Abstract
Background
The extent to which welfare states may influence health outcomes has not been explored. It was hypothesised that policies which target the poor are associated with greater income inequality in oral health quality of life than those that provide earnings-related benefits to all citizens.
Methods
Data were from nationally representative surveys in the UK (n=4064), Finland (n=5078), Germany (n=1454) and Australia (n=2292) conducted from 1998 to 2002. The typology of Korpi and Palme classifies these countries into four different welfare states. In each survey, subjects completed the Oral Health Impact Profile (OHIP-14) questionnaire, which evaluates the adverse consequence of dental conditions on quality of life. For each country, survey estimation commands were used to create linear regression models that estimated the slope of the gradient between four quartiles of income and OHIP-14 severity scores. Parameter estimates for income gradients were contrasted across countries using Wald χ2 tests specifying a critical p value of 0.008, equivalent to a Bonferroni correction of p<0.05 for the six pairwise tests.
Results
Statistically significant income gradients in OHIP-14 severity scores were found in all countries except Germany. A global test confirmed significant cross-national differences in the magnitude of income gradients. In Australia, where a flat rate of benefits targeted the poor, the mean OHIP-14 severity score reduced by 1.7 units (95% CI −2.15 to −1.34) with each increasing quartile of household income, a significantly steeper gradient than in other countries.
Conclusion
The coverage and generosity of welfare state benefits appear to influence levels of inequality in population oral health quality of life.
The welfare state has long held interest to social scientists for its effect on poverty.1,2 Recently it has gained epidemiological attention for its association with population health.3–7 To understand the public health consequences of the welfare state, Lundberg8 recommends comparing the coverage and generosity of specific programmes across welfare states. In the earliest typology to classify welfare states, Esping-Andersen9 proposed “three worlds of welfare capitalism” represented by the UK, Germany and Sweden as prototypic ideals. Despite acclaim for its seminal contribution, critics contested this typology on analytic10 or theoretical grounds,3,11–13 arguing, for example, that Australia was misclassified as a Liberal welfare state.14 In the debate that ensued, 11 alternative typologies emerged (for reviews see Arts and Gelissen15 and Bambra16).
Korpi and Palme17 addressed these critiques, defining welfare states according to the capacity of their social insurance programmes to alleviate income inequality and poverty—objectives that lie at the heart of the welfare state. They selected two programmes responsive to the certainty of ageing (old age pensions) and the risk of illness (sickness cash benefits), which provided protection from risk to all citizens irrespective of socioeconomic position. Korpi and Palme17 classified the programmes on the bases for eligibility for benefits (coverage) and the principle for setting benefit levels (generosity). This classification answered two questions: (i) are benefits targeted to low-income groups or are they universal? (ii) Are benefits offered at a flat rate equally to all citizens or are they earnings related?
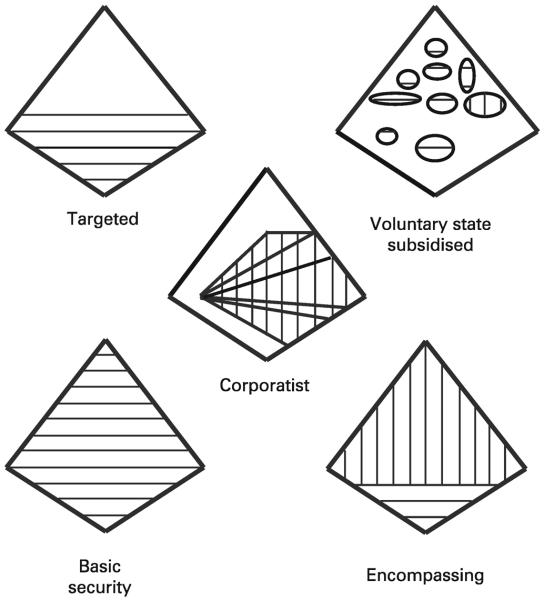
Their classification yielded five welfare states into which they fitted 18 Organization for Economic Co-operation and Development (OECD) countries (fig. 1). Using published data they evaluated the impact of these programmes on income inequality and poverty. Findings challenged the widely held assumption that inequality and poverty are alleviated with policies that target the poor and offer all citizens the same level of benefits. Korpi and Palme17 concluded, “The more we target benefits at the poor only and the more concerned we are with creating equality via equal public transfers to all, the less likely we are to reduce poverty and inequality.” (p 681).
Figure 1.
