Abstract
Aim:
The aim is to review and discuss the strategies available for use of platelet rich fibrin as healing aid in dentistry.
Background:
Platelet rich fibrin (PRF) is a fibrin matrix in which platelet cytokines, growth factors, and cells are trapped and may be released after a certain time and that can serve as a resorbable membrane. Choukroun and his associates were amongst the pioneers for using PRF protocol in oral and maxillofacial surgery to improve bone healing in implant dentistry. Autologous PRF is considered to be a healing biomaterial, and presently, studies have shown its application in various disciplines of dentistry.
Materials and Methods:
By using specific keywords, electronic search of scientific papers was carried out on the entire PubMed database with custom range of 5 years. The electronic search yielded 302 papers; based on inclusion and exclusion criteria which were specifically predetermined, 72 papers were identified as suitable to the inclusion criteria and the remaining 230 papers were excluded. After adding three more selected papers through hand search, full text of all the articles retrieved and review was done. By pooling the extracted data from selected papers, the reviewed data was synthesized.
Conclusion:
Recently by showing good promising results with use of the PRF, it has proved to have a good prospect for its use as healing aid in various aspects of the dentistry.
Keywords: Growth factors, platelet rich fibrin, platelet rich plasma, wound healing
INTRODUCTION
Development of the bioactive surgical additives is one of the great challenges of clinical research which has been used to regulate inflammation and increase the speed of healing process.[1] A wide range of intra- and extraarticular events and various signaling proteins mediate and regulate the healing process of both hard and soft tissues, respectively. But understanding this entire process is still incomplete; however, it is known that platelets play a crucial role not only in hemostasis, but also in the wound healing process.[2]
In 1974, platelets regenerative potentiality was introduced, and Ross et al.,[3] were first to describe a growth factor from platelets. After activation of the platelets which are trapped within fibrin matrix, growth factors released and stimulate the mitogenic response in the bone periosteum during normal wound healing for repair of the bone.[4] Better understanding of physiologic properties of platelets in wound healing since last two decades led to increase its therapeutic applications in the various forms showing varying results.
MATERIALS AND METHODS
Structured electronic search of scientific papers published up to 15th March 2013 was carried out on the (http://www.ncbi.nlm.nih.gov/pubmed) entire PubMed database with a custom range of 5 years and hand search for term “platelet rich fibrin” (PRF); which was further filtered using Boolean operators (AND, OR, NOT) and combination of specific keywords as following: “Platelet rich fibrin Choukroun”, “platelet rich fibrin in dentistry”, “platelet rich fibrin dental”, “platelet rich fibrin in maxillofacial surgery”, “platelet rich fibrin implant”, “platelet rich fibrin periodontal”, “platelet rich fibrin extraction”, and “platelet rich fibrin oral”; abstracts of all relevant papers were thoroughly scrutinized and in the end and articles pertaining to the topic (PRF) were included. Relevant literature for “platelet rich fibrin” in common dental textbooks and for additional information bibliographies of papers and review articles together with appropriate peer reviewed journals were also scrutinized. The inclusion criteria set for this review were: All case reports, case series, original research papers, review papers, in vitro/in vivo studies, animal studies, and controlled clinical trials on PRF used in dentistry related studies. Exclusion criteria consisted of studies that did not meet the above inclusion criteria.
The electronic search yielded 302 papers, out of which 72 were identified as suitable papers to the inclusion criteria and the remaining 230 were excluded [Figure 1]. Only 75 papers selected, 72 from electronic search and three from other searches and full text of all articles retrieved and reviewed [Table 1], out of which 22 in vivo studies, 13 in vitro studies, 14 case reports, 11 animal studies, six controlled clinical trials, two combined in vivo and in vitro studies, and seven reviews [Figure 2].
Figure 1.
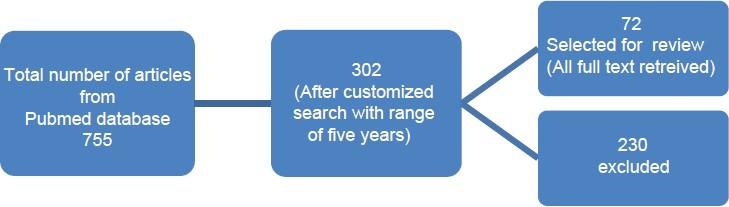
Search flowchart on PubMed database
Table 1.
Literature on platelet rich fibrin
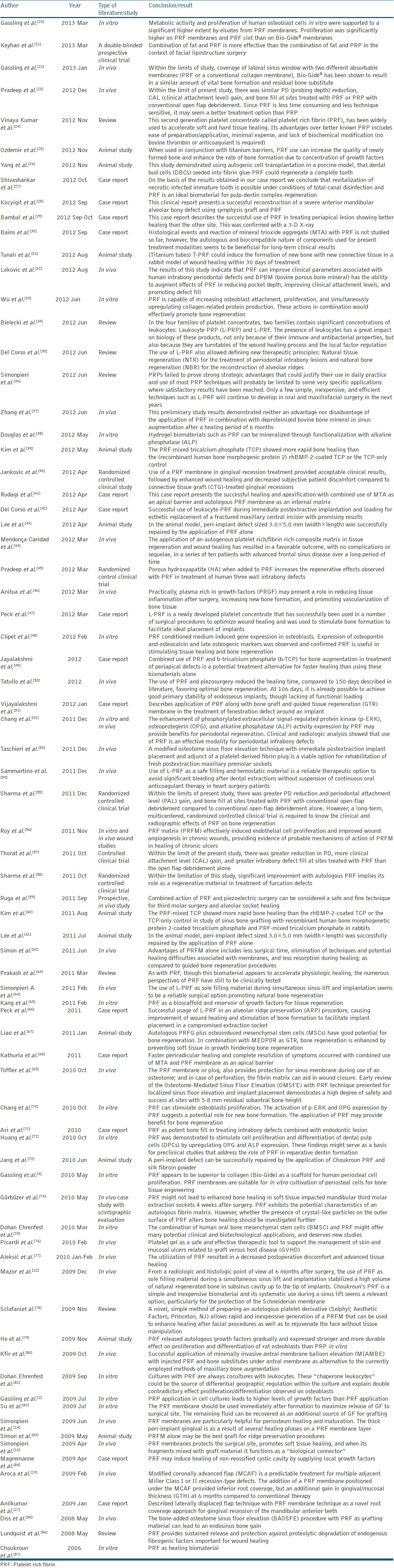
Figure 2.
