Abstract
Background:
Surgical endodontic therapy comprises of exposure of the involved root apex, resection of the apical end of the root, preparation of a class I cavity, and insertion of a root end filling material. Mineral trioxide aggregate (MTA) is now the gold standard among all root end filling materials. MTA is however difficult to handle, expensive and has a very slow setting reaction.
Aim:
(1) To compare the sealing ability of MTA, polymethylmethacrylate (PMMA) bone cement and CHITRA Calcium phosphate cement (CPC) when used as root end filling material using Rhodamine B dye evaluated under a confocal laser scanning microscope. (2) To compare the seal of root ends prepared using an ultrasonic retroprep tip and an Er: YAG laser using three different root end filling materials.
Statistical Analysis:
Statistical analysis was performed using a one-way ANOVA and a two-way ANOVA, independent samples t-test and Scheffe's post hoc test using SPSS Version 16 for Windows.
Results:
All the three materials, namely MTA, PMMA BONE CEMENT and CHITRA CPC, showed microleakage. Comparison of microleakage showed maximum peak value of 0.86 mm for MTA, 0.24 mm for PMMA bone cement and 1.37 mm for CHITRA CPC. The amount of dye penetration was found to be lesser in root ends prepared using Er: YAG laser when compared with ultrasonics, but the difference was found to be not statistically significant.
Conclusion:
PMMA bone cement is a better material as root end filling material to prevent apical microleakage. MTA still continues to be a gold standard root end filling material showing minimum microleakage. Er: YAG laser is a better alternative to ultrasonics for root end preparations.
Keywords: CHITRA calcium phosphate cement, confocal scanning laser microscope, Er: YAG laser mineral trioxide aggregate, polymethylmethacrylate bone cement, polymethylmethacrylate, root end filling materials
INTRODUCTION
Radicular lesions develop only when root canals are exposed to the oral flora, and the root canal system has the capacity to harbor several species of bacteria as well as their toxins and by products. Engress of these irritants from the root canal system into radicular tissues results in the formation of radicular lesions. Because of the complexity of the root canal system and the difficulty to completely clean it using the present techniques and instruments, root canals cannot always be adequately treated using a non-surgical orthograde approach.[1]
When non-surgical attempts prove unsuccessful or are contraindicated, surgical endodontic therapy is needed to save the tooth. The procedure usually comprises of exposure of the involved apex, resection of the apical end of the root, preparation of a class I cavity and insertion of a root end filling material.[1]
Dental material development is fundamental to the improvement of clinical outcomes in dentistry. Along with advancements in equipment technology, procedural improvements and therapeutic knowledge, the integration of these new materials into clinical practice can open treatment horizons that would have been otherwise impossible to envision. An ideal root end filling material should adhere and adapt to the dentinal walls of the root end preparation, should prevent leakage of microorganisms and their by-products into the periradicular tissues, should be biocompatible, should be insoluble in oral tissue fluids, should be dimensionally stable and should not be affected by the presence of moisture.[2,3]
Mineral trioxide aggregate (MTA) is now the gold standard among all root end filling materials.[2] However, MTA has certain drawbacks such as difficulty in handling and very slow setting reaction, which might contribute to leakage, surface disintegration, loss of marginal adaptation and continuity of the material.[2]
Two new materials that might potentially provide the necessary properties of a root end filling material, polymethylmethacrylate (PMMA) bone cement and calcium phosphate bone cement (CHITRA CPC), were compared with MTA in the present study with regard to its sealing ability using Rhodamine B fluorescent dye and confocal laser scanning microscope. Besides this, the study also compared the seal of root ends prepared using an Ultrasonic retroprep tip and an Er: YAG laser.
MATERIALS AND METHODS
Eighty sound, caries-free, mandibular premolars with single canals were shaped up to size 50 K file and obturated with gutta-percha and AH plus sealer. After removal of 2 mm of the filling material, the access cavity was sealed with light-cured glass ionomer cement. Apical root resection was then performed by removing 3-4 mm of the apex at 90° to the long axis of the root with a straight fissure bur in a high-speed handpiece with water coolant.