Ideal–typical models of social insurance institutions. Reprinted with permission from Korpi W, Palme J. The paradox of redistribution and strategies of equality: welfare state institutions, inequality, and poverty in the western countries. Am Sociol Rev 1998;63:661–87. The four-sided figures represent the social structure of society with high-income earners at the top and low-income earners at the bottom. White areas represent the non-covered population. Horizontal lines indicate flat-rate benefits. Vertical lines indicate earnings-related benefits. Ellipses in the voluntary state-subsidised model indicate separate insurance programmes. Angled lines in the corporatist model indicate insurance programmes organised separately for different occupational categories. Targeted welfare state: has a means-tested scheme of flat-rate benefits financed through taxation of the economically active. Benefits are minimal and coverage limited to low income earners. Australia was the only country that fitted this typology. Basic Security welfare state: Benefits are modest but coverage is universal. Like the Targeted state, depends on middle and high income earners seeking supplementary insurance through private providers. Countries were the UK, Canada, Denmark, Netherlands, Ireland, New Zealand, Switzerland and the United States. Corporatist welfare state: Eligibility for benefits is based on compulsory membership in specified occupational categories and benefits are earnings-related (as opposed to flat-rate). This produces a much bigger budget allowing substantially greater expenditure on benefits than do the Targeted or Basic Security regimes. The more generous provision upholds the accustomed higher standards of living of middle income earners, acting as disincentive to seek private insurance arrangements. Countries were Germany, Austria, Belgium, France, Italy and Japan. Encompassing welfare state: Earnings-related benefits for all citizens that tend to be generous. This suppresses demand for private insurance from the middle and high income earning segments of the population. Countries were Finland, Norway and Sweden. Voluntary State Subsidised welfare state: No country was fitted.
Just as low income is associated with greater disease prevalence, so socioeconomic inequality in oral health quality of life across the life course18–21 is not explained by risk behaviour.22 Hence the primary objective of this study was to determine whether the magnitude of income inequalities in oral health varied among different welfare states. A secondary objective was to investigate whether any differences were in accordance with this typology. We hypothesised that income inequalities in oral health quality of life would be greatest in Australia where policies target the poor rather than all citizens. Furthermore we hypothesised that income inequalities would be least pronounced in Germany where benefits are offered to all citizens at levels commensurate with earnings.
MATERIALS AND METHODS
Study design and study population
Germany, Finland, the UK and Australia represented the Corporatist, Encompassing, Basic Security and Targeted welfare states respectively. We used cross-sectional survey data for representative samples of adults in these countries independently surveyed over a five year period in the UK (Adult Dental Health Survey, 1998), Finland (Health 2000 Health Examination Survey, 2000), Germany (2001) and Australia (National Dental Telephone Interview Survey, 2002). Sampling and data collection are described in detail elsewhere.23–26 In brief, sampling followed a multistage stratified random design, where households were sampled at random from within primary sampling units and one occupant was sampled at random to participate in the survey. In the UK, enhanced samples of residents were drawn in Scotland, Wales and Northern Ireland to allow comparison between England and the other three home countries.
Data collection
Face-to-face interviews were conducted in Germany and the UK. Finnish subjects completed an interview and a self-administered questionnaire and Australians completed a telephone interview and a self-administered questionnaire. All surveys included the Oral Health Impact Profile (OHIP-14) questionnaire.27,28 OHIP is the most extensively studied measure of oral health quality of life adapted for oral health29 from the WHO International Classification of Impairments, Disabilities and Handicaps.30 The questionnaire has been validated empirically28,31 and translated into over 20 languages. OHIP items evaluate the adverse consequences of oral diseases and conditions on well-being. Responses are made on an ordinal scale coded 0=never, 1=hardly ever, 2=occasionally, 3=fairly often, 4=very often. The English language short-form OHIP-14 was administered in the UK and Australia,28 Finns completed a Finnish translation of this questionnaire and Germans completed the German language 49-item OHIP (OHIP-G).32 OHIP-G contains the OHIP-14 subset of items and analysis was limited to this subset. In the UK and Australia subjects were asked how often they had the impact in the past year. In Germany and Finland the reference interval was the past month. Participation was in 60.0% in Germany (N=2026), 74.6% in Finland (N=5987), 74.0% in the UK (N=6764). The questionnaire mailed to Australians yielded a response rate of 65.5% (N=3131).
Dependent variable
The OHIP-14 severity score was the sum of ordinal responses across 14 items yielding a potential range from 0 to 56. Higher scores denote greater adverse impact of oral conditions on well-being, that is worse oral health quality of life. Subjects missing more than two OHIP-14 values were eliminated from analysis. Otherwise the mean item score was imputed for missing values. The proportion of subjects with complete OHIP-14 data was 96.8%, 87.1%, 99.8% and 94.5% in Germany, Finland, UK and Australia, respectively, and missing values were imputed for 0.1%, 4.3%, 0.0% and 1.8% of subjects in these countries respectively.
