ABSTRACT
Purpose: To determine the physiotherapy-related needs of people with stroke at discharge, 6 months after discharge, and 1 year after discharge from hospital, and to examine the results stratified by participants' acute Functional Independence Measure (FIM) scores. Methods: A total of 241 adults with recent stroke were recruited into this longitudinal cohort study. As well as participating in a semi-structured interview that included questions about mobility needs and barriers, participants were asked to complete and return a closed-ended needs-assessment survey. Results: During the interview, participants reported needs and barriers related to motor control, walking, stairs, fatigue, prevention of falls, and access to physiotherapy services. The survey identified many more needs, including transfers, wheelchair use, higher-level balance and mobility skills, and access to physiotherapy and suitable exercise facilities. Frequencies of needs and barriers tended to be lower among participants with higher acute FIM scores. There was no consistent trend for needs and barriers to decrease over time. Conclusions: Over the first year after discharge from hospital, people with stroke report a large and varied number of persistent mobility-related needs. Physiotherapists have a role to play in advocating for adequate follow-up services and informing health policy with respect to the needs of their patients with stroke.
Key Words: mobility limitation, needs assessment, rehabilitation, stroke
RÉSUMÉ
Objectif : Établir les besoins en physiothérapie des personnes ayant subi un accident vasculaire cérébrale (AVC) lors de leur congé de l'hôpital, 6 mois après leur congé et 1 an après leur congé, et examiner les résultats stratifiés en fonction des pointages de mesure de l'autonomie fonctionnelle aigüe (Functional Independence Measure, FIM). Méthodologie : On a recruté en tout 241 adultes ayant récemment subi un ACV pour cette étude longitudinale de cohorte. En plus de participer à une entrevue semi-structurée comprenant des questions sur leurs besoins et sur les obstacles en matière de mobilité, les participants ont dû remplir et retourner un sondage d'évaluation des besoins avec questions fermées. Résultats : Au cours de l'entrevue, les participants ont fait part de besoins et d'obstacles liés au contrôle de leur motricité, à la marche, aux escaliers, à la fatigue, à la prévention des chutes et à l'accès à des services de physiothérapie. Le sondage a permis d'établir de nombreux autres besoins, dont la nécessité de transferts, l'utilisation d'un fauteuil roulant, un plus grand équilibre et de plus grandes habiletés motrices ainsi que l'accès à la physiothérapie et à des installations adaptées à leurs besoins en exercice. La fréquence des besoins et des obstacles avait tendance à diminuer chez les participants qui avaient obtenu des pointages plus élevés à l'échelle FIM. On n'a observé aucune tendance constante de diminution des besoins et des obstacles au fil du temps. Conclusions : Au cours de la première année suivant le congé de l'hôpital, les personnes qui ont subi un AVC font état d'un grand nombre de besoins variés et persistants en matière de mobilité. Les physiothérapeutes doivent faire pression pour des services de suivi adéquat et doivent contribuer à l'inclusion des besoins des patients qui ont subi un AVC dans les politiques en matière de santé.
Mots clés : AVC, évaluation des besoins, spécialité de la physiothérapie, limitations dans la mobilité, réadaptation
The Heart and Stroke Foundation of Canada has reported that the yearly incidence of stroke is approximately 50,000 and that approximately 300,000 Canadians live with the residual effects of stroke.1 The majority of people hospitalized after a stroke return to the community after a short acute stay or a period of in-patient rehabilitation.2 In both settings, a key role for physiotherapists is discharge planning and preparation; to better prepare patients for successful community re-integration and to ensure adequate follow-up, therapists need to understand the needs of people with stroke after discharge from hospital.
