Abstract
Background
Food insecurity is increasingly recognized as a barrier to optimal treatment outcomes but there is little data on this issue. We assessed associations between food insecurity and mortality in HIV-infected antiretroviral therapy (ART)-treated individuals in Vancouver, British Columbia (BC), and whether body max index (BMI) modified associations.
Methods
Individuals were recruited from the BC HIV/AIDS drug treatment program in 1998 and 1999, and were followed until June 2007 for outcomes. Food insecurity was measured with the Radimer/Cornell questionnaire. Cox proportional hazard models were used to determine associations between food insecurity, BMI and non-accidental deaths when controlling for confounders.
Results
Among 1119 participants, 536 (48%) were categorized as food insecure and 160 (14%) were categorized as underweight (BMI <18.5). After a median follow-up time of 8.2 years, 153 individuals (14%) had died from non-accidental deaths. After controlling for adherence, CD4 counts, and socioeconomic variables, people who were food insecure and underweight were nearly two times more likely to die (Adjusted hazard ratio [AHR]=1.94, 95% Confidence interval [CI]=1.10-3.40) compared with people who were not food insecure or underweight. There was also a trend towards increased risk of mortality among people who were food insecure and not underweight (AHR= 1.40, 95% CI=0.91-2.05). In contrast, people who were underweight but food secure were not more likely to die.
Conclusions
Food insecurity is a risk factor for mortality among ART-treated individuals in BC, particularly among individuals who are underweight. Innovative approaches to address food insecurity should be incorporated into HIV treatment programs.
Keywords: Food insecurity, HIV/AIDS, mortality, Vancouver
Introduction
The advent of highly active antiretroviral therapy (HAART) in 1996 has led to dramatic declines in HIV-related morbidity and mortality. 1-3 Despite this success, significant disparities in HIV treatment outcomes remain, especially among the urban poor. Racial and ethnic minorities, homeless and marginally housed individuals, individuals with lower education and incomes, and people with a history of mental illness and substance abuse have been found to have lower rates of HAART utilization, initiation of HAART at later stages of disease, lower adherence to antiretroviral (ARV) therapy, and higher mortality rates. 4-15
Food insecurity, defined as the “limited or uncertain availability of nutritionally adequate, safe foods or the inability to acquire personally acceptable foods in socially acceptable ways,” 16 is also an important and under-recognized cause of disparities in health care access and health outcomes in marginalized populations. Food insecurity leads to worse health outcomes across a range of diseases and is associated with higher rates of heart disease, diabetes, obesity, and depression. 17-22 Food insecurity is also associated with increased hospitalizations and emergency department use, and postponing needed medical care and medications, even after controlling for other measures of socioeconomic status. 23, 24 Increasingly, food insecurity is becoming recognized as a key driver of the HIV epidemic internationally and as a potential cause of worse health outcomes among people living with HIV/AIDS. 25, 26 Studies from both San Francisco and Vancouver, BC, have found that nearly half of urban poor HIV-infected individuals in HAART treatment programs are food insecure. 16, 27 Food insecurity is independently associated with incomplete HIV RNA suppression among homeless and marginally housed HIV-infected individuals in San Francisco, an effect that appeared to be mediated through both behavioral and biologic pathways. 27
No studies to date have specifically assessed the impact of food insecurity on mortality. In addition, no studies have looked at the extent to which possible negative HIV clinical outcomes associated with food insecurity are explained by poor nutritional status. We therefore set out to examine associations between food insecurity, body mass index, and non-accidental mortality among over 1100 ART-treated participants enrolled in BC's Province-wide Drug Treatment Program. We hypothesized that food insecurity would be independently associated with mortality and that body mass index would modify associations between food insecurity and mortality.
Methods
HIV/AIDS Drug Treatment Program
The BC Centre for Excellence in HIV/AIDS' Drug Treatment Program provides HAART free of charge to clinically eligible HIV-infected individuals throughout the province. All HAART patients are entered into an Oracle-based monitoring and evaluation reporting system that uses standardized indicators to prospectively track the antiretroviral use and clinical and laboratory status of HIV-1 infected individuals. Physicians enrolling an HIV-1 infected individual into the system must complete a drug request enrolment prescription form, which compiles information on the applicant's age, ethnicity, address, past HIV-specific drug history, CD4 cell counts, plasma HIV-1 RNA, current drug requests, and enrolling physician data. The Providence Health Care Ethics Committee for Human Experimentation approved use of the Drug Treatment Program data for research purposes. In 1998-1999, a sample of participants from the BC drug treatment program participated in a self-administered survey as previously described. 16 Domains of inquiry for the survey included sociodemographic characteristics such as age, gender, ethnicity, housing status, income, employment and education; history of opportunistic infections and AIDS-defining illnesses; drug and alcohol use; incarceration, health and clinical status; and food insecurity.
Study Participants
Patients follow-up every one to three months to renew prescriptions and monitor HIV progression through laboratory tests. Participants were eligible if they were ARV naïve at the time they initiated HAART, and if they were >=18 years of age. All participants included in this study initiated HAART between 1992 and 1999. Eligible participants must have completed at least one questionnaire and undertaken at least two follow-up CD4 cell count and HIV plasma viral load tests. Participants were followed from admittance into the treatment until June 2007 for clinical outcomes. All study procedures were approved by the research ethics board of St. Paul's hospital and Providence Health Care.
Measures
The primary predictor was food insecurity, which was measured by a modified version of the Radimer/Cornell questionnaire. 28, 29 The Radimer/Cornell questionnaire covers a range of concepts such as insufficient food intake, the physical sensation of hunger, problems with household food supply, diet quality, anxiety related to food insecurity, and efforts made to maintain household food supplies.28, 29 We chose food insecurity at the individual level as our primary predictor (rather than at the household level) because we postulated that individual food insecurity would be most likely to impact upon malnutrition and mortality. As recommended by Kendall et al., individuals were categorized as food insecure at the individual level if they gave a minimum of 1 positive answer (often/sometimes) to any 1 out of the 8 items in the measure referring to individual food insecurity. If they answered one question in this manner they were deemed food insecure.
The primary outcome in the study was time to non-accidental mortality. This outcome was chosen to best approximate HIV-related mortality, as it excluded individuals who died from injuries, accidents, trauma, assaults, drug overdose, and suicide. Deaths were identified on a continuous basis through physician records and linkage with the BC Division of Vital Statistics. Event free subjects were censored in June of 2007.
