Abstract
The behavioral phenotype of 47,XXY (Klinefelter syndrome) includes increased risks for developmental delays, language-based learning disabilities, executive dysfunction/ADHD, and social-emotional difficulties. However there is significant variability between individuals with 47,XXY, and many children and adolescents have minimal or no behavioral features while others have quite significant involvement. This paper describes behavioral features in a cohort of 57 children and adolescents with 47,XXY, including results on standardized measures of behavior (BASC-2), attention (Conner’s Rating Scales), and social skills (Social Responsiveness Scale). A subset was directly assessed for autism spectrum disorders using the ADOS and ADI-R. We discuss our results within the context of previous literature, including implications for genetic counseling, recommendations for care, and areas for future research.
Keywords: XXY, Klinefelter syndrome, behavioral phenotype, ADHD, autism, social skills, genetic counseling
Introduction
47,XXY, or Klinefelter syndrome, was initially described in 1942 by Dr. Harry Klinefelter, an adult endocrinologist, who identified a cohort of post-pubertal males presenting with infertility, hypogonadism, gynecomastia and increased gonadotropin levels (1). An extra X chromosome in males was found to be the cause of Klinefelter syndrome in 1959 (2). Since the initial description, further studies have demonstrated KS to have a broad clinical phenotype that also includes neurodevelopmental and psychological features. The prevalence of XXY is approximately 1/650 males based on large newborn screening studies (3, 4); however there is a much lower rate of diagnosis in the general population. A population study showed that approximately 10% of identified cases of XXY are diagnosed prenatally, 3% are identified before age 20 due to developmental delays and behavioral problems, and 2% are diagnosed in adolescence due to hypogonadism or gynecomastia (5). An additional 17% are diagnosed in adulthood due to hypogonadism or infertility, leaving the remaining 68% of males with XXY undiagnosed throughout their lifetime (6). This low frequency of ascertainment is believed to be partially due to the broad spectrum of physical features and psychological findings seen in the clinical phenotype of XXY.
Physical features and medical problems in adolescents and adults with XXY include tall stature, hypergonadotropic hypogonadism, and fertility problems. In addition to the physical and medical findings, children and adolescents with an XXY karyotype may present with a variety of developmental and behavioral features that make up the behavioral phenotype of XXY. The behavioral phenotype of XXY includes increased prevalence of developmental delays, verbal cognition and language impairments, reading disabilities, and various behavioral and emotional differences. A systematic review of neurocognitive outcomes in cohorts of patients with XXY ascertained at birth by newborn screening showed that overall mean cognitive abilities on standardized tests of intelligence were in the average range, however mean verbal cognitive scores were approximately 10 points lower than performance scores, and significantly decreased in relation to comparison groups (7). In a review by Bender et al, cognitive scores in XXY are represented as falling in a normal distribution, but with the mean score shifted slightly to the left. This demonstrates that the spectrum of cognitive abilities across individuals with XXY closely overlaps that in the general population, but with a slightly larger percentage of the population with scores in the low average and borderline ranges (See Figure 1) (8). Studies consistently show mean verbal cognitive abilities in the low average range with elevated risks for academic difficulties and language based learning disabilities. Academic difficulties of mild to more significant severity are found in 60–85% of individuals with XXY (9–11).
Figure 1.
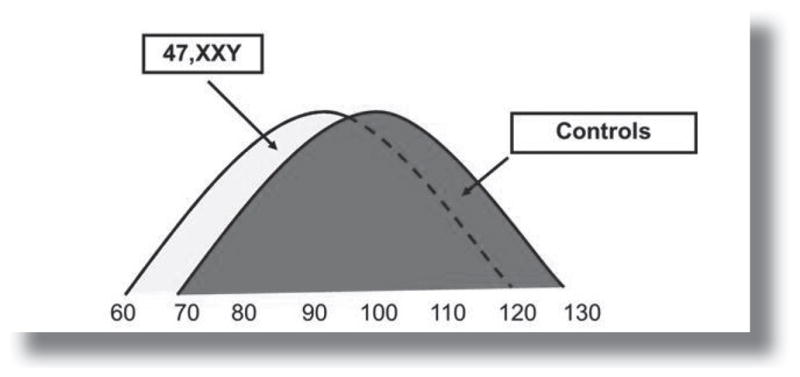
Estimated Full-Scale IQ (FSIQ) distribution for individuals with 47, XXY compared to controls. Adapted and reprinted with permission from Bender et al, 1986.
Consistent with the cognitive risks seen in XXY, many studies also describe vulnerabilities in the psychological domain as well, including attentional problems and Attention-Deficit/ Hyperactivity Disorder (ADHD), anxiety, depression, social difficulties including autism spectrum disorders, and other psychiatric disorders. These behavioral and emotional disorders have been described in prenatally diagnosed samples, newborn screening studies, and clinically ascertained cases of 47,XXY (12–17), however, when describing behavioral features, most studies have reported on historical diagnoses by parent-provided history or medical records, rather than on direct assessment of individuals with XXY. In this report, we aim to further describe the spectrum of the behavioral phenotype in a group of children and adolescents age 6 to 21 years with XXY, including results on standardized measures of behavior, attention and social skills. We discuss our results within the context of previous literature, including implications for genetic counseling, recommendations for care, and areas for future research.
