Abstract
Objective
To evaluate the likelihood of developing de novo erectile dysfunction (ED) after anterior urethroplasty and to determine if this likelihood is influenced by age, stricture length, number of previous procedures or timing of evaluation.
Materials and Methods
PubMed, Embase, Cochrane, and Google Scholar databases were searched for the terms `urethroplasty', `urethral obstruction', `urethral stricture', `sexual function', `erection', `erectile function', `erectile dysfunction', `impotence' and `sexual dysfunction'.
Two reviewers evaluated articles for inclusion based on predetermined criteria.
Results
In a meta-analysis of 36 studies with a total of 2323 patients, de novo ED was rare, with an incidence of 1%.
In studies that assessed postoperative erectile function at more than one time point, ED was transient and resolved at between 6 and 12 months in 86% of cases.
Conclusions
Men should be counselled regarding the possibility of transient or permanent de novo ED after anterior urethroplasty procedures.
Increasing mean age was associated with an increased likelihood of de novo ED, but this was not statistically significant.
Keywords: erectile dysfunction, meta-analysis, systematic review, urethroplasty
Introduction
Urethroplasty is the `gold standard' for treatment of urethral stricture disease. Recently, an increased focus has been placed on the potential risk of erectile dysfunction (ED) after urethroplasty procedures. De novo ED after urethroplasty is thought to be attributable to cavernous and[1] perineal nerve injury, or to the disruption of bulbar artery flow[2]. Proposed surgical methods for reducing injury to these structures during urethroplasty include bulbospongiosus and perineal nerve preservation[3], bulbar artery preservation[4], and non-transection of the corpus spongiosum[5].
The objective of the present study was to assimilate and summarize the available data on de novo ED stemming from anterior urethroplasty procedures. We wanted to determine the incidence of de novo ED after anterior urethroplasty and assess if this incidence was associated with age or number of previous urethroplasty procedures, and to determine whether all patients were questioned about postoperative erectile function. We also wanted to assess if de novo ED resolved or persisted over time. To our knowledge no guideline-based[6,7] systematic review or meta-analysis has been completed on this topic.
Materials and Methods
Systematic review
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and Meta-analysis of Observational Studies in Epidemiology (MOOSE) criteria were followed for systematic review [6,7]. All inclusion and exclusion criteria were determined by author consensus before the literature search was begun.
Literature search
Electronic searches of PubMed, EMBASE, Google Scholar and Cochrane databases were conducted using the search terms, `urethroplasty', `urethral obstruction', `urethral stricture', `sexual function', `erection', `erectile function', `erectile dysfunction', `impotence' and `sexual dysfunction'. The search strategy and search terms were constructed with the assistance of an experienced medical librarian. The search was limited to human studies. A manual search of reference lists from the articles selected for inclusion in this study was also performed. Abstracts presented at national urology meetings appropriate for inclusion in the present study were identified through EMBASE and Google Scholar searches to identify additional studies (`grey material') and studies that may have a negative result. These abstracts were matched with the corresponding articles written later by the same groups when a complete article was available for inclusion, and only the completed article was included for review. Experts in reconstructive urology were also queried to identify any additional articles that should be included for review.
Eligibility criteria
Eligibility criteria were determined before the literature search was begun. We included only English-language studies on patients who underwent anterior urethroplasty procedures because of difficulties obtaining standardized translation of non-English-language studies. As urethroplasty techniques have evolved over time and systematic standards for assessing surgical complications have become more universal, we included studies from the last 15 years. Manuscripts with a cohort that included both adult and paediatric patients were included, with efforts made to extract data on adult patients only when possible as little to no assessment on erectile function has been performed on paediatric patients.
Exclusion criteria consisted of patients undergoing posterior urethroplasty, case reports/case series with nine or fewer patients, and studies with only paediatric patients aged ≤18 years. Studies in which the majority of patients had ED owing to pelvic trauma before urethroplasty, and studies comparing urethroplasty with primary realignment in pelvic fracture urethral distraction defects were excluded. Abstracts with incomplete data about the number of patients with postoperative ED were also excluded, as these data could not be properly interpreted.
