 0° and 30°, 60°, and 90° of flexion. The flexion angle of a subject was monitored using a goniometer.
Two virtual cameras were created to represent the X-ray sources of the 2 fluoroscopes using the modeling software. The radiographs were placed to reproduce the position of the 2 intensifiers of the fluoroscopes. The 3D knee model was imported into the virtual fluoroscopic system and manually oriented under visual inspection in 6 degrees of freedom until its projection as viewed from the 2 directions matched the outlines of the 2 fluoroscopic images. Once the knee model was matched to the fluoroscopic images, the position of the model reproduced the position of the subject’s knee during the quasistatic lunge. The method has been rigorously validated and has an accuracy of 0.1 mm in translation and 0.18° in rotation.12
Knee Kinematics
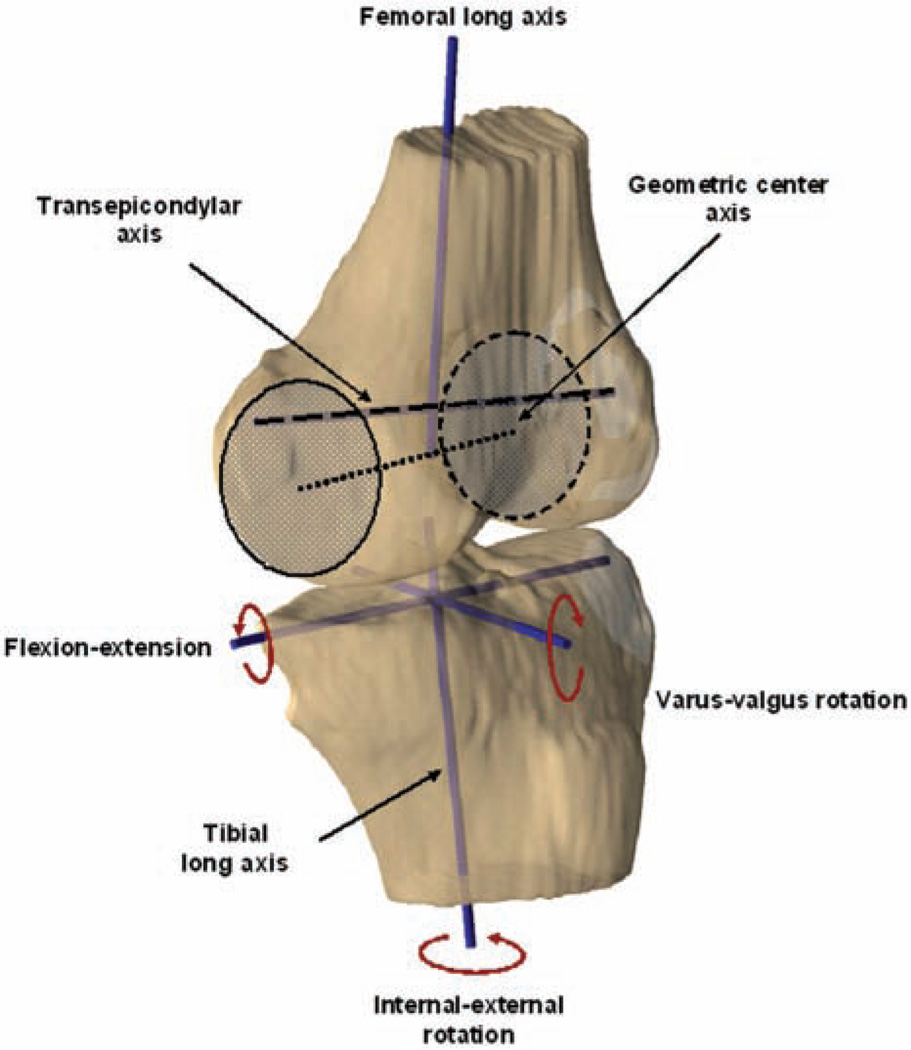
Two different coordinate systems, widely adopted by numerous investigators, were used separately to analyze the kinematics of the knee.14 One coordinate system was based on the transepicondylar axis of the femur,5,15,22 and the other system used the geometric center axis of the femur5 (Figure 1).
Figure 1.
Coordinate systems used to define knee joint motion.
