Abstract
The sixth cranial nerve runs a long course from the brainstem to the lateral rectus muscle. Based on the location of an abnormality, other neurologic structures may be involved with the pathology related to this nerve. Sixth nerve palsy is frequently due to a benign process with full recovery within weeks, yet caution is warranted as it may portend a serious neurologic process. Hence, early diagnosis is often critical for some conditions that present with sixth nerve palsy. This article outlines a simple clinical approach to sixth nerve palsy based on its anatomy.
Keywords: Sixth Nerve Anatomy, Sixth Nerve Palsy
INTRODUCTION
Dysfunction of the sixth cranial (abducens) nerve can result from lesions occurring anywhere along its course between the sixth nerve nucleus in the dorsal pons and the lateral rectus muscle within the orbit. The sixth nerve has the longest subarachnoid course of all cranial nerves and innervates the ipsilateral lateral rectus (LR) which abducts the eye.
The long and tortuous course of the nerve is divided into five sections. Lesions within each section are frequently recognizable by involvement of contiguous structures. By understanding this anatomical schema, the clinician can recall the relevant clinical signs and symptoms, and also the many possible etiologies. Early diagnosis is often critical in some conditions that present with sixth nerve palsy. Table 1, summarizes seven retrospective studies available in the literature.1-7
Table 1.
Summary of six retrospective studies on patients with sixth nerve paresis
| Etiologies of acquired VI nerve palsy | |||||||
|---|---|---|---|---|---|---|---|
| Schrader1 (1960) (isolated) | Rucker2 (1966) | Johnston3 (1968) | Robertson4 (1970) (children) | Rush5 (1981) | Potel6 (2004) | Bagheri7 (2010) | |
| Total number of patients | 104 | 607 | 158 | 133 | 419 | 137 | 33 |
| Etiologies (%) | |||||||
| Neoplasm | 7 | 33 | 13 | 39 | 15 | 5 | 2 |
| Trauma | 3 | 12 | 32 | 20 | 17 | 12 | 18 |
| Aneurysm | 0 | 3 | 1 | 3 | 3 | 2 | 0 |
| Ischemic | 36 | 8 | 16 | 0 | 18 | 16 | 1 |
| Miscellaneous* | 30 | 24 | 30 | 29 | 18 | 19 | 6 |
| Undetermined** | 24 | 20 | 8 | 9 | 29 | 26 | 6 |
6% to 30% attributed to a miscellaneous group of causes that includes leukemia, migraine, pseudotumor cerebri, multiple sclerosis; the miscellaneous group of etiologies reflects the poor localizing value of sixth nerve paresis.
6% to 29%, etiology undetermined, reflecting vulnerability of the nerve to conditions which are transient, benign and unrecognizable.
If the signs and symptoms are not consistent with one of these five syndromes and there is no relevant historical information, the patient can be classified as a case of isolated sixth nerve palsy which constitutes the sixth syndrome.8-10
Manifestations and diagnosis of sixth nerve palsy, also known as lateral rectus palsy are reviewed herein. This article presents a simple clinical approach to sixth nerve palsy based on the anatomy of the abducens nerve and will conclude with recommendations for management of isolated sixth nerve palsy, and a review of the six major mimickers of abducens nerve palsy.11
ANATOMICAL CONSIDERATIONS
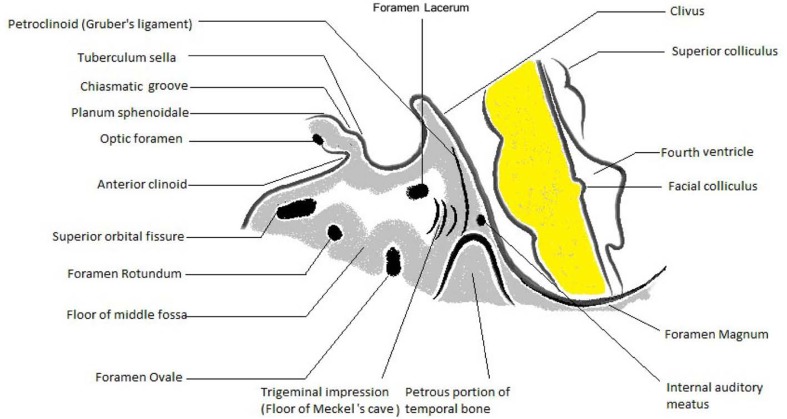
Figure 1, identifies structures in the posterior fossa, the skull base and the middle cranial fossa that serve as landmarks in the study of the abducens nerve.12,13
Figure 1.
Schematic representation of the landmarks, temporal view.
This schematic representation includes a sagittal section of the brainstem and is the framework upon which relevant cranial nerve and neurologic structures will be superimposed.
For the purpose of this review, knowledge of the following are required: internal auditory meatus, foramen lacerum, foramen ovale, foramen rotundum, superior orbital fissure and optic foramen (Fig. 1).
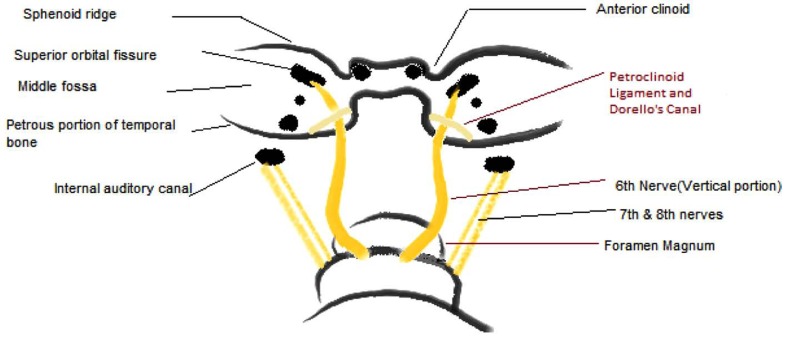
The foramina rotundum and ovale are located along the floor of the middle cranial fossa. The petroclinoid ligament extends, at an angle of approximately 30 degrees, from the medial third of the petrous ridge to the posterior clinoid. It thereby creates the compartment (Dorello’s canal) through which the abducens nerve travels (Fig. 2).
