Abstract
AIM: To detect and manage residual common bile duct (CBD) stones using ultraslim endoscopic peroral cholangioscopy (POC) after a negative balloon-occluded cholangiography.
METHODS: From March 2011 to December 2011, a cohort of 22 patients with CBD stones who underwent both endoscopic retrograde cholangiography (ERC) and direct POC were prospectively enrolled in this study. Those patients who were younger than 20 years of age, pregnant, critically ill, or unable to provide informed consent for direct POC, as well as those with concomitant gallbladder stones or CBD with diameters less than 10 mm were excluded. Direct POC using an ultraslim endoscope with an overtube balloon-assisted technique was carried out immediately after a negative balloon-occluded cholangiography was obtained.
RESULTS: The ultraslim endoscope was able to be advanced to the hepatic hilum or the intrahepatic bile duct (IHD) in 8 patients (36.4%), to the extrahepatic bile duct where the hilum could be visualized in 10 patients (45.5%), and to the distal CBD where the hilum could not be visualized in 4 patients (18.2%). The procedure time of the diagnostic POC was 8.2 ± 2.9 min (range, 5-18 min). Residual CBD stones were found in 5 (22.7%) of the patients. There was one residual stone each in 3 of the patients, three in 1 patient, and more than five in 1 patient. The diameter of the residual stones ranged from 2-5 mm. In 2 of the patients, the residual stones were successfully extracted using either a retrieval balloon catheter (n = 1) or a basket catheter (n = 1) under direct endoscopic control. In the remaining 3 patients, the residual stones were removed using an irrigation and suction method under direct endoscopic visualization. There were no serious procedure-related complications, such as bleeding, pancreatitis, biliary tract infection, or perforation, in this study.
CONCLUSION: Direct POC using an ultraslim endoscope appears to be a useful tool for both detecting and treating residual CBD stones after conventional ERC.
Keywords: Balloon-occluded cholangiography, Common bile duct stones, Endoscopic retrograde cholangiography, Peroral cholangioscopy, Residual stones
Core tip: Balloon-occluded cholangiography is generally performed to confirm bile duct clearance after performing endoscopic retrograde cholangiography (ERC) for stone retrieval. However, balloon-occluded cholangiography may be an imperfect tool for this diagnostic purpose. In this case series, we demonstrated that 22.7% of patients still had residual stones detected on peroral cholangioscopy after a negative balloon-occluded cholangiography was obtained. All of the residual stones were retracted on the cholangioscopy. Our results reveal that peroral cholangioscopy appears to be a useful tool for both detecting and treating residual common bile duct stones after conventional ERC.
INTRODUCTION
Endoscopic sphincterotomy (ES) has become the cornerstone of therapeutic endoscopic retrograde cholangiography (ERC). It is most commonly performed to remove common bile duct (CBD) stones[1-3]. Endoscopic papillary balloon dilatation (EPBD) has been used as an alternative approach to ES[4,5]. After ES/EPBD for stone retrieval, balloon-occluded cholangiography is generally performed to confirm bile duct clearance. However, small stones may be left undetected by the balloon-occluded cholangiography[6-8]. These small stone fragments run the risk of acting as nidi for future stone formation, leading to the recurrence of CBD stones[9-11]. Therefore, it is crucial to achieve a level of stone clearance that is as complete as possible to prevent stone recurrence. Intraductal ultrasound (IDUS) has been applied to confirm the clearance of CBD stones after stone retrieval by ES[6,9,12]. Tsuchiya et al[9] reported that performing IDUS after stone extraction decreased the recurrence rate of CBD stones to 3.4% from the 13.2% recurrence rate of the control group. However, IDUS poses problems, such as probe fragility and a high cost. In addition, it is a highly operator-dependent technology. Poor images and the consequent oversight of residual stones are possible, especially in patients with extensive pneumobilia[9]. Ohashi et al[6] reported that IDUS examination failed to detect residual stones after bile duct clearance in 14.6% (6/41) of the patients.
