Abstract
Primary effusion lymphoma (PEL) is a very rare subgroup of B-cell lymphomas presenting as pleural, peritoneal and pericardial neoplastic effusions in the absence of a solid tumor mass or recognizable nodal involvement. There is strong evidence that Kaposi’s sarcoma associated herpesvirus (KSHV) is a causal agent of PEL. PEL tumor cells are latently infected by KSHV with consistent expression of several viral proteins and microRNAs that can affect cellular proliferation, differentiation and survival. The most relevant data on pathogenesis and biology of KSHV have been provided by studies on PEL derived cell lines. Fourteen continuous cell lines have been established from the malignant effusions of patients with AIDS-and non-AIDS-associated PEL. These KSHV+ EBV+/− cell lines are wellcharacterized, authenticated and mostly available from public biological ressource centers. The PEL cell lines display unique features and are clearly distinct from other lymphoma cell lines. PEL cell lines represent an indispensable tool for the understanding of KSHV biology and its impact on the clinical manifestation of PEL. Studies on PEL cell lines have shown that a number of viral genes, expressed during latency or lytic life cycle, have effects on cell binding, proliferation, angiogenesis and inflammation. Also PEL cell lines are important model systems for the study of the pathology of PEL including the lack of invasive or destructive growth patterns and the peculiar propensity of PEL to involve body cavity surfaces.
Keywords: PEL, PEL cell lines, KSHV/HHV8, HIV-associated lymphomas, malignant effusions
Introduction
Primary effusion lymphoma (PEL) is a very rare subgroup of B-cell lymphomas presenting as pleural, peritoneal and pericardial (body cavity) lymphomatous effusions in the absence of a solid tumor mass or recognizable nodal involvement [1]. Because of the identification of Kaposi’s sarcoma associated herpesvirus (KSHV) in all of the cases presenting as primary lymphomatous effusions in early studies, the presence of this virus has been incorporated as a diagnostic criterion for PEL [2–4]. Cases that are KSHV-positive but without an effusion also exist, and are considered as extracavitary variants of PEL [5–7]. There is strong evidence that KSHV is a causal agent of PEL [8,9] and the other KSHV-associated diseases, i.e. Kaposi’s sarcoma and multicentric Castleman’s disease (MCD) [10].
Because of the rarity of PEL, much of the clinical and pathological information comes from case reports or small series of patients, with a few studies that have examined biopsy tissues and/or aspirates. By contrast, the most relevant data on pathogenesis and biology of KSHV have been provided by studies on PEL derived cell lines that have shown that a number of viral genes, expressed during latency or lytic life cycle, have effects on cell binding, proliferation, angiogenesis and inflammation [11–13].
We review here the current knowledge on the unique clinical presentation of PEL, its diagnosis and classification. We also review what we know about pathogenesis, and the salient features of PEL derived cell lines as a tool for understanding the unique presentation and pathobiology of PEL.
Clinical presentation of PEL. Diagnosis and classification
Definition of PEL
The initial description of PEL refers to a B-cell lymphoma characterized by the elective involvement of serous body cavities with the effusions in absence of tumor masses [1–3,14,15]. It was subsequently emphasized that PEL spreads along serous membranes, without infiltrative growth patterns [16,17]. The increased knowledge about PEL led to the identification of cases with contemporary nodal involvement and extranodal non-serous sites of localization [reviewed in 18,19]. Extracavitary lymphomas have also been reported following resolution of PEL. Morphologic, immunophenotypic and virologic features consistent with the diagnosis of PEL have also been recognized without lymphoma localization in serous cavities at diagnosis [reviewed in 18, 19]. The common pathobiological features of KSHV-related lymphomas, in their liquid and solid presentation, allowed the recognition of these entities as part of the spectrum of PEL [6,7].
Diagnosis of PEL
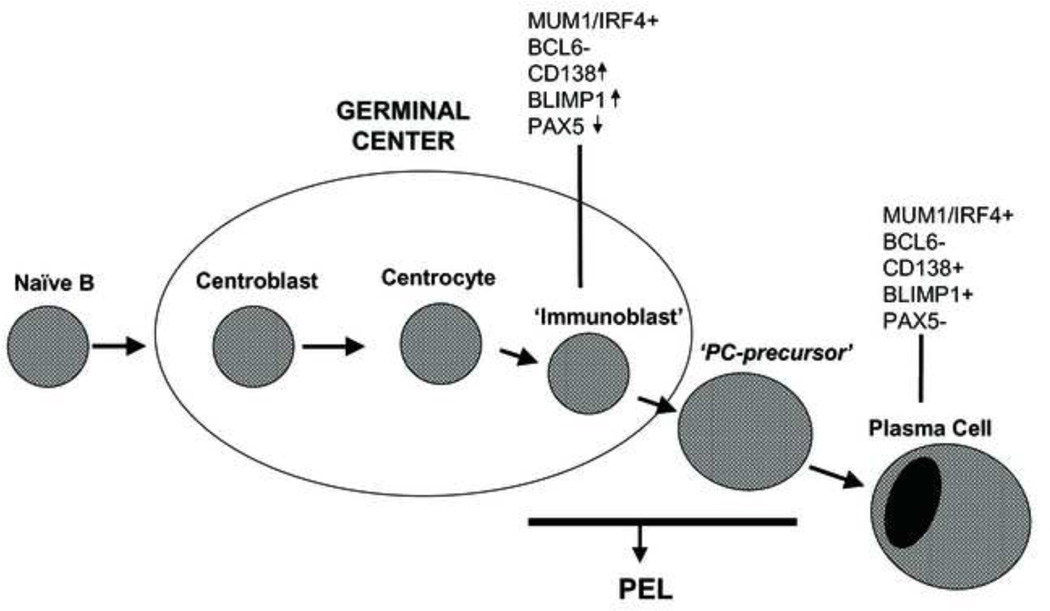
As PEL usually lacks a tumor mass component, its diagnosis is mainly based on the cytologic examination of body fluid [20]. Morphologically, PEL tumor cells show intriguing features. The most frequent appearance bridges immunoblastic and anaplastic large-cell lymphomas, and displays a variable degree of plasma cell differentiation [2,3,20]. Cells displaying nuclear fragmentation and karyopyknosis may also be present in PEL specimens, consistent with a certain degree of apoptosis. Reactive cells, including small lymphocytes, macrophages and rare mesothelial cells, may be admixed with the neoplastic population. Expression of the CD45 antigen confirms the hematolymphoid derivation of PEL cells, and positivity for the CD138/syndecan-1 molecule, coupled to immunogenotypic features, indicates that the lymphoma reflects an advanced stage of B-cell differentiation, close to plasma cells (pre-plasma cells) (Figs. 1 and 2). In addition to CD45, CD138/syndecan-1 and MUM1/IRF4, PEL cells generally express various phenotypic markers associated with activation, including CD30, CD38, CD71, and epithelial membrane antigen (EMA). Expression of the CD20 B-cell antigen and of very low levels of cytoplasmic immunoglobulin (Ig) molecules may occur in a small fraction of PEL cases. However, its usual phenotype is indeterminate although PEL is consistently composed of a monoclonal B-cell population [1,3,5,20]. Sporadic cases of PEL with T cell antigen expression have been described [21,22]. In these cases, tumor cells had either a corresponding T-cell genotype or additional rearrangements of the immunoglobulin genes [21,22]. Demonstration of viral infection by KSHV in the neoplastic cells is required for the diagnosis of PEL. Immunocytochemical staining for ORF73/ latency-associated nuclear antigen (LANA) is the standard assay to detect evidence of KSHV infection in the neoplastic cells. In addition to the association with KSHV, most cases of PEL also contain the Epstein Barr virus (EBV). The combined presence of these two viruses appears to be unique to PEL [23].
Figure 1.
The phenotypic profile of PEL suggests a plasmablastic derivation.
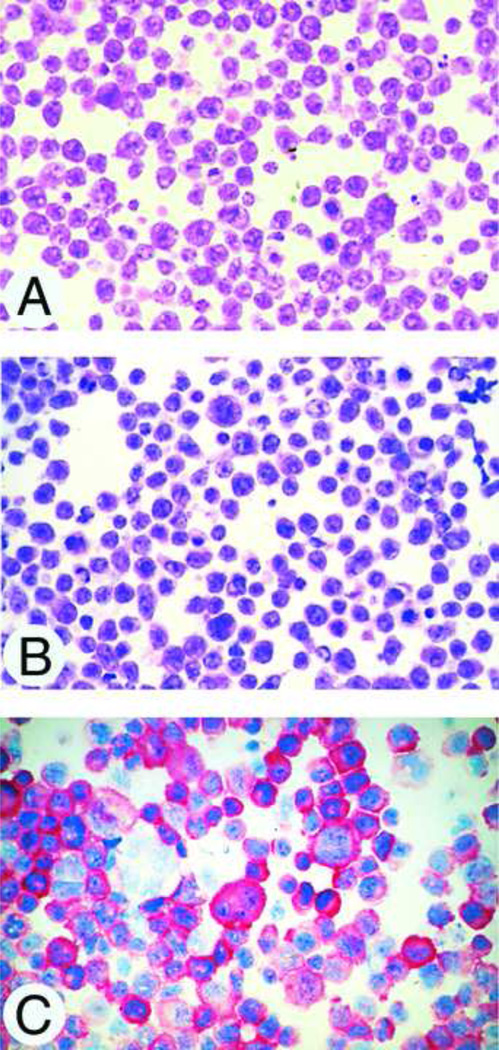
Figure 2.