First the kinematics were measured using a coordinate system based on the transepicondylar axis of the femur. The long axis of the tibial shaft was drawn first. An anteriorposterior axis and a medial-lateral axis were drawn perpendicular to the long axis of the tibia. The axes intersected at the center of the tibial plateau to form a Cartesian coordinate system. Next, 2 axes were drawn on the femur: the long axis of the femur and the transepicondylar line. Translation was defined as the motion of the midpoint of the transepicondylar line relative to the tibial coordinate system.14 Femoral translations were then converted to tibial translations so the data could be reported in a manner consistent with previous studies in the sports medicine literature. The rotation of the knee was measured in a fashion similar to that described by Grood and Suntay.8,20 Flexion was defined as the angle between the long axes of the femur and tibia, projected onto the sagittal plane of the tibia. Internal-external rotation was defined as rotation about the long axis of the tibia. Varus-valgus rotation was defined as the angle between the long axis of the tibia and the transepicondylar line projected onto the frontal plane of the tibia, with the neutral position corresponding to a right angle between these 2 axes. In this fashion, anterior-posterior, medial-lateral, and superior-inferior translations and internal-external and varus-valgus rotations of the tibia relative to the femur were determined during the quasistatic lunge.3 These data were then averaged across each patient group as a function of flexion.
Subsequently, the knee kinematics were measured again using a geometric center axis of the femur. For the femoral coordinate system, the flexion axis (geometric center axis) was constructed by fitting circles to the medial and lateral condyles and by connecting the centers of these circles with a line (Figure 1). The long axis was drawn parallel to the posterior wall of the femoral shaft in the sagittal plane. The middle point of the flexion axis was used as the origin of the femoral coordinate system. The anterior-posterior axis was obtained as the product of intersection of the flexion and the long axis. The tibial coordinate system remained the same as in previous measurement.
Statistical Analysis
A 1-way analysis of variance (ANOVA) was used as a significance test to detect differences in kinematics between the study groups. The level of significance was set at P < .05. When no significant differences were detected, a power analysis was performed to ensure that the statistical tests had sufficient statistical power. Statistical software Statistica (StatSoft Inc, Tulsa, Oklahoma) was used to perform the statistical analyses.
