Abstract
Objective
Few studies have examined the correlates of psychosis in children and adolescents with Bipolar Disorder (BPD). We examined psychiatric comorbidity, familiality, and psychosocial functioning in multiple domains in BPD children and adolescents with and without psychotic features.
Methods
As part of two ongoing family-based studies of children and adolescents with BPD, we compared youth and their families with psychotic symptoms (BPD+P) and without psychotic symptoms (BPD−P). All youth and family members were assessed by structured psychiatric interviews in a blinded manner. One study was conducted from January 2000 through December 2004, and the other study was conducted from February 1997 through September 2006.
Results
Of the 226 youth with BPD, 33% manifested psychotic symptoms, as defined by the presence of hallucinations or delusions. We found that BPD+P had a greater number of BPD episodes, more psychiatric hospitalizations, and significantly higher rates of psychiatric comorbidity compared to BPD−P. Additionally, a higher percentage of BPD+P had a family history of psychosis. There was a lower processing speed and lower arithmetic scaled score in BPD+P youth, but no other meaningful differences in cognitive variables were identified between the two BPD groups. Psychosis in BPD was also associated with decreased family cohesion and poorer overall global functioning.
Conclusions
In children and adolescents with BPD, those who manifest psychotic features have higher rates of comorbid psychopathology, family history of psychosis, and poorer overall functioning in multiple domains than BPD children without psychosis. Future studies should examine neuroimaging correlates, medication response, and longitudinal course of BPD children and adolescents who manifest psychosis as part of their clinical picture.
Keywords: Pediatric Bipolar Disorder, Psychosis, Comorbidity, Subtype
Introduction
Juvenile bipolar disorder (BPD) is a serious illness that is estimated to affect approximately 1–4% of children.1 Studies in child psychiatric outpatient centers have shown that up to one fifth of child and adolescent referrals present with BPD.2, 3 A large body of evidence supports that BPD can cause severe disability among youth, resulting in increased numbers of psychiatric hospitalization and severe psychosocial disability, affecting relationships with family, friends, and classmates.4–10 In addition, systematic studies of BPD youth have found high rates of psychiatric comorbidity.3, 10–16
Despite ongoing controversy over the phenomenology and characteristics of pediatric BPD, the available literature seems to suggest that juvenile BPD is highly heterogeneous in its presentation. The clinical manifestations of BPD in children and adolescents appear to differ from those in adults.17 For instance, adult-onset forms of BPD are often characterized by distinct prolonged mood states and inter-episode recovery, whereas childhood-onset forms often have courses of brief mood episodes with rapid cycling, mixed states, and almost no inter-episode recovery. 17 Also, unlike adult-onset forms, juvenile BPD has been reported to be associated with higher rates of psychosis, which may be related to the heterogeneity in the diagnosis of BPD.18
Studies have found that an earlier age of onset of BPD is related to more lifetime psychotic symptoms 19 and that 16%–75% of pediatric patients with BPD have had psychotic features during their disease course. 17, 20–23 The wide variability in the rate of psychosis may be related to differing definitions of psychosis in children, including, for example, whether grandiosity is a psychotic delusion or a manic symptom, or whether flight of ideas constitutes disordered thought or a symptom of mania. For instance, Tillman et al.23 recently reported that visual hallucinations and grandiose delusions were most common in psychotic pediatric BPD. Another study found that auditory hallucinations were most common in children with BPD.24 In the review by Pavuluri et al.,18 grandiose delusions were reported to be the most common delusions and auditory hallucinations the most common type of hallucinations in children with BPD.
Even though psychotic symptoms have been clearly reported in children and adolescents with BPD25, their impact and significance remain understudied. Among adults, previous research suggests that psychosis linked with mood is associated with poorer functioning, more severe symptomatology, and a worsened prognosis and psychosocial functioning in comparison to non-psychotic mood disorders.26–31 Some groups have suggested or debated whether psychotic mood disorders may represent a separate subtype of mood disorders. 26 Other studies have examined the disease course and prognosis in psychotic and nonpsychotic juveniles with BPD. Psychosis in pediatric BPD has been associated with more rapid mood changes, more psychiatric hospitalizations, greater psychiatric comorbidity, poorer outcome, and suicidal ideation and attempts.32–37 Moreover, a significantly higher percentage of depression, anxiety, and suicide attempts was found in first-degree family members of individuals with psychosis compared to those without psychosis.35
Although it is generally believed that children with BPD with psychotic features ultimately do worse than those without, there is limited data on why this is so. Thus, a better understanding of the clinical characteristics and functional capacity of BPD juveniles with and without psychotic features would be helpful to further understand the differences in functioning and outcome in this population. Furthermore, while the limited data available suggest the possibility that BPD with psychotic features might represent a subtype of BPD rather than simply a specifier of BPD severity, as has been suggested for mood disorders with psychotic features in adults, further examination of clinical features and familiality can assist in addressing this.
To this end, as part of two ongoing and controlled, longitudinal family studies of BPD in children and adolescents, we examined the impact of psychotic symptoms in juveniles with BPD. Based on the literature, we hypothesized that youth with psychosis as part of their bipolarity would have a more severe form of BPD, as characterized by higher rates of psychiatric comorbidity and increased impairment in social, family, cognitive, and overall functioning. Secondly, we examined whether BPD youth with psychotic features (BPD+P) also had differences in the intrinsic features of BPD compared to BPD youth without psychotic features (BPD−P), namely in onset of BPD, duration, episodicity, symptomatology, and family history.
Method
Subjects
Subjects were derived from two identically-designed ongoing longitudinal, case-control family studies of BPD children and adolescents. The methods of the study have been described in detail in recent reports.38, 39 Briefly, subjects were recruited from the same catchment area through newspaper advertisements, internet postings, clinical referrals to our program, and internal postings within the Partners/Massachusetts General Hospital (MGH) system.
Probands were between the ages of 4 and 18 with at least one parent available to complete an interview about the child. Potential subjects were excluded from initial ascertainment if they had been adopted or if their nuclear family was not available for study. We excluded any youth with major sensorimotor handicaps, profound disorders of language such as autism, inadequate command of the English language, or a Full Scale IQ less than 70. Parents provided written informed consent for their children, and children provided written assent to participate. The institutional review board at MGH approved this study.
