Abstract
Objective
To assess the relationship between body mass index (BMI) and adiposity as well as the influence of injury level on this relationship in 24 women with spinal cord injury (SCI) and 23 able-bodied (AB) women with similar age, race, and BMI.
Design and methods
Body composition was measured by dual energy x-ray absorptiometry (DXA). Analysis of covariance was performed to compare total and regional soft tissue percent fat (PF) measures between groups.
Results
Women with SCI had a higher soft tissue PF than AB women at any given BMI. The BMI-adjusted soft tissue PF (mean ± SE) was 44.4 ± 1.8%, 37.8 ± 1.3%, and 35.9 ±1.1% for tetraplegic, paraplegic, and AB women, respectively. The BMI explained about equal amounts of the variance in soft tissue PF among paraplegic and AB women (65%), but only 28% in tetraplegic women.
Conclusion
This study confirms a limited use of BMI in measuring adiposity in women with SCI, particularly among those with tetraplegia. Our observation of lower BMI cutoff points for defining obesity (28 kg/m2 for paraplegia and 21 kg/m2 for tetraplegia) needs further confirmation. The underweight/malnutrition issue also deserves the consideration while proposing the ideal weight and BMI range for persons with SCI.
Introduction
Because of neurological impairment, body composition drastically deteriorates, as early as 6 months after spinal cord injury (SCI) 1 with loss of lean mass below the level of injury and an increased total fat mass. 2, 3 Lower metabolic rates as a result of reduced lean mass further accelerate the development of excess adipose tissue (obesity) in individuals with SCI. Obesity has been shown to be associated with a broad range of diseases and metabolic abnormalities that affect several different organ systems in the body via atherogenic, neuro-humoral, and hemodynamic mechanisms in the able-bodied (AB) as well as SCI populations. 4–6
Body mass index (BMI) has been widely used in clinical care and research in determining whether an individual is overweight or obese. While BMI is a useful non-invasive screening tool in many epidemiological studies 7, its inability to distinguish between fat mass and lean mass still remains as a major limitation when assessing adiposity. Several studies have shown that as compared to the AB population with similar BMIs, individuals with SCI possessed higher total body percent fat (PF) and fat mass.8–10 Moreover, current BMI guidelines have yielded inconsistent results in the identification of cardiovascular risk factors in individuals with SCI 11. These results suggest that the population-based BMI standards may not be applicable to individuals with SCI in defining overweight and obesity. As a result, lower BMI cut-off points have been proposed in the SCI population 8–10 to account for decreased lean mass. These recommendations, however, are predominantly based on studies of men, and their applications to women with SCI are virtually unknown. Moreover it is well documented in the general population that the relationship between BMI and total body PF is dependent of gender 12,15 and the prevalence of overweight and obesity has been shown to vary by level and completeness of injury in persons with SCI 13,14. Therefore, this study was conducted to: 1) assess the relationship between BMI and adiposity in women SCI as compared to AB women and 2) examine the influence of injury level on this relationship.
Methods
Twenty four healthy women with mobility limitation as a result of SCI (15 with paraplegia [11 thoracic and 4 lumbar injuries], 9 with tetraplegia [2 C4 and 7 C5–C8 injuries]; injury duration: 13.7 ± 12.7 years) and 23 AB women were recruited and frequency-matched for age (42.4 ± 10.5 vs. 43.8 ± 11.6 years), race (19 White, 4 African American, 1 Hispanic vs. 18 White, 4 African American, 1 Hispanic), and BMI (26.1 ± 7.2 vs. 26.8 ± 6.2 kg/m2). Sixteen SCI women had a motor complete lesion (American Spinal Injury Association Impairment Scale [AIS] A or B), while 8 women had an incomplete lesion (AIS C or D). Study participants were recruited from the University of Alabama at Birmingham (UAB) SCI Model System via mailings and community fitness centers via advertising fliers. The study was approved by the UAB Institutional Review Board, and written consent was given before the testing was initiated.