RESULTS
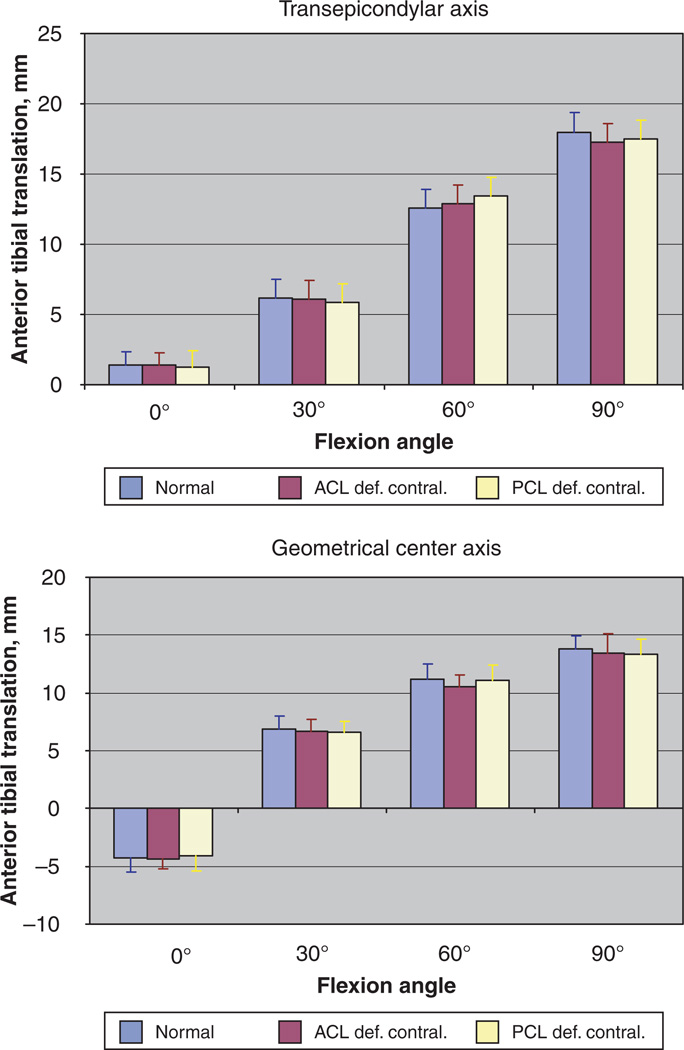
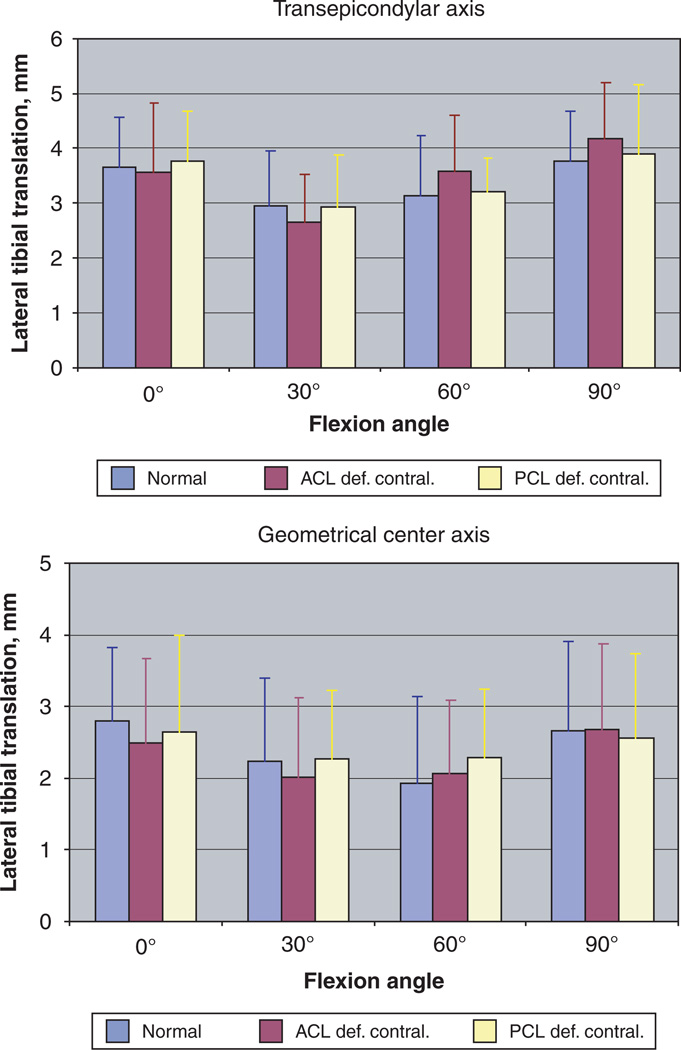
No significant differences were found across the groups in all rotations and translations, using either coordinate system (P > .95). In all study groups, the tibia consistently translated anteriorly from 0° to 90° of flexion (Figure 2). At 0°, the origin of the tibial coordinate system was 1.4 ± 1.0 mm anterior from the center of the transepicondylar axis in the normal knees, 1.4 ± 0.9 mm anterior in the uninjured contralateral knees of the ACL-deficient group, and 1.3 ± 1.1 mm anterior in the uninjured contralateral knees of the PCL-deficient group. When measured with the geometrical center axis of the femur, the tibia was 4.3 ± 1.2 mm posterior from the center of the femoral axis in the normal knees, 4.3 ± 0.9 mm posterior in the uninjured contralateral knees of the ACL-deficient group, and 4.1 ± 1.3 mm posterior in the uninjured contralateral knees of the PCL-deficient group at 0°. With flexion the tibia translated anteriorly and at 90° of flexion, the tibia was 18.0 ± 1.3 mm anterior from the center of the transepicondylar axis in the normal knees, 17.3 ± 1.3 mm anterior in the uninjured contralateral knees of the ACL-deficient group, and 17.5 ± 1.4 mm anterior in the uninjured contralateral knees of the PCL-deficient group. When measured with the geometrical center axis of the femur, the tibia was 13.8 ± 1.2 mm posterior from the center of the femoral axis in the normal knees, 13.4 ± 1.6 mm posterior in the uninjured contralateral knees of the ACL-deficient group, and 13.3 ± 1.3 mm posterior in the uninjured contralateral knees of the PCL-deficient group. From 0° to 90° of flexion, the center of the tibial coordinate system was lateral to the origin of the femoral coordinate system, and the excursions in the mediolateral direction were, on average, less than 2 mm (Figure 3).
Figure 2.
Anteroposterior translation of the tibia with respect to the femur in subjects with bilateral healthy knees (normal) and patients with contralateral ACL (ACL def. contral.) and PCL (PCL def. contral.) deficiency. Kinematics were analyzed using the transepicondylar femoral axis-based (top) and geometric center axis-based (bottom) coordinate systems. Positive values denote an anterior position of the tibia relative to the femur, while negative values represent a posterior position of the tibia relative to the femur. No significant differences between the groups were detected at all flexion angles (P > .95).
