Abstract
Objective
Weight changes may be an important indicator of an ongoing pathological process. Retrospective self-report might be the only possibility to capture prior weight. The objective of the study was to evaluate the accuracy of retrospective recall of body weight in old age and factors that might predict accuracy.
Design and Methods
In 2007, 646 participants (mean age, 71.6 years) of the Swedish Adoption/Twin Study of Aging (SATSA) answered questions about their present weight and how much they weighed 20-years ago. Of these, 436 had self-reported their weight twenty years earlier and among these 134 had also had their weight assessed at this time point.
Results
Twenty year retrospectively recalled weight underestimated the prior assessed weight by −1.89 ± 5.9 kg and underestimated prior self-reported weight by −0.55 ± 5.2 kg. Moreover, 82.4% of the sample were accurate within 10%, and 45.8% were accurate within 5% of their prior assessed weights; similarly, 84.2% and 58.0 % were accurate within 10% and 5% respectively, for prior self-reported weight. Current higher body mass index and preferences of reporting weights ending with zero or five was associated with an underestimation of prior weight, while greater weight change over 20 year, and low Mini-Mental State Scores (MMSE) (<25) led to an overestimation of prior weight.
Conclusions
Recalled weight comes close to the assessed population mean, but at the individual level there is a large variation. The accuracy is affected by current BMI, changes in weight, end-digit preferences, and current cognitive ability. Recalled weight should be used with caution.
Keywords: Accuracy, Aging, Body Mass Index, Self-report, Weight
Introduction
Weight is an important indicator of a person’s health status. It is well-known that excess weight in midlife is associated with various negative health outcomes (1). However, in late life the association between weight and health is less clear cut as excess weight may be associated with both negative and positive health outcomes (2–5). Most research has focused on current weight in relation to health outcomes in late life. But current weight does not tell the story of past weight. The negative effect of excess weight is proposed to be delayed (1). Moreover, being overweight or obese over a longer period of time is associated with more severe negative health outcomes (6), for example long-term excess weight has been associated with a higher risk of diabetes (6) and lower cognitive functioning in late life (7, 8). Additionally, weight change may be an indication of ongoing pathological processes. For example, weight decline is predictive of dementia (9) and mortality (10, 11), and weight fluctuations are predictive of functional disability and mortality (12). Hence, weight history and changes in weight may be important information to collect in order to appreciate the etiology underlying current weight and health associations, to reach correct diagnoses, and to provide health recommendations.
Both in clinical practice and in research, self-report might be the only possibility to capture prior weight information. The usefulness of using retrospectively recalled weight relies both on individuals’ willingness to recall and the accuracy of the recalled weight. In the Manitoba Follow-up Study about seventy-five percent of the male sample attempted to recall their past weight, and those who did not attempt to recall their past weight were older, had more limitations in instrumental activities of daily living (IADL), and were more often unmarried (13), To our knowledge, except for the Manitoba Follow-up Study no other study has evaluated self-selection effects on retrospectively recall weight. However, several studies have focused on recall accuracy in old age (13–18), and there seems to be a general tentative opinion that recalled weight can be used. But there are several important factors that have not been addressed in these studies or have only been addressed in a couple of studies. For example, two studies only included men (13, 18), which might overestimate the accuracy as women are more likely to underreport their weight, at least when current self-reported weight is used (19). Only one study took into account weight fluctuations and end-digit reporting preferences (13), i.e. when subjects report their weights as ending with “0” or “5”, and only one study took memory problems into account (17). Furthermore, studies differ in their definitions of accuracy, the follow-up times (1 to 65 years), the representativeness of the sample, and the age at recall (50 to 100 years). Several factors have been proposed to affect recall accuracy, such as age (14, 15, 17, 18), gender (14, 16), education (14, 17), race (14, 17), previous weight or body mass index (BMI) (13, 16), present weight or BMI (14, 18), and change in weight (13–15), although not consistently across studies.