Cholangioscopy offers a crucial advantage over IDUS in that it permits direct visualization of the bile duct and further management of any bile duct stones[13-15]. Direct peroral cholangioscopy (POC) may play a role in the detection of bile duct stones, but there is a lack of studies on this subject[16]. Although conventional POC using a mother-baby endoscopic system has been available for more than three decades, its role remains limited because of its many disadvantages[17,18]. Recently, direct POC using an ultraslim endoscope has been reported to be feasible and superior to the conventional mother-baby endoscopic system because it provides superior endoscopic images and a larger working channel[19-22]. Furthermore, it can be performed by a single endoscopist. The aim of this study is to evaluate the utility of ultraslim endoscopic POC in the diagnosis and management of residual CBD stones after performing bile duct clearance and confirming the procedure using balloon-occluded cholangiography.
MATERIALS AND METHODS
Patients
From March 2011 to December 2011, the patients who underwent ERC performed by the two endoscopists (Tsou YK and Lin CH) in Chang Gung Memorial Hospital who met the following criteria were prospectively enrolled in this study: CBD stones were diagnosed based on imaging studies, such as abdominal ultrasonography, computed tomography scans, and/or magnetic resonance cholangiopancreatography before the index ERC (n = 92); The exclusion criteria were as follows: (1) patients who were younger than 20 years of age, pregnant, or critically ill (n = 5); (2) patients with concomitant gallbladder stones (n = 42); (3) patients with CBD diameters of less than 10 mm (n = 9); and (4) patients who were unable to provide informed consent for POC (n = 14).
ERC
ERC was performed using a duodenoscope (JF or TJF 260-V, Olympus, Tokyo, Japan) under conscious sedation with the patients in a prone position. ES was performed using a standard pull-type sphincterotome (Ultratome; Boston Scientific Co., Spencer, IN, United States). EPBD was carried out using a controlled radial expansion (CRE) balloon. During the index ERC, EPBD was carried out in 13 patients (including the 8 patients who had previously undergone ES or EPBD); ES then EPBD were performed in 6 patients (including 1 patient who had received a previous ES); and extended ES was performed in 1 patient to facilitate the stone extraction and/or the performance of the POC. Two other patients did not undergo ES or EPBD during the index ERC because the papillary orifice created by EPBD during the previous procedure(s) was large enough to permit stone extraction and performing the POC.
A contrast medium at a 1:1 dilution was used for the cholangiography. The instruments used to extract the CBD stones included a retrieval balloon catheter alone (n = 16) and a combination of a balloon and a basket catheter (n = 6). Two patients underwent lithotripsy because the CBD stones were difficult to extract using a balloon catheter. After the stone extraction, balloon-occluded cholangiography was performed to confirm the complete clearance of the CBD stones. If any residual stones were observed during the balloon-occluded cholangiography, additional endoscopic treatments were performed until the balloon-occluded cholangiography was negative (Figure 1).
Figure 1.
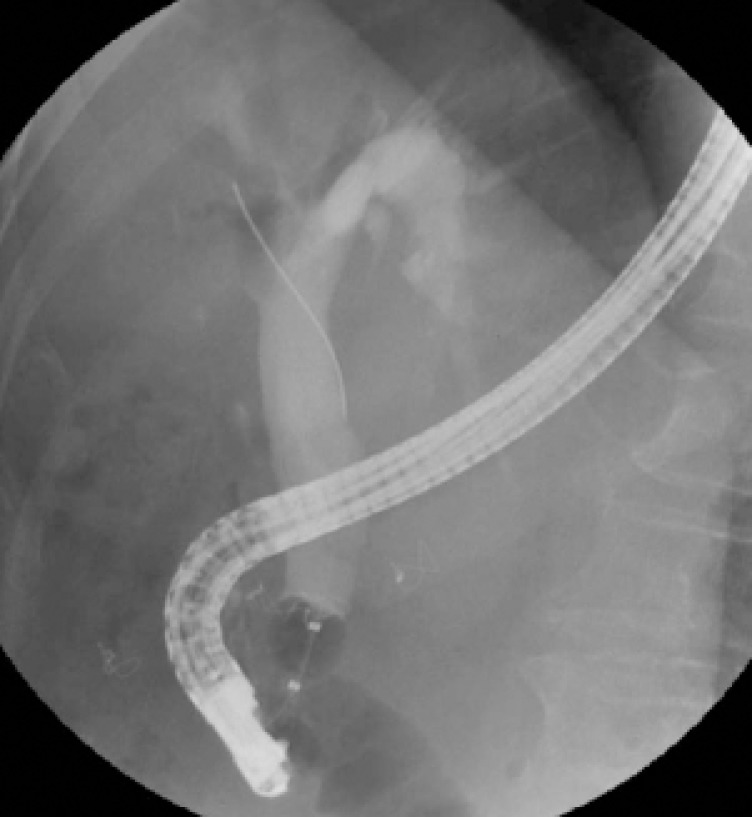
Balloon-occluded cholangiography failed to reveal any filling defects of stones in the biliary tree after endoscopic retrograde cholangiography with bile duct clearance.