Figure 3.
Medial and lateral translation of the tibia with respect to the femur in subjects with bilateral healthy knees (normal) and patients with contralateral ACL (ACL def. contral.) and PCL (PCL def. contral.) deficiency. Kinematics were analyzed using the transepicondylar femoral axis-based (top) and geometric center axis-based (bottom) coordinate systems. Positive values denote a lateral position of the tibia relative the femur, while negative values represent a medial position of the tibia relative to the femur. No significant differences between the groups were detected at all flexion angles (P > .95).
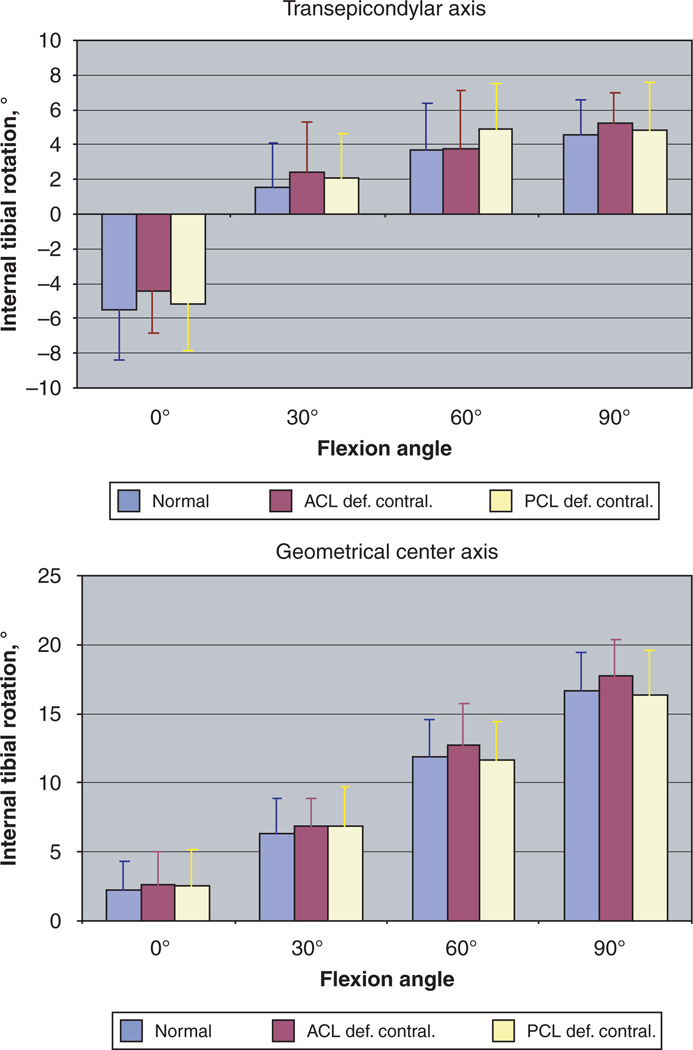
Rotations in the transverse plane were also not significantly different between the groups (P > .94). In all 3 groups and using either coordinate system, the tibia rotated internally relative to the femur with increasing flexion angle (Figure 4). At 0° the tibia was rotated 5.5° ± 2.9° externally relative to the femur in the normal group, 4.4° ± 2.4° externally in the uninjured contralateral knees of the ACL-deficient group, and 5.1° ± 2.7° externally in the uninjured contralateral knees of the PCL-deficient group, when measured with the transepicondylar axis–based coordinate system. With the geometrical center axis–based coordinates, the tibia in the normal group was rotated internally by 2.2° ± 2.1°. In the uninjured contralateral knees of the ACL- and PCL-deficient groups, the tibia was also rotated internally 2.6° ± 2.4° and 2.5° ± 2.6°, respectively. The tibia rotated further internally with increasing flexion and at 90° of flexion reached 4.6° ± 2.0°, 5.2° ± 1.8°, and 4.8° ± 2.8° of internal rotation in the normal and the uninjured contralateral knees of the ACL- and PCL-deficient groups, respectively, when measured with transepicondylar axis–based coordinates. Measurement with geometrical center axis–based coordinates detected the tibia to be 16.6° ± 2.8°, 17.7° ± 2.7°, and 16.3° ± 3.2° internally rotated in the normal and the uninjured contralateral knees of the ACL-and PCL-deficient groups, respectively.