By comparing prior assessed and self-reported weights to retrospectively recalled weight from the population-based longitudinal Swedish Adoption/Twin Study of Aging (SATSA), the current study evaluates the ability to recall, the accuracy of recall, and evaluates a variety of demographic and weight-related factors with methodological refinements that might affect the accuracy of 20-year retrospectively recalled weight.
Method
Participants and study design
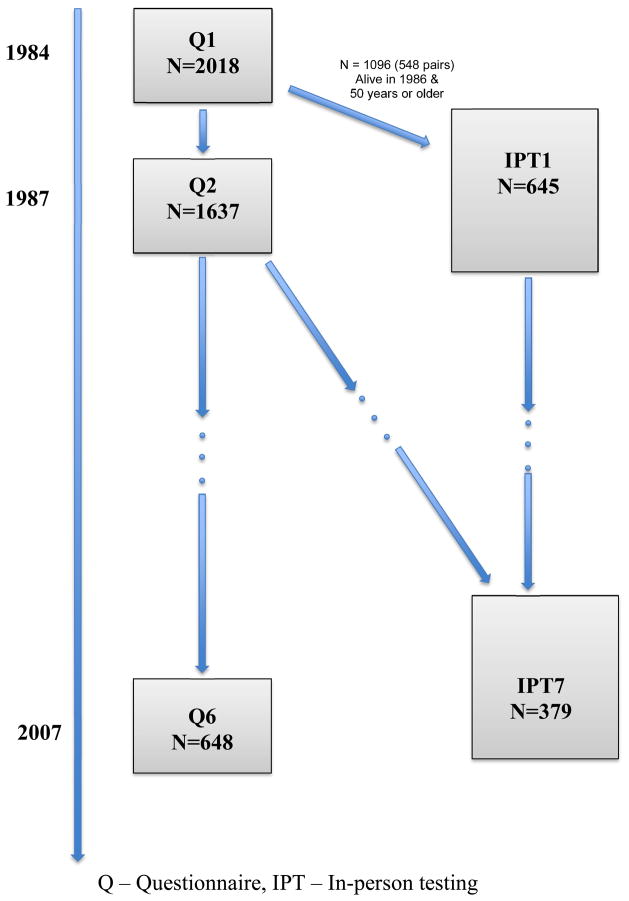
The participants in SATSA were drawn from the Swedish Twin Registry (20), and the sample and selection criteria have been described in detail previously (21). In brief, all twins who had been reared apart and a sample matched for birth-year, county of birth, and sex were invited to participate. These twins were first mailed a questionnaire (Q1) in 1984 and 2019 twins responded. Among those twin pairs where both twins responded to Q1, 548 pairs (1096 twins) aged 50 years and older were invited to participate in an in-person testing (IPT1) of health and cognitive functioning. At the first IPT in 1986, 645 twins participated. Since then, these twins and all twins that responded to Q1 and who turned 50 years of age since the last IPT were systemically interviewed and assessed every three years (except in 1995) by trained research nurses in a primary care facility close to their home. Alongside the IPTs, questionnaires (Q) containing questions about health, psychological and social factors have been sent regularly to the twins that participated in Q1. This study is based on the 648 persons responded to the questionnaire (Q6) in 2007 that contained questions about previous weight. Of these, 436 had self-reported their weight twenty years earlier (Q2), and among these, 134 had also had their weight assessed at IPT1 (figure 1).
Figure 1.