Direct peroral cholangioscopy
An ultraslim endoscope (GIF-N260, Olympus) and an overtube (ST-SB1, Olympus) were used for the POC procedures. All of the POC procedures were performed by two endoscopists (Tsou YK and Lin CH) who are experienced in this endoscopy and were carried out immediately after a negative balloon-occluded cholangiography was obtained during a single endoscopic session. The details of the POC procedures are described in our previous study[20]. Briefly, the overtube containing the endoscope is advanced into the distal gastric antrum (or into the afferent loop for patients with a post-operative stomach); the overtube balloon is then inflated to anchor the overtube. The endoscope is further advanced into the orifice of the major papilla either directly or after performing a J-turn of the endoscopic tip. Then, the endoscope is advanced into the bile duct as far as possible. The POC time is defined as the interval between the ultraslim endoscope entering the mouth of the patient and reaching the farthest site of the biliary tree.
In the text and tables, the continuous variables are expressed in the form mean ± SD. The study protocol was approved by the ethical committee at Chang Gung Memorial Hospital (IRB No: 99-2585C).
RESULTS
A cohort of 22 patients with CBD stones undergoing both ERC and direct POC were prospectively enrolled in this study (Table 1). The patient age was 73.4 ± 11.8 years (range, 40-89 years), and 15 (68%) of the patients were men. The patients were categorized into the following gallbladder status groups: intact without stones (n = 3), post laparoscopic cholecystectomy (n = 2), and post open cholecystectomy (n = 17). Eight patients (36.4%) had juxtapapillary diverticulum. Three patients (13.6%) had a medical history of subtotal gastrectomy with Billroth-II anastomosis (n = 2) or total gastrectomy with Roux-en-Y anastomosis (n = 1).
Table 1.
Patient characteristics n (%)
| Characteristics | n = 22 |
| Age (yr) | 73.4 ± 11.8 (range, 40-89) |
| Gender (male) | 15 (68) |
| Prior cholecystectomies1 | 19 (86.4) |
| Acalculous gallbladder | 3 (13.6) |
| Juxtapapillary diverticulum | 8 (36.4) |
| Subtotal gastrectomy with Billroth-II anastomosis | 2 (9.1) |
| Total gastrectomy with Roux-en-Y anastomosis | 1 (4.5) |
| Patients with recurrent CBD stones | 12 (54.5) |
Including 17 cases of open cholecystectomy and 2 cases of laparoscopic cholecystectomy. CBD: Common bile duct.
The ERC results are listed in Table 2. The maximum diameter of the CBD was 17.9 ± 5.1 mm (range, 10-30 mm). Twelve of the patients (54.5%) had recurrent CBD stones. The number of CBD stones was one each in 10 patients, two in 2 patients, three in 4 patients, and more than three in 6 patients. The maximum stone diameter was 13.4 ± 5.6 mm (range, 5-25.4 mm). Sixteen patients had brown stones, 2 patients had black stones, and 4 patients had mixed brown and black stones. During the index ERC, the CBD stones were removed intact in 11 patients (50%).
Table 2.
Results of endoscopic retrograde cholangiography n (%)
| Characteristics | n = 22 |
| CBD stones | |
| No. of stones (one/two/three/more than three) | 10/2/4/6 |
| Mean maximum diameter (mm) | 13.4 ± 5.6 (range, 5-25.4) |
| Mean maximum diameter of CBD (mm) | 17.9 (range, 10-30) |
| ES and/or EPBD | |
| ES | 1 (4.5) |
| EPBD | 13 (59.1) |
| ES + EPBD | 6 (27.3) |
| None1 | 2 (9.1) |
| Mean maximum inflated diameter during EPBD2 (mm) | 13.6 (range, 12-15) |
| Stone extraction methods | |
| Balloon and/or basket | 20 (90.9) |
| Mechanical lithotripter | 2 (9.1) |
| Intact stone extraction | 11 (50) |
Endoscopic papillary balloon dilatation (EPBD) was performed during the previous endoscopic session, and the papillary orifice was adequate;
A total of 15 cases underwent EPBD. CBD: Common bile duct; ES: Endoscopic sphincterotomy.
