Abstract
AIM: To investigate an appropriate strategy for the treatment of patients with acute sigmoid volvulus in the emergency setting.
METHODS: A retrospective review of 28 patients with acute sigmoid volvulus treated in the Department of Colorectal Surgery, Changhai Hospital, Shanghai from January 2001 to July 2012 was performed. Following the diagnosis of acute sigmoid volvulus, an initial colonoscopic approach was adopted if there was no evidence of diffuse peritonitis.
RESULTS: Of the 28 patients with acute sigmoid volvulus, 19 (67.9%) were male and 9 (32.1%) were female. Their mean age was 63.1 ± 22.9 years (range, 21-93 years). Six (21.4%) patients had a history of abdominal surgery, and 17 (60.7%) patients had a history of constipation. Abdominal radiography or computed tomography was performed in all patients. Colonoscopic detorsion was performed in all 28 patients with a success rate of 92.8% (26/28). Emergency surgery was required in the other two patients. Of the 26 successfully treated patients, seven (26.9%) had recurrent volvulus.
CONCLUSION: Colonoscopy is the primary emergency treatment of choice in uncomplicated acute sigmoid volvulus. Emergency surgery is only for patients in whom nonoperative treatment is unsuccessful, or in those with peritonitis.
Keywords: Sigmoid colon, Volvulus, Emergency, Colonoscopy
Core tip: Early and correct diagnosis of acute sigmoid volvulus is essential for appropriate treatment aimed at correcting abnormal pathophysiological changes and restoring intestinal transit caused by the volvulus. There is still much debate as to the ideal management of sigmoid volvulus. The results of this study suggest that colonoscopic decompression and derotation is the primary emergency treatment of choice in uncomplicated acute sigmoid volvulus and is a safe treatment modality for recurrent sigmoid volvulus. Emergency surgery is required for patients in whom nonoperative treatment is unsuccessful, or in those with peritonitis, bowel gangrene or perforation.
INTRODUCTION
Acute sigmoid volvulus is defined as torsion of the sigmoid colon around its mesenteric axis, which leads to acute large intestine obstruction, which, if left untreated, often results in life-threatening complications, such as bowel ischemia, gangrene, and perforation[1,2]. Early and correct diagnosis of this disease is essential for appropriate treatment aimed at correcting abnormal pathophysiological changes and restoring intestinal transit caused by the volvulus.
Despite significant progress in the treatment of this disease, no consensus has been reached[3-8]. Emergency surgery is the appropriate treatment for those who present with diffuse peritonitis, intestinal perforation or ischemic necrosis[9,10]. Nonoperative treatment is adopted if there is no evidence of these conditions. Barium enema, rectal tubes, rigid and flexible sigmoidoscopy as therapeutic methods have been adopted by clinicians[11,12]. Colonoscopy, besides being a therapeutic measure, allows the evaluation of colonic mucosa and therefore the presence or absence of signs of ischemia[13], and is effective in more than 70% of patients[14]. The initial management of clinically stable patients in good general condition with sigmoid volvulus is colonoscopic decompression as a first therapeutic option in the emergency setting in our hospital. The objectives of this study were to review our experience and the benefits of colonoscopy in the treatment of patients with acute sigmoid volvulus in the emergency setting.
MATERIALS AND METHODS
We performed a retrospective clinical data review of patients with acute sigmoid volvulus treated in the Department of Colorectal Surgery, Changhai Hospital, Shanghai, China, from January 2001 to July 2012. We included 28 patients who were diagnosed with acute sigmoid volvulus in the emergency department and then admitted to our department for treatment. Patient data included demographics, comorbidities, clinical manifestations, radiological investigations, colonoscopic findings and interventions, and clinical outcome.
Following the diagnosis of acute sigmoid volvulus, an initial colonoscopic approach was adopted if there was no evidence of diffuse peritonitis. If patients failed in the colonoscopic derotation, surgical intervention would be performed. Figure 1 illustrates the flowchart of patients who were admitted to our hospital with acute sigmoid volvulus.
Figure 1.