Flowchart of the data collection
Measures
In Q6, the participants were asked to estimate their weight twenty years ago. For those persons who reported a weight range the mean was used (19 respondents from Q2 (4.4%)) and 6 participants from IPT1 (4.4%)). Weight was self-reported in the questionnaire phase of SATSA and a trained research nurse assessed participants’ weights in clothing at IPT1. BMI was calculated as weight in kilograms divided by height in meters squared. BMI scores were calculated from both the assessed data (IPT1 and IPT7) and from the self-reported data (Q2 and Q6). Further, in line with previous research (13) accuracy of recall was defined by calculating the relative difference between recalled and assessed/self-reported weights ((Recalled Weight – Prior Weight)/Prior Weight * 100%). Relative weight differences within 10% were considered accurate and within 5% were considered very accurate. Further, persons who have lost and gained weight several times over the life span might be less able to remember their prior weight. Using the standard deviation (SD) function in SPSS (version 17) an individual standard deviation of the IPT weight (up to six possible) and Q weight (up to six possible) was calculated for each subject who had at least two assessments of weight across the study. This measure was calculated both from the assessed and self-reported weight. As persons with fewer points in any analyses are more likely to have bigger SD’s on average, the number of occasions was added as covariate in the analyses. The difference between the current (Q6 and IPT7) and prior assessment (Q2 and IPT1) of weight was calculated for the self-reported and assessed measures, respectively, where positive numbers indicate weight gain. Level of education was self-reported and coded as six years of education and less, or seven years and more. A Mini-Mental State Examination (MMSE) was performed at IPT7 The MMSE score was dichotomized at 24, 24 or lower (impaired) = 1 and above 24 (intact) = 0, and used as an indication of cognitive impairment.
Statistical analyses
Persons attempting to recall their weight 20 years ago were compared with those who did not attempt to recall their weight using t- and χ2-tests when appropriate. Bland-Altman plots were used to illustrate and examine agreement between recalled and prior assessed weight, twenty years ago (22). The difference between recalled and prior assessed weight was plotted against the mean of the two values. Limits of agreement were calculated as the mean difference plus two standard deviations. Linear regression was used to evaluate characteristics that might affect the accuracy of recalled weight, which was calculated as the recalled weight minus the prior assessed or self-reported weight twenty years ago. The covariates were entered in three steps. In the first step age, sex, education, and present BMI were entered. Present BMI was chosen before prior BMI based on the assumption that researchers that might want to use and control for potential influences do not have access to prior BMI; hence, then they would not need to use recalled weight. In the second step, fluctuations in weight were entered, how many times weight was assessed or self-reported, end-digit preferences, and change in weight between last and first self-report of weight. Additionally, MMSE scores were dichotomized at 24, and entered in the final step. Higher MMSE (>24) score were the reference. For the analyses evaluating the difference between recalled and prior assessed weight, all weight related covariates were assessed and for the analyses assessing the difference between recalled and prior self-reported weight all weight related covariates were self-reported. As MMSE scores were not available for those who only participated in the questionnaire phase, the influence of cognitive function was not possible to analyze for these persons.
To detect potential collinearity, that is especially likely to occur among the weight related measures, we examined the correlations between the weight measures with Pearson’s correlation coefficients. All analyses mentioned above were performed with SPSS 17.0.(23)
Results
Characteristics of the total sample, and persons who attempted to recall their weight (n=518, 79.9% of the sample) were compared to those who did not attempt to recall their past weight (n=130, 20.1% of the sample) (table 1). Persons who attempted to recall their weight were younger, more likely to be men, and had a lower current self-reported BMI. There were no significant differences in level of education, self-rated health, or MMSE scores among those who tried to recall their weight and those who did not.
Table 1.
Sample Characteristics, Total Sample and by Recalled or Non-recalled Weight
| Total | Recalled Weight | Non-recalled Weight | P-Value | |
|---|---|---|---|---|
|
| ||||
| n= 648 | n = 518 | n = 130 | ||
| Age, mean (SD) | 71.6 (10.4) | 70.9 (10.2) | 74.2 (10.6) | .002 |
| Men, n (%) | 253 (39.0) | 217 (41.9) | 36 (27.7) | .003 |
| High education, n (%) | 301 (46.4) | 248 (47.9) | 53 (40.8) | .186 |
| Assessed BMIbaseline, mean (SD) | 25.2 (3.1) | 25.1 (3.6) | 25.6 (3.9) | .490 |
| Self-reported BMIbaseline, mean (SD) | 24.2 (3.1) | 24.1 (3.1) | 24.7 (3.2) | .054 |
| Assessed BMIfollow-up, mean (SD) | 26.7 (3.7) | 26.6 (4.0) | 27.1 (4.3) | .442 |
| Self-reported BMIfollow-up, mean (SD) | 25.8 (3.9) | 25.6 (3.9) | 26.8 (3.5) | .004 |
| Low MMSE, n (%) | 32 (4.9) | 24 (4.6) | 8 (6.1) | .392 |
Note. Assessed Baseline = IPT1; Self-Reported Baseline = Q2; Assessed Follow-up = IPT7; Self-Reported Follow-up = Q6.