(A,B,C). PEL tumor cells morphologically display pleomorphism and a variable degree of plasma cell differentiation (A,B). Expression of CD138 molecule, a marker associated with advanced stage of B-cell differentiation(C). Cytospin preparations, hematoxylin and eosin stain (A,B); APAAP immunostaining, hematoxylin counterstain (C); original magnification, x250
Clinical presentation
At presentation, deep immunodepression and severe depletion of circulating CD4+ lymphocytes or B symptoms are common. They reflect the disease aggressiveness and the frequent pre-existent compromise of general conditions of the affected patients. Other symptoms and signs of disease largely depend on distribution of sites of disease. The pattern of clinical presentation translates in heterogeneous aspects in the field of radioimaging (see below) [24].
PEL may be the primary presentation of KSHV infection. However, KSHV related diseases such as MCD and Kaposi’s sarcoma (KS) may precede or may occur contemporary to PEL. In only a minority of cases of PEL reported in the International Extranodal Lymphoma Study Group - IELSG series, a previous or concomitant diagnosis of KS has been reported and MCD was not frequent and when present it was exclusively described in the subset of HIV+ patients [25]. Apart from AIDS, PEL has also been reported in association with other immunodeficiency conditions, namely iatrogenic immunodeficiency following solid organ transplantation, cirrhosis and cancer. Interestingly, PELs developing in the HIV-negative patients selectively affect elder individuals from geographical areas at high prevalence of KSHV infection [26].
Prognostic factors
The strongest predictor of poor clinical outcome in the population of HIV-infected individuals is the absence of highly active antiretroviral therapy (HAART) before PEL diagnosis [27,28]. The HAART effect is probably based on the favourable impact of the reversion of severe immunodeficiency. Moreover, the control of HIV replication and the subsequent immunologic recovery induced by HAART could potentially slow down disease progression [27].
PEL and KSHV-unrelated lymphomas occurring in the body cavities
PELs possess an unique constellation of features that distinguish them from other lymphomas occurring in the body cavities. Lymphomas occurring in patients in whom effusions complicate a tissue-based lymphoma, the so called secondary lymphomatous effusions, closely mimick phenotypic and genotypic features of the corresponding tissue based lymphoma, and are consistently devoid of KSHV infection [29]. The pyothorax-associated lymphomas, now called diffuse large B-cell lymphomas associated with chronic inflammation, consistently present with a tumor mass localized in the body cavities, but only rarely give rise to a lymphomatous effusion and are devoid of KSHV sequences [30].
Other types of lymphomas involving the serous body cavities include cases of Burkitt lymphoma (BL), mainly occurring in the context of AIDS, which present as a primary lymphomatous effusions without mass formation [3,6]. KSHV infection (assessed by ORF73/LANA immunoreactivity), which clusters with PEL, and translocation of the c-MYC proto-oncogene, which segregates with BL [17], are mutually exclusive molecular events in the development of these distinct malignant effusions [3].
Other subtypes of lymphomas can present with a primary neoplastic effusion. Many of these cases are KSHV-unrelated large B-cell lymphomas, also termed KSHV-unrelated PEL-like lymphomas [31]. In these lymphomas the neoplastic cells do not display evidence of KSHV infection, but display morphologic, immunophenotypic and genotypic features related to large B-cell lymphoma [32].
PEL and KSHV-unrelated PEL-like lymphomas are different in terms of pathogenesis, morphologic-immunophenotypic features, clinical behaviour and prognosis. KSHV-unrelated PEL-like lymphoma cases, are associated with hepatitis C virus (HCV) (30–40%). The most frequently involved sites are peritoneum and pleura. The lymphoma cells usually show large cell morphology and B cell immunophenotype. The outcome of patients with KSHV-unrelated PEL-like lymphomas seems to be better than the one for PEL patients in the HIV + setting [27,31].
PEL as a lymphoma of the serous membranes
The basic pathologic feature of PEL is a diffuse spreading along the serous membranes without markedly infiltrative or destructive growth patterns [3,14,33]. PEL is associated with peculiar imaging features including: a) peritoneal effusion or bilateral/unilateral pleural effusions, usually associated with pericardial effusion, b) normal mediastinal and parenchymal imaging findings and c) diffuse slight thickening of the serous membranes at computed tomography (CT) [24]. As seen at autopsy PEL presents as multiple small tumor foci involving the serous membranes, which appear irregularly thickened [16,24,33]. Furthermore, the lymphomatous infiltration of serosal surfaces is adjacent to the site of primary malignant effusion. Notably, these aspects correlate closely with imaging findings of PEL revealed by CT scan. Overall, these features would indicate a primary serous membrane neoplasm. In the natural history of PEL the disease initially affects one single serous cavity, usually remains localized to body cavities throughout the clinical course of the lymphoma, and occasionally extends into tissues underlying the serous membranes, including the omentum and the outer parts of the gastrointestinal tract wall. Involvement of mediastinal lymph nodes, visceral lymphatics or other superficial and deep lymph nodes, with or without parenchymal infiltration, has been observed in some cases [2,3,16,33].
PEL pathogenesis and the role of KSHV on PEL development and progression
The exact mechanism by which KSHV promotes oncogenesis in B cells leading is an area of active investigation. In vitro infection of B cells with KSHV is ineficient, and does not lead to transformation of these cells [34]. Therefore, cell lines derived from PEL specimens, where natural infection by KSHV occurred in vivo, have been the only tool available to study the molecular effects of KSHV gene expression in a B cell background, and the molecular mechanisms of lymphomagenesis. KSHV does not replicate in untreated PEL cell lines in culture, and only a limited number of viral genes are expressed, which are designated as latent genes. In contrast, when these cell lines are treated with some chemical agants that include phorbol esters and butyrate, viral replication is induced with the production of infectious virion, and a large number of lytic viral genes are expressed. It is thought that with expression of latent genes, infected cells can undergo clonal expansion, eventually leading to neoplastic transformation through mechanisms of increased proliferation and impaired apoptosis, although the true role of transient expression of lytic genes during neoplastic transformation in vivo is not known.
Latent gene products
Five latent gene products that are thought to play significant roles in PEL pathogenesis are LANA (ORF73), viral cyclin (v-Cyc, ORF72), viral FLICE inhibitory protein (v-FLIP, ORF71), viral interferon regulatory factor 3 (vIRF-3 or LANA-2) and viral interleukin-6 (vIL-6, ORFK2).
LANA, encoded by ORF73, is required for the replication of the latent episomal viral DNA; it binds to the latent origin of replication in the terminal repeat subunits of the viral genome. In addition it is a multifunctional protein with the potential to significantly alter cellular physiology by recruiting a large variety of cellular proteins linked to transcriptional regulation or proliferation control, including p53, pRB, c-myc, brd2, brd4, CBP, DNAMt1, DNAMt3, GSK3β [reviewed in 35]. LANA is expressed during latency and represents the most consistently detected viral protein in KSHV-associated tumor cells.
V-cyclin (vCYC), encoded by ORF72, represents another candidate KSHV oncogene because of its homology to the human cyclin-D/Prad oncogene. In general, cyclin-D proteins (D1 D2, D3) associate with specific cyclin-dependent kinases (CDKs) and these complexes phosphorylate Rb family members. vCYC associates with cdk2, cdk4 and cdk6 but appears to promote phosphorylation of its targets mainly in concert with cdk6 [36,37]. Targets of vCYC include not only Rb, but also other cellular targets including histone H1, Id2, CDC6, cdc25A, Orc-1, the anti-apoptotic protein bcl-2 and the cdk inhibitors p27Kip and p21CIP [37,38]. Phosphorylation of p27 Kip by the vcyc/cdk6 complex on Ser 10 during latency leads to sequestration of p27 Kip in the cytoplasm, thereby allowing PEL cells to proliferate in the presence of high p27 Kip levels [37]. Likewise, phosphorylation of p21 CIP1 on serine 130 by vCYC allows this viral protein to bypass the p21 CIP1 -mediated G1 arrest [38]. vCYC has been shown to promote S-phase entry and also to induce apoptosis in cells with high cdk6 expression, which can be counteracted by the action of the viral bcl-2 homologue, vBCL-2, which is expressed durin the lytic cycle [39]. vCYC can also induce a DNA damage response in endothelial cells [40]. It is likely that some of these biochemical features of vCYC play a role in PEL pathogenesis.
vFLIP, encoded by ORF-K13 (also called ORF 71) is transcribed from the LANA promoter in a tricistronic transcript that also contains vCYC, and is translated from an internal ribosome entry site [41,42]. It is therefore thought to be expressed during latency and in all tumor cells. The vFLIP protein expression is very weak in PEL cells, but has been detected by Western blot in PEL cell lines [43] and also epithelial cells carrying a recombinant KSHV genome. It inhibits CD95/F AS -induced apoptosis in vitro by blocking caspase-3, −8 and −9 [44]. Both CD95/Fas-L and TRAIL/TNF-alpha induce apoptosis through a similar mechanism [45,46]. A more recent line of inquiry found vFLIP to be involved in NF-κB signalling by binding to IKKy/NEMO [47,48]. TRAF-2 is also invovled in vFLIP signaling to NF-κB [49]. Eliminating either vFLIP or NF-κB activity from PEL induces apoptosis [50–52], demonstrating that this pathway is essential for lymphomagenesis.
