In PNAS, Chen et al. (1) present findings that implicate long-term exposure to air pollution as contributing to enormous loss of life expectancy (LE) in China. These results are based on a clever quasiexperimental, regression discontinuity design exploiting a Chinese policy that provided free coal for heating in cities north of the Huai River, but not in the south. A spatial discontinuity for particulate matter air pollution (PM), presumably from coal combustion, was observed. A spatial discontinuity of reduced LE of 5+ y was also observed. If true, these results suggest enormous health costs associated with air pollution in China and have important environmental, economic, and public health policy implications. However, are the results plausible? Are they coherent with other epidemiological studies?
Evidence Base for PM and Mortality
Early evidence that short-term elevations in ambient PM contribute to mortality came from well-documented extreme air pollution episodes in the 1930s to 1950s (2). More recently, numerous daily time-series and case-crossover studies have observed small but statistically robust associations between daily mortality and short-term elevations in PM (3). Population-based cross-sectional studies of long-term exposure to PM (mostly from the 1970s and 1980s) observed mortality rates associated with PM air pollution (4), but were largely discounted because they were unable to control for cigarette smoking or other individual risk factors.
In the mid-1990s, survival analyses of two United States prospective cohort studies were reported. Statistically robust associations between mortality risk and fine PM were observed even controlling for smoking and other individual risk factors. These two prospective cohort studies have undergone extensive reanalysis, replication, and extended analysis (5–7). Additional cohort studies have also been reported, and when evaluated in a meta-analytic review framework there is significant evidence that fine PM exposure contributes to risk of mortality (8–10).
Further evidence regarding mortality effects of long-term PM exposure comes from quasiexperimental studies. Between 1980 and 2000, partially as a result of public policy efforts to control air pollution, there were significant improvements in air quality in the United States, especially in the areas that were initially most polluted. Differential reductions in air pollution during this two-decade period provided the basis for a nationwide, natural experiment (11). A first-difference regression analysis of United States county-level changes in air pollution and life expectancies, controlling for changes in socioeconomic, demographic, and smoking variables, indicated that reductions in fine PM were associated with significant improvements in LE (11). Similar results were observed in an analysis of more counties for the shorter time period of 2000–2007 (12).
This Chinese study reported in PNAS (1) provides one of the most dramatic and interesting quasiexperimental studies reported. The remarkable Chinese policy that produced this natural experiment and the adept use of a well-developed regression discontinuity approach has resulted in a unique and important contribution.
Comparison of Estimates Across Studies
Table 1 presents comparisons of extrapolated PM-mortality effect estimates for representative studies of long-term PM exposure. The Chinese study (1) is problematic because it uses TSP (total suspended particles) as its measure of PM. There is ample evidence that the most harmful constituents of PM pollution are in the fine fraction of PM (particles with an aerodynamic diameter < 2.5 µm, PM2.5). The prospective cohort studies typically found the most robust mortality associations with PM2.5. The correct equivalency conversion to compare the Chinese study with studies based on PM2.5 is unknown, but United States data from 1979 to 1983 (6) indicate that ∼30% of TSP was PM2.5. In Table 1, a 100 µg/m3 difference in TSP is compared with a 30 µg/m3 difference in PM2.5. Concentrations of 30 µg/m3 PM2.5 approximately equal average concentrations in the most polluted United States cities in the late 1970s and are greater than current concentrations, even in the most polluted United States cities (6, 11, 12). Long-term exposures of 30 µg/m3 of PM2.5 or more are common in population centers of China, India, and other developing countries.
Table 1.