The teeth were randomly allocated into two control groups of 16 teeth each and experimental groups of 48 teeth each. In half of the samples, the apical cavity was prepared using an ultrasonic retropreparation diamond tip (SybronEndo; BK3-R) with water coolant. In the rest of the samples, apical cavity preparation was performed using an Er: YAG hard tissue laser (Fidelis Laser; Fotona [400 mJ, 10 Hz]) under copious irrigation with water to prevent charring of the samples. The cavities were enlarged and deepened to 3 mm depth and 2 mm diameter. Two coats of nail varnish was applied to the external surface of each root. To reduce the amount of dye penetration through the exposed dentinal tubules, the resected surfaces were sealed with a layer of Scotchbond multipurpose adhesive (3M ESPE) followed by application of nail varnish.
GROUPS
Group I: MTA (Angelus) used as the root end filling material
IA: Ultrasonic retroprep tip used for root end preparation
IB: Er: YAG laser used for root end preparation
Group II: PMMA bone cement (DePuy, Johnson and Johnson) used as root end filling material
IIA: Ultrasonic retroprep tip used for root end preparation
IIB: Er: YAG laser used for root end preparation
Group III: CHITRA CPC (CHITRA CPC; Sri Chitra Tirunal Institute for Medical Sciences and Technology) used as root end filling material
IIIA: Ultrasonic retroprep tip used for root end preparation
IIIB: Er: YAG laser used for root end prep
Group IV: Negative control. In 16 teeth, the entire root surface was coated with two coats of nail polish to act as negative controls
Group V: Positive control. The remaining 16 teeth were not filled with any root end filling material to act as positive controls.
All the roots were wrapped in wet pieces of gauze and stored in 100% humidity for 24 h. The roots were then totally immersed in a solution of Rhodamine B fluorescent dye for 24 h. Using a diamond disc, each root was longitudinally sectioned into two halves. Each specimen was then examined as to the adaptation of the root end filling material to the cavity walls, the presence and absence of gaps and voids and the extent of dye penetration using confocal laser scanning microscope and oil immersion objectives in conjunction with a green filter (wavelength 546 nm).
Rhodamine B dye gave a red-orange fluorescence when excited with green light of 546 nm wavelength. The amount of dye penetration was measured in μm using the ZEISS LSM IMAGE BROWSER SOFTWARE (Version 4.2.0.121). Statistical analysis was done using a one-way ANOVA and a two-way ANOVA, independent samples t-test and Scheffers post hoc test using SPSS Version 16 for Windows.
RESULTS
Comparision of dye penetration [Table 1 and 2]
Table 1.
Root end preparation done with ultrasonics (A)
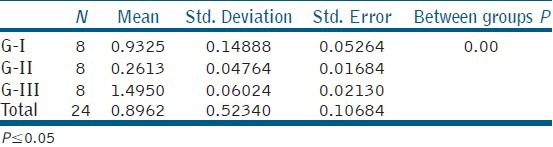
Table 2.
Root end preparation done with laser (B)
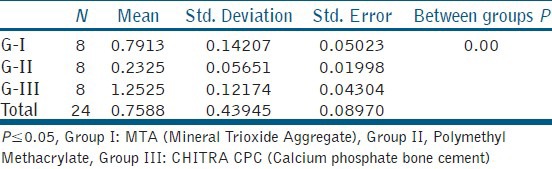
Group I : MTA (Mineral Trioxide Aggregate);
Group II : (PMMA, Polymethylmethacrylate bone cement,)
Group III : CHITRA CPC (Calcium phosphate bone cement)
Complete dye penetration was noted between gutta-percha and the dentinal walls in the positive control samples. No dye penetration was seen in the negative control samples. All the three materials, namely MTA, PMMA BONE CEMENT and CHITRA CPC, showed microleakage. Comparison of microleakage showed maximum peak value of 0.86 mm for MTA, 0.24 mm for PMMA bone cement and 1.37 mm for CHITRA CPC [Figure 1].
Figure 1.