Study selection process
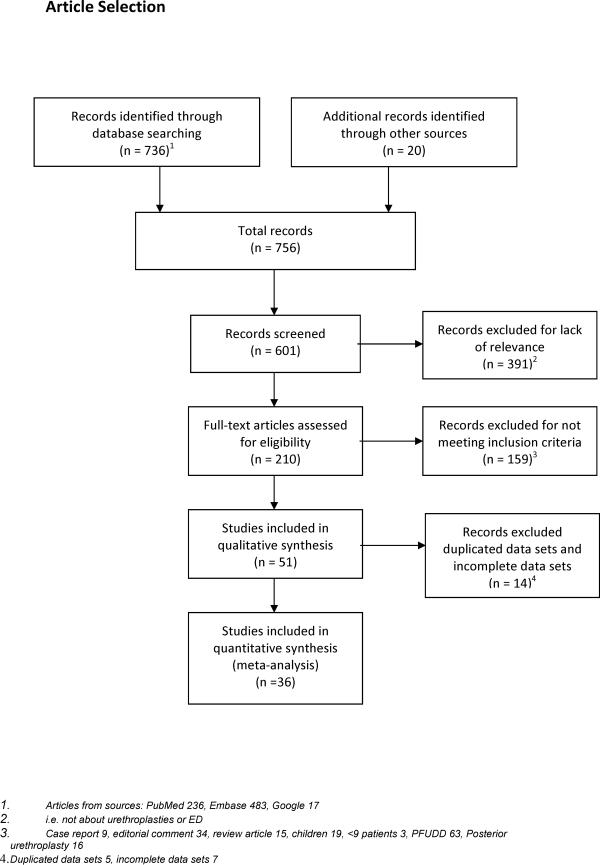
Our initial search using English-language and human participant limits identified 736 articles. An additional 20 articles were included based on identification from the references of the included articles. The titles and abstracts of these articles were reviewed by two authors, and a final 36 articles were selected for inclusion based on independent review and consensus discussion between the authors of the present study. Articles were excluded owing to lack of relevance (391), not meeting defined inclusion criteria (159), and duplication or incomplete information (14) (Fig. 1). Manuscripts for all selected articles were obtained and analysed.
Fig. 1.
Flow chart of inclusion and exclusion of studies for the meta-analysis.
Data extraction
Two authors independently extracted predetermined categorical information data from the selected articles. This information included: study dates; number and age of patients; mean stricture length; location of the stricture; type of urethroplasty performed; number of patients with de novo ED after urethroplasty; whether or not this ED resolved during the timeframe of the study; length of study follow-up whether or not all patients were questioned about erectile function; whether or not patients were questioned about erectile function before their operation; whether or not a standardized questionnaire such as the International Index of Erectile Function (IIEF) was used; and whether the study was prospective or retrospective (Table 1[2,5,8–41]).
Table 1.
Characteristics of studies included for analysis
| Authors, year | Study Type | No. of pati ents | Age (range), years | Months follow-up (range) | All Patients questioned about ED, pre-/postoperatively? | Questionnaire | de novo postoperative ED, n (%) | Urethroplasty type | Stricture location | Comments |
|---|---|---|---|---|---|---|---|---|---|---|
| Iselin CE, Webster GD, 1999 [15] | retrospective | 29 | 43 (10–81) | 19 (10–37) | Not stated/Not stated | No | 4 (14) | DO: 12 DO + EPA: 13 DO + PF: 4 27 used MG, 2 used BMG |
Bulbar | Moderate ED that resolved spontaneously in three patients at 6-month follow-up, one patient required PDE5i |
| Coursey JW, et al., 2001 [20] | retrospective | 152 | 45.7 (17–83) | 36 (3–149) | No/Yes | Internally validated questionnaire | 47 (30.9) | EPA: 56 BMG: 26 PF: 44 Other: 26 |
Anterior | Worse ED associated with longer stricture length, no significant difference in ED rates when compared with circumcision control group |
| Guralnick ML, Webster GD, 2001 [35] | retrospective | 29 | 44 (15–79) | 28 (3–126) | No/Yes | Non-standardized questionnaire | 1 (3.4) | DO augmented anastomosis: 20 VO augmented anastomosis: 9 7 used PF, 22 used BMG or MG |
Bulbar | - |
| Rao HS, et al., 2001 [18] | prospective | 12 | 40.5 (20–66) | 15.6 (5–25) | Not stated/Not stated | Not stated | 0 | PF | Bulbar: 5 Bulbopenile: 5 Penile: 2 |
- |
| Santucci RA, et al., 2002 [10 | retrospective | 168 | 38 (6–82) | 70 (6–291) | Not stated/Not stated | Not stated | 1 (1) | EPA | Bulbar | - |
| Dubey D, et al., 2003 [33] | retrospective | 109 | 39.5 (11–62) | 33.5 (11.4–58.7) | Not stated/Not stated | Not stated | 10 (9) | Ventral PF: 52 Dorsal PF: 23 VO + BMG or MG: 18 DO BMG or MG: 16 |
Bulbar: 56 Bulbopenile: 39 Penile: 14 |
No significant ED difference in dorsal vs ventral onlay |
| Kessler TM, et al., 2003 [26] | retrospective | 238 | 43 (28–59) | 28.9 (12–73) | Yes/Not stated | Not stated | 8 (3.4) | BMG: 30 PF: 100 EPA: 40 MG: 68 |
Membranous: 13 Membranobulbar: 12 Bulbar: 59 Bulbopenile: 67 Penile: 54 Fossa: 20 Entire length: 13 |