Figure 4.
Internal-external rotation of the tibia relative to the femur in subjects with bilateral healthy knees (normal) and patients with contralateral ACL (ACL def. contral.) and PCL (PCL def. contral.) deficiency. Kinematics were analyzed using the transepicondylar femoral axis-based (top) and geometric center axis-based (bottom) coordinate systems. Positive values denote an internal tibial rotation, while negative values represent an external tibial rotation. No significant differences between the groups were detected at all flexion angles (P > .95).
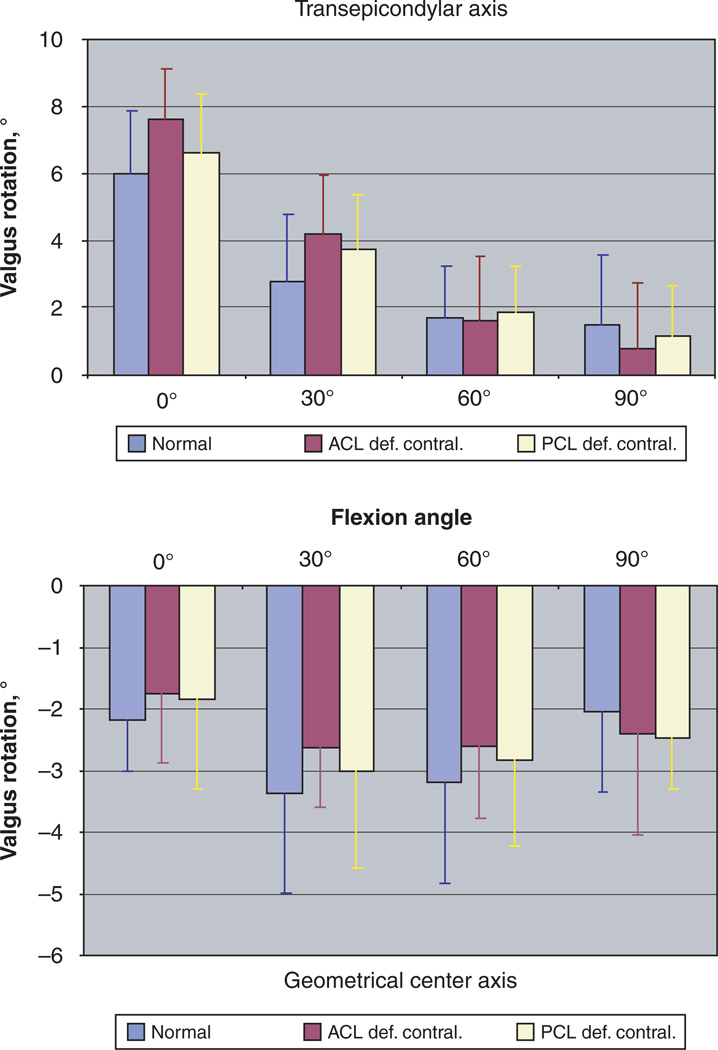
No significant differences were detected between the groups in varus-valgus rotation (P > .9). On average, knees in the 3 groups had a valgus alignment from 0° to 90° of flexion when measured using the transepicondylar axis (Figure 5). Varus alignment was measured throughout the range of flexion in all groups when the geometric center axis of the femur was used. The average excursions in the varus-valgus rotation were less than 2° from 0° to 90° of flexion.
Figure 5.
Varus-valgus alignment of the tibia relative to the femur in subjects with bilateral healthy knees (normal) and patients with contralateral ACL (ACL def. contral.) and PCL (PCL def. contral.) deficiency. Kinematics were analyzed using the transepicondylar femoral axis-based (top) and geometric center axis-based (bottom) coordinate systems. Positive values denote a valgus orientation of the tibia, while negative values represent a varus tibial orientation. No significant differences between the groups were detected at all flexion angles (P > .95).
DISCUSSION
Most of the in vivo kinematic studies on ACL and PCL deficiency use the uninjured contralateral side as a normal control.3,11,16–18.Altered knee kinematics were found in both the ACL- and the PCL-deficient knees in vivo.3,11 However, the reliability of using contralateral knees as normal kinematic control has not been determined. In this study, we compared the in vivo kinematics of the uninjured contralateral knees of patients with unilateral ACL or PCL deficiency with the kinematics of the knee joint of age-matched subjects without joint injury. Two different coordinate systems based on 2 femoral flexion axes (Figure 1) were used to analyze the kinematics.5,14,15,22 The data indicated no statistically significant differences between the groups in anterior-posterior and medial-lateral translation as well as in internal-external and varus-valgus rotations at 0°, 30°, 60°, and 90° of flexion.