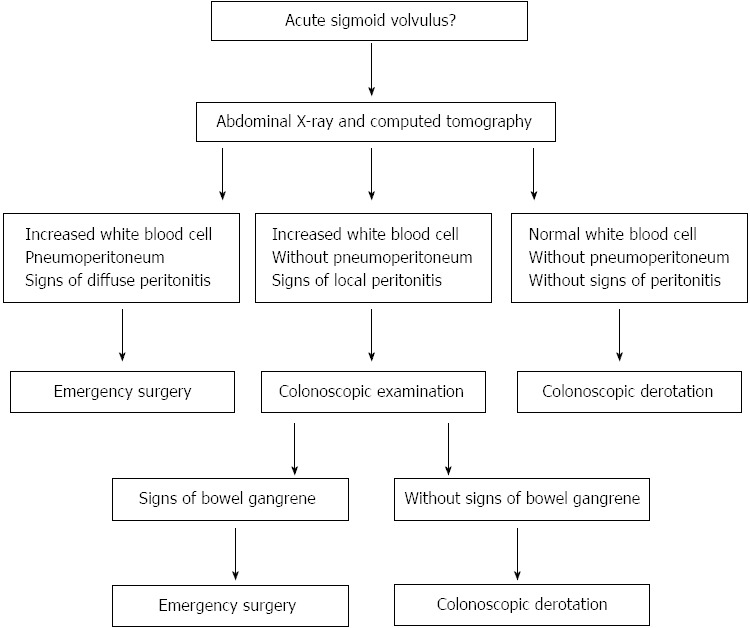
Flowchart of emergency therapeutic strategy for acute sigmoid volvulus.
RESULTS
Of the 28 patients with acute sigmoid volvulus, 19 (67.9%) were male and 9 (32.1%) were female. The mean age was 63.1 ± 22.9 years (range, 21-93 years). Six patients (21.4%) had a history of abdominal surgery. Seventeen patients (60.7%) had a history of constipation.
All patients presented with acute large intestine obstruction. The interval between the development of symptoms and hospitalization ranged from 15 h to 7 d (mean 37.3 ± 28.2 h). Clinical manifestations included abdominal pain in all patients (100%) and vomiting in 8 patients (28.6%). Abdominal examination revealed marked abdominal distension in 20 patients (71.4%). A visible intestinal loop was noted in 8 patients (28.6%). Following rectal examination, blood on the examining finger was absent in all patients (0%).
During the diagnostic period, all 28 patients underwent plain abdominal X-rays (100%), followed by computed tomography (CT) scan of the abdomen in 20 (71.4%). Blood chemistry and hematological profile were routinely studied. Abdominal radiographs showed multiple air/fluid levels and a dilated sigmoid colon in all patients (Figure 2). All patients were found to have positive sigmoid volvulus findings by CT scanning, such as a dilated sigmoid colon and a whirl pattern in the mesentery (Figure 3).
Figure 2.

Plain abdominal X-ray film obtained in the supine position reveals gross dilatation of the colon.
Figure 3.
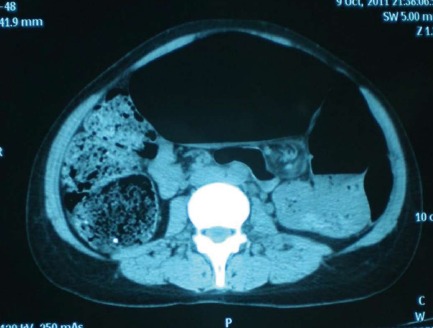
Computed tomography reveals dilated colon with an air/fluid level, as well as the “whirl sign” composed of mesentery and twisted colon.
After early and effective resuscitation, colonoscopy was performed in all patients in order to complete decompression and derotation, and was successful in 26 (92.9%) patients. Emergency surgery was performed in a 41-year-old woman in whom colonoscopic derotation was unsuccessful. A 90-year-old man who did not receive derotation underwent immediate surgery due to a perforation with inlaid adipose tissue 50 cm from the edge of the anus (Figure 4).
Figure 4.