Low body mass index (BMI) was evaluated as a possible effect modifier in the relationship between food insecurity and non-accidental mortality, and was defined as a BMI <18.5. 30 The BMI, which was obtained at the time of the survey in 1998/1999, is calculated from weight and height measurements, using the formula weight in kg divided by height in m−2. The BMI reflects protein and fat reserves, and a person with a low BMI is underweight for their height.31
Covariates for the study included age (continuous), sex (male versus female), ethnicity (aboriginal or non-aboriginal), annual income (>=$10,000/year versus < $10,000/year which approximates the low income cut off for Canada), education (>=high school graduation versus < high school graduation), history of treatment in a drug or alcohol program (yes versus no), CD4 cell count (continuous +100 cells), number of years on HAART (continuous), season of the interview (Winter, Spring, Summer, Fall), and log viral load (continuous). CD4 cell counts and viral loads were the most recent values obtained within 6 months prior to the survey date. Unstable housing was defined as living in a hotel, boarding house, group home, jail, in the street, or having no fixed address at the time of the survey. History of injection drug use was defined as having ever injected illicit drugs (by physician or self-report). Adherence was estimated using pharmacy refill data during the year preceding the survey, and was estimated by dividing the number of months of medication dispensed by the number of months of follow-up. Individuals were defined as non-adherent if they received ARVs for less than 95% of the follow-up period as previously described. 32, 33 This measure of adherence has been found to be independently associated with mortality in previous studies. 33, 34 All covariates were obtained at the time of the baseline survey in 1998/1999, except where indicated above.
Statistical Analysis
Cox proportional hazard confounder models were used to determine the association between food insecurity, BMI and non-accidental deaths when controlling for other confounders. Data were analyzed using SAS software version 9.1.3. (SAS Institute, Cary, North Carolina, Version 9) Data are presented within categories as frequencies [n (%)] or as median and interquartile range (IQR). We compared categorical variables between groups using Pearson's χ2 test, and comparisons of continuous variables were carried out using Wilcoxon's rank-sum test. We first assessed the association between food insecurity and non-accidental deaths when controlling for several baseline confounders using Cox proportional hazards. Variable selection was conducted using a backward-selection method suggested by Maldonado and Greenland, by first including all variables in the model and then dropping one variable at each step using the relative change in the coefficient for the variable related to food security as a criterion until the maximum change from the model exceeded 10%. 35 This method has been used in several previous papers, both from our Centre 36, 37 and elsewhere, 38 and has been found to perform well with regard to minimizing bias. 35 Next, in testing BMI for effect modification, we tried to determine whether the relationship between food insecurity and mortality was equally strong in each strata defined by BMI. If the association between food insecurity and mortality differed significantly across the different levels of body mass index, then there would be statistical interaction between food security and BMI, indicating that the effect of food insecurity on survival varies depending on the BMI level. For this analysis, we created a 4-level categorical variable combining food insecurity (present or absent) and BMI (>=18.5 or <18.5). Diagnostic procedures yielded no evidence of multi-collinearity or overly influential outliers in any of the models.
Results
In total, 1214 individuals were recruited into the drug treatment cohort. Of these, 1119 individuals (92%) had consistent follow-up during all years of the study and were included in the analysis. At the time of the interview, 536 participants (48%) were food insecure. The median age of all participants was 41 years, 91% of participants were male, 42% had completed high school, and 21% had a history of IDU (Table 1). The median CD4 cell count was 380 (IQR 220-540), the median viral load was 2.6 (log 10 copies/ml) 2 (IQR 2.6-3.3), 4.6 % had an AIDS diagnosis, and 22% were less than 95% adherent during the first year of follow-up. The overall all cause mortality was 16.4% and 13.7% died by non-accidental deaths during the study period.
Table 1.
A Comparison of Baseline Socioeconomic and Clinical Characteristic by Food Security Status
| Variable | Food Secure N=583 N (column %) | Food Insecure (N=536) N (column %) | Totals (column %) | P-value |
|---|---|---|---|---|
|
| ||||
| Gender, | ||||
| Female | 36 (6.2) | 57 (10.6) | 93 (8.3) | 0.01 |
| Male | 547 (93.8) | 479 (89.4) | 1026 (91.7) | |
|
| ||||
| Age | ||||
| Median | 42.0 | 39.0 | 1119 | < 0.001 |
| Interquartile range | 36.0-48.0 | 35.0-45.0 | ||
|
| ||||
| AIDS diagnosis | ||||
| Yes | 31 (5.3) | 21 (3.9) | 52 (4.6) | 0.27 |
| No | 552 (94.7) | 515 (96.1) | 1067(95.4) | |
|
| ||||
| Aboriginal status | ||||
| Yes | 35 (6.0) | 89 (16.6) | 124 (11.1) | < 0.001 |
| No | 548 (94.0) | 447 (83.4) | 995 (88.9) | |
|
| ||||
| CD4 Cell Count (per 100 cells)1 | ||||
| Median | 4.0 | 3.6 | 3.8 | <0.001 |
| Interquartile range | 2.4-5.6 | 2.0-5.33 | 2.2 – 5.4 | |
|
| ||||
| Plasma HIV viral load (log 10 copies/ml) 2 | ||||
| Median | 2.6 | 2.6 | 2.6 | 0.01 |
| Interquartile range | 2.6-3.0 | 2.6-3.5 | 2.6 – 3.3 | |
|
| ||||
| Adherence (>=95%) 3 | ||||
| Yes | 489 (83.9) | 381 (71.2) | 870 (77.8) | <0.001 |
| No | 94 (16.1) | 154 (28.8) | 248 (22.2) | |
|
| ||||
| History of injection drug use4 | ||||
| No | 514 (90.2) | 330 (64.2) | 844 (77.9) | <0.001 |
| Yes | 56 (9.8) | 184 (35.8) | 240 (22.1) | |
|
| ||||