Figure 2.
Schematic representation of the anatomical landmarks, occipital view.
Figure 2 is a schematic of these structures viewed from the occipital pole. The brainstem is reflected posteriorly to permit visualization of the clivus, posterior clinoids, and petroclinoid (Gruber’s) ligament. It also indicates that the abducens nerve makes two 90-degree bends as it courses forward to the superior orbital fissure.
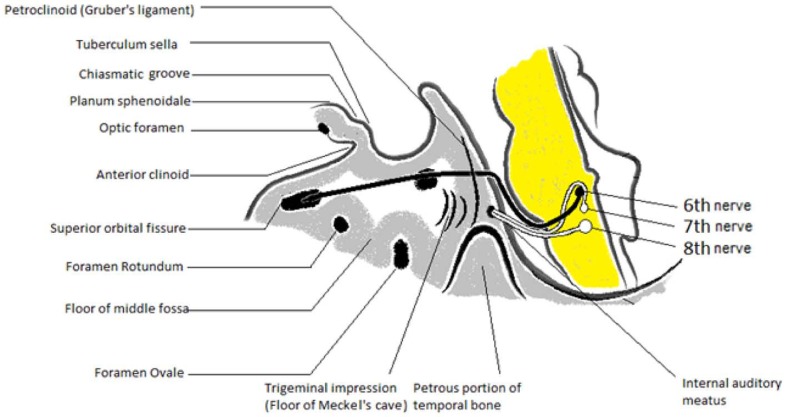
Figure 3 illustrates the S-shaped pathway of the sixth nerve, viewed from the temporal aspect. The first bend occurs as the nerve exits from the lower pons. It then travels vertically along the clivus, pierces the dura and turns anteriorly over the edge of the petrous pyramid, through Dorello’s canal and under Gruber’s ligament.
Figure 3.
Composite diagram illustrating the third through eighth cranial nerves.
The nerve then runs a direct anterior course, lying medial to the trigeminal ganglion and on the lateral aspect of the internal carotid artery which enters through the foramen lacerum. The abducens nerve enters the posterior aspect of the cavernous sinus, through which it travels together with the oculomotor and trochlear nerves, as well as the ophthalmic and maxillary divisions of the trigeminal nerve, and the internal carotid artery and carotid sympathetic plexus (Fig. 3).
Figure 3 also contain a sketch of the position and course of the seventh and eighth cranial nerves. The facial (VII) nerve fascicle loops around the nucleus of the sixth (VI) nerve, creating the facial colliculus, and turns anterolaterally to join the eighth nerve in its exit from the lower pons. They then travel upward and laterally to enter the internal auditory meatus.
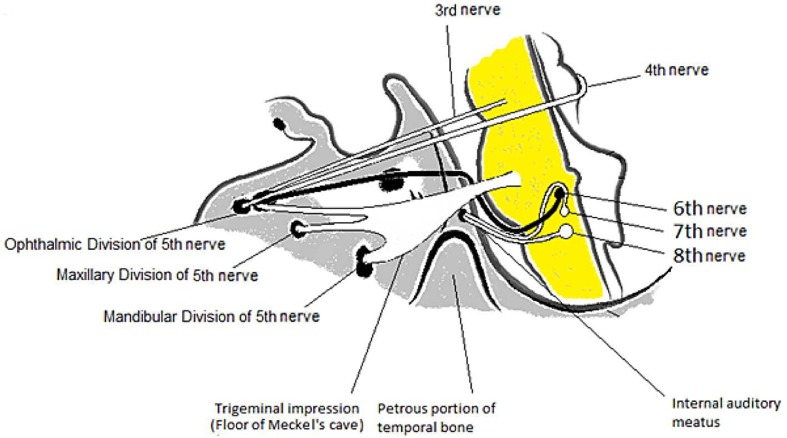
The third, fourth and fifth cranial nerves add to the framework and thereby complete the anatomic sketch that will become our reference. The oculomotor nerve takes a direct path anteriorly to the superior orbital fissure. In the posterior portion of the cavernous sinus it lies superior and lateral to the sixth nerve. More anteriorly, the oculomotor nerve is inferior and medial to the sixth nerve and lies close to the carotid. The trochlear nerve also makes a direct line to the superior orbital fissure, lying on the lateral wall of the cavernous sinus. The three divisions of the fifth nerve exit the middle fossa through three of the six holes. The mandibular division exits through foramen ovale, the maxillary division leaves through the foramen rotundum and the ophthalmic division enters the orbit through the superior orbital fissure (Fig. 4).
Figure 4.
Composite diagram divided into five sections, corresponding to the syndromes of the sixth nerve (VI1-VI5).
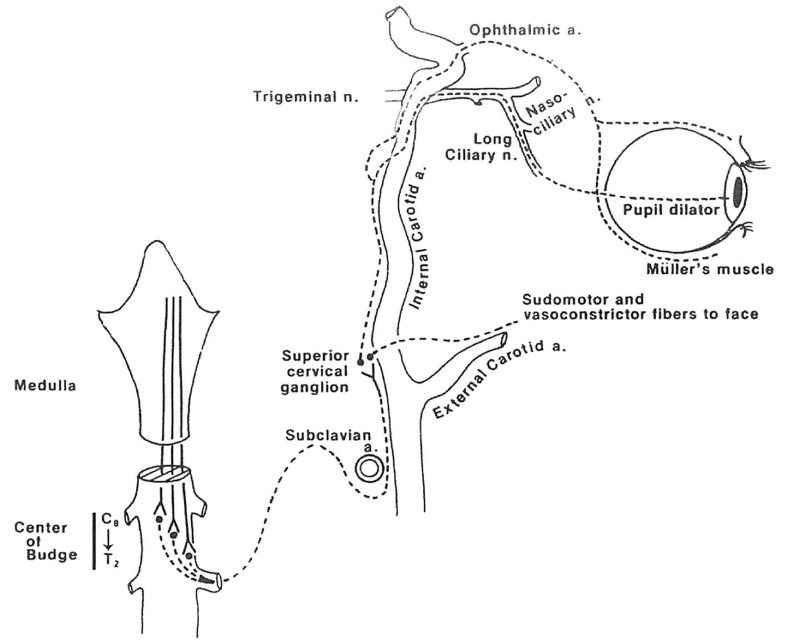
The sympathetic pathway is thought to be located in the lateral part of the medulla. The central neuron synapses with the cell body of the preganglionic neuron at the C8-T2 level, forming the ciliospinal center of Budge.