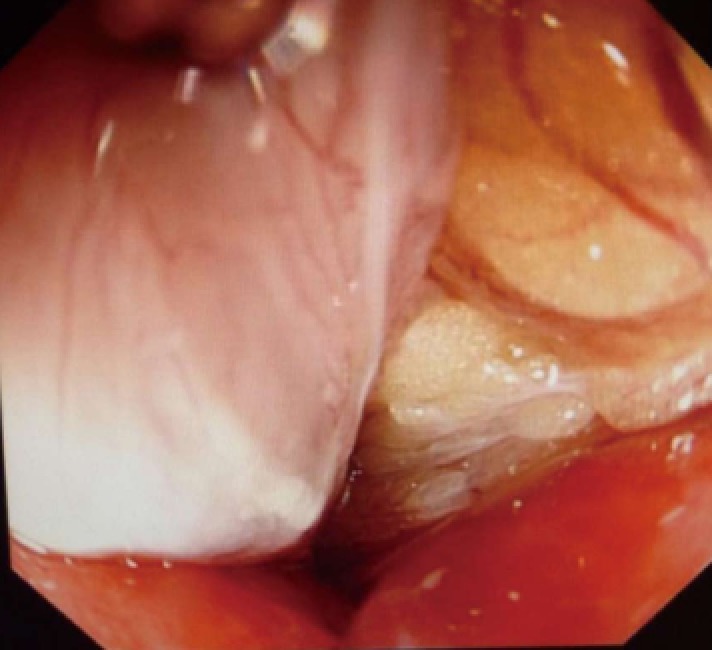
Colonoscopic examination shows a perforation with inlaid adipose tissue.
There was no mortality or morbidity in the colonoscopic treatment group. One of two patients in the surgical treatment group died. Exploration revealed a 3-cm perforation in the sigmoid colon with omentum adhesion, and a dilated, dusky segment of the descending and transverse colon in this patient. Left hemicolectomy and end colostomy were performed. Postoperatively, he was treated in the intensive care unit but died 1 day later due to sepsis with progressive multiple organ failure.
The overall recurrence rate was 26.9% (7/26) after colonoscopic derotation. These patients underwent repeat colonoscopic detorsion without mortality or morbidity.
DISCUSSION
Acute sigmoid volvulus is the third most common cause of large bowel obstruction[15]. It has a wide geographic variation and it differs significantly between high-incidence countries and low-incidence countries[16]. This variation may be associated with differences in anatomy[17]. Acute sigmoid volvulus usually occurs in adult men. The mean age was found to be between 56 and 77 years and nearly one-third of all colonic emergencies in elderly patients are due to sigmoid volvulus[18]. In our patient group, age ranged from 21 to 93 years with a mean of 63.1 ± 22.9 years which showed that the Chinese population with acute sigmoid volvulus also included many younger patients. A preponderance in males compared with females was found and the ratio in our group was 2.1:1 (19 vs 9). This indicated that male preponderance in acute sigmoid volvulus is pronounced in the Chinese population.
The presence of a redundant and mobile sigmoid colon, with a narrow base at the mesenteric root, is one of the major predisposing factors for sigmoid volvulus. Other predisposing factors, such as a high-fiber diet, constipation, previous abdominal surgery, pregnancy, diabetes, or neurological and psychiatric diseases such as dementia or schizophrenia have been described in the literature[19]. In our group, 60.7% of the patients had a history of chronic constipation, and over 15% suffered from diabetes or neurological diseases, and 21.4% of patients had a history of previous abdominal surgery.
The diagnosis of acute sigmoid volvulus is established by clinical and radiological findings. In the majority of patients, a thorough physical examination and abdominal radiographs are adequate to achieve the diagnosis. Typical symptoms include sudden abdominal pain and distension followed by constipation. The most common signs are abdominal tenderness and asymmetrical abdominal distention. Other findings include abnormal bowel sounds, abdominal tympany, a palpable abdominal mass, empty rectum, and dehydration[18]. Plain radiographs are diagnostic in 57%-90% of patients[20,21]. The classical sign of acute sigmoid volvulus is the coffee bean sign. Abdominal CT usually reveals a dilated colon with an air/fluid level and the “whirl sign”, which represents twisted colon and mesentery[22].
Raveenthiran et al[23] recently provided more insight into the pathophysiology of acute sigmoid volvulus. Increasing intraluminal pressure impairs capillary perfusion following the occurrence of acute sigmoid volvulus. Mechanical obstruction due to twisting of mesenteric vessels and thrombosis of mesosigmoid veins contribute to ischemia. Ischemic injury in the mucosa occurs earlier than in other colonic layers and facilitates bacterial translocation and toxemia. A competent ileo-cecal valve converts the proximal colon into a second “closed loop”. Increased intra-abdominal pressure results in the “abdominal compartment syndrome”. Prompt and optimal correction of these pathophysiological features is vital to improve the prognosis of acute sigmoid volvulus.