Methods
Sample
Participants were recruited for a study on health and development in all forms of supernumerary sex chromosome aneuploidy through national advocacy groups for males with XXY (KS&A, AAKSIS) and through clinics in developmental pediatrics, endocrinology, genetics, and general pediatrics at the UC-Davis MIND Institute and The Children’s Hospital in Denver from 2005–2010. From this larger cohort, 57 children and adolescents age 6 to 21 years with a karyotype of 47,XXY were included in this analysis. The study was approved by the Institutional Review Boards at each institution. The parents of all participants signed informed consent, and participants provided assent.
Assessments
The assessment battery included both individually administered psychological tests, as well as parent-completed questionnaires. To assess overall cognitive ability, participants were administered either the Wechsler Intelligence Scale for Children- Fourth Edition (WISC-IV) (18) or the Wechsler Abbreviated Scale of Intelligence (WASI) (19). The parents or primary caretakers of all participants completed a battery of standardized questionnaires to assess behavioral and emotional features, attentional problems, and social skills. A subset of patients also participated in a sub-study of social development and directly evaluated for autism spectrum disorders. This subset included 20 sequential patients seen during a specified time period from 2006–2007. There were not additional inclusion or exclusion criteria or screenings for participation in this sub-study. All measures are further described below and were scored via standard procedures for each scale.
The Parent Rating Scale (PRS) of the BASC and BASC-2 includes 134–160 items (depending on the age of the child) assessing behavioral, emotional, and adaptive functioning (20, 21). Items are rated on a four-point scale of frequency ranging from “Never” to “Almost Always.” The forms for children 6 to 11 and adolescents age 12 to 21 years were used. Parent responses yield scores for 9 clinical scales (Hyperactivity, Aggression, Conduct Problems, Anxiety, Depression, Somatization, Attention Problems, Atypicality, Withdrawal) and 5 adaptive behavior scales (Adaptability, Social Skills, Leadership, Activities of Daily Living, Functional Communication). Normative T scores are calculated for each scale, with a mean of 50 and a standard deviation of 10. Descriptive score classifications are provided for both the clinical and adaptive scales. For clinical scales, higher scores are considered at-risk (60–69) or clinically significant (>70), while for adaptive scales, lower scores are considered at-risk (30–39) or clinically significant (<30).
Assessment of ADHD symptoms was completed using either the Conners’ Parent Rating Scale (22) or the SNAP-IV (23), which each contain the Diagnostic and Statistical Manual-IV (DSM-IV) (24) diagnostic criteria for ADHD. Subjects were determined to meet criteria for ADHD if they were noted to have moderate to severe symptoms in 6 of the 9 inattentive items (ADHD-Inattentive subtype), or in 6 of the 9 items in both inattentive and hyperactive/impulsive domains (ADHD-Combined subtype).
Social skills were assessed using the Social Responsiveness Scale (SRS), a parent report questionnaire used to quantify social skills across different domains and to provide quantitative measures of symptomatology of autism and the broader autism phenotype (25). The SRS contains 65 items in 5 domains including social awareness, social cognition, social communication, social motivation, and autistic mannerisms. Scores are reported as T scores, with a mean of 50 and a standard deviation of 10. Scores between 60 and 75 are in the “mild to moderate” range of severity, and scores of 76 or above are in the “severe” range. As described earlier, a subset of patients (n=20) was directly evaluated for autism spectrum disorders using the Autism Diagnostic Observation Schedule (ADOS) and the Autism Diagnostic Interview – Revised (ADI-R) (26, 27). The ADOS is a semi-structured assessment using developmentally appropriate social and play-based interactions in a 40–60 minute session designed to elicit symptoms of autism. The ADI-R is a semi-structured standardized parent interview developed to assess the presence and severity of autism symptoms throughout childhood. The combination of the ADOS and ADI-R are considered the ‘gold standard’ for a research diagnosis of autism.
Results
Study Participants
A total of 57 participants with 47,XXY from age 6 to 21 years (M= 12.26; SD= 4.33) were included. A description of sample characteristics including age, race, ethnicity, cognitive scores, and timing of ascertainment are shown in Table 1. Forty-six percent of the group was diagnosed in the prenatal period, while the remaining 54% were diagnosed postnatally due to presence of developmental or academic concerns (35%) or endocrine findings related to hypogonadism or gynecomastia (19%). Cognitive data were obtained from 40 participants using either the WISC-IV (n= 17) or the WASI (n= 23), with a mean Full Scale IQ score of 95.2 (SD= 17.91).
Table 1.
