Abstract
Mid-twentieth century malaria eradication campaigns largely eliminated malaria from Paraguay and Sri Lanka. Using these interventions as quasi-experiments, I estimate malaria’s effect on lifetime female educational attainment through the combination of pre-existing geographic variation in malarial intensity and cohort exposure based on the timing of the national anti-malaria campaigns. The estimates from Sri Lanka and Paraguay are similar and indicate that malaria eradication increased years of educational attainment and literacy. The similarity of the estimates across the countries reinforces our confidence in the validity of the identification strategy.
Malaria is endemic in 91 countries. Almost 40 percent of the world’s population is at risk for malaria infection, and the disease infects more than 300 million people annually. In Africa, malaria accounts for 10 percent of the overall disease burden, 40 percent of public health expenditure, and 30–50 percent of inpatient admissions (Roll Back Malaria 2009). This paper estimates the effects of this disease burden on lifetime educational attainment, focusing on two countries that have devoted extensive resources to malaria’s eradication.
Malaria might affect educational attainment through several mechanisms. First, malaria in pregnant women can result in anemia and interruption of in utero nutritional transmission, each of which can affect subsequent cognitive, physical, and neurosensory development, potentially affecting a child’s likelihood of advancing through or attending school (Patrick E. Duffy and Robert S. Desowitz 2001). Second, childhood sufferers of severe malaria can have lifelong cognitive difficulties, suffer learning impairments, and have increased susceptibility to other illnesses (World Health Organization 2003). Third, since advanced cognitive development depends on prior development, any disease-related interruption may affect all subsequent development (James J. Heckman and Alan B. Krueger 2003). The full developmental effects of early-life malaria infections may not be realized until higher order functions are required of individuals during schooling age (P. A. Holding and R. W. Snow 2001). Fourth, even if a child is not directly infected, malaria infections in the household or in the larger community can reduce income available for nutrition and schooling, force children to become caregivers, and alter education investments.
I use national malaria eradication campaigns in Sri Lanka and Paraguay as quasi-experiments to estimate the effect of malaria (or malaria eradication) on lifetime educational attainment. In each country, I combine data from the Demographic and Health Surveys (DHS) with measures of sub-national malaria incidence. The source of identification is the heterogeneity in malaria rates within a country, based in part on climatic and geographic factors, and the exogenous reduction of malaria during the national malaria eradication campaigns that led to some cohorts being exposed to malarious conditions, and other cohorts living during periods after its eradication. This identification strategy isolates malaria’s effects from nationwide trends and time-invariant heterogeneity across regions. I also include regional trends in some specifications to control for the potential of regional convergence. In each country, regions with the highest pre-eradication malaria rates experienced the largest gains in education as measured by years of completed schooling or literacy. Despite the potential differences between the countries, the effects of malaria on schooling and literacy are quite similar. The preferred estimates suggest that reducing malaria incidence by 10 percentage points leads to an increase in completed schooling of approximately 0.1 years and an increase in the probability of being literate by 1 percentage point.
These results are consistent with a growing literature on the educational effects of malaria. Hoyt Bleakley (2007b) used malaria eradication campaigns in the United States, Brazil, Colombia, and Mexico to estimate the effect of childhood exposure to malaria in pre-eradication periods. He found increases in adult literacy and income when malaria was eradicated.1
Besides its specific estimates, this study also contributes to the broader literature on the importance of health in human capital accumulation and the debate on the sources of underdevelopment in developing countries (e.g., Gallup and Sachs 2001; Acemoglu and Johnson 2007). Finally, I clarify the economic rationale for eradication by concluding with a simple cost-benefit analysis, weighing the expected increase in GDP per capita versus the cost of an insecticide-treated bednet, a common intervention to protect against malaria infections.
I. Background
Malaria is a parasitic disease that is transmitted to humans by the female Anopheles mosquito. Transmission to humans requires infected mosquitoes, adequate rain-fall, warm temperatures, and an altitude below 2000 meters. By reducing contact between humans and mosquitoes, eradication campaigns reduce the probability that the disease is transmitted from mosquito to human, or vice versa. If the cycle of transmission between people and mosquitoes can be broken long enough, malaria can be eliminated. One of the founding goals of the World Health Organization (WHO) was worldwide malaria eradication. While this goal has yet to be achieved, malaria eradication campaigns were undertaken in much of Latin America and South Asia, typically using DDT spraying. This study focuses on two countries with DDT-based eradication campaigns that are sufficiently old to facilitate the study of lifetime outcomes: Sri Lanka and Paraguay.
Sri Lanka was one of the first countries with a WHO eradication campaign, “a classic case of malaria eradication” (Peter Newman 1965, 7). Importantly, Sri Lanka has excellent data on the district-level incidence of malaria, collected prior to the start of the eradication campaign. Paraguay has the same strain of malaria (Plasmodium vivax) and implemented a similar WHO malaria eradication campaign. Paraguay is unique in one important respect. It suffered an epidemic and sharp rise in malaria just before the start of its campaign, a feature for which I allow in empirical specifications. Prior research has focused on periods of declining malaria incidence.
Both campaigns were based on DDT interior residual spraying.2 Trained spray teams were given instructions regarding when and where to spray and the concentration of DDT to use. In Sri Lanka, the spraying rotation was originally once every ten weeks, but was lengthened to once every 12 weeks as the incidence of malaria declined (W. G. Wickremesinghe 1953). In Paraguay, houses within malarious areas were sprayed four times a years, slowing to three times a year as malaria episodes decreased (Republica del Paraguay 1973).3 In both cases, all malarial areas of the country were designated to be sprayed.
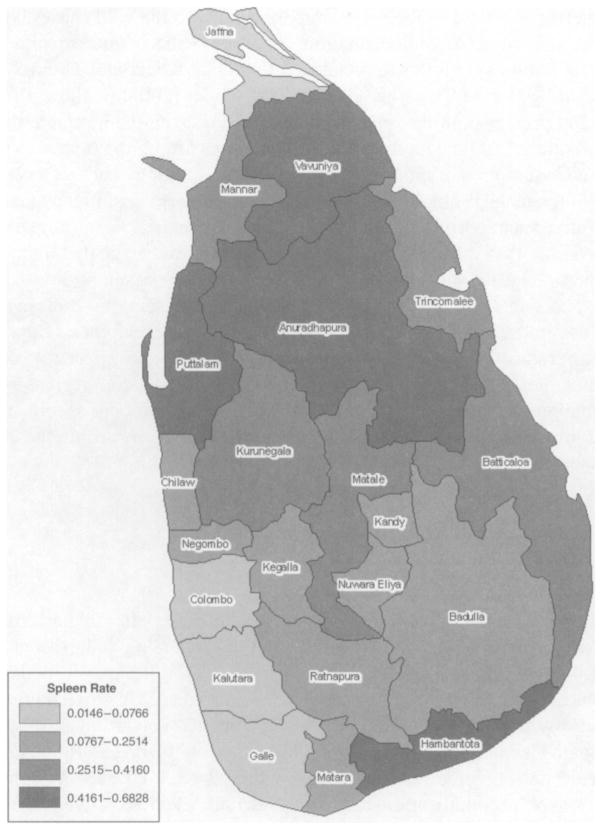
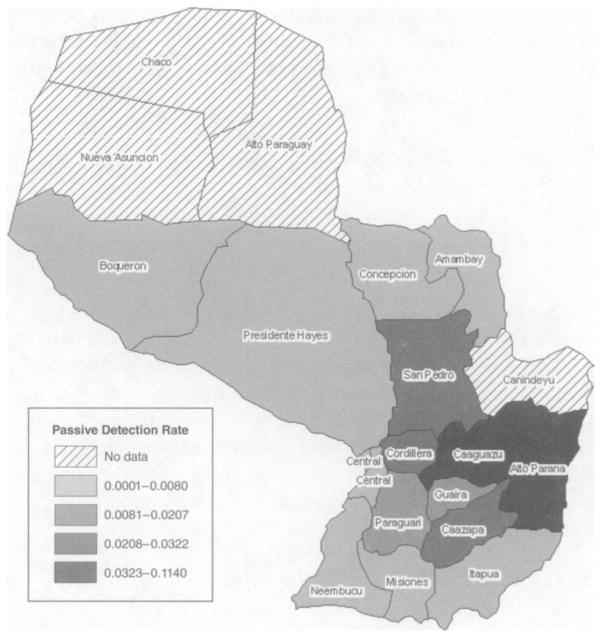
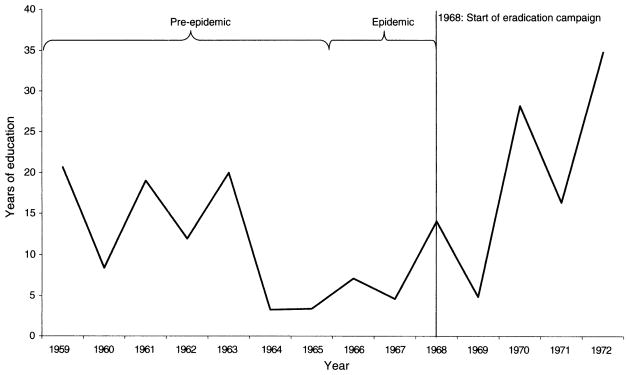
The eradication efforts in Sri Lanka resulted in a gradual decline of malaria. DDT spraying began in 1945 in Anuradhapura, with nationwide reach attained in 1947. Figure 1 plots the regional time series of the spleen rate—the percentage of school aged children who have enlarged spleens—formerly a common way to measure long-standing malaria. Figure 2 illustrates the rapid decline of Paraguay’s malaria incidence following the commencement of spraying in 1968. Since regional malaria rates are not available prior to 1967, the national incidence rate (number of cases divided by the population) is displayed starting in 1958. For the regional malaria levels, the passive detection rate (the number of individuals who presented themselves at clinics within a region and tested positive for malaria divided by the total population) appears on the right axis. In both countries, malaria was reduced to effectively zero in all regions.4
Figure 1.
