Abstract
Tremendous progress has been made in recent years to generate retinal cells from pluripotent cell sources. These advances provide hope for those suffering from blindness due to lost retinal cells. Understanding the intrinsic genetic network in model organisms, like fly and frog, has led to a better understanding of the extrinsic signaling pathways necessary for retinal progenitor cell formation in mouse and human cell cultures. This review focuses on the culture methods used by different groups, which has culminated in the generation of laminated retinal tissue from both embryonic and induced pluripotent cells. The review also briefly describes advances made in transplantation studies using donor retinal progenitor and cultured retinal cells.
Keywords: Embryonic Stem Cells, ES; Induced Pluripotent Stem Cells, iPS; Genetic Network; Stromal Cells; Noggin; Signaling Pathways; Cone Photoreceptors; Ganglion Cells; Retina; Eye; Artificial Retina
EMBRYONIC DEVELOPMENT OF RETINAL PROGENITORS
New research on stem cells provides hope for those suffering from vision loss due to degenerating or damaged retinal cells. In order to generate a large population of cells for vision repair, we first need to understand how these cells are formed in the developing embryo. Once we understand the extrinsic and intrinsic events involved, the conditions can be recreated in culture. These cells can also be employed to model degenerative diseases and to tailor treatment for patients before they lose vision.
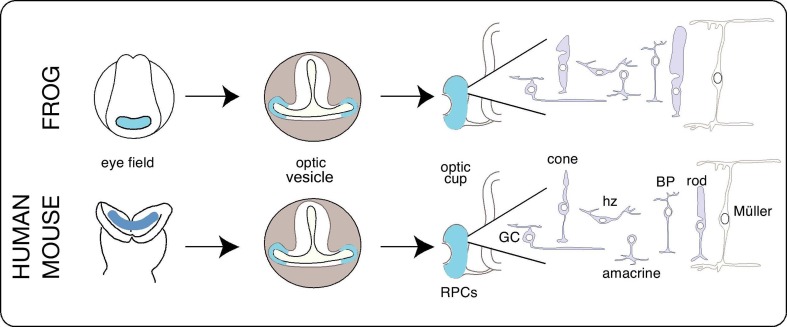
In order to elucidate the parameters needed to generate retinal cells in culture, we need to first understand how the embryonic eye develops. The eye primordia, or the eye field, takes shape just posterior to the neural ridge in humans, mice and amphibians (Fig. 1, blue area).1,2 This region contains proliferating cells that evaginate laterally from the diencephalon. The budding tissue grows until it reaches the
Figure 1.
Schematic of eye development in frog, mouse and human; the eye develops from cells in the anterior neural plate and is drawn in blue throughout all stages of development. The optic vesicle schematic is a cross-section of the embryo, showing the eye bud. Retinal progenitor cells (RPCs) are found in the optic cup after evagination. The retinal cells are born in order shown from left to right. GC, ganglion cell; hz, horizontal cell; BP, bipolar cell; Müller, müller glia
overlying ectoderm, whereupon it invaginates, giving rise to both the light-sensing neural retina and the light-absorbing retinal pigmented epithelium (RPE). These early eye field cells have interchangeably been called, “retinal progenitor cells” and “retinal stem cells”. Stem cells have classically been defined as cells that can generate new stem cells, as well as a variety of differentiated cell types; progenitor cells are more restricted, generating a minimal population of new progenitor cells and forming only a restricted set of cell types.3 Therefore, in this review, we will refer to the cells in the developing eye field, as retinal progenitor cells. In adult chicken, fish and amphibian eyes, proliferating cells are located in the periphery of the retina in a region called the ciliary marginal zone (CMZ). As these animals grow, the CMZ cells contribute to retinal tissue growth, adding newly differentiated cells.4 We will refer to these as retinal stem cells, as they continually generate copies of themselves while contributing differentiated cells to retinal growth.
The search for retinal stem cells in the mammalian retina led to the finding of quiescent ciliary epithelial cells in both adult murine and human retinas. When cultured, these cells could be clonally expanded and formed neurospheres.5,6 While these cells were highly celebrated upon their discovery, closer examination has revealed that they maintain characteristics of their pigmented cellular origins when they are cultured. In fact, when meticulously examined by electron microscope analysis, each cell within a given neurosphere maintains ciliary epithelial morphology and its characteristic pigmentation. Furthermore, these ciliary epithelial cells fail to fully differentiate into retinal cells and express retinal markers, either in culture or when transplanted into the permissive newborn subretinal space.7 The evidence suggests that ciliary epithelial cells can proliferate in culture under certain circumstances, yet the conditions to transdifferentiate them into retinal cells remain unknown. Although initially an attractive hypothesis, this further suggests that the CMZ, and its potential source of stem cells, appear to have been lost in mammals. On the other hand, understanding the mechanism used by lower vertebrates to maintain this retinal stem cell population may give us clues towards understanding how to recover this potential sight saving process in humans.8
Another potential source of retinal cells for retinal repair could be the RPE which forms a monolayer of cuboidal, pigmented cells behind the retina. In amphibians, fish and embryonic birds, removing the retina activates a repair mechanism that stimulates the RPE to regenerate an entirely new retinal tissue.9,10 During this process, the newly formed neuroepithelium loses pigmentation and begins to proliferate and differentiate into a tri-layered retina. This process does not occur in higher vertebrates. However, if RPE cells are removed from a human retina and are allowed to grow in culture, a subset of these cells will proliferate. When differentiated, these cells generate new RPE or mesenchymal cells.11 The conditions to transdifferentiate these cells into retinal cells has not been discovered, nevertheless, generating RPE cells from pluripotent human embryonic stem cells has already been demonstrated.12-14 Slightly modified conditions are required to generate retinal progenitors from pluripotent stem cells.
GENETIC NETWORK REGULATING RETINA FORMATION
The genetic network that drives retinal specification was originally discovered in fly when the genes required for eye specification were shown to be expressed at the same time and place for eyes to form.15 These genes are part of the Retinal Determination Gene Network (RDGN)16 and regulate each other’s expression. Surprisingly, similar to the fly eye, we discovered a vertebrate eye specification network regulated by the eye field transcription factors (EFTFs). The EFTFs include Pax6, Rax/Rx, Tbx3, Six6, Six3, Nr2e1/Tlx, and the anterior neuroectoderm specification factor, Otx2. When overexpressed during early development, these gene products drove ectopic Lhx2 expression and generated ectopic eyes outside the neural plate.17 Generating functional retinal tissue required only these seven EFTFs. Pluripotent primitive ectoderm cells from Xenopus embryos were transformed into functional retinal tissue by either overexpressing EFTFs or treating the cells with high concentrations of Noggin protein. The transplanted cells replaced endogenous eye field tissue in both structure and function.18 Similar observations were made by another group, in which they revealed that low Noggin concentrations yielded brain tissue, while high concentrations exclusively made retina.19 Noggin is a bone morphogenetic protein (BMP) antagonist. Repression of BMP signaling, along with Wnt signal repression, is required for neural versus epidermal cell fate.20 Recently, Bayramov has represented that the more potent, Noggin2, can inhibit BMP, Activin/Nodal and Wnt signaling in the anterior neural plate to affect forebrain specification during late gastrulation.21 It is unclear whether or not the generation of functional eye tissue uses a similar mechanism.