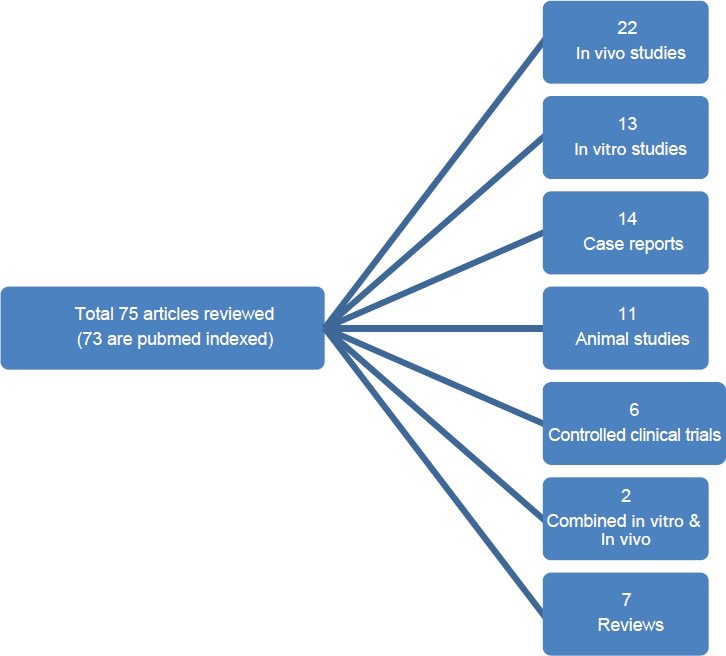
Flowchart of total scrutinized articles
PLATELET CONCENTRATE EVOLUTION
Platelets isolated from the peripheral blood acts as autologous source of growth factors. In general medical practice, platelet concentrate which is derived from blood can be used for the prevention and treatment of bleeding due to conditions like severe thrombocytopenia, severe oral hemorrhage associated with medullary aplasia, acute leukemia, etc.[5] The use of fibrin adhesives helps to initiate the development of platelet concentrate as a bioactive surgical additive. Several components in blood has been recognized since 1990, which are a part of the natural healing process and have the potential to accelerate wound healing when added to wounded tissues or surgical sites. In 1970, fibrin glue formed by polymerizing fibrinogen with thrombin and calcium was first described. Actually, it was prepared using donor plasma; but the stability and quality of fibrin glue was low because of low concentration of fibrinogen in plasma. These fibrin adhesives can be derived autologously from the patient or can be obtained commercially, but with a small risk of disease transmission for the latter one.
PLATELET RICH PLASMA
It has been shown in several studies that bone regenerative procedures may be enhanced by the addition of specific growth factors.[6] platelet rich plasma (PRP) was used as a method of introducing concentrated growth factors platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), and insulin-like growth factor 1 (IGF-1) to the surgical site, thereby enriching the natural blood clot in order to hasten wound healing and stimulate bone regeneration.[7] A natural human blood clot consists of 95% red blood cells (RBCs), 5% platelets, less than 1% white blood cells (WBCs), and numerous amounts of fibrin strands. A PRP blood clot, on the other hand, contains 4% RBCs, 95% platelets, and 1% WBCs.[6] The PRP preparation protocol requires collection of blood with anticoagulant, centrifugation in two steps, and induced polymerization of the platelet concentrate using calcium chloride and bovine thrombin.[8] PRP has been used in conjunction with different grafting materials in bone augmentation procedures since the day of its introduction; the results from these studies are controversial and no conclusions can be drawn regarding the bone regenerative effect of PRP till date.
PRF
PRF represents a new revolutionary step in the platelet gel therapeutic concept.[1] Unlike other platelet concentrates, this technique does not require any gelifying agent, but not more than centrifugation of the natural blood without additives.[8] Choukroun et al.,[9] developed the PRF in 2001 at France and the production protocol of PRF attempts to accumulate platelets and released cytokines in a fibrin clot. Actually the platelets and leukocyte cytokines are important part in role play of this biomaterial, but the fibrin matrix supporting them is very helpful in constituting the determining elements responsible for real therapeutic potential of PRF.[1] Cytokines are immediately used and destroyed in a healing wound. The harmony between cytokines and their supporting fibrin matrix has much more unique importance than any other constant. A fibrin glue, enriched with cytokines (such as PRP) with large uncontrollable and short-term effect is less better than a physiologic fibrin matrix (such as PRF) with good and better effects.