Exposure of interest
Household income was the exposure of interest. In Germany, total net income after deductions was self-reported from nine categories that ranged from <1000 to 8000+ German Marks. Total gross monthly income in Finland was obtained from tax authorities and ranged from zero to over 2 million Finnish Marks. In the UK, household income before deductions was derived from self-reported response to several questions. Values ranged from zero to 5288 summarising income from all sources. Australians self-reported total annual household income from nine categories ranging from <$A12,000 to $A80,000+. Income data were missing for 13.6% of subjects in Germany, 11.6% in the UK, 5.3% in Germany, and in Finland there was no missing income data. We computed quartiles of household income to enable cross-national comparison on a relative scale. This distribution-based measure of income was adopted so that gradients would reflect the direction and magnitude of difference in OHIP-14 scores associated with people's relative socioeconomic position within their country.
Covariates
Sex and age in years were selected as covariates based on prior evidence of association of these factors with oral conditions including OHIP scores.
Data analysis
To maximise cross-national comparability, analysis was restricted to dentate subjects aged 30 years or older. Initial analyses assessed the crude associations of household income, sex and age group with OHIP-14 severity scores separately for each country. Data were analysed in STATA 10.1 using survey estimation commands to adjust for the complex survey designs.33 For each country, survey estimation commands were used to create linear regression models that estimated the slope of the gradient between four quartiles of income and OHIP-14 severity scores. Because of heteroscedasticity in the regression model, we generated bootstrap estimates of standard errors for the parameters in the model using the normal (t test) method with 1000 bootstrap samples for each country. Although under central limits theorem large samples such as these are robust to violations of assumptions,34,35 other health quality-of-life research has advocated bootstrapping where ordinal scales induce heteroscedasticity.36 Parameter estimates for income gradients in OHIP-14 severity scores were contrasted across countries using Wald χ2 tests and we specified a critical p value of 0.008, equivalent to a Bonferroni correction of p<0.05 for the six pair-wise tests.
In linear regression ordinal income quartiles were modelled as a grouped linear variable to test for trend, with adjustment for covariates. Results are interpreted as the average change in OHIP-14 severity score for every one quartile increase in household income. We tested the global null hypothesis that the magnitude of income inequalities in OHIP-14 scores did not differ between countries. Where cross-national differences were found we performed post hoc contrasts to identify where differences were found using the CATMOD procedure in SAS Version 10.0 for adjacent-categories logit models.37
Ethical approval
Ethical approval in the UK was obtained from the relevant multicentre and local National Health Service (NHS) research ethics committees and for each of the other surveys was obtained from the appropriate institutional review boards in each country.
RESULTS
The final sample comprised 1454 subjects in Germany, 5078 in Finland, 4064 in the UK and 2292 in Australia (table 1).
Table 1.
Characteristics of dentate study subjects aged 30 years and older in Germany (2001), Finland (2000), UK (1998) and Australia (2002)
| Germany | Finland | UK | Australia | |
|---|---|---|---|---|
| Study subjects (n) | 1454 | 5078 | 4064 | 2292 |
| Male (%) | 48.8 | 48.2 | 49.6 | 50.3 |
| Age group (%) | ||||
| 30–44 years | 38.0 | 39.9 | 44.4 | 43.0 |
| 45–59 years | 34.0 | 38.8 | 32.4 | 33.4 |
| 60+ years | 28.0 | 21.4 | 23.2 | 23.6 |
| Household income (%) | ||||
| Quartile 1 (low) | 26.9 | 24.3 | 25.4 | 30.4 |
| Quartile 2 | 25.6 | 25.1 | 25.4 | 23.9 |
| Quartile 3 | 29.1 | 25.3 | 23.3 | 18.3 |
| Quartile 4 (high) | 18.4 | 25.3 | 25.8 | 27.5 |
In unadjusted analysis, mean (95% CI) OHIP-14 severity scores (table 2) were lowest in Finland on average (3.5, 3.3 to 3.7), followed by Germany (4.5, 3.7 to 5.3) and the UK (4.9, 4.7 to 5.1) and were highest in Australia (7.0, 6.6 to 7.5).
Table 2.