The preganglionic neuron then diverges from the cord and travels up to the superior cervical ganglion. The postganglionic fibers form a plexus around the internal carotid artery and travel with it through the foramen lacerum and cavernous sinus. The fibers, intended for pupil and Muller’s muscle, enter the orbit through the superior orbital fissure, traveling with the fifth and third nerves, respectively. The sudomotor fibers to the face travel with the external carotid artery (Fig. 5).
Figure 5.
Diagram of oculosympathetic pathway
The composite diagram in figure 4 can be divided into the five sections that may aid in determining the diagnosis of sixth nerve palsy:12
VI1: the brainstem syndrome
VI2: the elevated intracranial pressure syndrome
VI3: the petrous apex syndrome
VI4: the cavernous sinus syndrome
VI5: the orbital syndrome
Brainstem Syndrome
A lesion in the posterior fossa (Fig. 4) may be compressive, ischemic, inflammatory (most commonly multiple sclerosis in young adults) or degenerative and may involve the fifth, seventh and eighth cranial nerves, as well as the pyramidal tract on the anterior aspect of the pons and the cerebellum behind it.14
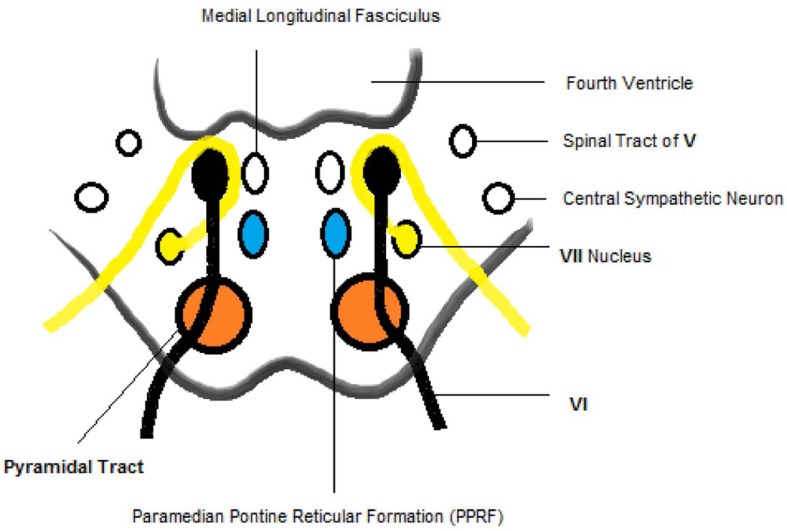
Figure 6 contains a cross-sectional diagram of the lower pons which includes four internal structures, namely the central neuron of oculosympathetic pathway, the spinal tract of five cranial nerves, the medial longitudinal fasciculus (MLF), and the paramedian pontine reticular formation (PPRF).15
Figure 6.
Diagram of cross-section of the lower pons, through the sixth nucleus and fascicle.
It is believed the PPRF sends a fiber to the ipsilateral sixth nucleus and a fiber that crosses immediately to ascend in the MLF to the contralateral medial rectus subnucleus which is more vulnerable in multiple sclerosis.
After taking a short digression through the internal anatomy of the pons, a list can be compiled of the possible accompanying clinical signs in the brainstem syndrome of the sixth nerve as summarized below: 16
1- Raymond’s syndrome:
Sixth nerve paresis
Contralateral hemiparesis (pyramidal tract)
2- Millard-Gubler syndrome:
Sixth nerve paresis
Ipsilateral seventh nerve paresis
Contralateral hemiparesis (pyramidal tract)
3- Foville’s syndrome:
Sixth nerve paresis
Horizontal conjugate gaze palsy
Ipsilateral V, VII, VIII cranial nerve palsy
Ipsilateral Horner’s syndrome
Elevated Intracranial Pressure Syndrome
Subarachnoid space syndrome
The second syndrome of the sixth nerve corresponds to the vertical course of the nerve as it ascends the clivus and turns 90 degrees anteriorly to enter Dorello’s canal (Fig. 3). The syndrome is placed in this portion of the diagram, not because it is due to lesions located in this area, but rather because lesions located elsewhere intracranially can secondarily affect the sixth nerve; this is an example of the poor localizing value of a sixth nerve palsy.
Changes in intracranial pressure (ICP) either increased or decreased may result in downward displacement of the brainstem causing stretching of the sixth nerve which is tethered as its exits the pons and inside Dorello’s canal.17-19 Approximately 30% of patients with pseudotumor cerebri have sixth nerve paresis as the only neurologic deficit,20 in addition to papilledema and concomitant visual field changes that result in blind spot enlargement. Normal or small-sized ventricles are often present on magnetic resonance imaging.
Other pathologies in the subarachnoid space leading to sixth nerve palsy include hemorrhage, meningeal or parameningeal infections (viral, bacterial, fungal), inflammation (sarcoidosis) or infiltrations (lymphoma, leukemia, carcinoma).21
Petrous Apex Syndrome
The next section of the course of the sixth nerve is under the petroclinoid ligament. Contact with the tip of the petrous pyramid makes the portion of the sixth nerve within Dorello’s canal susceptible to pathologic processes. This is especially important in cases secondary to localized inflammations or extra-dural abscesses due to complicated otitis media. In 1904 the syndrome was introduced by Giuseppe Gradenigo described as a constellation of sixth nerve palsy, ipsilateral decreased hearing (VIII nerve involvement), ipsilateral facial pain in distribution of cranial nerve V and ipsilateral facial paralysis (VII nerve involvement).22
Of note, lesions of the cerebellopontine angle (especially acoustic neuroma or meningioma) may involve the sixth and other contiguous cranial nerves, cause decreased hearing with vestibular symptoms, and decrease corneal sensitivity that can imitate the petrous apex syndrome.23
Pseudo-Gradenigo’s syndrome23
Hearing deficits in association with sixth nerve palsy and trigeminal symptoms may be due to brianstem lesions, such as cerebello-pontine angle tumor. Nasopharyngeal carcinoma may also mimic Gradenigo’s syndrome, since it can obstruct the Eustachian tube, resulting in serous otitis media. Additionally, the carcinoma may subsequently invade the cavernous sinus, causing sixth nerve paresis.23
Cavernous Sinus Syndrome (CSS)
The course of the sixth nerve through the cavernous sinus associates it with third, fourth and fifth (ophthalmic and maxillary divisions) cranial nerves as well as the internal carotid artery and the carotid sympathetic plexus.