When performing our transplantation studies, we also noticed that dosage could affect the efficiency with which the transplanted eye tissue was generated. Each EFTF had to be injected at the optimal concentration in order to provide the maximal number of host animals with EFTF-induced retinal cells. Mice with null mutations in EFTF genes may unveil which EFTF are needed at higher versus lower concentrations. For example, in double mutants, loss of Otx1 (null mutant) and lower levels of Otx2 (+/-) can be rescued by adding back one copy of either Otx1 or Otx2.22 When comparing Pax6 mutant phenotypes, a correlation was found between Pax6 activity level and eye formation; mice with Pax6 activity level of 50% have small eyes while those with no Pax6 have no eyes.23Six3 heterozygotes have defects in just forebrain development while Six3-null littermates, lack entire forebrain and eyes. Decreasing levels of Six3 expression coincided with a gradual increase in Wnt1 transcript induction, a crucial signal that needs to be repressed during normal eye formation.24 Interestingly, Rax/Rx1, Lhx2 and Six6 heterozygous mice develop normal looking eyes while null mutants have eye defects, suggesting that the transcript levels produced by one allele for these genes is sufficient for normal eye development.25-27
Future work could unravel a new genetic network that describes both the genetic interactions and thresholds necessary for each regulatory event. This could lead to better understanding of how retinal progenitor cells are derived from pluripotent cells.
GENERATION OF RETINAL PROGENITOR CELLS
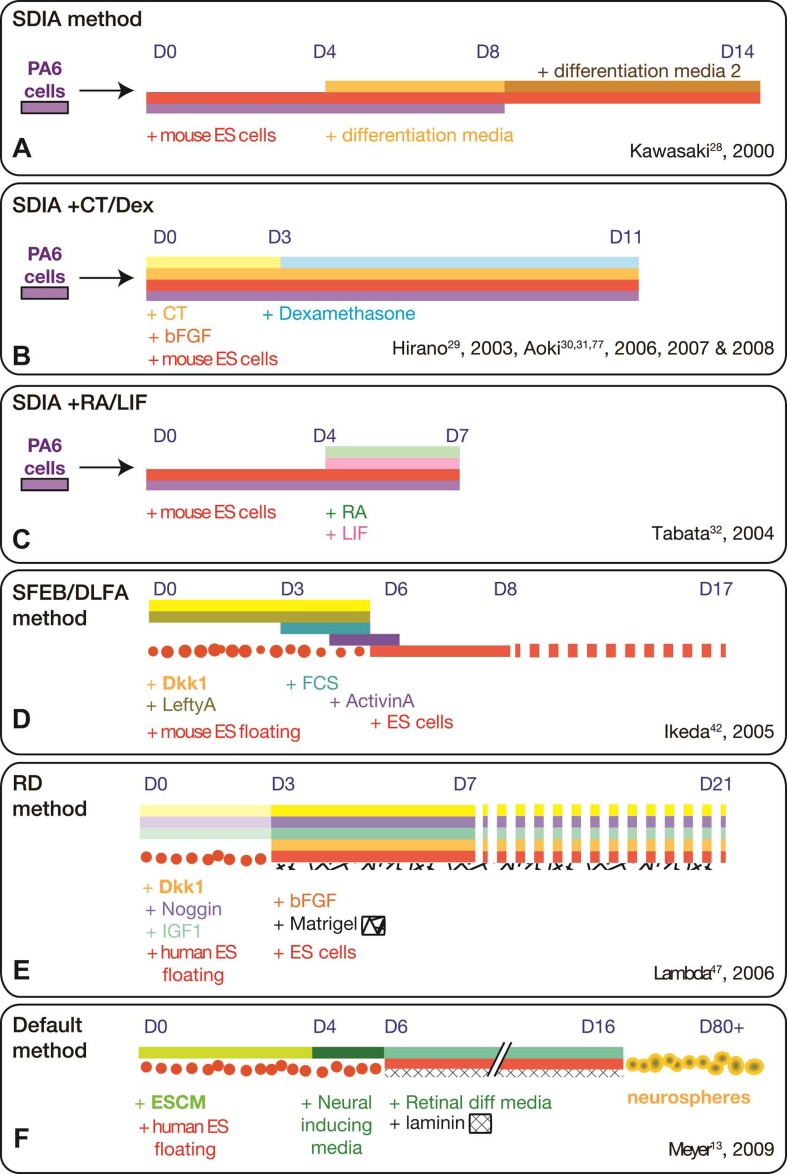
Investigators who studied early embryonic development in Xenopus knew the importance of BMP repression for neural cell formation and were eager to test mouse embryonic stem (ES) cells with this protocol. Unexpectedly, attempts to directly repress BMP signaling by adding Chordin, Follistatin, or a dominant negative BMP receptor to mouse ES cells, failed to even generate TuJ-positive neural cells. A more successful approach for inducing neurons in ES cell cultures was applying the stromal cell- derived inducing activity (SDIA) method, a term coined by the Sasai lab (Fig. 2A).28 In this method, bone-marrow derived stromal cell line, PA6, provide unknown factors to the ES cells co- cultured over them. A variation of this protocol (co-culturing mouse ES cells with stromal cells and then treating with basic fibroblast growth factor (bFGF), dexamethasone, and cholera toxin) led the cells to adopt the characteristic morphology of RPE and express markers for retina and lens cells (Fig. 2B). These markers were not induced in ES cultures derived from Pax6 null-mutant mice with anophthalmia.29 When transplanted into a chick embryonic eye, these cells formed RPE-like monolayers, and expressed a marker for early-born retinal ganglion cells (TuJ-1).30 Co-culturing with adult mouse retinal explants in which ganglion cells were chemically damaged, the ES-derived cells migrated across all layers, settled in the ganglion cell layer, and expressed markers for retinal ganglion cells.31 By combining the stromal cell culture method with retinoic acid (RA) treatment and Rx/Rax overexpression, the treated ES cells migrated into retinal explants and convincingly expressed markers for horizontal cells (Fig. 2C).32
Figure 2.
Ilustration summarizing the cell culture methods used to generate retinal cells from embryonic stem cell cultures; the method name is in the upper left hand corner. Days in culture are indicated above the bars. Each culture ingredient is indicated by the same color words above or underneath the bars. Adherent cultures are solid bars while floating cultures are dots. CT, cholera toxin; RA, retinoic acid; LIF, leukemia inhibitory factor; FCS, fetal calf serum; DKK-1, Dickkopf WNT signaling pathway inhibitor 1; IGF-1, insulin-like growth factor 1; bFGF, basic fibroblast growth factor; ESCM, embryonic stem cell media; Retinal diff media, retinal differentiation media
Nevertheless, the SDIA method had its limitations. While lens could also be formed in both mouse and non-human primate cell cultures,33,34 it was discovered that the SDIA method preferentially induced midbrain dopaminergic neurons and only a low level of markers for telencephalic neurons.35 An alternative, serum-free culture method was discovered to give rise to neural precursors in over half of the cultured mouse ES cells. The cells carried a transgene for the promoter of the early neural marker, Sox1, driving green fluorescent protein (GFP) expression. Fluorescent neural precursors could be fluorescence activated cell for FAC (FAC sorted) for higher purity and then studied.36 While screening for genes induced in Sox1-positive cells, a Wnt antagonist, i.e. secreted frizzled-related protein-2 (SFRP2), was uncovered.37
Nodal signaling was also found to repress neural differentiation of mouse ES cells while Nodal antagonists promoted neuroectoderm formation in human ES cells.38,39 Years before, it was discovered that an inducer of head formation, Cerberus, repressed three signaling pathways in early head formation: Wnt, BMP and Nodal.40 Yet, by repressing just Wnt and Nodal signaling in culture, telencephalic precursors were generated from mouse ES cells.41 Further adaptation and refinement of this protocol in mouse ES cultures led to the generation of retinal progenitors that were Rx and Pax6 positive (Fig. 2D).42
The physical environment of the culture was also determined to play a role. When ES cells were forced to come in close contact and form embryoid bodies (EBs), greater than half the cultures expressed cortical cell markers. The EBs launched the process by forming hollow spheres, then the spheres collapsed on themselves and formed neural rosettes by the end of the week.20
The pinnacle of success has been the recent generation of an entire optic cup in culture. By adding matrigel or pure extracellular matrix proteins, laminin and entactin, with Nodal and over the course of a week, optic cup structures were formed from the walls of the EB cultures. Remarkably, the optic cup could evaginate and invaginate on its own, without the benefit of the overlying lens, surface ectoderm and surrounding mesenchyme. The invaginated optic cup formed not only expressed markers for both RPE and neural retina but also the tri-layered structure characteristic of this tissue.43 This remarkable advance could lead the way to understanding early steps in mammalian eye formation that were difficult to determine since the eyes develop in utero.