KSHV encodes four homologues to the cellular interferon regulatory factors, an important family of trascription factors involved in interferon signaling. Only one of these is is expressed in latently infected PEL cells, which is vIRF-3, also called LANA-2, encoded by encoded by ORF K10. 6. The functional aspects of this viral protein were recently reviewed [53]. Importantly, when vIRF-3 is knocked down with RNA interference techniques in PEL cell lines, there is a reduction of proliferation and induction of apoptosis, suggesting that this viral protein is indeed involved in the pathogenesis of PEL [54].
Cytokines
Investigative studies on the pathogenesis of PEL have revealed a peculiar profile of cytokines, characterized by secretion of large amounts of human IL6, vIL6, IL10 and VEGF (Fig. 3) that play a role in PEL pathogenesis in vitro and/or in vivo. vIL-6, encoded by ORF K2, is considered to by a lytic viral protein, but is expressed in a variable but significant proportion of PEL cells, both in primary tumors and established cell lines [55,56]. vIL6 is a multifunctional cytokine which is capable of promoting hematopoiesis, plasmacytosis and angiogenesis [57]. It is a homologue of interleukin 6 (IL-6), but differs from the cellular protein in that it can signal through gp130 in the absence of the IL-6 receptor α subunit (gp80), making this viral cytokine able to affect a broader range of cell types [56,58]. As vIL-6 is secreted, it can affect neighboring cells in a paracrine fashion, and support their growth [59].
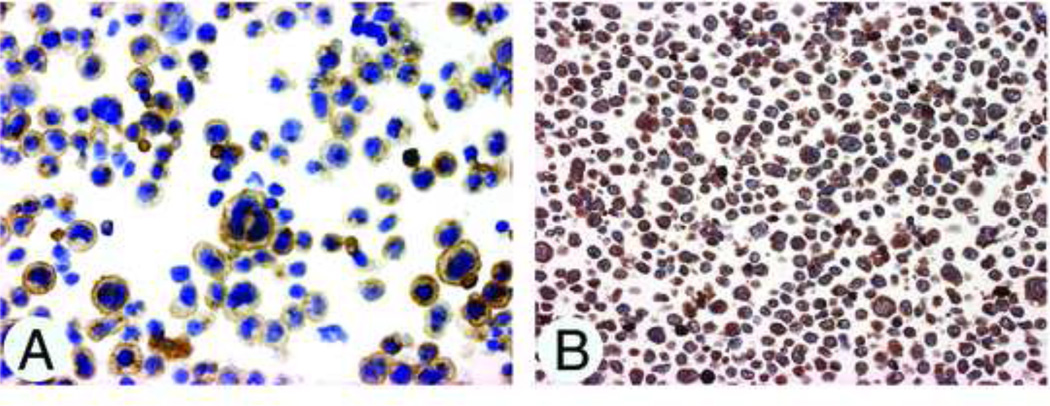
Figure 3.
(A,B). Expression of IL-10 (A), and VEGF (B) on CRO-AP/5 PEL-derived cell lines. Cytospin preparations, avidin-biotin-peroxidase complex immunostaining, hematoxylin counterstain; original magnification, x250.
PEL produce and release IL-6 and IL-10 both in vitro and in vivo [12], and both have been shown to support the growth of PEL cells [59]. The precise role of IL10 in PEL growth in vivo is debated, but it is thought that this cytokine may modulate the host immune response against the tumor.
VEGF, angiogenesis and vascular permeability
Several PEL cell lines produce high levels of VEGF [60] probably because KSHV has the potential to promote VEGF secretion through vIL6 [57]. Because VEGF is released by PEL cells into the surrounding environment, it is conceivable that this growth factor contributes to effusion formation through increased vascular permeability of serous membrane vessels. The release of high concentrations of VEGF by PEL cells is also consistent with the marked degree of angiogenesis associated with the in vivo growth of PEL cells.
Deregulation of VEGF appears to be a feature common to all KSHV related disorders. However, in contrast to KS and MCD, the role exerted by VEGF in PEL would be essentially to accelerate vascular permeability [60].
Future research. PEL-derived cell lines
A number of continuous lymphoma cell lines have been established from different specimens obtained from patients with AIDS- and non-AIDS-associated PEL. The names of 22 PEL cell lines can be found in the literature. Two cell lines are sisters of already existing lines which were established from the same patients, but independently in other laboratories; one cell line was published under two different designations. Fourteen PEL-derived cell lines are well characterized and described [61–74] (Table 1). Five additional PEL cell lines have been described in the literature: cell line BC-4 [75]; BC-5 [76]; HH-B2 [77]; PEL-5 [78]; and VG-1 [79].
Table 1.
Authenticated PEL-Derived Cell Lines
| Cell Line | Patient | Diagnosis | Disease Status | Specimen for Cell Line |
Year of Est- ablishment |
Viral Status of Cell Line | Authentication | Immuno- profile |
Karyotype | Availability | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|
| BC-1a | 46 M HIV+ | PEL + AIDS | at diagnosis | ascites | 1992 | EBV+ KSHV+ HIV- HTLV1/2- | yes (by IGH rearrangement, EBV sequencing) | yes | yes | ATCC | Cesarman 1995 [61] |
| BC-2 | 31 M HIV+ | PEL + AIDS | at diagnosis | pleural effusion | 1992 | EBV+ KSHV+ HIV- HTLV1/2- | yes (EBV sequencing) | yes | yes | ATCC | Cesarman 1995 [61] |
| BC-3b | 85 M HIV- | PEL | at diagnosis | pleural effusion | 1995 | CMV- EBV- KSHV+ HIV- HSV1/2- | yes (by IGH rearrangement) | yes | yes | ATCC | Arvanitakis 1996 [62] |
| BCBL-1 | 40 M HIV+ | Kaposi -> PEL + AIDS |
no data | ascites | no data | EBV- KSHV+ HIV- | no (at DSMZ unique DNA profile) | (yes) | yes | NIH AIDS Program |
Renne 1996 [63] |
| BCP-1 | 94 M HIV- | Kaposi -> PEL | at diagnosis | peripheral blood | 1995 | CMV- EBV- HHV6- KSHV+ HIV- | yes (by IGH rearrangement) | yes | yes | ATCC | Boshoff 1998 [64] |
| Cra-BCBL | 37 M HIV+ | PE L+ AIDS | at diagnosis | pleural effusion | 1996 | EBV+ KSHV+ | yes (by IGH rearrangement, EBV/KSHV Southerns) |
yes | no | not known | Lacoste 2000 [65] |
| CRO-AP/2 | 49 M HIV+ | Kaposi -> PEL + AIDS |
at diagnosis | pleural effusion | 1996 | EBV+ HBV- HCV- KSHV+ HIV- HTLV1/2- |
yes (by IGH rearrangement) | yes | yes | DSMZ | Carbone 1997 [66] |
| CRO-AP/3 | 42 M HIV+ | PEL + AIDS | at diagnosis | ascites | 1997 | EBV- HBV- HCV- KSHV+ HIV- HTLV1/2- | yes (by IGH rearrangement) | yes | yes | DSMZ | Carbone 1998 [67] |
| CRO-AP/5 | 35 M HIV+ | Kaposi -> PEL + AIDS |
progressive, terminal |
pleural effusion | 1998 | EBV+ HBV- HCV- KSHV+ HIV- HTLV1/2- |
yes (by IGK rearrangement) | yes | yes | DSMZ | Carbone 1998 [67] |
| CRO-AP/6 | 35 M HIV+ | PEL + AIDS | at diagnosis | pleural effusion | 1999 | EBV- HBV- HCV- KSHV+ HIV-HTLV1/2- | yes (by IGH rearrangement) | yes | yes | DSMZ | Carbone 2000 [68] |
| JSC-1 | 52 M HIV+ | PEL | no data | ascites | no data | EBV+ KSHV+ | yes (IGH rearrangement) | (yes) | yes | ATCC | Cannon 2000 [69] |
| LH5-21 | 62 M HIV- | Kaposi -> PEL | no data | pleural effusion | no data | EBV- KSHV+ | yes (by IGH rearrangement, cytogenetics) | yes | yes | not known | Waller 1993 [70] |
| RM-P1 | 63 M HIV- | PEL | at diagnosis | pericardial effusion | no data | EBV+ KSHV+ | yes (by IGH rearrangement, cytogenetics) | yes | no | not known | Miyagi 2002 [71] |
| TY-1 | 47 M HIV+ | PEL + AIDS | at diagnosis | pericardial effusion | 1996 | EBV+ KSHV+ HIV- | no | yes | yes | Original authors |
Katano 1999 [72] |
Abbreviations: AIDS, acquired immunodeficiency syndrome; ATCC, American Type Culture Collection; CMV, cytomegalovirus; DSMZ, Deutsche Sammlung von Mikroorganismen und Zellkulturen (German Collection of Microorganisms and Cell Cultures); EBV, Epstein-Barr virus; HBV, hepatitis B virus; HCV, hepatitis C virus; HHV6; human herpesvirus 6; HIV, human immunodeficiency virus; HSV1/2, herpes simplex virus type 1/2; HTLV1/2, human T-cell leukemia virus type 1/2; IGH/IGK, immunoglobulin heavy/ka+ppa light chain gene; M, male; NIH, National Institutes of Health; PEL, primary effusion lymphoma.; KSHV, Kaposi sarcoma associated herpesvirus
HBL-6 is an independently (in another laboratory) established sister cell line of BC-1, also from ascites from the same partient, but with some immunoprofile, cytogenetic, functional differences [73]
KS-1 is an independently (in another laboratory) established sister cell line of BC-3, also from pleural effusion from the same patient, with similar profile [74].