ADVANTAGES OF PRF OVER PRP
No biochemical handling of blood.[15]
Simplified and cost-effective process.[15]
Use of bovine thrombin and anticoagulants not required.[15]
Favorable healing due to slow polymerization.[15]
More efficient cell migration and proliferation.[15]
PRF has supportive effect on immune system.[15]
PRF helps in hemostasis.[15]
PREPARATION OF PRF
The protocol for PRF preparation is very simple and simulates that of PRP. It includes collection of whole venous blood (around 5 ml) in each of the two sterile vacutainer tubes (6 ml) without anticoagulant and the vacutainer tubes are then placed in a centrifugal machine [Figure 3] at 3,000 revolutions per minute (rpm) for 10 min, after which it settles into the following three layers: Upper straw-colored acellular plasma, red-colored lower fraction containing red blood cells (RBCs), and the middle fraction containing the fibrin clot [Figure 4]. The upper straw-colored layer is then removed and middle fraction is collected, 2 mm below to the lower dividing line, which is the PRF [Figure 5]. The mechanism involved in this is; the fibrinogen concentrated in upper part of the tube, combines with circulating thrombin due to centrifugation to form fibrin. A fibrin clot is then formed in the middle between the red corpuscles at bottom and acellular plasma at the top. The middle part is platelets trapped massively in fibrin meshes. The success of this technique entirely depends on time gap between the blood collection and its transfer to the centrifuge and it should be done in less time. The blood sample without anticoagulant, starts to coagulate almost immediately upon contact with the glass, and it decreases the time of centrifugation to concentrate fibrinogen. Following proper protocol and quick handling is the only way to obtain a clinically usable PRF clot charged with serum and platelets. Resistant autologous fibrin membranes may be available by driving out the fluids trapped in fibrin matrix.
Figure 3.

Collection of blood, blood in vacutainer tube after centrifugation, and centrifuge machine
Figure 4.
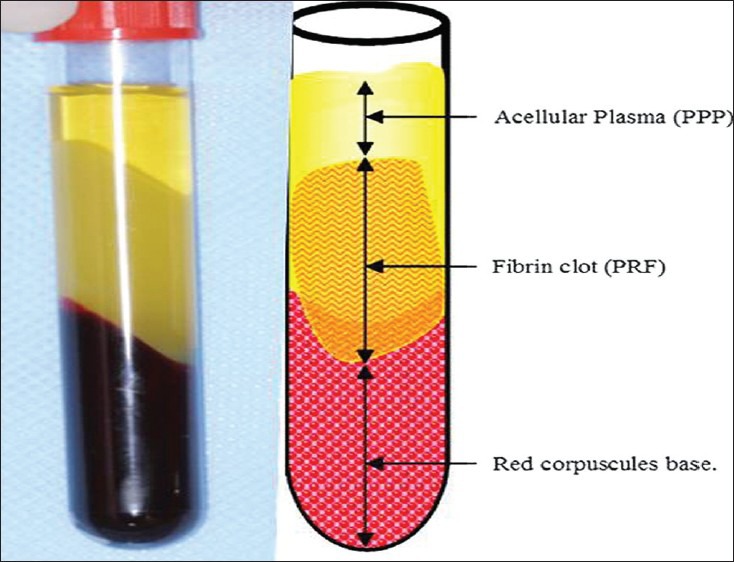
Blood in the vacutainer tubes after centrifugation at 3,000 rpm for 10 min divided into three fractions; lower fraction of red blood cells, middle fraction containing fibrin clot, and upper acellular plasma fraction
Figure 5.

Isolated platelet rich fibrin
CLINICAL APPLICATION
Choukroun et al.,[9] are well known for using autologous PRF protocol in oral and maxillofacial surgery to improve bone healing in implant dentistry.[9] The most common encountered problems are lack of adequate bone and proximity to anatomic structures at the implantation site and recent advancements of PRF usage in surgical procedures can predictably combat such difficulties.
Choukroun et al.,[11] attempted to evaluate the potential of PRF in combination with freeze-dried bone allograft (FDBA) in sinus floor elevation to enhance bone regeneration and nine sinus floor augmentations were performed. Out of nine; in six sites, FDBA with PRF (test group), and in three sites FDBA without PRF (control group) was used. After 4 months, the test group and for the control group after 8 months; bone specimens from the augmented region during the implant insertion procedure were harvested and evaluated. After 4 months of healing time, histologic maturation of the test group appears to be identical to that of the control group which was for a period of 8 months with equivalent quantities for both protocols.[11]
In various bone reconstruction procedures Choukroun's PRF could provide a possible new bone. Mazor et al.,[12] stated that use of PRF as the sole filling material during a simultaneous sinus lift and implantation procedure had stabilized a good amount of regenerated bone in the subsinus cavity up to the tip of implants in a case series through a radiological and histological evaluation at after 6 months from the surgery.[12] Also they advocated that Choukroun's PRF, which is a simple and inexpensive biomaterial in systematic use during a sinus lift seems as an acceptable option.[12]
Simonpieri et al.,[13,14] reported and confirmed the validate usage of PRF membranes in reconstruction protocols along with FDBA, 0.5% metronidazole solution in about 20 patients who were treated using this new technique and followed-up during 1-5 years, and finally 184 dental implants were placed and they found no implant or graft loss in a case series.[13] PRF membranes protects the surgical site; promotes soft tissue healing; and when its fragments mixes with graft material, it functions as a “biological connector” between the different elements of graft and acts as a matrix which supports neoangiogenesis, capture of stem cells, and migration of osteoprogenitor cells to the center of graft.[14]
PRF plugs can also be used in treating the residual extraction sockets.[15] Use of autologous PRF in extracted socket filling after immediate bone augmentation using titanium membranes applied to the socket walls and primary closure was found to be feasible and safe with adequate bone filling after 8 weeks or above for implant fixation.[16]
Anilkumar et al.,[17] has reported PRF as a potential novel root coverage approach for treating gingival recession in mandibular anterior teeth using combined laterally positioned flap technique and PRF membrane.[17] Combined use of PRF and bone graft with good results has also been reported for combined periodontic-endodontic furcation defect.[18] Aroca et al.,[19] in the 6 month of their randomized clinical trial, concluded that addition of a PRF membrane positioned under the MCAF (modified coronally advanced flap) provided inferior root coverage, but an additional gain in gingival/mucosal thickness (GTH) at 6 months compared to conventional therapy [Table 1].[19]
DISCUSSION
PRF first described by Choukroun et al.,[9] is a new second generation of platelet concentrate. Simplified processing technique without any complex handling makes it superior to PRP. PRF can be used to promote wound healing, bone regeneration, graft stabilization, wound sealing, and hemostasis. Because the fibrin matrix is better organized, it is able to more efficiently direct stem cell migration and the healing program. Release of growth factors from PRF through in vitro studies and good results from in vivo studies led to optimize the clinical application of PRF. It was shown that there are better results of PRF over PRP. Dohan et al.,[88] proved a slower release of growth factors from PRF than PRP and observed better healing properties with PRF. It was observed and shown that the cells are able to migrate from fibrin scaffold; while some authors demonstrated the PRF as a supportive matrix for bone morphogenetic protein as well.