- |
| Hosseini J, Soltanzadeh K., 2004 [8] | retrospective | 37 | 28.5 (5–50) | 27.5 (6–50) | Not stated/No | Not stated | 1 (2.7) | VO + BMG: 18 VO + PF: 19 |
Bulbar: 13 Bulbopenile: 11 Penile: 13 |
Temporary ED, resolved after 12 months |
| Dubey D, et al., 2005, [13] | retrospective | 39 | 32.2 (11–48) | 32.5 (3–52) | Not stated/No | Not stated | 0 (0) | DO + BMG(1 stage): 25 DO + BMG(2 stage): 14 |
Bulbopenile: 30 Penile: 9 |
- |
| MacDonald MF, et al., 2005 [27] | retrospective | 54 | 46 (18–78) | 27 (3–51) | Not stated/Not stated | Not stated | 6 (11.1) | EPA: 34 VO + BMG: 20 |
Membranobulbar: 7 Bulbar: 43 Penile: 4 |
All ED was mild and responded to PDE5i |
| Raber M, et al., 2005 [16] | prospective | 30 | 42 (18–69) | 51 (20–74) | Yes/Yes | IIEF | 0 (0) | DO + MG: 17 DO + BMG:13 |
Bulbar | - |
| Morey AF, Kizer WS 2006 [32] | retrospective | 22 | 39.95 (not stated) | 26.1 (16–64) | Not stated/No | Internally validated questionnaire | 2 (9.09) | EPA | Proximal bulbar | No ED difference between end-to-end and extended anastomotic techniques |
| Anger JT, et al., 2007 [37] | prospective | 25 | 39 (26–66) | 6.2 (not stated) | Yes/Yes | IIEF | 1 (4) | EPA: 9 Augment EPA + BMG: 15 DO: 2 |
Pan-bulbar: 5 Mid-post bulbar: 13 Mid-distal bulbar: 7 |
Nonsignificant change when comparing pre- and postoperative ED; older men (>47 years) with worse preoperative EF trended towards worse postoperative EF but not significantly. |
| Barbagli G, et al., 2007 [25] | retrospective | 153 | 39 (20–50) | 68 (12–218) | No/No | Non-standardized questionnaire | 0 (0) | EPA | Bulbar | - |
| Eltahawy EA, et al., 2007 [24] | retrospective | 260 | 38.4 (14–78) | 50.2 (6–122) | Not stated/Not stated | Not stated | 6 (2.3) | EPA | Bulbar | Four with good erections with oral PDE5i, others declined therapy |
| Erickson BA, et al., 2007 [21] | retrospective | 59 | 41.7 (15–65) | 22.3 (7.5–37.1) | No/Yes | O'Leary | 13 (25) | EPA: 23 DO or VO + BMG: 22 2 stage w/BMG: 7 |
Anterior | No significant ED difference pre- vs postoperatively; postoperative EF scores improved 1 year after surgery; type of repair did not affect EF scores |
| Jain DK, et al., 2007 [30] | retrospective | 12 | 38.9 (17–58) | 14.2 (2–26) | Not stated/Not stated | Not stated | 0 | DO + BMG | Bulbar: 2 Bulbopenile: 4 Penile: 6 |
- |
| Levine LA, et al., 2007 [11] | retrospective | 53 | 45 (21–75) | 53 (15–120) | Not stated/Not stated | Not stated | 0 (0) | DO + BMG: 24 VO + BMG: 22 2 stage: 7 |
Bulbar: 35 Penile: 18 |
- |
| O'Riordan, A, et al., 2008 [29] | prospective | 52 | 39 (19–61) | 34 (12–80) | Not stated/No | Not stated | 3 (6) | DO + BMG | Bulbar | Postoperative ED resolved in two patients, not in one patient with DM |
| Singh PB, et al., 2008 [17] | retrospective | 55 | 29 (18–58) | 17.5 (not stated) | Not stated/Not stated | Not stated | 0 (0) | DO + BMG | Bulbar: 14 Penile: 11 Bulbopenile: 30 |
- |
| Ammani A, et al., 2009 [41] | prospective | 20 | 34 (19–45) | 32 (14–68) | Not stated/Yes | IIEF | 0 (0) | EPA | Bulbar | - |
| Das SK, et al., 2009 [23] | retrospective | 30 | 28 (18–58) | 9 (4–12) | Not stated/Not stated | Not stated | 0 (0) | DO + BMG | Bulbar: 6 Bulbopenile: 6 Penile: 18 |
- |
| Meeks JJ, Eriksson B,2009 [39] | not stated | 21 | 46 (18–77) | 18 (5–42) | Not stated/Not stated | Not stated | 1 (4.7) | Full thickness abdominal skin grafts | Bulbar: 11 Penile: 13 Fossa: 8 Bulbopenile: 4 |
- |
| Ortega JLL, Pena CP 2009 [34] | retrospective | 100 | 41 (18–79) | Not stated (5–125) | Not stated/Not stated | Not stated | 7 (7) | EPA: 57 DO or VO + BMG: 20 PF: 23 |
Bulbar: 78 Penile: 22 |