Comparison of PM-mortality effect estimates from key representative studies
| Comparable studies | Difference in exposure | Elevated risk (%) | Difference in LE (y) |
| Harvard Six-Cities Cohort study (5) | 30 µg/m3 PM2.5 | 56 | 5.4* |
| ACS CPS-II Cohort study (6) | 30 µg/m3 PM2.5 | 20 | 2.2* |
| Medicare Cohort study (8) | 30 µg/m3 PM2.5 | 12 | 1.3* |
| Canadian Cohort study (9) | 30 µg/m3 PM2.5 | 33 | 3.4* |
| Metaestimate of Cohort studies (10) | 30 µg/m3 PM2.5 | 20 | 2.2* |
| First difference analysis of United States county-level changes in life expectancy 1980–2000 (11) | 30 µg/m3 PM2.5 | — | 1.8 |
| First difference analysis of United States county-level changes in life expectancy 2000–2007 (12) | 30 µg/m3 PM2.5 | — | 1.1 |
| China quasiexperimental, regression discontinuity study, North vs. South of Huai River (1) | 100 µg/m3 TSP or approximately 30 µg/m3 PM2.5 | 14 | 3.0 |
| Active smoking (5, 6). | Active smoker vs. never smoker | 100 | 7.8* |
Derived from life-table analysis using estimated change in mortality risk from birth for air pollution and from age 18 for smoking.
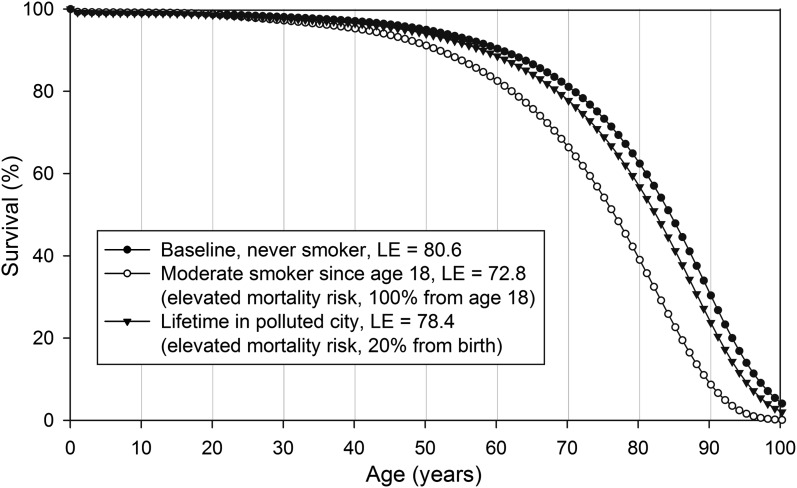
Prospective cohort studies provide estimates of elevated mortality risk from PM, but not direct estimates of LE. Estimates of survival curves and LE are derived using standard life-table techniques and death rates from the 2008 life tables for the total population of the United States (13). The counterfactual baseline LE for nonsmokers is calculated adjusting mortality rates for ages 18 y and older to be 80% of rates from the total population. Life table-derived LE estimates are derived by adjusting for excess risks estimated from the cohort studies, including active smoking for comparison purposes (Fig. 1). As observed in Table 1, PM-mortality estimates, including the Chinese study (1), are roughly comparable.
Fig. 1.
Survival curves for alternative risk assumptions.
Biological Plausibility
The Chinese study (1) finds PM associations with cardiovascular and respiratory disease mortality but not with other causes of death, which is also generally consistent with the overall literature. Biological plausibility is enhanced by observations in the literature of a coherent cascade of respiratory and cardiovascular health effects (14). Pathophysiological pathways linking exposure to cardiorespiratory mortality risk are not fully understood, but it is becoming clear that there are multiple mechanistic pathways that are complex and interdependent. Evidence suggests that pathophysiological pathways that link PM exposure to cardiorespiratory disease include pollution-induced pulmonary and systemic oxidative stress and inflammation, enhanced initiation and progression of vascular dysfunction and atherosclerosis, altered cardiac autonomic function, and translocation of particle constituents (14).
An argument against plausibility concerns the effects of ambient PM pollution compared with cigarette smoking, especially considering the vastly larger dose that comes from active smoking. A comparison of the effects of air pollution and active cigarette smoking is reported in Table 1, and the relative size of the effect of air pollution is disconcertingly large when considering that breathing ambient pollution is ubiquitous and involuntary. However, recent research that evaluated the exposure–response relationship across exposures associated with air pollution, second-hand smoke, and active smoking indicates largest incremental effects at low levels of exposure, including exposure to second-hand smoke and air pollution. Long-term, relatively low-level exposure may be sufficient to induce adverse biological processes and increase the risk of cardiovascular disease mortality (15).