The following refers to the 14 well characterized PEL cell lines (Table 1). All cell lines were derived from male patients with PEL associated with (n = 9) or without AIDS (n = 5); 10/14 patients were HIV-seropositive. Their ages ranged from 31 to 94 years. Five of the patients had pre-existing Kaposi`s sarcoma. Cell lines were established from malignant pleural effusions (n = 7), ascites (n = 4), pericardial effusion (n = 2), and peripheral blood (n = 1). As far as described, the status of the disease during which the samples for the cultures were obtained was at diagnosis (n = 10) or at relapse/terminal disease (n = 1). All cell lines grow autonomously as single cell suspension cultures in common culture media supplemented with fetal bovine serum without any further supplements (e.g. cytokines) under standard cell culture conditions.
It is important to point out that the derivation of 13 of the 14 PEL cell lines is authenticated (Table 1), that means that it has been proven that the new cell line was indeed derived from the patients whose primary cells were seeded into culture and was not the result of an inadvertent cross-contamination with cells from an established, faster growing cell line. Overall, in a recent large study some 15% of human leukemia-lymphoma cell lines were found to be cross-contaminated with other cell lines [80]. With regard to the PEL cell lines, comparisons of primary cells and cell lines using immunoglobulin heavy and light chain gene rearrangement patterns, EBV sequencing, cytogenetic analysis and DNA fingerprinting proved the correct derivation.
Availability of cell lines is another important issue. Ten of the PEL cell lines listed in Table 1 can be obtained from public repositories such as American Type Culture (ATCC), German Collection of Microorganisms and Cell Cultures (DSMZ) or the NIH AIDS Program. One cell line was received directly from the original investigators.
Characteristic features of PEL-derived cell lines
Consistent with their derivation, all 14 PEL cell lines are KSHV-positive. It has been reported that a switch from latent infection to productive (lytic) replication of KSHV could be induced, e.g. in cells exposed to the phorbol ester TPA or butyrate [63,69,72]. Eight PEL cell lines are co-infected with EBV, showing a monoclonal pattern, whereas the remaining six cell lines are EBV-negative (Table 1). None of the cell lines were found to be positive for other herpes viruses such as CMV (0/2), HHV6 (0/1), or HSV1/2 (0/1); the cell lines are further negative for HBV (0/4), HCV (0/4), HIV (0/10), and HTLV1/2 (0/6).
Except for two cell lines with limited immunoprofiles, the PEL cell lines were extensively immunophenotyped using large panels of immunomarkers. In general the cells are devoid of any lineage-specific or –associated markers. None of the cell lines express any markers asssociated with the T-cell or natural killer cell lineages (CD2, CD3, CD4, CD5, CD7, CD8, CD56). The cells are also generally negative for typical B-cell antigens such as CD10, CD19, CD20, CD21, CD22, CD40, CD72, CD79a/b, CD80 or surface immunoglobulin. Some B-cell markers are occasionally positive: CD23 (56% of the cell lines), CD37 (60%), CD39 (60%), CD74 (80%) - and of particular note late B-cell/plasma cell marker CD138 (100%). As expected all myelomonocytic markers are negative (CD13, CD14, CD15, CD33 and others). There is variable expression of non-lineage markers and activation-associated antigens: HLA-DR (80%), CD30 (83%), CD34 (0%), CD38 (89%), CD45 (92%), CD45RA (25%), CD45RO (40%), CD70 (100%), CD71 (100%). All cell lines tested express epithelial membrane antigen (EMA). Finally, expression of adhesion markers is again variable: CD11a (67%), CD11b (20%), CD11c (0%), CD18 (0%), CD43 (67%), CD44 (80%), CD49a (0%), CD49d (80%), CD49f (100%), CD54 (71%), CD58 (67%). In summary, the cells are generally negative for classical T-, NK and B-cell immunomarkers, except for CD138 suggesting a pre-terminal B or plasma cell stage, and are positive at variable levels for some activation and adhesion markers.
Complete karyotypes have been published from 12/14 PEL cell lines (Table 1) [11,80]. All cell lines carry numerical and structural chromosomal aberrations. The structural abnormalities are complex and clonal with a mostly hyperdiploid karyotype. No recurrent aberration which might be specific or associated with PEL is apparent in the cell lines analyzed. The cell lines do not carry a t(2;5), t(3;14), t(8;14), t(11;14) or t(14;18) which are associated with anaplastic large cell lymphoma, diffuse large cell lymphoma, BL, mantle cell lymphoma or follicular lymphoma, respectively.
Southern blot analysis of the PEL cell lines demonstrated clonal rearrangements of the heavy and/or light chain immunoglobulin genes, indicating their B-cell derivation. No rearrangements of the proto-oncogenes MYC, BCL1, BCL2 or BCL6 were found [11]. Also the tumor suppressor gene p53 was always seen in its wild-type form without any point mutations. The majority of the PEL cell lines examined were described as carrying mutations of the BCL-6 5` non-coding regions [11].
Several PEL cell lines could be successfully heterotransplanted into immunocompromised mice (e.g. BNX, NOD/SCID, or SCID) where the malignant cells proliferated developping tumors, lymphomatous effusions and marked angiogenesis [64,74,81].
Several cell lines (BC-1, BC-2, BC-3, BCBL-1, CRO-AP/2, CRO-AP/3, CRO-AP/5) were shown to produce constitutively high levels of the cytokines interleukin-6 (IL-6), IL-10 and HGF (hepatocyte growth factor) [11]. In the colony formation assay on agar, two cell lines (BCP-1 and HBL-6) had high colony-forming efficiency, attesting to their malignant nature.
The cell line STR-428 was derived from a 53-year-old male with HIV-KSHV- “malignant effusion lymphoma” which according to the authors corresponds to diffuse large B-cell lymphoma in the WHO classification [82]. The cell line is EBV- KSHV-, carries various surface B-cell immunomarkers (CD19, CD20, CD22, kappa light chain), and finally also contains the for other lymphomas characteristic t(14;18)(q32:q21) with the IGH-BCL2 fusion and a MYC rearrangement [82]. Hence STR-428 represents a unique high-grade B-cell lymphoma-derived cell line and has features that are clearly distinct from those of canonical PEL cell lines.
A concise summary of the most relevant and distinctive features of PEL cell lines is given in Table 2. These cell lines are very well characterized and described. Their profiles in the various areas (virology, immunophenotypes, cytogenetics, molecular genetics, functional aspects) are unique and taken together characteristic. The number of cell lines established is limited, but the majority of them is available from public repositories. As they are continuously available model systems, the PEL cell lines represent valuable and indispensable tools for the pathophysiological characterization of the primary effusion lymphomas. Furthermore, these cell lines provide a permanent source for the analysis of KSHV sequences. Notably, PEL-derived cell lines stably retain the KSHV latent viral genome in high copy number (50–100 copies/cell), while latent genomes do not persist in latently infected primary endothelial cells derived from KS lesion, nor in epithelial, endothelial or fibroblast cell lines. [83,84].
Table 2.
Summary of Characteristic Features of PEL-Derived Lymphoma Cell Linesa
|
Fourteen continuous cell lines have been established from the malignant effusions of patients with AIDS- and non-AIDS-associated PEL. These KSHV+ EBV+/− cell lines are well-characterized, authenticated and mostly available from public biological ressource centers. Lacking the common immunomarkers of the T-, B- and NK cell lineages, nevertheless these cells express CD138 and have rearranged immunoglobulin genes and are thus of B-cell origin. Complex clonal hyperdiploid karyotypes with multiple structural chromosomal abnormalities are seen, but without the characteristic alterations at the chromosomal and gene level which are associated with the common types of B-cell lymphoma.
Gene expression profiling of PEL-derived cell lines
A major instrument toward the definition of PEL phenotype and cell biology has been gained with characterization by gene expression profiling (GEP) analysis of a number of PEL cell lines representative of EBV positive and EBV negative PEL [85–87].