Description of study participants
| XXY (n=57) | |||
|---|---|---|---|
| Mean | SD | Range | |
| Age in years | 12.26 | 4.33 | 6–20 |
| IQ (n= 40) | 95.2 | 17.91 | 40–125 |
| Ethnicity | 7 % Hispanic or Latino | ||
| Race | 96% White; 2% African-American; 2% Asian | ||
| Ascertainment | 46% prenatal diagnosis (n=26) 54% postnatal diagnosis (n=31) Developmental or academic concerns (35%) Hypogonadism or gynecomastia (19%) |
||
Behavior Assessment System for Children
Parents or primary caregivers completed the PRS of either the BASC (n= 23) or BASC-2 (n= 34). Given the high correlation between the BASC and BASC-2 (Reynolds & Kamphaus, 2004), commensurate scales from the two measures were combined to assess overall group performance. However, the BASC-2 includes two adaptive scales not in the original version, Functional Communication and Activities of Daily Living. As such, scores for these two scales represent only the 34 participants whose parents completed the BASC-2. A summary of means and standard deviations for the total group on these measures combined is provided in Table 2. As shown in Table 2, mean BASC/BASC-2 scores for the entire group are generally in the average range for both clinical and adaptive scales, with the exception of the Withdrawal and Functional Communication scales, which are both in the At-Risk range.
Table 2.
Means and standard deviations for BASC scales.
| BASC Scale | Mean | SD |
|---|---|---|
| Clinical Scales | ||
| Hyperactivity | 50.32 | 12.42 |
| Aggression | 49.67 | 10.71 |
| Conduct Problems | 52.72 | 12.82 |
| Anxiety | 53.81 | 12.81 |
| Depression | 55.44 | 12.75 |
| Somatization | 57.84 | 17.04 |
| Atypicality | 52.91 | 11.52 |
| Withdrawal | 60.09 | 14.66 |
| Attention Problems | 58.05 | 10.73 |
| Externalizing Composite | 51.32 | 12.32 |
| Internalizing Composite | 56.98 | 13.88 |
| Behavioral Symptoms Index | 55.12 | 11.81 |
| Adaptive Scales | ||
| Adaptability | 45.40 | 11.19 |
| Social Skills | 44.21 | 11.90 |
| Leadership | 42.21 | 10.87 |
| Activities of Daily Living | 41.03 | 11.46 |
| Functional Communication | 39.09 | 10.64 |
| Adaptive Skills Composite | 41.98 | 11.49 |
To further explore the distribution of the group’s performance, scores were classified into Average, At-Risk, or Clinically Significant ranges according to the scheme provided by the test’s authors (Reynolds & Kamphaus, 2004).
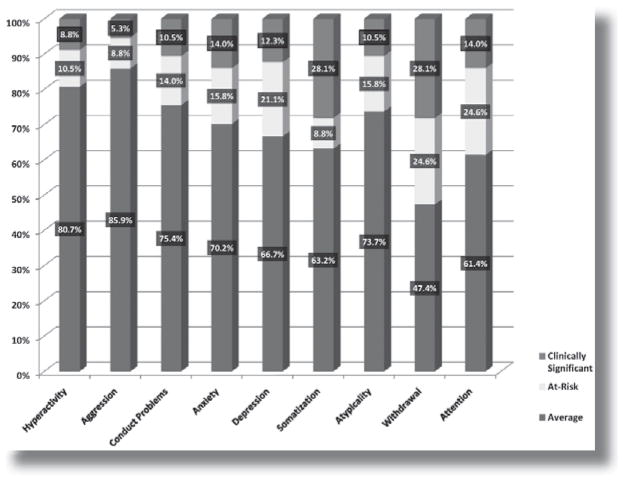
As demonstrated in Figure 2, a majority of the sample obtained Average range scores on the clinical scales, with the exception of the Withdrawal scale, where only 47.4% of the group obtained an average score. However, for 6 of the subscales (Anxiety, Depression, Somatization, Atypicality, Withdrawal, and Attention Problems) a relatively significant portion of the sample (at least 25%) obtained scores in the At-Risk or Clinically Significant ranges, with over half of the sample (52.7%) obtaining an At-Risk or Clinically significant score on the Withdrawal scale.
Figure 2.
Distribution of scores on the clinical scales of the BASC
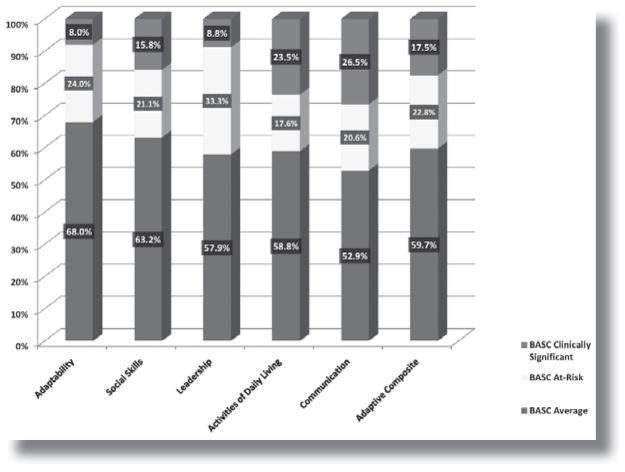
This pattern is even more apparent for the adaptive (life skills) scales, as documented in Figure 3. Again, the majority of the sample obtained scores in the average range. However, on all adaptive scales, at least 30% of the sample obtained either At-Risk or Clinically Significant scores, and almost half of the sample (47.1%) had scores in these ranges on the Functional Communication scale.