A limited number of studies specifically examining the needs of people with stroke are relevant to physiotherapy in Canada. Two small focus-group studies have assessed the needs of people with stroke in Quebec;3,4 participants identified needs related to mobility, arm and hand rehabilitation, general exercise, fall prevention, and access to physiotherapy. In an epidemiologically based needs assessment for eastern Ontario, Hunter and colleagues used population survey and registry data to estimate the prevalence of stroke-related disability;5 they determined optimal levels of rehabilitation service based on published post-stroke rehabilitation practice guidelines, then compared these optimal levels to actual service data, identifying a 25% rate of unmet rehabilitation needs. Unfortunately, unmet need for physiotherapy was not reported separately from unmet needs for other rehabilitation therapies, which limits the study's usefulness as a guide for physiotherapy practice. In a survey of 24 families of people with stroke in the United States,6 participants identified needs related to fall prevention (71%), staying active (63%), and dexterity and general function (46%). Sampling procedures for the study were not described, and validity was compromised by a low response rate of 14%.
Several international studies have been published that examined the needs of people with stroke. In two questionnaire studies carried out in the Netherlands, unmet mobility needs were identified in 31%7 and 47%8 of participants with stroke. In a British survey of young survivors of stroke,9 15% of participants reported an unmet need for physiotherapy. When 10 patients of an Australian day hospital rehabilitation programme were interviewed, more than half identified needs related to regaining functional ability and having opportunities to practise everyday skills.10 Similarly, Lui and Mackenzie11 identified the concept of physical need (therapy and mobilization) from an ethnographic needs study of 15 patients with stroke in Hong Kong, but because details of therapy and mobilization were not reported, it is difficult to determine what aspects of therapy (e.g., more therapy, reduced waiting times) and mobilization (e.g., independence, tolerance, and/or safety) were needed.
Overall, the findings of the studies described above3–11 indicate that post-discharge mobility and service-related needs are going unmet for people with stroke. Unfortunately, these studies have not provided the level of detail about these needs that would help to direct physiotherapists' decision making. In addition, patient needs have consistently been documented at a single time point; because of changes in personal factors, environment, and service provision, however, we may expect that the nature and extent of patients' perceived needs will change over time. Information related to the longitudinal needs of people with stroke could help hospital- and community-based therapists to more effectively plan physiotherapy service beyond the initial period of returning home. Previous studies3–11 have also tended to present patients with stroke as a relatively homogeneous group. It seems reasonable to expect, however, that the needs of people with mild stroke impairment will differ from those of people with more severe impairment and limited function. Van de Port and colleagues8 found that people who had significant residual motor impairment at 3 years post stroke were three times as likely to report unmet needs as those with minimal or no motor impairment.
Our purpose in this study was to enumerate the physiotherapy-related needs of people with a history of stroke at three time points during the first year after discharge from hospital. To provide data that could help therapists prepare specific patient groups for discharge home, we stratified participants into three groups based on acute functional status, as measured by the Functional Independence Measure (FIM), scored between day 7 and day 10 post stroke.
Methods
Our study used a subset of physiotherapy-relevant findings from a larger comprehensive needs assessment of people who had been hospitalized for stroke,12 which is described in detail elsewhere.12 According to definitions of needs assessment, this was an assessment of felt needs13 in people admitted to hospital with acute stroke. Participants were recruited from three teaching hospitals in Hamilton and one community hospital in Burlington, Ontario. Patients were included if they were in hospital with a primary diagnosis of stroke, were at least 18 years old, and could participate in the interview independently or through a translator. Participants were recruited consecutively, and each participant provided informed consent. The Research Ethics Boards of all recruitment sites approved the study.
To determine sample size, we calculated that a 95% CI±10% on the point estimates of the frequencies of needs would be sufficient to interpret the results. Based on this CI and an anticipated attrition of 37% due to deaths2 and drop-outs at 1 year, the target sample size was 95 participants in each FIM group. Because our primary purpose was to enumerate the needs of individuals after stroke, the sample size was not powered to detect between- or within-group differences.