The cavernous sinus syndrome may consist of deficits of two or more of these structures. The pituitary gland, optic nerve, and chiasm may also become affected in this syndrome. The sixth nerve may be involved in the cavernous sinus by a variety of processes including the following.
Nasopharyngeal carcinoma
Nasopharyngeal carcinoma is the most dreaded etiology of sixth nerve palsy and most frequently occurs between the ages of 40 and 70 years. It may present with various symptoms including nasal obstruction, rhinorrhea, epistaxis and serous otitis media secondary to obstruction of the Eustachian tube. The sphenoid sinus is also frequently involved by superior extension of the tumor.24,25
Intracavernous internal carotid artery aneurysm
The prominent, tortuous course of the internal carotid artery in the cavernous sinus raises the suspicion of an aneurysm as a common etiology of the cavernous sinus syndrome. The sixth and third cranial nerves are most vulnerable in this syndrome.26,27 However, as seen in Table 1, aneurysms represent a small proportions of the causes of sixth nerve palsy, ranging from zero to 3% of cases. Schrader1 found no case of aneurysm in 104 patients with isolated sixth nerve palsy. Locksley28, reported that out of 2,695 cases of single aneurysms (ruptured and unruptured) only 50 (1.9%) were located in the intracavernous portion of the internal carotid artery.
Carotid-cavernous fistula (CCF)
A defect of the internal carotid artery within the cavernous sinus will result in arterialization of the sinus, and of the orbital and ocular veins which will result in the following signs and symptoms: pain, proptosis, bruit, ocular pulsation, red eye, chemosis and tearing, double vision and decreased vision.
The abducens nerve is most frequently involved followed by the third, fourth and fifth cranial nerves. It is difficult at times to determine if the patient’s double vision is due to a distinct palsy of a cranial nerve or simply to mechanical displacement of the globe secondary to orbital congestion.
Approximately 75% of CCF cases have been attributed to head trauma while 25% appear spontaneously secondary to arteriosclerosis or preexisting aneurysms.29,30 The low mortality associated with rupture of the internal carotid within the cavernous sinus is attributed to the dural and bony protection afforded by its extradural location, which prevents subarachnoid and intracerebral hemorrhage.31 However, the fistula results in the aforementioned signs and symptoms as well as diminution of flow to the more distal internal carotid artery resulting in ischemic symptoms of the cerebral hemisphere.
Tolosa-Hunt syndrome
Tolosa-Hunt syndrome is an idiopathic, sterile inflammation that primarily affects the anterior portion of the cavernous sinus. Schatz and Farmer,32 provided a comprehensive review of the historical development of the Tolosa-Hunt syndrome. They emphasized that it represents an example of the clinical description “painful ophthalmoplegia”. They also pointed out that the entity referred to as “superior orbital fissure syndrome” cannot be distinguished from cases in which the anterior cavernous sinus is involved. Other causes include trauma, syphilitic periostitis and neoplasms in the region of the superior orbital fissure.33-37 These patients present with orbital pain, ipsilateral involvement of the second through sixth cranial nerves, as well as oculosympathetic palsy (Horner syndrome). Spontaneous remission occurs in some cases after some days or weeks and the response to corticosteroid therapy is good. Histopathology of the lesion reveals chronic granulomatous reaction evidenced by the presence of epithelioid giant cell and plasma cells with necrosis but no caseation.33
Meningioma
Meningioma located along the medial aspect of the sphenoid ridge, the anterior clinoid process or the tuberculum sellae may present with clinical features described for the cavernous sinus syndrome of the sixth nerve.38 Exophthalmos and visual loss or visual field defects such as bitemporal hemianopia, monocular blindness and upper-temporal field defects in the other eye (junctional scotoma) may occur.38
Miscellaneous
A list of possible etiologies of the cavernous sinus syndrome of the sixth nerve is quite extensive and includes metastatic lesions, neurofibroma, craniopharyngioma, multiple myeloma, lymphoma, herpes zoster, temporal arteritis and syphilis.39-44 The clinician must be prepared to proceed with an extensive medical investigation when the etiology of the cavernous sinus syndrome is not determined by routine investigations including contrast neuroradiologic studies.
Orbital Syndrome of the Sixth Nerve
Proptosis is an early sign of the orbital syndrome and is frequently accompanied by congestion of conjunctival vessels and conjunctival chemosis.38,45 The optic nerve may be involved manifesting as optic atrophy or papilledema. It is frequently difficult to distinguish between cranial nerve (III, IV and VI) palsy and mechanical displacement of the globe.38 Horner syndrome may be present, but the ptosis may not be recognized because of proptosis.38 Trigeminal signs are limited to the ophthalmic and maxillary division. Such a clinical presentation may be seen with tumors of the orbit,46 orbital pseudotumor,38 thyroid eye disease, orbital cellulitis or myositis.38
Isolated Sixth Nerve Palsy Syndrome
The patient who demonstrates only lateral rectus weakness and no historical data to implicate a specific etiology, is categorized as having “isolated sixth nerve palsy”.37,47
There are often vascular risk factors such as diabetes mellitus, hypertension48,49 or history of a recent viral infection.50,51 Benign, remitting palsies do occur in children however, and may be recurrent in nature.50,51 The lesion in abducens palsy from ophthalmic migraine is variable, either central or peripheral,52 and it may be impossible in an individual case to decide which type of palsy is present if imaging studies are inconclusive.52,53 Immunologic damage to the abducens nerve may occur anywhere along its length.54 In each case, the main purpose in a case of isolated six nerve palsy is to ensure that signs and symptoms of the other five syndromes have been assessed and ruled out.