The treatment of colonic volvulus remains controversial, and depends on the elected procedure and the most appropriate therapeutic approach in terms of the clinical status of the patient, the location of the problem, the suspicion or presence of peritonitis, bowel viability and the experience of the surgical team[19].
Emergency surgery is associated with significant mortality and morbidity. Kassi et al[24] reported that the mortality rate was 12% (n = 3) for Hartmann’s procedure. Surgical site infections (42.86%) were the most common complications. Eleven (50%) of 22 patients had intestinal continuity restored. Bhatnagar et al[25] reported that the risk factors for mortality were: (1) age over 60 years; (2) presence of shock on admission; and (3) positive history of a previous episode of volvulus. With regard to the former two risk factors, special efforts are necessary by intensive care staff to monitor homeostatic disturbance and reduce mortality in older patients (> 60 years) and those presenting with shock at the time of admission. One of our patients died due to sepsis with progressive multiple organ failure on postoperative day 1.
Nonoperative detorsion is advocated as the primary treatment choice in uncomplicated acute sigmoid volvulus. Although rectal tubes, barium enemas or rigid sigmoidoscopy have been widely used, flexible sigmoidoscopy is now the preferred nonoperative procedure. Nonoperative treatment is successful in 70%-91% of cases, with reported complication rates of 2%-4.7% in geriatric patients[26,27]. However, in our patients, the success rate of colonoscopic derotation was 92.9%. Compared with sigmoidoscopy, colonoscopy is readily used in our hospital for endoscopic derotation for several reasons. In addition to a superior success rate and safety profile, it is of adequate length to reach beyond the second constricting point. It also allows better visualization of the colonic mucosa and can guide the decompression and derotation procedure. Colonoscopic suctioning of the proximal colon facilitates quick recovery by removing bacterial toxins. Furthermore, the authors adopt modified double-operating colonoscopy which can help minimize the risk of perforation. Colonoscopic derotation simply converts an emergency into an elective procedure, which facilitates treatment of comorbidity and allows preparation of the bowel prior to definitive surgery. The results from the present study suggest that colonoscopy is a safe and effective treatment modality for acute sigmoid volvulus.
Following derotation, ischemia-reperfusion injury aggravates intestinal dysfunction, and even intestinal ulcer and perforation. Peritoneal exudate, high intestinal fluid accumulation, electrolyte disturbances, and hypoproteinemia lead to serious adverse consequences. Consequently, effective treatment following colonoscopic derotation is very important. Fluid resuscitation should be performed immediately. Vasodilator therapy should be continued, as the use of these agents can ameliorate intestinal tissue microcirculation. Broad-spectrum antibiotics are indicated to control bacterial translocation across the ischemic intestinal wall.
Colonoscopic derotation was followed by recurrence in 26.9% of our patients. These patients underwent successful repeat colonoscopic detorsion without mortality or morbidity. These results suggest that colonoscopy is the primary choice in the treatment of recurrent sigmoid volvulus, particularly in elderly patients who refuse elective surgery.
In conclusion, colonoscopic decompression and derotation is the primary emergency treatment of choice in uncomplicated acute sigmoid volvulus and is a safe treatment modality for recurrent sigmoid volvulus. Emergency surgery is reserved for gangrene and failed decompression, and in patients with a high recurrence rate it may be prudent to consider interval semi-elective resection and primary anastomosis several days after successful decompression.
COMMENTS
Background
Acute sigmoid volvulus is common worldwide, and leads to acute large intestine obstruction, which, if left untreated, often results in life-threatening complications, such as bowel ischemia, gangrene, and perforation. Despite significant progress in the treatment of this disease, no consensus has been reached.
Research frontiers
As the authors described, there is still considerable debate on the ideal management of acute sigmoid volvulus. In this study, the authors demonstrated that colonoscopy is the primary emergency treatment of choice in uncomplicated acute sigmoid volvulus. Surgery is reserved for patients in whom nonoperative treatment is unsuccessful, or in those with peritonitis.
Innovations and breakthroughs
Barium enema, rectal tubes, rigid and flexible sigmoidoscopy have been adopted by clinicians as therapeutic methods. Colonoscopy, besides being a therapeutic measure, allows evaluation of the colonic mucosa and therefore the presence or absence of signs of ischemia, and is effective in more than 70% of patients. The initial management of clinically stable patients in good general condition with sigmoid volvulus is colonoscopic decompression as a first therapeutic option with satisfactory results in the emergency setting.