Within 10 days of stroke onset, participants were assessed by the treating physiotherapist using the FIM, a reliable and valid measure of activities of daily living (ADL);14 therapists administering the FIM received standardized training and met FIM testing criteria. Demographic and other clinical data were gathered by one of the investigators. Patients were stratified into three groups, based on evidence that FIM score is strongly associated with discharge disposition and need for rehabilitation:15 Acute FIM score ≤40, Acute FIM score 41–80, and Acute FIM score >80.
Self-reported mobility and physiotherapy needs were assessed via (1) a semi-structured interview and (2) a comprehensive closed-ended quantitative survey. Participants' needs were assessed within 1 month of discharge from hospital, at 6 months post discharge, and at 12 months post discharge.
The interview and questionnaire were developed in collaboration with a multidisciplinary advisory team and pilot-tested with people with a recent history of stroke; no revisions to the interview or questionnaire were required as a result of pilot testing. The test–retest reliability of the survey was estimated by having a convenience sample of 11 consecutive participants complete two copies of the questionnaire within 2 days of each other. To assess agreement between responses on the two questionnaires, the prevalence-adjusted, bias-adjusted kappa (κ) was calculated for each questionnaire item; median κ for all items was 0.75 (interquartile range 0.63–0.77), indicating substantial agreement.16
The open-ended interview questions were structured to first ask participants whether they had problems in a given area and then ask what would be needed to deal with or overcome these problems. In an effort to comprehensively identify participant issues, we also asked questions about barriers to participation. All questions included standard interviewer prompts if a participant could not respond. The open-ended questions of interest to physiotherapy were the following: Do you have any physical difficulties as a result of the stroke? If yes, what are they? What do you think you need to help deal with or overcome these difficulties? What would you say are the major barriers to you fully participating in and enjoying life? Would you consider any of your physical symptoms a major barrier to enjoying life? Trained research assistants conducted the interviews in each participant's place of residence and recorded responses in writing in detail.
To enumerate physiotherapy needs and barriers from the interviews, all three investigators reviewed a sample of 10 interviews and assigned physiotherapy descriptors to code the responses. Further interviews were examined until no further descriptors were found. Two research assistants (a social worker and an occupational therapy student) independently identified the occurrence of descriptors in the remaining interviews; new descriptors were added as needed.
The interview data were analyzed by calculating frequencies17 and 95% CIs of participants reporting a need or barrier that fit into a specific descriptor. This analysis was completed for each FIM group and for each time period, using the statistical software SPSS 18.0 (SPSS Inc., Chicago, IL) and PEPI 4.04x (JH Abramson & PM Gahlinger, Salt Lake City, UT). As a secondary analysis, we visually examined the graphs for within-group and between-group trends. To avoid the problems associated with multiplicity of testing, we did not carry out inferential statistical testing: as there were 441 potential comparisons, 22 would be expected to be significant by chance alone.
After the interview, participants were given the questionnaire, along with a pre-addressed stamped envelope in which to return it. Of 160 questionnaire items, 34 focused on needs and barriers related to physiotherapy. The magnitude of the specific needs and barriers was scored on a five-point scale (0=not a need; 4=very large need). For each need and barrier, the frequency, 95% CI, and mean magnitude (if scored >0) were calculated using SPSS 18.0 and PEPI 4.04x. To organize presentation of the results, we grouped the survey items into three categories: body structure and function, activities and participation, and service-related needs.18
Results
Recruitment took place from October 2002 to February 2006. We were unable to achieve the proposed sample size of 95 for the lowest FIM group (≤40) because of low recruitment levels and deaths before the first interview. A total of 241 participants were recruited into the study, of whom 32 dropped out before the first interview after discharge. One participant in the FIM >80 group was originally misclassified into the FIM 41–80 group. At the discharge assessment, there were 12 participants in the FIM ≤40 group, 94 in the FIM 41–80 group, and 103 in the FIM >80 group. Demographic and clinical characteristics for each time point are presented in Table 1. There were no statistically significant differences between participants who dropped out before the first interview and those who completed the first interview.
Table 1.