The Six Mimickers of Sixth Nerve Palsy
Before sending our patient out of the office door with his return appointment in hand, there are six bells that should ring in our minds; the six conditions that may imitate isolated lateral rectus weakness:38
Thyroid eye diseases
Myasthenia gravis
Duane’s syndrome
Spasm of the near reflex
Delayed break in fusion
Old blowout fracture of the orbit
An old contusion injury of the orbit may have resulted in fracture of the ethmoid bone (lamina papyracea) with fibrosis or entrapment of the medial rectus muscle and resultant restriction of abduction.55
This diagnosis, as well as thyroid eye disease, may be confirmed by performing a forced duction test on the affected eye. If the eye cannot be abducted passively with a cotton swab or forceps, true weakness of the lateral rectus is not present and restriction or adhesion of the medial rectus is the cause of limited abduction.56
MANAGEMENT
Once an isolated sixth nerve palsy has been established, patients can be divided into two groups: The pediatric group and the adult group.57,58 Adult patients should undergo the following initial studies:59
Blood pressure measurement
Complete blood count (CBC)
Glucose tolerance test
Sedimentation rate
Syphilis serology/VDRL
Thyroid function tests
Neuroimaging and radiological studies such as MRI with enhancement
Skull series and stereoscopic submental- vertex basal views of the skull (for nasopharyngeal carcinoma)
Chest radiography
Superior orbital fissure views
Otolaryngologic evaluation
In adults, the most likely etiology of isolated sixth nerve palsy is ischemic mononeuropathy that may be due to diabetes mellitus, arteriosclerosis, hypertension, temporal arteritis or anemia.48,49,60 CBC may also pick up an occult blood dyscrasia.
Neuroimaging evaluations are used to study areas of the skull that play roles in each of the syndromes61,62 i.e. the superior orbital fissures, the clinoid, the sella turcica and the foramina along the skull base. Baseline evaluation can be extended to include consultation with an otolaryngologist if there are sign or symptoms of nasopharyngeal or ear involvement.63-65
Indirect visualization of the nasopharynx may be sufficient, however, if symptoms are suggestive, random biopsies of the nasopharynx should be considered.64,65
Sixth nerve palsy in patients under 40 years of age warrants neuroimaging, often a tensilon test and lumbar puncture.38,47
The maximum amount of time that may be allowed for an isolated sixth nerve palsy to improve is debatable. Many improve within three to four months but some take longer.57 Some cases do improve spontaneously.66
The first aim of management in pediatric cases with isolated sixth nerve palsy should be to identify and treat the cause of the condition, where possible, and to relieve the symptoms.38,57 In children, who rarely appreciate diplopia, the aim is to maintain binocular vision and thus promote proper visual development.55,56
Challenges of management in pediatric patients have been described. Robertson4 reported that neoplasms, especially of the posterior fossa account for 39% of an entire group of 133 children with sixth nerve palsy. On the other hand, Bagheri et al7 reported that trauma accounts for 54.4% of causes among 33 children with sixth nerve palsy (Table 1). Development of an abducens nerve palsy following minimal head trauma67,68 should raise the suspicion of a compressive lesion such as a tumor,69,70 and the child should be evaluated by a pediatric neurologist to look for subtle signs of a skull base tumor. However one should keep in mind that spontaneous recovery of an abducens nerve palsy may occur even with skull base tumors or leukemia, perhaps from axonal regeneration, resorption of hemorrhage in tumors or immune response to the tumor.63,71
Symptom Relief and/or Binocular Vision Maintenance
This goal is most commonly achieved through the use of Fresnel prisms.72 These slim flexible plastic prisms can be attached to the patients’ glasses, or onto plano glasses if the patient has no refractive error, and serve to compensate for a fixed degree of misalignment. As an affected individual’s degree of misalignment will vary depending upon the direction of gaze, they may still experience diplopia when looking to the affected side.
Other management options at this initial stage include the use of botulinum toxin (BT), which is injected into the ipsilateral medial rectus.73 The use of BT serves a number of purposes. Firstly, it helps to prevent contracture of the medial rectus. Secondly, by reducing the size of the deviation temporarily, it might allow prismatic correction to be used if this was not previously possible.74
CONCLUSION
Considering the long course of the sixth cranial nerve from the brainstem to the lateral rectus muscle, and depending on the location of the abnormality, other neurologic signs may accompany sixth nerve palsy. Sixth nerve palsy may not always be due to a benign process that permits full return of function within months. Hence, the clinician must consider the potential of a serious neurologic process when evaluating sixth nerve palsy. Early diagnosis is often critical in some conditions that present with sixth nerve palsy.
Acknowledgments
The authors would like to thank Dr. Ramin Sahebghalam for his cooperation in composing the figures of this manuscript.
Footnotes
Conflicts of Interest
None.