CONCLUSION
Although PRF belongs to a new generation of platelet concentrates, the biologic activity of fibrin molecule is enough in itself to account for significant cicatricial capacity of the PRF. The slow polymerization mode confers to PRF membrane as a particularly favorable physiologic architecture to support the healing process.
However, it is now necessary to look further into platelet and inflammatory features of this biomaterial. Only a perfect understanding of its components and their significance will enable us to comprehend the clinical results obtained and subsequently extend the fields of therapeutic application of this protocol.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part I: Technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e37–44. doi: 10.1016/j.tripleo.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 2.Gassling VL, Açil Y, Springer IN, Hubert N, Wiltfang J. Platelet-rich plasma and platelet-rich fibrin in human cell culture. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:48–55. doi: 10.1016/j.tripleo.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 3.Ross R, Glomset J, Kariya B, Harker L. A platelet-dependent serum factor that stimulates the proliferation of arterial smooth muscle cells in vitro. Proc Natl Acad Sci U S A. 1974;71:1207–10. doi: 10.1073/pnas.71.4.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gassling V, Douglas T, Warnke PH, Açil Y, Wiltfang J, Becker ST. Platelet-rich fibrin membranes as scaffolds for periosteal tissue engineering. Clin Oral Implants Res. 2010;21:543–9. doi: 10.1111/j.1600-0501.2009.01900.x. [DOI] [PubMed] [Google Scholar]
- 5.Sunitha Raja V, Munirathnam Naidu E. Platelet-rich fibrin: Evolution of a second-generation platelet concentrate. Indian J Dent Res. 2008;19:42–6. doi: 10.4103/0970-9290.38931. [DOI] [PubMed] [Google Scholar]
- 6.Nevins M, Giannobile WV, McGuire MK, Kao RT, Mellonig JT, Hinrichs JE, et al. Platelet-derived growth factor stimulates bone fill and rate of attachment level gain: Results of a large multicenter randomized controlled trial. J Periodontal. 2005;76:2205–15. doi: 10.1902/jop.2005.76.12.2205. [DOI] [PubMed] [Google Scholar]
- 7.Soffer E, Ouhayoun JP, Anagnostou F. Fibrin sealants and platelet preparations in bone and periodontal healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:521–8. doi: 10.1067/moe.2003.152. [DOI] [PubMed] [Google Scholar]
- 8.Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR. Platelet-rich plasma: Growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:638–46. doi: 10.1016/s1079-2104(98)90029-4. [DOI] [PubMed] [Google Scholar]
- 9.Choukroun J, Adda F, Schoeffler C, Vervelle A. Une opportunité en paro-implantologie: Le PRF. Implantodontie. 2001;42:55–62. [Google Scholar]
- 10.Saluja H, Dehane V, Mahindra U. Platelet-Rich fibrin: A second generation platelet concentrate and a new friend of oral and maxillofacial surgeons. Ann Maxillofac Surg. 2011;1:53–7. doi: 10.4103/2231-0746.83158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part V: Histologic evaluations of PRF effects on bone allograft maturation in sinus lift. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:299–303. doi: 10.1016/j.tripleo.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 12.Mazor Z, Horowitz RA, Del Corso M, Prasad HS, Rohrer MD, Dohan Ehrenfest DM. Sinus floor augmentation with simultaneous implant placement using Choukroun's platelet-rich fibrin as the sole grafting material: A radiologic and histologic study at 6 months. J Periodontol. 2009;80:2056–64. doi: 10.1902/jop.2009.090252. [DOI] [PubMed] [Google Scholar]
- 13.Simonpieri A, Del Corso M, Sammartino G, Dohan Ehrenfest DM. The relevance of Choukroun's platelet-rich fibrin and metronidazole during complex maxillary rehabilitations using bone allograft. Part I: A new grafting protocol. Implant Dent. 2009;18:102–11. doi: 10.1097/ID.0b013e318198cf00. [DOI] [PubMed] [Google Scholar]
- 14.Simonpieri A, Del Corso M, Sammartino G, Dohan Ehrenfest DM. The relevance of Choukroun's platelet-rich fibrin and metronidazole during complex maxillary rehabilitations using bone allograft. Part II: Implant surgery, prosthodontics, and survival. Implant Dent. 2009;18:220–9. doi: 10.1097/ID.0b013e31819b5e3f. [DOI] [PubMed] [Google Scholar]
- 15.Toffler M, Toscano N, Holtzclaw D, Corso MD, Dohan Ehrenfest DM. Introducing Choukroun's platelet rich fibrin (PRF) to the reconstructive surgery milieu. J Implant Adv Clin Dent. 2009;1:21–30. [Google Scholar]
- 16.Kfir E, Kfir V, Kaluski E. Immediate bone augmentation after infected tooth extraction using titanium membranes. J Oral Implantol. 2007;33:133–8. doi: 10.1563/1548-1336(2007)33[133:IBAAIT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Anilkumar K, Geetha A, Umasudhakar, Ramakrishnan T, Vijayalakshmi R, Pameela E. Platelet-rich-fibrin: A novel root coverage approach. J Indian Soc Periodontol. 2009;13:50–4. doi: 10.4103/0972-124X.51897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kanakamedala A, Ari G, Sudhakar U, Vijayalakshmi R, Ramakrishana T, Emmadi P. Treatment of a furcation defect with a combination of platelet rich fibrin and bone graft-A case report. ENDO (Lond Engl) 2009;3:127–35. [Google Scholar]