| Ever enrolled in an alcohol or drug treatment program? 5 | ||||
| No | 500 (90.1) | 383 (74.8) | 883 (82.8) | <0.001 |
| Yes | 55 (9.9) | 129 (25.2) | 184(17.2) | |
|
| ||||
| High School Education or greater | ||||
| No | 202 (34.6) | 272 (50.7) | 474 (42.4) | < 0.001 |
| Yes | 381 (65.4) | 264 (49.3) | 645 (57.6) | |
| Income (<= Canadian $10000) | ||||
| No | 493 (89.0) | 244 (49.5) | 717 (69.8) | <0.001 |
| Yes | 61 (11.0) | 249 (50.5) | 310 (30.2) | |
|
| ||||
| Stable Housing? 6 | ||||
| No | 13 (2.3) | 51 (9.8) | 64 (5.9) | <0.001 |
| Yes | 553(97.7) | 469 (90.2) | 1022 (94.1) | |
|
| ||||
| Body Mass Index (BMI) | ||||
| Underweight (BMI < 18.5) | 73 (12.5) | 87 (16.2) | 160 (14.3) | 0.09 |
| Not Underweight (BMI >=18.5) | 510 (87.5) | 449 (83.8) | 959 (85.7) | |
|
| ||||
| Number of years on ART | ||||
| Median | 2.75 | 2.25 | 2.50 | <.0001 |
| Interquartile range | 1.42 – 4.83 | 1.08 – 3.33 | 1.25 – 4.00 | |
|
| ||||
| Non-accidental deaths | ||||
| No | 529 (90.7) | 437 (81.5) | 966 (86.3) | <.0001 |
| Yes | 54 (9.3) | 99 (18.5) | 153 (13.7) | |
|
| ||||
| All-cause mortality | ||||
| No | 520 (89.2) | 416 (77.6) | 936 (83.7) | <0.0001 |
| Yes | 63 (10.8) | 120 (22.4)) | 183 (16.4) | |
|
| ||||
| Season survey completed | ||||
| Winter | 304 (52.1) | 264 (49.2) | 568 (50.7) | 0.309 |
| Spring | 123 (21.1) | 138 (25.8) | 261 (23.3) | |
| Summer | 61 (10.5) | 56 (10.5) | 117 (10.5) | |
| Fall | 95 (16.3) | 78 (14.5) | 173 (15.5) | |
Data missing for 86 patients.
Data missing for 20 patients.
Data missing for 1 patient.
Data missing for 35 patients.
Data missing for 52 patients.
Data missing for 33 patients.
Examining participant characteristics according to food security status, a significantly higher proportion of women and individuals of aboriginal descent were food insecure. Food insecurity was also significantly associated with lower median ages, lower median CD4 cell counts and higher viral loads, fewer years on HAART, history of injection drug use, history of enrollment in an alcohol or drug treatment program, lower education, and unstable housing (Table 1). In addition, 62% of individuals who were food insecure were non-adherent with their HAART regimens compared to 38% of individuals who were food secure (p<0.001). Twenty-two percent of individuals who were food insecure died by non-accidental deaths, compared to 11% of individuals who were food secure.
Factors associated with non-accidental mortality
In unadjusted analyses (see Table 2, first column), individuals who were food insecure were more than two times more likely to die compared to individuals who were not food insecure (Hazard Ratio [HR]=2.15, 95% CI=1.55-3.00). Higher age, female gender, lower CD4 cell counts, higher viral loads, lower HAART adherence, lower income, history of injection drug use and drug or alcohol treatment, history of unstable housing, and aboriginal ethnicity were all significantly associated with morality.
Table 2. Probability of Non-Accidental Deaths.
| Variable | Unadjusted Model HR, 95% CI | Adjusted Model HR, 95% CI | Adjusted Model with BMI as Possible Effect Modifier HR, 95% CI |
|---|---|---|---|
|
| |||
| Male vs. Female | 0.59 (0.37,0.95) | - | - |
|
| |||
| Age (+ x/years) | 1.04 (1.02,1.06) | 1.05 (1.03,1.07) | 1.05 (1.03,1.07) |
|
| |||
| CD4 Cell Count (per 100 cells) | 0.79 (0.72 0.86) | 0.80 (0.74,0.87) | 0.80 (0.74, 0.88) |
|
| |||
| Log10 Viral Load | 1.63 (1.40,1.90) | - | - |
|
| |||
| < high school vs. >= high school | 1.68 (1.22,2.30) | - | - |
|
| |||
| Income <10000 vs >=10000 | 1.92 (1.37,2.70) | - | - |
|
| |||
| History of injection drug use (Yes vs. No) | 3.44 (2.49,4.76) | 3.46 (2.40,4.99) | 3.43 (2.38, 4.94) |
| Ethnicity (Native vs. Non-Native) | 1.90 (1.25,2.88) | - | - |
| Ever been in an Alcohol or Drug program (Yes vs. No) | 2.33 (1.63,3.32) | - | - |
|
| |||
| Number of years on ART (for every year increase) | 0.97 (0.89 – 1.06) | - | - |
|
| |||
| Adherence >=95% vs. <95% | 0.44 (0.32 – 0.62) | - | - |
| Stable housing (Yes vs No) | 0.55 (0.32,0.95) | - | - |
|
| |||
| Food Insecure? (Yes vs. No) | 2.15 (1.55,3.00) | 1.51 (1.03,2.23) | NA |
|
| |||
| Food Secure and not underweight | 1.00 (-) | 1.00 (-) | |
|
| |||
| Food Secure and underweight | 0.70 (0.28,1.76) | 0.70 (0.28,1.78) | |
|
| |||
| Food insecure and not underweight | 1.93 (1.35,2.77) | 1.40 (0.91,2.05) | |
|
| |||
| Food Insecure and underweight | 2.81 (1.69,4.69) | 1.94 (1.10,3.40) | |
|
| |||
| Season survey completed | |||
| Winter | 1.00 (-) | ||
| Spring | 0.87 (0.58,1.31) | ||
| Summer | 0.88 (0.50, 1.54) | ||
| Fall | 1.06 (0.67,1.65) | ||
The second column of Table 2 shows factors associated with non-accidental mortality when adjusting for all possible confounders excluding BMI. In adjusted analyses, individuals who were food insecure were 50% more likely to die compared with individuals who were not food insecure (AHR=1.51, 95% CI=1.03-2.23). Individuals with higher CD4 counts were less likely to die, and individuals who were older and had a history of injection drug use were significantly more likely to die in adjusted analyses. In our analyses, we created a 4-level categorical variable combining levels of food insecurity (food insecure and food secure) and BMI (Underweight: BMI<18.5 verus normal weight: BMI>=18.5) and found that BMI was an effect modifier in the relationship between food insecurity and mortality. The third column of Table 2 presents models showing the interaction between food insecurity, body mass index and mortality. After controlling for all confounders, individuals who were both food insecure and underweight were nearly two times more likely to die compared to individuals who were neither food insecure nor underweight (AHR=1.94, 95% CI=1.10-3.40). There was also a trend towards increased risk of mortality among individuals who were food insecure but had normal weights (AHR=1.40, 95% CI=0.91-2.05). In contrast, individuals who were underweight but food secure were not more likely to die.