REFERENCES
- 1.Shrader EC, Schlezinger NS. Neuro- ophthalmologic evaluation of abducens nerve paralysis. Arch Ophthalmol. 1960;63:84–91. doi: 10.1001/archopht.1960.00950020086013. [DOI] [PubMed] [Google Scholar]
- 2.Rucker CW. The causes of paralysis of the third, forth, and sixth cranial nerves. Am J Ophthalmol. 1966;61:1293–1298. doi: 10.1016/0002-9394(66)90258-3. [DOI] [PubMed] [Google Scholar]
- 3.Johnston AC. Etiology and treatment of abducens paralysis. Trans Pac Coast Otoophthalmol Soc Annu Meet. 1968;49:259–277. [PubMed] [Google Scholar]
- 4.Robertson DM, Hines JD, Rucker CW. Acquired sixth-nerve paresis in children. Arch Ophthalmol. 1970;83:574–579. doi: 10.1001/archopht.1970.00990030574008. [DOI] [PubMed] [Google Scholar]
- 5.Rush JA, Younge BR. Paralysis of cranial nerves III, IV, and VI. Cause and prognosis in 1000 cases. Arch Ophthalmol. 1981;99:76–79. doi: 10.1001/archopht.1981.03930010078006. [DOI] [PubMed] [Google Scholar]
- 6.Patel SV, Mutyala S, Leske DA, Hodge DO, Holmes JM. Incidence, associations, and evaluation of sixth nerve palsy using a population-based method. Ophthalmology. 2004;111:369–375. doi: 10.1016/j.ophtha.2003.05.024. [DOI] [PubMed] [Google Scholar]
- 7.Bagheri A, Babsharif B, Abrishami M, Salour H, Aletaha M. Outcomes of surgical and non-surgical treatment for sixth nerve palsy. J Ophthalmic Vis Res. 2010;5:32–37. [PMC free article] [PubMed] [Google Scholar]
- 8.Galetta SL, Smith JL. Chronic isolated sixth nerve palsies. Arch Neurol. 1989;46:79–82. doi: 10.1001/archneur.1989.00520370081024. [DOI] [PubMed] [Google Scholar]
- 9.Miller NR, Biousse V, Hwang T, Patel S, Newman NJ, Zee DS. Isolated acquired unilateral horizontal gaze paresis from a putative lesion of the abducens nucleus. J Neuroophthalmol. 2002;22:204–207. doi: 10.1097/00041327-200209000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Depper MH, Truwit CL, Dreisbach JN, Kelly WM. Isolated abducens nerve palsy: MR imaging findings. AJR Am J Roentgenol. 1993;160:837–841. doi: 10.2214/ajr.160.4.8456676. [DOI] [PubMed] [Google Scholar]
- 11.Pane A, Burdon MA, Miller NR. The neuro- ophthalmology survival guide. London: Elsevier Health Sciences; 2007. [Google Scholar]
- 12.Kline LB. Neruro-ophthalmology review manual. 6th ed. Thorofare, NJ: Slack Incorporated; 2007. [Google Scholar]
- 13.Büttner-Ennever JA, Büttner U. Neuroanatomy of the ocular motor pathways. Baillieres Clin Neurol. 1992;1:263–287. [PubMed] [Google Scholar]
- 14.Schmidt D. Classical brainstem syndrome. Definitions and history. Ophthalmologe. 2000;97:411–417. doi: 10.1007/s003470070090. [DOI] [PubMed] [Google Scholar]
- 15.Krasnianski M, Neudecker S, Zierz S. Classical crossed pontine syndromes. Fortschr Neurol Psychiatr. 2004;72:460–468. doi: 10.1055/s-2004-818392. [DOI] [PubMed] [Google Scholar]
- 16.Silverman IE, Liu GT, Volpe NJ, Galetta SL. The crossed paralyses. The original brain-stem syndromes of Millard-Gubler, Foville, Weber, and Raymond-Cestan. Arch Neurol. 1995;52:635–638. doi: 10.1001/archneur.1995.00540300117021. [DOI] [PubMed] [Google Scholar]
- 17.Kurbanyan K, Lessell S. Intracranial hypotension and abducens palsy following upper spinal manipulation. Br J Ophthalmol. 2008;92:153–155. doi: 10.1136/bjo.2007.119313. [DOI] [PubMed] [Google Scholar]
- 18.Anwar S, Nalla S, Fernando DJ. Abducens nerve palsy as a complication of lumbar puncture. Eur J Intern Med. 2008;19:636–637. doi: 10.1016/j.ejim.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 19.Kuhl V, Andreas J, Müller-Forell W, Thömke F, Hopf HC. Spontaneous intracranial hypotension syndrome in cervicothorackc cerebrospinal fluid leak. Nuklearmedizin. 2000;39:N22–24. [PubMed] [Google Scholar]
- 20.Krishna R, Kosmorsky GS, Wright KW. Pseudotumor cerebri sine papilledema with unilateral sixth nerve palsy. J Neuroophthalmol. 1998;18:53–55. [PubMed] [Google Scholar]
- 21.Kim L, Glantz MJ. Neoplastic meningitis. Curr Treat Options Oncol. 2001;2:517–527. doi: 10.1007/s11864-001-0073-x. [DOI] [PubMed] [Google Scholar]
- 22.Gradenigo G. A special syndrome of endocranial otitic complications (paralysis of the motor oculi externus of otitic origin). Ann Otol. 1904;13:637–639. [Google Scholar]
- 23.Reinhardt F, Lange E. The vascular cerebellopontile angle syndrome. Psychiatr Neurol Med Psycho (Leipz) 1997;29:266–274. [PubMed] [Google Scholar]
- 24.Takami T, Ohata K, Tsuyuguchi N, Mao Y, Inoue Y, Wakasa K, et al. Cavernous sinus metastasis from thyroid papillary adenocarcinoma. J Clin Neurosci. 2002;9:598–600. doi: 10.1054/jocn.2002.1101. [DOI] [PubMed] [Google Scholar]
- 25.Dare AO, Gibbons KJ, Proulx GM, Fenstermaker RA. Resection followed by radiosurgery for advanced juvenile nasopharyngeal angiofibroma: report of two cases. Neurosurgery. 2003;52:1207–1211. [PubMed] [Google Scholar]
- 26.Killer HE, Matzkin DC, Sternman DC, Jahre C, Burde RM. Intracavernous carotid aneurysm as a rare case of isolated sixth nerve palsy in an eight- year-old child. Neuro-Ophthalmol. 1993;13:147–150. [Google Scholar]