- |
| Rourke K 2009 [31] | prospective | 93 | Not stated | 12 (12–57) | Not stated/Not stated | Subjective symptom analysis | 5 (5) | DO + BMG augmented anastomosis | Bulbar | - |
| Seitz M, et al., 2009 [38] | not stated | 13 | 53.8 (24–76) | 12 (not stated) | Not stated/Yes | Non-standardized questionnaire | 0 | EPA: 8 DO + MG: 5 |
Bulbar: 9 Penile: 4 |
- |
| Arlen AM, et al., 2010 [12] | retrospective | 24 | 43.2 (26–71) | 10.5 (1–72) | Not stated/Not stated | No | 0 (0) | BMG | Anterior | - |
| Erickson BA, et al., 2010 [2] | prospective | 52 | 40.67 (26–56) | 7.2 (17 days to 22.8mo) | Yes/Yes | IIEF | 20 (38) | EPA: 20 Augmented EPA: 15 VO: 11 2 stage: 6 |
Bulbar: 35 Penile: 17 |
Recovery of EF in all but two patients between 92 and 398 days |
| Lumen N, et al., 2010 [40] | prospective | 10 | 36.5 (16–60) | 46.6 (15–79) | Not stated/Yes | Non-standardized questionnaire | 0 | Ventral longitudinal stricturotomy w/transverse closure 4 pts had concurrent urethroplasty at another site: PF (2 penile), BMG (2; 1 bulbar, 1 penile) | Bulbar: 6 Fossa: 4 |
- |
| Onol SY, et al., 2010 | retrospective | 16 | Not stated | 24.6 (4–96) | Not stated/Not stated | Not stated | 0 | Circular BMG | Meatal | - |
| Singh UP, et al., 2010 [22] | retrospective | 150 | 40 (18–73) | 33 (4–72) | No/Yes | O'Leary | 0 (0) | EPA: 59 DO + BMG: 55 PF: 36 |
Bulbar: 95 Bulbopenile: 47 Penile: 8 |
- |
| Andrich DE, Mundy AR 2011 [5] | retrospective | 22 | 34 (21–65) | 12 (6–21) | No/ Not stated | No | 2 (9) | Non-transecting EPA | Bulbar | Temporary ED, resolved spontaneously |
| Dogra PN, et al., 2011 [19] | prospective | 78 | 37.9 (21–71) | 15.5 (13.2–17.8) | Yes/Yes | IIEF | 15 (20) | PF: 14 DO + BMG: 29 DO + MG: 3 EPA: 32 |
Bulbar: 53 Penile: 25 |
96% recovery at 6 months, three who did not recover EF were older and had mild-to-moderate ED preoperatively. |
| Grossgold E, et al., 2011 [28] | retrospective | 28 | 46 (not stated) | 28.7 (1–114) | No/No | No | 4 (14) | DO + BMG augmented anastomosis for recurrent stricture | Bulbar | - |
| Sharma V, et al.,2011 [9] | prospective | 34 | 34.6 (18–60) | 8.4 (3–13) | Yes/Yes | O'Leary | 8 (24) | EPA: 18 Progressive perineal: 9 DO + BMG: 9 Staged: 7 |
Bulbomembranous: 2 Bulbar: 18 Penile: 7 Entire length: 7 |
- |
| Welk BK, Kodama RT 2012 [36] | retrospective | 44 | 40 (34–55) | 27.6 (14.4–45.6) | Not stated/No | Non-standardized questionnaire | 0 (0) | Non-transecting EPA: 21 DO + BMG: 23 |
Prox bulbar: 31 Distal bulbar: 10 Penile: 3 |
- |
BMG, buccal mucosa graft; DM, diabetes mellitus; DO, dorsal onlay; EPA, excision and primary anastomosis; EF, erectile function; MG, mesh graft; PDE5i, phosphodiesterase 5 inhibitor.
PF, pedicled flap; VO, ventral onlay.
Statistical analysis
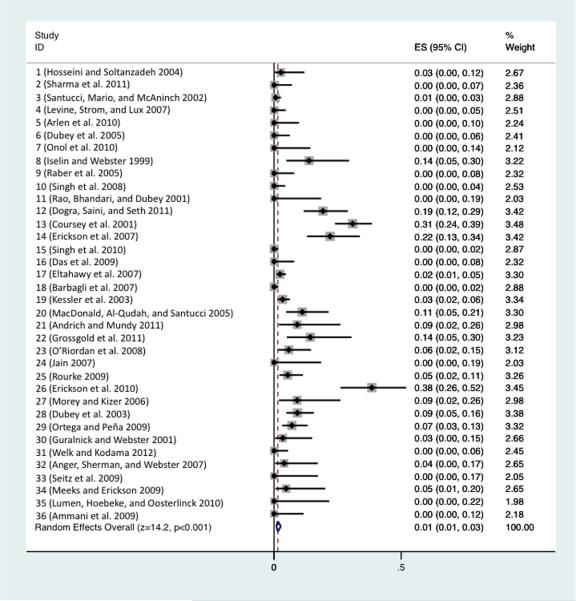
A random effects meta-analysis was performed using the metan command in Stata Version 12.1 (StataCorp, College Station, TX, USA)[42]. The inputs to the meta-analysis were the proportion of patients with de novo ED and associated 95% CI for each of the studies. As a number of the studies had zero patients with de novo ED, CIs were derived using the Jeffreys method[43] as implemented in the ci command in Stata 12. Analyses were conducted on the log-transformed scale and then back-transformed for display purposes in the forest plot. Associations of the proportion of de novo ED with study-level characteristics were evaluated by both meta-regression and subgroup forest plots. Statistical analyses were performed by the University of California San Francisco Clinical and Translational Science Institute Biostatistics Consultation Service.