Figure 3.
Distribution of scores on the adaptive scales of the BASC.
ADHD Rating Scales
To further explore attentional concerns and to determine if the severity of attentional difficulties was such to consider a diagnosis of ADHD, standardized rating scales that included the DSM-IV criteria for a diagnosis of ADHD were completed by parents or caregivers (n=56). Categorical diagnoses of no ADHD, ADHD-Inattentive subtype, and ADHD-Combined subtype are included in Figure 4. Overall, 36% met criteria for ADHD. While 34% showed predominantly inattentive symptoms, only 2% demonstrated combined inattentive and hyperactive/impulsive symptoms.
Figure 4.
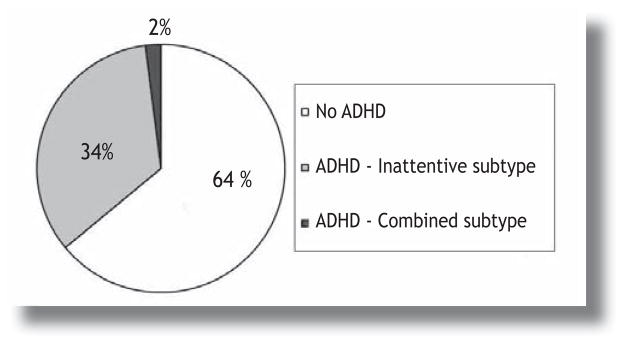
Categorical diagnosis of ADHD in 47,XXY based on parent report of DSM-IV ADHD diagnostic criteria
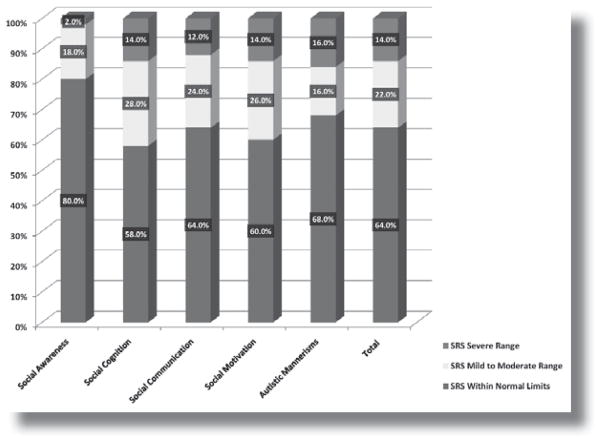
Social Responsiveness Scale and Autism Assessment
The SRS was completed by parents or primary caregivers for 42 of the participants. Overall, scores were in the normal range for over 50% of the group across all domains of the SRS. However, over 25% of the participants obtained scores in the mild-to-moderate or severe range in all domains of social responsiveness with the exception of social awareness. These scores indicate an increased risk for social difficulties in a large percentage of participants with XXY, and this high proportion of individuals with deficits in domains of social cognition, social communication, social motivation, and autistic mannerisms raises questions as to whether these participants may also meet criteria for diagnosis of an autism spectrum disorder (ASD).
A subset of 20 sequential participants was directly assessed for ASD using the ADOS and ADIR. Based on this assessment, only 1 participant met criteria for an autism spectrum disorder (Pervasive Developmental Disorder – Not otherwise specified; PDD-NOS). These results are presented in Figure 6. Of the remaining 19 who did not reach diagnostic criteria for ASD, 42% were found to have significant deficits in either communication or reciprocal social interactions but did not have the severity or quantity of deficits across both domains needed for a categorical diagnosis of ASD.
Figure 6.
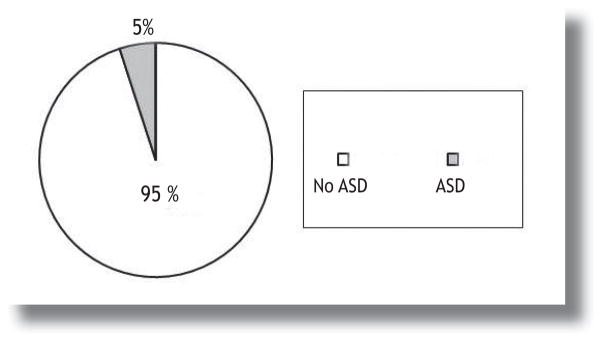
Categorical diagnosis of autism spectrum disorders in a subset of 20 participants assessed using the ADOS and ADI-R.