Figure 1 shows the crude Kaplan Meier of survival stratified by food security status and body mass index. The mortality rate was quite distinct among the different food security status and body mass index groups, with food insecure and underweight individuals having the highest mortality rates (log-rank test P-value: <0.0001). When only food secure patients were considered, the mortality rate was similar for those who were underweight and at normal weights (log-rank test P-value, 0.71). When only food insecure patients were considered, the mortality rate was similar for those who were underweight and at normal weights (log-rank test P-value 0.43). When only underweight patients were considered, the mortality rate was elevated for those who were food insecure (log-rank test P-value 0.008). When only normal weight patients were considered, the mortality rate was elevated for those who were food insecure (log-rank test P-value <0.0001).
Figure 1.
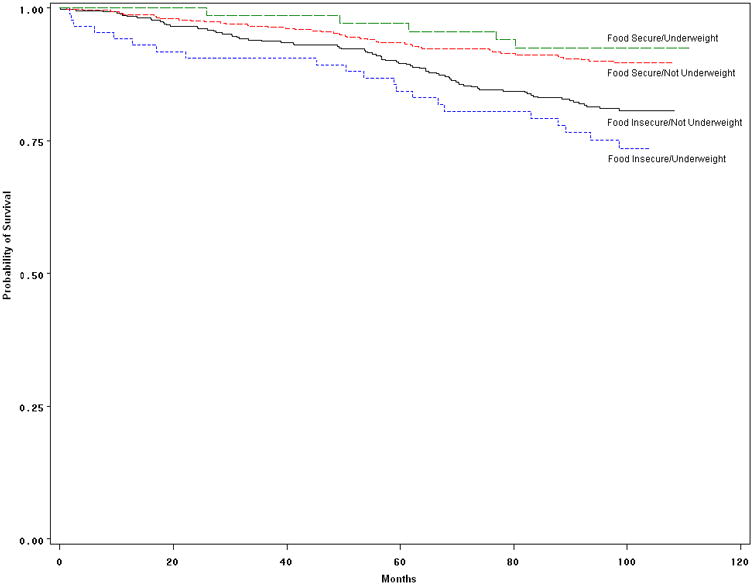
Crude Kaplan-Meier Survival Probabilities for the 1119 Patients Stratified by Food Security and BMI Levels.
| People remaining in the study | 0 months | 20 months | 40 months | 60 months | 80 months | 100 months |
| Food Insecure/Underweight | 87 (7.8%) | 75 (6.7%) | 73 (6.5%) | 68 (6.1%) | 62 (5.5%) | 40 (3.6%) |
| Food Insecure/Not Underweight | 449 (40.1%) | 418 (37.4%) | 394 (35.2%) | 362 (32.4%) | 331 (29.6%) | 156 (13.9%) |
| Food Secure/Underweight | 73 (6.5%) | 70 (6.3%) | 68 (6.1%) | 65 (5.8%) | 60 (5.4%) | 38 (3.4%) |
| Food Secure/Not Underweight | 510 (45.6%) | 485 (43.3%) | 464 (41.5%) | 442 (39.5%) | 428 (38.2%) | 232 (20.7%) |
Discussion
While malnutrition has been found to be associated with mortality for individuals both on and off HAART in both developed and developing countries, 39-47no previous studies to our knowledge have examined the association between food insecurity and mortality. We found that HAART-treated individuals who were food insecure were significantly more likely to die of non-accidental deaths compared to individuals who were not food insecure. The very high prevalence of food insecurity in our study sample (48%) has been previously reported in this population, 16 and suggests that the negative impacts of food insecurity on health outcomes may be experienced by a large proportion of urban poor HIV-infected individuals. These results are also consistent with our previous work in San Francisco, where we found that 49% of HIV-infected individuals on HAART were food insecure and that food insecurity was significantly associated with incomplete viral load suppression among homeless and marginally housed individuals. 27 Taken together, these results argue that food insecurity should be an important target for intervention for HIV-infected individuals on HAART to improve clinical outcomes and decrease mortality. Our findings support recommendations by the World Health Organization, the Joint United Nations Programme on HIV/AIDS, and the World Food Program that food assistance should be integrated into HIV AIDS programming where possible. 48-50While these recommendations are typically aimed at under-resourced settings, our findings suggest that targeted food supplementation coupled with other measures to alleviate poverty should also be a priority among urban poor HIV-infected individuals in well-resourced settings.
Another key finding was that body mass index (BMI) modified associations between food insecurity and mortality in that the effects of food insecurity on mortality were most pronounced among individuals who were also underweight. There is a rich body of literature examining the impacts of malnutrition on HIV clinical, immunologic and virologic outcomes. Studies from both Westernized and developing settings have shown that malnutrition, measured by low body mass index (BMI) and low albumin, hastens progression to immunologic decline, opportunistic infections, AIDS and death in untreated individuals.39-43, 51-56 In terms of the impact of malnutrition on HIV outcomes for patients on HAART, Tang et al. has shown that loss of weight and of lean body mass remain independent predictors of mortality in the HAART era among patients in Massachussets.44 Similarly, studies from Westernized settings have found associations between weight loss or low BMI and higher HIV RNA levels. 57, 58 Negative impacts of poor nutritional status have also been shown in sub-Saharan Africa where several studies reported that low BMI and low hemoglobin were predictive of mortality, especially in the early phases of HAART initiation. 45-47 Our findings, coupled with those of others, suggests that interventions using targeted food supplementation may have the most benefit among individuals who are both food insecure and underweight.