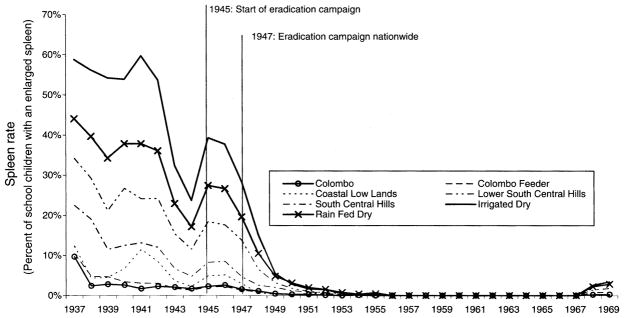
Malaria in Sri Lanka
Sources: 1937–1941 and 1946–1955 Newman (1965); 1942–1945 and 1962–1969 predicted from national time series. 1957–1961 interpolated.
Figure 2.
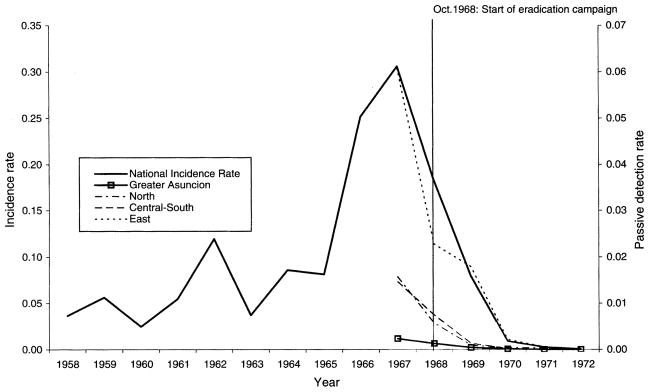
Malaria in Paraguay
Notes: The National Incidence Rate is the number of cases divided by the population. The Passive Detection Rate is the number of individuals who presented themselves at clinics and tested positive for malaria divided by the total population.
Sources: Regional rates, Republica del Paraguay (1973); National rates, PAHO (1975).
II. Empirical Strategy
The primary conceptual challenges in identifying the effects of malaria on educational attainment are the direction of causation and both measures’ potential correlation with unobservable regional characteristics. Regions with high levels of malaria transmission are often poorer and have lower educational attainment than regions with lower levels of malaria transmission. Further, changes in malaria rates are often the result of changes in income levels. To address these issues, this paper exploits the exogenous change in the malaria rate that resulted from the malaria eradication campaigns.
To identify the effect of malaria, I begin with a standard difference-in-differences specification:
| (1) |
where educijc is an education outcome of individual i in region j, who is a member of cohort c; malariaj is the regional pre-eradication malaria intensity; prec is a dummy variable indicating membership in a pre-eradication cohort; Xijc are individual-level controls; δj are regional fixed effects; and δc are cohort fixed effects.5 I initially define membership in the pre-eradication cohort as being born in a year prior to the first full year of the eradication campaign. For Sri Lanka, prec = 1 for birth year ≤ 1947 and 0 otherwise. For Paraguay, prec = 1 for birth year ≤ 1968 and 0 otherwise.6 If malaria adversely affects educational outcomes, then cohorts born before eradication in regions with higher pre-eradication malaria should have lower educational attainment than those born after eradication in the same region.
Equation (1) relies on two sources of variation. First, as Figures 1 and 2 illustrate, regions with higher malaria rates prior to eradication benefited relatively more from eradication than regions with low initial rates. The effective treatment intensity in each region is the change in malaria levels as a result of the program. Since malaria levels in both countries were reduced to approximately zero, the regional intensity of the program is effectively the pre-eradication malaria level. Second, it relies on the differential exposure of cohorts to the timing of eradication.
Equation (1) effectively assumes that the malaria effect is limited to the year of birth, following a fetal-origins hypothesis. As an alternative specification, I define malaria “exposure” of cohort c as the percentage of years prior to age 18 that are spent in the pre-eradication period. The analogous specification is
| (2) |
with other notation as in equation (1).
Because of the potential for serial correlation within a region, an error correction method is necessary for both specifications. As there are only seven regional categories available in the Sri Lanka DHS survey, the typical cluster-robust approach suggested by Marianne Bertrand, Esther Duflo, and Sendhil Mullainathan (2004) could result in inappropriately small standard errors. In addition to calculating these standard errors, I calculate the p-values associated with the wild cluster bootstrap-T method developed by A. Colin Cameron, Jonah B. Gelbach, and Douglas L. Miller (2008). For Paraguay, I follow the Gelbach, Jonathan Klick, and Thomas Stratman (2007) modification of Cameron, Gelbach, and Miller (2008) to allow for only four clusters and present both the conventional standard errors with regional clustering and the p-values from the modified wild cluster bootstrap-T method.
The key assumption of the identification strategy, in both equations, is that in the absence of the malaria eradication program there are no differential changes in educational attainment correlated with initial levels of malaria. For example, an eradication program that specifically targeted regions that were expected to have greater prospects for educational development would violate this assumption. According to published accounts, the eradication campaigns targeted spraying exclusively on the basis of the malaria incidence, and not other aspects of development. But, even with a national eradication campaign, pre-existing regional convergence or concurrent education or health programs targeting the most heavily infected regions would bias the estimation of the malaria effect. Thus, I estimate additional specifications that control for regional trends and report qualitative evidence regarding the absence of other concurrent programs.
III. Sri Lanka
A. Data
To implement the empirical strategy in Sri Lanka, I define malaria rates using district-level malaria spleen rates, a measure of long-standing malaria among school children. I aggregate the district rates to the regional level to match the lowest level geographical variable in the individual-level Sri Lanka data. The seven mutually exclusive regions were noted in Figure 1: Colombo, Colombo Feeder, Coastal Low Lands, Lower South Central Hills, South Central Hills, Irrigated Dry, and Rain Fed Dry.
Climatic and geographic differences within Sri Lanka greatly influence the distribution of pre-eradication malaria (Newman 1965; S. A. Meegama 1986; Flemming Konradsen et al. 2000). The country has three broad climatic zones: dry, intermediate, and wet. The dry zone in the north and south east receives less than 80 inches of rain per annum and has the highest historical malaria incidence rates. The area around Colombo in the southwest comprises the wet zone with rainfall in excess of 100 inches per year. This abundance of rainfall washes away suitable vector breeding sites; malaria in the wet zone is the lowest in the country. The intermediate zone has levels of malaria between these two extremes. The pre-eradication levels of malaria very closely follow this rainfall pattern as can be seen in Figure 3.7
Figure 3.
Sri Lanka Average Spleen Rates, 1937–1941
The microeconomic data for Sri Lanka are the Demographic and Health Survey (DHS) of ever-married women aged 15–49 conducted in 1987. The sample was drawn from areas containing 86 percent of the 1986 population.8 I limit the sample to those born domestically, aged 18 or older at the time of the survey. I then define four measures of education: (i) years of completed education, (ii) years of completed primary education, (iii) ability to read a newspaper or letter easily (“highly literate”), and (iv) ability to read a newspaper or letter easily or with difficulty (“at least minimally literate”).
Sri Lanka’s malaria eradication campaign started in 1945 and all regions of the country had been treated at least once by the end of 1947; 1948 was the first full year in which all regions were treated. Thus, I define births in 1947 or earlier as pre-eradication. In the estimations, malariaj are the regional spleen rates from 1937. The Xijc matrix includes indicator variables for type of childhood residence (town, countryside, and missing, with city as the omitted category) and ethnicity (Up Sinhalese, Sri Lanka Tamil, Indian Tamil, Sri Lanka Moor, Burgher, Malay, other, and missing, with Low Sinhalese as the omitted category).
B. Results
Panel A of Table 1 presents initial evidence of a malaria effect. Regions with the highest levels of malaria prior to eradication had the largest increases in educational attainment when comparing the averages of women born prior to 1948 (i.e., prec = 1) to those of women born in 1948 or later. This table only allows for two classifications of malaria levels, “high” or “low,” and classifies each cohort as either pre-eradication or post-eradication.
Table 1.