Mean (95% CI) Oral Health Impact Profile (OHIP-14) severity scores for study subjects in Germany (2001), Finland (2000), UK (1998) and Australia (2002)
| Germany (n = 1454) |
Finland (n = 5078) |
UK (n = 4064) |
Australia (n = 2,292) |
|||||
|---|---|---|---|---|---|---|---|---|
| Mean (95% CI) | p Value | Mean (95% CI) | p Value | Mean (95% CI) | p Value | Mean (95% CI) | p Value | |
| Total | 4.5 (3.7 to 5.3) | 3.5 (3.3 to 3.7) | 4.9 (4.7 to 5.1) | 7.0 (6.6, 7.5) | ||||
| Sex | 0.081 | 0.003 | 0.003 | 0.281 | ||||
| Female | 4.2 (3.4 to 4.9) | 3.3 (3.0 to 3.5) | 5.3 (4.9 to 5.6) | 7.3 (6.6 to 7.9) | ||||
| Male | 4.9 (3.9 to 5.9) | 3.8 (3.5 to 4.1) | 4.6 (4.3 to 4.9) | 6.8 (6.1 to 7.4) | ||||
| Age group | 0.059 | <0.001 | <0.001 | 0.455 | ||||
| 30–44 years | 3.8 (2.8 to 4.8) | 2.8 (2.5 to 3.1) | 5.0 (4.7 to 5.4) | 7.1 (6.3 to 7.9) | ||||
| 45–59 years | 4.9 (3.8 to 5.9) | 3.7 (3.4 to 4.0) | 5.6 (5.1 to 6.0) | 7.3 (6.5 to 8.0) | ||||
| 60+ years | 5.0 (4.0 to 6.0) | 4.5 (4.1 to 5.0) | 3.8 (3.3 to 4.2) | 6.6 (5.9 to 7.3) | ||||
| Household income | 0.197 | <0.001 | 0.029 | <0.001 | ||||
| Quartile 1 (low) | 4.9 (4.0 to 5.9) | 5.0 (4.5 to 5.4) | 5.7 (5.2 to 6.3) | 8.6 (7.8 to 9.3) | ||||
| Quartile 2 | 5.0 (3.7 to 6.2) | 3.7 (3.3 to 4.1) | 5.0 (4.6 to 5.5) | 7.9 (6.8 to 9.0) | ||||
| Quartile 3 | 3.9 (3.0 to 4.7) | 3.0 (2.7 to 3.4) | 4.7 (4.3 to 5.2) | 6.6 (5.5 to 7.7) | ||||
| Quartile 4 (high) | 5.1 (2.7 to 7.5) | 2.4 (2.1 to 2.7) | 4.7 (4.3 to 5.1) | 5.0 (4.2 to 5.8) | ||||
The OHIP-14 severity score is calculated as the sum of ordinal responses (coded 0–4) across the 14 OHIP-14 items. Higher scores denote greater adverse impact of oral conditions on well-being, ie, worse oral health quality of life.
Bivariate association of income and OHIP-14 score in each country
Significant unadjusted income gradients in OHIP-14 severity scores were found in each country except Germany. Despite having the lowest absolute severity scores, Finland had the largest relative inequalities in OHIP-14 severity scores with a twofold difference on average between low and high household income quartiles.
Construction of separate linear regression models for each country revealed that significant effects of household income on OHIP-14 severity scores persisted after adjustment for sex and age in Finland, the UK and Australia. Two points warrant attention in the covariate adjusted association of income gradients in oral health quality of life. The first is that in Australia, for example, the OHIP severity score reduced by 1.7 with each increasing quartile of household income. Graphically (fig 2) this shows as a steep gradient such that adults in the lowest income quartile have substantially worse OHIP-14 severity scores than the other three countries. The second point is that among adults in the highest income quartile Germans had elevated OHIP-14 scores relative to the other countries.
Figure 2.
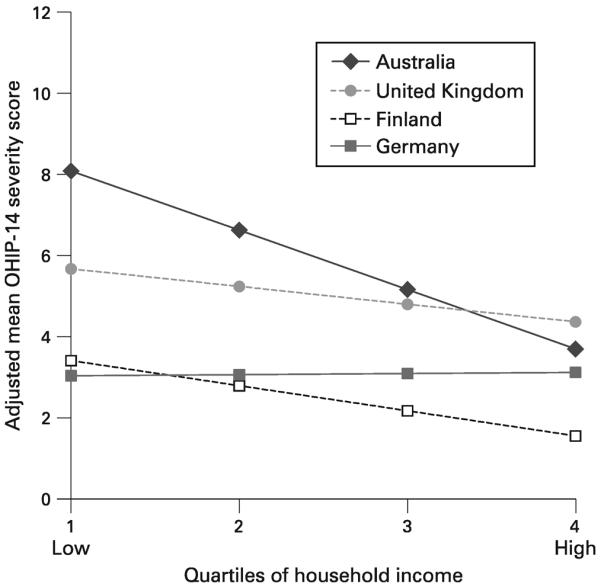
Household income gradients in adjusted mean Oral Health Impact Profile (OHIP-14) severity scores per person for dentate adults in Germany (2001), Finland (2000), the UK (1998) and Australia (2002). Adjustment for sex and age in years was achieved using separate linear regression models for each country.