It is interesting that associations between low body mass index and mortality in this study were not seen among individuals who were food secure, and that there was a trend towards increased risk of mortality among individuals who were food insecure but not underweight. This suggests that associations seen between nutritional status and mortality among HAART-treated individuals in other studies may be mediated to some extent by food insecurity. It also suggests that the adverse impact of food insecurity on mortality may be explained in part by mechanisms other than poor nutritional status. In terms of possible additional biologic mechanisms to explain associations between food insecurity and mortality, food insecurity may also impede optimal absorption of certain antiretroviral drugs, which may contribute to treatment failure, progression to AIDS and death. For instance, several protease inhibitors such as nelfinavir and ritonavir require food for maximal absorption, and the absence of food may negatively affect the pharmikokinetics of these drugs. 59-61
As for behavioral mechanisms, we found that food insecurity was significantly associated with antiretroviral adherence at baseline, so it is likely that lower adherence to HAART may have contributed to negative clinical impacts of food insecurity. Since we did not collect longitudinal data on food insecurity, we were unable to better explore interactions between food insecurity and adherence over time and how they may have affected mortality. Other studies have also found associations between food insecurity and HAART non-adherence. A number of qualitative and small quantitative studies have reported that food insecurity is an important barrier to HAART adherence in under-resourced settings. 62-64 Similarly, in a study among nearly 5000 HIV-infected individuals in France, food privation was associated with increased odds of HAART non-adherence among heterosexual men and a trend towards increased odds of non-adherence among heterosexual women. 65 Associations between food insecurity and non-adherence have also been reported for other diseases such as tuberculosis.66, 67 More studies are needed to better understand the role of HAART non-adherence and treatment interruptions in mediating the negative clinical impacts of food insecurity.
Food insecurity was strongly associated with both baseline drug and alcohol use, as well as with markers of socioeconomic status such as low income, lower education and unstable housing. While these factors were controlled for in our confounder models, socioeconomic status is a complex concept that may not be adequately captured by income, education and housing status, and we did not evaluate all drugs of abuse. Consequently, it is possible that low socioeconomic status and drug abuse may in part account for associations seen between food insecurity and mortality. In addition, other studies have found associations between food insecurity and depression17, 18, 20, and depression is well known to be associated with worse clinical outcomes and mortality among individuals on HAART. 68 Consequently, it is possible that depression and other mental illnesses may also be on the causal pathway between food insecurity and poor health outcomes.
There were a number of other important limitations that may affect interpretation of our results. As previously mentioned, we did not gather longitudinal data on food insecurity so were unable to better assess interactions between food insecurity, body mass index, adherence and viral load suppression over time to better understand mechanisms for how food insecurity may impact upon mortality. In addition, we did not use more comprehensive measures of nutritional status such as anthropometry, lab markers of overall nutrition, nutrient assays and body composition measures. Future studies should use more rigorous measures of nutritional status in further exploring interactions between food insecurity, nutritional status and clinical outcomes. Few patients were HAART naïve at the time of the food security interview and it is likely that the impacts of food insecurity on clinical outcomes and mortality may be different among people first initiating HAART. Finally, as with all observational studies, bias is inherent due to uncontrolled confounders.
In conclusion, we found that nearly half of HAART-treated patients from the BC HIV Drug Treatment Program were food insecure and that food insecurity strongly and significantly increased the likelihood of mortality. The effect of food insecurity on mortality was most pronounced in individuals who were also underweight. Addressing food insecurity and relieving hunger among the urban poor is an important goal by itself to improve quality of life and overall health. The potential impact of food support on mortality for HIV-infected individuals on HAART provides additional rationale for meeting broad needs, including food provisions, for urban poor individuals living with HIV/AIDS. Novel interventions to alleviate food insecurity and poverty among urban poor individuals in resource-rich settings are needed to avoid clinical deterioration and excess mortality. Towards this goal, clinicians caring for HIV-infected individuals may consider working in multi-disciplinary teams that include both case managers and nutritionists. These teams can screen individuals for food insecurity and poor nutritional status, inquire about barriers to food access, and help individuals who are food insecure identify reliable sources of good quality food in their communities.
Acknowledgments
This study was funded by the Canadian Institute of Health Research. Dr Weiser received additional funding from NIMH 79713-01. We would like to thank Svetlana Draskovic for administrative assistance and Keith Chan for statistical support.
Funding sources: This study was funded by the Canadian Institute of Health Research. Dr Weiser received additional funding from NIMH 79713-01.
Footnotes
The Positive Health Program and Center for AIDS Prevention Studies are programs of the UCSF AIDS Research Institute.
Preliminary data presented at: XVII International AIDS Conference, Mexico city, Mexico, August 2008
Author contributions: RH and JM developed and maintained the regional population-based cohort within which this study took place. RH, EB, VL, and JM were responsible for design and implementation of the current study, and for acquisition of data. SW, RH, AA, KF and DB contributed substantially to conception of the idea for the manuscript, and to data analysis and interpretation. SW drafted the manuscript. SW, KF, EB, VL, AA, DB, JM, and RH contributed substantially to critical editing and revision of the manuscript. All authors approved the final version of the manuscript.
Conflict of Interest Statement: None declared.