MOUSE VERSUS HUMAN EMBRYONIC STEM CELL CULTURES
Mouse and human ES cells are derived from the blastula at slightly different stages of embryonic development.44 Whereas mouse ES cells proliferate in the presence of leukemia inhibitory factor (LIF) and are derived from the inner cell mass of the blastula, human ES cells proliferate in media containing Activin/ Nodal and bFGF, and seem to arise from a slightly later cell fate, the epiblast.45 Therefore, it is not surprising that slightly different conditions were necessary for generating retinal progenitor cells from human and mouse cells. For example, mouse ES cells were unresponsive to the neuralizing effects of BMP antagonists (as stated above), yet human ES cells briefly treated with Noggin, and then continually cultured in epidermal growth factor (EGF) and bFGF, produced neural cells within 4 weeks of culture. In these cells, semi-quantitative polymerase chain reaction (PCR) showed expression of the EFTFs and photoreceptor-specific genes. Even so, proteins for these markers were not detected and transplantation into retina failed to produce photoreceptors with outer segments.46 Treating human ES cell embryoid bodies for three days in low concentrations of Noggin, Wnt-inhibitor, Dickkopf WNT signaling pathway inhibitor 1 (Dkk-1), and insulin-like growth factor 1 (IGF-1) then switching to higher amounts and plating on Matrigel for 7 to 21 days, caused the ES cells to express transcripts for EFTFs and photoreceptor- specific genes (Fig. 2E).47 Transplanting these cells into neonatal mouse retinas produced cells with photoreceptor morphology, including outer segments.48
Human ES cells have a natural capacity to form a subset of anterior neuroepithelial cells. In this way, an alternative approach to adding extrinsic factors was discovered by the Gamm lab. They selected rosette-forming cells at day 16, cultured these cells and found greater than 95% expressed Rx and Pax6 (Fig. 2F). Interestingly, both Dkk1 and Noggin were detected in these cells by Western blotting, while adding Wnt3A and BMP4 to the cultures stopped Rx and Pax6 expression. Cells with characteristic RPE morphology and RPE gene expression were detected in these cultures, as were cells expressing photoreceptor-specific proteins.13
The ability to form retinal cells from human ES cells has been a great advance toward generating a population of cells useful for cell replacement therapy. Both the Gamm and Sasai labs have revealed that they can generate laminated retinas using either pluripotent iPS or ES cells.49,50 The human ES-derived eye cups could be frozen down and later, thawed and re-cultured.49 This is the first step in generating populations of cells for the clinic. Many studies are now focused on biasing these cells toward a homogenous culture of one retinal cell type.
GENERATION OF PHOTORECEPTOR AND GANGLION CELLS FROM MAMMALIAN EMBRYONIC STEM CELL CULTURES
Generation of photoreceptors has been of particular interest, since photoreceptor cell degeneration is the primary cause of blindness in retinitis pigmentosa and age-related macular degeneration; two diseases that affect a growing number of Americans. Intrinsic transcription factors that guide photoreceptor formation have been recently reviewed.51,52 Therefore, we will focus on extrinsic factors that induce photoreceptor formation.
The involvement of Notch signaling in photoreceptor formation was first discovered when interference of this pathway in retinal progenitors caused photoreceptor cell increase in the Xenopus retina.53 Consistent with this finding, photoreceptor cells were also predominantly increased when Notch1 was removed from the developing mouse and chick retina.54-56 When indirectly inhibiting Notch signaling in ES cell cultures by treating with the γ-secretase inhibitor IX, DAPT, the Takahashi lab discovered that photoreceptor-specific transcripts and protein could be induced in ES cell culture from mouse, monkey and human57. Similarly, when human ES-derived eye cups were treated with DAPT, there was a large increase in the number of cells expressing the cone-rod homeobox (Crx) marker, suggesting that photoreceptor cells were increased within these cultures.49
In addition to removing Notch, the Takahashi group also tested a variety of growth factors that were shown previously to promote rod photoreceptor formation in the embryo (Table 1; reviewed by Levine, 2000)66. These factors were tested on mouse ES cells treated by the serum-free floating culture of embryoid body-like aggregates (SFEB) combined with treatment with Dkk1, left-right determination factor 2 (LeftyA), fetal calf serum, and Activin (DLFA) (Fig. 2D). Adding factors shown in Table 1, they found rod photoreceptor cell production increased from 5% to 17% of the total Rx-positive cells grown in adherent cultures. For monkey and human ES cell cultures, they found that Dkk1 and LeftyA treatment of floating ES cultures was necessary after SFEB treatment. Besides, taurine and retinoic acid were the only factors necessary for inducing 12% rhodopsin-positive cells in monkey and about 9% rhodopsin- positive cells in human cultured ES cells. Cone photoreceptors (red/green cones and blue cones) were also found at similar percentages, making the total number of cells generated into photoreceptors approximately 25-35%.57 It is interesting to note that similar percentages of ES-derived photoreceptors were found after co-culturing the ES-derived Rx/Pax6-positive cells with E17.5 retinal cells.42 This suggests that the factors used in the study by Osakada et al57 are as effective as the factors produced by the embryonic retina.
Table 1.
Extrinsic factors: factors shown to promote rod photoreceptor formation
| factor | optimal concentration | model organism | References | mouse ES cells | monkey & human ES cells |
|---|---|---|---|---|---|
| DAPT | 2 µM | Chick | Kubo56 | 10 µM | - |
| aFGF | 20-100 ng/ml | Chick | Guillemot58 | 50 ng/ml | - |
| bFGF | 10-100 ng/ml | Chick | Guillemot58 | 10 ng/ml | - |
| Pittack59 | |||||
| Taurine | 100 µM | Rat | Altshuler60 | 1 mM | 100 µM |
| Shh | 2.4 nM | Rat | Levine61 | 3 nM | - |
| All-trans RA | 500 nM | Rat | Kelley62 | 500 nM | 1 µM |
| 9-cis RA | 100 nM | Rat | Kelley62, 1994 | ||
| β2-laminin | Rat | Hunter63 | |||
| Activin A | 100 ng/ml | Rat | Davis64 | ||
| T3 | 6.5 nM | Rat | Kelley65 |
Optimal concentration was reported in the reference listed on cultured retinal progenitor cells. The last two columns (red) show successful concentrations reported by Osakada et al,57 in mouse, monkey and human embryonic stem (ES) cell cultures, while the green rows are factors reported only by other studies.