- 19.Aroca S, Keglevich T, Barbieri B, Gera I, Etienne D. Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet-rich fibrin membrane for the treatment of adjacent multiple gingival recessions: A 6-month study. J Periodontol. 2009;80:244–52. doi: 10.1902/jop.2009.080253. [DOI] [PubMed] [Google Scholar]
- 20.Gassling V, Hedderich J, Açil Y, Purcz N, Wiltfang J, Douglas T. Comparison of platelet rich fibrin and collagen as osteoblast-seeded scaffolds for bone tissue engineering applications. Clin Oral Implants Res. 2013;24:320–8. doi: 10.1111/j.1600-0501.2011.02333.x. [DOI] [PubMed] [Google Scholar]
- 21.Keyhan SO, Hemmat S, Badri AA, Abdeshahzadeh A, Khiabani K. Use of platelet-rich fibrin and platelet-rich plasma in combination with fat graft: Which is more effective during facial lipostructure? J Oral Maxillofac Surg. 2013;71:610–21. doi: 10.1016/j.joms.2012.06.176. [DOI] [PubMed] [Google Scholar]
- 22.Gassling V, Purcz N, Braesen JH, Will M, Gierloff M, Behrens E, et al. Comparison of two different absorbable membranes for the coverage of lateral osteotomy sites in maxillary sinus augmentation: A preliminary study. J Craniomaxillofac Surg. 2013;41:76–82. doi: 10.1016/j.jcms.2012.10.015. [DOI] [PubMed] [Google Scholar]
- 23.Pradeep AR, Rao NS, Agarwal E, Bajaj P, Kumari M, Naik SB. Comparative evaluation of autologous platelet-rich fibrin and platelet-rich plasma in the treatment of 3-wall intrabony defects in chronic periodontitis: A randomized controlled clinical trial. J Periodontol. 2012;83:1499–507. doi: 10.1902/jop.2012.110705. [DOI] [PubMed] [Google Scholar]
- 24.Vinaya Kumar R, Shubhashini N. Platelet rich fibrin: A new paradigm in periodontal regeneration. Cell Tissue Bank. 2012 doi: 10.1007/s10561-012-9349-6. [DOI] [PubMed] [Google Scholar]
- 25.Ozdemir H, Ezirganli S, Isa Kara M, Mihmanli A, Baris E. Effects of platelet rich fibrin alone used with rigid titanium barrier. Arch Oral Biol. 2013;58:537–44. doi: 10.1016/j.archoralbio.2012.09.018. [DOI] [PubMed] [Google Scholar]
- 26.Yang KC, Wang CH, Chang HH, Chan WP, Chi CH, Kuo TF. Fibrin glue mixed with platelet-rich fibrin as a scaffold seeded with dental bud cells for tooth regeneration. J Tissue Eng Regen Med. 2012;6:777–85. doi: 10.1002/term.483. [DOI] [PubMed] [Google Scholar]
- 27.Shivashankar VY, Johns DA, Vidyanath S, Kumar MR. Platelet Rich Fibrin in the revitalization of tooth with necrotic pulp and open apex. J Conserv Dent. 2012;15:395–8. doi: 10.4103/0972-0707.101926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kocyigit ID, Tuz HH, Alp YE, Atil F, Tekin U, Coskunses FM. Correction of postsurgical alveolar ridge defect with vertical alveolar distraction of the onlay block graft. J Craniofac Surg. 2012;23:1550–2. doi: 10.1097/SCS.0b013e31825c74b4. [DOI] [PubMed] [Google Scholar]
- 29.Bambal D, Manwar NU, Chandak M, Rudagi K. A comparative evaluation of the healing ability of bilateral periapical lesions treated with and without the use of platelet-rich fibrin. Todays FDA. 2012;24:54–7. [PubMed] [Google Scholar]
- 30.Bains R, Bains VK, Loomba K, Verma K, Nasir A. Management of pulpal floor perforation and grade II Furcation involvement using mineral trioxide aggregate and platelet rich fibrin: A clinical report. Contemp Clin Dent. 2012;3(Suppl 2):S223–7. doi: 10.4103/0976-237X.101100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tunali M, Ozdemir H, Küçükodacı Z, Akman S, Fıratlı E. In vivo evaluation of titanium-prepared platelet-rich fibrin (T-PRF): A new platelet concentrate. Br J Oral Maxillofac Surg. 2012 doi: 10.1016/j.bjoms.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 32.Lekovic V, Milinkovic I, Aleksic Z, Jankovic S, Stankovic P, Kenney EB, et al. Platelet-rich fibrin and bovine porous bone mineral vs. platelet-rich fibrin in the treatment of intrabony periodontal defects. J Periodontal Res. 2012;47:409–17. doi: 10.1111/j.1600-0765.2011.01446.x. [DOI] [PubMed] [Google Scholar]
- 33.Wu CL, Lee SS, Tsai CH, Lu KH, Zhao JH, Chang YC. Platelet-rich fibrin increases cell attachment, proliferation and collagen-related protein expression of human osteoblasts. Aust Dent J. 2012;57:207–12. doi: 10.1111/j.1834-7819.2012.01686.x. [DOI] [PubMed] [Google Scholar]
- 34.Bielecki T, Dohan Ehrenfest DM, Everts PA, Wiczkowski A. The role of leukocytes from L-PRP/L-PRF in wound healing and immune defense: New perspectives. Curr Pharm Biotechnol. 2012;13:1153–62. doi: 10.2174/138920112800624373. [DOI] [PubMed] [Google Scholar]
- 35.Del Corso M, Vervelle A, Simonpieri A, Jimbo R, Inchingolo F, Sammartino G, et al. Current knowledge and perspectives for the use of platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in oral and maxillofacial surgery part 1: Periodontal and dentoalveolar surgery. Curr Pharm Biotechnol. 2012;13:1207–30. doi: 10.2174/138920112800624391. [DOI] [PubMed] [Google Scholar]