Difference in Means
| Panel A. Sri Lanka | Pre-eradication | Eradication | Increase |
|---|---|---|---|
| Years of schooling | |||
| Highly malarious | 4.273 (3.334) | 6.211 (3.381) | 1.938 |
| Less malarious | 5.714 (3.742) | 6.600 (3.582) | 0.886
|
| 1.052 | |||
| Highly literate | |||
| Highly malarious | 0.604 (0.490) | 0.764 (0.425) | 0.160 |
| Less malarious | 0.694 (0.454) | 0.751 (0.432) | 0.057
|
| 0.103 | |||
| Years of primary schooling | |||
| Highly malarious | 3.185 (1.967) | 4.081 (1.604) | 0.896 |
| Less malarious | 3.713 (1.902) | 4.102 (1.682) | 0.389
|
| 0.507 | |||
| At least minimally literate | |||
| Highly malarious | 0.724 (0.448) | 0.862 (0.345) | 0.138 |
| Less malarious | 0.792 (0.406) | 0.845 (0.362) | 0.053
|
| 0.085 | |||
|
| |||
| Panel B. Paraguay | Pre-eradication | Eradication | Increase |
|
| |||
| Years of schooling | |||
| Highly malarious | 5.788 (3.413) | 6.152 (2.744) | 0.364 |
| Less malarious | 7.478 (3.841) | 7.458 (3.186) | −0.020
|
| 0.384 | |||
| Highly literate | |||
| Highly malarious | 0.653 (0.476) | 0.792 (0.407) | 0.139 |
| Less malarious | 0.815 (0.388) | 0.820 (0.384) | 0.005
|
| 0.134 | |||
| Years of primary schooling | |||
| Highly malarious | 4.665 (1.689) | 5.152 (1.437) | 0.487 |
| Less malarious | 5.273 (1.350) | 5.429 (1.180) | 0.156
|
| 0.331 | |||
| At least minimally literate | |||
| Highly malarious | 0.904 (0.295) | 0.948 (0.222) | 0.044 |
| Less malarious | 0.957 (0.204) | 0.965 (0.185) | 0.008
|
| 0.036 | |||
Notes: Panel A: The pre-eradication period is 1937–1947. The highly malarious regions are Dry Irrigated and Dry Rain Fed. Panel B: The pre-eradication period is 1958–1968. The highly malarious region is East.
An alternative test is to estimate a less restricted version of equation (1), replacing β(malariaj × prec) with a separate interaction term for each cohort.9 Figure 4 plots the cohort-specific coefficient estimates with the years of education as the dependent variable. The coefficients fluctuate around 0 for the years prior to 1948. After 1947, all coefficient estimates but one are positive. These findings are consistent with malaria affecting total educational attainment prior to schooling age. Also, this confirms that the cohorts born prior to 1948 can validly be defined as pre-eradication cohorts, as in equation (1).
Figure 4.
Timing of Effect, Sri Lanka
Notes: Plot of coefficients on malariaj × cohortc. Dependent variable is years of completed education.
The estimates of equation (1), including all four measures of educational attainment, appear in columns 1–4 of Table 2. Columns 5–8 contain the estimates of equation 2 for the same dependent variables. Cluster-robust standard errors appear in parentheses and two tailed p-values associated with the wild cluster bootstrap-T method appear in square brackets. In all cases, both methods indicate statistically significant findings.
Table 2.
Effects on Educational Attainment, Sri Lanka
| Exposure to malaria in year of birth
|
Years of exposure to malaria
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Years of completed schooling | Highly literate | Years of completed primary schooling | At least minimally literate | Years of completed schooling | Highly literate | Years of completed primary schooling | At least minimally literate | |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| Pre-eradication cohort × 1937 malaria rate | −3.612*** (0.515) [0.033] | −0.294*** (0.036) [0.014] | −1.616*** (0.156) [0.024] | −0.269*** (0.038) [0.060] | ||||
| Percent of first 18 years with malaria exposure × 1937 malaria rate | −9.047*** (1.873) [0.033] | −0.888*** (0.100) [0.014] | −4.603*** (0.602) [0.024] | −0.751*** (0.140) [0.040] | ||||
| Additional covariates | ||||||||
| Childhood residence (omitted = city) | ||||||||
| Town | −0.971** (0.371) | −0.0819** (0.032) | −0.314* (0.137) | −0.044 (0.024) | −0.963** (0.375) | −0.0812** (0.033) | −0.310* (0.138) | −0.044 (0.024) |
| Countryside | −3.086*** (0.649) | −0.326*** (0.064) | −1.348*** (0.277) | −0.248*** (0.048) | −3.083*** (0.655) | −0.326*** (0.065) | −1.348*** (0.280) | −0.248*** (0.049) |
| Missing | 0.447 (0.238) | 0.105** (0.042) | 0.384 (0.225) | 0.070 (0.037) | 0.531* (0.248) | 0.112* (0.047) | 0.420 (0.256) | 0.076 (0.043) |
| Ethnicity (omitted = Low Sinhalese) | ||||||||
| Up Sinhalese | −0.510** (0.174) | −0.0496* (0.023) | −0.228** (0.066) | −0.0369** (0.012) | −0.507** (0.175) | −0.0493* (0.022) | −0.226** (0.065) | −0.037** (0.012) |
| Sri Lanka Tamil | −1.460* (0.616) | −0.161** (0.064) | −0.630* (0.324) | −0.117* (0.059) | −1.448* (0.620) | −0.160** (0.065) | −0.623 (0.325) | −0.115 (0.059) |
| Indian Tamil | −2.612*** (0.311) | −0.344*** (0.043) | −1.271*** (0.209) | −0.285*** (0.040) | −2.608*** (0.311) | −0.343*** (0.043) | −1.267*** (0.208) | −0.284*** (0.040) |
| Sri Lanka Moor | −1.161** (0.425) | −0.104*** (0.024) | −0.399* (0.189) | −0.101** (0.035) | −1.156** (0.426) | −0.103*** (0.024) | −0.396* (0.190) | −0.100** (0.035) |
| Burgher | 0.812 (0.419) | 0.157*** (0.015) | 0.480** (0.165) | 0.0934*** (0.016) | 0.839* (0.410) | 0.158*** (0.015) | 0.487** (0.162) | 0.095*** (0.016) |
| Malay | −1.029 (0.530) | −0.201** (0.055) | −0.491 (0.370) | −0.112 (0.074) | −0.960 (0.550) | −0.195** (0.056) | −0.458 (0.388) | −0.107 (0.077) |
| Other/ethnicity | −2.381 (1.637) | −0.301 (0.246) | −1.283 (0.937) | −0.37 (0.243) | −2.323 (1.619) | −0.297 (0.245) | −1.258 (0.928) | −0.366 (0.242) |
| Missing | −4.498** (1.516) | −0.344 (0.279) | −2.257 (1.515) | −0.465 (0.322) | −4.500** (1.501) | −0.344 (0.278) | −2.257 (1.511) | −0.465 (0.322) |
| Regression statistics: | ||||||||
| Observations | 5,822 | 5,822 | 5,822 | 5,822 | 5,822 | 5,822 | 5,822 | 5,822 |
| R2 | 0.17 | 0.14 | 0.16 | 0.14 | 0.17 | 0.14 | 0.16 | 0.14 |
Notes: All regressions include region and birth year fixed effects. Values of robust standard errors clustered at the regional level appear in parenthesis. The two tailed p-values associated with the wild cluster bootstrap-T method appear in square brackets. Pre-eradication cohorts are those born 1937–1947.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
Malaria has a negative and significant effect on years of completed education and literacy. The highest regional spleen rate in Sri Lanka in 1937 was 58.8 percent in the Irrigated Dry Zone. Based on the point estimates in column 1 of Table 2, a reduction of the spleen rate from 58.8 percent to 0 would lead to an increase in the expected number of years of completed education of 2.12 years. In the Irrigated Dry Zone, the average number of years of completed education increased from 3.20 years (for those born between 1937 and 1939) to 7.36 years (for those born between 1967 and 1969). Thus, eradication roughly accounts for half of the increase in completed education over that period.
Based on the estimate for a high level of literacy, eradication in the most heavily infected region increased the probability of literacy by 17.3 percentage points, an increase of 33.0 percent over the level of the 1937–1939 cohorts in the Irrigated Dry Zone. Comparing the cohorts born in the irrigated dry zone in 1937–1939 to those born in 1967–1969, there was a 40.4 percentage point increase in the probability of being able to read easily and a 25.0 percentage point increase in the probability of being able to read easily or with some difficulty; I attribute 43 percent and 63 percent of these gains, respectively, to malaria eradication. The estimates in column 3 are also consistent with these findings.
Columns 5–8 report estimates based on equation 2. From column 5, the expected increase in years of education for an individual born in 1937 in the Irrigated Dry Zone would be 3.25 years, larger than the gains predicted for that cohort in column 1. Each successive cohort would gain less, with those born in 1947 in the same region predicted to gain only 0.295 years of additional education versus an individual born in 1948. The exposure estimates predict smaller gains for the cohorts born closer to eradication than estimations using the fetal-origins hypothesis, but cohorts born after eradication are still expected to have higher levels of education than those born prior to eradication.
IV. Paraguay
A. Data
I define department-level malaria rates in Paraguay as the pre-eradication passive detection rates (see Republica del Paraguay 1973). Passive detection rates are the number of individuals who presented themselves at clinics within a region and tested positive for malaria divided by the total population. The passive detection rates reflect, in part, within-country climatic variation.10 Rainfall increases from west to east with the highest rainfall (and malaria rates) occurring in the far eastern part of the country (see Figure 5).
Figure 5.