DAPT, γ-secretase inhibitor IX; aFGF, acidic fibroblast growth factor; bFGF, basic fibroblast growth factor; Shh, sonic hedgehog; Alltrans RA, all-trans retinoic acid; 9-cis RA, 9-cis retinoic acid; T3, triiodothyronine (active thyroid hormone)
Other factors have also been implicated in coaxing retinal progenitor cells toward photoreceptors (green rows, Table 1). Retinoic acid (RA) treatment produces different results by its two isomers. While all-trans retinoic acid treatment results in 10 times as many rods in retinal progenitor cultures as controls, 9-cis retinoic acid treatment results in 25 times as many rods with one fifth of the concentration (100 versus 500 nanomolar).62 Increasing Activin signaling (adding Activin A) has also been demonstrated to promote rod photoreceptors in retinal progenitor culture, while the Activin-βA knockout mouse has fewer photoreceptors.64 Thyroid hormones (like T3) have been demonstrated to be important for regulating cone opsin expression. Thyroid hormone receptor beta isoform 2 protein was first found in retinal progenitor cells shortly after mouse cone genesis.67,68 In mice with a null-mutation in either thyroid receptor β2 (TRβ2) or retinoid X receptor gamma (RXRγ), S-opsin was universally expressed in all cones, instead of their usual dorsal to ventral, low to high expression gradient.69,70 These factors (RA, Activin A, T3, along with Taurine and Shh) were used to promote photoreceptor formation in human ES cultures incorporating these factors into the RD method (Fig. 2E). At 45 days, the cells reached a peak percentage of S-opsin- positive cells (52%), yet dropped to ~4% S-opsin-positive by day 60, suggesting that conditions to maintain these cells in culture still needs to be discovered.71
Retinal ganglion cell production from ES cell cultures has also been reported. In one study, mouse ES cells were transfected with a neomycin-resistant, Pax6-expressing plasmid. Cells were selected for their ability to induce six3, shh and ganglion cell specific transcripts. Transplantation into the mouse renal capsule showed neural-like processes.72 Using these cells for cell replacement therapy will be quite a challenge since the healthy donor cells would have to integrate and not only establish correct synaptic connections inside the retina, but also navigate outside the retina to make proper connections in the brain.
GENERATION OF RETINAL CELLS FROM INDUCED PlURIPOTENT CELLS
Another source of pluripotent cells are induced pluripotent cells, or iPS cells. Since iPS cells can be made from a patient’s own skin or blood cells, they are anticipated to have reduced immune rejection in cell replacement therapy. Also, once iPS cells could be reliably made into retinal cells, the cells of patients with rare retinal diseases could be studied in the isolated environment of the culture dish, where drug treatments could be tested to reduce the effects of retinal degeneration. Finally, the use of iPS cells circumvents usual ethical issues surrounding ES cell research. For these reasons, generating retinal cells from iPS cells has recently gained great interest in the field.
All iPS cell lines are not the same; some lines express higher neural markers than others. To generate retinal cells, the Gamm lab chose an iPS line known to express high levels of Pax6 and used these in their default method to generate retinal progenitor cells.13 Other iPS cell lines, with lower neural potential, were used by carefully selecting for an optic vesicle-like structure during the differentiation protocol. Using this approach, iPS-derived RPE cells were generated from a gyrate atrophy patient; a genetically heterogeneous disease. In gyrate atrophy patients, blindness is primarily due to a defect within the RPE. The cultured RPE cells, generated by this method, were tested for their response to levels of pharmacological agents that could treat the retinal disease. By understanding how the affected cells respond to treatment in a Petri dish, physicians could more effectively treat patients with appropriate concentrations of drugs and treatment paradigm for that individual.14
Patients with retinitis pigmentosa, which primarily affects rod photoreceptor cells, would also benefit from first testing iPS-derived rod photoreceptors in the dish, but first the conditions to generate these cells should be defined.
In order to maximize photoreceptor production, the human iPS cell line, IMR90-4, was studied over other available human iPS cell lines because the ‘default method’ of differentiation caused the formation of Pax6-positive cells by culture day 10 (Fig. 2F). Growing these cells to day 80 using this method, the authors found that 14% of all colonies expressed the early photoreceptor marker, Crx.13 The same percentage of Crx-positive cells were found at day 80 when human iPS cells were cultured using the SFEB/DLFA method (Fig. 2D). These culture conditions yielded Rx-positive colonies that were frequently also expressing an early marker for RPE progenitors, Mitf. Treating these cells with retinoic acid and taurine, increased Crx expression, and induced later photoreceptor markers, Recoverin and Rhodopsin.73 Crx- positive cells (23%) were also induced in mouse iPS cell lines by first putting them through a neural induction protocol and then exposing the cells to rat retinal P1 (PN1CM) or rat retinal E14 conditioned media (E14CM). Interestingly, the age of the conditioned media biased the retinal cells to form age-corresponding cells; that is, E14CM induced early-born, cone and ganglion cell markers, while PN1CM promoted late-born, rod and bipolar cell markers.74
In order to further favor photoreceptor formation, human iPS cell lines were tested for the highest increase in Crx after culturing by applying the RD method of retinal induction (Fig. 2E). These cells were infected with a photoreceptor-specific promoter driving GFP expression [interphotoreceptor retinoid-binding protein (IRBP) >GFP] during the culture period. Once a substantial number expressed GFP (10%), the cells were FAC sorted and transplanted into adult wild type mice eyes to be tested for integration. While a few cells integrated into the photoreceptor layer, none were found growing a morphologically characteristic outer segment.75
All iPS cell lines used in the above studies were derived from human or mouse fibroblast cells. A different approach used blood cells (T-lymphocytes) to derive an iPS cell line. Again, using the ‘default method,’ the authors generated retinal cells from T-lymphocyte- derived human iPS cells (TiPSCs). These TiPSCs formed optic vesicle-like spheres, just as when ES or iPS-derived from fibroblasts were employed. Some neurospheres were observed to have a laminated structure with photoreceptor-specific markers expressed in cells on the outer rim and ganglion-specific marker cells on the inner rim of the sphere.50 The ability to generate retinal cells from easily accessible blood cells is a great step toward developing protocols for clinical use. Other pluripotent cell sources have not been as successful. In a recent study, amniotic fluid-derived stem cells were collected from three different lines of mice: two expressing GFP under the control of photoreceptor-specific promoters (Nrl>GFP and Crx>GFP), and one line expressing GFP driven by a retinal progenitor- specific promoter (Fgf15>GFP). After culturing amniotic cells from each of these mice using the SFEB/DLFA method (Fig. 2D) and growing them on mouse retinal explants, these cells failed to differentiate into retinal cells did not express GFP.76 Therefore, it is important that these cells be tested for their ability to function in the retinal environment that the cells would repair.