Discussion
The goal of this review is to represent the spectrum of the behavioral phenotype in male children and adolescents diagnosed with 47, XXY, and to describe areas of both strength and risk in this genetic condition in order to inform treatment recommendations and genetic counseling. As with any study describing a cohort of participants ascertained by recruitment into research, there are multiple sources of bias that must be considered to determine if a study sample is indeed representative of the population of interest. The prospective newborn screening studies of the 1970’s and 1980’s conducted at various sites around the world were the most comprehensive studies to date of the developmental and behavioral phenotype of 47,XXY, with the least influence of ascertainment and recruitment biases (8, 15, 28, 29). These studies demonstrated the increased risks for language deficits and verbal cognitive impairments, as well as behavioral difficulties such as attentional problems, shyness and social withdrawal, and social difficulties. However, with the lack of additional large scale newborn screening projects, researchers today who wish to expand upon these findings and inform clinical recommendations generally rely upon smaller sample sizes that are often recruited through national advocacy groups or clinical samples as we have done in this study. While some studies propose that an unbiased alternative to the newborn screening study is to include only those ascertained in the prenatal period, there is bias toward improved outcomes in a prenatal sample, as this group tends to have higher socioeconomic status and higher familial cognitive abilities. Furthermore, there is an increased likelihood of developmental screenings and early interventions with a known genetic diagnosis (30, 31). This argues for inclusion of both prenatally and postnatally diagnosed participants to capture the complete spectrum of XXY.
Although there may be bias in our study results if conclusions are generalized to all 1:650 males who have 47, XXY, if one considers that there is a diagnosis rate of approximately 15–20% prior to adulthood (with about half of these diagnosed in the prenatal period), generalizing results of our study to a population of pediatric and adolescent males diagnosed with XXY is appropriate. Our XXY sample follows a comparable pattern to the pediatric and adolescent patients described in Abramsky and Chappel’s population study, with approximately 50% with a prenatal diagnosis, and those in the postnatally diagnosed group less than 20 years of age ascertained due to either developmental delays or endocrine findings of hypogonadism/gynecomastia in an approximately 2:1 ratio (6). Additionally, the mean cognitive score (95.2) and standard deviation (17.9) in our sample are consistent with other studies in large cohorts with XXY and similar to what is demonstrated in Figure 1 (8, 32). Thus, we present these results as generally representative of the behavioral phenotype in the diverse group of child and adolescent males who have been diagnosed with XXY.
In examining the spectrum of behavioral and emotional functioning of our sample, several important points emerge. First, boys with XXY generally demonstrate average behavioral and emotional functioning, with the vast majority of the sample obtaining average scores on scales of the BASC assessing both internalizing and externalizing behaviors. However, an equally important finding is that a significant percentage of the sample, at least 25%, endorsed concerns in the areas of anxiety, depression, and somatic complaints, and over 50% reported concerns regarding social withdrawal. In contrast, problems with hyperactivity and aggressive behaviors were uncommon. These findings suggest that while most boys with XXY do not fall in the at-risk or clinically significant for behavioral symptoms of psychiatric disorders, a significant percentage exhibit some characteristics of internalizing distress, which may impact both their self-esteem and their daily functioning.
Indeed, similar findings were noted in the realm of adaptive functioning on the BASC, with average overall group performance, but with at least 30% of the sample endorsing concerns with adaptability, social skills, leadership, and activities of daily living. Almost half of the parents reported concerns regarding communication skills, which is not unexpected given the high prevalence of language disorders in XXY. This finding of adaptive functioning concerns is especially striking given that the mean IQ score for the sample was in the average range, since there is typically a strong correlation between cognitive and adaptive skills in the general population. This suggests that factors other than overall cognitive ability may be interfering with boys’ ability to function effectively in their daily environments. These factors may include language deficits, learning disabilities, and the behavioral and emotional characteristics outlined previously.
Attentional problems were identified in 38% of the sample based on the BASC responses, and further investigation of ADHD symptoms applying the DSM-IV diagnostic criteria were consistent, showing that 36% of the sample met criteria for a diagnosis of ADHD based on parent report. Strikingly, all but one of those who met DSM-IV criteria were classified as having ADHD – Inattentive subtype (previously known as ADD), without significant symptoms of hyperactivity and impulsivity. It is important to point out that standard of care evaluation for ADHD includes assessment of symptomatology in more than one setting (i.e., school or work), as well as exclusion of other psychiatric and medical diagnoses that could account for attentional problems. Thus, in consideration of the complex neurocognitive phenotype in XXY, additional studies that directly evaluate attention and executive functions, and investigate the effect of language skills, cognitive abilities, and emotional symptoms on attention across multiple settings are required to better quantify clinical diagnoses of ADHD in children and adolescents with XXY.
When considering results of the social responsiveness assessment, it is again important to point out that the majority of participants scored in the average range across all domains and did not demonstrate significant social difficulties. Social awareness was an area of relative strength, including areas such as recognizing social differences from others and being aware of certain social cues, such as facial expressions and body language. However, for the other domains including social communication, social motivation, and social cognition, scores were elevated in over 40% of the sample, indicating the presence of social difficulties despite generally average cognitive abilities. Autistic behaviors have been described in other recent studies in children and adults with XXY (12, 13, 16), and these SRS results raise questions about whether the social and communication deficits are such that those with social deficits meet criteria for autism spectrum disorders. As shown in Figure 5, when ASD was assessed directly using standard diagnostic measures, only 5% (1 of 20 participants with XXY) met criteria for an ASD. Thus, despite deficits in language and social difficulties, in most cases they were not sufficiently elevated to reach a clinical diagnosis of ASD. However there were clear difficulties in social situations identified by the SRS scales that could be related to language and verbal processing abilities, emotional symptoms, or other factors. It is important to note that while a relatively small percentage of the sample (1 out of 20) was diagnosed with an ASD, a 5% rate of ASD is 4 to 5 times higher than in the general population estimate in male children of 1% to 1.4% (33), suggesting that there may be a higher risk of ASD in XXY.