We selected subjects through a two-stage ascertainment procedure if they were not clinically referred. The first stage assessed the diagnosis of BPD by screening all children using a telephone questionnaire conducted with their primary caregiver, which queried about symptoms of BPD and study exclusion criteria. The second stage confirmed the diagnosis of BPD using a clinical and structured psychiatric interview, as described below. Only subjects who received a positive diagnosis at both stages were included in the study sample. In only one of the studies, we also screened for non-mood disordered controls in two stages.39 First, control primary caregivers responded to the telephone questionnaire; then eligible controls meeting study entry criteria were recruited for the study and received the diagnostic assessment with a structured interview. Controls were selected only if they were classified as not having any mood disorders at both stages. We excluded controls with any mood disorder because of concerns about potential “manic switching” from dysthymia or unipolar depression to BPD.9
Assessments
All diagnostic assessments were made using DSM-IV-based structured diagnostic interviews performed by carefully selected and extensively trained raters with bachelor's or master's degrees in psychology. The interviewers first underwent several weeks of classroom-style training, learning interview mechanisms, diagnostic criteria, and coding algorithms. Then they observed interviews by experienced raters and clinicians. They subsequently conducted at least six practice (non-study) interviews and at least six practice (study) interviews while being observed by senior interviewers. Trainees were not permitted to conduct interviews independently until they executed at least three interviews that achieved perfect diagnostic agreement with an observing senior interviewer. Senior investigators supervised the interviewers throughout the study.40
Interviewers were blind to the ascertainment status of the subjects. Psychiatric assessments of youth relied on the DSM-IV Kiddie Schedule for Affective Disorders-Epidemiologic Version (KSADS-E)41 and were based on indirect interviews with the primary caregivers about the subject as well as direct interviews with subjects. Psychiatric diagnosis of relatives older than 18 years relied on the DSM-IV Structured Clinical Interview (SCID-IV)42 supplemented with modules from the K-SADS-E to capture childhood disorders.
All rates of disorders were reported as lifetime prevalence. During the interview, subjects were asked to report the ages of onset and offset for each symptom they endorsed. Subjects were also asked to classify the impairment associated with a given diagnosis (i.e. minimal, moderate, or severe), as well as the type and ages of onset and offset of treatment (therapy, medication, and/or hospitalization) for the diagnosis.43 A disorder was considered positive if DSM-IV diagnostic criteria were unequivocally met. We combined data from both direct and indirect interviews by considering a diagnostic criterion positive if it was endorsed in either interview.40 Although standardized algorithms were used to determine each diagnosis, interviewers needed a mechanism to determine the clinical relevance of symptoms when subjects were only able to provide unclear or imprecise information. Thus, a committee of board-certified child and adult psychiatrists who were blind to the subject's status, referral source, and all other data resolved diagnostic uncertainties. Diagnoses presented for review were considered positive only when the committee determined that diagnostic criteria were met to a clinically meaningful degree. We estimated the reliability of the diagnostic review process by computing kappa coefficients of agreement for clinician reviewers. For these diagnoses, the median reliability between individual clinicians and the review committee assigned diagnoses was 0.87.
To assess the reliability of our overall diagnostic procedures, we computed kappa coefficients of agreement by having three experienced, blinded, board-certified child and adult psychiatrists listen to audio-taped interviews of assessment staff administering the structured diagnostic interview to the subjects. While listening, the psychiatrists conducted their own assessment of the subject. The kappa coefficient was than calculated to measure the diagnostic inter-rater reliability between the assessment staff and the psychiatrist. Thus, both raters had access to the same information to calculate their diagnosis for each subject. Based on 500 assessments from interviews of children and adults, the median kappa coefficient was 0.98. Kappa coefficients for individual diagnoses included: major depression (1.0), mania (0.95), attention deficit hyperactivity disorder (ADHD; 0.88), conduct disorder (CD; 1.0), oppositional defiant disorder (ODD; 0.90), antisocial personality disorder (ASPD; 0.80), and substance use disorder (1.0).
As reported previously,44 for a subject to be diagnosed with BPD, he or she had to meet full DSM-IV criteria for bipolar I or II disorder. We classified the child as having bipolar I disorder if they met full criteria for a manic or mixed episode with associated impairment not induced exclusively by substances or attributable to other psychiatric illnesses. Therefore, the child had to meet criterion A for a period, lasting one week or longer, of extreme and persistently elevated, expansive, or irritable mood; plus criterion B, manifested by three (four if the mood was irritable only) of seven symptoms during the period of mood disturbance; plus criterion C, associated impairment. To be given a diagnosis of subthreshold BPD, the child must have met criterion A for a period of four days or longer, have at least two (three if the mood was irritable only) of the seven criterion B symptoms, and have associated impairment.43
For the SCID, subjects were diagnosed in a similar manner to the KSADS-E. To establish a period of time characterized by the mood features, in section A of the mania section we asked screening questions about euphoria and irritability. Then, for each screen that was endorsed, we addressed the corresponding criteria in section B. To be classified as having a mixed episode, the child must have met both the DSM-IV criteria for a manic episode and for a major depressive episode nearly every day during at least a one-week period. The mood disturbance must have been sufficiently severe to cause marked impairment in occupational functioning, usual social activities, relationships with others, or to necessitate hospitalization to prevent harm to self or others. The symptoms must not have been due to the direct physiological effects of a substance or a general medical condition.
We classified the child as having bipolar II disorder if they had a clinical course characterized by one or more major depressive episodes accompanied by at least one hypomanic episode not induced by substances or attributable to other psychiatric illnesses.44 Hypomania was diagnosed when subjects had active manic mood and associated symptoms for at least 4 days but did not meet full duration criteria for mania, or if the subjects did not manifest at least marked impairment during an episode (e.g. hospitalization). In all cases, the mood disturbance must have been sufficiently severe to cause marked impairment.
Lifetime BPD episodes were classified as the number of distinct and separate BPD episodes that met either full or subthreshold DSM-IV criteria for Mania. The subject was then asked to quantify the number of episodes he/she experienced. If he/she reported a discrete number of episodes, data on the age at which they experienced it and the length of each episode were gathered. Otherwise, the subject was asked to quantify the number of episodes he or she had per year or month. If the subject gave a range for the number of episodes, the higher number of episodes was used to calculate the total number of episodes experienced. In the case that a subject met both subthreshold criteria at one point and full criteria at another, only the number of episodes during which the subject met full criteria was coded.
To be classified as having psychosis, the child had to meet the criteria based on the DSM-IV KSADS-E. The following symptoms were recorded as delusions: delusion of guilt or sin, reference delusion, grandiosity, somatic delusion, thought insertion delusion, delusion of persecution, nihilism, delusion of control, delusion of message from TV or radio, thought broadcasting, or other delusions. The following symptoms were recorded as hallucinations: auditory, visual, tactile, olfactory, or other hallucinations. All cases of psychosis were further reviewed with a senior child and adolescent psychiatrist or psychologist.