TRANSPLANTATION STUDIES TO VERIFY FUNCTION/FEASIBILITY OF CELL REPLACEMENT
The ability of cultured cells to integrate, form connections and morphologically resemble retinal cells adds evidence that cultured cells are forming bonafide retinal cell types. The ES-derived eye-like cells induced in stromal cultures were transplanted but failed to integrate and differentiate in the adult mouse retina (Fig. 2B).77 Upon ganglion cell damage [induced by N-methyl-D-aspartate (NMDA) injection], the ganglion-like cells from these culture integrated into an adult eye, yet host animals failed to produce a vision evoked response. This suggests that these cells were not able to replace lost ganglion cells.77 In another study, ES cells treated with retinoic acid for four days were transplanted into the vitreous of retinal degeneration mice (rd1). These cells partially migrated into the retina and expressed neural cell markers but failed to differentiate into morphologically characteristic retinal cells.78 Using dissociated retinal progenitors from transgenic mice expressing GFP in rod progenitors (Nrl>GFP), it was determined that cells already specified toward a rod cell fate had the best integration rate and formed remarkably characteristic outer segments in the adult wild type retina. This study proposed that the developmental age of the donor cell should be considered, since much younger retinal progenitors failed to integrate as well as their postnatal counterparts.79 With this in mind, cone progenitors were isolated from earlier developmental stages. In order to perform this, FAC sorted Crx-positive cells were isolated at developmental stages that would favor the isolation of cone over rod progenitors (E12.5, E14.5 and E15.5). Surprisingly, when these donor cells were transplanted into the wild-type retina, many failed to integrate. The peak amount of cones (10 integrated cells) was observed from the E14.5 donor population.80 These results suggests that cone progenitors are still very rare and the number of these cell types needs to be favored for more robust number of integrated cells.
Retinal cells derived from mouse ES cells by the SFEB/DLFA method (Fig. 2D) were characterized for their expression of pluripotent markers and markers of early and late photoreceptor-specific expression. NRL-positive cells were infrequently found (0.2%) while the transcript for crx, nrl, nr2e3 and rhodopsin were all present in these cells. Transplantation of cultured cells at peak NRL expression (day 28), which were 60% Crx-positive, failed to integrate and formed tumors.81 This suggests that the expression profile of the cells may not be an indicator of proper integration and potential retinal repair. However, cell surface markers for photoreceptor progenitor cells may be a better indicator. Sorting developing retinal cells using antibodies against CD24 and/or CD73, the same investigators found an increase in integration (18-fold) over the unsorted retinal cells of the same developmental age.82 This presents an exciting new way of isolating cultured retinal cells from pluripotent cell sources. Retinal cells from all different culture methods could be sorted using these two commercially available antibodies and tested in future transplantation studies.
One problem with transplanting individual cells is that they form rosettes because apical and basal cues are lost in the microenvironment. One way around this problem would be to create a three-dimensional scaffold that would provide the orientation in vitro, prior to transplantation. Dissociated mouse retinal progenitors and human ES cells put through the RD protocol were grown on a three-dimensional polylactic- co-glycolic acid (PLGA) scaffold, designed to support the columnar organization characteristic of differentiating retinal progenitor cells. Both mouse and human cells aligned themselves in a pattern consistent with their location in the developing retina; that is, Pax6-positive cells lined up above Otx2-positive retinal cells.83 Ultrathin sheets of RPE already have been successfully transplanted in the sub- retinal space. The cells were first grown on a 4 micron parylene substrate and then injected in the rat eye. Only 2% of the transplanted cells were lost using this technique.84 Future studies could combine these two cultures to create an entirely new retina in culture, ready for transplantation.
ARTIFICIAL RETINA
Recent excitement has surrounded the retinal prosthesis field. Patients with advanced stages of retinitis pigmentosa were again able to recognize letters and words. The 60-electrode, Argus II epiretinal prosthesis was surgically fitted on top of their inner limiting membranes to stimulate remaining retinal ganglion cells. The patients receiving this device were then tested for letter recognition. Of the 30 subjects, six were able to correctly identify letters and even words after surgery.85 An alternative 16-electrode array has been developed by Zrenner’s group in Germany, called the Tübingen array. Rather than intravitreal placement, surgeons implant the 16-electrode array in the subretinal space, in an effort to stimulate remaining bipolar and ganglion cells. Of the 11 patients treated, 8 were able to process electrical stimulation as visual images.86 These prosthetic devices hold great promise as the arrays become more sophisticated and the costs become more affordable ($150,000/ implantation in the US).87 Retinal prosthesis may be another option to repair damaged or degenerating retinas.
Acknowledgments
This review was written by support from the National Eye Institute (R01EY019517), Research to Prevent Blindness (unrestricted grant to the Ophthalmology Department) and the Lions of Central New York (District 20Y1). Also, special thanks to Michael Zuber and Barry Knox for their support of this review.
Footnotes
Conflicts of Interest
None.
REFERENCES
- 1.Müller F, O’Rahilly R. The first appearance of the neural tube and optic primordium in the human embryo at stage 10. Anat Embryol (Berl) 1985;172:157–169. doi: 10.1007/BF00319598. [DOI] [PubMed] [Google Scholar]
- 2.Zuber ME, Harris WA. Formation of the eye field. In: Sernagor E, Eglen S, Harris WA, Wong R, editors. Retinal Development. Cambridge: Cambridge University Press; 2006. pp. 8–29. [Google Scholar]
- 3.Lanza RP. Essentials of stem cell biology. Boston: Elsevier/Academic Press; 2009. [Google Scholar]
- 4.Amato MA, Arnault E, Perron M. Retinal stem cells in vertebrates: parallels and divergences. Int J Dev Biol. 2004;48:993–1001. doi: 10.1387/ijdb.041879ma. [DOI] [PubMed] [Google Scholar]
- 5.Coles BL, Angénieux B, Inoue T, Del Rio-Tsonis K, Spence JR, McInnes RR, et al. Facile isolation and the characterization of human retinal stem cells. Proc Natl Acad Sci U S A. 2004;101:15772–15777. doi: 10.1073/pnas.0401596101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tropepe V, Coles BL, Chiasson BJ, Horsford DJ, Elia AJ, McInnes RR, et al. Retinal stem cells in the adult mammalian eye. Science. 2000;287:2032–2036. doi: 10.1126/science.287.5460.2032. [DOI] [PubMed] [Google Scholar]