- 36.Simonpieri A, Del Corso M, Vervelle A, Jimbo R, Inchingolo F, Sammartino G, et al. Current knowledge and perspectives for the use of platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in oral and maxillofacial surgery part 2: Bone graft, implant and reconstructive surgery. Curr Pharm Biotechnol. 2012;13:1231–56. doi: 10.2174/138920112800624472. [DOI] [PubMed] [Google Scholar]
- 37.Zhang Y, Tangl S, Huber CD, Lin Y, Qiu L, Rausch-Fan X. Effects of Choukroun's platelet-rich fibrin on bone regeneration in combination with deproteinized bovine bone mineral in maxillary sinus augmentation: A histological and histomorphometric study. J Craniomaxillofac Surg. 2012;40:321–8. doi: 10.1016/j.jcms.2011.04.020. [DOI] [PubMed] [Google Scholar]
- 38.Douglas TE, Gassling V, Declercq HA, Purcz N, Pamula E, Haugen HJ, et al. Enzymatically induced mineralization of platelet-rich fibrin. J Biomed Mater Res A. 2012;100:1335–46. doi: 10.1002/jbm.a.34073. [DOI] [PubMed] [Google Scholar]
- 39.Kim BJ, Kwon TK, Baek HS, Hwang DS, Kim CH, Chung IK, et al. A comparative study of the effectiveness of sinus bone grafting with recombinant human bone morphogenetic protein 2-coated tricalcium phosphate and platelet-rich fibrin-mixed tricalcium phosphate in rabbits. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:583–92. doi: 10.1016/j.tripleo.2011.04.029. [DOI] [PubMed] [Google Scholar]
- 40.Jankovic S, Aleksic Z, Klokkevold P, Lekovic V, Dimitrijevic B, Kenney EB, et al. Use of platelet-rich fibrin membrane following treatment of gingival recession: A randomized clinical trial. Int J Periodontics Restorative Dent. 2012;32:e41–50. [PubMed] [Google Scholar]
- 41.Rudagi KB, Rudagi B. One-step apexification in immature tooth using grey mineral trioxide aggregate as an apical barrier and autologus platelet rich fibrin membrane as an internal matrix. J Conserv Dent. 2012;15:196–9. doi: 10.4103/0972-0707.94582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Del Corso M, Mazor Z, Rutkowski JL, Dohan Ehrenfest DM. The use of leukocyte- and platelet-rich fibrin during immediate postextractive implantation and loading for the esthetic replacement of a fractured maxillary central incisor. J Oral Implantol. 2012;38:181–7. doi: 10.1563/AAID-JOI-D-12-CL.3802. [DOI] [PubMed] [Google Scholar]
- 43.Lee JW, Kim SG, Kim JY, Lee YC, Choi JY, Dragos R, et al. Restoration of a peri-implant defect by platelet-rich fibrin. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:459–63. doi: 10.1016/j.tripleo.2011.03.043. [DOI] [PubMed] [Google Scholar]
- 44.Mendonça-Caridad J, Lopez PJ, Fayos FV, Miery G. A novel approach to human cranial tissue regeneration and frontal sinus obliteration with an autogenous platelet rich/fibrin-rich composite matrix: 10 patients with a 6-10 year follow-up. J Tissue Eng Regen Med. 2012 doi: 10.1002/term.534. [DOI] [PubMed] [Google Scholar]
- 45.Pradeep AR, Bajaj P, Rao NS, Agarwal E, Naik SB. Platelet-Rich Fibrin combined with a porous hydroxyapatite graft for the treatment of three-wall intrabony defects in chronic periodontitis: A randomized controlled clinical trial. J Periodontol. 2012 doi: 10.1902/jop.2012.110722. [DOI] [PubMed] [Google Scholar]
- 46.Anitua E, Prado R, Orive G. Bilateral sinus elevation evaluating plasma rich in growth factors technology: A report of five cases. Clin Implant Dent Relat Res. 2012;14:51–60. doi: 10.1111/j.1708-8208.2009.00233.x. [DOI] [PubMed] [Google Scholar]
- 47.Peck MT, Marnewick J, Stephen LX, Singh A, Patel N, Majeed A. The use of leukocyte- and platelet-rich fibrin (L-PRF) to facilitate implant placement in bone-deficient sites: A report of two cases. (58-9).SADJ. 2012;67:54–6. [PubMed] [Google Scholar]
- 48.Clipet F, Tricot S, Alno N, Massot M, Solhi H, Cathelineau G, et al. In vitro effects of Choukroun's platelet-rich fibrin conditioned medium on 3 different cell lines implicated in dental implantology. Implant Dent. 2012;21:51–6. doi: 10.1097/ID.0b013e31822b9cb4. [DOI] [PubMed] [Google Scholar]
- 49.Jayalakshmi KB, Agarwal S, Singh MP, Vishwanath BT, Krishna A, Agrawal R. Platelet Rich Fibrin with β-Tricalcium Phosphate-A noval approach for bone augmentation in chronic periapical lesion: A case report. Case Rep Dent 2012. 2012 doi: 10.1155/2012/902858. 902858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tatullo M, Marrelli M, Cassetta M, Pacifici A, Stefanelli LV, Scacco S, et al. Platelet Rich Fibrin (PRF) in reconstructive surgery of atrophied maxillary bones: Clinical and histological evaluations. Int J Med Sci. 2012;9:872–80. doi: 10.7150/ijms.5119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vijayalakshmi R, Rajmohan CS, Deepalakshmi D, Sivakami G. Use of platelet rich fibrin in a fenestration defect around an implant. J Indian Soc Periodontol. 2012;16:108–12. doi: 10.4103/0972-124X.94616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chang YC, Zhao JH. Effects of platelet-rich fibrin on human periodontal ligament fibroblasts and application for periodontal infrabony defects. Aust Dent J. 2011;56:365–71. doi: 10.1111/j.1834-7819.2011.01362.x. [DOI] [PubMed] [Google Scholar]