Recumbent height is measured on the right side of the body from the top of the participant’s head to his or her heels while the participant is in a supine position with a non-stretch tape in both groups. Body weight was measured on a wheelchair scale with the subject in the wheelchair first, and then wheelchair was weighed by itself and subtracted from the total weight. Able-bodied women were weighed standing on the same wheelchair balance scale used for women with SCI. Body mass index was calculated by dividing the body weight (kg) by height (m2). Total body and regional (arm, leg, and trunk) fat and lean masses were measured by dual energy x-ray absorptiometry ([DXA]; Hologic QDR-4500W, Madison, WI). Bone tissue was excluded from PF calculations for minimizing the bias from metal fixation attached to the spine or bones.
Statistical Analysis
Data were analyzed using Statistical Package for Social Sciences version 19 (IBM SPSS Statistics 19, IBM Corp., Somers, NY, USA). Descriptive analyses were conducted to summarize the total and regional fat mass, lean mass, and PF across 3 groups. To account for the BMI difference between the paraplegic and tetraplegic groups (27.7 ± 8.2 vs. 23.3 ± 4.2), analysis of covariance was performed to compare body composition between groups while adjusting for BMI. Significance level was set a priori at p < 0.05.
Results
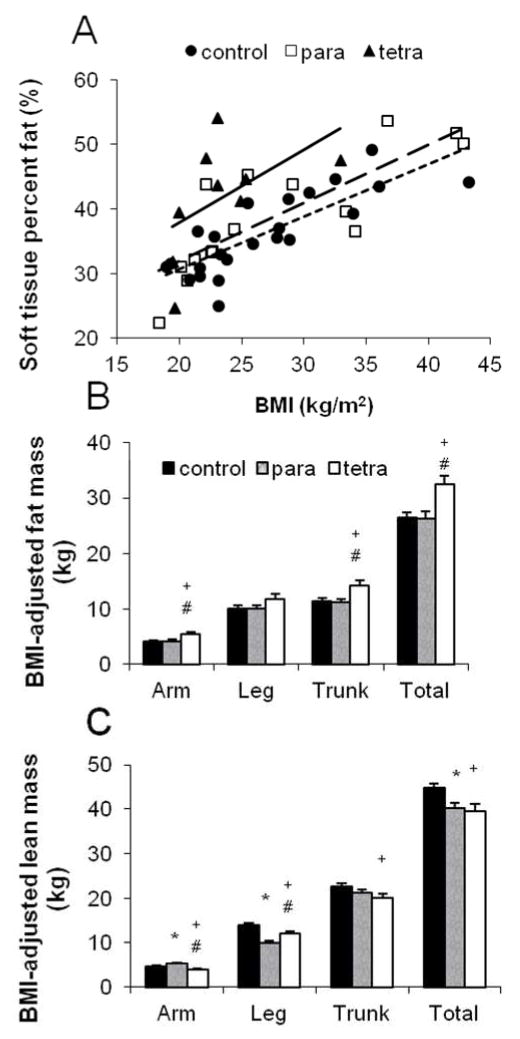
Regardless of injury level, women with SCI had a higher soft tissue PF than AB women at any given BMI. The BMI-adjusted soft tissue PF (mean ± SE) was 44.4 ± 1.8%, 37.8 ± 1.3%, and 35.9 ±1.1% for tetraplegic, paraplegic, and AB women, respectively (Figure 1A). Women with tetraplegia possessed significantly larger amount of total fat mass (kg) than AB and paraplegic women, particularly in the trunk and arm areas (Figure 1B). There was no significant difference in the total and regional fat mass between AB and paraplegic women. As compared with the AB group, women with tetraplegia had significantly lower total and regional (trunk, arm, and leg) lean mass, while women with paraplegia had significantly lower total and leg lean mass, but higher arm lean mass (Figure 1C). Interestingly, women with tetraplegia possessed a lower amount of lean mass in arms, but a higher amount of lean mass in legs than women with paraplegia.
Figure 1.