The results of POC are given in Table 3. The POC time was 8.2 ± 2.9 min (range, 5-18 min). The ultraslim endoscope was able to be advanced to the hepatic hilum or the intrahepatic bile duct (IHD) in 8 patients (36.4%) (Figure 2); to the extrahepatic bile duct where the hilum could be visualized in 10 patients (45.5%); and to the distal CBD where the hilum could not be visualized in 4 patients (18.2%). During POC, residual CBD stones were found in 5 patients (22.7%) (Figure 3). One residual stone was found in each of 3 patients, three in 1 patient, and multiple (more than five) in 1 patient. The diameter of the residual stones ranged from 2-5 mm. In 2 patients, the residual stones were extracted successfully using a retrieval balloon catheter (n = 1) or a basket catheter (n = 1) under direct endoscopic visualization (Figure 4). In the remaining 3 patients, the residual stones were removed using direct endoscopic suction after normal saline irrigation. For the patient with multiple residual stones, a balloon catheter was inserted proximally to the stones through the endoscope and the endoscopic tip was placed distally to the stones. Using synchronic normal saline irrigation via the balloon catheter and endoscopic suction, the stones and the endoscope were slowly pulled down to the distal bile duct and finally to the duodenum. No serious procedure-related complications, such as bleeding, pancreatitis, biliary tract infection, or perforation, were observed in this study. The ultraslim endoscope used as the cholangioscope did not sustain any obvious damage during the study period.
Table 3.
Results of peroral cholangioscopy n (%)
| Characteristics | n = 22 |
| Mean procedure time (min) | 8.2 (range, 5-18) |
| The endoscope reached | |
| Hilum or IHD | 8 (36.4) |
| CBD and the hilum was seen | 10 (45.5) |
| Distal CBD and the hilum was not seen | 4 (18.2) |
| Residual stones on the POC | |
| No. of patients | 5 (22.7) |
| No. of residual stones (one/three/multiple) | 3/1/1 |
| Maximum diameter of stones (range, mm) | 2-5 |
IHD: Intrahepatic duct; CBD: Common bile duct; POC: Peroral cholangioscopy
Figure 2.

Ultraslim endoscope was advanced to the common bile duct (dotted arrow) and up to the left intrahepatic duct (arrow) using an overtube balloon (arrow head)-assisted technique.
Figure 3.

Residual stones in the bile duct visualized using direct peroral cholangioscopy.
Figure 4.
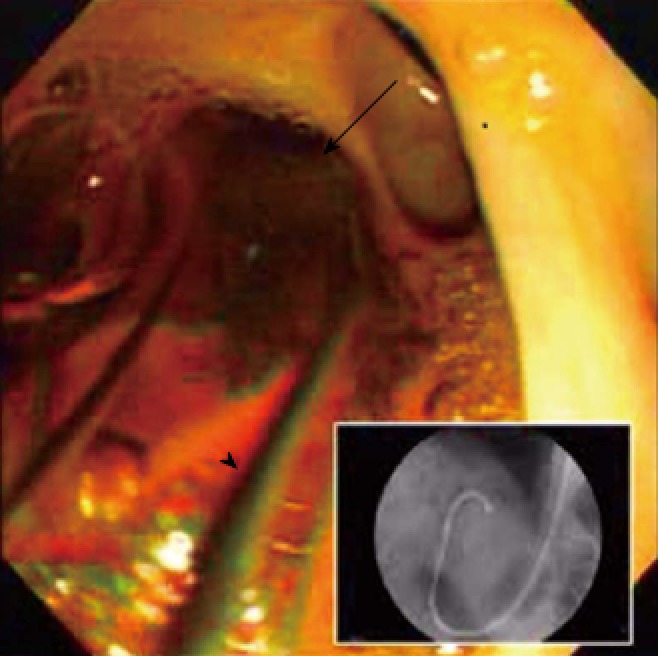
A basket catheter (arrow head) was used to retrieve the residual bile duct stones (arrow) under direct endoscopic control.