Figure 5.
Distribution of scores in the social responsiveness domains of the SRS
Comparisons to other studies in XXY
It is informative to compare our results to other recent studies evaluating the behavioral phenotype of XXY. In 2009, Bruining et al published results from a study of 50 Dutch males with XXY age 5 to 19 recruited from a Dutch support group and clinics. (16) In addition to similarities to our sample in age range, sample size, and recruitment, 50% of their sample was also ascertained in the prenatal period. Their results showed significantly higher rates of ADHD (63% compared to 36% in our study) and ASD (27% compared to 5% in our study) using fairly similar diagnostic strategies. In contrast, their methodology for assessment of behavioral and emotional symptoms included a more intensive semi-structured diagnostic interview, compared to our use of parent-report questionnaires which identify behavioral symptoms but which are not diagnostic. They identified anxiety disorders in 32% and depressive disorder in 24%, which are approximately double the rates of “clinically significant” anxiety and depression in our study (14% and 12%, respectively). The most striking difference between our sample and the Dutch cohort was in overall cognitive functioning, with an average overall IQ of 80 for the Dutch sample, compared to our sample mean of 95. This suggests that more severe cognitive impairments are likely associated with more significant emotional and behavioral disorders in XXY, and the relationship between these factors requires further exploration. Despite the Bruining sample showing more severe difficulties, the patterns of symptoms including communication deficits, ADHD with predominantly inattentive symptoms, emotional symptoms of anxiety and depression, and social difficulties were very similar between our two distinct cohorts and their concluding recommendations for heightened awareness and screening for emotional difficulties and timely treatments are valid and important.
Another recent study by Bishop et al included 19 males with XXY age 4–16 who were all diagnosed in the prenatal period (12). Eleven percent of their prenatal sample had been previously diagnosed with ASD, with additional social difficulties noted in a percentage of those without ASD. Their methods differed, however, in that they reported ASD based on previous assessment by an outside provider, while our study directly assessed individuals for ASD. Their study also directly assessed adaptive skills using an interview called the Vineland, and they found similar results of somewhat depressed adaptive skills, most significant in the communication domain. Direct comparisons to our study results are more difficult as they did not directly assess the study participants or report on cognitive scores; however their results identified similar concerns related to communication, adaptive functioning and social skills.
Implications for Clinical Care
Professionals working with individuals with XXY should be aware of the broad behavioral phenotype, with recognition that a majority of patients will not have significant problems. However, our results and multiple previous studies show increased risks for problems with learning, communication, adaptive functioning, emotional disorders, attention deficits and ADHD, social difficulties, and autism spectrum disorders. Future research is needed to better understand how these factors interact and influence adult outcomes, and to identify interventions to prevent or treat these difficulties.
Currently, professionals should recognize the elevated risks in these areas, and provide routine screenings rather than waiting for the presentation of severe clinical symptoms. Concerns related to anxiety, depression, social withdrawal, and other internalizing problems should be referred to psychology or other mental health professionals, and therapies should be initiated but may need to be adapted somewhat related to communication or learning impairments. Since children and adolescents with the inattentive subtype of ADHD are not typically disruptive in the classroom, inattentive ADHD symptoms can be misattributed as “poorly motivated,” “a slow worker,” or “disorganized,” and thus these concerns should raise red flags to indicate the need for further assessment. All children with XXY should have a neuropsychological evaluation in early grade school to identify any symptoms of learning disabilities, executive function, or ADHD. Please see the paper by Carole Samango-Sprouse in this issue for further recommendations related to developmental screenings and interventions in infancy and preschool.
Concerns about social skills should lead to evaluation by a psychologist with sufficient experience to consider the influences of language deficits and emotional symptoms in XXY, and who can perform a diagnostic assessment for autism spectrum disorders, if needed.
Additional risks for problems in daily, adaptive living skills are seen even in children and adolescents with XXY with average cognitive ability. Professionals should keep in mind that males with XXY may demonstrate immature daily functioning skills, which can affect compliance and ability to follow through with both educational and therapeutic interventions. Thus, some individuals with XXY may not show age appropriate skills related self-care, affecting medical treatments such as testosterone therapy or other medications to treat psychological symptoms.
Implications for Genetic Counseling
The results of this study support genetic counseling in the prenatal setting by endorsing the broad clinical spectrum of boys with an XXY karyotype and demonstrating that the majority of individuals fall within the average range in regard to behavior, attention, social skills and adaptive functioning. It is important to take into consideration that many families seeking information in the context of a prenatal diagnosis often commence an intense search to find information to acquire an accurate depiction of what the future holds for a child with XXY. These parents should be cautioned about the excess of inaccurate information throughout the internet as well as the potential bias of information provided from parents of children with XXY found through online chat rooms and national support groups. Parents of children with XXY who participate in these forums and actively tell their stories online may represent a negative bias of information, which draws them to these support forums to begin with, or may represent an optimistic bias as their child is doing quite well and they eagerly volunteer to share their positive stories. Furthermore, the significant and critical impact of both the autosomal genes and environmental variables should be stressed when considering behavioral outcomes.