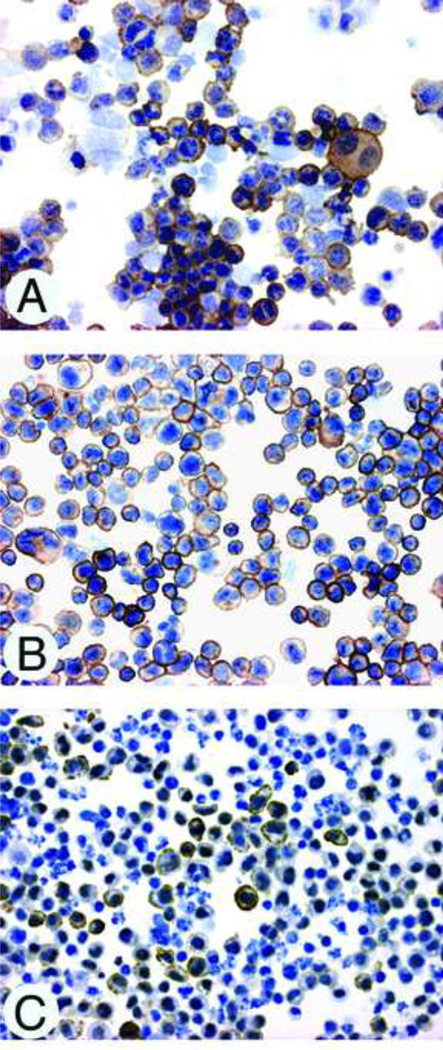
By GEP PELs were defined by the overexpression of genes that are involved in inflammation, cell adhesion, and invasion, which may be responsible for their presentation in body cavities [85]. Klein et al. [86] used GEP (of 12 000 genes) of PEL- primary specimens to further define the phenotype of AIDS-related PEL and to investigate the relationship of lymphoma to normal B-cells and to other tumor subtypes, including NHL of immunocompetent hosts and AIDS-NHL. The comparative analysis of the PEL profiles versus those of normal and malignant B cells identified several genes and their products that were not previously associated with PEL. They included aquaporin-3, a water channel protein involved in water transport; the P-selectin glycoprotein ligand PSGL-1/SELPLG, a ligand for P-selectin involved in leukocyte adhesion and upregulated on the cell surface of plasma cells in mice; mucin-1, originally identified as a tumor-associated glycoprotein that is highly upregulated on various tumor types (e.g. adenocarcinoma); and the vitamin D3-receptor which is expressed on various cell types of the immune system (Fig. 4).
Figure 4.
(A,B,C). Expression of Aquaporin3 (A), P-selectin glycoprotein ligand (B) and Vitamin D receptor (C) on CRO-AP/5 (B,C) and CRO-AP/3 (A) PEL-derived cell lines. Cytospin preparations, avidin-biotin-peroxidase complex immunostaining, hematoxylin counterstain; original magnification, x250.
Proteomics
Inoculation of a KSHV-associated PEL cell line into the peritoneal cavity of severe combined immunodeficiency mice resulted in the formation of effusion and solid lymphomas in the peritoneal cavity. Proteomics using two-dimensional difference gel electrophoresis and DNA microarray analyses identified 14 proteins and 105 genes, respectively, whose expression differed significantly between effusion and solid lymphomas. Among these, 49 and 56 genes were identified as showing higher expression in effusion and solid lymphomas, respectively. The group showing predominant expression in effusion lymphoma contained transactivator/cell cycle-associated genes (MAPKAPK2, C/EBPD, G protein-coupled receptor, RRAS, etc), enzymes and a cell surface antigen (CD68). The group showing predominant expression in solid lymphoma contained structural proteins (collagens, proteoglycans), adhesion molecules (integrins) and cell cycle-associated genes (MAPKs, IRF1, etc.). Moreover, KSHV-encoded lytic proteins, including viral interleukin- 6, were highly expressed in effusion lymphoma compared with solid lymphoma. These data suggested that differences in gene and protein expression between effusion and solid lymphomas may be associated with the formation of effusion lymphoma or invasive features of solid lymphoma [88].
Unresolved research issues
Taken together, the PEL cell lines display unique features, are clearly distinct from other lymphoma cell lines, represent important model systems for the study of the pathology of PEL and are useful tools for the analysis of KSHV. Notably, PEL have been instrumental in determining the genomic sequence of KSHV as well as in establishing the expression pattern and function of several of the genes harbored by the virus [89–94]. Furthermore, PEL cell lines represent an indispensable tool for the understanding of the impact of KSHV biology on the pathology of PEL. Ongoing research should lead to a deeper understanding of additional questions relevant to the pathobiology of PEL, with the hope of eventual improvement in patient care. Aspects of PEL that merit further investigation include:
The peculiar propensity of PEL to involve body cavity surfaces. This propensity could be the result of a typical homing pattern induced by KSHV infection. Data mainly derived from PEL cell lines point to heterogeneity in the expression of homing receptors, with no univocal pattern [64,67]. In line with these data, is the fact that PEL tumor cells are potentially able to form also solid tumor masses, as observed in a minority of PEL patients and in animal models [3,4,6,7,33,88,95]. Nevertheless, mechanism whereby the majority of patients present with primary lymphomatous effusions remains unresolved.
Identification of the cellular products responsible for the scarce cohesiveness and liquid growth pattern of PEL may provide insights into the mechanisms responsible for cell-to-cell and cell-to-extracellular matrix adhesion of normal and neoplastic B cells.
The reasons for the unique clinical presentation of PEL, as to regards the lack of invasive or destructive growth patterns, may also be clarified through the investigation of PEL cell adhesion mechanisms. For example, the invariable expression by PEL of CD138/syndecan-1, which has been shown to bind several extracellular matrix molecules, may cause enhanced adhesiveness to extracellular matrix components, and may therefore account for the lack of invasive growth pattern of this lymphoma [15].
Acknowledgements
This work was supported in part by a Grant from the Ministero della Salute, Rome, within the framework of the “Progetto Integrato Oncologia-Advanced Molecular Diagnostics” project (RFPS-2006-2-342010.7) (to AC) and National Institutes of Health/National Cancer Institute grants R01CA068939 and R01CA103646 (to EC).
Footnotes
Contribution: A.C. designed the Review. All authors contributed to the writing and proofreading of the paper
References
- 1.Banks PM, Warnke RA. Primary effusion lymphoma. In: Jaffe ES, Harris NL, Stein H, Vardiman JW, editors. World Health Organization Classification of Tumours, Pathology and Genetics of Tumours of Haematopoietic and Lymphoid Tissues. Lyon: IARC Press; 2001. pp. 179–180. [Google Scholar]
- 2.Cesarman E, Chang Y, Moore PS, Said JW, Knowles DM. Kaposi's sarcoma-associated herpesvirus-like DNA sequences in AIDS-related body-cavity-based lymphomas. N Engl J Med. 1995;332:1186–1191. doi: 10.1056/NEJM199505043321802. [DOI] [PubMed] [Google Scholar]
- 3.Nador RG, Cesarman E, Chadburn A, Dawson DB, Ansari MQ, Sald J, et al. Primary effusion lymphoma: a distinct clinicopathologic entity associated with the Kaposi's sarcoma-associated herpes virus. Blood. 1996;88:645–656. [PubMed] [Google Scholar]
- 4.Carbone A, Gloghini A, Vaccher E, Zagonel V, Pastore C, Dalla Palma P, et al. Kaposi's sarcoma-associated herpesvirus DNA sequences in AIDS-related and AIDS-unrelated lymphomatous effusions. Br J Haematol. 1996;94:533–543. doi: 10.1046/j.1365-2141.1996.d01-1826.x. [DOI] [PubMed] [Google Scholar]
- 5.Carbone A, Gloghini A. KSHV/HHV8-associated lymphomas. Br J Haematol. 2008;140:13–24. doi: 10.1111/j.1365-2141.2007.06879.x. [DOI] [PubMed] [Google Scholar]
- 6.Chadburn A, Hyjek E, Mathew S, Cesarman E, Said J, Knowles DM. KSHV-positive solid lymphomas represent an extra-cavitary variant of primary effusion lymphoma. Am J Surg Pathol. 2004;28:1401–1416. doi: 10.1097/01.pas.0000138177.10829.5c. [DOI] [PubMed] [Google Scholar]
- 7.Carbone A, Gloghini A, Vaccher E, Cerri M, Gaidano G, Dalla-Favera R, et al. Kaposi's sarcoma-associated herpesvirus/human herpesvirus type 8-positive solid lymphomas. A tissue-based variant of primary effusion lymphoma. J Mol Diagn. 2005;7:17–27. doi: 10.1016/S1525-1578(10)60004-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bouvard V, Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F for the WHO International Agency for Research on Cancer Monograph Working Group. A review of human carcinogens--Part B: biological agents. Lancet Oncol. 2009;10:321–322. doi: 10.1016/s1470-2045(09)70096-8. [DOI] [PubMed] [Google Scholar]