Functioning Assessments
The DSM-IV Global Assessment of Functioning (GAF) rating scale was used to rate the overall functioning of subjects. Subjects were given a score of 0–90, with 90 being the highest possible score indicating the least impairment in their social, occupational, psychological and physical functioning.45 GAF scores were assigned to each participant based on the information obtained through the diagnostic interviews, and were also reviewed by the committee. Scores reported represent lowest lifetime score.
The Hollingshead Four-Factor Index was used to assess socioeconomic status (SES) on a scale of 1–5; 1 representing the most affluent social class and 5 the least affluent.46 The Social Adjustment Inventory for Children and Adolescents (SAICA),47 a semi-structured interview administered to the child or parent, was used to measure social functioning in children 6 to 18 years old. Content areas assessed included activities, peer relations, family relations, and academic performance. The Family environment scale (FES)48, a series of true or false statements administered following the structured interview, was used to measure cohesion, intactness, and freedom of expression in the family environment of the subject. We present a summary number for the FES score.
Cognitive testing
The methods of our cognitive testing are described in past reports.49 We estimated Full-Scale IQ (FSIQ50) from the Vocabulary and Block Design subtests of the Wechsler Intelligence Scale for Children – Third Edition (WISC-III51) for individuals aged 7–17 years and the Wechsler Adult Intelligence Scale – Third Edition (WAIS-III52) for all individuals aged >17 years. The remaining tests included components of attention, executive functions, processing speed and verbal learning.49 All scores reflect age-based standard scores from published manuals. Tests were administered and scored by psychometricians trained and supervised by licensed neuropsychologists.49
Statistical Analysis
We examined the demographic factors between probands with and without psychosis (BPD+P versus BPD−P). We used Student's t-test for continuous outcomes, the Wilcoxon rank-sum tests for SES, and Pearson's χ2 tests for binary outcomes.
To examine the impact of psychotic symptoms in juveniles with BPD, we used Pearson's χ2 tests for binary outcomes, Student's t-tests for linear outcomes, and the Wilcoxon rank-sum tests for ordinal outcomes. We also used logistic regression for binary outcomes, linear regression for linear outcomes, and ordered logistic regression for ordinal outcomes when adjusting for age. To analyze information from the SAICA, we created a binary variable to represent any negative response (rated 3 or 4 on any question). We conducted all statistical analyses using Stata 10.0.53 Diagnoses were defined as any positive response at any assessment. All tests were two-tailed, and our alpha level was set at 0.05 for all analyses. Data are presented as mean±standard deviation (SD) unless otherwise specified.
Results
Demographic Characteristics
Among the 330 probands available for study, 98 controls were dropped from all analyses, as well as 4 (1%) of BPD probands due to missing data. The final sample size consisted of 226 subjects, including 151 (67%) BPD−P and 75 (33%) BPD+P.
We stratified our sample by those with and without psychotic symptoms as part of their clinical picture (Table 1). Compared to BPD−P, BPD+P subjects had a greater number of BPD episodes and were older at time of assessment. BPD+P subjects also had a greater number of lifetime BPD symptoms and a greater number of lifetime psychiatric hospitalizations compared to BPD−P subjects. We did not find any significant differences between the groups in sex, age of BPD onset, gender, race, or the mean number of psychiatric medications taken per subject throughout their lifetime (all p values >0.05).
Table 1.
Demographics of Sample Population (N=226)
| BPD−P (N=151) | BPD+P (N=75) | p-value | |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
|
| |||
| Age | 12.81 (3.35) | 13.80 (3.53) | 0.04 |
| SES* | 1.94 (0.97) | 2.00 (0.97) | 0.65 |
| BPD Onset | 7.04 (3.92) | 6.54 (4.01) | 0.37 |
| # BPD Symptoms ** | 5.77 (1.33) | 6.19(1.13) | 0.02 |
| # BPD Episodes *** | 19.92(34.48) | 63.39(126.33) | 0.00 |
| BPD Treatment Onset | 8.18(3.43) | 7.89(3.74) | 0.5 |
| Psychiatric Medication** | 1.01(1.60) | 1.47(1.94) | 0.06 |
| Psychiatric Hospitalizations ** | 0.93(1.76) | 2.11(2.38) | 0.00 |
|
| |||
| N (%) | N (%) | ||
|
| |||
| Gender (% Male) | 110 (73) | 59 (79) | 0.34 |
| Race (% White) | 143(95) | 69 (95) | 0.92 |
The Hollingshead Four-Factor Index was used to assess socioeconomic status (SES) on a scale of 1 through 5; 1 representing most affluent social class, 5 least affluent.46
Total number per subject throughout his or her lifetime
The number of episodes represents distinct and separate BPD episodes that met either full or subthreshold DSM-IV criteria for Mania.
BPD = Bipolar Disorder
BPD+P = Bipolar Disorder with Psychosis
BPD−P = Bipolar Disorder without Psychosis
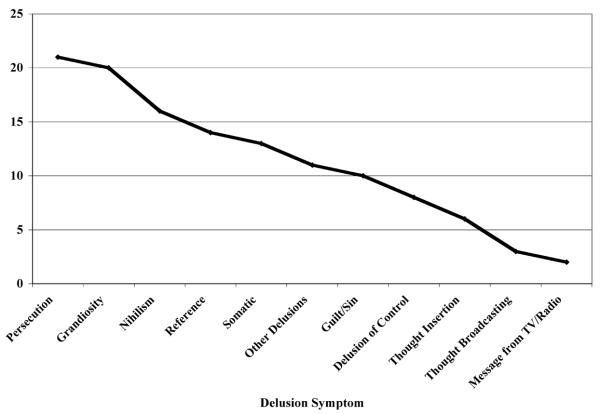
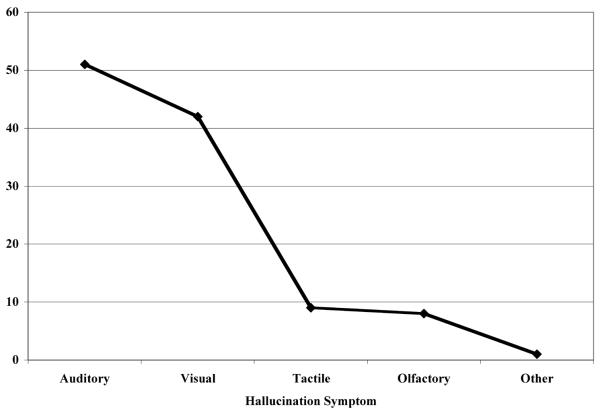
Figure 1 (a and b) shows the number of BPD+P subjects who endorsed specific delusion or hallucination symptoms, respectively. We found that persecutory delusions were the most common type of delusion in this group, and auditory hallucinations were the most frequently endorsed type of hallucination.