Paraguay Average Passive Detection Rates, 1967
The survey data are from the 1990 DHS, a sample of ever-married women aged 49 and younger. I remove from the sample those who were not yet 18 at the time of the survey and those born abroad. The sample is further limited to those who were born in 1958 or later, since 1958 was the first year that the National Malaria Eradication Scheme reported data on nationwide malaria rates (regional rates are only reported starting in 1967, as in Figure 2). Paraguay is prone to epidemic episodes; I cannot assume that the malaria level in 1958 was the malaria level in the preceding years. I will report estimates that include cohorts born prior to 1958, in order to test for the robustness of the main findings.
Based on the national time series of malaria rates since 1958, there are three periods of malaria incidence: pre-epidemic, epidemic, and post-eradication. Thus, the timing of the eradication campaign in Paraguay allows the analysis of educational effects of an epidemic.11 In expectation, individuals born (or very young) during the epidemic spike that started in 1966, and continued until the commencement of the eradication campaign in October 1968, should have lower educational attainment than those who were older during the years of the epidemic or not yet born. To capture this possibility, I estimate equation (1) with two interaction terms to capture the effect of being a member of the cohort born prior to the epidemic (malariaj * prec) and being a member of the cohort born during the epidemic (malariaj * epidemicc). The modified equation is
| (3) |
where the pre-epidemic cohorts (prec = 1) are those born 1958–1965, the epidemic cohorts (epidemicc = 1) are those born 1966–1968, and Xijc are individual-level controls for place of childhood residence. β1 and β2 are the coefficients of interest: the incremental educational cost to someone born in the pre- or epidemic period. One expects negative coefficients: individuals in regions of higher indigenous malaria endemicity gained relatively more with eradication in comparison to those native to areas with a lower level of endemicity. I can further compare coefficient estimates in order to assess whether epidemic malaria worsens attainment more than positive but non-epidemic levels.
B. Results
Table 1, panel B contains initial evidence of the eradication effect: regions that were less infected with malaria experienced smaller gains in all measures of education over the period than the more infected regions. I next allow the effect to vary by each birth cohort by estimating a less restrictive version of equation (1), replacing β(malariaj × prec) with a separate interaction term for each cohort. Figure 6 plots the series of coefficients estimated from the cohort-specific interaction terms with years of education as the dependent variable.12 The smaller estimates of the cohort-specific coefficients for those cohorts born during, and just before, the epidemic reflect the lower educational attainment of those cohorts. The pattern of the coefficients is consistent with a three-category classification of cohorts: those born prior to the epidemic (1958–1965), those born during the epidemic years (1966–1968), or those born during the eradication period (after 1968).
Figure 6.
Timing of Effect, Paraguay
Notes: Plot of coefficients on malariaj × cohortc. Dependent variable is years of completed education.
The full results for Paraguay are presented in Table 3. As with the Sri Lanka specification, I present the conventional standard errors with regional clustering in parentheses. The lower tail p-values (relative to a null hypothesis of malaria having no effect) from the Gelbach et al. (2007) modified wild cluster bootstrap T-method appear in square brackets. The point estimates in columns 1–4 imply that being in a region with a higher malaria level exerted a negative impact on lifetime educational attainment. Under the conventional standard errors approach, the effect of being born during an epidemic of malaria is statistically significant. When using the more conservative standard errors, the estimated effects are not significant.
Table 3.
Effects on Educational Attainment, Paraguay
| Independent variables | Exposure to malaria in year of birth
|
Years of exposure to malaria
|
||||||
|---|---|---|---|---|---|---|---|---|
| Years of completed schooling | Highly literate | Years of completed primary schooling | At least minimally literate | Years of completed schooling | Highly literate | Years of completed primary schooling | At least minimally literate | |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| Pre-epidemic cohort × 1967 malaria rate | −10.38 (9.950) [0.295] | −3.033** (0.628) [0.138] | −8.428** (2.190) [0.146] | −0.957** (0.212) [0.140] | ||||
| Epidemic cohort × 1967 malaria rate | −12.68* (4.845) [0.180] | −2.241*** (0.350) [0.118] | −6.055** (1.733) [0.168] | −0.679* (0.248) [0.173] | ||||
| Percent of first 18 years with pre-epidemic malaria exposure × 1967 malaria rate | 19.401 (12.437) [0.737] | −1.205 (0.638) [0.108] | 1.894 (5.795) [0.588] | −0.595 (0.710) [0.315] | ||||
| Percent of first 18 years with epidemic malaria exposure × 1967 malaria rate | −89.144* (36.993) [0.184] | −15.244** (2.974) [0.124] | −53.995*** (2.969) [0.041] | −5.178*** (0.391) [0.057] | ||||
| Additional covariates | ||||||||
| Childhood residence (omitted = city) | ||||||||
| Town | −1.149** (0.231) | −0.0866** (0.018) | −0.148** (0.040) | −0.0245*** (0.004) | −1.147** (0.229) | −0.086** (0.018) | −0.147** (0.041) | −0.024*** (0.004) |
| Countryside | −3.073*** (0.060) | −0.206** (0.049) | −0.727** (0.136) | −0.0450* (0.017) | −3.069*** (0.063) | −0.206** (0.049) | −0.726** (0.136) | −0.045* (0.017) |
| Missing | −3.242*** (0.398) | −0.180 (0.174) | −1.021* (0.355) | −0.0368 (0.047) | −3.216*** (0.404) | −0.175 (0.173) | −1.003* (0.355) | −0.035 (0.046) |
| Regression statistics | ||||||||
| Observations | 2,931 | 2,931 | 2,931 | 2,931 | 2,931 | 2,931 | 2,931 | 2,931 |
| R2 | 0.26 | 0.12 | 0.14 | 0.03 | 0.26 | 0.12 | 0.14 | 0.03 |
| F-test of (malaria × pre = malaria × epidemic) | 0.20 | 6.93 | 18.30 | 54.25 | 19.44 | 23.63 | 373.00 | 59.18 |
| p-value of F-test | 0.68 | 0.08 | 0.02 | 0.01 | 0.02 | 0.02 | 0.00 | 0.00 |
Notes: All regressions include region and birth year fixed effects. Values of robust standard errors clustered at the regional level appear in parenthesis. The p-values associated with the wild cluster bootstrap-T method appear in square brackets. Pre-Eradication cohorts are those born 1958–1965. Epidemic cohorts are those born 1966–1968.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
The equality of the coefficients on the two malaria periods can be rejected with the exception of the years of completed schooling. Contrary to expectations, the coefficients on the period prior to the epidemic are of larger absolute magnitude. This suggests that the fetal-origins hypothesis could be the incorrect specification. Individuals of a young age during the epidemic could have suffered just as severely as those born during the epidemic, plus they had longer total exposure to malaria.
The highest passive detection rate in 1967 was 6.09 percent. Therefore, those born during the epidemic period in the most infected region would be expected to have 0.77 fewer years of schooling than a cohort born after the epidemic.13 Those born in the most heavily infected region during the epidemic period had an average of 5.89 years of completed schooling. Those in the same region born after the epidemic had 6.15 years of completed schooling, an increase of 0.26 years. Attributing the entire gain in education to eradication in the previously most highly infected regions to malaria seems unrealistic. However, during this period there were no statistically significant gains to national average levels of education when comparing those cohorts born prior to 1967 to those born after.
Columns 5–8 contain the estimates of the exposure specification. For all measures of education, exposure in the pre-epidemic period is not statistically significant. Exposure to the epidemic period does have a negative and significant effect for all measures of education based on the conventional standard errors, and for two out of the four measures based on the wild cluster bootstrap-T method.14 These estimates imply that exposure to the epidemic, regardless of the age, is more important than exposure to pre-epidemic malaria.
V. Standardization and Interpretation
The point estimates of the coefficients are not immediately comparable across countries given different measures of malaria prevalence. Sri Lankan data used spleen rates rather than a true incidence rate. To effect a conversion, I use the years in which data are available for both the spleen rate and the incidence rate to estimate that a 10 percentage point decrease in the incidence rate is equivalent to a 3.14 percentage point decrease in the spleen rate.15 Applying this to the Sri Lankan estimates, I calculate that 10 percentage point reduction in incidence leads to increases of 0.114 years of schooling, 0.924 percentage points of high literacy, 0.054 years of primary schooling, and 0.846 percentage points of minimal literacy.
The Paraguayan estimates use passive detection rates. To convert this to incidence, I use available data for the Alto Parana district where incidence rates of approximately 77 percent correspond to a passive detection rate of 7.16 percent prior to eradication (Gladys N. Conly 1975). Based on this ratio, a 10 percentage point decrease in the incidence rate is equivalent to a decrease in the passive detection rate of 0.93 percentage points. Correspondingly, a 10 percentage point decrease in the incidence rate results in an increase in the number of years of completed education of 0.118, an increase in the probability of being literate of 2.083 percentage points, an increase in the years of completed primary education of 0.056, and an increase in at least minimal literacy of 0.631 percentage points.
The standardized results, broadly similar across countries, are summarized in Table 4. For three of the four education measures, the Sri Lanka estimate is smaller than the Paraguay estimates. A number of factors unrelated to the identification strategy could lead to the differences between the estimates. First, the effect of an epidemic could be larger than the effect of a high level of ongoing malaria. Second, the Paraguayan conversion of passive detection rates to incidence rates could be less precise.
Table 4.