- 9.Said J, Cesarman E. Primary effusion lymphoma. In: Swerdlow SH, Campo E, Harris NL, Jaffe E, Pileri SA, Stein H, et al., editors. World Health Organization Classification of Tumours, Pathology and Genetics of Tumours of Haematopoietic and Lymphoid Tissues. Lyon: IARC Press; 2008. pp. 260–261. [Google Scholar]
- 10.Rainbow L, Platt GM, Simpson GR, et al. The 222- to 234-kilodalton latent nuclear protein (LNA) of Kaposi's sarcoma-associated herpesvirus (human herpesvirus 8) is encoded by orf73 and is a component of the latency-associated nuclear antigen. J Virol. 1997;71:5915–5921. doi: 10.1128/jvi.71.8.5915-5921.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drexler HG, Uphoff CC, Gaidano G, Carbone A. Lymphoma cell lines: in vitro models for the study of HHV-8+ primary effusion lymphomas (body cavity-based lymphomas) Leukemia. 1998;12:1507–1517. doi: 10.1038/sj.leu.2401160. [DOI] [PubMed] [Google Scholar]
- 12.Drexler HG, Meyer C, Gaidano G, Carbone A. Constitutive cytokine production by primary effusion (body cavity-based) lymphoma-derived cell lines. Leukemia. 1999;13:634–640. doi: 10.1038/sj.leu.2401371. [DOI] [PubMed] [Google Scholar]
- 13.Gaidano G, Capello D, Fassone L, Gloghini A, Cilia AM, Ariatti C, et al. Molecular characterization of HHV-8 positive primary effusion lymphoma reveals pathogenetic and histogenetic features of the disease. J Clin Virol. 2000;16:215–224. doi: 10.1016/s1386-6532(99)00082-7. [DOI] [PubMed] [Google Scholar]
- 14.Knowles DM, Inghirami G, Ubriaco A, Dalla-Favera R. Molecular genetic analysis of three AIDS-associated neoplasms of uncertain lineage demonstrates their B-cell derivation and the possible pathogenetic role of the Epstein-Barr virus. Blood. 1989;73:792–799. [PubMed] [Google Scholar]
- 15.Walts AE, Shintaku IP, Said JW. Diagnosis of malignant lymphoma in effusions from patients with AIDS by gene rearrangement. Am J Clin Path. 1990;94:170–175. doi: 10.1093/ajcp/94.2.170. [DOI] [PubMed] [Google Scholar]
- 16.Carbone A, Gaidano G. HHV-8 positive body cavity-based lymphoma: A novel lymphoma entity. Br J Haematol. 1997;97:515–522. doi: 10.1046/j.1365-2141.1997.00064.x. [DOI] [PubMed] [Google Scholar]
- 17.Gaidano G, Carbone A. Primary effusion lymphoma A liquid phase lymphoma of fluid-filled body cavities. Adv Cancer Res. 2001;80:115–146. doi: 10.1016/s0065-230x(01)80014-2. [DOI] [PubMed] [Google Scholar]
- 18.Carbone A, Gloghini A. HHV-8 associated lymphoma. “State of art”. Acta Haematol. 2007;117:129–131. doi: 10.1159/000097459. [DOI] [PubMed] [Google Scholar]
- 19.Conconi A, Carbone A. Primary effusion lymphoma. In: Cavalli F, Stein H, Zucca E, editors. Extranodal Lymphomas. Pathology and Management. London: Informa Healthcare; 2008. pp. 299–306. [Google Scholar]
- 20.Brimo F, Michel RP, Khetani K, Auger M. Primary effusion lymphoma: a series of 4 cases and review of the literature with emphasis on cytomorphologic and immunocytochemical differential diagnosis. Cancer Cytopathol. 2007;111:224–233. doi: 10.1002/cncr.22691. [DOI] [PubMed] [Google Scholar]
- 21.Coupland SE, Charlotte F, Mansour G, Maloum K, Hummel M, Stein H. HHV-8-associated T-cell lymphoma in a lymph node with concurrent peritoneal effusion in an HIV-positive man. Am J Surg Pathol. 2005;29:647–652. doi: 10.1097/01.pas.0000157937.01624.1d. [DOI] [PubMed] [Google Scholar]
- 22.Said JW, Shintaku IP, Asou H, deVos S, Baker J, Hanson G, et al. Herpesvirus 8 inclusions in primary effusion lymphoma: report of a unique case with T-cell phenotype. Arch Pathol Lab Med. 1999;123:257–260. doi: 10.5858/1999-123-0257-HIIPEL. [DOI] [PubMed] [Google Scholar]
- 23.Carbone A, Cesarman E, Spina M, Gloghini A, Schulz TF. HIV-associated lymphomas and gamma-herpesviruses. Blood. 2009;113:1213–1224. doi: 10.1182/blood-2008-09-180315. [DOI] [PubMed] [Google Scholar]
- 24.Morassut S, Vaccher E, Balestreri L, Gloghini A, Gaidano G, Volpe R, et al. HIV-associated HHV-8 positive primary lymphomatous effusions: Radiological findings in six patients. Radiology. 1997;205:459–463. doi: 10.1148/radiology.205.2.9356629. [DOI] [PubMed] [Google Scholar]
- 25.Conconi A, Spina M, Ascoli V, Lopez-Guillermo A, Cortelazzo S, Re A, et al. An IELSG international survey on Primary Effusion Lymphoma (PEL) Blood. 2004;104 3265 (abstr) [Google Scholar]
- 26.Schulz TF. Epidemiology of Kaposi’s sarcoma-associated herpesvirus/ human herpesvirus 8. Adv Cancer Res. 1999;76:121–160. doi: 10.1016/s0065-230x(08)60775-7. [DOI] [PubMed] [Google Scholar]
- 27.Simonelli C, Spina M, Cinelli R, Talamini R, Tedeschi R, Gloghini A, et al. Clinical Features and Outcome of Primary Effusion Lymphoma in HIV-Infected Patients: A Single-Institution Study. J Clin Oncol. 2003;21:3948–3954. doi: 10.1200/JCO.2003.06.013. [DOI] [PubMed] [Google Scholar]
- 28.Boulanger E, Gerard L, Gabarre J, Molina JM, Rapp C, Abino JF, et al. Prognostic factors and outcome of human herpesvirus 8-associated primary effusion lymphoma in patients with AIDS. J Clin Oncol. 2005;23:4372–4380. doi: 10.1200/JCO.2005.07.084. [DOI] [PubMed] [Google Scholar]
- 29.Das DK. Serous effusions in malignant lymphomas: a review. Diagn Cytopathol. 2006;34:335–347. doi: 10.1002/dc.20432. [DOI] [PubMed] [Google Scholar]
- 30.Cesarman E, Nador RG, Aozasa K, Delsol G, Said JW, Knowles DM. Kaposi's sarcoma-associated herpesvirus in non-AIDS related lymphomas occurring in body cavities. Am J Pathol. 1996;149:53–57. [PMC free article] [PubMed] [Google Scholar]
- 31.Kobayashi Y, Kamitsuji Y, Kuroda J, Tsunoda S, Uoshima N, Kimura S, et al. Comparison of human herpes virus 8 related primary effusion lymphoma with human herpes virus 8 unrelated primary effusion lymphoma-like lymphoma on the basis of HIV: report of 2 cases and review of 212 cases in the literature. Acta Haematol. 2007;117:132–144. doi: 10.1159/000097460. [DOI] [PubMed] [Google Scholar]
- 32.Matsumoto Y, Nomura K, Ueda K, Satoh K, Yasuda N, Taki T, et al. Human herpesvirus 8-negative malignant effusion lymphoma. A distinct cilinical entity and successful treatment with rituximab. Leuk Lmphoma. 2005;46:415–419. doi: 10.1080/10428190400018364. [DOI] [PubMed] [Google Scholar]
- 33.Komanduri KV, Luce JA, McGrath MS, Herndier BG, Ng VL. The natural history and molecular heterogeneity of HIV-associated primary malignant lymphomatous effusions. J Acquir Immune Defic Syndr. 1996;13:215–226. doi: 10.1097/00042560-199611010-00003. [DOI] [PubMed] [Google Scholar]
- 34.Mesri EA, Cesarman E, Arvanitakis L, Rafii S, Moore MA, Posnett DN, et al. Human herpesvirus-8/Kaposi's sarcoma-associated herpesvirus is a new transmissible virus that infects B cells. J Exp Med. 1996;183:2385–2390. doi: 10.1084/jem.183.5.2385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schulz TF. The pleiotropic effects of Kaposi's sarcoma herpesvirus. J Pathol. 2006;208:187–198. doi: 10.1002/path.1904. [DOI] [PubMed] [Google Scholar]
- 36.Chang Y, Moore PS, Talbot SJ, Boshoff CH, Zarkowska T, Godden-Kent, et al. Cyclin encoded by KS herpesvirus. Nature. 1996;382:410. doi: 10.1038/382410a0. [DOI] [PubMed] [Google Scholar]
- 37.Sarek G, Järviluoma A, Ojala PM. KSHV viral cyclin inactivates p27KIP1 through Ser10 and Thr187 phosphorylation in proliferating primary effusion lymphomas. Blood. 2006;107:725–732. doi: 10.1182/blood-2005-06-2534. [DOI] [PubMed] [Google Scholar]