Figure 1a.
Specific Delusions Endorsed by BPD Children and Adolescents with Psychosis (N=69)
Figure 1b.
Specific Hallucination Symptoms Endorsed by BPD Children and Adolescents with Psychosis (N=69)
Psychiatric Comorbidity in Youth with BPD
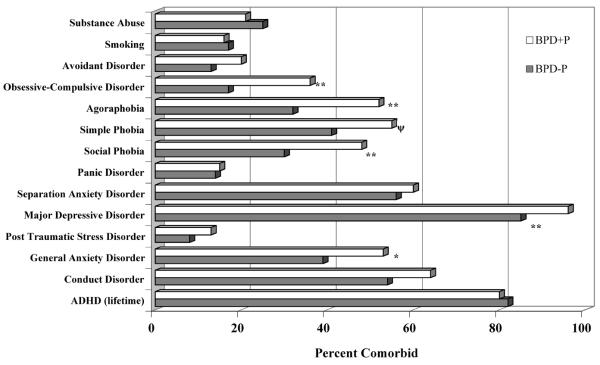
We found that BPD+P youth had significantly more comorbid mood and anxiety disorders than BPD−P youth (Figure 2). Compared to BPD−P subjects, a significantly greater percentage of BPD+P subjects had lifetime Major Depressive Disorder (χ2=6.20, 1 d.f., p=0.01), Generalized Anxiety Disorder (χ2=4.14, 1 d.f., p=0.04), Agoraphobia (χ2=8.65, 1d.f., p<0.01), Social Phobia (χ2=6.67, 1 d.f., p=0.01), and Obsessive Compulsive Disorder (χ2=9.85, 1 d.f., p<0.01). Due to the significant difference in age between the two groups, we additionally adjusted for age. All associations remained significant with only Generalized Anxiety Disorder as a trend (p=0.058).
Figure 2.
Psychiatric comorbidity stratified by psychosis among BPD children and adolescents (N=226)
*p <0.05
**p≤0.01
Ψ trend, p=0.05.
BPD+P = Bipolar Disorder with Psychosis; BPD−P = Bipolar Disorder without Psychosis.
Psychosocial and Cognitive Functioning
To evaluate how our youth with BPD were performing, we examined global, family, and cognitive functioning. Children and adolescents with BPD+P had significantly lower past GAF scores compared to BPD−P (35.75 ± 4.59 and 40.32 ± 5.84; t(224)=5.93, p<0.01). When we examined family environment through the FES, we found that BPD+P youth had lower current cohesion than BPD−P (z=2.05; p=0.04); however, no differences emerged in comparing expression and conflict scores between groups (all p-values >0.05). Additionally, when we examined social and academic functioning through the SAICA, we found no significant differences between groups (all p-values >0.05).
Through cognitive assessments, we found that BPD+P compared to BPD−P group had a lower arithmetic scaled score (8.67 ± 3.64 compared to 9.79 ± 3.44; z=2.072, p=0.04) and a lower mean processing speed (85.1 ± 2.18 compared to 90.4 ± 1.32; t(169)=2.21, p=0.03). However, when examining other cognitive measures, including vocabulary IQ, full IQ, and WRAT vocabulary, we did not find any significant difference between the two groups (all p-values > 0.05). When we adjusted for age, current cohesion on the FES became a trend (p=0.07), while no other association gained or lost significance.
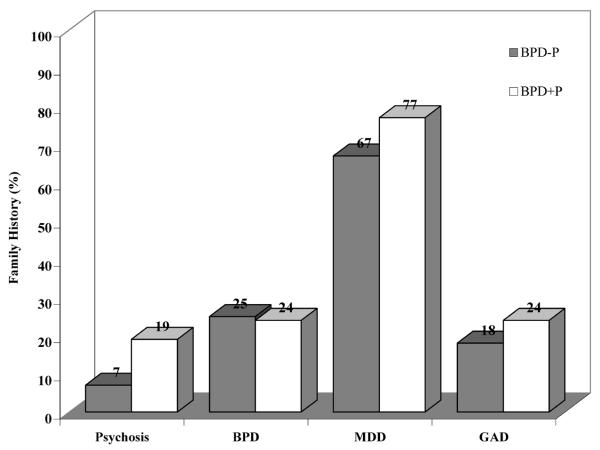
Familiality
We then examined the familiality of psychosis within BPD (Figure 3). Significantly more BPD+P subjects had a positive family history of psychosis (either parent must have met criteria for lifetime diagnosis) compared to their BPD−P counterparts (χ2=7.66, 1 d.f., p=0.01). More specifically, we found that 19% (N=14/75) of BPD+P and 7% (N=10/151) of BPD−P youth had a history of psychosis in parents. There was no significant difference between groups in family history of the other disorders measured.
Figure 3.
Family history stratified by psychosis among BPD children and adolescents (N=226)
BPD+P vs BPD−P (Psychosis: χ2=7.66, 1 d.f., p=0.01).
BPD+P = Bipolar Disorder with Psychosis; BPD−P = Bipolar Disorder without Psychosis.
When we examined family history of comorbid BPD and psychosis in more detail, we found that BPD+P subjects were more likely to have parents with both BPD and psychosis (N=8/75, 11%) than BPD−P subjects (N=5/151, 3%; χ2=5.00, 1 d.f., p=0.03). We also found that among all subjects with parents with BPD (N=32), BPD+P youth (N=8/12, 67%) were more likely to have parents with comorbid psychosis than were BPD−P youth (N=5/20, 25%; χ2=5.40, 1 d.f., p=0.02). Finally, among all subjects with parents who have psychosis (N=16), BPD+P subjects (N=8/9, 89%) were not more likely than BPDP subjects to have parents with comorbid BPD (BPD−P: N=5/7, 71%; χ2=0.79, 1 d.f., p=0.4).
Discussion
We found that one-third of children and adolescents with BPD manifest psychotic symptoms, as defined by the presence of delusions and hallucinations. As hypothesized, BPD+P manifest more impairment and psychiatric comorbidity compared to BPD−P. BPD+P youth had more bipolar episodes, symptoms, hospitalizations and lower cohesion in their family environment. In addition, BPD youth with psychosis also manifested more psychiatric comorbidity compared to those without psychosis, particularly anxiety disorders. We also found that BPD+P youth were more likely to have a positive family history of psychosis. These findings indicate that BPD+P youth manifest greater psychiatric comorbidity, severity of BPD, and functional impairment in multiple domains.