References
- 1.Hogg RS, O'Shaughnessy MV, Gataric N, et al. Decline in deaths from AIDS due to new antiretrovirals. Lancet. 1997;349(9061):1294. doi: 10.1016/S0140-6736(05)62505-6. [DOI] [PubMed] [Google Scholar]
- 2.Hogg RS, Yip B, Chan KJ, et al. viral load after initiating triple-drug therapy. JAMA. 2001;286(20):2568–2577. doi: 10.1001/jama.286.20.2568. [DOI] [PubMed] [Google Scholar]
- 3.Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008 Jul 26;372(9635):293–299. doi: 10.1016/S0140-6736(08)61113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jain S, Schwarcz S, Katz M, Gulati R, McFarland W. Elevated risk of death for African Americans with AIDS, San Francisco, 1996-2002. J Health Care Poor Underserved. 2006 Aug;17(3):493–503. doi: 10.1353/hpu.2006.0106. [DOI] [PubMed] [Google Scholar]
- 5.Tegger MK, Crane HM, Tapia KA, Uldall KK, Holte SE, Kitahata MM. The effect of mental illness, substance use, and treatment for depression on the initiation of highly active antiretroviral therapy among HIV-infected individuals. AIDS Patient Care STDS. 2008 Mar;22(3):233–243. doi: 10.1089/apc.2007.0092. [DOI] [PubMed] [Google Scholar]
- 6.Tucker JS, Burnam MA, Sherbourne CD, Kung FY, Gifford AL. Substance use and mental health correlates of nonadherence to antiretroviral medications in a sample of patients with human immunodeficiency virus infection. Am J Med. 2003 May;114(7):573–580. doi: 10.1016/s0002-9343(03)00093-7. [DOI] [PubMed] [Google Scholar]
- 7.Weiser SD, Wolfe WR, Bangsberg DR. The HIV Epidemic Among Individuals with Mental Illness in the United States. Curr Infect Dis Rep. 2004 Oct;6(5):404–410. doi: 10.1007/s11908-004-0041-2. [DOI] [PubMed] [Google Scholar]
- 8.Leaver CA, Bargh G, Dunn JR, Hwang SW. The effects of housing status on health-related outcomes in people living with HIV: a systematic review of the literature. AIDS Behav. 2007 Nov;11(6 Suppl):85–100. doi: 10.1007/s10461-007-9246-3. [DOI] [PubMed] [Google Scholar]
- 9.McFarland W, Chen S, Hsu L, Schwarcz S, Katz M. Low socioeconomic status is associated with a higher rate of death in the era of highly active antiretroviral therapy, San Francisco. J Acquir Immune Defic Syndr. 2003 May 1;33(1):96–103. doi: 10.1097/00126334-200305010-00014. [DOI] [PubMed] [Google Scholar]
- 10.Wood E, Kerr T, Palepu A, Zhang R, Strathdee SA, Tyndall MW, Montaner JS, Hogg RS. Slower uptake of HIV antiretroviral therapy among Aboriginal injection drug users. J Infect. 2006;52(4):233–236. doi: 10.1016/j.jinf.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 11.Miller CL, Spittal PM, Wood E, Chan K, Schechter MT, Montaner JS, Hogg RS. Inadequacies in antiretroviral therapy use among Aboriginal and other Canadian populations. AIDS Care. 2006;18(8):968–976. doi: 10.1080/09540120500481480. [DOI] [PubMed] [Google Scholar]
- 12.Miller CL, Kerr T, Strathdee SA, Li K, Wood E. Factors associated with premature mortality among young injection drug users in Vancouver. Harm Reduct J. 2007;4:1. doi: 10.1186/1477-7517-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lima VD, Kretz P, Palepu A, Bonner S, Kerr T, Moore D, Daniel M, Montaner JS, Hogg RS. Aboriginal status is a prognostic factor for mortality among antiretroviral naïve HIV-positive individuals first initiating HAART. AIDS Res Ther. 2006;3(14) doi: 10.1186/1742-6405-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spittal PM, Hogg RS, Li K, Craib KJ, Recsky M, Johnston C, Montaner JS, Schechter MT, Wood E. Drastic elevations in mortality among female injection drug users in a Canadian setting. AIDS Care. 2006;18(2):101–108. doi: 10.1080/09540120500159292. [DOI] [PubMed] [Google Scholar]
- 15.Joy R, Druyts EF, Brandson EK, Lima VD, Rustad CA, Zhang W, Wood E, Montaner JS, Hogg RS. Impact of Neighborhood-Level Socioeconomic Status on HIV Disease Progression in a Universal Health Care Setting. J Acquir Immune Defic Syndr. 2008;47(4):500–505. doi: 10.1097/QAI.0b013e3181648dfd. [DOI] [PubMed] [Google Scholar]
- 16.Normen L, Chan K, Braitstein P, et al. Food insecurity and hunger are prevalent among HIV-positive individuals in British Columbia, Canada. J Nutr. 2005 Apr;135(4):820–825. doi: 10.1093/jn/135.4.820. [DOI] [PubMed] [Google Scholar]
- 17.Siefert K, Heflin CM, Corcoran ME, Williams DR. Food insufficiency and physical and mental health in a longitudinal survey of welfare recipients. J Health Soc Behav. 2004 Jun;45(2):171–186. doi: 10.1177/002214650404500204. [DOI] [PubMed] [Google Scholar]
- 18.Heflin CM, Siefert K, Williams DR. Food insufficiency and women's mental health: findings from a 3-year panel of welfare recipients. Soc Sci Med. 2005 Nov;61(9):1971–1982. doi: 10.1016/j.socscimed.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 19.Che J, Chen J. Food insecurity in Canadian households. Health Rep. 2001 Aug;12(4):11–22. [PubMed] [Google Scholar]
- 20.Alaimo K, Olson CM, Frongillo EA. Family food insufficiency, but not low family income, is positively associated with dysthymia and suicide symptoms in adolescents. J Nutr. 2002 Apr;132(4):719–725. doi: 10.1093/jn/132.4.719. [DOI] [PubMed] [Google Scholar]
- 21.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999-2002. J Gen Intern Med. 2007 Jul;22(7):1018–1023. doi: 10.1007/s11606-007-0192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vozoris NT, Tarasuk VS. Household food insufficiency is associated with poorer health. J Nutr. 2003 Jan;133(1):120–126. doi: 10.1093/jn/133.1.120. [DOI] [PubMed] [Google Scholar]
- 23.Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006 Jan;21(1):71–77. doi: 10.1111/j.1525-1497.2005.00278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kersey MA, Beran MS, McGovern PG, Biros MH, Lurie N. The prevalence and effects of hunger in an emergency department patient population. Acad Emerg Med. 1999 Nov;6(11):1109–1114. doi: 10.1111/j.1553-2712.1999.tb00112.x. [DOI] [PubMed] [Google Scholar]
- 25.Gillespie S, Kadiyala S. [Accessed September, 23, 2008];HIV/AIDS and Food and Nutrition Security: From Evidence to Action. http://www.ifpri.org/pubs/fpreview/pv07/pv07.pdf.
- 26.Castleman T, Seumo-Fosso E, Cogill B. [Accessed September 23, 2008];Food and Nutrition Implications of Antiretroviral Therapy in Resource Limited Settings. http://www.fantaproject.org/downloads/pdfs/tn7_ARVs.pdf.