Demographic and Clinical Characteristics of the Sample
| % of patients* |
||||||
|---|---|---|---|---|---|---|
| Characteristics | Completed discharge interview (n=209) |
Returned discharge survey (n=94) |
Completed 6-month interview (n=182) |
Returned 6-month survey (n=67) |
Completed 1-year interview (n=148) |
Returned 1-year survey (n=47) |
| Sex, male/female | 51/49 | 49/51 | 52/48 | 51/49 | 54/46 | 49/51 |
| Age, mean (SD) y | 73 (11.2) | 73 (10.5) | 73 (11.2) | 72 (10.4) | 73 (11.2) | 73 (10.2) |
| Marital status, married or partner | 59 | 62 | 58 | 64 | 60 | 63 |
| Living situation before stroke | ||||||
| Own home | 82 | 83 | 80 | 86 | 86 | 87 |
| Living alone | 24 | 22 | 25 | 20 | 25 | 20 |
| Education, >high school | 60 | 66 | 59 | 65 | 63 | 64 |
| L1 English | 78 | 80 | 75 | 73 | 75 | 72 |
| Employed pre-stroke | 19 | 20 | 17 | 14 | 16 | 11 |
| Indep ADL pre-stroke | 87 | 93 | 86 | 86 | 85 | 87 |
| Indep IADL pre-stroke | 75 | 87 | 72 | 82 | 77 | 83 |
| First stroke | 72 | 76 | 74 | 70 | 71 | 62 |
| Type of stroke | ||||||
| Ischemic | 88 | 87 | 87 | 88 | 89 | 87 |
| Haemorrhagic | 12 | 13 | 13 | 12 | 11 | 13 |
| Side of hemiplegia | ||||||
| Right | 44 | 47 | 45 | 48 | 45 | 43 |
| Left | 45 | 37 | 42 | 39 | 42 | 48 |
| Bilateral | 11 | 16 | 13 | 12 | 13 | 9 |
| No. of comorbidities, mean (SD) | 3.9 (2.1) | 3.7 (2.1) | 4.0 (2.1) | 4.0 (2.1) | 3.9 (2.1) | 4.1 (2.2) |
| Acute FIM score, mean (SD) | 82 (26.2) | 86 (25.6) | 82 (26.6) | 83 (27.0) | 82 (26.6) | 82 (29.5) |
| Location | ||||||
| Own home | 68 | 79 | 71 | 81 | 75 | 77 |
| Nursing home | 13 | 6 | 14 | 6 | 12 | 9 |
| FIM score, mean (SD) | 106 (21.8) | 110 (20.1) | 107 (23.5) | 112 (19.0) | 110 (20.5) | 112 (21.2) |
Unless otherwise indicated.
L1=first language; Indep=independent; ADL=activities of daily living; IADL=instrumental activities of daily living; FIM=Functional Independence Measure.
We interviewed 209 participants within 1 month of discharge from hospital; of these, 182 (87%) were also interviewed at 6 months and 148 (71%) at 12 months after discharge. Of the original 209 participants interviewed, 94 (45%) returned their survey at discharge, 67 (37%) at 6 months after discharge, and 47 (32%) at 1 year after discharge. There was a statistically significant difference (p<0.05) in side of hemiplegia between interview dropouts (33% right, 59% left, 5% bilateral) and responders (45% right, 42% left, 13% bilateral) at 6 months post discharge. At discharge and 1 year after discharge, there were no statistically significant differences between dropouts and responders.
Semi-structured interview results
The frequencies of needs are presented in Figure 1. For presentation, the 47 physiotherapy-related descriptors were collapsed into seven categories: motor control (e.g., upper extremity, lower extremity, fine motor), walking ability (e.g., walking related to social, recreational, and role effects), stairs, fitness (including strength), fatigue, balance (including balance confidence), and need for physiotherapy. For example, if a participant expressed a need for improved ability to move his or her leg and foot, this was counted as a motor-control-related need. Figure 1 shows that frequencies of needs tended to decrease as acute FIM score increased. Needs related to impaired motor control were most frequently reported across all FIM groups. The frequency of reported needs in the FIM >80 group tended to decrease from the first interview after discharge to the final interview at 1-year follow-up; this pattern was not observed in the FIM ≤40 or FIM 41–80 groups.