Our finding that one-third of our youth with BPD had psychosis falls within the range of most reports indicating that 15% to 76% of pediatric groups with BPD also have psychotic symptoms.3, 10, 17, 19, 23, 31, 32, 54, 55 For instance, Findling et al. showed 17% of their youth with BPD also had psychotic features.17 Likewise, Birmaher et al. reported that an identical 33% of their youth with BPD manifested psychotic symptoms.15 Also in agreement with other studies, we found that the rate of psychosis in prepubescent children does not differ significantly from that in adolescents.56 Our results do differ greatly, however, from the Tillman et al. study, which found a 76% rate of psychosis in juveniles.23 This may be due to methodological differences in their use of structured interviewing and the fact that grandiosity was required in the diagnosis of BPD in this cohort of subjects, with severity of the grandiose beliefs determining whether or not they were classified as psychotic.
Like others,18, 24 we found that auditory hallucinations were the most common hallucinations, occurring in 74% of our psychotic youth. Several other groups have also shown that grandiose delusions are the most common type of delusion.18, 23, 31 Carlson et al., however, reported that paranoid delusions were more common than grandiose delusions in adolescents with BPD (100% vs. 74%, respectively).57 In the current study, we found similar rates for both persecutory delusions and grandiosity (21 out of 69 [30%] and 20 out of 69 [29%], respectively).
In congruence with previous findings, our data suggest that BPD+P youth have early-onset academic and behavior problems and more severe impairment, as determined by an increased number of depressive/manic episodes and more hospitalizations, compared to BPD−P youth.57 For instance, we found statistically significant lower global functioning scores in those with BPD+P compared to BPD−P. In addition, the cohesion score in the Family Environment Scale was significantly lower in BPD+P than in BPD−P, suggesting increased isolation. Our current findings support recently reported results showing that youth who endorsed current psychotic symptoms had greater impairment in interpersonal, work, recreational, and total domains.54 Interestingly, we failed to find differences in social functioning between groups.
We also found evidence of cognitive impairment associated with BPD+P. Compared to BPD−P, youth with BPD+P had diminished processing speed and decreased arithmetic scaled score, potentially contributing to more impaired academic and social functioning. It is noteworthy that decreased processing speed is especially frustrating in children given its covert nature.58 These children take more time and effort to complete tasks, potentially leading to poor self-esteem.58
Because children with BPD often have other psychiatric comorbidities,59, 60 we also examined if psychosis was associated with a greater burden of additional psychiatric diagnoses. In fact, as others have reported,22, 57 our data show higher risk for psychiatric comorbidity, particularly in anxiety disorders in those with psychosis. Although ADHD and conduct disorder are commonly comorbid with juvenile BPD,20, 60, 61 our BPD+P youth did not exhibit greater comorbidity with these two disorders than did BPD−P youth. We also did not find increased nicotine or substance use disorders in this subset of children.
We found that a statistically larger number of BPD+P had a parent with psychotic symptoms compared to BPD−P. We also found that among subjects with parents with BPD, BPD+P subjects were more likely to have parents who also had psychosis compared to BPD−P subjects. This is in agreement with Potash et al., who found that more psychotic probands had at least one first-degree relative who suffered from a psychotic affective disorder than nonpsychotic probands (64% vs 28%62). In the same study, clustering of psychosis was found in families of probands with bipolar type I versus probands with non-psychotic mania or hypomania. Potash et al. further suggested that the familial aggregation of psychotic symptoms possibly defined a more genetically homogeneous subtype of BPD with psychosis and that there would be value in using this subtype, especially in genetic and biological studies.62
The apparent increase in symptom severity, greater functional impairment, increased comorbidity, and high degree of familiality associated with BPD+P features that others have found and our current data support calls for more research into this entity. Improved understanding of juvenile BPD+P features could help to focus resources on the most severe cases and assist clinicians and caretakers alike in caring for these children. It is imperative that psychosis be screened when asking about symptoms of BPD. Conversely, even if it seems that psychosis alone is present, investigation into mood symptoms must be conducted as well.
The current study has several important implications. Psychosis should be carefully queried in all children with BPD. In addition, it is important to ask parents about the presence of BPD and psychosis. Children who present with psychosis as part of their BPD symptomatology must be carefully examined for the presence of further comorbidity and impairment. It is also important to note that psychosis may predict a variable treatment response. For example, it has been proposed that maintenance with an antidepressant and atypical antipsychotic in psychotic depression in adults improves prognosis and decreases relapse rate.27 Some studies in juvenile BPD have reported that response rate, as evidenced by decreased psychotic and mood symptoms, seems to be improved when an anti-psychotic is combined with a mood stabilizer.63–65 Given the high risk for anxiety associated with psychosis in BPD, treatment (pharmacological and/or psychotherapeutic) targeting anxiety might be further beneficial in management of the child's symptoms. Clearly, future studies integrating neuroimaging and genetics in juvenile BPD+P, as well as treatment effects both short and longer-term, are necessary.
There are a number of limitations in the current study. We did not have a control group of youth with psychosis without BPD, limiting our generalizability only to BPD. Although we had a relatively large sample size, we had a small sample of those subjects with available data for certain measures, such as the SAICA (N=134) and the FES (N=203). Because our sample consisted mainly of Caucasian subjects, our results may not generalize to other racial or ethnic groups. Also, since the sample was referred, our findings may not generalize to the community. Despite these limitations, this study has a number of strengths, including a relatively large sample size and a comprehensive assessment across a number of important domains, including comorbidity, cognitive testing, and family data.
Our findings show that one-third of youth with BPD manifest psychosis. These BPD children with psychosis have higher rates of other psychiatric illness, as well as more specific areas of functional impairment. Future studies need to be undertaken to examine underlying brain structure, genetic relationship, course, and treatment response in BPD children and adolescents with and without psychosis.
Acknowledgement
Funding for this study came from RO1 DA12945 (TW), K24 DA016264 (TW), K08 MH01503 (JW) and R01MH066237 (JW)
Footnotes
Previous Presentation: Dr.Liwei Hua presented preliminary findings at the 56th Annual American Academy of Child & Adolescent Psychiatry Meeting as well as the 2009 MGH-Ryan Licht Sang Bipolar Foundation Pediatric Bipolar Disorder Conference.
Conflicts of Interests: Dr. Timothy Wilens receives grant support from the following sources: Abbott, McNeil, Lilly,NIH(NIDA), Merck, and Shire. Dr. Timothy Wilens is a speaker for the following speaker's bureaus: Lilly, McNeil, Novartis, and Shire. Dr. Timothy Wilens is a consultant for: Abbott, McNeil, Lilly, NIH (NIDA), Novartis, Merck, Shire.