- 53.Taschieri S, Del Fabbro M. Postextraction osteotome sinus floor elevation technique using plasma-rich growth factors. Implant Dent. 2011;20:418–24. doi: 10.1097/ID.0b013e3182354063. [DOI] [PubMed] [Google Scholar]
- 54.Sammartino G, Dohan Ehrenfest DM, Carile F, Tia M, Bucci P. Prevention of hemorrhagic complications after dental extractions into open heart surgery patients under anticoagulant therapy: The use of leukocyte- and platelet-rich fibrin. J Oral Implantol. 2011;37:681–90. doi: 10.1563/AAID-JOI-D-11-00001. [DOI] [PubMed] [Google Scholar]
- 55.Sharma A, Pradeep AR. Treatment of 3-wall intrabony defects in patients with chronic periodontitis with autologous platelet-rich fibrin: A randomized controlled clinical trial. J Periodontol. 2011;82:1705–12. doi: 10.1902/jop.2011.110075. [DOI] [PubMed] [Google Scholar]
- 56.Roy S, Driggs J, Elgharably H, Biswas S, Findley M, Khanna S, et al. Platelet-rich fibrin matrix improves wound angiogenesis via inducing endothelial cell proliferation. Wound Repair Regen. 2011;19:753–66. doi: 10.1111/j.1524-475X.2011.00740.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thorat M, Pradeep AR, Pallavi B. Clinical effect of autologous platelet-rich fibrin in the treatment of intra-bony defects: A controlled clinical trial. J Clin Periodontol. 2011;38:925–32. doi: 10.1111/j.1600-051X.2011.01760.x. [DOI] [PubMed] [Google Scholar]
- 58.Sharma A, Pradeep AR. Autologous platelet-rich fibrin in the treatment of mandibular degree II furcation defects: A randomized clinical trial. J Periodontol. 2011;82:1396–403. doi: 10.1902/jop.2011.100731. [DOI] [PubMed] [Google Scholar]
- 59.Ruga E, Gallesio C, Boffano P. Platelet-rich fibrin and piezoelectric surgery: A safe technique for the prevention of periodontal complications in third molar surgery. J Craniofac Surg. 2011;22:1951–5. doi: 10.1097/SCS.0b013e31822ea76b. [DOI] [PubMed] [Google Scholar]
- 60.Kim BJ, Kwon TK, Baek HS, Hwang DS, Kim CH, Chung IK, et al. A comparative study of the effectiveness of sinus bone grafting with recombinant human bone morphogenetic protein 2-coated tricalcium phosphate and platelet-rich fibrin-mixed tricalcium phosphate in rabbits. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011 doi: 10.1016/j.tripleo.2011.04.029. [DOI] [PubMed] [Google Scholar]
- 61.Lee JW, Kim SG, Kim JY, Lee YC, Choi JY, Dragos R, et al. Restoration of a peri-implant defect by platelet-rich fibrin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011 doi: 10.1016/j.tripleo.2011.03.043. [DOI] [PubMed] [Google Scholar]
- 62.Simon BI, Gupta P, Tajbakhsh S. Quantitative evaluation of extraction socket healing following the use of autologous platelet-rich fibrin matrix in humans. Int J Periodontics Restorative Dent. 2011;31:285–95. [PubMed] [Google Scholar]
- 63.Prakash S, Thakur A. Platelet concentrates: Past, present and future. J Maxillofac Oral Surg. 2011;10:45–9. doi: 10.1007/s12663-011-0182-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Simonpieri A, Choukroun J, Del Corso M, Sammartino G, Dohan Ehrenfest DM. Simultaneous sinus-lift and implantation using microthreaded implants and leukocyte- and platelet-rich fibrin as sole grafting material: A six-year experience. Implant Dent. 2011;20:2–12. doi: 10.1097/ID.0b013e3181faa8af. [DOI] [PubMed] [Google Scholar]
- 65.Kang YH, Jeon SH, Park JY, Chung JH, Choung YH, Choung HW, et al. Platelet-rich fibrin is a Bioscaffold and reservoir of growth factors for tissue regeneration. Tissue Eng Part A. 2011;17:349–59. doi: 10.1089/ten.TEA.2010.0327. [DOI] [PubMed] [Google Scholar]
- 66.Peck MT, Marnewick J, Stephen L. Alveolar ridge preservation using leukocyte and platelet-rich fibrin: A report of a case. Case Rep Dent 2011. 2011 doi: 10.1155/2011/345048. 345048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liao HT, Chen CT, Chen CH, Chen JP, Tsai JC. Combination of guided osteogenesis with autologous platelet-rich fibrin glue and mesenchymal stem cell for mandibular reconstruction. J Trauma. 2011;70:228–37. doi: 10.1097/TA.0b013e3181e12b56. [DOI] [PubMed] [Google Scholar]
- 68.Kathuria A, Chaudary S, Talwar S, Verma M. Endodontic management of single rooted immature mandibular second molar with single canal using MTA and platelet-rich fibrin membrane: A case report. J Clin Exp Dent. 2011;3:e487–90. [Google Scholar]
- 69.Toffler M, Toscano N, Holtzclaw D. Osteotome-mediated sinus floor elevation using only platelet-rich fibrin: An early report on 110 patients. Implant Dent. 2010;19:447–56. doi: 10.1097/ID.0b013e3181f57288. [DOI] [PubMed] [Google Scholar]
- 70.Chang IC, Tsai CH, Chang YC. Platelet-rich fibrin modulates the expression of extracellular signal-regulated protein kinase and osteoprotegerin in human osteoblasts. J Biomed Mater Res A. 2010;95:327–32. doi: 10.1002/jbm.a.32839. [DOI] [PubMed] [Google Scholar]