Results
Thirty-six articles with 2323 total patients who underwent anterior urethroplasty procedures met the inclusion criteria for meta-analysis. The incidence of post-urethroplasty de novo ED ranged from 0 to 38%. The present meta-analysis found that de novo ED was rare, with an incidence of 1% (CI 1–3%)(Fig.2). The five studies that reported a de novo post-urethroplasty ED incidence of >20% were all conducted after 2001, all used a questionnaire to assess ED, and all patients were directly questioned about ED postoperatively.
Fig. 2.
Forest plot of de novo ED after anterior urethroplasty across all studies.
Interestingly, the de novo ED incidence was not increased when patients were directly asked about erectile function (odds ratio [OR] 0.83 [CI 0.06–10.90]). Five of the 12 studies that stated all patients were asked about erectile function reported 0% de novo postoperative ED. Additionally, de novo ED was not associated with stricture location or type of repair (Table 1).
In many cases de novo ED resolved 6–12 months after surgery. Seven of the 21 studies that reported de novo ED reported resolution of ED in 86% (50/58) of cases (Table 1). Fourteen of the studies did not report resolution of ED over time and did not assess ED postoperatively at more than one time point.
Before initiating the present study, we hypothesized that patients who had undergone multiple failed previous procedures for their urethral stricture disease would have a higher risk of de novo ED. This was not demonstrated in our statistical analysis. There was no statistically significant association between number of failed previous direct vision internal urethrotomies, urethral dilations or urethroplasty procedures and de novo ED (OR 1.003 [CI 0.994–1.012 per every additional failed previous procedure]). There was also no association between mean stricture length and de novo ED (OR 0.91 [CI 0.66–1.25 per each additional 1 cm mean stricture length]).
Since ED increases with age, we hypothesized that older patients would have an increased risk of de novo ED. There was a slight association between mean age in the study group and de novo ED with an OR 1.12 (CI 0.97–1.31) for each additional year in mean age, but this was not significant.
Discussion
This systematic review and meta-analysis of urethroplasty and ED examining articles from 1997 to 2012 with 2323 total patients found that the incidence of de novo ED was low (1%, CI 1–3%). Although this incidence is low, there was substantial heterogeneity in the studies (I-squared=93%, P<0.001) indicating that there was more variation than would be expected by chance alone (Fig. 2). The substantial heterogeneity in these studies has a large impact on the result and may underestimate the risk of de novo ED after urethroplasty. This heterogeneity may be attributable, in part, to the variation in how ED was reported and assessed in each study. Although not explicitly stated, some studies that did not question all patients postoperatively about erectile function may have relied on patient volunteered self-reporting, which may underestimate de novo ED. Future studies on urethroplasty outcomes should include pre- and postoperative analysis of ED to allow better future analyses and comparisons across studies.
The strengths of the present study include that fact that it provides a comprehensive review of the urethroplasty literature with broad inclusion criteria. To our knowledge, this is the first systematic review of ED related to urethroplasty procedures that follow the standardized systematic review PRISMA and MOOSE criteria[6,7]. Study limitations include the limiting of the search criteria to English-language studies and lack of specific data on whether or not all patients had been questioned regarding erectile function before surgery in some series. Little information was available on patient characteristics that may influence ED risk, such as vascular disease and diabetes. There was also a lack of a standardized validated questionnaires administered to patients in most series. In studies that used a validated questionnaire such as the IIEF, the authors of those studies determined whether the decline in IIEF constituted ED and did not all use a standardized decrease in IIEF score to determine de novo ED. In some studies, it was unclear as to whether all patients were evaluated for ED or if only patients who self-reported ED were included. Many studies did not clearly delineate the number of patients who underwent previous urethroplasty procedures vs internal urethrotomy or dilation procedures, so all previous procedures had to be assessed together. We have addressed these limitations by including information on these variables for each study included for meta-analysis (Table 1), but we do acknowledge that these limitations may greatly influence the outcomes of the present study, especially with potential under-reporting of de novo ED in studies that did not question all patients about ED pre- and postoperatively.
The present article shows the change in urethroplasty outcome reporting over time. More recent studies were more likely to use a questionnaire and were more likely to assess ED both pre- and postoperatively. This stresses the importance of assessing all patients before and after urethroplasty operations to obtain similar results across studies. It also suggests that older studies that did not question all patients pre- and postoperatively may be under-reporting the true incidence of de novo ED.