Dr. Joseph Biederman is currently receiving research support from the following sources: Alza, AstraZeneca, Bristol Myers Squibb, Eli Lilly and Co., Janssen Pharmaceuticals Inc., McNeil, Merck, Organon, Otsuka, Shire, NIMH, and NICHD. In 2009, Dr. Joseph Biederman received a speaker's fee from the following sources: Fundacion Areces, Medice Pharmaceuticals, and the Spanish Child Psychiatry Association. In previous years, Dr. Joseph Biederman received research support, consultation fees, or speaker's fees for/from the following additional sources: Abbott, AstraZeneca, Celltech, Cephalon, Eli Lilly and Co., Esai, Forest, Glaxo, Gliatech, Janssen, McNeil, NARSAD, NIDA, New River, Novartis, Noven, Neurosearch, Pfizer, Pharmacia, The Prechter Foundation, Shire, The Stanley Foundation, UCB Pharma, Inc. and Wyeth.
Dr. Wozniak is the author of the book, “Is Your Child Bipolar” published May 2008, Bantam Books. During 2005–2009, she has been a speaker for McNeil, Primedia/MGH Psychiatry Academy, on the Advisory Board for Pfizer and Shire and received research support from NIMH, McNeil, Shire and Lilly. Her spouse John Winkelman MD, PhD has been on the Speakers Bureau for Boehringer-Ingelheim, Cephalon, GlaxoSmithKline, King, Sanofi-Aventis, Sepracor, Takeda, on the Advisory Board for Axon Labs, Boehringer-Ingelheim, GlaxoSmithKline, Jazz Pharmaceuticals, Novartis, Neurogen, Novadel Pharma, Pfizer, UCB (Schwarz) Pharma, Sepracor, Takeda, Covance, Impax Laboratories, Luitpold, Zeo Inc and received research support from Boehringer-Ingelheim, GlaxoSmithKline, UCB (Schwarz) Pharma, Sepracor.
Dr. Liwei Hua reports no conflict of interest.
Ms. Mary Kate Martelon reports no conflicts of interest.
Ms. Patricia Wong reports no conflict of interest.
References
- 1.Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. J Am Acad Child Adolesc Psychiatry. 1995;34(4):454–463. [PubMed] [Google Scholar]
- 2.Weller RA, Weller EB, Tucker SG, Fristad MA. Mania in prepubertal children: has it been underdiagnosed? Journal of Affective Disorders. 1986;11:151–154. doi: 10.1016/0165-0327(86)90022-4. [DOI] [PubMed] [Google Scholar]
- 3.Wozniak J, Biederman J, Kiely K, et al. Mania-like symptoms suggestive of childhood-onset bipolar disorder in clinically referred children. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:867–876. doi: 10.1097/00004583-199507000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Weller EB, Weller RA, Fristad MA. Bipolar disorder in children: Misdiagnosis, underdiagnosis, and future directions. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34(6):709–714. doi: 10.1097/00004583-199506000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Wozniak J, Biederman J, Kiely K, Ablon JS, Faraone S. Scientific Proceedings of the American Academy of Child and Adolescent Psychiatry. San Antonio, TX: 1993. Prepubertal mania revisited; p. 36. [Google Scholar]
- 6.Geller B, Craney JL, Bolhofner K, Nickelsburg MJ, Williams M, Zimerman B. Two-year prospective follow-up of children with a prepubertal and early adolescent bipolar disorder phenotype. Am J Psychiatry. 2002;159(6):927–933. doi: 10.1176/appi.ajp.159.6.927. [DOI] [PubMed] [Google Scholar]
- 7.Birmaher B. Bipolar Consortium. Boston, MA: 2004. Adolescent outcome in BPD. [Google Scholar]
- 8.Geller B, Tillman R, Craney JL, Bolhofner K. Four-year prospective outcome and natural history of mania in children with a prepubertal and early adolescent bipolar disorder phenotype. Arch Gen Psychiatry. 2004 May;61(5):459–467. doi: 10.1001/archpsyc.61.5.459. [DOI] [PubMed] [Google Scholar]
- 9.Geller B, Tillman R, Bolhofner K, Zimerman B, Strauss NA, Kaufmann P. Controlled, blindly rated, direct-interview family study of a prepubertal and early-adolescent bipolar I disorder phenotype: morbid risk, age at onset, and comorbidity. Arch Gen Psychiatry. 2006 Oct;63(10):1130–1138. doi: 10.1001/archpsyc.63.10.1130. [DOI] [PubMed] [Google Scholar]
- 10.Axelson D, Birmaher B, Strober M, et al. Phenomenology of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006 Oct;63(10):1139–1148. doi: 10.1001/archpsyc.63.10.1139. [DOI] [PubMed] [Google Scholar]
- 11.Geller B, Zimerman B, Williams M, et al. Diagnostic characteristics of 93 cases of a prepubertal and early adolescent bipolar disorder phenotype by gender, puberty and comorbid attention deficit hyperactivity disorder. Journal of Child and Adolescent Psychopharmacology. 2000;10(3):157–164. doi: 10.1089/10445460050167269. [DOI] [PubMed] [Google Scholar]
- 12.Strober M, DeAntonio M, Schmidt-Lackner S, Freeman R, Lampert C, Diamond J. Early childhood attention deficit hyperactivity disorder predicts poorer response to acute lithium therapy in adolescent mania. Journal of Affective Disorders. :1–18. doi: 10.1016/s0165-0327(98)00213-4. [DOI] [PubMed] [Google Scholar]
- 13.Carlson G, Bromet E, Jandorf L. Conduct disorder and mania: What does it mean in adults. Journal of Affective Disorders`. 1998;48:199–205. doi: 10.1016/s0165-0327(97)00176-6. [DOI] [PubMed] [Google Scholar]
- 14.Geller B, Sun K, Zimerman B, Luby J, Frazier J, Williams M. Complex and rapid-cycling in bipolar children and adolescents: A preliminary study. Journal of Affective Disorders. 1995;34(4):259–268. doi: 10.1016/0165-0327(95)00023-g. [DOI] [PubMed] [Google Scholar]
- 15.Birmaher B, Axelson D. Course and outcome of bipolar spectrum disorder in children and adolescents: a review of the existing literature. Dev Psychopathol. 2006 Fall;18(4):1023–1035. doi: 10.1017/S0954579406060500. [DOI] [PubMed] [Google Scholar]
- 16.Rende R, Birmaher B, Axelson D, et al. Childhood-onset bipolar disorder: Evidence for increased familial loading of psychiatric illness. J Am Acad Child Adolesc Psychiatry. 2007 Feb;46(2):197–204. doi: 10.1097/01.chi.0000246069.85577.9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Findling RL, Gracious BL, McNamara NK, et al. Rapid, continuous cycling and psychiatric comorbidity in pediatric bipolar I disorder. Bipolar Disord. 2001 Aug;3(4):202–210. [PubMed] [Google Scholar]