Standardization of Malaria Estimates
| Increase in years of schooling | Increase in high literacy (percentage points) | Increase in years of primary schooling | Increase in minimal literacy (percentage points) | |
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Sri Lanka | 0.114 (0.016) | 0.924 (0.113) | 0.051 (0.005) | 0.846 (0.121) |
| Paraguay | 0.118 (0.045) | 2.083 (0.325) | 0.056 (0.016) | 0.631 (0.231) |
| Bleakley (2007b) | ||||
| Brazil | −0.14 to 0.13 | 0.63 to 2.25 | ||
| Mexico | −0.02 to 0.01 | 0.32 to 1.28 | ||
| Colombia | −0.048 to 0.07 | 0.08 to 2.00 | ||
Notes: All coefficients have been converted to the common metric of a 10 percentage point change in the incidence rate. See text for details of calculations.
Source: Bleakley (2007b, tables 3 and 4)
Still, the similarity across two different countries bolsters confidence in the identification strategy. The final rows of Table 4 report the range of estimates from Bleakley (2007b). My point estimates for literacy are within the ranges. For years of completed education, my results are within or slightly higher than the range of point estimates in Bleakley (2007b). Differential effects by sex could be one reason why my estimates are in the top range of the other estimates since my sample is limited to women.
When considering these results as they apply more broadly, there are a few important considerations. First, both countries could have suffered from selective mortality: members of the older cohorts who survived to the time of survey are a selected sample. Differential mortality by income level or ability will bias the results towards zero. These same reductions in mortality would be expected in any current eradication campaign. Second, the primary form of malaria in both countries is Plasmodium vivax, a less virulent and deadly strain than the strain that is more often found in Sub-Saharan Africa. Decreases in selective mortality and early life effects would be stronger if eradication takes place in a country with the more deadly and debilitating form of malaria. Third, because the data do not allow sub-regional assignment of a local malaria rate, malaria rates are assigned with the assumption of uniform levels across the region. Classical measurement error would bias the results towards zero. Fourth, malaria eradication could increase fertility (Adrienne M. Lucas 2010). Because of the potential quantity/quality trade-off, the initial gains in education could understate the full effect of malaria on education. Lastly, these data are limited to women. There is no biological reason why the direct effects should differ by sex, but indirect effects might (e.g., female children being kept home from school to provide care or as substitute domestic labor), with females potentially gaining more from eradication than males.
VI. Robustness
A. Specification Checks
Tables 5 and 6 report several specification checks for Sri Lanka and Paraguay, respectively, using variants of equation (1). Column 2 in each table limits controls to only cohort and region dummy variables, excluding individual-level controls. In all cases, the results are robust to the exclusion of individual-level controls. For Sri Lanka, all cohorts born 1937–1969 were used in the original specifications. Thus in column 3 of Table 5, I limited the sample to cohorts born 10 years before and 10 years after eradication. The samples have very similar results, well within one standard error of each other. For Paraguay only the cohorts from 1958 to 1972 are used in the original specification as these are the cohorts with national level malaria data. Column 3 of Table 6 expands the sample to the additional cohorts born prior to 1958 that were available in the micro survey data. The results are robust to the inclusion of these additional cohorts.
Table 5.
Specification Check, Sri Lanka
| Baseline (Table 2) | Exclude controls | Cohorts 1938– 1958 | Non-movers | IV with malaria ecology | Fake intervention: 1943 (1937–1947 cohorts) | Fake intervention: 1958 (1948–1969 cohorts) | |
|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
| Dependent variable: Years of schooling | |||||||
| Pre-eradication cohort × 1937 malaria rate | −3.612*** (0.515) | −3.587*** (0.475) | −3.506*** (0.632) | −3.091*** (0.462) | −3.372** (1.013) | −0.0869 (0.670) | −0.527 (0.432) |
| Observations | 5,822 | 5,822 | 4,217 | 2,079 | 5,822 | 1,738 | 4,084 |
| R2 | 0.17 | 0.09 | 0.17 | 0.16 | 0.17 | 0.19 | 0.14 |
|
| |||||||
| Dependent variable: Highly literate | |||||||
| Pre-eradication cohort × 1937 malaria rate | −0.294*** (0.036) | −0.290*** (0.047) | −0.307*** (0.029) | −0.0569 (0.122) | −0.200 (0.115) | −0.154** (0.059) | 0.0102 (0.041) |
| Observations | 5,822 | 5,822 | 4,217 | 2,079 | 5,822 | 1,738 | 4,084 |
| R2 | 0.14 | 0.06 | 0.14 | 0.13 | 0.14 | 0.15 | 0.13 |
|
| |||||||
| Dependent variable: Years of primary schooling | |||||||
| Pre-eradication cohort × 1937 malaria rate | −1.616*** (0.156) | −1.601*** (0.166) | −1.671*** (0.202) | −1.159** (0.362) | −1.376** (0.458) | −0.558** (0.228) | 0.0724 (0.219) |
| Observations | 5,822 | 5,822 | 4,217 | 2,079 | 5,822 | 1,738 | 4,084 |
| R2 | 0.16 | 0.09 | 0.16 | 0.16 | 0.16 | 0.17 | 0.14 |
|
| |||||||
| Dependent variable: At least minimal literacy | |||||||
| Pre-eradication cohort × 1937 malaria rate | −0.269*** (0.038) | −0.265*** (0.046) | −0.286*** (0.034) | −0.171 (0.161) | −0.157 (0.117) | −0.0648 (0.046) | 0.041 (0.043) |
| Observations | 5,822 | 5,822 | 4,217 | 2,079 | 5,822 | 1,738 | 4,084 |
| R2 | 0.14 | 0.06 | 0.14 | 0.14 | 0.14 | 0.15 | 0.12 |
Notes: Values of robust standard errors clustered at the regional level appear in parenthesis. Column 1 repeats columns 1–4 of Table 2. Column 2 includes only region and year dummies in addition to the regressors of interest. All other columns include the same controls as column 1. Column 3 limits the cohorts to those born ten years before and after eradication. Column 4 is limited to those to remain in their village or city of birth. Column 5 uses Kisezewki et al. (2004) malaria ecology data to instrument for pre-eradication malaria levels. Columns 6 and 7 use alternative dates for eradication at times when eradication is known not to have occurred.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
Table 6.
Specification Check, Paraguay
| Baseline (Table 3) | Exclude controls | Additional cohorts (1940–1972 cohorts) | Nonmovers | IV with malaria ecology | Fake epidemic: 1955–1957 (1940–1972 cohorts) | |
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Dependent variable: Years of schooling | ||||||
| Pre-epidemic cohort × 1967 malaria rate | −10.38 (9.950) | −7.794 (8.792) | −7.128 (10.366) | −16.696 (12.426) | −47.884 (50.112) | 3.952 (4.791) |
| Epidemic cohort × 1967 malaria rate | −12.68* (4.845) | −10.960** (3.070) | −12.721* (5.028) | −21.711** (5.873) | −32.512 (26.885) | −3.458 (3.773) |
| Observations | 2,931 | 2,931 | 5,038 | 1,748 | 2,931 | 5,038 |
| R2 | 0.26 | 0.15 | 0.28 | 0.29 | 0.24 | 0.28 |
| F-test of (Pre-epidemic cohort × malaria = epidemic cohort × malaria) | 0.20 | 0.30 | 1.08 | 0.55 | 0.44 | 16.89 |
| p-value of F-test | 0.68 | 0.62 | 0.38 | 0.51 | 0.56 | 0.03 |
|
| ||||||
| Dependent variable: Highly literate | ||||||
| Pre-epidemic cohort × 1967 malaria rate | −3.033** (0.628) | −2.855** (0.552) | −3.026* (1.159) | −3.905** (0.725) | −5.359 (3.104) | −1.189 (1.267) |
| Epidemic cohort × 1967 malaria rate | −2.241*** (0.350) | −2.112*** (0.242) | −2.166** (0.388) | −3.582*** (0.465) | −4.367 (2.895) | −1.108 (0.677) |
| Observations | 2,931 | 2,931 | 5,038 | 1,748 | 2,931 | 5,038 |
| R2 | 0.12 | 0.08 | 0.15 | 0.13 | 0.12 | 0.15 |
| F-test of (pre-epidemic cohort × malaria = epidemic cohort × malaria) | 6.93 | 5.35 | 1.18 | 0.63 | 1.23 | 0.02 |
| p-value of F-test | 0.08 | 0.10 | 0.36 | 0.49 | 0.35 | 0.90 |
|
| ||||||
| Dependent variable: Years of primary schooling | ||||||
| Pre-epidemic cohort × 1967 malaria rate | −8.428** (2.190) | −7.806** (2.038) | −9.761* (4.140) | −13.774** (2.880) | −12.761 (7.139) | −6.547 (4.332) |
| Epidemic cohort × 1967 malaria rate | −6.055** (1.733) | −5.792** (1.423) | −5.922* (1.925) | −9.313*** (1.232) | −12.184 (7.727) | −2.619 (2.392) |
| Observations | 2,931 | 2,931 | 5,038 | 1,748 | 2,931 | 5,038 |
| R2 | 0.14 | 0.09 | 0.20 | 0.15 | 0.14 | 0.20 |
| F-test of (pre-epidemic cohort × malaria = epidemic cohort × malaria) | 18.30 | 10.07 | 2.90 | 5.63 | 0.02 | 3.97 |
| p-value of F-test | 0.02 | 0.05 | 0.19 | 0.10 | 0.90 | 0.14 |
|
| ||||||
| Dependent variable: At least minimally literate | ||||||
| Pre-epidemic cohort × 1967 malaria rate | −0.957** (0.212) | −0.922** (0.202) | −1.350* (0.519) | −1.379*** (0.219) | −1.591 (0.839) | −1.282 (0.616) |
| Epidemic cohort × 1967 malaria rate | −0.679* (0.248) | −0.646* (0.228) | −0.658* (0.266) | −1.222** (0.249) | −1.186 (0.842) | −0.223 (0.376) |
| Observations | 2,931 | 2,931 | 5,038 | 1,748 | 2,931 | 5,038 |
| R2 | 0.03 | 0.02 | 0.06 | 0.04 | 0.03 | 0.06 |
| F-test of (pre-epidemic cohort × malaria = epidemic cohort × malaria) | 54.25 | 73.34 | 7.32 | 11.45 | 2.95 | 17.45 |
| p-value of F-test | 0.01 | 0.00 | 0.07 | 0.04 | 0.18 | 0.02 |
Notes: Values of robust standard errors clustered at the regional level appear in parenthesis. Column 1 repeats columns 1–4 of Table 3. Column 2 includes only region and year dummies in addition to the regressors of interest. All other columns include the same controls as column 1. Column 3 includes the oldest cohorts (born 1940–1957). Column 4 is limited to those to remain in their village or city of birth. Column 5 uses Kisezewski et al. (2004) malaria ecology to instrument for pre-eradication malaria levels. Column 6 considers an alternative date for the epidemic in which no epidemic occurred.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
An additional specification check for each country is to limit the sample to those respondents who remain in the same village or city since birth.16 Selective migration of high education individuals to previously malarious regions would bias the results towards finding a malaria effect. For the Sri Lanka nonmover sample (Table 6, column 4), the results are smaller in absolute magnitude and both measures of literacy are no longer statistically significant. Based on the regional classification in the DHS, the correct non-mover sample are those who have not moved from their region of birth. This designation is not available in the data. By limiting the sample to those who live in the same village or city since birth, the nonmover classification is too restrictive. According to the 1981 Sri Lankan census, 87 percent of women lived in their district of birth, but the DHS non-mover classification includes only 36 percent of the sample (Department of Census and Statistics 1985). In Paraguay, the results are larger in the nonmover sample (Table 6, column 4). As with the Sri Lanka sample, this classification is overly restrictive.