- 38.Järviluoma A, Child ES, Sarek G, Sirimongkolkasem P, Peters G, Ojala PM, et al. Phosphorylation of the cyclin-dependent kinase inhibitor p21Cip1 on serine 130 is essential for viral cyclin-mediated bypass of a p21Cip1-imposed G1 arrest. Mol Cell Biol. 2006;26:2430–2440. doi: 10.1128/MCB.26.6.2430-2440.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ojala PM, Tiainen M, Salven P, Veikkola T, Castaños-Vélez E, Sarid R, et al. Kaposi's sarcoma-associated herpesvirus-encoded v-cyclin triggers apoptosis in cells with high levels of cyclin-dependent kinase 6. Cancer Res. 1999;59:4984–4989. [PubMed] [Google Scholar]
- 40.Koopal S, Furuhjelm JH, Järviluoma A, Jäämaa S, Pyakurel P, Pussinen C, et al. Viral oncogene-induced DNA damage response is activated in Kaposi sarcoma tumorigenesis. PLoS Pathog. 2007;3:1348–1360. doi: 10.1371/journal.ppat.0030140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grundhoff A, Ganem D. Mechanisms governing expression of the v-FLIP gene of Kaposi's sarcoma-associated herpesvirus. J Virol. 2001;75:1857–1863. doi: 10.1128/JVI.75.4.1857-1863.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Low W, Harries M, Ye H, Du MQ, Boshoff C, Collins M. Internal ribosome entry site regulates translation of Kaposi's sarcoma-associated herpesvirus FLICE inhibitory protein. J Virol. 2001;75:2938–2945. doi: 10.1128/JVI.75.6.2938-2945.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Efklidou S, Bailey R, Field N, Noursadeghi M, Collins MK. vFLIP from KSHV inhibits anoikis of primary endothelial cells. J Cell Sci. 2008;121:450–457. doi: 10.1242/jcs.022343. [DOI] [PubMed] [Google Scholar]
- 44.Djerbi M, Screpanti V, Catrina AI, Bogen B, Biberfeld P, Grandien A. The inhibitor of death receptor signaling, FLICE-inhibitory protein defines a new class of tumor progression factors. J Exp Med. 1999;190:1025–1032. doi: 10.1084/jem.190.7.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Medema JP, Scaffidi C, Kischkel FC, Shevchenko A, Mann M, Krammer PH, et al. FLICE is activated by association with the CD95 death-inducing signaling complex (DISC) EMBO J. 1997;16:2794–2804. doi: 10.1093/emboj/16.10.2794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Muzio M, Chinnaiyan AM, Kischkel FC, O'Rourke K, Shevchenko A, Ni J, Scaffidi C, et al. FLICE, a novel FADD-homologous ICE/CED-3-like protease, is recruited to the CD95 (Fas/APO-1) death--inducing signaling complex. Cell. 1996;85:817–827. doi: 10.1016/s0092-8674(00)81266-0. [DOI] [PubMed] [Google Scholar]
- 47.An J, Sun Y, Sun R, Rettig MB. Kaposi's sarcoma-associated herpesvirus encoded vFLIP induces cellular IL-6 expression: the role of the NF-kappaB and JNK/AP1 pathways. Oncogene. 2003;22:3371–3385. doi: 10.1038/sj.onc.1206407. [DOI] [PubMed] [Google Scholar]
- 48.Field N, Low W, Daniels M, Howell S, Daviet L, Boshoff C, et al. KSHV vFLIP binds to IKK-gamma to activate IKK. J Cell Sci. 2003;116:3721–3728. doi: 10.1242/jcs.00691. [DOI] [PubMed] [Google Scholar]
- 49.Guasparri I, Wu H, Cesarman E. The KSHV oncoprotein vFLIP contains a TRAF-interacting motif and requires TRAF2 and TRAF3 for signalling. EMBO Rep. 2006;7:114–119. doi: 10.1038/sj.embor.7400580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Guasparri I, Keller SA, Cesarman E. KSHV vFLIP is essential for the survival of infected lymphoma cells. J Exp Med. 2004;199:993–1003. doi: 10.1084/jem.20031467. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 51.Keller SA, Schattner EJ, Cesarman E. Inhibition of NF-kappaB induces apoptosis of KSHV-infected primary effusion lymphoma cells. Blood. 2000;96:2537–2542. [PubMed] [Google Scholar]
- 52.Godfrey A, Anderson J, Papanastasiou A, Takeuchi Y, Boshoff C. Inhibiting primary effusion lymphoma by lentiviral vectors encoding short hairpin RNA. Blood. 2005;105:2510–2518. doi: 10.1182/blood-2004-08-3052. [DOI] [PubMed] [Google Scholar]
- 53.Offermann MK. Kaposi sarcoma herpesvirus-encoded interferon regulator factors. Curr Top Microbiol Immunol. 2007;312:185–209. doi: 10.1007/978-3-540-34344-8_7. [DOI] [PubMed] [Google Scholar]
- 54.Wies E, Mori Y, Hahn A, Kremmer E, Stürzl M, Fleckenstein B, et al. The viral interferon-regulatory factor-3 is required for the survival of KSHV-infected primary effusion lymphoma cells. Blood. 2008;111:320–327. doi: 10.1182/blood-2007-05-092288. [DOI] [PubMed] [Google Scholar]
- 55.Cannon JS, Nicholas J, Orenstein JM, Mann RB, Murray PG, Browning PJ, et al. Heterogeneity of viral IL-6 expression in HHV-8-associated diseases. J Infect Dis. 1999;180:824–828. doi: 10.1086/314956. [DOI] [PubMed] [Google Scholar]
- 56.Aoki Y, Yarchoan R, Braun J, Iwamoto A, Tosato G. Viral and cellular cytokines in AIDS-related malignant lymphomatous effusions. Blood. 2000;96:1599–1601. [PubMed] [Google Scholar]
- 57.Aoki Y, Jaffe ES, Chang Y, Jones K, Teruya-Feldstein J, Moore PS, et al. Angiogenesis and hematopoiesis induced by Kaposi's sarcoma-associated herpesvirus-encoded interleukin-6. Blood. 1999;93:4034–4043. [PubMed] [Google Scholar]
- 58.Molden J, Chang Y, You Y, Moore PS, Goldsmith MA. A Kaposi's sarcoma-associated herpesvirus-encoded cytokine homolog (vIL-6) activates signaling through the shared gp130 receptor subunit. J Biol Chem. 1997;272:19625–19631. doi: 10.1074/jbc.272.31.19625. [DOI] [PubMed] [Google Scholar]
- 59.Jones KD, Aoki Y, Chang Y, Moore PS, Yarchoan R, Tosato G. Involvement of interleukin-10 (IL-10) and viral IL-6 in the spontaneous growth of Kaposi's sarcoma herpesvirus-associated infected primary effusion lymphoma cells. Blood. 1999;94:2871–2879. [PubMed] [Google Scholar]
- 60.Aoki Y, Tosato G. Role of vascular endothelial growth factor/vascular permeability factor in the pathogenesis of Kaposi's sarcoma-associated herpesvirus-infected primary effusion lymphomas. Blood. 1999;94:4247–4254. [PubMed] [Google Scholar]
- 61.Cesarman E, Moore PS, Rao PH, Inghirami G, Knowles DM, Chang Y. In vitro establishment and characterization of two acquired immunodeficiency syndrome-related lymphoma cell lines (BC-1 and BC-2) containing Kaposi’s sarcoma-associated herpesvirus-like (KSHV) DNA sequences. Blood. 1995;86:2708–2714. [PubMed] [Google Scholar]
- 62.Arvanitakis L, Mesri EA, Nador RG, Said JW, Asch AS, Knowles DM, et al. Establishment and characterization of a primary effusion (body cavity-based) lymphoma cell line (BC-3) harboring Kaposi's sarcoma-associated herpesvirus (KSHV/HHV-8) in the absence of Epstein-Barr virus. Blood. 1996;88:2648–2654. [PubMed] [Google Scholar]
- 63.Renne R, Zhong W, Herndier B, McGrath M, Abbey N, Kedes D, et al. Lytic growth of Kaposi's sarcoma-associated herpesvirus (human herpesvirus 8) in culture. Nat Med. 1996;2:342–346. doi: 10.1038/nm0396-342. [DOI] [PubMed] [Google Scholar]
- 64.Boshoff C, Gao SJ, Healy LE, Matthews S, Thomas AJ, Coignet L, et al. Establishing a KSHV+ cell line (BCP-1) from peripheral blood and characterizing its growth in Nod/SCID mice. Blood. 1998;91:1671–1679. [PubMed] [Google Scholar]
- 65.Lacoste V, Judde JG, Bestett G, Cadranel J, Antoine M, Valensi F, et al. Virological and molecular characterisation of a new B lymphoid cell line, established from an AIDS patient with primary effusion lymphoma, harbouring both KSHV/HHV8 and EBV viruses. Leuk Lymphoma. 2000;38:401–409. doi: 10.3109/10428190009087032. [DOI] [PubMed] [Google Scholar]
- 66.Carbone A, Cilia AM, Gloghini A, Canzonieri V, Pastore C, Todesco M, et al. Establishment of HHV-8-positive and HHV-8-negative lymphoma cell lines from primary lymphomatous effusions. Int J Cancer. 1997;73:562–569. doi: 10.1002/(sici)1097-0215(19971114)73:4<562::aid-ijc18>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 67.Carbone A, Cilia AM, Gloghini A, Capello D, Todesco M, Quattrone S, et al. Establishment and characterization of EBV-positive and EBV-negative primary effusion lymphoma cell lines harbouring human herpesvirus type-8. Br J Haematol. 1998;102:1081–1089. doi: 10.1046/j.1365-2141.1998.00877.x. [DOI] [PubMed] [Google Scholar]