Figure 1.
Frequency (%) and 95% CIs of reported needs from interview responses at discharge, 6 months after discharge, and 12 months after discharge of participants in acute FIM categories (a) ≤40, (b) 41–80, and (c) >80.
FIM=Functional Independence Measure; PT=physiotherapy; d/c=discharge.
The barrier descriptors found in the interview data were motor control (e.g., upper extremity, lower extremity, fine motor), walking, stairs, fatigue, balance, falls (including fear of falling), and waiting lists for therapy. The results are presented in Figure 2. In the FIM ≤40 group, impaired motor control and limited walking ability were the greatest barriers, while balance was not a barrier. Fatigue was also identified as a major barrier in the FIM 41–80 and FIM >80 groups. Barriers did not always diminish over time.
Figure 2.
Frequency (%) and 95% CIs of reported barriers from interview responses at discharge, 6 months after discharge, and 12 months after discharge of participants in acute FIM categories (a) ≤40, (b) 41–80, and (c) >80.
FIM=Functional Independence Measure; PT=physiotherapy; d/c=discharge.
Survey results
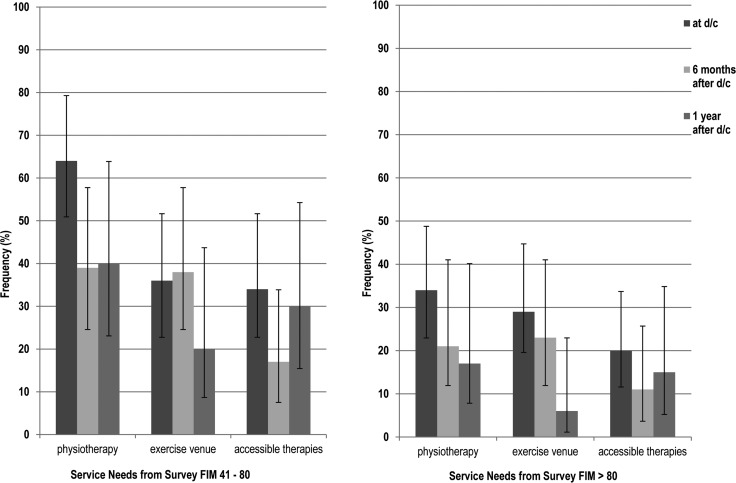
Figures 3–5 present the results of the survey. Because there were only four survey respondents in the FIM ≤40 group, the results for this group are not reported. Compared to the interview, the survey elicited many more needs at greater frequencies; because of the volume of data, needs have been concatenated with barriers in the discussion that follows.
Figure 4.
Frequency (%) and 95% CIs of reported activity participation–related needs from survey responses at discharge, 6 months after discharge, and 12 months after discharge for patients in acute FIM categories (a) 41–80 and (b) >80.
FIM=Functional Independence Measure; PT=physiotherapy; d/c=discharge.
Figure 3.
Frequency (%) and 95% CIs of reported body structure/function–related needs from survey responses at discharge, 6 months after discharge, and 12 months after discharge for participants in acute FIM categories (a) 41–80 and (b) >80.
FIM=Functional Independence Measure; PT=physiotherapy; d/c=discharge.
Figure 5.
Frequency (%) and 95% CIs of reported service-related needs from survey responses at discharge, 6 months after discharge, and 12 months after discharge for participants in acute FIM categories (a) 41–80 and (b) >80.
FIM=Functional Independence Measure; PT=physiotherapy; d/c=discharge.