Accuracy of recalled weight and factors affecting the recalled weight
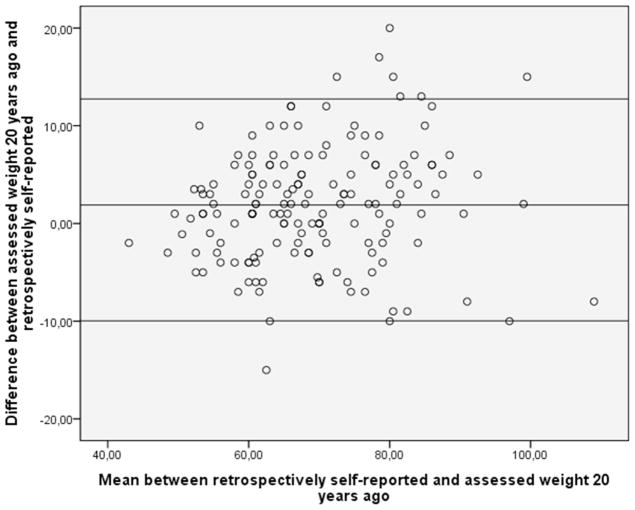
The difference scores between recalled and prior weight ranged from −20 to 20 kg for assessed weight and −23 to 16 kg for self-reported weight. Recalled weight was highly correlated with both prior assessed and self-report weight twenty years ago, r = 0.88 and 0.91, respectively. Persons underestimated their 20-year prior assessed weight by −1.89 by −1.89 ± 5.9 kg and persons underestimated their 20-year prior self-reported weight by −0.55 ± 5.5 kg. This is illustrated with Bland-Altman plots in figure 2. Further, 82.4% of the sample were accurate within 10%, and 45.8% were accurate within 5% of their measured weights, and the comparable accuracies were 84.2% and 58.0%, respectively, for self-reported weight.
Figure 2.
Accuracy of self-reported weight (difference between assessed weight twenty years ago and retrospectively self-reported). Each dot represents one individual.
Linear regression analyses showed that persons with higher current BMI tended to underestimate their prior assessed weight (table 2). Persons who gained weight over the past 20 years overestimated their previous weight (table 2). Among those who had their weight assessed 20 years prior the recall (in IPT1), 45% reported their prior weight ending with a zero or a five and the corresponding percentage for those who participated in the questionnaire phase only was 46%. Those applying an end-digit preference tended to underestimate the prior self-reported weight, but not the prior assessed weight. Persons with lower MMSE scores overestimated the previous weight (table 2). All these analyses were first run using the assessed weight measures and secondly with the self-reported measures, except for the third step that was only run for those with assessed data, as MMSE scores were not available for those that only participated in the questionnaire phase. As can be noticed in table 2, results are in the same direction using either the assessed or the self-reported measures of BMI, although significance levels vary due to sample size.
Table 2.