Most studies evaluating ED after urethroplasty do not include a control surgery for comparison. A study comparing ED after anterior urethroplasty to ED in age-matched control patients receiving circumcision found 30.9% of urethroplasty patients and 27.3% of circumcision patients reported ED[20]. While circumcision incision may alter penile sensation, it does not significantly alter penile blood flow or erectile innervation, and psychogenic effects on erectile function associated with any penile surgery must be taken into consideration.
For most patients who underwent urethroplasty and who experienced de novo ED, ED resolved over time, with the majority of patients returning to baseline erectile function between 5 and 12 months after treatment [2,5,8,19]. This suggests that ED after urethroplasty may be attributable to both long-term and short-term effects. Long-term effects include neurovascular damage from the operation itself and may include postoperative alterations in blood supply unmasking vasculogenic ED in older patients. Shortterm effects are more likely to be caused by the psychological impact of surgery and catheterization. Short-term effects may also include alterations in blood supply that are compensated for by revascularization during healing.
We propose that future urethroplasty studies include prospectively collected validated questionnair on ED and that standardized follow-up periods for evaluation of ED be used. This will allow a more systematic assessment of ED after urethroplasty that will be comparable across cohort studies. This may allow for alterations in urethroplasty technique based on ED risk in particular cases. Additionally, patients may be better counselled preoperatively on possible risks of ED in the short and long term.
In conclusion, the present meta-analysis found that the risk of de novo ED after anterior urethroplasty was low at 1%. Many cases of de novo ED resolved within 6–12 months; however, the possibility of de novo post-urethroplasty ED, even if transient from the psychological impact of surgery or during revascularization, should be discussed during preoperative evaluation.
Supplementary Material
List of excluded studies and reason for exclusion
PRISMA criteria checklist
Acknowledgements
We appreciate the guidance and recommendations of Gloria Won, MLIS with review of our search terms for inclusion of all relevant studies and for assistance with our EMBASE search.
We appreciate the assistance of John Boscardin and the University of California San Francisco Clinical and Translational Science Institute with biostatistical analysis. This project was supported by the National Center for Research Resources, the National Center for Advancing Translational Sciences, and the Office of the Director, National Institutes of Health, through UCSF-CTSI Grant Number KL2 RR024130. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
This research was supported by the National Institute for Health grant K12DK083021 (BNB).
Abbreviations
- ED
erectile dysfunction
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- MOOSE
Meta-analysis of Observational Studies in Epidemiology
- IIEF
International Index of Erectile Function.
References
- 1.Lue TF, Zeineh SJ, Schmidt RA, Tanagho EA. Neuroanatomy of penile erection: its relevance to iatrogenic impotence. JURO. 1984 Feb.131(2):273–80. doi: 10.1016/s0022-5347(17)50344-4. [DOI] [PubMed] [Google Scholar]
- 2.Erickson BA, Granieri MA, Meeks JJ, Cashy JP, Gonzalez CM. Prospective Analysis of Erectile Dysfunction After Anterior Urethroplasty: Incidence and Recovery of Function. J. Urol. Elsevier Inc. 2010 Feb.183(2):657–61. doi: 10.1016/j.juro.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 3.Barbagli G, De Stefani S, Annino F, De Carne C, Bianchi G. Muscle- and Nerve-sparing Bulbar Urethroplasty: A New Technique. European Urology. 2008 Aug.54(2):335–43. doi: 10.1016/j.eururo.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 4.Jordan GH, Eltahawy EA, Virasoro R. The Technique of Vessel Sparing Excision and Primary Anastomosis for Proximal Bulbous Urethral Reconstruction. J. Urol. 2007 May;177(5):1799–802. doi: 10.1016/j.juro.2007.01.036. [DOI] [PubMed] [Google Scholar]