- 27.O’Connor PS, Glaser JS. Intracavernous aneurysms and isolated sixth nerve palsy. In: smith JL, editor. Neuro-ophthalmology Focus. New York: Masson; 1981. pp. 155–159. [Google Scholar]
- 28.Locksley HB. Natural history of subarachnoid hemorrhage, intracranial aneurysms and arteriovenous malformations. Based on 6368 cases in the cooperative study. J Neurosurg. 1966;25:219–239. doi: 10.3171/jns.1966.25.2.0219. [DOI] [PubMed] [Google Scholar]
- 29.Biosse V. Cerebrovascular disease. In: Miller NR, Nowman NJ, editors. Walsh & Hoyt’s clinical neuro- ophthalmology. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 30.Brismar G, Brismar J. Spontaneous carotid- cavernous fistulas. Clinical symptomatology. Acta Ophthalmol (Copenh) 1976;54:542–552. doi: 10.1111/j.1755-3768.1976.tb01284.x. [DOI] [PubMed] [Google Scholar]
- 31.Lewis AI, Tomsick TA, Tew JM. Management of 100 consecutive direct carotid-cavernous fistulas: results of treatment with detachable balloons. Neurosurgery. 1995;36:239–244. doi: 10.1227/00006123-199502000-00001. [DOI] [PubMed] [Google Scholar]
- 32.Schatz NJ, Farmer P. Tolosa- Hunt syndrome: the pathology of painful ophthalmoplegia. In: Smith JL, editor. Neuro-ophthalmology. St. Louis: C.V. Mosby; 1972. [Google Scholar]
- 33.Campbell RJ, Okazaki H. Painful ophthalmoplegia (Tolosa-Hunt variant): autopsy findings in a patient with necrotizing intracavernous carotid vasculitis and inflammatory disease of the orbit. Mayo Clin Proc. 1987;62:520–526. doi: 10.1016/s0025-6196(12)65478-0. [DOI] [PubMed] [Google Scholar]
- 34.Klin LB. The Tolosa-Hunt syndrome. Surv Ophthalmol. 1982;27:79–95. doi: 10.1016/0039-6257(82)90190-4. [DOI] [PubMed] [Google Scholar]
- 35.Klin LB, Hoyt WF. The Tolosa-Hunt syndrome. J Neurol Neurosurg Psychiatry. 2001;7:577–582. doi: 10.1136/jnnp.71.5.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Acierno MD, Trobe JD, Cornblath WT, Gebarski SS. Painful oculomotor palsy caused by posterior- draining dural carotid cavernous fistulas. Arch Ophthalmol. 1995;113:1045–1049. doi: 10.1001/archopht.1995.01100080097035. [DOI] [PubMed] [Google Scholar]
- 37.Moster ML. Paresis of isolated and multiple cranial nerves and painful ophthalmologia. In: Yanoff M, Ducker JS, editors. Ophthalmology. 2nd ed. St Louis: Mosby; 2004. [Google Scholar]
- 38.Kline LB, Bhatti MT, Chung SM, Eggenberger E, Foroozan R. Basic and clinical science course; Neuro-ophthalmology. San Francisco: American Academy of Ophthalmology; 2010-2011. [Google Scholar]
- 39.Sakalas R, Harbison JW, Vines FS, Becker DP. Chronic sixth nerve palsy. An initial sign of basisphenoid tumors. Arch Ophthalmol. 1975;93:186–190. doi: 10.1001/archopht.1975.01010020194005. [DOI] [PubMed] [Google Scholar]
- 40.Eisenberg MB, Al-Mefty O, DeMonte F, Burson GT. Benign nonmeningeal tomurs of the cavernous sinus. Neurosurgery. 1999;44:949–955. doi: 10.1097/00006123-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 41.Iwai Y, Yamanaka K, Ishiguro T. Gamma knife radiosurgery for the treatment of cavernous sinus meningiomas. Neurosurgery. 2003;52:517–524. doi: 10.1227/01.neu.0000047814.18819.9f. [DOI] [PubMed] [Google Scholar]
- 42.Zorlu F, Yildiz F, Ertoy D, Atahan IL, Erden E. Dermatofibrosarcoma protuberans metastasizing to cavernous sinuses and lungs: a case report. Jpn J Clin Oncol. 2001;31:557–561. doi: 10.1093/jjco/hye117. [DOI] [PubMed] [Google Scholar]
- 43.Dufour H, Diaz A, Metellus P, Fuentes S, Chinot O, Figarella-Branger D, et al. Burkitt lymphoma of the cavernous sinus. Apropos of a case. Neurochirurgie. 2001;47:564–567. [PubMed] [Google Scholar]
- 44.Arimoto H, Shirotani T, Nakau H, Hashizume K, Sakai Y, Matsukuma S. Primary malignant lymphoma of the cavernous sinus--case report. Neurol Med Chir (Tokyo) 2000;40:275–279. doi: 10.2176/nmc.40.275. [DOI] [PubMed] [Google Scholar]
- 45.Mombaerts I, Goldschmeding R, Schlingemann RO, Koornneef L. What is orbital pseudotumor? Surv Ophthalmol. 1996;41:66–78. doi: 10.1016/s0039-6257(97)81996-0. [DOI] [PubMed] [Google Scholar]
- 46.Rootman J, Goldberg C, Robertson W. Primary orbital schwannomas. Br J Ophthalmol. 1982;66:194–204. doi: 10.1136/bjo.66.3.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moster ML, Savino PJ, Sergott RC, Bosley TM, Schatz NJ. Isolated sixth nerve palsies in younger adults. Arch Ophthalmol. 1984;102:1328–1330. doi: 10.1001/archopht.1984.01040031078029. [DOI] [PubMed] [Google Scholar]
- 48.Jacobson DM, McCanna TD, Layde PM. Risk factors for ischemic ocular motor nerve palsies. Arch Ophthalmol. 1994;112:961–966. doi: 10.1001/archopht.1994.01090190109029. [DOI] [PubMed] [Google Scholar]
- 49.Kobashi R, Ohtsuki H, Hasebe S. Clinical studies of ocular motility disturbances: Part 2. Risk factors for ischemic ocular motor nerve palsy [corrected]. Jpn J Ophthalmol. 1997;41:115–119. doi: 10.1016/s0021-5155(97)00006-3. [DOI] [PubMed] [Google Scholar]