- 7.Cicero SA, Johnson D, Reyntjens S, Frase S, Connell S, Chow LM, et al. Cells previously identified as retinal stem cells are pigmented ciliary epithelial cells. Proc Natl Acad Sci U S A. 2009;106:6685–6690. doi: 10.1073/pnas.0901596106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Locker M, El Yakoubi W, Mazurier N, Dullin JP, Perron M. A decade of mammalian retinal stem cell research. Arch Ital Biol. 2010;148:59–72. [PubMed] [Google Scholar]
- 9.Hitchcock P, Ochocinska M, Sieh A, Otteson D. Persistent and injury-induced neurogenesis in the vertebrate retina. Prog Retin Eye Res. 2004;23:183–194. doi: 10.1016/j.preteyeres.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 10.Tsonis PA, Del Rio-Tsonis K. Lens and retina regeneration: transdifferentiation, stem cells and clinical applications. Exp Eye Res. 2004;78:161–172. doi: 10.1016/j.exer.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 11.Salero E, Blenkinsop TA, Corneo B, Harris A, Rabin D, Stern JH, et al. Adult human RPE can be activated into a multipotent stem cell that produces mesenchymal derivatives. Cell Stem Cell. 2012;10:88–95. doi: 10.1016/j.stem.2011.11.018. [DOI] [PubMed] [Google Scholar]
- 12.Idelson M, Alper R, Obolensky A, Ben-Shushan E, Hemo I, Yachimovich-Cohen N, et al. Directed differentiation of human embryonic stem cells into functional retinal pigment epithelium cells. Cell Stem Cell. 2009;5:396–408. doi: 10.1016/j.stem.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 13.Meyer JS, Shearer RL, Capowski EE, Wright LS, Wallace KA, McMillan EL, et al. Modeling early retinal development with human embryonic and induced pluripotent stem cells. Proc Natl Acad Sci USA. 2009;106:16698–16703. doi: 10.1073/pnas.0905245106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meyer JS, Howden SE, Wallace KA, Verhoeven AD, Wright LS, Capowski EE, et al. Optic vesicle-like structures derived from human pluripotent stem cells facilitate a customized approach to retinal disease treatment. Stem Cells. 2011;29:1206–1218. doi: 10.1002/stem.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kumar JP, Moses K. EGF receptor and Notch signaling act upstream of Eyeless/Pax6 to control eye specification. Cell. 2001;104:687–697. doi: 10.1016/s0092-8674(01)00265-3. [DOI] [PubMed] [Google Scholar]
- 16.Silver SJ, Rebay I. Signaling circuitries in development: insights from the retinal determination gene network. Development. 2005;132:3–13. doi: 10.1242/dev.01539. [DOI] [PubMed] [Google Scholar]
- 17.Zuber ME, Gestri G, Viczian AS, Barsacchi G, Harris WA. Specification of the vertebrate eye by a network of eye field transcription factors. Development. 2003;130:5155–5167. doi: 10.1242/dev.00723. [DOI] [PubMed] [Google Scholar]
- 18.Viczian AS, Solessio EC, Lyou Y, Zuber ME. Generation of functional eyes from pluripotent cells. PLoS Biol. 2009;7:e1000174. doi: 10.1371/journal.pbio.1000174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lan L, Vitobello A, Bertacchi M, Cremisi F, Vignali R, Andreazzoli M, et al. Noggin elicits retinal fate in Xenopus animal cap embryonic stem cells. Stem Cells. 2009;27:2146–2152. doi: 10.1002/stem.167. [DOI] [PubMed] [Google Scholar]
- 20.Eiraku M, Watanabe K, Matsuo-Takasaki M, Kawada M, Yonemura S, Matsumura M, et al. Self- organized formation of polarized cortical tissues from ESCs and its active manipulation by extrinsic signals. Cell Stem Cell. 2008;3:519–532. doi: 10.1016/j.stem.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 21.Bayramov AV, Eroshkin FM, Martynova NY, Ermakova GV, Solovieva EA, Zaraisky AG. Novel functions of Noggin proteins: inhibition of Activin/Nodal and Wnt signaling. Development. 2011;138:5345–5356. doi: 10.1242/dev.068908. [DOI] [PubMed] [Google Scholar]
- 22.Acampora D, Avantaggiato V, Tuorto F, Simeone A. Genetic control of brain morphogenesis through Otx gene dosage requirement. Development. 1997;124:3639–3650. doi: 10.1242/dev.124.18.3639. [DOI] [PubMed] [Google Scholar]
- 23.Favor J, Gloeckner CJ, Neuhäuser-Klaus A, Pretsch W, Sandulache R, Saule S, et al. Relationship of Pax6 activity levels to the extent of eye development in the mouse, Mus musculus. Genetics. 2008;179:1345–1355. doi: 10.1534/genetics.108.088591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lagutin OV, Zhu CC, Kobayashi D, Topczewski J, Shimamura K, Puelles L, et al. Six3 repression of Wnt signaling in the anterior neuroectoderm is essential for vertebrate forebrain development. Genes Dev. 2003;17:368–379. doi: 10.1101/gad.1059403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li X, Perissi V, Liu F, Rose DW, Rosenfeld MG. Tissue-specific regulation of retinal and pituitary precursor cell proliferation. Science. 2002;297:1180–1183. doi: 10.1126/science.1073263. [DOI] [PubMed] [Google Scholar]
- 26.Mathers PH, Grinberg A, Mahon KA, Jamrich M. The Rx homeobox gene is essential for vertebrate eye development. Nature. 1997;387:603–607. doi: 10.1038/42475. [DOI] [PubMed] [Google Scholar]
- 27.Yun S, Saijoh Y, Hirokawa KE, Kopinke D, Murtaugh LC, Monuki ES, et al. Lhx2 links the intrinsic and extrinsic factors that control optic cup formation. Development. 2009;136:3895–3906. doi: 10.1242/dev.041202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kawasaki H, Mizuseki K, Nishikawa S, Kaneko S, Kuwana Y, Nakanishi S, et al. Induction of midbrain dopaminergic neurons from ES cells by stromal cell- derived inducing activity. Neuron. 2000;28:31–40. doi: 10.1016/s0896-6273(00)00083-0. [DOI] [PubMed] [Google Scholar]
- 29.Hirano M, Yamamoto A, Yoshimura N, Tokunaga T, Motohashi T, Ishizaki K, et al. Generation of structures formed by lens and retinal cells differentiating from embryonic stem cells. Dev Dyn. 2003;228:664–671. doi: 10.1002/dvdy.10425. [DOI] [PubMed] [Google Scholar]
- 30.Aoki H, Hara A, Nakagawa S, Motohashi T, Hirano M, Takahashi Y, et al. Embryonic stem cells that differentiate into RPE cell precursors in vitro develop into RPE cell monolayers in vivo. Exp Eye Res. 2006;82:265–274. doi: 10.1016/j.exer.2005.06.021. [DOI] [PubMed] [Google Scholar]
- 31.Aoki H, Hara A, Niwa M, Motohashi T, Suzuki T, Kunisada T. An in vitro mouse model for retinal ganglion cell replacement therapy using eye-like structures differentiated from ES cells. Exp Eye Res. 2007;84:868–875. doi: 10.1016/j.exer.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 32.Tabata Y, Ouchi Y, Kamiya H, Manabe T, Arai K, Watanabe S. Specification of the retinal fate of mouse embryonic stem cells by ectopic expression of Rx/rax, a homeobox gene. Mol Cell Biol. 2004;24:4513–4521. doi: 10.1128/MCB.24.10.4513-4521.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kawasaki H, Suemori H, Mizuseki K, Watanabe K, Urano F, Ichinose H, et al. Generation of dopaminergic neurons and pigmented epithelia from primate ES cells by stromal cell-derived inducing activity. Proc Natl Acad Sci U S A. 2002;99:1580–1585. doi: 10.1073/pnas.032662199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ooto S, Haruta M, Honda Y, Kawasaki H, Sasai Y, Takahashi M. Induction of the differentiation of lentoids from primate embryonic stem cells. Invest Ophthalmol Vis Sci. 2003;44:2689–2693. doi: 10.1167/iovs.02-1168. [DOI] [PubMed] [Google Scholar]