Conclusion
With regard to the health effects of air pollution there remains much to be learned. A large literature provides evidence that breathing combustion-related fine PM, even at exposure levels common to populations throughout the world, contributes to cardiorespiratory disease mortality and diminished LE. There is also encouraging evidence that improving air quality contributes to improvements in human health and LE (5, 11, 12). The results reported by Chen et al. (1) in PNAS make an important contribution to this evidence base that is growing hard to ignore, and begs to be better understood.
Footnotes
The authors declare no conflict of interest.
See companion article on page 12936.
References
- 1.Chen Y, Ebenstein A, Greenstone M, Hongbin L. Evidence on the impact of sustained exposure to air pollution on life expectancy from China’s Huai River policy. Proc Natl Acad Sci USA. 2013;110:12936–12941. doi: 10.1073/pnas.1300018110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Logan WPD. Mortality in the London fog incident, 1952. Lancet. 1953;264(Feb. 14):336–338. doi: 10.1016/s0140-6736(53)91012-5. [DOI] [PubMed] [Google Scholar]
- 3.Bell ML, Samet JM, Dominici F. Time-series studies of particulate matter. Annu Rev Public Health. 2004;25:247–280. doi: 10.1146/annurev.publhealth.25.102802.124329. [DOI] [PubMed] [Google Scholar]
- 4.Özkaynak H, Thurston GD. Associations between 1980 U.S. mortality rates and alternative measures of airborne particle concentration. Risk Anal. 1987;7(4):449–461. doi: 10.1111/j.1539-6924.1987.tb00482.x. [DOI] [PubMed] [Google Scholar]
- 5.Laden F, Schwartz J, Speizer FE, Dockery DW. Reduction in fine particulate air pollution and mortality: Extended follow-up of the Harvard Six Cities study. Am J Respir Crit Care Med. 2006;173(6):667–672. doi: 10.1164/rccm.200503-443OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pope CA, 3rd, et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA. 2002;287(9):1132–1141. doi: 10.1001/jama.287.9.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krewski D, et al. Extended Follow-Up and Spatial Analysis of the American Cancer Society Study Linking Particulate Air Pollution and Mortality: Special Report. Cambridge, MA: Health Effects Institute; 2009. [PubMed] [Google Scholar]
- 8.Zeger SL, Dominici F, McDermott A, Samet JM. Mortality in the Medicare population and chronic exposure to fine particulate air pollution in urban centers (2000–2005) Environ Health Perspect. 2008;116(12):1614–1619. doi: 10.1289/ehp.11449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crouse DL, et al. Risk of nonaccidental and cardiovascular mortality in relation to long-term exposure to low concentrations of fine particulate matter: A Canadian national-level cohort study. Environ Health Perspect. 2012;120(5):708–714. doi: 10.1289/ehp.1104049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoek G, et al. Long-term air pollution exposure and cardio-respiratory mortality: A review. Environ Health. 2013;12(1):43. doi: 10.1186/1476-069X-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pope CA, 3rd, Ezzati M, Dockery DW. Fine-particulate air pollution and life expectancy in the United States. N Engl J Med. 2009;360(4):376–386. doi: 10.1056/NEJMsa0805646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Correia AW, et al. Effect of air pollution control on life expectancy in the United States: An analysis of 545 U.S. counties for the period from 2000 to 2007. Epidemiology. 2013;24(1):23–31. doi: 10.1097/EDE.0b013e3182770237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arias E. United States life tables, 2008. Natl Vital Stat Rep. 2012;61(3):1–63. [PubMed] [Google Scholar]
- 14.Brook RD, et al. American Heart Association Council on Epidemiology and Prevention, Council on the Kidney in Cardiovascular Disease, and Council on Nutrition, Physical Activity and Metabolism Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010;121(21):2331–2378. doi: 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- 15.Pope CA, 3rd, et al. Lung cancer and cardiovascular disease mortality associated with ambient air pollution and cigarette smoke: Shape of the exposure-response relationships. Environ Health Perspect. 2011;119(11):1616–1621. doi: 10.1289/ehp.1103639. [DOI] [PMC free article] [PubMed] [Google Scholar]