- 27.Weiser SD, Frongillo EA, Ragland K, Hogg RS, Riley ED, Bangsberg DR. Food Insecurity is Associated with Incomplete HIV RNA Suppression among Homeless and Marginally Housed HIV-infected Individuals in San Francisco. Journal of General Internal Medicine. 2008 doi: 10.1007/s11606-008-0824-5. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kendall A, Olson CM, Frongillo EA., Jr Validation of the Radimer/Cornell measures of hunger and food insecurity. J Nutr. 1995 Nov;125(11):2793–2801. doi: 10.1093/jn/125.11.2793. [DOI] [PubMed] [Google Scholar]
- 29.Radimer KL, Olson CM, Campbell CC. Development of indicators to assess hunger. J Nutr. 1990 Nov;120(11):1544–1548. doi: 10.1093/jn/120.suppl_11.1544. [DOI] [PubMed] [Google Scholar]
- 30.Ferro-Luzzi A, Sette S, Franklin M, James WP. A simplified approach of assessing adult chronic energy deficiency. Eur J Clin Nutr. 1992 Mar;46(3):173–186. [PubMed] [Google Scholar]
- 31.James WP, Ferro-Luzzi A, Waterlow JC. Definition of chronic energy deficiency in adults. Report of a working party of the International Dietary Energy Consultative Group. Eur J Clin Nutr. 1988 Dec;42(12):969–981. [PubMed] [Google Scholar]
- 32.Low-Beer S, Yip B, O'Shaughnessy MV, Hogg RS, Montaner JS. Adherence to triple therapy and viral load response. J Acquir Immune Defic Syndr. 2000 Apr 1;23(4):360–361. doi: 10.1097/00126334-200004010-00016. [DOI] [PubMed] [Google Scholar]
- 33.Lima VD, Geller J, Bangsberg DR, et al. The effect of adherence on the association between depressive symptoms and mortality among HIV-infected individuals first initiating HAART. Aids. 2007 May 31;21(9):1175–1183. doi: 10.1097/QAD.0b013e32811ebf57. [DOI] [PubMed] [Google Scholar]
- 34.Hogg RS, Heath K, Bangsberg D, et al. Intermittent use of triple-combination therapy is predictive of mortality at baseline and after 1 year of follow-up. Aids. 2002 May 3;16(7):1051–1058. doi: 10.1097/00002030-200205030-00012. [DOI] [PubMed] [Google Scholar]
- 35.Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993 Dec 1;138(11):923–936. doi: 10.1093/oxfordjournals.aje.a116813. [DOI] [PubMed] [Google Scholar]
- 36.Lima VD, Geller J, Bangsberg DR, Patterson TL, Daniel M, Kerr T, Montaner JS, Hogg RS. The effect of adherence on the association between depressive symptoms and mortality among HIV-infected individuals first initiating HAART. AIDS Care. 2007;21(9):1175–1183. doi: 10.1097/QAD.0b013e32811ebf57. [DOI] [PubMed] [Google Scholar]
- 37.Wood E, Hogg RS, Lima VD, et al. Highly active antiretroviral therapy and survival in HIV-infected injection drug users. Jama. 2008 Aug 6;300(5):550–554. doi: 10.1001/jama.300.5.550. [DOI] [PubMed] [Google Scholar]
- 38.Dietz PM, Spitz AM, Anda RF, et al. Unintended pregnancy among adult women exposed to abuse or household dysfunction during their childhood. Jama. 1999 Oct 13;282(14):1359–1364. doi: 10.1001/jama.282.14.1359. [DOI] [PubMed] [Google Scholar]
- 39.Kotler DP, Tierney AR, Wang J, Pierson RN., Jr Magnitude of body-cell-mass depletion and the timing of death from wasting in AIDS. Am J Clin Nutr. 1989 Sep;50(3):444–447. doi: 10.1093/ajcn/50.3.444. [DOI] [PubMed] [Google Scholar]
- 40.Wheeler DA, Gibert CL, Launer CA, et al. Weight loss as a predictor of survival and disease progression in HIV infection. Terry Beirn Community Programs for Clinical Research on AIDS. J Acquir Immune Defic Syndr Hum Retrovirol. 1998 May 1;18(1):80–85. doi: 10.1097/00042560-199805010-00012. [DOI] [PubMed] [Google Scholar]
- 41.van der Sande MA, van der Loeff MF, Aveika AA, et al. Body mass index at time of HIV diagnosis: a strong and independent predictor of survival. J Acquir Immune Defic Syndr. 2004 Oct 1;37(2):1288–1294. doi: 10.1097/01.qai.0000122708.59121.03. [DOI] [PubMed] [Google Scholar]
- 42.Guenter P, Muurahainen N, Simons G, et al. Relationships among nutritional status, disease progression, and survival in HIV infection. J Acquir Immune Defic Syndr. 1993 Oct;6(10):1130–1138. [PubMed] [Google Scholar]
- 43.Chlebowski RT, Grosvenor MB, Bernhard NH, Morales LS, Bulcavage LM. Nutritional status, gastrointestinal dysfunction, and survival in patients with AIDS. Am J Gastroenterol. 1989 Oct;84(10):1288–1293. [PubMed] [Google Scholar]
- 44.Tang AM, Forrester J, Spiegelman D, Knox TA, Tchetgen E, Gorbach SL. Weight loss and survival in HIV-positive patients in the era of highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2002 Oct 1;31(2):230–236. doi: 10.1097/00126334-200210010-00014. [DOI] [PubMed] [Google Scholar]
- 45.Zachariah R, Fitzgerald M, Massaquoi M, et al. Risk factors for high early mortality in patients on antiretroviral treatment in a rural district of Malawi. Aids. 2006 Nov 28;20(18):2355–2360. doi: 10.1097/QAD.0b013e32801086b0. [DOI] [PubMed] [Google Scholar]
- 46.Anastos A, Shi Q, Lu D, et al. Association of pre-treatment nutritional status with CD4 and viral load response to ART in Rwandan women. Paper presented at: 15th Conference on Retroviruses and Opportunistic Infections; 2008; Boston, MA. [Google Scholar]
- 47.May M, Boulle A, Messou E, et al. Mortality of HIV-1-infected patients starting ART in sub-Saharan Africa: the IeDEA prognostic model. Paper presented at: 15th Conference on Retroviruses and Opportunistic Infections; 2008; Boston, MA. [Google Scholar]
- 48.Programming in the Era of AIDS: WPF's Response to HIV/AIDS. [Accessed September 23, 2008]; http://reliefweb.int/rw/lib.nsf/db900sid/PANA-7DSFKW/$file/wfp_jan2003.pdf?openelement.