- 35.Mizuseki K, Sakamoto T, Watanabe K, Muguruma K, Ikeya M, Nishiyama A, et al. Generation of neural crest-derived peripheral neurons and floor plate cells from mouse and primate embryonic stem cells. Proc Natl Acad Sci U S A. 2003;100:5828–5833. doi: 10.1073/pnas.1037282100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ying QL, Stavridis M, Griffiths D, Li M, Smith A. Conversion of embryonic stem cells into neuroectodermal precursors in adherent monoculture. Nat Biotechnol. 2003;21:183–186. doi: 10.1038/nbt780. [DOI] [PubMed] [Google Scholar]
- 37.Aubert J, Dunstan H, Chambers I, Smith A. Functional gene screening in embryonic stem cells implicates Wnt antagonism in neural differentiation. Nat Biotechnol. 2002;20:1240–1245. doi: 10.1038/nbt763. [DOI] [PubMed] [Google Scholar]
- 38.Parisi S, D’Andrea D, Lago CT, Adamson ED, Persico MG, Minchiotti G. Nodal-dependent Cripto signaling promotes cardiomyogenesis and redirects the neural fate of embryonic stem cells. J Cell Biol. 2003;63:303–314. doi: 10.1083/jcb.200303010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smith JR, Vallier L, Lupo G, Alexander M, Harris WA, Pedersen RA. Inhibition of Activin/Nodal signaling promotes specification of human embryonic stem cells into neuroectoderm. Dev Biol. 2008;313:107–117. doi: 10.1016/j.ydbio.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 40.Piccolo S, Agius E, Leyns L, Bhattacharyya S, Grunz H, Bouwmeester T, et al. The head inducer Cerberus is a multifunctional antagonist of Nodal, BMP and Wnt signals. Nature. 1999;397:707–710. doi: 10.1038/17820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Watanabe K, Kamiya D, Nishiyama A, Katayama T, Nozaki S, Kawasaki H, et al. Directed differentiation of telencephalic precursors from embryonic stem cells. Nat Neurosci. 2005;8:288–296. doi: 10.1038/nn1402. [DOI] [PubMed] [Google Scholar]
- 42.Ikeda H, Osakada F, Watanabe K, Mizuseki K, Haraguchi T, Miyoshi H, et al. Generation of Rx+/ Pax6+ neural retinal precursors from embryonic stem cells. Proc Natl Acad Sci U S A. 2005;102:11331–11336. doi: 10.1073/pnas.0500010102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eiraku M, Takata N, Ishibashi H, Kawada M, Sakakura E, Okuda S, et al. Self-organizing optic- cup morphogenesis in three-dimensional culture. Nature. 2011;472:51–56. doi: 10.1038/nature09941. [DOI] [PubMed] [Google Scholar]
- 44.Rossant J. Stem cells and early lineage development. Cell. 2008;132:527–531. doi: 10.1016/j.cell.2008.01.039. [DOI] [PubMed] [Google Scholar]
- 45.Brons IG, Smithers LE, Trotter MW, Rugg-Gunn P, Sun B, Chuva de, et al. Derivation of pluripotent epiblast stem cells from mammalian embryos. Nature. 2007;448:191–195. doi: 10.1038/nature05950. [DOI] [PubMed] [Google Scholar]
- 46.Banin E, Obolensky A, Idelson M, Hemo I, Reinhardtz E, Pikarsky E, et al. Retinal incorporation and differentiation of neural precursors derived from human embryonic stem cells. Stem Cells. 2006;24:246–257. doi: 10.1634/stemcells.2005-0009. [DOI] [PubMed] [Google Scholar]
- 47.Lamba DA, Karl MO, Ware CB, Reh TA. Efficient generation of retinal progenitor cells from human embryonic stem cells. Proc Natl Acad Sci U S A. 2006;103:12769–12774. doi: 10.1073/pnas.0601990103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lamba DA, Karl MO, Reh TA. Strategies for retinal repair: cell replacement and regeneration. Prog Brain Res. 2009;175:23–31. doi: 10.1016/S0079-6123(09)17502-7. [DOI] [PubMed] [Google Scholar]
- 49.Nakano T, Ando S, Takata N, Kawada M, Muguruma K, Sekiguchi K, et al. Self-formation of optic cups and storable stratified neural retina from human ESCs. Cell Stem Cell. 2012;10:771–785. doi: 10.1016/j.stem.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 50.Phillips MJ, Wallace KA, Dickerson SJ, Miller MJ, Verhoeven AD, Martin JM, et al. Blood-derived human iPS cells generate optic vesicle-like structures with the capacity to form retinal laminae and develop synapses. Invest Ophthalmol Vis Sci. 2012;53:2007–2019. doi: 10.1167/iovs.11-9313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gregory-Evans CY, Wallace VA, Gregory-Evans K. Gene networks: dissecting pathways in retinal development and disease. Prog Retin Eye Res. 2013;33:40–66. doi: 10.1016/j.preteyeres.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 52.Swaroop A, Kim D, Forrest D. Transcriptional regulation of photoreceptor development and homeostasis in the mammalian retina. Nat Rev Neurosci. 2010;11:563–576. doi: 10.1038/nrn2880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dorsky RI, Chang WS, Rapaport DH, Harris WA. Regulation of neuronal diversity in the Xenopus retina by Delta signalling. Nature. 1997;385:67–70. doi: 10.1038/385067a0. [DOI] [PubMed] [Google Scholar]
- 54.Jadhav AP, Mason HA, Cepko CL. Notch 1 inhibits photoreceptor production in the developing mammalian retina. Development. 2006;133:913–923. doi: 10.1242/dev.02245. [DOI] [PubMed] [Google Scholar]
- 55.Yaron O, Farhy C, Marquardt T, Applebury M, Ashery-Padan R. Notch1 functions to suppress cone- photoreceptor fate specification in the developing mouse retina. Development. 2006;133:1367–1378. doi: 10.1242/dev.02311. [DOI] [PubMed] [Google Scholar]
- 56.Kubo F, Takeichi M, Nakagawa S. Wnt2b inhibits differentiation of retinal progenitor cells in the absence of Notch activity by downregulating the expression of proneural genes. Development. 2005;132:2759–2770. doi: 10.1242/dev.01856. [DOI] [PubMed] [Google Scholar]
- 57.Osakada F, Ikeda H, Mandai M, Wataya T, Watanabe K, Yoshimura N, et al. Toward the generation of rod and cone photoreceptors from mouse, monkey and human embryonic stem cells. Nat Biotechnol. 2008;26:215–224. doi: 10.1038/nbt1384. [DOI] [PubMed] [Google Scholar]
- 58.Guillemot F, Cepko CL. Retinal fate and ganglion cell differentiation are potentiated by acidic FGF in an in vitro assay of early retinal development. Development. 1992;114:743–754. doi: 10.1242/dev.114.3.743. [DOI] [PubMed] [Google Scholar]
- 59.Pittack C, Jones M, Reh TA. Basic fibroblast growth factor induces retinal pigment epithelium to generate neural retina in vitro. Development. 1991;113:577–588. doi: 10.1242/dev.113.2.577. [DOI] [PubMed] [Google Scholar]
- 60.Altshuler D, Lo Turco JJ, Rush J, Cepko C. Taurine promotes the differentiation of a vertebrate retinal cell type in vitro. Development. 1993;119:1317–128. doi: 10.1242/dev.119.4.1317. [DOI] [PubMed] [Google Scholar]
- 61.Levine EM, Roelink H, Turner J, Reh TA. Sonic hedgehog promotes rod photoreceptor differentiation in mammalian retinal cells in vitro. J Neurosci. 1997;17:6277–6288. doi: 10.1523/JNEUROSCI.17-16-06277.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kelley MW, Turner JK, Reh TA. Retinoic acid promotes differentiation of photoreceptors in vitro. Development. 1994;120:2091–2102. doi: 10.1242/dev.120.8.2091. [DOI] [PubMed] [Google Scholar]