Linear regression of differences between assessed or self-reported weight about twenty years earlier and recalled weight.a
| Recalled weight vs Assessed n=134 unadjusted R2 =.171 | Recalled weight vs Self-Report n=436 unadjusted R2 =.117 | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Beta | SE | P | Beta | SE | P | |
| Age | .085 | .090 | .344 | .023 | .028 | .404 |
| Education | −.042 | 1.019 | .967 | .114 | .485 | .815 |
| Sex | 1.162 | 1.011 | .253 | −.280 | .497 | .574 |
| BMIfollow-up | −.413 | .144 | .005 | −.362 | .085 | <.001 |
| Weight fluctuationb | .063 | .315 | .841 | .205 | .127 | .109 |
| End-digit preferences | −1.125 | .650 | .086 | −.654 | .321 | .042 |
| Change in weightc | .336 | .087 | <.001 | .267 | .043 | <.001 |
| MMSE >24 ref. | 2.945 | 1.461 | 0.046 | -- | -- | -- |
Analyses controlled for number of times a person participated in the in-person testing.
Weight fluctuation refers to standard deviation of longitudinally assessed weight, for the recalled versus assessed weight this is based on assessed weight information, but for the difference between recalled and self-reported this is based on the self-reported weights.
Change in self-reported weight from baseline to follow-up.
Mini-Mental State Examination, dichotomized at 24. MMSE scores were not available for those that only participated in the questionnaire phase.
We evaluated the correlations among weight-related predictors to consider the impact to the linear regression analyses reported above. Weight related measures were moderately to strongly correlated amongst one another although correlations with end-digit preference were small. Specifically, for the assessed measures, higher current BMI was significantly correlated with greater change in BMI, r = 0.377, p < .001. Current BMI did not correlate significantly with fluctuations in BMI r = 0.125, p = .156, or end-digit preferences, r = 0.145, p = .098. For the self-reported measures, higher current BMI was associated with greater change in BMI r = 0.540, p < .001, greater fluctuations in BMI r = 0.463, p < .001, and end-digit preferences, r = 0.160, p = .001. Furthermore, greater fluctuations in BMI correlated significantly with end-digit preferences, r = 0.143, p = .002, and with greater change in weight r = 0.347, p < .001.
Discussion
This study shows that 20-year recalled weight yields high accuracy at the mean level. The deviance from the true mean value of barely two kilos is comparable to the deviance between assessed and self-reported weight measured at the same time point (19, 24–27), for example, in SATSA the deviance ranged from 0.5 to 1.7 (19). But, it should be noted that the standard deviation of 5.9 for recalled weight is bigger than the standard deviation of between 2.7 and 3.4 that has been reported from SATSA when self-reported weight is compared to weight at the same time point (19). However, the standard deviation for recalled weight may be larger as the sample is relatively small, or increased due to end-digit rounding. In addition, about four out of five reported their weight with accuracy (within 10% of the assessed weight) and a little less then half of the sample were very accurate (within 5% of the assessed weight). Compared with the Manitoba Follow-up Study the accuracy in the SATSA study is high (13).
Although the retrospectively recalled weight yielded high accuracy on the mean level, it should be remembered that one out of five elderly persons that participated in the study did not attempt to recall their weight twenty years ago. This rate is slightly better than the Manitoba Follow-up Study where one in four did not attempt to recall their previous weight (13). The elderly persons who did not attempt to recall their previous weight were older and had a higher BMI at the time of recall, and were more likely to be women. Older persons might be less motivated to fill out questionnaires or less able to recall due to memory problems. Additionally, both for women and for persons with higher weight we speculate that questions about weight might be more sensitive than for men (28) and persons of normal weight. Hence, these persons might be less willing to report. On the other hand, there was no difference between men and women in recall accuracy among those who attempted to recall their weight.