The clinical data on the patients with (n = 5) and without (n = 17) residual stones on POC are listed in Table 4. Because the patient sample size was small, we did not perform any statistical analysis. However, recurrent CBD stones and prior choledocholithotomy were more frequently observed in the patients with residual stones than in the patients without (80% vs 41.2% and 60% vs 35.3%, respectively). Intact stone extraction during the index ERC was less common in patients with residual stones than in patients without (20% vs 58.9%, respectively). These patients were followed up for 17.5 ± 4.9 mo (range, 12-24 mo) after the POC. Four patients (18.2%) had recurrent CBD stones documented on ERC during a follow-up; two of these four had residual stones on POC.
Table 4.
Clinical features between the patients with and without residual bile duct stones n (%)
| With residual stones (n = 5) | Without residual stones (n = 17) | |
| Age (yr) | 69 ± 18.6 | 74.7 ± 9.5 |
| Sex (male) | 4 (80) | 11 (64.7) |
| Recurrent CBD stones | 4 (80) | 7 (41.2) |
| Prior choledocholithotomy | 3 (60) | 6 (35.3) |
| Mean maximum CBD diameter (mm) | 19 ± 7.6 | 17.6 ± 4.5 |
| Stones number (single) | 2 (40) | 8 (47) |
| Mean maximum stone diameter (mm) | 14.1 ± 7.2 | 13.2 ± 5.2 |
| Lithotripsy | 0 (0) | 2 (11.8) |
| Intact stone extraction | 1 (20) | 10 (58.9) |
| Diameter of EPBD1 (mm) | 13.5 ± 1.7 (n = 4) | 13.5 ± 1.4 |
Mean maximum inflated diameter of the balloon during endoscopic papillary balloon dilatation (EPBD). CBD: Common bile duct.
DISCUSSION
Balloon-occluded cholangiography is an imperfect tool to confirm complete bile duct clearance after ES/EPBD for stone retrieval. In this study, we observed that balloon-occluded cholangiography failed to detect residual CBD stones in 22.7% of the patients. Tsuchiya et al[9] used IDUS and reported that balloon-occluded cholangiography did not detect any residual CBD stones in 23.7% (14/59) of the patients[9]. Itoi et al[7] performed POC using a mother-baby system 0-20 d (median, 6.2 d) after ERC with CBD stone retrieval. In all of these patients, the bile duct was confirmed to be free of stones using balloon-occluded cholangiography. It was later found that 24% (26/108) of these patients had residual CBD stones on the POC, although in some of the patients, the CBD stones might have migrated from the gallbladder after the stone retrieval. Our results are consistent with those of other studies, revealing that balloon-occluded cholangiography fails to detect residual CBD stones in nearly one quarter of patients.
The residual CBD stones not detected by balloon-occluded cholangiography in the previous reports using IDUS were usually small[23-25]. The present study confirmed (using POC) that the undetected residual CBD stones are small and no more than 5 mm in diameter. It is unclear whether these small residual stones have clinical significance[26]. Because the orifice of the major papilla after ES/EPBD is large enough, spontaneous passage of the stones is possible. However, Itoi et al[7] performed POC an average of 6 d after stone retrieval by ERC and found that 24% of the patients still had residual stones. Their result suggests that residual stones might not be excreted for a long time and may eventually cause stone recurrence. Several studies that have aimed to analyze the risk factors for recurrent CBD stones suggest that residual stones are a possible cause of recurrent CBD stones[9,10,27]. Therefore, it may be important to detect and remove residual CBD stones after ES/EPBD for stone retrieval. Further studies are needed to clarify whether the residual stones have clinical significance and whether the removal of residual stones minimizes the risk of stone recurrence.
The ultraslim endoscopic POC has several advantages over the mother-baby endoscopic system[20,21]. One is that it enables the extraction of residual CBD stones under direct endoscopic visualization, as demonstrated in the present study. In contrast, the residual stones in the 26 patients reported by Itoi et al[7] were not directly removable using the mother-baby system. A 5-Fr balloon or basket catheter can pass through the 2-mm working channel of the ultraslim endoscope to grasp the residual stones. However, to remove the grasped stones, the ultraslim endoscope with the balloon/basket must be withdrawn to the duodenum. This maneuver can be complicated when there are multiple residual stones. In this case, the irrigation and suction method described above offers an effective way to remove the stones, especially for small soft stones. Placing the tip of a balloon catheter proximally to the stones can avoid flushing them upstream.