- 71.Ari G, Anil Kumar K, Ramakrishnan T. Treatment of an intrabony defect combined with an endodontic lesion: A case report. Endo (lond Engl) 2010;4:215–22. [Google Scholar]
- 72.Huang FM, Yang SF, Zhao JH, Chang YC. Platelet-rich fibrin increases proliferation and differentiation of human dental pulp cells. J Endod. 2010;36:1628–32. doi: 10.1016/j.joen.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 73.Jang ES, Park JW, Kweon H, Lee KG, Kang SW, Baek DH, et al. Restoration of peri-implant defects in immediate implant installations by Choukroun platelet-rich fibrin and silk fibroin powder combination graft. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:831–6. doi: 10.1016/j.tripleo.2009.10.038. [DOI] [PubMed] [Google Scholar]
- 74.Gürbüzer B, Pikdöken L, Tunali M, Urhan M, Küçükodaci Z, Ercan F. Scintigraphic evaluation of osteoblastic activity in extraction sockets treated with platelet-rich fibrin. J Oral Maxillofac Surg. 2010;68:980–9. doi: 10.1016/j.joms.2009.09.092. [DOI] [PubMed] [Google Scholar]
- 75.Dohan Ehrenfest DM, Doglioli P, de Peppo GM, Del Corso M, Charrier JB. Choukroun's platelet-rich fibrin (PRF) stimulates in vitro proliferation and differentiation of human oral bone mesenchymal stem cell in a dose-dependent way. Arch Oral Biol. 2010;55:185–94. doi: 10.1016/j.archoralbio.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 76.Picardi A, Lanti A, Cudillo L, Cerretti R, Dentamaro T, De Angelis G, et al. Rome Transplant Network. Platelet gel for treatment of mucocutaneous lesions related to graft-versus-host disease after allogeneic hematopoietic stem cell transplant. Transfusion. 2010;50:501–6. doi: 10.1111/j.1537-2995.2009.02439.x. [DOI] [PubMed] [Google Scholar]
- 77.Aleksić Z, Janković S, Dimitrijević B, Divnić-Resnik T, Milinković I, Leković V. The use of platelet-rich fibrin membrane in gingival recession treatment. Srp Arh Celok Lek. 2010;138:11–8. doi: 10.2298/sarh1002011a. [DOI] [PubMed] [Google Scholar]
- 78.Sclafani AP. Applications of platelet-rich fibrin matrix in facial plastic surgery. Facial Plast Surg. 2009;25:270–6. doi: 10.1055/s-0029-1242033. [DOI] [PubMed] [Google Scholar]
- 79.He L, Lin Y, Hu X, Zhang Y, Wu H. A comparative study of platelet-rich fibrin (PRF) and platelet-rich plasma (PRP) on the effect of proliferation and differentiation of rat osteoblasts in vitro. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:707–13. doi: 10.1016/j.tripleo.2009.06.044. [DOI] [PubMed] [Google Scholar]
- 80.Kfir E, Goldstein M, Yerushalmi I, Rafaelov R, Mazor Z, Kfir V, et al. Minimally invasive antral membrane balloon elevation-Results of a multicenter registry. Clin Implant Dent Relat Res. 2009;11(Suppl 1):e83–91. doi: 10.1111/j.1708-8208.2009.00213.x. [DOI] [PubMed] [Google Scholar]
- 81.Dohan Ehrenfest DM, Diss A, Odin G, Doglioli P, Hippolyte MP, Charrier JB. In vitro effects of Choukroun's PRF (platelet-rich fibrin) on human gingival fibroblasts, dermal prekeratinocytes, preadipocytes, and maxillofacial osteoblasts in primary cultures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:341–52. doi: 10.1016/j.tripleo.2009.04.020. [DOI] [PubMed] [Google Scholar]
- 82.Su CY, Kuo YP, Tseng YH, Su CH, Burnouf T. In vitro release of growth factors from platelet-rich fibrin (PRF): A proposal to optimize the clinical applications of PRF. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:56–61. doi: 10.1016/j.tripleo.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 83.Simon BI, Zatcoff AL, Kong JJ, O’Connell SM. Clinical and histological comparison of extraction socket healing following the use of autologous platelet-rich fibrin matrix (PRFM) to ridge preservation procedures employing demineralized freeze dried bone allograft material and membrane. Open Dent J. 2009;3:92–9. doi: 10.2174/1874210600903010092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Magremanne M, Baeyens W, Awada S, Vervaet C. Solitary bone cyst of the mandible and platelet rich fibrin (PRF) Rev Stomatol Chir Maxillofac. 2009;110:105–8. doi: 10.1016/j.stomax.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 85.Diss A, Dohan DM, Mouhyi J, Mahler P. Osteotome sinus floor elevation using Choukroun's platelet-rich fibrin as grafting material: A 1-year prospective pilot study with microthreaded implants. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:572–9. doi: 10.1016/j.tripleo.2007.08.021. [DOI] [PubMed] [Google Scholar]
- 86.Lundquist R, Dziegiel MH, Agren MS. Bioactivity and stability of endogenous fibrogenic factors in platelet-rich fibrin. Wound Repair Regen. 2008;16:356–63. doi: 10.1111/j.1524-475X.2007.00344.x. [DOI] [PubMed] [Google Scholar]
- 87.Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part IV: Clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e56–60. doi: 10.1016/j.tripleo.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 88.Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part II: Platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e45–50. doi: 10.1016/j.tripleo.2005.07.009. [DOI] [PubMed] [Google Scholar]