Overall, the factors that are related to weight had the greatest impact on the recall bias. From studies on the accuracy of current self-reported weight it is well-known that persons with higher BMI scores tend to underreport their weight (27, 29–32). In this study we additionally show that persons with higher BMI scores at the time of recall tended to underestimate what they weighed 20 years age to a larger extent than persons with lower BMI. The importance of prior or current BMI on accuracy of recalled weight has been shown in several studies (14–18). In addition, greater weight change over twenty years predicted recall accuracy, as in several other studies (13–15). Persons who had gained more weight tended to overestimate their previous weight. It could be hypothesized that persons who have gained weight overestimate their recalled weight as a defense mechanism, to reduce the total amount of gained weight. We were not able to replicate the finding from the Manitoba Follow-up Study that weight fluctuations predict recall accuracy. It could be hypothesized that this difference is due to different assessment methods of weight fluctuations: whereas we used the standard deviation function to calculate person-specific estimates of fluctuation and controlled for the number of times a person had participated, in the Manitoba Follow-up Study weight fluctuations were scored based on a 0.5–1.0% difference in weight between the assessments. However, we think it is likely that the non-significant association in the present study is due to shared variance with weight change.
It should be noted that the difference between the recalled weight and the prior self-reported weight was smaller than the deviance between the recalled weight and the prior assessed weight, and the standard deviation was smaller. Hence, perceptions of weight seem to remain stable over time. The same factors were associated with recall accuracy in the comparisons between recalled weight and assessed weight as between recalled weight and self-reported weight.
Almost half of the sample reported their recalled weight to end with “0” or “5”. As in the Manitoba follow-up study (13) end-digit preference predicted recall accuracy, especially for the prior self-reported weight. Specifically, end-digit preferences led to an underestimation of previous weight. Given the large number of persons using zero or five in the end, end-digit preference needs to be taken into account when recalled weight is used. Studies including more participants should evaluate whether the bias attributed to end-digit preferences can be adjusted for statistically by considering information from those participants who do not show such a bias.
We also found that lower performance on the MMSE was associated with overestimation of the prior assessed weight. A low MMSE score is an indication of low cognitive function and in many cases a sign of preclinical dementia (33). Hence, it is not surprising that the MMSE score may be of importance for recall accuracy.
The strength of this study is the long follow-up time, access to both self-reported and assessed weight measurements, and relevant covariates. The longitudinal design of SATSA might skew results, as individuals continuously seeing a health professional might provide more accurate information about body measures. However, the regression models were controlled for participation rate in the study. Another limitation is that the measured weight was assessed over a two-year span, i.e. some persons had their weight assessed 21 years ago and some 19 years ago. On the other hand, we might underreport the reliability of recalled weight. In SATSA, the participants’ weight was assessed in clothes, but we believe that most people tend to report their morning weight without clothes. Adding about 1 kg to the recalled self-reported weight would remove half of the average difference between recalled and measured weight.
In conclusion, recalled weight comes close to the assessed population mean, but at the individual level there is a large variation and a substantial number of people do not answer the question about previous weight. Furthermore, the accuracy is especially affected by weight related measures and a preference to report weights ending with zero or five. Retrospectively recalled weight should be used with caution.
Acknowledgments
This study is supported by National Institute of Aging (AG04563, AG10175, AG08724), The MacArthur Foundation Research Network on Successful Aging, the Swedish Council for Working Life and Social Research (FAS) (97:0147:1B, 2009-0795, postdoc grant 2010-0704, FLARE postdoc grant 2010-1852), and Swedish Research Council (825-2007-7460, 825-2009-6141).
Footnotes
Conflict of Interest
Anna K. Dahl and Chandra A. Reynolds report no disclosure.