I next use the malaria transmission index in Anthony Kiszewski et al. (2004) as an instrument for pre-eradication malaria.17 For Sri Lanka the point estimates are similar, but there is a substantial increase in the standard errors for the literacy measures. For Paraguay, the first stage of the regression is quite weak and leads to changes in the point estimates away from zero and a high degree of imprecision.18
Finally, I create a “fake” intervention as an additional specification check. For Sri Lanka, the data are sufficient to allow the fake intervention to occur both earlier and later. With an intervention five years earlier in 1943, two of the four coefficients (literacy and primary education) are negative and statistically significant, and one half the size of the baseline estimates. The malaria levels in 1943 and 1944 were lower than normal in the endemic malaria regions because of an abundance of rain in those two years eliminated suitable breeding sites. Also, limited spraying began in 1945. Thus, it might be expected to have generated a limited educational improvement. When the fake intervention is in 1958, a small, marginally significant effect is evident for years of completed education. For Paraguay, when the epidemic is moved ten years earlier (1955–1957), there is no statistical difference between the three periods, as expected. The strength of the baseline findings do not appear for the fake interventions.
B. Convergence
Tables 7 and 8 consider whether regional convergence could account for the effects. If regions had differential trends of educational attainment prior to the eradication campaigns, then the gains in education could have happened even in the absence of the eradication campaign. As a first check, I include regional-specific time trends for all but one region, also allowing time fixed effects to remain in the model. I then include the average level of the dependent variable by region for early cohorts as an additional explanatory variable to check for mean reversion. The results for Sri Lanka are in Table 7, columns 2 and 3. With the inclusion of either regional trends or the checks for mean reversion, the coefficients on the malaria effect remain negative and significant, but of smaller absolute magnitude. The literacy estimates with the regional trends are more similar to the baseline estimates. The estimates that allow for mean reversion in some cases deviate more from the baseline estimates. If high levels of malaria had been keeping levels of education artificially low in the pre-eradication period, then this test for mean reversion could be absorbing some of the malaria effect, making the point estimate on the malaria effect closer to zero.
Table 7.
Regional Convergence, Sri Lanka
| Baseline (Table 2) | Regional trends | Mean reversion (includes interaction with regional average 1937–1939) | |
|---|---|---|---|
| (1) | (2) | (3) | |
| Dependent variable: Years of schooling | |||
| Pre-eradication cohort × 1937 malaria rate | −3.612*** (0.515) | −2.477** (0.730) | −2.485*** (0.551) |
| Pre-eradication cohort × (1937–1939 dependent variable) | 0.164*** (0.019) | ||
| Observations | 5,822 | 5,822 | 5,822 |
| R2 | 0.17 | 0.17 | 0.17 |
|
| |||
| Dependent variable: Highly literate | |||
| Pre-eradication cohort × 1937 malaria rate | −0.294*** (0.036) | −0.281*** (0.060) | −0.185*** (0.041) |
| Pre-eradication cohort × (1937–1939 dependent variable) | 0.179*** (0.017) | ||
| Observations | 5,822 | 5,822 | 5,822 |
| R2 | 0.14 | 0.14 | 0.14 |
|
| |||
| Dependent variable: Years of primary schooling | |||
| Pre-eradication cohort × 1937 malaria rate | −1.616*** (0.156) | −1.339*** (0.236) | −1.171*** (0.157) |
| Pre-eradication cohort × (1937–1939 dependent variable) | 0.149*** (0.017) | ||
| Observations | 5,822 | 5,822 | 5,822 |
| R2 | 0.16 | 0.17 | 0.16 |
|
| |||
| Dependent variable: At least minimal literacy | |||
| Pre-eradication cohort × 1937 malaria rate | −0.269*** (0.038) | −0.298*** (0.036) | −0.171** (0.047) |
| Pre-eradication cohort × (1937–1939 dependent variable) | 0.193*** (0.038) | ||
| Observations | 5,822 | 5,822 | 5,822 |
| R2 | 0.14 | 0.14 | 0.14 |
Notes: Values of robust standard errors clustered at the regional level appear in parentheses. Column 1 repeats columns 1–4 of Table 2. All other columns include the baseline controls. Column 2 includes regional trends as additional controls. Column 3 includes an interaction with the regional average of the dependent variable as an additional control.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
Table 8.
Regional Convergence, Paraguay
| Baseline (Table 3) | Regional trends | Mean reversion (includes interaction with regional average 1958–1960) | |
|---|---|---|---|
| (1) | (2) | (3) | |
| Dependent variable: Years of schooling | |||
| Pre-epidemic cohort × 1967 malaria rate | −10.38 (9.950) | −8.716 (6.030) | 8.171 (4.700) |
| Epidemic cohort × 1967 malaria rate | −12.68* (4.845) | −12.774** (3.120) | −5.972 (3.438) |
| Pre-epidemic cohort × (1958–1960 dependent Variable) | 0.412** (0.080) | ||
| Epidemic cohort × (1958–1960 dependent variable) | 0.166* (0.059) | ||
| Observations | 2,931 | 2,931 | 2,931 |
| R2 | 0.26 | 0.26 | 0.26 |
| F-test of (pre-epidemic cohort × malaria = epidemic cohort × malaria) | 0.20 | 1.93 | 122.60 |
| p-value of F-test | 0.68 | 0.26 | 0.00 |
|
| |||
| Dependent variable: Highly literate | |||
| Pre-epidemic cohort × 1967 malaria rate | −3.033** (0.628) | −2.575* (0.812) | −2.006** (0.520) |
| Epidemic cohort × 1967 malaria rate | −2.241*** (0.350) | −2.102** (0.432) | −2.360** (0.463) |
| Pre-epidemic cohort × (1958–1960 dependent variable) | 0.226 (0.105) | ||
| Epidemic cohort × (1958–1960 dependent variable) | −0.02 (0.092) | ||
| Observations | 2,931 | 2,931 | 2,931 |
| R2 | 0.12 | 0.12 | 0.12 |
| F-test of (pre-epidemic cohort × malaria = epidemic cohort × malaria) | 6.93 | 1.47 | 21.20 |
| p-value of F-test | 0.08 | 0.31 | 0.02 |
|
| |||
| Dependent variable: Years of primary schooling | |||
| Pre-epidemic cohort × 1967 malaria rate | −8.428** (2.190) | −6.231** (1.687) | −3.021** (0.556) |
| Epidemic cohort × 1967 malaria rate | −6.055** (1.733) | −5.398*** (0.269) | −3.623 (1.784) |
| Pre-epidemic cohort × (1958–1960 dependent variable) | 0.362*** (0.023) | ||
| Epidemic cohort × (1958–1960 dependent variable) | 0.174 (0.092) | ||
| Observations | 2,931 | 2,931 | 2,931 |
| R2 | 0.14 | 0.14 | 0.14 |
| F-test of (pre-epidemic cohort × malaria = epidemic cohort × malaria) | 18.30 | 0.21 | 0.23 |
| p-value of F-test | 0.02 | 0.68 | 0.66 |
|
| |||
| Dependent variable: At least minimally literate | |||
| Pre-epidemic cohort × 1967 malaria rate | −0.957** (0.212) | 0.120 (0.487) | −0.325 (0.201) |
| Epidemic cohort × 1967 malaria rate | −0.679* (0.248) | −0.271* (0.088) | 0.228* (0.076) |
| Pre-epidemic cohort × (1958–1960 dependent variable) | 0.425** (0.120) | ||
| Epidemic cohort × (1958–1960 dependent variable) | 0.606*** (0.034) | ||
| Observations | 2,931 | 2,931 | 2,931 |
| R2 | 0.03 | 0.03 | 0.03 |
| F-test of (pre-epidemic cohort × malaria = epidemic cohort × malaria) | 54.25 | 0.79 | 17.11 |
| p-value of F-test | 0.01 | 0.44 | 0.03 |
Notes: Values of robust standard errors clustered at the regional level appear in parentheses. Column 1 repeats columns 1–4 of Table 2. All other columns include the baseline controls. Column 2 includes regional trends. Column 3 includes an interaction with the regional average of the dependent variable.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
Using the above approaches in the Paraguay sample, Table 8 shows that the baseline results are robust to the inclusion of trends. The literacy estimation that includes controls for pre-eradication levels of education is quite similar to the baseline. This is consistent with other papers like Bleakley (2007b) that found a more substantial effect on lower levels of educational attainment.