- 49.World Health Organization. Nutrient Requirements for People Living with HIV/AIDS: Report of a Technical Consultation. [Accessed September 23, 2008]; http://www.who.int/nutrition/publications/Content_nutrient_requirements.pdf.
- 50.Seume-Fosso E, Rajabiun S, Cogill B, Elder L, Castleman T, Sheckler A. [Accessed September 23, 2008];Food and Nutrition Technical Assistance. HIV/AIDS: A Guide For Nutritional Care and Support. Oct; http://www.fantaproject.org/publications/HIVguide.shtml.
- 51.Chlebowski RT, Grosvenor M, Lillington L, Sayre J, Beall G. Dietary intake and counseling, weight maintenance, and the course of HIV infection. J Am Diet Assoc. 1995 Apr;95(4):428–432. doi: 10.1016/S0002-8223(95)00115-8. quiz 433-425. [DOI] [PubMed] [Google Scholar]
- 52.Macallan DC, Noble C, Baldwin C, et al. Energy expenditure and wasting in human immunodeficiency virus infection. N Engl J Med. 1995 Jul 13;333(2):83–88. doi: 10.1056/NEJM199507133330202. [DOI] [PubMed] [Google Scholar]
- 53.Jones CY, Hogan JW, Snyder B, et al. Overweight and human immunodeficiency virus (HIV) progression in women: associations HIV disease progression and changes in body mass index in women in the HIV epidemiology research study cohort. Clin Infect Dis. 2003;37(2):S69–80. doi: 10.1086/375889. [DOI] [PubMed] [Google Scholar]
- 54.Calmy A, Pinoges L, Szumilin E, Zachariah R, Ford N, Ferradini L. Generic fixed-dose combination antiretroviral treatment in resource-poor settings: multicentric observational cohort. Aids. 2006 May 12;20(8):1163–1169. doi: 10.1097/01.aids.0000226957.79847.d6. [DOI] [PubMed] [Google Scholar]
- 55.Melchior JC, Niyongabo T, Henzel D, Durack-Bown I, Henri SC, Boulier A. Malnutrition and wasting, immunodepression, and chronic inflammation as independent predictors of survival in HIV-infected patients. Nutrition. 1999 Nov-Dec;15(11-12):865–869. [PubMed] [Google Scholar]
- 56.Lindan CP, Allen S, Serufilira A, et al. Predictors of mortality among HIV-infected women in Kigali, Rwanda. Ann Intern Med. 1992 Feb 15;116(4):320–328. doi: 10.7326/0003-4819-116-4-320. [DOI] [PubMed] [Google Scholar]
- 57.Batterham MJ, Garsia R, Greenop P. Prevalence and predictors of HIV-associated weight loss in the era of highly active antiretroviral therapy. Int J STD AIDS. 2002 Nov;13(11):744–747. doi: 10.1258/095646202320753682. [DOI] [PubMed] [Google Scholar]
- 58.Campa A, Yang Z, Lai S, et al. HIV-related wasting in HIV-infected drug users in the era of highly active antiretroviral therapy. Clin Infect Dis. 2005 Oct 15;41(8):1179–1185. doi: 10.1086/444499. [DOI] [PubMed] [Google Scholar]
- 59.Gustavson L, Lam W, Bertz R, et al. Assessment of the bioequivalence and food effects for liquid and soft gelatin capsule co-formulations of ABT-378/ritonavir (ABT-378/r) in healthy subjects. Paper presented at: 40th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2000; Toronto, Canada. [Google Scholar]
- 60.Bardsley-Elliot A, Plosker GL. Nelfinavir: an update on its use in HIV infection. Drugs. 2000 Mar;59(3):581–620. doi: 10.2165/00003495-200059030-00014. [DOI] [PubMed] [Google Scholar]
- 61.Abbot Laboratories. [Accessed November 14, 2007];Kaletra, US package insert. Available at: http://www.fda.gov/cder/foi/label/2005/021226s016lbl.pdf.
- 62.Nachega JB, Knowlton AR, Deluca A, et al. Treatment supporter to improve adherence to antiretroviral therapy in HIV-infected South African adults. A qualitative study. J Acquir Immune Defic Syndr. 2006 Dec 1;43(1):S127–133. doi: 10.1097/01.qai.0000248349.25630.3d. [DOI] [PubMed] [Google Scholar]
- 63.Au JT, Kayitenkore K, Shutes E, et al. Access to adequate nutrition is a major potential obstacle to antiretroviral adherence among HIV-infected individuals in Rwanda. Aids. 2006 Oct 24;20(16):2116–2118. doi: 10.1097/01.aids.0000247580.16073.1b. [DOI] [PubMed] [Google Scholar]
- 64.Hardon AP, Akurut D, Comoro C, et al. Hunger, waiting time and transport costs: time to confront challenges to ART adherence in Africa. AIDS Care. 2007 May;19(5):658–665. doi: 10.1080/09540120701244943. [DOI] [PubMed] [Google Scholar]
- 65.Peretti-Watel P, Spire B, Schiltz MA, et al. Vulnerability, unsafe sex and non-adherence to HAART: Evidence from a large sample of French HIV/AIDS outpatients. Soc Sci Med. 2006 May;62(10):2420–2433. doi: 10.1016/j.socscimed.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 66.Farmer P, Robin S, Ramilus SL, Kim JY. Tuberculosis, poverty, and “compliance”: lessons from rural Haiti. Semin Respir Infect. 1991 Dec;6(4):254–260. [PubMed] [Google Scholar]
- 67.Baldwin MR, Yori PP, Ford C, et al. Tuberculosis and nutrition: disease perceptions and health seeking behavior of household contacts in the Peruvian Amazon. Int J Tuberc Lung Dis. 2004 Dec;8(12):1484–1491. [PMC free article] [PubMed] [Google Scholar]
- 68.Ickovics J, Hamburger M, Vlahov D, et al. Mortality, CD4 count decline and depressive symptoms among HIV-seropositive women. Longitudinal analysis from the HIV Epidemiology Research Study. JAMA. 2001;285(11):1466–1474. doi: 10.1001/jama.285.11.1466. [DOI] [PubMed] [Google Scholar]