(A) Soft tissue percent fat in relation to body mass index (BMI) for women with tetraplegia ([tetra]; y = 15.55 + 1.12 x, R2 = 0.28) and paraplegia ([para]; y = 14.13 + 0.89 x, R2 = 0.65) and able-bodied ([control]; y = 14.65 + 0.81 x, R2 = 0.65) women. The slopes did not differ significantly (p= 0.79). (B) BMI-adjusted total and regional fat mass (kg) among groups. (C) BMI-adjusted total and regional lean mass (kg) among groups.*p<0.05, control vs para; +p <0.05, control vs tetra; and #p <0.05, para vs tetra.
Discussion
To our knowledge, this is the first study of women with SCI conducted to examine the relationship between BMI and adiposity and the influence of injury level on this relationship. Our finding of approximately 8.5% higher soft tissue PF in women with SCI is consistent with previous studies of primarily men with SCI 6, 8, 9, 11, 13 that showed a 7.5–10.2 % greater total body PF in the SCI group versus the AB group with similar BMI. This study also supports the premise that BMI is limited in detecting the loss of lean mass and accumulation of fat mass after SCI as a result of decrease in physical activity and lack of neuronal stimulation below the injury level.
Previous studies reported that the BMI explained about 35% of the variance in measured total body PF in persons with SCI.11 The present study further demonstrated that the underestimation of BMI in describing adiposity is particularly problematic for women with tetraplegia. For example, BMI explained about equal amounts of the variance in soft tissue PF among paraplegic and AB women (65%), but only 28% in tetraplegic women (Figure 1A).
A BMI cutoff of 22.1–26.5 kg/m2 has been suggested for use in defining obesity in the SCI population by a previous study of 63 men and 14 women with SCI, based on risk levels of the total body PF and C-reactive protein.8 Because of the common issue concerning metal fixation attached to the spine and bones in persons with SCI, the present study computed soft tissue PF, but not total body PF, for comparison across groups. To preliminarily investigate the BMI cutoff for obesity in women with SCI, we first identified the soft tissue PF corresponding to a BMI of 30 in the AB group (Figure 1A), which is 39%. Our observation based on 23 AB women with an average age of 44 years is reasonably close to the recent NHANES findings of 42%, 41%, and 42% total body PF cut-offs corresponding to a BMI of 30 for non-Hispanic whites, non-Hispanic blacks, and the Hispanic of Mexican origin among women of age 30–49 years. 15 Given a soft tissue PF of 39%, the corresponding BMI in this study was approximately 28 kg/m2 for paraplegic women and 21 kg/m2 for tetraplegic women.
Interestingly, we observed that leg lean mass was significantly higher in women with tetraplegia than women with paraplegia, which might be partially explained by the difference in the completeness of injury. There are more motor incomplete injuries in the tetraplegia group than in the paraplegia group (22 % vs. 13 %), which indicates a higher degree of motor function and preservation of lean mass in the lower extremities among women with tetraplegia.
In conclusion, this study confirms a limited use of BMI in measuring adiposity in women with SCI, particularly among those with tetraplegia. Our observation of lower BMI cutoff points for defining obesity needs further confirmation by studies of a large and representative sample of men and women with SCI across various injury characteristics as well as validation with well-defined health outcomes, using sensitivity and specificity analyses. The underweight/malnutrition issue also deserves the consideration while proposing the ideal weight and BMI range for persons with SCI, as the prevalence of underweight (BMI < 18.5 kg/m2) is much higher in the SCI population than in the general population (4.5%–7.5% vs 0.7%–2.4%).4 The limitations of the present study include a small sample size that precluded this study from stratifying the analysis by completeness of injury. DXA measurements may underestimate the loss of lean muscle tissue in the SCI population; therefore caution should be used when employing DXA alone to estimate body composition in adults with SCI.
Acknowledgments
This study was funded by NIH/NICHD (K12-HD01402) and NIH/NCRR (M01 RR00032) grants.
Footnotes
Disclosure
The authors have no competing interests.