- 5.Andrich DE, Mundy AR. Non-transecting anastomotic bulbar urethroplasty: a preliminary report. BJU Int. 2011 Sep. doi: 10.1111/j.1464-410X.2011.10508.x. no-no. [DOI] [PubMed] [Google Scholar]
- 6.Moher D, Liberati A, Tetzlaff J. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine. 2009 [PMC free article] [PubMed] [Google Scholar]
- 7.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 8.Hosseini J, Soltanzadeh K. A comparative study of long-term results of Buccal Mucosal Graft and Penile Skin Flap techniques in the management of diffuse anterior urethral strictures: first report in Iran. Urol J. 2004;1(2):94–8. [PubMed] [Google Scholar]
- 9.Sharma V, Kumar S, Mandal AK, Singh SK. A Study on Sexual Function of Men with Anterior Urethral Stricture before and after Treatment. Urol Int. 2011;87(3):341–5. doi: 10.1159/000330268. [DOI] [PubMed] [Google Scholar]
- 10.Santucci RA, Mario LA, McAninch JW. Anastomotic urethroplasty for bulbar urethral stricture: analysis of 168 patients. J. Urol. 2002 Apr.167(4):1715–9. [PubMed] [Google Scholar]
- 11.Levine LA, Strom KH, Lux MM. Buccal Mucosa Graft Urethroplasty for Anterior Urethral Stricture Repair: Evaluation of the Impact of Stricture Location and Lichen Sclerosus on Surgical Outcome. J. Urol. 2007 Nov.178(5):2011–5. doi: 10.1016/j.juro.2007.07.034. [DOI] [PubMed] [Google Scholar]
- 12.Arlen AM, Powell CR, Hoffman HT, Kreder KJ. Buccal Mucosal Graft Urethroplasty. TheScientificWorldJOURNAL. 2010;10:74–9. doi: 10.1100/tsw.2010.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DUBEY D, SEHGAL A, SRIVASTAVA A, MANDHANI A, KAPOOR R, KUMAR A. BUCCAL MUCOSAL URETHROPLASTY FOR BALANITIS XEROTICA OBLITERANS RELATED URETHRAL STRICTURES: THE OUTCOME OF 1 AND 2-STAGE TECHNIQUES. J. Urol. 2005 Feb.173(2):463–6. doi: 10.1097/01.ju.0000149740.02408.19. [DOI] [PubMed] [Google Scholar]
- 14.J Sex Med. Vol. 7. Blackwell Publishing Inc; 2010. POSTER PRESENTATIONS; pp. 403–64. [Google Scholar]
- 15.Iselin CE, Webster GD. Dorsal onlay graft urethroplasty for repair of bulbar urethral stricture. JURO. 1999 Mar.161(3):815–8. [PubMed] [Google Scholar]
- 16.Raber M, Naspro R, Scapaticci E, Salonia A, Scattoni V, Mazzoccoli B, et al. Dorsal Onlay Graft Urethroplasty Using Penile Skin or Buccal Mucosa for Repair of Bulbar Urethral Stricture: Results of a Prospective Single Center Study. European Urology. 2005 Dec.48(6):1013–7. doi: 10.1016/j.eururo.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 17.Singh PB, Das SK, Kumar A, Sharma GK, Pandey AK, Swain S, et al. Dorsal onlay lingual mucosal graft urethroplasty: Comparison of two techniques. International Journal of Urology. 2008 Sep.15(11):1002–5. doi: 10.1111/j.1442-2042.2008.02151.x. [DOI] [PubMed] [Google Scholar]
- 18.Rao HS, Bhandari M, DUBEY D. Dorsal placement of the pedicled preputial/penile onlay flap for anterior urethral stricture: is it more logical? Arch. Esp. Urol. 2001 Sep.54(7):749–55. [PubMed] [Google Scholar]
- 19.Dogra PN, Saini AK, Seth A. Erectile dysfunction after anterior urethroplasty: a prospective analysis of incidence and probability of recovery–single-center experience. Urology. 2011 Jul.78(1):78–81. doi: 10.1016/j.urology.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 20.Coursey JW, Morey AF, McAninch JW, Summerton DJ, Secrest C, White P, et al. Erectile function after anterior urethroplasty. J. Urol. 2001 Dec.166(6):2273–6. [PubMed] [Google Scholar]
- 21.Erickson BA, Wysock JS, McVary KT, Gonzalez CM. Erectile function, sexual drive, and ejaculatory function after reconstructive surgery for anterior urethral stricture disease. BJU Int. 2007 Mar.99(3):607–11. doi: 10.1111/j.1464-410X.2006.06669.x. [DOI] [PubMed] [Google Scholar]
- 22.Singh UP, Maheshwari R, Kumar V, Srivastava A, Kapoor R. Impact on sexual function after reconstructive surgery for anterior urethral stricture disease. Indian J Urol. 2010 Apr.26(2):188–92. doi: 10.4103/0970-1591.65384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Das SK, KUMAR A, Sharma GK, Pandey AK, Bansal H, Trivedi S, et al. Lingual Mucosal Graft Urethroplasty for Anterior Urethral Strictures. URL. 2009 Jan.73(1):105–8. doi: 10.1016/j.urology.2008.06.041. Elsevier Inc. Elsevier Inc. [DOI] [PubMed] [Google Scholar]
- 24.Eltahawy EA, Virasoro R, Schlossberg SM, McCammon KA, Jordan GH. Long-Term Followup for Excision and Primary Anastomosis for Anterior Urethral Strictures. J. Urol. 2007 May;177(5):1803–6. doi: 10.1016/j.juro.2007.01.033. [DOI] [PubMed] [Google Scholar]