The SAS CATMOD procedure, which compared all four countries in one analysis, showed an overall significant difference in the β coefficients representing the income gradient in OHIP-14 severity scores between the four countries (p = 0.0001, Wald χ2) after adjustment for covariates (results not tabulated). Post hoc comparisons (table 3) indicated that the magnitude of income inequalities in OHIP-14 severity scores was significantly greater in all countries than in Germany and significantly higher in Australia than in Germany, Finland and the UK
Table 3.
Comparison of the magnitude of income inequalities in Oral Health Impact Profile (OHIP-14) severity scores with Bonferroni correction for multiple tests
| Contrast | χ 2 | p Value |
|---|---|---|
| Germany vs Finland | 8.76 | 0.003 |
| Germany vs UK | 3.35 | 0.067 |
| Germany vs Australia | 27.41 | <0.001 |
| Finland vs UK | 2.63 | 0.105 |
| Finland vs Australia | 15.16 | <0.001 |
| UK vs Australia | 21.46 | <0.001 |
DISCUSSION
Statement of principal findings
Significant variation in the magnitude of income inequalities in oral health quality of life was found under different welfare state regimes. These differences were in accordance with the Korpi and Palme typology. Where coverage of programmes was universal and earnings related, as in Germany, income inequalities in outcomes were absent. Here the poorest quartile was relatively better off than their Australian counterparts while the wealthiest quartile fared comparatively worse than those in Australia, Finland and the UK. Consistent with the typology, where coverage was a minimal flat-rate, as in Australia, income inequalities were greatest. It is possible that coverage and generosity of social programmes are important to public health because they underlie policy decisions that redistribute resources, and hence risk, through taxes, transfers and spending.
Income gradients that were statistically significant were also substantive: for example, in Australia, the reduction of 1.7 units of the OHIP-14 score for each increase in income quartile was equivalent to a difference in OHIP score of 7.0 units between the lowest and the highest quartiles. By way of comparison, a clinical study of general dental treatment among older dental patients in Australia documented a reduction of 6.2 units of the OHIP score 6 months after completion of treatment.38 In a similar study of Canadians, there was a 4.3 unit reduction in OHIP-14 scores after treatment, and the authors concluded that the minimal important difference for the OHIP-14 was of 5-scale points.39 Other observational studies have reported higher OHIP scores among people with relatively greater levels of dental morbidity (eg tooth loss, dental decay and periodontal disease) and among groups with limited access to dental care.40 Numerous population studies have found the OHIP to have good reliability and validity as a measure of adverse functional and psychosocial impacts arising from oral disorders.41
Strengths and weaknesses of the study
Our findings supported the study hypotheses and are noteworthy for four reasons. First, despite recognition that healthcare has little impact on social gradient in health,42 few studies have investigated macrolevel determinants upstream from health care. Second, to our knowledge this is the only study to explicitly apply the Korpi and Palme typology17 to public health outcomes. Third, our empirical findings are based on nationally representative data using the same outcome measure in each country. Finally, this study sheds light on possible ways that social inequalities in health are produced and how they might be managed. Although our findings are limited to oral health quality of life, there is no reason to believe that they are not widely generalisable to other health outcomes.
Our decision not to adjust for smoking, tooth loss and denture wearing status was intentional. Since these are intermediate on the causal pathway between income and oral health quality of life, their statistical adjustment can result in bias.43
Since different reference periods were used in answering the OHIP-14 questionnaire, estimates may under-enumerate severity scores in Germany and Finland. Certainly there was a trend to lower estimates with a shorter reference period. Consequently we compared relative differences between income categories, paying less heed to absolute differences. This was a conservative approach, since previous testing of differing reference intervals on OHIP scores failed to find a significant effect.44
In principle, it would be informative to use clinical measures themselves as additional outcome measures to address our study aims. However, oral health surveys notoriously vary in the methods of measuring clinical parameters. For example, in the datasets used here, there was inconsistency among countries in recording even basic measures such as tooth loss. This highlights one benefit of including a standardised and validated subject-reported measure, such as the OHIP, in such surveys. Finally we focused only on income differences, choosing not to examine alternative socioeconomic indicators.