These findings compare favorably with other reports of tibiofemoral kinematics of the contralateral uninjured knees in ACL-deficient patients. Shefelbine et al18 studied tibiofemoral kinematics in vivo in 8 ACL-deficient patients and 10 normal subjects using MRI and a load-bearing apparatus that applied 125 N axial loads to the foot at full extension and at 42.7° ± 8.3° of flexion of the knee. No significant differences in anteroposterior and mediolateral alignment of the tibia and femur were found between extension and flexion for uninjured knees of the ACL-deficient and normal groups. Recently, Scarvell et al17 studied sagittal plane tibiofemoral contact kinematics in 20 patients before and after ACL reconstruction and 12 healthy knees using an open MRI. Distances of tibiofemoral contact from the posterior tibial cortex at different flexion angles were compared, and no differences in tibiofemoral contact patterns were found between the uninjured contralateral knees of patients with acute ACL deficiency and healthy control subjects.
It has been hypothesized, based on measurements of anteroposterior laxity, that patients with cruciate ligament deficiency might have a preexisting increased laxity predisposing them to cruciate ligament injury.2,6,19 Using an instrumented knee laxity tester, Edixhoven et al6 measured anteroposterior laxity (Lachman test) of the knee joint in patients with acute and chronic ACL insufficiency. Measurements were taken on the injured ipsilateral and the uninjured contralateral knees as well as in a reference group of 34 subjects with bilateral healthy knees. The authors found a significantly increased anteroposterior laxity in uninjured contralateral knees in 8 patients with acute ACL injuries and 29 patients with chronic ACL injuries when compared with the normal reference group. Using a similar method, Shino et al19 reported measurements of anteroposterior stability of the knee with forces of up to 250 N applied at 20° of flexion. They measured anterior laxity at 200 N loads and anterior stiffness (force to produce 1 mm of displacement) at 50 N loads. Both parameters were increased on the uninjured side of 22 patients with contralateral ACL-deficient knees when compared with the normal reference group with both healthy knees. Daniel et al2 performed instrumented measurements of anteroposterior knee laxity in 338 normal subjects and 89 patients with unilateral ACL disruption. The authors used a KT-2000 arthrometer to apply anterior and posterior displacement loads up to 89 N. In their study, uninjured knees of patients with contralateral ACL disruption had a significantly greater anterior displacement compared with normal subjects.
Other studies, on the contrary, did not find increased laxity in the uninjured contralateral knees of ACL-deficient patients. In a more recent study, Daniel et al1 measured anteroposterior laxity in 138 patients with acute ACL deficiency and 120 normal subjects at 30° ± 5° of flexion using a KT-1000 arthrometer. No significant difference in anterior and posterior displacement between the uninjured knees of patients with ACL deficiency and the normal group was found when a 9.071-kg (20–lb) displacement force was applied. Markolf et al13 used an arthrometric apparatus to measure anteroposterior knee stability in 35 patients with unilateral ACL deficiency and 49 normal subjects applying anterior and posterior displacement loads of up to 200 N (45 lb or 20.411 kg) at 0°, 20°, and 90° of knee flexion. They, too, found no differences in the average magnitude of anteroposterior displacement between the uninjured contralateral knees of the ACL-deficient group and normal subjects.