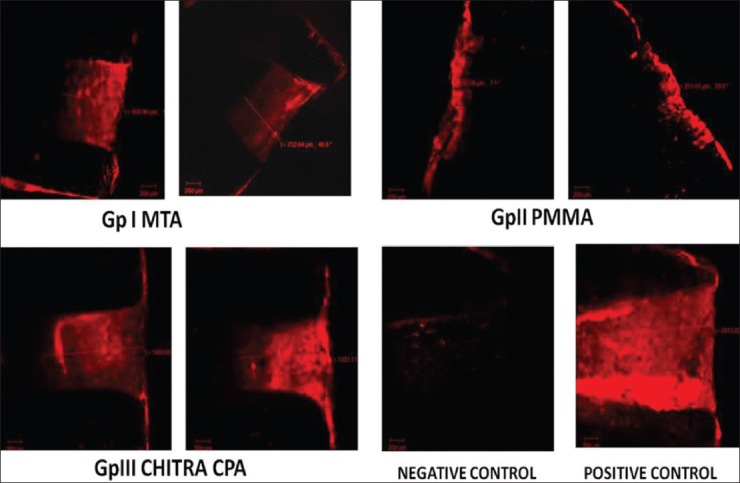
Microleakage seen under CLSM
The mean microleage values, arranged in order, starting from the least to the maximum, were:
Group IV: Negative control (0.0) < Group II PMMA (0.2469) < Group I MTA (0.8619) < Group III CHITRA CPC (1.3738) < Group V Positive control (3.00).
ANOVA was applied to test for any possibility of equality of mean among the categories. Results of the test indicated that there was a “high significant difference” in the values among the five groups (P = 0.0001). The statistical significance is considered if P ≤ 0.05.
Independent samples t-test was used for comparison between the subgroups of each group. There was no significant difference in the microleakage values between the subgroups in Group I (P = 0.07) and Group II (P = 0.29), while a significant difference was found in Group III (P = 0.00). Although there was a difference in the microleakage between the samples prepared using ultrasonic and laser, the difference was not found to be statistically significant.
DISCUSSION
Apical seal is the single and most important factor in achieving success in surgical endodontics. A retrograde root filling is placed to establish an apical seal to prevent the passage of microorganisms or their products into periapical tissues.[1] MTA has been a mainstay of clinical endodontics since its introduction in the mid-1990s. It is the first restorative material that consistently allows for the overgrowth of cementum and formation of bone, and also facilitates the regeneration of the periodontal ligament. It is now accepted as the gold standard material for root end filling.[2]
MTA, however, is not perfect. It has certain drawbacks like difficulty in handling and a slow setting reaction, which might contribute to leakage, surface disintegration, loss of marginal adaptation and continuity of the material. Besides, MTA has an alkaline ph. During setting, MTA changes from ph 10.2 to ph 12.5 in 3 h. Because of the interaction between MTA and the organic phase of dentin, this results in a degradation of type 1 collagen, and the microhardness of dentin is altered.[3]
PMMA bone cement has been widely used in orthopedic surgery, mainly for the fixation of prosthesis and also for stabilizing compressive vertebral fractures or filling bone defects. PMMA bone cement has excellent adaptation to the cavity margins, in spite of the well-known polymerization shrinkage of acrylics. This is because the volume of cement increases to a maximum during polymerization before shrinking slightly, although not to its initial volume. The cement also tolerates a moist environment very well and is not affected by blood contamination.[3]
PMMA bone cement does not seem to have any negative effects, even in large quantities needed during total hip arthroplasty. The amounts required in endodontics are much less than would be needed in orthopedics. The lesser amount required would produce a much lower exothermic reaction and a much reduced amount of monomer. Besides, heat dispersion is favored when the cement is in contact with a flowing liquid (blood).[3,4]
CPCs are new-generation bone substitutes. Scientists at the Sree CHITRA Tirunal Institute for Medical Sciences and Technology (SCTIMST), Thiruvananthapuram, had developed a novel formulation of CPC named “CHITRA-CPC,” which has enhanced viscous and cohesive properties than conventional CPC. CHITRA-CPC could be mixed in varying consistencies, from mouldable putty to injectable paste. This flexibility provides immense advantage in clinical application as a bone and dentine substitute.[5,6,7] Besides this, it has a neutral ph during setting, is highly adaptable and adheres to the root canal surface.[8] It is also dimensionally stable, easy to handle and has the property of osteotransductivity (i.e., active resorption at bony sites, facilitating bone remodeling).[9]
In the present study, PMMA bone cement showed a mean microleakage of 0.24 mm, which was much less than MTA (0.86 mm) and CHITRA CPC (1.37 mm). The study showed that all materials exhibited microleakage, but there was significantly less microleakage in PMMA BONE CEMENT when compared with CHITRA CPC and MTA. Microleakage in CHITRA CPC cement was found to be more when compared with MTA.