Genetic counseling for both prenatal and postnatal diagnoses provides unique opportunities of anticipatory guidance regarding the likelihood of and appropriate screening for possible behavioral concerns. While the majority of children and adolescents with XXY fall within the average range of behaviors, Figures 2–6 in this report demonstrate the various areas of possible behavioral concerns and their relative likelihood. Genetic counseling should accurately educate families about the likelihood of these possible behavioral difficulties, encourage families to present any concerns to their child’s physician and proactively seek out psychological evaluation. Counselors may also convey that families avoid becoming hyper focused and attributing all behaviors to the diagnosis of XXY, keeping in mind that typical children vary widely in behaviors, attention, social skills and adaptive functioning. If behavior problems are identified in a professional evaluation, interventions and supports should be instituted as soon as possible to promote the psychological health and development of the child. Moreover, counselors may also need to provide families with information identifying appropriate community resources for such evaluations and treatment, as well as available local resources for support, should the family so desire.
Future Directions
Additional research is needed to better understand the factors that explain the large spectrum of the behavioral phenotype in boys with an XXY karyotype, including biological factors such as differences in gene expression or genetic polymorphisms, and environmental factors including family support, socioeconomic status, and previous interventions. Based on previous and current research, it is difficult to determine if the behavioral and emotional problems detected in a subset of individuals with XXY are primary to the condition, or secondary to other vulnerabilities related to neurodevelopmental differences, such as language disorders, attentional disorders, or learning disabilities. In addition, it is critical that individuals without significant symptoms are included in studies in order to better understand factors that contribute to resiliency in this group. Research is required to explore the factors contributing to the unexpected weaknesses detected in adaptive functioning. Once these are better understood, targeted interventions can be developed to improve the daily life and adult outcomes of the boys and adolescents with Klinefelter syndrome.
Footnotes
Disclosure
The authors of this article declare no conflict of interest.
References
- 1.Klinefelter H, Reifenstein E, Albright F. Syndrome characteristized by gynecomastia spermatogenes without A-leydigism, increased excretion of follicle stimulating hormone. Journal of clinical endocrine metabolism. 1942;2:615–627. [Google Scholar]
- 2.Jacobs PA, Strong JA. A case of human intersexuality having a possible XXY sex-determining mechanism. Nature. 1959;183(4657):302–303. doi: 10.1038/183302a0. [DOI] [PubMed] [Google Scholar]
- 3.Coffee B, Keith K, Albizua I, Malone T, Mowrey J, Sherman SL, Warren ST. Incidence of fragile X syndrome by newborn screening for methylated FMR1 DNA. Am J Hum Genet. 2009;85(4):503–514. doi: 10.1016/j.ajhg.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evans JA, de von Flindt R, Greenberg C, Ramsay S, Hamerton JL. A cytogenetic survey of 14,069 newborn infants. IV. Further follow-up on the children with sex chromosome anomalies Birth defects. Orig Artic Ser. 1982;18:169–184. [PubMed] [Google Scholar]
- 5.Abramsky L, Chapple J. 47,XXY (Klinefelter syndrome) 47,XYY: estimated rates of and indication for postnatal diagnosis with implications for prenatal counselling. prenat diagn. 1997;4:363–368. doi: 10.1002/(sici)1097-0223(199704)17:4<363::aid-pd79>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 6.Leggett V, Jacobs P, Nation K, Scerif G, Bishop DV. Neurocognitive outcomes of individuals with a sex chromosome trisomy: XXX, XYY, or XXY: a systematic review. Dev Med child neurol. 2010;52:119–129. doi: 10.1111/j.1469-8749.2009.03545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bender B, Puck M, Salbenblatt J, Robinson A. In: Cognitive development of children with sex chromosome abnormalities. Smith S, editor. San Diego: College Hill Press; 1986. pp. 175–201. [Google Scholar]
- 8.Bender BG, Puck MH, Salbenblatt JA, Robinson A. Dyslexia in 47,XXY boys identified at birth. Behav Genet. 1986;16(3):343–354. doi: 10.1007/BF01071315. [DOI] [PubMed] [Google Scholar]
- 9.Pennington B, Bender B, Puck M, Salbenblatt J, Robinson A. Learning disabilities in children with sex chromosome anomalies. Child Dev. 1982;53(5):1182–1192. [PubMed] [Google Scholar]