In this study we found no significant differences in kinematics between the uninjured contralateral knees of ACL-or PCL-deficient patients and subjects with bilateral healthy knees. As the contralateral joint kinematics of the injured patients were not affected by the ligament injury in the short term, physicians and researchers might use the contralateral knee as a reliable normal kinematic control when evaluating 6 degrees of freedom kinematics of the knee after ACL or PCL injury. On the basis of the data of this study, we cannot conclude that preexisting abnormal kinematics were present in the selected groups of cruciate-deficient patients. We also noted that measurements with the transepicondylar axis yielded higher values of posterior translation than measurements done with the geometrical center axis. On the other hand, internal-external rotation of the tibia was greater when measured with the geometrical center axis. These trends compare favorably with other reports in the literature that also found greater tibial rotation with geometrical center axis measurements and higher values of posterior tibial translation with the transepicondylar axis measurements.5,7,14
There are possible limitations of this study that should be noted. Knee kinematics were measured during a quasistatic lunge. Only 4 flexion angles were studied, and a goniometer was used to control the flexion angle. The significance test did not have enough statistical power to detect small rotational changes in internal-external rotation of the tibia (2°). In order to achieve 80% power, 180 subjects would have to be enrolled. On the other hand, a post hoc power analysis to determine the probability of type II error using 1-way ANOVA as a significance test indicated that the significance test had 82% power to detect 2 mm differences between group means in translation for measurements with both flexion axes and 80% power to detect 2.5° differences between group means in varus-valgus rotation using the geometric center axis. When the transepicondylar axis was used to measure varus-valgus rotation, the power was 65% due to higher inter-subject variability (σ ≤ 2.09°). In the future, the effects of cruciate ligament deficiency on the kinematics of the uninjured contralateral knee should also be investigated under dynamic conditions (eg, gait, stair climbing, stair ascent, and descent). Furthermore, the average time from injury was 2.5 months in the ACL-deficient group and 4 months in the PCL-deficient group. It is not known how unilateral deficiency of the ACL or PCL affects the kinematics of the contralateral knee in the long term. Patients with a long history of ACL deficiency, even reconstructed, might have measurable changes in contact kine-matics in the contralateral knees in the long term. Future studies will therefore investigate the kinematic changes that occur in the contralateral knee in the long term.
In summary, the data of this study demonstrate that there is no statistically significant difference between the in vivo kinematics of the uninjured contralateral knee joint of patients with acute unilateral ACL or PCL deficiency and subjects without knee injury. These findings suggest that the included patients with ACL or PCL deficiency did not have preexisting abnormality in the knee in 6 degrees of freedom kinematics during weightbearing flexion. Furthermore, as the contralateral joint kinematics of the injured patients were not affected by the ligament injury in the short term, physicians and researchers can use the contralateral knee as a reliable normal kinematic control. In the future, the effect of chronic cruciate ligament deficiency on the kinematics of the contralateral knee joint should be investigated.
ACKNOWLEDGMENT
The authors gratefully acknowledge the patients and subjects who participated in this study. The authors also acknowledge the financial support of the National Institute of Health (R01 AR052408, R21 AR051078) and the Department of Orthopaedic Surgery at Massachusetts General Hospital.
Footnotes
No potential conflict of interest declared.
REFERENCES
- 1.Daniel DM, Malcom LL, Losse G, Stone ML, Sachs R, Burks R. Instrumented measurement of anterior laxity of the knee. J Bone Joint Surg Am. 1985;67(5):720–726. [PubMed] [Google Scholar]
- 2.Daniel DM, Stone ML, Sachs R, Malcom L. Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am J Sports Med. 1985;13(6):401–407. doi: 10.1177/036354658501300607. [DOI] [PubMed] [Google Scholar]
- 3.Defrate LE, Papannagari R, Gill TJ, Moses JM, Pathare NP, Li G. The 6 degrees of freedom kinematics of the knee after anterior cruciate ligament deficiency: an in vivo imaging analysis. Am J Sports Med. 2006;34(8):1240–1246. doi: 10.1177/0363546506287299. [DOI] [PubMed] [Google Scholar]