References
- 1.Kopelman PG. Obesity as a medical problem. Nature. 2000;404:635–43. doi: 10.1038/35007508. [DOI] [PubMed] [Google Scholar]
- 2.Stenholm S, Koster A, Alley DE, et al. Joint association of obesity and metabolic syndrome with incident mobility limitation in older men and women--results from the Health, Aging, and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2010;65:84–92. doi: 10.1093/gerona/glp150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luchsinger JA, Patel B, Tang M-X, Schupf N, Mayeux R. Measures of adiposity and dementia risk in the elderly. Arch Neurol. 2007;64:392–8. doi: 10.1001/archneur.64.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dahl A, Lopponen M, Isoaho R, Berg S, Kivela SL. Overweight and obesity in old age are not associated with greater dementia risk. J Am Geriatr Soc. 2008;56:2261–6. doi: 10.1111/j.1532-5415.2008.01958.x. [DOI] [PubMed] [Google Scholar]
- 5.Kulminski AM, Arbeev KG, Kulminskaya IV, et al. Body mass index and nine-year mortality in disabled and nondisabled older U.S. individuals. J Am Geriatr Soc. 2008;56:105–10. doi: 10.1111/j.1532-5415.2007.01494.x. [DOI] [PubMed] [Google Scholar]
- 6.Jeffreys M, Lawlor DA, Galobardes B, et al. Lifecourse weight patterns and adult-onset diabetes: the Glasgow Alumni and British Women’s Heart and Health studies. Int J Obes. 2005;30:507–12. doi: 10.1038/sj.ijo.0803161. [DOI] [PubMed] [Google Scholar]
- 7.Dahl AK, Hassing LB, Fransson EI, Gatz M, Reynolds CA, Pedersen NL. Body Mass Index Across Midlife and Cognitive Change in Late Life. Int J Obes. doi: 10.1038/ijo.2012.37. Epub a head of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sabia S, Kivimaki M, Shipley MJ, Marmot MG, Singh-Manoux A. Body mass index over the adult life course and cognition in late midlife: the Whitehall II Cohort Study. Am J Clin Nutr. 2009;89:601–7. doi: 10.3945/ajcn.2008.26482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gao S, Nguyen JT, Hendrie HC, et al. Accelerated weight loss and incident dementia in an elderly African-American cohort. J Am Geriatr Soc. 2011;59:18–25. doi: 10.1111/j.1532-5415.2010.03169.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee CG, Boyko EJ, Nielson CM, et al. Mortality risk in older men associated with changes in weight, lean mass, and fat mass. J Am Geriatr Soc. 2011;59:233–40. doi: 10.1111/j.1532-5415.2010.03245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Somes GW, Kritchevsky SB, Shorr RI, Pahor M, Applegate WB. Body Mass Index, Weight Change, and Death in Older Adults. Am J Epidemiol. 2002;156:132–8. doi: 10.1093/aje/kwf019. [DOI] [PubMed] [Google Scholar]
- 12.Arnold AM, Newman AB, Cushman M, Ding J, Kritchevsky S. Body weight dynamics and their association with physical function and mortality in older adults: the Cardiovascular Health Study. J Gerontol A Biol Sci Med Sci. 2010;65:63–70. doi: 10.1093/gerona/glp050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bayomi DJ, Tate RB. Ability and accuracy of long-term weight recall by elderly males: the Manitoba follow-up study. Ann Epidemiol. 2008;18:36–42. doi: 10.1016/j.annepidem.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 14.Perry GS, Byers TE, Mokdad AH, Serdula MK, Williamson DF. The validity of self-reports of past body weights by U.S. adults. Epidemiol. 1995;6:61–6. doi: 10.1097/00001648-199501000-00012. [DOI] [PubMed] [Google Scholar]
- 15.de Fine Olivarius N, Andreasen AH, Loken J. Accuracy of 1-, 5- and 10-year body weight recall given in a standard questionnaire. Int J Obes. 1997;21:67–71. doi: 10.1038/sj.ijo.0800365. [DOI] [PubMed] [Google Scholar]
- 16.Must A, Willett WC, Dietz WH. Remote recall of childhood height, weight, and body build by elderly subjects. Am J Epidemiol. 1993;138:56–64. doi: 10.1093/oxfordjournals.aje.a116777. [DOI] [PubMed] [Google Scholar]