Implications for policy
The welfare state in Australia remains targeted today. Minimal benefits are redistributed by the state to a means-tested eligible minority that is typically economically inactive, by taxing the income of the economically active majority. Eligible adults are entitled to utilise publicly subsidised dental care, but this care is rationed through limited facilities and a shortage of dentists.45 Indeed, recipients face greater odds of tooth extraction than their more affluent private sector counterparts.46
Unlike Australia, which targets those at the margins, Germany, Finland and the UK are inclusive in their social assistance. Our finding of no social gradient in oral health quality of life in Germany is consistent with previous cross-national research comparing educational health inequalities among 78 000 adults in 23 European countries, where the smallest health inequalities were found in corporatist countries.47 In other research, an inverse social gradient was found in serum IgG and IgA among children in Germany.48 It is reasonable to speculate that the redistributive effect of social programmes ameliorates income-related differences in public health outcomes.
At the time of the data collection, the system in the UK for dental care was of universal benefits for most of the population, with all but those on the lowest income contributing to the cost of care. Two points are of note though. The first is that the rates paid were capped by the system and generally much lower than would be available in private care. Nevertheless, the vast majority of the population at the time were under the care of the National Health Service for their dentistry. The second point is that this system actually differs from the rest of health care, which was universal and free to all at the point of delivery.
Finland, like the UK, offers benefits to all citizens, not only those with the lowest income. While Finland attempts to pay benefits that replace lost income, the UK pays a flat, modest rate to all citizens.
This study drew on a typology purposefully designed to highlight differential effects of social policy on poverty and income inequality. We can conclude that income gradients in health differed between countries belonging to different welfare states. These findings build on mounting cross-national evidence that welfare states do play an influential role in public health outcomes.
What is already known on this subject
-
▶
Macrolevel characteristics that arise in the policy arena are, by definition, amenable to policy intervention.
-
▶
The welfare state has long been of interest to economists, sociologists and political scientists for its effect on poverty and inequality, yet is effect on public health is less well understood.
What this study adds
-
▶
This study compared four affluent countries under different welfare state regimes.
-
▶
Where eligibility for benefits was limited and the level of benefits set at a flat rate, income differences in oral health were large.
-
▶
Conversely, where coverage was universal and earnings related, we found no evidence of income inequalities in oral health.
Acknowledgments
Funding: This study was supported by NIH/NIDCR R21-DE018980. The Health 2000 Health Examination Survey in Finland was organised by the National Public Health Institute (KTL) of Finland (http://www.ktl.fi/health2000), and partly supported by the Finnish Dental Society Apollonia and the Finnish Dental Association. The National Dental Telephone Interview Survey 2002 was supported by the Australian Government Department of Health and Ageing, Population Health Division. AES is an Australian National Health and Medical Research Council Sidney Sax (Public Health) Fellow.
Footnotes
Competing interests: None.
Ethics approval: Institutional Review Board consisting of members of the German Dental Association, Association of German Chambers of Dentists and Federal Association of Statutory Health Insurance Dentists.
REFERENCES
- 1.Brady D. The welfare state and relative poverty in rich western democracies, 1967–1997. S Soc Forces. 2005;83:1329–64. [Google Scholar]
- 2.Moller S, Bradley D, Huber E, et al. Determinants of relative poverty in advanced capitalist democracies. Am Sociol Rev. 2003;68:22–51. [Google Scholar]
- 3.Bambra C, Pope DP, Swami V, et al. Gender, health inequalities and welfare state regimes: a cross-national study of thirteen European countries. J Epidemiol Community Health. 2009;63:38–44. doi: 10.1136/jech.2007.070292. [DOI] [PubMed] [Google Scholar]