- 18.Pavuluri MN, Herbener ES, Sweeney JA. Psychotic symptoms in pediatric bipolar disorder. J Affect Disord. 2004 May;80(1):19–28. doi: 10.1016/S0165-0327(03)00053-3. [DOI] [PubMed] [Google Scholar]
- 19.Suominen K, Mantere O, Valtonen H, et al. Early age at onset of bipolar disorder is associated with more severe clinical features but delayed treatment seeking. Bipolar Disord. 2007 Nov;9(7):698–705. doi: 10.1111/j.1399-5618.2007.00388.x. [DOI] [PubMed] [Google Scholar]
- 20.Wozniak J, Biederman J, Mundy E, Mennin D, Faraone SV. A pilot family study of childhood-onset mania. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34(12):1577–1583. doi: 10.1097/00004583-199512000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Craney JL, Geller B. A prepubertal and early adolescent bipolar disorder-I phenotype: review of phenomenology and longitudinal course. Bipolar Disord. 2003 Aug;5(4):243–256. doi: 10.1034/j.1399-5618.2003.00044.x. [DOI] [PubMed] [Google Scholar]
- 22.Mantere O, Suominen K, Leppamaki S, Valtonen H, Arvilommi P, Isometsa E. The clinical characteristics of DSM-IV bipolar I and II disorders: baseline findings from the Jorvi Bipolar Study (JoBS) Bipolar Disord. 2004 Oct;6(5):395–405. doi: 10.1111/j.1399-5618.2004.00140.x. [DOI] [PubMed] [Google Scholar]
- 23.Tillman R, Geller B, Klages T, Corrigan M, Bolhofner K, Zimerman B. Psychotic phenomena in 257 young children and adolescents with bipolar I disorder: delusions and hallucinations (benign and pathological) Bipolar Disord. 2008 Feb;10(1):45–55. doi: 10.1111/j.1399-5618.2008.00480.x. [DOI] [PubMed] [Google Scholar]
- 24.Ulloa RE, Birmaher B, Axelson D, et al. Psychosis in a pediatric mood and anxiety disorders clinic: phenomenology and correlates. J Am Acad Child Adolesc Psychiatry. 2000;39(3):337–345. doi: 10.1097/00004583-200003000-00016. [DOI] [PubMed] [Google Scholar]
- 25.Youngstrom EA, Birmaher B, Findling RL. Pediatric bipolar disorder: validity, phenomenology, and recommendations for diagnosis. Bipolar Disord. 2008 Feb;10(1 Pt 2):194–214. doi: 10.1111/j.1399-5618.2007.00563.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Keller J, Schatzberg AF, Maj M. Current issues in the classification of psychotic major depression. Schizophr Bull. 2007 Jul;33(4):877–885. doi: 10.1093/schbul/sbm065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Matthews JD, Siefert C, Dording C, et al. An open study of aripiprazole and escitalopram for psychotic major depressive disorder. J Clin Psychopharmacol. 2009 Feb;29(1):73–76. doi: 10.1097/JCP.0b013e318193dfb4. [DOI] [PubMed] [Google Scholar]
- 28.Goes FS, Sadler B, Toolan J, et al. Psychotic features in bipolar and unipolar depression. Bipolar Disord. 2007 Dec;9(8):901–906. doi: 10.1111/j.1399-5618.2007.00460.x. [DOI] [PubMed] [Google Scholar]
- 29.Coryell W, Leon AC, Turvey C, Akiskal HS, Mueller T, Endicott J. The significance of psychotic features in manic episodes: a report from the NIMH collaborative study. J Affect Disord. 2001 Dec;67(1–3):79–88. doi: 10.1016/s0165-0327(99)00024-5. [DOI] [PubMed] [Google Scholar]
- 30.Kempf L, Hussain N, Potash JB. Mood disorder with psychotic features, schizoaffective disorder, and schizophrenia with mood features: trouble at the borders. Int Rev Psychiatry. 2005 Feb;17(1):9–19. doi: 10.1080/09540260500064959. [DOI] [PubMed] [Google Scholar]
- 31.Canuso CM, Bossie CA, Zhu Y, Youssef E, Dunner DL. Psychotic symptoms in patients with bipolar mania. J Affect Disord. 2008 Dec;111(2-3):164–169. doi: 10.1016/j.jad.2008.02.014. [DOI] [PubMed] [Google Scholar]
- 32.Birmaher B, Axelson D, Strober M, et al. Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006 Feb;63(2):175–183. doi: 10.1001/archpsyc.63.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goldstein TR, Birmaher B, Axelson D, et al. History of suicide attempts in pediatric bipolar disorder: factors associated with increased risk. Bipolar Disord. 2005 Dec;7(6):525–535. doi: 10.1111/j.1399-5618.2005.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Caetano SC, Olvera RL, Hunter K, et al. Association of psychosis with suicidality in pediatric bipolar I, II and bipolar NOS patients. J Affect Disord. 2006 Mar;91(1):33–37. doi: 10.1016/j.jad.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 35.Rende R, Birmaher B, Axelson D, et al. Psychotic symptoms in pediatric bipolar disorder and family history of psychiatric illness. J Affect Disord. 2006 Nov;96(1-2):127–131. doi: 10.1016/j.jad.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 36.Werry JS, McClellan JM, Chard L. Childhood and adolescent schizophrenic, bipolar, and schizoaffective disorders: a clinical and outcome study. J Am Acad Child Adolesc Psychiatry. 1991 May;30(3):457–465. doi: 10.1097/00004583-199105000-00017. [DOI] [PubMed] [Google Scholar]
- 37.McClellan JM, Werry JS, Ham M. A follow-up study of early onset psychosis: comparison between outcome diagnoses of schizophrenia, mood disorders, and personality disorders. J Autism Dev Disord. 1993 Jun;23(2):243–262. doi: 10.1007/BF01046218. [DOI] [PubMed] [Google Scholar]
- 38.Wozniak J, Monuteaux M, Richards J, Lail KE, Faraone S, Biederman J. Convergence between structured diagnostic interviews and clinical assessment on the diagnosis of pediatric-onset mania. Biological Psychiatry. 2003;11:938–944. doi: 10.1016/s0006-3223(03)00344-5. [DOI] [PubMed] [Google Scholar]