Applications
By understanding abnormal pathophysiological changes associated with acute sigmoid volvulus, this study may represent a future strategy for therapeutic intervention in the treatment of this condition.
Terminology
Acute sigmoid volvulus is defined as torsion of the sigmoid colon around its mesenteric axis, which leads to acute large intestine obstruction, which, if left untreated, often results in life-threatening complications, such as bowel ischemia, gangrene, and perforation.
Peer review
The authors present a well-written case series describing their experience with sigmoid volvulus. There is still much debate as to the ideal management for this condition. Emergency surgery is reserved for gangrene and failed decompression, and due to a high recurrence rate, it may be prudent to consider interval semi-elective resection and primary anastomosis several days after successful decompression.
Footnotes
Supported by Changhai Hospital 1255 project Fund, No.CH125542500
P- Reviewer Samuel J S- Editor Wen LL L- Editor A E- Editor Ma S
References
- 1.Katsikogiannis N, Machairiotis N, Zarogoulidis P, Sarika E, Stylianaki A, Zisoglou M, Zervas V, Bareka M, Christofis C, Iordanidis A. Management of sigmoid volvulus avoiding sigmoid resection. Case Rep Gastroenterol. 2012;6:293–299. doi: 10.1159/000339216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raveenthiran V. Observations on the pattern of vomiting and morbidity in patients with acute sigmoid volvulus. J Postgrad Med. 2004;50:27–29. [PubMed] [Google Scholar]
- 3.Sule AZ, Misauno M, Opaluwa AS, Ojo E, Obekpa PO. One stage procedure in the management of acute sigmoid volvulus without colonic lavage. Surgeon. 2007;5:268–270. doi: 10.1016/s1479-666x(07)80023-0. [DOI] [PubMed] [Google Scholar]
- 4.Safioleas M, Chatziconstantinou C, Felekouras E, Stamatakos M, Papaconstantinou I, Smirnis A, Safioleas P, Kostakis A. Clinical considerations and therapeutic strategy for sigmoid volvulus in the elderly: a study of 33 cases. World J Gastroenterol. 2007;13:921–924. doi: 10.3748/wjg.v13.i6.921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cartwright-Terry T, Phillips S, Greenslade GL, Dixon AR. Laparoscopy in the management of closed loop sigmoid volvulus. Colorectal Dis. 2008;10:370–372. doi: 10.1111/j.1463-1318.2007.01340.x. [DOI] [PubMed] [Google Scholar]
- 6.Akcan A, Akyildiz H, Artis T, Yilmaz N, Sozuer E. Feasibility of single-stage resection and primary anastomosis in patients with acute noncomplicated sigmoid volvulus. Am J Surg. 2007;193:421–426. doi: 10.1016/j.amjsurg.2006.08.077. [DOI] [PubMed] [Google Scholar]
- 7.Kuzu MA, Aşlar AK, Soran A, Polat A, Topcu O, Hengirmen S. Emergent resection for acute sigmoid volvulus: results of 106 consecutive cases. Dis Colon Rectum. 2002;45:1085–1090. doi: 10.1007/s10350-004-6364-0. [DOI] [PubMed] [Google Scholar]
- 8.Renzulli P, Maurer CA, Netzer P, Büchler MW. Preoperative colonoscopic derotation is beneficial in acute colonic volvulus. Dig Surg. 2002;19:223–229. doi: 10.1159/000064217. [DOI] [PubMed] [Google Scholar]
- 9.Suleyman O, Kessaf AA, Ayhan KM. Sigmoid volvulus: long-term surgical outcomes and review of the literature. S Afr J Surg. 2012;50:9–15. [PubMed] [Google Scholar]