C. Contemporaneous Programs
Education or health programs that differentially affected regions with high, pre-existing malaria levels would lead to the overestimation of the malaria effect: incorrectly attributing both the effects of the other program and malaria eradication to the malaria eradication campaign. This was less likely in Paraguay because the authoritarian regime invested little in education. The first falsification test, then, is simply that the estimates for Sri Lanka are smaller than those for Paraguay.
In Sri Lanka there were not differential education programs in the areas in which malaria was the highest (S. B. Ekanayake 1982). Public health availability in the endemic region was superior to that in the less malarial regions prior to eradication: the population per hospital was lower, the population per hospital bed was similar, the population adjusted admission rates were higher, and the coverage of the central dispensaries with in-patient care was better in the highly malarial area. In the post-war era “there is no evidence for an unbalanced improvement in medical services” (R. H. Gray 1974). The malaria effect is also not due to increased smallpox vaccination (C. M. Langford 1996).
Otherwise, there were national improvements in health services, and evidence that there were some educational improvements in the capital region in which malaria was lower than the national average at the start of the program. If anything, the latter would bias results towards zero. There is also no evidence of differential nutritional improvements. Instead, individuals in the highly malarious zone had higher nutritional value in their diets than their peers in villages of lower malaria endemicity in the pre-war period (measured by daily consumption of protein, carbohydrate, calories, and minerals and a lower prevalence of malnutrition) (see Gray 1974 for a summary of this literature; Andrew Pearse 1980). Even though the timing of the decrease in malaria rates in Sri Lanka is partially coincidental with the introduction of high yield variety (HYV) rice, its introduction did not lead to differential increases in real income correlated with malaria reduction (Lester R. Brown 1970; Pearse 1980).
In Paraguay, a series of two- and five-year economic plans were written starting in 1965, but the plans were never achieved (Dannin M. Hanratty and Sandra W. Meditz 1988). A loan feasibility study undertaken in 1966 resulted in recommendations to extend infrastructure and financial services throughout the country. These proposals had not been implemented by 1975 (Conly 1975). Following the eradication there was an increase in cotton and soybean production, partly due to higher international prices and the improved health from malaria eradication. These two crops were concentrated in the districts where malaria had been the highest. Other results omitting these districts (not presented here) indicate a larger malaria effect than the baseline estimates. A final potential source of overestimation of the malaria effect is the Itaipu Dam. The dam zone is in the Departments of Alto Parana and Canendiyu, two departments that are in the more heavily malarial region. Construction on the dam started in October of 1975 and was completed in 1982. The project began producing electricity in 1984. Since the youngest woman under study was born in 1972, her compulsory primary school should have been completed by 1984 when she was 12. Therefore, the years of completed primary schooling will not be affected by electrical production. The dam lies between Brazil and Paraguay and produces electricity for both countries, but Brazil was the main beneficiary of the electricity generated as part of the project; prior to its completion Paraguay produced enough electricity to satisfy its own national requirements. Brazil was also favored in the construction contracts, producing 81 percent of the equipment used in construction. The area immediately surrounding the construction site in Paraguay was primarily settled by foreign-born Brazilians who are omitted from my sample. During the construction phase, only one third of all labor was Paraguayan, peaking at approximately 12,000 workers (Gerd Kohlhepp 1987).
VII. Conclusions
To estimate the human capital costs of continued malaria endemicity, I analyze malaria eradication campaigns from the 1940s and 1970s in Paraguay and Sri Lanka. The quasi-experimental nature of each country’s campaign allows the identification of malaria’s effects on completed education and literacy. In both countries, I find a negative and significant effect of the malaria rate on educational attainment. A 10 percentage point decrease in the incidence rate leads to an increase in the years of completed schooling of 0.1 years; an increase in the probability of being literate of 1 to 2 percentage points; an increase in years of primary schooling of 0.05 to 0.06 years; and an increase in the probability of being at least minimally literate of 0.6 to 0.8 percentage points. These findings are close to the range found by Bleakley 2007b in other countries.
To relate these estimates to countries with current malaria endemicity, the highest incidence rate of malaria reported for 2005 in Africa was 47.8 percent in Uganda (World Health Organization 2005). From this level, complete eradication would result in an increase in the years of completed education of 0.5 years. While substantial, the translation of this gain into GDP per capita in the steady state would lead to an increase far smaller than that predicted by Gallup and Sachs 2001. Of the countries with the highest level of malaria endemicity in 2005, at most 13 percent of the gain predicted in Gallup and Sachs 2001 can be attributed to the education increases from malaria eradication.19 Therefore, while continued malaria endemicity does have a first-order effect on GDP per capita in Sub-Saharan Africa through the channel of educational attainment, the Gallup and Sachs estimate of the aggregated cost of malaria is much larger than that which can be accounted for with only education.
Current malaria control and eradication campaigns place a strong emphasis on the use of insecticide-treated bed nets (ITN). Estimates for the costs and distribution of a long lasting insecticide treated bed net are $10 or less and a single ITN can cover more than one family member while sleeping. The steady state approximation of the gains in GDP per capita from eradication through the education channel alone would be $15 to $75, well beyond the cost of an ITN without taking into account the other economic channels and decreases in pain and suffering.
Acknowledgments
For generosity with their Stata code, I thank Doug Miller and Jonah Gelbach. For useful comments and suggestions, I thank Hoyt Bleakley, Andrew Foster, Douglas Gollin, Brian Knight, Isaac Mbiti, Patrick McEwan, Mark Pitt, Nancy Qian, Yona Rubinstein, David Weil, seminar participants, and three anonymous referees.
Footnotes
To comment on this article in the online discussion forum, or to view additional materials, visit the articles page at http://www.aeaweb.org/articles.php?doi=10.1257/app.2.2.46.
Other estimates of the effect of malaria come from both the growth and the development literatures. In the growth literature, John Luke Gallup and Jeffrey D. Sachs (2001) found malaria cost heavily infected countries 1.3 percentage points of per capita GDP growth per year, while Daron Acemoglu and Simon Johnson (2005) found that eradication does not increase GDP per capita or average levels of education. In the development literature, Gladys N. Conly (1975) used retrospective cost-of-illness analysis in Paraguay and estimated that individual instances of malaria result in decreased rural labor productivity. Similar findings from across Africa are summarized in D. S. Shepard et al. (1991). Other studies have quantified the importance of nonmalaria health improvements on schooling attainment (e.g., Edward Miguel and Michael Kremer 2004, Bleakley 2007a, and Seema Jayachandran and Adriana Lleras-Muney 2009).
For DDT interior residual spraying a diluted measure of DDT is sprayed on the interior walls of a house. Mosquitoes that rest on the treated walls (even after the mixture has dried) die.
In some regions of Paraguay, the National Malaria Eradication Services (NMES) placed the house numbering scheme directly on the houses to guide the spray teams (Conly 1975).
In Sri Lanka, at the low point in malaria transmission in 1963, there were 17 cases. Malaria transmission increased from this low point, and malaria continues to be a public health concern outside of the capital district. Paraguay’s low point was 1973 with 41 reported cases. Malaria has increased from this level and transmission continues to occur in the far eastern part of the country.
In Sri Lanka, regions consist of multiple districts. In Paraguay, regions consist of multiple departments.
Later specifications make allowances for different effects during the epidemic and pre-epidemic periods in Paraguay.
The Jaffna Peninsula appears to be an outlier in the correlation between climate and malaria due to data collection problems (Newman 1965). This region is excluded from the analysis because civil disturbances prevented the collection of individual survey data.
The Eastern Coastal Belt and Northern Province were excluded due to civil disturbances.
Formally, the series of β̂c are estimated from . Full results are available from the author.
Differential access to health services or knowledge about malaria could bias this number. The bias would understate the level of malaria outside of the capital district. Since the capital district has the lowest level of malaria in the sample, understatement of the malaria rates in the rest of the country could lead to an overstatement of the effect of a unit change in the malaria rate.