- 4.DeFrate LE, Sun H, Gill TJ, Rubash HE, Li G. In vivo tibiofemoral contact analysis using 3D MRI-based knee models. J Biomech. 2004;37(10):1499–1504. doi: 10.1016/j.jbiomech.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 5.Eckhoff DG, Dwyer TF, Bach JM, Spitzer VM, Reinig KD. Three-dimensional morphology of the distal part of the femur viewed in virtual reality. J Bone Joint Surg Am. 2001;83(Suppl 2)(Pt 1):43–50. doi: 10.2106/00004623-200100021-00010. [DOI] [PubMed] [Google Scholar]
- 6.Edixhoven P, Huiskes R, de Graaf R. Anteroposterior drawer measurements in the knee using an instrumented test device. Clin Orthop Relat Res. 1989;247:232–242. [PubMed] [Google Scholar]
- 7.Freeman M, Pinskerova V. The movement of the knee studied by magnetic resonance imaging. Clin Orthop. 2003;410:35–43. doi: 10.1097/01.blo.0000063598.67412.0d. [DOI] [PubMed] [Google Scholar]
- 8.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of 3-dimensional motions: application to the knee. J Biomech Eng. 1983;105(2):136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 9.Jordan SS, DeFrate LE, Nha KW, Papannagari R, Gill TJ, Li G. The in vivo kinematics of the anteromedial and posterolateral bundles of the anterior cruciate ligament during weightbearing knee flexion. Am J Sports Med. 2007;35(4):547–554. doi: 10.1177/0363546506295941. [DOI] [PubMed] [Google Scholar]
- 10.Li G, Moses JM, Papannagari R, Pathare NP, DeFrate LE, Gill TJ. Anterior cruciate ligament deficiency alters the in vivo motion of the tibiofemoral cartilage contact points in both the anteroposterior and mediolateral directions. J Bone Joint Surg Am. 2006;88(8):1826–1834. doi: 10.2106/JBJS.E.00539. [DOI] [PubMed] [Google Scholar]
- 11.Li G, Papannagari R, Li M, Bingham J, Nha KW, Allred D, Gill T. Effect of posterior cruciate ligament deficiency on in vivo translation and rotation of the knee during weightbearing flexion. Am J Sports Med. 2008;36(3):474–479. doi: 10.1177/0363546507310075. [DOI] [PubMed] [Google Scholar]
- 12.Li G, Wuerz TH, DeFrate LE. Feasibility of using orthogonal fluoro-scopic images to measure in vivo joint kinematics. J Biomech Eng. 2004;126(2):314–318. doi: 10.1115/1.1691448. [DOI] [PubMed] [Google Scholar]
- 13.Markolf KL, Kochan A, Amstutz HC. Measurement of knee stiffness and laxity in patients with documented absence of the anterior cruciate ligament. J Bone Joint Surg Am. 1984;66(2):242–252. [PubMed] [Google Scholar]
- 14.Most E, Axe J, Rubash H, Li G. Sensitivity of the knee joint kinematics calculation to selection of flexion axes. J Biomech. 2004;37(11):1743–1748. doi: 10.1016/j.jbiomech.2004.01.025. [DOI] [PubMed] [Google Scholar]
- 15.Olcott CW, Scott RD. The Ranawat Award. Femoral component rotation during total knee arthroplasty. Clin Orthop Relat Res. 1999;367:39–42. [PubMed] [Google Scholar]
- 16.Papannagari R, Gill TJ, Defrate LE, Moses JM, Petruska AJ, Li G. In vivo kinematics of the knee after anterior cruciate ligament reconstruction: a clinical and functional evaluation. Am J Sports Med. 2006;34(12):2006–2012. doi: 10.1177/0363546506290403. [DOI] [PubMed] [Google Scholar]
- 17.Scarvell JM, Smith PN, Refshauge KM, Galloway HR, Woods KR. Does anterior cruciate ligament reconstruction restore normal knee kinematics? A prospective MRI analysis over 2 years. J Bone Joint Surg Br. 2006;88(3):324–330. doi: 10.1302/0301-620X.88B3.16787. [DOI] [PubMed] [Google Scholar]
- 18.Shefelbine SJ, Ma CB, Lee KY, et al. MRI analysis of in vivo meniscal and tibiofemoral kinematics in ACL-deficient and normal knees. J Orthop Res. 2006;24(6):1208–1217. doi: 10.1002/jor.20139. [DOI] [PubMed] [Google Scholar]
- 19.Shino K, Inoue M, Horibe S, Nakamura H, Ono K. Measurement of anterior instability of the knee. A new apparatus for clinical testing. J Bone Joint Surg Br. 1987;69(4):608–613. doi: 10.1302/0301-620X.69B4.3611167. [DOI] [PubMed] [Google Scholar]
- 20.Suntay WJ, Grood ES, Hefzy MS, Butler DL, Noyes FR. Error analysis of a system for measuring 3-dimensional joint motion. J Biomech Eng. 1983;105(2):127–135. doi: 10.1115/1.3138396. [DOI] [PubMed] [Google Scholar]
- 21.Van de Velde SK, DeFrate LE, Gill TJ, Moses JM, Papannagari R, Li G. The effect of anterior cruciate ligament deficiency on the in vivo elongation of the medial and lateral collateral ligaments. Am J Sports Med. 2007;35(2):294–300. doi: 10.1177/0363546506294079. [DOI] [PubMed] [Google Scholar]
- 22.Yoshino N, Takai S, Ohtsuki Y, Hirasawa Y. Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty. 2001;16(4):493–497. doi: 10.1054/arth.2001.23621. [DOI] [PubMed] [Google Scholar]