- 25.Barbagli G, De Angelis M, Romano G, Lazzeri M. Long-Term Followup of Bulbar End-to-End Anastomosis: A Retrospective Analysis of 153 Patients in a Single Center Experience. J. Urol. 2007 Dec.178(6):2470–3. doi: 10.1016/j.juro.2007.08.018. [DOI] [PubMed] [Google Scholar]
- 26.KESSLER TM, SCHREITER F, KRALIDIS G, HEITZ M, OLIANAS R, FISCH M. Long-term Results of Surgery For Urethral Stricture: A Statistical Analysis. J. Urol. 2003 Sep.170(3):840–4. doi: 10.1097/01.ju.0000080842.99332.94. [DOI] [PubMed] [Google Scholar]
- 27.MacDonald MF, Al-Qudah HS, Santucci RA. Minimal impact urethroplasty allows same-day surgery in most patients. Urology. 2005 Oct.66(4):850–3. doi: 10.1016/j.urology.2005.04.057. [DOI] [PubMed] [Google Scholar]
- 28.Grossgold E, Tisdale B, Bayne C, Parrillo L, Tonkin J, McCammon K, et al. 5 OUTCOME OF DORSAL BUCCAL GRAFT AUGMENTED ANASTOMOSIS FOR URETHRAL STRICTURES AFTER A FAILED RECONSTRUCTION. JURO. 2011 Apr.185(S):e2. Elsevier Inc. [Google Scholar]
- 29.O'Riordan A, Narahari R, Kumar V, Pickard R. Outcome of dorsal buccal graft urethroplasty for recurrent bulbar urethral strictures. BJU Int. 2008 Nov.102(9):1148–51. doi: 10.1111/j.1464-410X.2008.07763.x. [DOI] [PubMed] [Google Scholar]
- 30.Jain D. Outcome of Dorsal Onlay Buccal Mucosa Substitution Urethroplasty in Long Strictures of Anterior Urethra. Jan. 2007. pp. 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rourke K. OUTCOMES AND COMPLICATIONS OF URETHRAL RECONSTRUCTION USING A DORSAL ONLAY AUGMENTED ANASTOMOSIS WITH BUCCAL MUCOSA: IS THIS THE EVOLVING GOLD STANDARD FOR TREATMENT OF THE LONG SEGMENT BULBAR URETHRAL STRICTURE? JURO. 2009 Apr.181(4):13–3. [Google Scholar]
- 32.Morey AF, Kizer WS. Proximal Bulbar Urethroplasty Via Extended Anastomotic Approach—What Are the Limits? J. Urol. 2006 Jun.175(6):2145–9. doi: 10.1016/S0022-5347(06)00259-X. [DOI] [PubMed] [Google Scholar]
- 33.DUBEY D, KUMAR A, Bansal P, SRIVASTAVA A, KAPOOR R, MANDHANI A, et al. Substitution urethroplasty for anterior urethral strictures: a critical appraisal of various techniques. BJU Int. 2003 Feb.91(3):215–8. doi: 10.1046/j.1464-410x.2003.03064.x. [DOI] [PubMed] [Google Scholar]
- 34.Lozano Ortega JL, Pertusa Peña C. Surgical treatment of urethral stenosis. Results of 100 urethroplasties. Arch. Esp. Urol. 2009 Mar.62(2):109–14. doi: 10.4321/s0004-06142009000200004. [DOI] [PubMed] [Google Scholar]
- 35.Guralnick ML, Webster GD. The augmented anastomotic urethroplasty: indications and outcome in 29 patients. J. Urol. 2001 May;165(5):1496–501. [PubMed] [Google Scholar]
- 36.Welk BK, Kodama RT. The Augmented Nontransected Anastomotic Urethroplasty for the Treatment of Bulbar Urethral Strictures. URL. 2012 Feb.:1–5. doi: 10.1016/j.urology.2011.12.008. Elsevier Inc. [DOI] [PubMed] [Google Scholar]
- 37.Anger JT, Sherman ND, Webster GD. The Effect of Bulbar Urethroplasty on Erectile Function. J. Urol. 2007 Sep.178(3):1009–11. doi: 10.1016/j.juro.2007.05.053. [DOI] [PubMed] [Google Scholar]
- 38.Seitz M, Liedl B, Becker A, Gratzke C, Reich O, Stief C. Upper transverse scrotal approach for muscle-and nerve-sparing urethral stricture repair. World J Urol. 2009 Mar.27(5):667–72. doi: 10.1007/s00345-009-0385-1. [DOI] [PubMed] [Google Scholar]
- 39.Meeks J, Erickson B. USE OF ABDOMINAL WALL SKIN FOR URETHROPLASTY IN MEN WITH EXTENSIVE STRICTURES AND PRIOR RECONSTRUCTION. The Journal of Urology. 2009 [Google Scholar]
- 40.Lumen N, Hoebeke P, Oosterlinck W. Ventral Longitudinal Stricturotomy and Transversal Closure: the Heineke-Mikulicz Principle in Urethroplasty. URL. 2010 Dec.76(6):1478–82. doi: 10.1016/j.urology.2010.06.051. Elsevier Inc. [DOI] [PubMed] [Google Scholar]
- 41.Ammani A, Abbar M, Dakkak Y, Janane A, Ameur A, Ghadouane M. UP-1.168: Voiding and Erectile Functions after Anastomotic Urethroplasty. URL. 2009 Oct.74(4):S223–3. [Google Scholar]
- 42.Kontopantelis E. metaan: Random-effects meta-analysis. Stata Journal. 2010 [Google Scholar]
- 43.Cai T, DasGupta A. JSTOR: Statistical Science. 2001 May;16(2):101–117. Statistical Science. 2001. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
List of excluded studies and reason for exclusion
PRISMA criteria checklist