There are two major limitations to this study. One is that the hilum or IHD could be reached by the POC in only 36.4% of the patients. For the purpose of this study, seeing the hilum may be enough to verify bile duct clearance, and in 71.8% of the patients, the hilum could be seen. However, in 18.2% of the patients, the hilum could not be seen by the POC. One possible reason for this limitation was that many (41%) of our patients had undergone choledocholithotomy with T-tube drainage, resulting in a tortuous CBD. Direct POC using an intraductal anchoring balloon method may be able to improve the rate of seeing the hilum, but the anchoring device was withdrawn from the market due to an increased risk of air embolism[28]. Therefore, the rate of residual CBD stones may be higher if some of the residual stones were not visualized during the POC in our patients.
The other limitation is that we enrolled only patients without GB stones or without GB to avoid the risk of “migrated GB stones” being confused with the residual stones. As a result, 19 of the 22 patients (86.4%) had a previous cholecystectomy. Therefore, the study results may be only applied to this subgroup of patients. In this study, we found that recurrent CBD stones as an indication for index ERC, prior choledocholithotomy, and fragmented stones during stones retrieval on the index ERC were more frequently observed in patients with residual stones. It might be worthwhile to perform POC for patients with these characteristics.
In conclusion, conventional ERC with balloon-occluded cholangiography is not a reliable method for confirming the complete extraction of CBD stones. Direct POC using an ultraslim endoscope appears to be a useful tool to confirm the clearance of CBD stones and to extract the residual CBD stones in selected patients.
COMMENTS
Background
Balloon-occluded cholangiography is generally performed to confirm bile duct clearance after bile duct stone retrieval. However, small stones may remain undetected on the balloon-occluded cholangiography.
Research frontiers
Cholangiography is a direct image which is at least theoretically better than the indirect image of balloon-occluded cholangiography. Therefore, the authors perform direct peroral cholangiography (POC) to examine if there are residual bile duct stones after obtaining a negative balloon-occluded cholangiography. The method of POC is using an ultraslim endoscope with overtube balloon-assisted technique.
Innovations and breakthroughs
The authors demonstrate that 22.7% of the patients still have residual stones detected on the direct POC after a negative balloon-occluded cholangiography is obtained. All of the residual stones are small (range 2-5 mm) and extracted successfully during the POC.
Applications
The results indicate that direct POC using an ultraslim endoscope appears to be a useful tool for both detecting and treating residual bile duct stones after conventional endoscopic retrograde cholangiography.
Terminology
Direct POC is to insert an endoscope perorally into the bile ducts. Direct POC using a mother-baby endoscope system is not widely used because of its many disadvantages. Recently, direct POC using an ultraslim endoscope has been reported to be feasible and superior to the conventional mother-baby endoscopic system because it provides superior endoscopic images and a larger working channel. Furthermore, it can be performed by a single endoscopist.
Peer review
In this study, the value of peroral cholangioscopy for detecting remaining bile duct stones after balloon-occluded cholangiography was evaluated in 22 patients. Despite a negative balloon-occluded cholangiography, additional bile duct stones were detected in 5 patients (23%). The stone diameter was generally small (2-5 mm). Unfortunately the authors did not perform intraductal ultrasound in their 22 patients simultaneously, that would have allowed comparison of the two methods.