- 10.Coban S, Yilmaz M, Terzi A, Yildiz F, Ozgor D, Ara C, Yologlu S, Kirimlioglu V. Resection and primary anastomosis with or without modified blow-hole colostomy for sigmoid volvulus. World J Gastroenterol. 2008;14:5590–5594; discussion 5593. doi: 10.3748/wjg.14.5590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta SS, Singh O, Paramhans D, Mathur RK. Tube sigmoidostomy: a valuable alternative to sigmoidopexy for sigmoid volvulus. J Visc Surg. 2011;148:e129–e133. doi: 10.1016/j.jviscsurg.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 12.Madiba TE, Thomson SR. The management of sigmoid volvulus. J R Coll Surg Edinb. 2000;45:74–80. [PubMed] [Google Scholar]
- 13.Turan M, Sen M, Karadayi K, Koyuncu A, Topcu O, Yildirir C, Duman M. Our sigmoid colon volvulus experience and benefits of colonoscope in detortion process. Rev Esp Enferm Dig. 2004;96:32–35. doi: 10.4321/s1130-01082004000100005. [DOI] [PubMed] [Google Scholar]
- 14.Martínez Ares D, Yáñez López J, Souto Ruzo J, Vázquez Millán MA, González Conde B, Suárez López F, Alonso Aguirre P, Vázquez Iglesias JL. Indication and results of endoscopic management of sigmoid volvulus. Rev Esp Enferm Dig. 2003;95:544–548, 539-543. [PubMed] [Google Scholar]
- 15.Grossmann EM, Longo WE, Stratton MD, Virgo KS, Johnson FE. Sigmoid volvulus in Department of Veterans Affairs Medical Centers. Dis Colon Rectum. 2000;43:414–418. doi: 10.1007/BF02258311. [DOI] [PubMed] [Google Scholar]
- 16.Ballantyne GH. Review of sigmoid volvulus. Clinical patterns and pathogenesis. Dis Colon Rectum. 1982;25:823–830. doi: 10.1007/BF02553326. [DOI] [PubMed] [Google Scholar]
- 17.Akinkuotu A, Samuel JC, Msiska N, Mvula C, Charles AG. The role of the anatomy of the sigmoid colon in developing sigmoid volvulus: a case-control study. Clin Anat. 2011;24:634–637. doi: 10.1002/ca.21131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Atamanalp SS, Ozturk G. Sigmoid volvulus in the elderly: outcomes of a 43-year, 453-patient experience. Surg Today. 2011;41:514–519. doi: 10.1007/s00595-010-4317-x. [DOI] [PubMed] [Google Scholar]
- 19.Mulas C, Bruna M, García-Armengol J, Roig JV. Management of colonic volvulus. Experience in 75 patients. Rev Esp Enferm Dig. 2010;102:239–248. doi: 10.4321/s1130-01082010000400004. [DOI] [PubMed] [Google Scholar]
- 20.Osiro SB, Cunningham D, Shoja MM, Tubbs RS, Gielecki J, Loukas M. The twisted colon: a review of sigmoid volvulus. Am Surg. 2012;78:271–279. [PubMed] [Google Scholar]
- 21.Burrell HC, Baker DM, Wardrop P, Evans AJ. Significant plain film findings in sigmoid volvulus. Clin Radiol. 1994;49:317–319. doi: 10.1016/s0009-9260(05)81795-7. [DOI] [PubMed] [Google Scholar]
- 22.Hirao K, Kikawada M, Hanyu H, Iwamoto T. Sigmoid volvulus showing “a whirl sign” on CT. Intern Med. 2006;45:331–332. doi: 10.2169/internalmedicine.45.1643. [DOI] [PubMed] [Google Scholar]
- 23.Raveenthiran V, Madiba TE, Atamanalp SS, De U. Volvulus of the sigmoid colon. Colorectal Dis. 2010;12:e1–17. doi: 10.1111/j.1463-1318.2010.02262.x. [DOI] [PubMed] [Google Scholar]
- 24.Kassi AB, Lebeau R, Yenon KS, Katche E, Diane B, Kouassi JC. Morbidity and mortality of Hartmann’s procedure for sigmoid volvulus at the University Hospital of Cocody, Abidjan. West Afr J Med. 2011;30:169–172. [PubMed] [Google Scholar]
- 25.Bhatnagar BN, Sharma CL, Gautam A, Kakar A, Reddy DC. Gangrenous sigmoid volvulus: a clinical study of 76 patients. Int J Colorectal Dis. 2004;19:134–142. doi: 10.1007/s00384-003-0534-8. [DOI] [PubMed] [Google Scholar]
- 26.Avots-Avotins KV, Waugh DE. Colon volvulus and the geriatric patient. Surg Clin North Am. 1982;62:249–260. doi: 10.1016/s0039-6109(16)42684-8. [DOI] [PubMed] [Google Scholar]
- 27.Bak MP, Boley SJ. Sigmoid volvulus in elderly patients. Am J Surg. 1986;151:71–75. doi: 10.1016/0002-9610(86)90014-0. [DOI] [PubMed] [Google Scholar]