- 17.Stevens J, Keil JE, Waid LR, Gazes PC. Accuracy of current, 4-year, and 28-year self-reported body weight in an elderly population. Am J Epidemiol. 1990;132:1156–63. doi: 10.1093/oxfordjournals.aje.a115758. [DOI] [PubMed] [Google Scholar]
- 18.Tamakoshi K, Yatsuya H, Kondo T, et al. The accuracy of long-term recall of past body weight in Japanese adult men. Int J Obes Relat Metab Disord. 2003;27:247–52. doi: 10.1038/sj.ijo.802195. [DOI] [PubMed] [Google Scholar]
- 19.Dahl AK, Hassing LB, Fransson EI, Pedersen NL. Agreement between self-reported and measured height, weight and body mass index in old age-a longitudinal study with 20 years of follow-up. Age Ageing. 2010;39:445–51. doi: 10.1093/ageing/afq038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lichtenstein P, deFaire U, Floderus B, Svartengren M, Svedberg P, Pedersen NL. The Swedish Twin Registry: A unique resource for clinical, epidemiological and genetic studies. J Intern Med. 2002;252:184–205. doi: 10.1046/j.1365-2796.2002.01032.x. [DOI] [PubMed] [Google Scholar]
- 21.Finkel D, Pedersen N. Processing speed and longitudinal trajectories of change for cognitive abilities: the Swedish adoption/twin study of aging. Aging, Neurpsych Cogn. 2004;11:325–45. [Google Scholar]
- 22.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurements. Lancet. 1986;1:307–10. [PubMed] [Google Scholar]
- 23.SPSS. SPSS Advanced models. Vol. 2007. SPSS; Chicago: 2007. [Google Scholar]
- 24.Lawlor DA, Bedford C, Taylor M, Ebrahim S. Agreement between measured and self-reported weight in older women. Results from the British Women’s Heart and Health Study. Age Ageing. 2002;31:169–74. doi: 10.1093/ageing/31.3.169. [DOI] [PubMed] [Google Scholar]
- 25.Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Diet Assoc. 2001;101:28–34. doi: 10.1016/S0002-8223(01)00008-6. quiz 5–6. [DOI] [PubMed] [Google Scholar]
- 26.Hill A, Roberts J. Body mass index: a comparison between self-reported and measured height and weight. J Public Health Med. 1998;20:206–10. doi: 10.1093/oxfordjournals.pubmed.a024744. [DOI] [PubMed] [Google Scholar]
- 27.Rowland ML. Self-reported weight and height. Am J Clin Nutr. 1990;52:1125–33. doi: 10.1093/ajcn/52.6.1125. [DOI] [PubMed] [Google Scholar]
- 28.Pliner P, Chaiken S, Flett GL. Gender Differences in Concern with Body Weight and Physical Appearance Over the Life Span. Personality and Social Psychology Bulletin. 1990;16:263–73. [Google Scholar]
- 29.Bostrom G, Diderichsen F. Socioeconomic differentials in misclassification of height, weight and body mass index based on questionnaire data. Int J Epidemiol. 1997;26:860–6. doi: 10.1093/ije/26.4.860. [DOI] [PubMed] [Google Scholar]
- 30.Faeh D, Marques-Vidal P, Chiolero A, Bopp M. Obesity in Switzerland: do estimates depend on how body mass index has been assessed? Swiss Med Wkly. 2008;138:204–10. doi: 10.4414/smw.2008.12065. [DOI] [PubMed] [Google Scholar]
- 31.Gunnell D, Berney L, Holland P, et al. How accurately are height, weight and leg length reported by the elderly, and how closely are they related to measurements recorded in childhood? Int J Epidemiol. 2000;29:456–64. [PubMed] [Google Scholar]
- 32.Payette H, Kergoat MJ, Shatenstein B, Boutier V, Nadon S. Validity of self-reported height and weight estimates in cognitively-intact and impaired elderly individuals. J Nutr Health Aging. 2000;4:223–8. [PubMed] [Google Scholar]
- 33.Dahl A, Berg S, Nilsson S. Dementia identification in epidemiological research: a study on the usefulness of different data sources. Aging Clin Exp Res. 2007;19:381–9. doi: 10.1007/BF03324718. [DOI] [PubMed] [Google Scholar]