The advantage of using ultrasonics for root end preparation is their smaller dimensions of the cavity prepared and improved access to the resected root-end cavity (Carr 1997).[10,11] However, its use has been shown to produce cracks on root canal walls.[12] Lasers, if used properly with optimal settings for the target tissue, yield favorable results, including a decrease in dentine permeability (Aranha et al., 2005) cavity preparation without vibration (Aoki et al., 1998), less crack formation on root canal walls (Wallace, 2006), improved bactericidal activity (Gordon et al., 2007) and effective removal of the smear layer and debris (Schoop et al., 2007).[13,14] Lasers have been shown to preserve the integrity of root end cavities better than ultrasonic devices from the standpoint of chipping.[15,16]
In the present study, the amount of dye penetration was found to be lesser in root ends prepared using Er: YAG laser when compared with ultrasonics. This may be due to better preservation of the integrity of root-end cavities from the standpoint of dentinal chipping. But, the difference was found to be not statistically significant (P > 0.05).
Confocal laser scanning microscopy is a simple method to test the adaptation of dental materials to the dentin. The advantages of CLSM include[17,18,19]
Non-destructive examination of the samples
Non-dehydrated samples can be used: Drying of samples, which is indispensable for conventional SEM or TEM, is not necessary with CLSM, leading to a decreased risk, of shrinking or other drying artefacts
No specific sectioning technique required: This decreases the possibility of artifacts produced during the preparation of the specimens by dehydration and sputter-coating procedure for SEM evaluation
Rapid sampling is also available.
CONCLUSION
From the present study, the following conclusions were derived:
PMMA bone cement is a better material as root end filling material to prevent microleakage
MTA still continues to be a gold standard root end filling material showing minimum microleakage
The amount of dye penetration was found to be lesser in root ends prepared using Er: YAG laser when compared with ultrasonics. But, the difference was found to be not statistically significant.
Further in vivo studies are needed to correlate with the finding of the present study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Torabinejad M, Watson TF, Pitt Ford TR. Sealing ability of a mineral trioxide aggregate when used as a root end filling material. J Endod. 1993;19:591–5. doi: 10.1016/S0099-2399(06)80271-2. [DOI] [PubMed] [Google Scholar]
- 2.Parirokh M, Torabinejad M. Mineral trioxide aggregate: A comprehensive literature review – Part I: Chemical, physical, and antibacterial properties. J Endod. 2010;36:16–27. doi: 10.1016/j.joen.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 3.Badr AE. Marginal adaptation and cytotoxicity of bone cement compared with amalgam and mineral trioxide aggregate as root end filling materials. J Endod. 2010;36:1056–60. doi: 10.1016/j.joen.2010.02.018. [DOI] [PubMed] [Google Scholar]
- 4.Majkowski RS, Bannister GC, Miles AW. The effect of bleeding on the cement bone interface. An experimental study. Clin Orthop Relat Res. 1994;299:293–7. [PubMed] [Google Scholar]
- 5.Fernandez AC, Mira M, Varma HK, Komath M. Safety and efficacy of CHITRA CPC calcium phosphate bone cement as bone substitute. Curr Sci. 2006;91:1678–84. [Google Scholar]