Footnotes
Supported by Chang Gung Memorial Hospital, No. CMRPG300011
P- Reviewers Endo I, van Erpecum KJ S- Editor Zhai HH L- Editor A E- Editor Ma S
References
- 1.Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909–918. doi: 10.1056/NEJM199609263351301. [DOI] [PubMed] [Google Scholar]
- 2.Maple JT, Ikenberry SO, Anderson MA, Appalaneni V, Decker GA, Early D, Evans JA, Fanelli RD, Fisher D, Fisher L, et al. The role of endoscopy in the management of choledocholithiasis. Gastrointest Endosc. 2011;74:731–744. doi: 10.1016/j.gie.2011.04.012. [DOI] [PubMed] [Google Scholar]
- 3.Williams EJ, Green J, Beckingham I, Parks R, Martin D, Lombard M. Guidelines on the management of common bile duct stones (CBDS) Gut. 2008;57:1004–1021. doi: 10.1136/gut.2007.121657. [DOI] [PubMed] [Google Scholar]
- 4.Jeong S, Ki SH, Lee DH, Lee JI, Lee JW, Kwon KS, Kim HG, Shin YW, Kim YS. Endoscopic large-balloon sphincteroplasty without preceding sphincterotomy for the removal of large bile duct stones: a preliminary study. Gastrointest Endosc. 2009;70:915–922. doi: 10.1016/j.gie.2009.04.042. [DOI] [PubMed] [Google Scholar]
- 5.Oh MJ, Kim TN. Prospective comparative study of endoscopic papillary large balloon dilation and endoscopic sphincterotomy for removal of large bile duct stones in patients above 45 years of age. Scand J Gastroenterol. 2012;47:1071–1077. doi: 10.3109/00365521.2012.690046. [DOI] [PubMed] [Google Scholar]
- 6.Ohashi A, Ueno N, Tamada K, Tomiyama T, Wada S, Miyata T, Nishizono T, Tano S, Aizawa T, Ido K, et al. Assessment of residual bile duct stones with use of intraductal US during endoscopic balloon sphincteroplasty: comparison with balloon cholangiography. Gastrointest Endosc. 1999;49:328–333. doi: 10.1016/s0016-5107(99)70009-x. [DOI] [PubMed] [Google Scholar]
- 7.Itoi T, Sofuni A, Itokawa F, Shinohara Y, Moriyasu F, Tsuchida A. Evaluation of residual bile duct stones by peroral cholangioscopy in comparison with balloon-cholangiography. Dig Endosc. 2010;22 Suppl 1:S85–S89. doi: 10.1111/j.1443-1661.2010.00954.x. [DOI] [PubMed] [Google Scholar]
- 8.Das A, Isenberg G, Wong RC, Sivak MV, Chak A. Wire-guided intraductal US: an adjunct to ERCP in the management of bile duct stones. Gastrointest Endosc. 2001;54:31–36. doi: 10.1067/mge.2001.115006. [DOI] [PubMed] [Google Scholar]
- 9.Tsuchiya S, Tsuyuguchi T, Sakai Y, Sugiyama H, Miyagawa K, Fukuda Y, Ando T, Saisho H, Yokosuka O. Clinical utility of intraductal US to decrease early recurrence rate of common bile duct stones after endoscopic papillotomy. J Gastroenterol Hepatol. 2008;23:1590–1595. doi: 10.1111/j.1440-1746.2008.05458.x. [DOI] [PubMed] [Google Scholar]
- 10.Ando T, Tsuyuguchi T, Okugawa T, Saito M, Ishihara T, Yamaguchi T, Saisho H. Risk factors for recurrent bile duct stones after endoscopic papillotomy. Gut. 2003;52:116–121. doi: 10.1136/gut.52.1.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheon YK, Lehman GA. Identification of risk factors for stone recurrence after endoscopic treatment of bile duct stones. Eur J Gastroenterol Hepatol. 2006;18:461–464. doi: 10.1097/00042737-200605000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Ang TL, Teo EK, Fock KM, Lyn Tan JY. Are there roles for intraductal US and saline solution irrigation in ensuring complete clearance of common bile duct stones. Gastrointest Endosc. 2009;69:1276–1281. doi: 10.1016/j.gie.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 13.Parsi MA. Peroral cholangioscopy in the new millennium. World J Gastroenterol. 2011;17:1–6. doi: 10.3748/wjg.v17.i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trikudanathan G, Navaneethan U, Parsi MA. Endoscopic management of difficult common bile duct stones. World J Gastroenterol. 2013;19:165–173. doi: 10.3748/wjg.v19.i2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Han JH, Park do H, Moon SH, Lee SS, Seo DW, Lee SK, Kim MH. Peroral direct cholangioscopic lithotripsy with a standard upper endoscope for difficult bile duct stones (with videos) Gastrointest Endosc. 2009;70:183–185. doi: 10.1016/j.gie.2008.09.042. [DOI] [PubMed] [Google Scholar]