- 4.Navarro V, Muntaner C, Borrell C, et al. Politics and health outcomes. Lancet. 2006;368:1033–7. doi: 10.1016/S0140-6736(06)69341-0. [DOI] [PubMed] [Google Scholar]
- 5.Chung H, Muntaner C. Welfare state matters: a typological multilevel analysis of wealthy countries. Health Policy. 2007;80:328–39. doi: 10.1016/j.healthpol.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 6.Navarro V, Shi L. The political context of social inequalities and health. Soc Sci Med. 2001;52:481–91. doi: 10.1016/s0277-9536(00)00197-0. [DOI] [PubMed] [Google Scholar]
- 7.Coburn D. Beyond the income inequality hypothesis: class, neo-liberalism, and health inequalities. Soc Sci Med. 2004;58:41–56. doi: 10.1016/s0277-9536(03)00159-x. [DOI] [PubMed] [Google Scholar]
- 8.Lundberg O. Commentary: Politics and public health—some conceptual considerations concerning welfare state characteristics and public health outcomes. Int J Epidemiol. 2008;37:1105–8. doi: 10.1093/ije/dyn078. [DOI] [PubMed] [Google Scholar]
- 9.Esping-Andersen G. The three worlds of welfare capitalism. Polity Press; London: 1990. [Google Scholar]
- 10.Kangas O. The politics of social security: on regressions, qualitative comparisons and cluster analysis. In: Janoski T, Hicks A, editors. The comparative political economy of the welfare state. Cambridge University Press; Cambridge: 1994. pp. 346–65. [Google Scholar]
- 11.Kautto M. Investing in services in West European welfare states. J Eur Soc Policy. 2002;12:53–65. [Google Scholar]
- 12.Bambra C. Cash versus services: “worlds of welfare” and the decommodification of cash benefits and welfare services. J Soc Policy. 2005;42:1–19. [Google Scholar]
- 13.Bonoli J. Classifying welfare states: a two-dimension approach. J Soc Policy. 1997;26:351–372. [Google Scholar]
- 14.Castles FG, Mitchell D. Worlds of welfare and families of nations. In: Castles FG, editor. Families of nations: patterns of public policy in Western Democracies. Dartmouth Publishing Company; Aldershot: 1993. [Google Scholar]
- 15.Arts WA, Gelissen J. Three worlds of welfare capitalism or more? A state-of-the-art report. J Eur Soc Policy. 2002;12:137–58. [Google Scholar]
- 16.Bambra C. Going beyond The three worlds of welfare capitalism: regime theory and public health research. J Epidemiol Community Health. 2007;61:1098–102. doi: 10.1136/jech.2007.064295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Korpi W, Palme J. The paradox of redistribution and strategies of equality: welfare state institutions, inequality, and poverty in the western countries. Am Sociol Rev. 1998;63:661–87. [Google Scholar]
- 18.Locker D. Disparities in oral health-related quality of life in a population of Canadian children. Community Dent Oral Epidemiol. 2007;35:348–56. doi: 10.1111/j.1600-0528.2006.00323.x. [DOI] [PubMed] [Google Scholar]
- 19.Lawrence HP, Thomson WM, Broadbent JM, et al. Oral health-related quality of life in a birth cohort of 32-year olds. Community Dent Oral Epidemiol. 2008;36:305–16. doi: 10.1111/j.1600-0528.2007.00395.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turrell G, Sanders AE, Slade GD, et al. The independent contribution of neighborhood disadvantage and individual-level socioeconomic position to self-reported oral health: a multilevel analysis. Community Dent Oral Epidemiol. 2007;35:195–206. doi: 10.1111/j.1600-0528.2006.00311.x. [DOI] [PubMed] [Google Scholar]
- 21.Makhija SK, Gilbert GH, Boykin MJ, et al. The relationship between sociodemographic factors and oral health-related quality of life in dentate and edentulous community-dwelling older adults. J Am Geriatr Soc. 2006;54:1701–12. doi: 10.1111/j.1532-5415.2006.00923.x. [DOI] [PubMed] [Google Scholar]
- 22.Sanders AE, Spencer AJ, Slade GD. Evaluating the role of dental behaviour in oral health inequalities. Community Dent Oral Epidemiol. 2006;34:1–9. doi: 10.1111/j.1600-0528.2006.00261.x. [DOI] [PubMed] [Google Scholar]
- 23.John MT, LeResche L, Koepsell TD, et al. Oral health-related quality of life in Germany. Eur J Oral Sci. 2003;111:483–91. doi: 10.1111/j.0909-8836.2003.00079.x. [DOI] [PubMed] [Google Scholar]
- 24.Aromaa A, Koskinen S, editors. Baseline results of the Health 2000 Health Examination Survey. Publications of National Public Health Institute, KTL B12/2004; Hakapaino; Helsinki: 2004. Health and functional capacity in Finland; pp. 11–23. [Google Scholar]
- 25.Steele J, Sanders AE, Slade GD, et al. How do age and tooth loss affect oral health impacts and quality of life? A study comparing two national samples. Community Dent Oral Epidemiol. 2003;32:107–14. doi: 10.1111/j.0301-5661.2004.00131.x. [DOI] [PubMed] [Google Scholar]