- 39.Wilens TE, Martelon M, Kruesi MJ, et al. Does conduct disorder mediate the development of substance use disorders in adolescents with bipolar disorder? A case-control family study. J Clin Psychiatry. 2009 Feb;:10. doi: 10.4088/jcp.08m04438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Biederman J, Monuteaux M, Mick E, et al. Young Adult Outcome of Attention Deficit Hyperactivity Disorder: A Controlled 10 year Follow-Up Study. Psychological Medicine. 2006;36:167–179. doi: 10.1017/S0033291705006410. [DOI] [PubMed] [Google Scholar]
- 41.Ambrosini PJ. Historical development and present status of the schedule for affective disorders and schizophrenia for school-age children (K-SADS) J Am Acad Child Adolesc Psychiatry. 2000;39(1):49–58. doi: 10.1097/00004583-200001000-00016. [DOI] [PubMed] [Google Scholar]
- 42.First M, Spitzer R, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders. American Psychiatric Press; Washington, D.C.: 1997. [Google Scholar]
- 43.Biederman J, Petty CR, Wilens TE, et al. Examination of concordance between maternal and youth reports in the diagnosis of pediatric bipolar disorder. Bipolar Disord. 2009 May;11(3):298–306. doi: 10.1111/j.1399-5618.2009.00671.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wilens T, Biederman J, Wozniak J, Gunawardene S, Wong J, Monuteaux M. Can Adults with Attention-Deficit Hyperactivity Disorder be Distinguished from those with Comorbid Bipolar Disorder: Findings from a Sample of Clinically Referred Adults. Biological Psychiatry. 2003;54(1):1–8. doi: 10.1016/s0006-3223(02)01666-9. [DOI] [PubMed] [Google Scholar]
- 45.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders: Fourth Edition Text Revision (DSM-IV-TR) 4th ed American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- 46.Hollingshead AB. Four factor index of social status. Yale University Press; New Haven, CT: 1975. [Google Scholar]
- 47.Orvaschel H, Walsh G. Assessment of Adaptive Functioning in Children: A Review of Existing Measures Suitable for Epidemiological and Clinical Services Research. U.S. Department of Health and Human Services, National Institute of Mental Health, Division of Biometry and Epidemiology; Washington, DC: 1984. [Google Scholar]
- 48.Moos RH, Moos BS. Manual for the Family Environment Scale. Consulting Psychologists Press; Palo Alto, CA: 1974. [Google Scholar]
- 49.Doyle AE, Wilens T, Kwon A, et al. Neuropsychological functioning in youth with bipolar disorder. Biological Psychiatry. 2005 doi: 10.1016/j.biopsych.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 50.Sattler J. Psychological Assessment. Fourth ed McGraw-Hill; New York: 1988. [Google Scholar]
- 51.Wechsler D. Manual for the Wechsler Intelligence Scale for Children. Third Edition The Psychological Corporation, Harcourt Brace Jovanovich, Inc.; San Antonio: 1991. [Google Scholar]
- 52.Wechsler D. Wechsler Adult Intelligence Scale III [manual] 3rd ed The Psychological Corporation; San Antonio, TX: 1997. [Google Scholar]
- 53.Stata Corporation . Stata User's Guide: Release 9. Stata Corp LP; College Station, TX: 2005. [Google Scholar]
- 54.Goldstein TR, Birmaher B, Axelson D, et al. Psychosocial functioning among bipolar youth. J Affect Disord. 2009 Apr;114(1-3):174–183. doi: 10.1016/j.jad.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Biederman J, Faraone SV, Wozniak J, et al. Clinical correlates of bipolar disorder in a large, referred sample of children and adolescents. J Psychiatr Res. 2005 Nov;39(6):611–622. doi: 10.1016/j.jpsychires.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 56.Geller B, Tillman R. Prepubertal and early adolescent bipolar I disorder: review of diagnostic validation by Robins and Guze criteria. J Clin Psychiatry. 2005;66(Suppl 7):21–28. [PubMed] [Google Scholar]
- 57.Carlson GA, Bromet EJ, Sievers S. Phenomenology and outcome of subjects with early- and adult-onset psychotic mania. Am J Psychiatry. 2000;157(2):213–219. doi: 10.1176/appi.ajp.157.2.213. [DOI] [PubMed] [Google Scholar]
- 58.Micco JA, Henin A, Biederman J, et al. Executive functioning in offspring at risk for depression and anxiety. Depress Anxiety. 2009;26(9):780–790. doi: 10.1002/da.20573. [DOI] [PubMed] [Google Scholar]
- 59.Kowatch RA, Fristad M, Birmaher B, Wagner KD, Findling RL, Hellander M. Treatment guidelines for children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2005 Mar;44(3):213–235. doi: 10.1097/00004583-200503000-00006. [DOI] [PubMed] [Google Scholar]
- 60.Wilens TE, Vitulano M, Upadhyaya H, et al. Cigarette Smoking Associated with Attention Deficit Hyperactivity Disorder. Journal of Pediatrics. 2008 Jun;:4. doi: 10.1016/j.jpeds.2008.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kovacs M, Pollock M. Bipolar disorder and comorbid conduct disorder in childhood and adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34(6):715–723. doi: 10.1097/00004583-199506000-00011. [DOI] [PubMed] [Google Scholar]
- 62.Potash JB, Willour VL, Chiu YF, et al. The familial aggregation of psychotic symptoms in bipolar disorder pedigrees. Am J Psychiatry. 2001 Aug;158(8):1258–1264. doi: 10.1176/appi.ajp.158.8.1258. [DOI] [PubMed] [Google Scholar]
- 63.Delbello MP, Schweirs H, Rosenberg H, Strakowski SM. A double-blind, randomized, placebo-controlled study of quetiapine as adjunctive treatment for adolescent mania. J Am Acad Child Adolesc Psychiatry. 2002;41:1216–1223. doi: 10.1097/00004583-200210000-00011. [DOI] [PubMed] [Google Scholar]
- 64.Kafantaris V, Coletti DJ, Dicker R, Padula G, Kane JM. Adjunctive antipsychotic treatment of adolescents with bipolar psychosis. J Am Acad Child Adolesc Psychiatry. 2001;40(12):1448–1456. doi: 10.1097/00004583-200112000-00016. [DOI] [PubMed] [Google Scholar]
- 65.Pavuluri MN, Henry DB, Carbray JA, Sampson G, Naylor MW, Janicak PG. Open-label prospective trial of risperidone in combination with lithium or divalproex sodium in pediatric mania. J Affect Disord. 2004 Oct;82(Suppl 1):S103–111. doi: 10.1016/j.jad.2004.05.017. [DOI] [PubMed] [Google Scholar]