- 16.Maple JT, Ben-Menachem T, Anderson MA, Appalaneni V, Banerjee S, Cash BD, Fisher L, Harrison ME, Fanelli RD, Fukami N, et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 2010;71:1–9. doi: 10.1016/j.gie.2009.09.041. [DOI] [PubMed] [Google Scholar]
- 17.Kodama T, Tatsumi Y, Sato H, Imamura Y, Koshitani T, Abe M, Kato K, Uehira H, Horii Y, Yamane Y, et al. Initial experience with a new peroral electronic pancreatoscope with an accessory channel. Gastrointest Endosc. 2004;59:895–900. doi: 10.1016/s0016-5107(04)01272-6. [DOI] [PubMed] [Google Scholar]
- 18.Moon JH, Terheggen G, Choi HJ, Neuhaus H. Peroral cholangioscopy: diagnostic and therapeutic applications. Gastroenterology. 2013;144:276–282. doi: 10.1053/j.gastro.2012.10.045. [DOI] [PubMed] [Google Scholar]
- 19.Larghi A, Waxman I. Endoscopic direct cholangioscopy by using an ultra-slim upper endoscope: a feasibility study. Gastrointest Endosc. 2006;63:853–857. doi: 10.1016/j.gie.2005.07.050. [DOI] [PubMed] [Google Scholar]
- 20.Tsou YK, Lin CH, Tang JH, Liu NJ, Cheng CL. Direct peroral cholangioscopy using an ultraslim endoscope and overtube balloon-assisted technique: a case series. Endoscopy. 2010;42:681–684. doi: 10.1055/s-0030-1255616. [DOI] [PubMed] [Google Scholar]
- 21.Moon JH, Ko BM, Choi HJ, Hong SJ, Cheon YK, Cho YD, Lee JS, Lee MS, Shim CS. Intraductal balloon-guided direct peroral cholangioscopy with an ultraslim upper endoscope (with videos) Gastrointest Endosc. 2009;70:297–302. doi: 10.1016/j.gie.2008.11.019. [DOI] [PubMed] [Google Scholar]
- 22.Choi HJ, Moon JH, Ko BM, Hong SJ, Koo HC, Cheon YK, Cho YD, Lee JS, Lee MS, Shim CS. Overtube-balloon-assisted direct peroral cholangioscopy by using an ultra-slim upper endoscope (with videos) Gastrointest Endosc. 2009;69:935–940. doi: 10.1016/j.gie.2008.08.043. [DOI] [PubMed] [Google Scholar]
- 23.Prat F, Amouyal G, Amouyal P, Pelletier G, Fritsch J, Choury AD, Buffet C, Etienne JP. Prospective controlled study of endoscopic ultrasonography and endoscopic retrograde cholangiography in patients with suspected common-bileduct lithiasis. Lancet. 1996;347:75–79. doi: 10.1016/s0140-6736(96)90208-1. [DOI] [PubMed] [Google Scholar]
- 24.Burtin P, Palazzo L, Canard JM, Person B, Oberti F, Boyer J. Diagnostic strategies for extrahepatic cholestasis of indefinite origin: endoscopic ultrasonography or retrograde cholangiography Results of a prospective study. Endoscopy. 1997;29:349–355. doi: 10.1055/s-2007-1004214. [DOI] [PubMed] [Google Scholar]
- 25.Palazzo L, Girollet PP, Salmeron M, Silvain C, Roseau G, Canard JM, Chaussade S, Couturier D, Paolaggi JA. Value of endoscopic ultrasonography in the diagnosis of common bile duct stones: comparison with surgical exploration and ERCP. Gastrointest Endosc. 1995;42:225–231. doi: 10.1016/s0016-5107(95)70096-x. [DOI] [PubMed] [Google Scholar]
- 26.Siddique I, Mohan K, Khajah A, Hasan F, Memon A, Kalaoui M, al-Shamali M, Patty I, al-Nakib B. Sphincterotomy in patients with gallstones, elevated LFTs and a normal CBD on ERCP. Hepatogastroenterology. 2003;50:1242–1245. [PubMed] [Google Scholar]
- 27.Saito M, Tsuyuguchi T, Yamaguchi T, Ishihara T, Saisho H. Long-term outcome of endoscopic papillotomy for choledocholithiasis with cholecystolithiasis. Gastrointest Endosc. 2000;51:540–545. doi: 10.1016/s0016-5107(00)70286-0. [DOI] [PubMed] [Google Scholar]
- 28.Parsi MA, Stevens T, Vargo JJ. Diagnostic and therapeutic direct peroral cholangioscopy using an intraductal anchoring balloon. World J Gastroenterol. 2012;18:3992–3996. doi: 10.3748/wjg.v18.i30.3992. [DOI] [PMC free article] [PubMed] [Google Scholar]