- 26.Carter KD, Stewart JF. National Dental Telephone Interview Survey 2002. AIHW Dental Statistics and Research Unit; Adelaide: 2003. AIHW cat. No. DEN 128. [Google Scholar]
- 27.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 28.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–90. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 29.Locker D. Measuring oral health: a conceptual framework. Community Dent Health. 1988;5:3–18. [PubMed] [Google Scholar]
- 30.World Health Organization . International classification of impairments disabilities and handicaps: a manual of classification. World Health Organization; Geneva: 1980. pp. 23–42. [Google Scholar]
- 31.Nuttall NM, Slade GD, Sanders AE, et al. An empirically derived population-response model of the short form of the Oral Health Impact Profile. Community Dent Oral Epidemiol. 2006;34:18–24. doi: 10.1111/j.1600-0528.2006.00262.x. [DOI] [PubMed] [Google Scholar]
- 32.John MT, Patrick DL, Slade GD. The German version of the Oral Health Impact Profile—translation and psychometric properties. Eur J Oral Sci. 2002;110:425–33. doi: 10.1034/j.1600-0722.2002.21363.x. [DOI] [PubMed] [Google Scholar]
- 33.StataCorp . Stata Statistical Software: Release 10. StataCorp LP; College Station, TX: 2007. [Google Scholar]
- 34.Lumley T, Diehr P, Emerson S, et al. The importance of the normality assumption in large public health data sets. Annu Rev Public Health. 2002;23:151–69. doi: 10.1146/annurev.publhealth.23.100901.140546. [DOI] [PubMed] [Google Scholar]
- 35.Cohen ME. Analysis of ordinal dental data: evaluation of conflicting recommendations. J Dent Res. 2001;80:309–13. doi: 10.1177/00220345010800010301. [DOI] [PubMed] [Google Scholar]
- 36.Walters SJ, Campbell MJ. The use of bootstrap methods for analysing Health-Related Quality of Life outcomes (particularly the SF-36) Health Qual Life Outcomes. 2004;2:70. doi: 10.1186/1477-7525-2-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.SAS: SAS/STAT Software, Release 10.0. SAS Institute, Inc.; Cary, NC: 2000. [Google Scholar]
- 38.Gagliardi DI, Slade GD, Sanders AE. Impact of dental care on oral health-related quality of life and treatment goals among elderly adults. Aust Dent J. 2008;53:26–33. doi: 10.1111/j.1834-7819.2007.00005.x. [DOI] [PubMed] [Google Scholar]
- 39.Locker D, Jokovic A, Clarke M. Assessing the responsiveness of measures of oral health-related quality of life. Community Dent Oral Epidemiol. 2004;32:10–8. doi: 10.1111/j.1600-0528.2004.00114.x. [DOI] [PubMed] [Google Scholar]
- 40.Slade GD. Assessment of Oral Health Related Quality of Life. In: Inglehart MR, Bagramian RA, editors. Oral health related quality of life. Quintessence Publishing Co.; Carl Stream: 2002. pp. 29–46. [Google Scholar]
- 41.Locker D, Allen F. What do measures of `oral health-related quality of life' measure? Community Dent Oral Epidemiol. 2007;35:401–11. doi: 10.1111/j.1600-0528.2007.00418.x. [DOI] [PubMed] [Google Scholar]
- 42.Evans RG, Stoddart GL. Producing health, consuming health care. Soc Sci Med. 1990;31:1347–63. doi: 10.1016/0277-9536(90)90074-3. [DOI] [PubMed] [Google Scholar]
- 43.Weinberg CR. Toward a clearer definition of confounding. Am J Epidemiol. 1993;137:1–8. doi: 10.1093/oxfordjournals.aje.a116591. [DOI] [PubMed] [Google Scholar]
- 44.Sutinen S, Lahti S, Nuttall NM, et al. Effect of a 1-month vs. a 12-month reference period on responses to the 14-item Oral Health Impact Profile. Eur J Oral Sci. 2007;115:246–9. doi: 10.1111/j.1600-0722.2007.00442.x. [DOI] [PubMed] [Google Scholar]
- 45.Marshall RI, Spencer AJ. Accessing oral health care in Australia. Med J Aust. 2006;185:59–60. doi: 10.5694/j.1326-5377.2006.tb00470.x. [DOI] [PubMed] [Google Scholar]
- 46.Brennan DS, Luzzi L, Roberts-Thomson KF. Dental service patterns among private and public adult patients in Australia. BMC Health Serv Res. 2008;3:1. doi: 10.1186/1472-6963-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Eikemo TA, Huisman M, Bambra C, et al. Health inequalities according to educational level in different welfare regimes: a comparison of 23 European countries. Sociol Health Illn. 2008;30:565–82. doi: 10.1111/j.1467-9566.2007.01073.x. [DOI] [PubMed] [Google Scholar]
- 48.Bolte G, Mielck A, Meyer I, et al. Inverse social gradient of secondary immune response parameters in children. Rev Environ Health. 1999;14:135–43. doi: 10.1515/reveh.1999.14.3.135. [DOI] [PubMed] [Google Scholar]