- 50.Cohen HA, Nussinovitch M, Ashkenazi A, Straussberg R, Kaushansky A. Benign abducens nerve palsy of childhood. Pediatr Neurol. 1993;9:394–395. doi: 10.1016/0887-8994(93)90110-x. [DOI] [PubMed] [Google Scholar]
- 51.Vallee L, Guilbert F, Lemiatre JF, Nuyts JP. Benign paralysis of the 6th cranial nerve in children. Ann Pediatr (Paris) 1990;37:303–305. [PubMed] [Google Scholar]
- 52.Lee TG, Choi WS, Chung KC. Ophthalmoplegic migraine with reversible enhancement of intraparenchymal abducens nerve on MRI. Headache. 2002;42:140–141. doi: 10.1046/j.1526-4610.2002.02031.x. [DOI] [PubMed] [Google Scholar]
- 53.De Renzi E, Nichelli P. Ophthalmoplegic migraine with persistent abducens nerve palsy. Eur Neurol. 1977;15:227–230. doi: 10.1159/000114837. [DOI] [PubMed] [Google Scholar]
- 54.Barr D, Kupersmith MJ, Turbin R, Bose S, Roth R. Isolated sixth nerve palsy: an uncommon presenting sign of multiple sclerosis. J Neurol. 2000;247:701–704. doi: 10.1007/s004150070114. [DOI] [PubMed] [Google Scholar]
- 55.Borchert MS. Principles and techniques of the examinations of ocular motility and alignment. In: Miller NR, Neumann NJ, editors. Clinical neuro- ophthalmology. 6th ed. Philadelphia: Lippincott, Williams & Wilkins; 2005. [Google Scholar]
- 56.Von Noorden GK, Campos EC. Binocular vision and ocular motility. 6th ed. New York: Mosby; 2002. [Google Scholar]
- 57.Harley RD. Paralytic strabismus in children. Etiologic incidence and management of the third, fourth, and sixth nerve palsies. Ophthalmology. 1980;87:24–43. doi: 10.1016/s0161-6420(80)35280-9. [DOI] [PubMed] [Google Scholar]
- 58.Sowka J, Gurwood AS, Kabat A. Handbook of ocular disease management. Jobson Publishing L.L.C.; 2000. [Google Scholar]
- 59.Rhee DJ, Pyfer MD. The Wills Eye Manual: office and emergency room diagnosis and treatment of eye disease. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 1999. [Google Scholar]
- 60.Asbury AK, Aldredge H, Hershberg R, Fisher CM. Oculomotor palsy in diabetes mellitus: a clinico- pathological study. Brain. 1970;93:555–566. doi: 10.1093/brain/93.3.555. [DOI] [PubMed] [Google Scholar]
- 61.Bendszus M, Beck A, Koltzenburg M, Vince GH, Brechtelsbauer D, Littan T, et al. MRI in isolated sixth nerve palsies. Neuroradiology. 2001;43:742–745. doi: 10.1007/s002340100572. [DOI] [PubMed] [Google Scholar]
- 62.Lee AG, Eggenberger E, Golnik K, Miller NR. MRI in isolated sixth nerve palsies. Neuroradiology. 2002;44:711–712. doi: 10.1007/s00234-002-0769-z. [DOI] [PubMed] [Google Scholar]
- 63.Volpe NJ, Lessell S. Remitting sixth nerve palsy in skull base tumors. Arch Ophthalmol. 1993;111:1391–1395. doi: 10.1001/archopht.1993.01090100099035. [DOI] [PubMed] [Google Scholar]
- 64.Godtfredsen E, lederman M. Diagnostic and prognostic roles of ophthalmoneurologic signs and symptoms in malignant nasopharyngeal tumors. Am J Ophthalmol. 1965;59:1063–1069. [PubMed] [Google Scholar]
- 65.Jing BS. Tumors of the nasopharynx. Radiol Clin North Am. 1970;3:323–342. [PubMed] [Google Scholar]
- 66.King AJ, Stacey E, Stephenson G, Trimble RB. Spontaneous recovery rates for unilateral sixth nerve palsies. Eye (Lond) 1995;9:476–478. doi: 10.1038/eye.1995.110. [DOI] [PubMed] [Google Scholar]
- 67.Calisaneller T, Ozdemir O, Altinors N. Posttraumatic acute bilateral abducens nerve palsy in a child. Childs Nerv Syst. 2006;22:726–728. doi: 10.1007/s00381-005-0036-9. [DOI] [PubMed] [Google Scholar]
- 68.Dwarakanath S;, Gopal S, Venkataramana NK. Post-traumatic bilateral abducens nerve palsy. Neurol India. 2006;54:221–222. [PubMed] [Google Scholar]
- 69.Currie J, Lubin JH, Lessell S. Chronic isolated abducens paresis from tumors at the base of the brain. Arch Neurol. 1983;40:226–229. doi: 10.1001/archneur.1983.04050040056009. [DOI] [PubMed] [Google Scholar]
- 70.Depper MH, Truwit CL, Dreisbach JN, Kelly WM. Isolated abducens nerve palsy: MR imaging findings. AJR Am J Roentgenol. 1993;160:837–841. doi: 10.2214/ajr.160.4.8456676. [DOI] [PubMed] [Google Scholar]
- 71.Wolfe GI, Galetta SL, Mollman JE. Spontaneous remission of papilledema and sixth nerve palsy in acute lymphoblastic leukemia. J Neuroophthalmol. 1994;14:91–94. doi: 10.3109/01658109409024031. [DOI] [PubMed] [Google Scholar]
- 72.American Academy of Ophthalmology . Basic and clinical science course; Pediatric ophthalmology and strabismus. San Francisco: American Academy of Ophthalmology; 2010-2011. [Google Scholar]
- 73.Lee J, Harris S, Cohen J, Cooper K, MacEwen C, Jones S. Results of a prospective randomized trial of botulinum toxin therapy in acute unilateral sixth nerve palsy. J Pediatr Ophthalmol Strabismus. 1994;31:283–286. doi: 10.3928/0191-3913-19940901-03. [DOI] [PubMed] [Google Scholar]
- 74.Repka MX, Lam GC, Morrison NA. The efficacy of botulinum neurotoxin A for the treatment of complete and partially recovered chronic sixth nerve palsy. J Pediatr Ophthalmol Strabismus. 1994;31:79–83. doi: 10.3928/0191-3913-19940301-04. [DOI] [PubMed] [Google Scholar]