- 68.Carbone A, Cilia AM, Gloghini A, Capello D, Fassone L, Perin T, et al. Characterization of a novel HHV-8-positive cell line reveals implications for the pathogenesis and cell cycle control of primary effusion lymphoma. Leukemia. 2000;14:1301–1309. doi: 10.1038/sj.leu.2401802. [DOI] [PubMed] [Google Scholar]
- 69.Cannon JS, Ciufo D, Hawkins AL, Griffin CA, Borowitz MJ, Hayward GS, et al. A new primary effusion lymphoma-derived cell line yields a highly infectious Kaposi's sarcoma herpesvirus-containing supernatant. J Virol. 2000;74:10187–10193. doi: 10.1128/jvi.74.21.10187-10193.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Waller EK, Ziemianska M, Bangs CD, Cleary M, Weissman I, Kamel OW. Characterization of posttransplant lymphomas that express T-cell-associated markers:immunophenotypes, molecular genetics, cytogenetics,and heterotransplantation in severe combined immunodeficient mice. Blood. 1993;82:247–261. [PubMed] [Google Scholar]
- 71.Miyagi J, Masuda M, Takasu N, Nagasaki A, Shinjyo T, Uezato H, et al. Establishment of a primary effusion lymphoma cell line (RM-P1) and in vivo growth system using SCID mice. Int J Hematol. 2002;76:165–172. doi: 10.1007/BF02982580. [DOI] [PubMed] [Google Scholar]
- 72.Katano H, Hoshino Y, Morishita Y, Nakamura T, Satoh H, Iwamoto A, et al. Establishing and characterizing a CD30-positive cell line harboring HHV-8 from a primary effusion lymphoma. J Med Virol. 1999;58:394–401. [PubMed] [Google Scholar]
- 73.Gaidano G, Cechova K, Chang Y, Moore PS, Knowles DM, Dalla-Favera R. Establishment of AIDS-related lymphoma cell lines from lymphomatous effusions. Leukemia. 1996;10:1237–1240. [PubMed] [Google Scholar]
- 74.Said W, Chien K, Takeuchi S, Tasaka T, Asou H, Cho SK, et al. Kaposi's sarcoma-associated herpesvirus (KSHV or HHV8) in primary effusion lymphoma: ultrastructural demonstration of herpesvirus in lymphoma cells. Blood. 1996;87:4937–4943. [PubMed] [Google Scholar]
- 75.Goy A, Ramdas L, Remache YK, Gu J, Fayad L, Hayes KJ, et al. Establishment and characterization by gene expression profiling of a new diffuse large B-cell lymphoma cell line, EJ-1, carrying t(14;18) and t(8;14) translocations. Lab Invest. 2003;83:913–916. doi: 10.1097/01.lab.0000074890.89650.ad. [DOI] [PubMed] [Google Scholar]
- 76.Li Z, Pan L, Cesarman E, Knowles DM. Alterations of mRNA splicing in primary effusion lymphomas. Leuk Lymphoma. 2003;44:833–840. doi: 10.1080/1042819031000068043. [DOI] [PubMed] [Google Scholar]
- 77.Gradoville L, Gerlach J, Grogan E, Shedd D, Nikiforow S, Metroka C, et al. Kaposi's sarcoma-associated herpesvirus open reading frame 50/Rta protein activates the entire viral lytic cycle in the HH-B2 primary effusion lymphoma cell line. J Virol. 2000;74:6207–6212. doi: 10.1128/jvi.74.13.6207-6212.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wu W, Rochford R, Toomey L, Harrington W, Jr, Feuer G. Inhibition of HHV-8/KSHV infected primary effusion lymphomas in NOD/SCID mice by azidothymidine and interferon-alpha. Leuk Res. 2005;29:545–555. doi: 10.1016/j.leukres.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 79.Brander C, Suscovich T, Lee Y, Nguyen PT, O'Connor P, Seebach J, et al. Impaired CTL recognition of cells latently infected with Kaposi's sarcoma-associated herpes virus. J Immunol. 2000;165:2077–2083. doi: 10.4049/jimmunol.165.4.2077. [DOI] [PubMed] [Google Scholar]
- 80.Drexler HG. Guide to Leukemias-Lymphoma Cell Lines. Ebook on CD, Braunschweig. 2005 [Google Scholar]
- 81.Keller SA, Hernandez-Hopkins D, Vider J, Ponomarev V, Hyjek E, Schattner EJ, et al. NF-kappaB is essential for the progression of KSHV- and EBV-infected lymphomas in vivo. Blood. 2006;107:3295–3302. doi: 10.1182/blood-2005-07-2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Taira T, Nagasaki A, Tomoyose T, Miyagi J, Kakazu N, Makino S, et al. Establishment of a human herpes virus-8-negative malignant effusion lymphoma cell line (STR-428) carrying concurrent translocations of BCL2 and c-MYC genes. Leuk Res. 2007;31:1285–1292. doi: 10.1016/j.leukres.2006.12.023. [DOI] [PubMed] [Google Scholar]
- 83.Foreman KE, Friborg J, Jr, Kong WP, Woffendin C, Polverini PJ, Nickoloff BJ, et al. Propagation of a human herpesvirus from AIDS-associated Kaposi's sarcoma. N Engl J Med. 1997;336:163–171. doi: 10.1056/NEJM199701163360302. [DOI] [PubMed] [Google Scholar]
- 84.Renne R, Blackbourn D, Whitby D, Levy J, Ganem D. Limited transmission of Kaposi's sarcoma-associated herpesvirus in cultured cells. J Virol. 1998;72:5182–5188. doi: 10.1128/jvi.72.6.5182-5188.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Jenner RG, Maillard K, Cattini N, Weiss RA, Boshoff C, Wooster R, et al. Kaposi’s sarcoma-associated herpesvirus- infected primary effusion lymphoma has a plasma cell gene expression profile. Proc Natl Acad Sciences U S A. 2003;100:10399–10404. doi: 10.1073/pnas.1630810100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Klein U, Gloghini A, Gaidano G, Chadburn A, Cesarman E, Dalla-Favera R, et al. Gene expression profile analysis of AIDS-related primary effusion lymphoma (PEL) suggests a plasmablastic derivation and identifies PEL-specific transcripts. Blood. 2003;101:4115–4121. doi: 10.1182/blood-2002-10-3090. [DOI] [PubMed] [Google Scholar]
- 87.Fan W, Bubman D, Chadburn A, Harrington WJ, Jr, Cesarman E, Knowles DM. Distinct subsets of primary effusion lymphoma can be identified based on their cellular gene expression profile and viral association. J Virol. 2005;79:1244–1251. doi: 10.1128/JVI.79.2.1244-1251.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yanagisawa Y, Sato Y, Asahi-Ozaki Y, Ito E, Honma R, Imai J, et al. Effusion and solid lymphomas have distinctive gene and protein expression profiles in an animal model of primary effusion lymphoma. J Pathol. 2006;209:464–473. doi: 10.1002/path.2012. [DOI] [PubMed] [Google Scholar]
- 89.Boshoff C, Weiss RA. Kaposi's sarcoma-associated herpesvirus. Adv Cancer Res. 1998;75:57–86. doi: 10.1016/s0065-230x(08)60739-3. [DOI] [PubMed] [Google Scholar]
- 90.Moore PS, Chang Y. Antiviral activity of tumor-suppressor pathways: clues from molecular piracy by KSHV. Trends Genet. 1998;14:144–150. doi: 10.1016/s0168-9525(98)01408-5. [DOI] [PubMed] [Google Scholar]
- 91.Russo JJ, Bohenzky RA, Chien MC, Chen J, Yan M, Maddalena D, et al. Nucleotide sequence of the Kaposi sarcoma-associated herpesvirus (HHV8) Proc Natl Acad Sci U S A. 1996;93:14862–14867. doi: 10.1073/pnas.93.25.14862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sarid R, Olsen SJ, Moore PS. Kaposi's sarcoma-associated herpesvirus: epidemiology, virology, and molecular biology. Adv Virus Res. 1999;52:139–232. doi: 10.1016/s0065-3527(08)60299-7. [DOI] [PubMed] [Google Scholar]
- 93.Schulz TF. Kaposi's sarcoma-associated herpesvirus (human herpesvirus-8) J Gen Virol. 1998;79:1573–1591. doi: 10.1099/0022-1317-79-7-1573. [DOI] [PubMed] [Google Scholar]
- 94.Schulz TF, Moore PS. Kaposi's sarcoma-associated herpesvirus: a new human tumor virus, but how? Trends Microbiol. 1999;7:196–200. doi: 10.1016/s0966-842x(99)01495-x. [DOI] [PubMed] [Google Scholar]
- 95.Picchio GR, Sabbe RE, Gulizia RJ, McGrath M, Herndier BG, Mosier DE. The KSHV/HHV8-infected BCBL-1 lymphoma line causes tumors in SCID mice but fails to transmit virus to a human peripheral blood mononuclear cell graft. Virol. 1997;238:22–29. doi: 10.1006/viro.1997.8822. [DOI] [PubMed] [Google Scholar]