- 6.Manoj K, Varma HK. Development of a fully injectable calcium phosphate cement for orthopedic and dental applications. Bull Mater Sci. 2003;26:415–22. [Google Scholar]
- 7.Manoj K, Varma HK. Current status of dental materials research in SCTIMST, Trivandrum Part II: Synthetic bone graft materials. KDJ. 2009;32:193–8. [Google Scholar]
- 8.George S, Shivana V, Dhanyakumar NM. Calcium phosphate cement; a new saviour for furcation perforation. An in vitro study. Endodontology. 2006;18:7–11. [Google Scholar]
- 9.Rajesh JB, Nandakumar K, Varma HK, Komath M. Calcium phosphate cement as a barrier graft for the treatment of human periodontal intraosseous defects. Indian J Dent Res. 2009;20:471–9. doi: 10.4103/0970-9290.59459. [DOI] [PubMed] [Google Scholar]
- 10.Shakouie S, Samiei M, Shahi S, Rahimi S, Yavari A, Reyhani MF. Sealing ability comparison of mineral trioxide aggregate in root end cavities prepared with ultrasonic and Er, Cr: YSGG laser. Afr. J. Biotechnol. 2012;11:8906–11. [Google Scholar]
- 11.Chailertvanitkul P, Saunders WP, Saunders EM, MacKenzie D. Polymicrobial coronal leakage of super EBA root end fillings following two methods of root end preparation. Int Endod J. 1998;31:348–53. doi: 10.1046/j.1365-2591.1998.00164.x. [DOI] [PubMed] [Google Scholar]
- 12.Rahimi S, Yavari HR, Shahi S, Zand V, Shakoui S, Reyhani MF, et al. Comparison of the effect of Er, Cr YSGG laser and ultrasonic retrograde root end cavity preparation on the integrity of root apices. J Oral Sci. 2010;52:77–81. doi: 10.2334/josnusd.52.77. [DOI] [PubMed] [Google Scholar]
- 13.Pozza DH, Fregapani PW, Xavier CB, Weber JB, Oliveira MG. CO(2), Er:YAG and Nd:YAG lasers in endodontic surgery. J Appl Oral Sci. 2009;17:596–9. doi: 10.1590/S1678-77572009000600011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Moura AA, Moura Netto C, Barletta FB, Vieira ND, Júnior, Eduardo Cde P. Morphological assessment of dentine and cementum following apicectomy with Zekrya burs and Er: YAG laser associated with direct and indirect Nd: YAG laser irradiation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e77–82. doi: 10.1016/j.tripleo.2009.12.032. [DOI] [PubMed] [Google Scholar]
- 15.Asnaashari M, Fekrazad R, Menshadi FD, Seifi M. The effect of Er, Cr:YSGG laser irradiation on the apical leakage of retrograde cavity. IEJ Fall. 2009;4:144–8. [PMC free article] [PubMed] [Google Scholar]
- 16.Shimizu T, Koba K, Kinoshita J, Matsumota K. Morphological study on apicectomy by high powered Er: Yag Laser. J Oral Laser Applications. 2008;8:245–55. [Google Scholar]
- 17.Marciano M, Ordinola Zapata R, Cavalini Cavenago B, del Carpio Perochina A, Monteiro Bramante C, Gomez de Moraes. The use of confocal laser scanning microscopy in endodontic research: Sealer/ dentin interfaces. Microscopy: Science, technology, applications and education. Formatex Microscopy Series. 2010;3:566–570. [Google Scholar]
- 18.Bramante CM, de Moraes IG, Bernardineli N, Garcia RB, Pidero CU, Ordinola Zapata R, et al. Effect of sputter coating on cracking of root end surfaces after ultrasonic retrograde preparation: A SEM study of resected root apices and their respective impressions. Acta Odontol Latinoam. 2010;23:53–7. [PubMed] [Google Scholar]
- 19.Pioch T, Stotz S, Staehle HJ, Duschner H. Applications of confocal laser scanning microscopy to dental bonding. Adv Dent Res. 1997;11:453–61. doi: 10.1177/08959374970110041201. [DOI] [PubMed] [Google Scholar]