Paraguay is prone to malaria epidemics resulting from variations in rainfall. The epidemic of 1965 was caused by an increase in rainfall which facilitated a longer malaria transmission season. Qualitative evidence of the period does not suggest widespread changes in productive capacity as a direct result of the increased rainfall (Conly 1975).
Formally, the series of β̂c are estimated from . Full results are available from the author.
Because the classification of cohorts is mutually exclusive, this calculation is from the estimate of the coefficient on malariaj × epidemicc.
Where the 1967 malaria rate has a maximum of 0.0609, when interacted with the years of epidemic exposure, the maximum value of the new interaction term is 0.0102 (exposure of three years). The new coefficients on the epidemic interaction are similar in scale to the fetal-origins estimates when divided by 6.
Based on the 12 years in which the national incidence rate and national spleen rate overlap, I estimate with an R2 of 0.98.
The ideal assignment to birth regions is not possible.
The index maps temperature, precipitation, and characteristics of the dominant mosquito species to 0.50 worldwide grid of malaria tranmission. From this index, I created a weighted average by area for each of the DHS regions in Sri Lanka and Paraguay.
The primary explanation for the weak relationship between the transmission index and the malaria rates in Paraguay is in the capital district (Greater Asuncion). The malaria levels were low there during the 1967 epidemic and beyond, but the index predicts a rate higher than other regions.
Formally, data on education and GDP are available in Barro and Lee 2000, and Heston, Summers, and Aten 2002 for 13 of the 20 most heavily endemic countries based on the classifications in World Health Organization 2005. From the Sri Lanka estimate, I calculate the expected increase in years of completed education with malaria eradication. Using the returns to education in Hall and Jones 1999, I estimate the increase in GDP per capita in the Solow steady state assuming no other changes to a country’s production function. Gallup and Sachs 2001 predict gains in steady state GDP per capita of up to 57 percent for these countries.
References
- Acemoglu Daron, Johnson Simon. Disease and Development: The Effect of Life Expectancy on Economic Growth. Journal of Political Economy. 2007;115(6):925–85. [Google Scholar]
- Barro Robert J, Lee Jong-Wha. Center for International Development at Harvard University Working Paper 42. 2000. International Data on Educational Attainment: Updates and Implications. [Google Scholar]
- Bertrand Marianne, Duflo Esther, Mullainathan Sendhil. How Much Should We Trust Differences-in-Differences Estimates? Quarterly Journal of Economics. 2004;119(1):249–75. [Google Scholar]
- Bleakley Hoyt. Disease and Development: Evidence from Hookworm Eradication in the American South. Quarterly Journal of Economics. 2007a;122(1):73–117. doi: 10.1162/qjec.121.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleakley Hoyt. Malaria in the Americas: A Retrospective Analysis of Childhood Exposure. 2007b doi: 10.1257/app.2.2.1. home.uchicago.edu/~bleakley/Bleakley_Malaria_August2007.pdf. [DOI] [PMC free article] [PubMed]
- Brown Lester R. Seeds of Change: The Green Revolution and Development in the 1970’s. New York: Praeger Publishers; 1970. [Google Scholar]
- Cameron A Colin, Gelbach Jonah B, Miller Douglas L. Bootstrap-Based Improvements for Inference with Clustered Errors. Review of Economics and Statistics. 2008;90(3):414–27. [Google Scholar]
- Conly Gladys N. Scientific Publication Number 297. Pan American Health Organization, Pan American Sanitary Bureau, Regional Office of the World Health Organization; Washington, DC: 1975. The Impact of Malaria on Economic Development: A Case Study. [Google Scholar]
- Department of Census and Statistics. Sri Lanka Census of Population and Housing 1981. Vol. 2. Colombo, Sri Lanka: 1985. Sep, [Google Scholar]
- Duffy Patrick E, Desowitz Robert S. Pregnancy Malaria Throughout History: Dangerous Labors. In: Duffy Patrick E, Fried Michal., editors. Malaria in Pregnancy: Deadly Parasite, Susceptible Host. New York: Taylor & Francis; 2001. pp. 1–27. [Google Scholar]
- Ekanayake SB. Multiple Class Teaching and Education of Disadvantaged Groups: National Studies India, Sri Lanka, Philippines, Republic of Korea. Bangkok, Thailand: United Nations Educational, Scientific, and Cultural Organization (UNESCO) Regional Office for Education in Asia and Pacific; 1982. National Case Study–Sri Lanka; pp. 40–77. [Google Scholar]
- Gallup John Luke, Sachs Jeffrey D. The Economic Burden of Malaria. American Journal of Tropical Medicine and Hygiene. 2001;64(1, 2 S):85–96. doi: 10.4269/ajtmh.2001.64.85. [DOI] [PubMed] [Google Scholar]
- Gelbach Jonah B, Klick Jonathan, Stratmann Thomas. Cheap Donuts and Expensive Broccoli: The Effect of Relative Prices on Obesity. 2007 www.law.yale.edu/documents/pdf/.../JKlick_Cheap_Donuts.pdf.
- Gray RH. The Decline of Mortality in Ceylon and the Demographic Effects of Malaria Control. Population Studies. 1974;28(2):205–29. [PubMed] [Google Scholar]
- Hall Robert E, Jones Charles I. Why Do Some Countries Produce So Much More Output Per Worker Than Others? Quarterly Journal of Economics. 1999;114(1):83–116. [Google Scholar]
- Hanratty Dannin M, Meditz Sandra W. A Country Study: Paraguay. Federal Research Division, Library of Congress; Washington, DC: 1988. Dec, [Google Scholar]
- Heckman James J, Krueger Alan B. Inequality in America: What Role for Human Capital Policies? Cambridge, MA: MIT Press; 2003. [Google Scholar]
- Heston Alan, Summers Robert, Aten Bettina. Penn World Table Version 6.1. Center for International Comparisons at the University of Pennsylvania (CICUP); Philadelphia: 2002. Oct, [Google Scholar]
- Holding PA, Snow RW. Impact of Plasmodium Falciparum Malaria on Performance and Learning: Review of the Evidence. American Journal of Tropical Medicine and Hygiene. 2001;64(1, 2 S):68–75. doi: 10.4269/ajtmh.2001.64.68. [DOI] [PubMed] [Google Scholar]
- Jayachandran Seema, Lleras-Muney Adriana. Life Expectancy and Human Capital Investments: Evidence from Maternal Mortality Declines. Quarterly Journal of Economics. 2009;124(1):349–97. [Google Scholar]
- Kiszewski Anthony, Mellinger Andrew, Spielman Andrew, Malaney Pia, Sachs Sonia Ehrlich, Sachs Jeffrey. A Global Index Representing the Stability of Malaria Transmission. American Journal of Tropical Medicine and Hygiene. 2004;70(5):486–98. [PubMed] [Google Scholar]
- Kohlhepp Gerd. Socio-economic and Ecological Consequences of the Itaipu Dam and Reservoir on the Rio Parana (Brazil/Paraguay) Braunschweig, Germany: Vieweg; 1987. Itaipu: Basic Geopolitical and Energy Situation. [Google Scholar]
- Konradsen F, Amerasinghe FP, van der Hoek W, Amerasinghe PH. Malaria in Sri Lanka: Current Knowledge on Transmission and Control. Colombo, Sri Lanka: International Water Management Institute; 2000. [Google Scholar]
- Langford CM. Reasons for the Decline in Mortality in Sri Lanka Immediately After the Second World War: A Re-Examination of the Evidence. Health Transition Review. 1996;6(1):3–23. [Google Scholar]
- Lucas Adrienne M. Impact of Malaria Eradication on Fertility. 2010. Unpublished. [Google Scholar]
- Meegama SA. Determinants of Mortality Change and Differentials in Developing Countries. New York: United Nations; 1986. The Mortality Transition in Sri Lanka. [Google Scholar]
- Miguel Edward, Kremer Michael. Worms: Identifying Impacts on Education and Health in the Presence of Treatment Externalities. Econometrica. 2004;72(1):159–217. [Google Scholar]
- Newman Peter. Malaria Eradication and Population Growth With Special Reference to Ceylon and British Guiana. Ann Arbor: University of Michigan School of Public Health; 1965. [Google Scholar]
- Pearse Andrew. Seeds of Plenty, Seeds of Want: Social and Economic Implications of the Green Revolution. Oxford: Clarendon Press; 1980. [Google Scholar]
- Republica del Paraguay. Technical Report. 1973. Evaluacion del Programa de Erradicacion del Paludismo. [Google Scholar]
- Roll Back Malaria. Roll Back Malaria Partnership Secretariat. World Health Organization; Geneva, Switzerland: 2009. Malaria in Africa Info Sheet. http://www.rollbackmalaria.org/multimedia/rbminfosheets.html. [Google Scholar]
- Shepard DS, Ettling MB, Brinkmann U, Sauerborn R. The Economic Cost of Malaria in Africa. Tropical Medicine and Parasitology. 1991;42(3):199–203. [PubMed] [Google Scholar]
- Wickremesinghe WG. Administration Report of the Acting Director of Health Services for 1952. Ceylon (Sri Lanka): Ceylon Government Press; 1953. [Google Scholar]
- World Health Organization. Africa Malaria Report 2003. World Health Organization/UNICEF; Geneva, Switzerland: 2003. [Google Scholar]
- World Health Organization. World Malaria Report 2005. World Health Organization/UNICEF; Geneva, Switzerland: 2005. [Google Scholar]