- 63.Hunter DD, Murphy MD, Olsson CV, Brunken WJ. S-laminin expression in adult and developing retinae: a potential cue for photoreceptor morphogenesis. Neuron. 1992;8:399–413. doi: 10.1016/0896-6273(92)90269-j. [DOI] [PubMed] [Google Scholar]
- 64.Davis AA, Matzuk MM, Reh TA. Activin A promotes progenitor differentiation into photoreceptors in rodent retina. Mol Cell Neurosci. 2000;15:11–21. doi: 10.1006/mcne.1999.0806. [DOI] [PubMed] [Google Scholar]
- 65.Kelley MW, Turner JK, Reh TA. Ligands of steroid/ thyroid receptors induce cone photoreceptors in vertebrate retina. Development. 1995;121:3777–3785. doi: 10.1242/dev.121.11.3777. [DOI] [PubMed] [Google Scholar]
- 66.Levine EM, Fuhrmann S, Reh TA. Soluble factors and the development of rod photoreceptors. Cell Mol Life Sci. 2000;57:224–234. doi: 10.1007/PL00000686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Applebury ML, Farhangfar F, Glösmann M, Hashimoto K, Kage K, Robbins JT, et al. Transient expression of thyroid hormone nuclear receptor TRbeta2 sets S opsin patterning during cone photoreceptor genesis. Dev Dyn. 2007;236:1203–1212. doi: 10.1002/dvdy.21155. [DOI] [PubMed] [Google Scholar]
- 68.Ng L, Ma M, Curran T, Forrest D. Developmental expression of thyroid hormone receptor beta2 protein in cone photoreceptors in the mouse. Neuroreport. 2009;20:627–631. doi: 10.1097/WNR.0b013e32832a2c63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ng L, Hurley JB, Dierks B, Srinivas M, Saltó C, Vennström B, et al. A thyroid hormone receptor that is required for the development of green cone photoreceptors. Nat Genet. 2001;27:94–98. doi: 10.1038/83829. [DOI] [PubMed] [Google Scholar]
- 70.Roberts MR, Hendrickson A, McGuire CR, Reh TA. Retinoid X receptor (gamma) is necessary to establish the S-opsin gradient in cone photoreceptors of the developing mouse retina. Invest Ophthalmol Vis Sci. 2005;46:2897–2904. doi: 10.1167/iovs.05-0093. [DOI] [PubMed] [Google Scholar]
- 71.Mellough CB, Sernagor E, Moreno-Gimeno I, Steel DH, Lako M. Efficient stage-specific differentiation of human pluripotent stem cells toward retinal photoreceptor cells. Stem Cells. 2012;30:673–686. doi: 10.1002/stem.1037. [DOI] [PubMed] [Google Scholar]
- 72.Kayama M, Kurokawa MS, Ueda Y, Ueno H, Kumagai Y, Chiba S, et al. Transfection with Pax6 gene of mouse embryonic stem cells and subsequent cell cloning induced retinal neuron progenitors, including retinal ganglion cell-like cells, in vitro. Ophthalmic Res. 2009;43:79–91. doi: 10.1159/000247592. [DOI] [PubMed] [Google Scholar]
- 73.Hirami Y, Osakada F, Takahashi K, Okita K, Yamanaka S, Ikeda H, et al. Generation of retinal cells from mouse and human induced pluripotent stem cells. Neurosci Lett. 2009;458:126–131. doi: 10.1016/j.neulet.2009.04.035. [DOI] [PubMed] [Google Scholar]
- 74.Parameswaran S, Balasubramanian S, Babai N, Qiu F, Eudy JD, Thoreson WB, et al. Induced pluripotent stem cells generate both retinal ganglion cells and photoreceptors: therapeutic implications in degenerative changes in glaucoma and age-related macular degeneration. Stem Cells. 2010;28:695–703. doi: 10.1002/stem.320. [DOI] [PubMed] [Google Scholar]
- 75.Lamba DA, McUsic A, Hirata RK, Wang PR, Russell D, Reh TA. Generation, purification and transplantation of photoreceptors derived from human induced pluripotent stem cells. PLoS One. 2010;5:e8763. doi: 10.1371/journal.pone.0008763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Decembrini S, Cananzi M, Gualdoni S, Battersby A, Allen N, Pearson RA, et al. Comparative analysis of the retinal potential of embryonic stem cells and amniotic fluid-derived stem cells. Stem Cells Dev. 2011;20:851–863. doi: 10.1089/scd.2010.0291. [DOI] [PubMed] [Google Scholar]
- 77.Aoki H, Hara A, Niwa M, Motohashi T, Suzuki T, Kunisada T. Transplantation of cells from eye-like structures differentiated from embryonic stem cells in vitro and in vivo regeneration of retinal ganglion-like cells. Graefes Arch Clin Exp Ophthalmol. 2008;246:255–265. doi: 10.1007/s00417-007-0710-6. [DOI] [PubMed] [Google Scholar]
- 78.Meyer JS, Katz ML, Maruniak JA, Kirk MD. Neural differentiation of mouse embryonic stem cells in vitro and after transplantation into eyes of mutant mice with rapid retinal degeneration. Brain Res. 2004;1014:131–144. doi: 10.1016/j.brainres.2004.04.019. [DOI] [PubMed] [Google Scholar]
- 79.MacLaren RE, Pearson RA, MacNeil A, Douglas RH, Salt TE, Akimoto M, et al. Retinal repair by transplantation of photoreceptor precursors. Nature. 2006;444:203–207. doi: 10.1038/nature05161. [DOI] [PubMed] [Google Scholar]
- 80.Lakowski J, Baron M, Bainbridge J, Barber AC, Pearson RA, Ali RR, et al. Cone and rod photoreceptor transplantation in models of the childhood retinopathy Leber congenital amaurosis using flow-sorted Crx-positive donor cells. Hum Mol Genet. 2010;19:4545–4559. doi: 10.1093/hmg/ddq378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.West EL, Gonzalez-Cordero A, Hippert C, Osakada F, Martinez-Barbera JP, Pearson RA, et al. Defining the integration capacity of ES cell-derived photoreceptor precursors. Stem Cells. 2012;30:1424–1435. doi: 10.1002/stem.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lakowski J, Han YT, Pearson RA, Gonzalez-Cordero A, West EL, Gualdoni S, et al. Effective transplantation of photoreceptor precursor cells selected via cell surface antigen expression. Stem Cells. 2011;29:1391–1404. doi: 10.1002/stem.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.McUsic AC, Lamba DA, Reh TA. Guiding the morphogenesis of dissociated newborn mouse retinal cells and hES cell-derived retinal cells by soft lithography-patterned microchannel PLGA scaffolds. Biomaterials. 2012;33:1396–1405. doi: 10.1016/j.biomaterials.2011.10.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hu Y, Liu L, Lu B, Zhu D, Ribeiro R, Diniz B, et al. A novel approach for subretinal implantation of ultrathin substrates containing stem cell-derived retinal pigment epithelium monolayer. Ophthalmic Res. 2012;48:186–191. doi: 10.1159/000338749. [DOI] [PubMed] [Google Scholar]
- 85.da Cruz L, Coley BF, Dorn J, Merlini F, Filley E, Christopher P, et al. The Argus II epiretinal prosthesis system allows letter and word reading and long-term function in patients with profound vision loss. Br J Ophthalmol. 2013;97:632–636. doi: 10.1136/bjophthalmol-2012-301525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wilke R, Gabel VP, Sachs H, Bartz Schmidt KU, Gekeler F, Besch D, et al. Spatial resolution and perception of patterns mediated by a subretinal 16-electrode array in patients blinded by hereditary retinal dystrophies. Invest Ophthalmol Vis Sci. 2011;52:5995–6003. doi: 10.1167/iovs.10-6946. [DOI] [PubMed] [Google Scholar]
- 87.Belluck P. Device offers partial vision for the blind. The New York Times Health. 2013 [Google Scholar]