- 10.Rovet J, Netley C, Keenan M, Bailey J, Stewart D. The psychoeducational profile of boys with Klinefelter syndrome. J Learn Disabil. 1996;29(2):180–196. doi: 10.1177/002221949602900208. [DOI] [PubMed] [Google Scholar]
- 11.Bishop DV, Jacobs PA, Lachlan K, Wellesley D, Barnicoat A, Boyd PA, Fryer A, Middlemiss P, Smithson S, Metcalfe K, Shears D, Leggett V, Nation K, Scerif G. Autism, language and communication in children with sex chromosome trisomies. Arch Dis Child. 2010 doi: 10.1136/adc.2009.179747. p. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van Rijn S, Swaab H, Aleman A, Kahn RS. Social behavior and autism traits in a sex chromosomal disorder: Klinefelter (47XXY) syndrome. J Autism Dev Disord. 2008;38(9):1634–1641. doi: 10.1007/s10803-008-0542-1. [DOI] [PubMed] [Google Scholar]
- 13.Leggett V, Jacobs P, Nation K, Scerif G, Bishop DV. Neurocognitive outcomes of individuals with a sex chromosome trisomy: XXX, XYY, or XXY: a systematic review. Dev Med Child Neurol. 52(2):119–129. doi: 10.1111/j.1469-8749.2009.03545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Netley CT. Summary overview of behavioural development in individuals with neonatally identified X and Y aneuploidy. Birth defects Orig Artic Ser. 1986;22(3):293–306. [PubMed] [Google Scholar]
- 15.Bruining H, Swaab H, Kas M, van Engeland H. Psychiatric characteristics in a self selected sample of boys with Klinefelter syndrome. Pediatrics. 2009;123(5):e865–870. doi: 10.1542/peds.2008-1954. [DOI] [PubMed] [Google Scholar]
- 16.van Rijn S, Aleman A, Swaab H, Kahn R. Klinefelter’s syndrome (karyotype 47,XXY) and schizophrenia-spectrum pathology. Br J Psychiatry. 2006;189:459–460. doi: 10.1192/bjp.bp.105.008961. [DOI] [PubMed] [Google Scholar]
- 17.Wechsler D. The Wechsler Intelligence Test for Children. 4. San Antonio: The Psychological Corporation; 2003. [Google Scholar]
- 18.Wechsler D. Weschler Abbreviated Scale of Intelligence. San Antonio: The Psychological Corporation; 1999. [Google Scholar]
- 19.Reynolds CR, Kamphaus RW. The Behavioral Assessment System for Children. Circle Pines, MN: American Guidance Service, Inc; 1998. [Google Scholar]
- 20.Reynolds CR, Kamphaus RW. Behavioral Assessment System for Children. 2. Circle Pines, MN: American Guidance Service; 2004. [Google Scholar]
- 21.Conners C. Conners’ Rating Scales: Revised. North Tonawanda, NY: Multi-Health Systems; 1997. [Google Scholar]
- 22.Swanson J, Kraemer H, Hinshaw S, et al. Clinical relevance of the primary findings of the MTA: Success rates based on severity of ADHD and ODD symptoms at the end of treatment. J Am Acad Child Adolesc Psychiatry. 2001;40:168–179. doi: 10.1097/00004583-200102000-00011. [DOI] [PubMed] [Google Scholar]
- 23.The Diagnostic and Statistical Manual of Mental Disorders - Text Revision. 4. Washington D.C: American Psychiatric Assosication; 2000. [Google Scholar]
- 24.Constantino J. The Social Responsiveness Scale. Los Angeles, California: Western Psychological Services; 2002. [Google Scholar]
- 25.Lord C. Autism Diagnostic Interview- Revised: a revised version of a diagnostic interview for caregivers of individulas with possible pervasive developmental disorders. J Autism Dev Disord. 1994;24(5):659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- 26.Lord C. The autism diagnostic observation schedule-generic:a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord. 2000;30(3):205–223. [PubMed] [Google Scholar]
- 27.Ratcliffe SG, Butler GE, Jones M. Edinburgh study of growth and development of children with sex chromosome abnormalities. IV Birth Defects Orig Artic Ser. 1990;26(4):1–44. [PubMed] [Google Scholar]
- 28.Robinson A, Bender BG, Linden MG, Salbenblatt JA. Sex chromosome aneuploidy: the Denver Prospective Study. Birth Defects Orig Artic Ser. 1990;26(4):59–115. [PubMed] [Google Scholar]
- 29.Linden MG, Bender BA. Robinson, Intrauterine diagnosis of sex chromosome aneuploidy. Obstetrics and Gynecology. 1996;87(3):468–475. doi: 10.1016/0029-7844(95)00419-x. [DOI] [PubMed] [Google Scholar]
- 30.Linden MG, Bender BG. Fifty-one prenatally diagnosed children and adolescents with sex chromosome abnormalities. Am J Med Genet. 2002;110(1):11–18. doi: 10.1002/ajmg.10394. [DOI] [PubMed] [Google Scholar]
- 31.Boada R, Janusz J, Hutaff-Lee C, Tartaglia N. The cognitive phenotype in Klinefelter syndrome: a review of the literature including genetic and hormonal factors. Dev Disabil Res Rev. 2009;15(4):284–294. doi: 10.1002/ddrr.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rice C. Prevalence of Autism Spectrum Disorders--Autism and Developmental Disabilities Monitoring Network, United States, 2006. Morbidity and Mortality Weekly Report. 2009;58(SS10):1–20. [PubMed] [Google Scholar]