References
- 1.Castro MJ, Apple DF, Jr, Staron RS, Campos GE, Dudley GA. Influence of complete spinal cord injury on skeletal muscle within 6 mo of injury. J Appl Physiol. 1999;86:350–358. doi: 10.1152/jappl.1999.86.1.350. [DOI] [PubMed] [Google Scholar]
- 2.Kocina P. Body composition of spinal cord injured adults. Sports medicine (Auckland, NZ. 1997;23:48–60. doi: 10.2165/00007256-199723010-00005. [DOI] [PubMed] [Google Scholar]
- 3.Spungen AM, Bauman WA, Wang J, Pierson RN., Jr Measurement of body fat in individuals with tetraplegia: a comparison of eight clinical methods. Paraplegia. 1995;33:402–408. doi: 10.1038/sc.1995.90. [DOI] [PubMed] [Google Scholar]
- 4.Chen Y, Cao Y, Allen V, Richards JS. Weight matters: physical and psychosocial well being of persons with spinal cord injury in relation to body mass index. Archives of physical medicine and rehabilitation. 92:391–398. doi: 10.1016/j.apmr.2010.06.030. [DOI] [PubMed] [Google Scholar]
- 5.Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. International journal of obesity (2005) 2008;32:959–966. doi: 10.1038/ijo.2008.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gater DR., Jr Obesity after spinal cord injury. Physical medicine and rehabilitation clinics of North America. 2007;18:333–351. vii. doi: 10.1016/j.pmr.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 7.Seidell JC, Kahn HS, Williamson DF, Lissner L, Valdez R. Report from a Centers for Disease Control and Prevention Workshop on use of adult anthropometry for public health and primary health care. The American journal of clinical nutrition. 2001;73:123–126. doi: 10.1093/ajcn/73.1.123. [DOI] [PubMed] [Google Scholar]
- 8.Laughton GE, Buchholz AC, Martin Ginis KA, Goy RE. Lowering body mass index cutoffs better identifies obese persons with spinal cord injury. Spinal cord. 2009;47:757–762. doi: 10.1038/sc.2009.33. [DOI] [PubMed] [Google Scholar]
- 9.Jones LM, Legge M, Goulding A. Healthy body mass index values often underestimate body fat in men with spinal cord injury. Archives of physical medicine and rehabilitation. 2003;84:1068–1071. doi: 10.1016/s0003-9993(03)00045-5. [DOI] [PubMed] [Google Scholar]
- 10.Maggioni M, Bertoli S, Margonato V, Merati G, Veicsteinas A, Testolin G. Body composition assessment in spinal cord injury subjects. Acta diabetologica. 2003;40 (Suppl 1):S183–186. doi: 10.1007/s00592-003-0061-7. [DOI] [PubMed] [Google Scholar]
- 11.Buchholz AC, Bugaresti JM. A review of body mass index and waist circumference as markers of obesity and coronary heart disease risk in persons with chronic spinal cord injury. Spinal cord. 2005;43:513–518. doi: 10.1038/sj.sc.3101744. [DOI] [PubMed] [Google Scholar]
- 12.Jackson AS, Stanforth PR, Gagnon J, Rankinen T, Leon AS, Rao DC, et al. The effect of sex, age and race on estimating percentage body fat from body mass index: The Heritage Family Study. Int J Obes Relat Metab Disord. 2002;26:789–796. doi: 10.1038/sj.ijo.0802006. [DOI] [PubMed] [Google Scholar]
- 13.Chen Y, Henson S, Jackson AB, Richards JS. Obesity intervention in persons with spinal cord injury. Spinal cord. 2006;44:82–91. doi: 10.1038/sj.sc.3101818. [DOI] [PubMed] [Google Scholar]
- 14.Rajan S, McNeely MJ, Warms C, Goldstein B. Clinical assessment and management of obesity in individuals with spinal cord injury: a review. The journal of spinal cord medicine. 2008;31:361–372. doi: 10.1080/10790268.2008.11760738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heo M, Faith MS, Pietrobelli, Heymsfield SB. Percentage of body fat cutoffs by sex, age, and race-ethnicity in the US adult population from NHANES 1999–20041–4. Am J Clin Nutr. 2012;95:594–602. doi: 10.3945/ajcn.111.025171. [DOI] [PubMed] [Google Scholar]