In the category body structure and function, fatigue was rated high in both FIM groups at all time points. Figure 3 suggests that needs tended to be reported less frequently in the higher FIM group. In addition to the needs identified during the interview, participants who completed the survey identified shoulder pain, spasticity, and fear of falling. In the category activities and participation, all participants reported needs related to higher-level mobility, such as getting up from the floor, walking outdoors, and managing stairs. In both categories, needs tended to remain stable across the three assessment periods. In the services category, needs were similar between the two FIM groups: 49% of the entire sample reported a need for physiotherapy at discharge, 34% at 6 months after discharge, and 30% at 1 year after discharge; 33% of all participants reported needing a suitable place to exercise at discharge, 31% at 6 months after discharge, and 14% at 1 year after discharge. Finally, between 22% and 27% of participants reported a need for more accessible therapies.
In an effort to summarize the survey results, we identified items with a mean rating from 2.5 (high–moderate need or barrier) to 4 (very large need or barrier) as particularly important to participants. Using this definition, the following needs were identified as important at discharge: toilet transfers, tub transfers, use of wheelchair, transferring to and from the floor, walking outdoors, walking in crowded places, going up and down stairs, ability to carry objects, more physiotherapy, a suitable place to exercise, ability to use hands, increased arm strength, increased leg strength, and reduced spasticity. High-rated barriers at discharge were physical symptoms of stroke, weakness in arm and leg, and difficulty in accessing therapy.
At 6 months after discharge, needs identified as important were standing for long periods, transferring to and from the floor, walking outdoors, walking in crowded places, therapy closer to their own home, suitable place to exercise, relief from pain, ability to use hand, improved standing balance, standing for long periods, increased leg strength, and participation in sports. Important barriers at 6 months after discharge were physical symptoms of stroke, weakness in arm and leg, and balance problems.
At 1 year after discharge, high-rated needs were toilet transfer, transferring in and out of tub, ability to use wheelchair, more physiotherapy, therapy closer to home, better communication between therapists and medical professionals, suitable place to exercise, and ability to use hand. Barriers deemed important at 1 year after discharge were physical symptoms of stroke, weakness in arm and leg, and accessing therapy.
Discussion
Our findings on the frequencies and importance of physiotherapy-related needs of individuals with stroke at discharge and at 6-month and 1-year follow-up concur with and expand on previous studies.3–11
Mobility-related needs
In the focus-group study by Vincent and colleagues,3 participants with chronic stroke reported motor activity needs including learning to walk, balance, and manage stairs. In addition to these needs, participants in our study identified some unmet basic mobility needs, such as bed mobility and toilet and tub transfers, as well as higher-level mobility needs such as getting up from the floor; walking outdoors, in crowds, and while carrying things; and moving more efficiently. The majority of these needs reflect the known demands of living and mobilizing in the community. Older adults' ventures into the community have been observed to include walking distances, navigating stairs, walking quickly to cross a street, carrying items, and walking through crowds.19 Similarly, Lord and colleagues20 found that three out of four stroke survivors identified community mobility as an essential or very important skill to be addressed through rehabilitation. It is important that we acknowledge the value that people put on returning to these higher-level activities; we must be careful not to restrict access to ongoing physiotherapy after basic mobility milestones have been achieved. While full remediation of motor control may not be realistic for everyone,21 physiotherapists may use compensatory and adaptive approaches to facilitate optimal community re-integration.
Fatigue and fitness level
Fatigue, mentioned by approximately 75% of participants in both FIM 41–80 and FIM >80 groups, was one of the most commonly reported issues on the survey. In the literature, the prevalence of fatigue has ranged from 38% to 77% in people with stroke;22 in a recent study, 50% of participants identified fatigue as among the most disabling of stroke symptoms.23 Interestingly, our participants with mild acute presentation (FIM >80) were just as likely to report fatigue as a problem as those with more severe limitations (FIM 41–80). While there is evidence that lower levels of physical function can be a risk factor for post-stroke fatigue,24 many patients with little or no physical impairment also report fatigue.25 It is likely that fatigue is multidimensional in its aetiology, sometimes linked to limited aerobic capacity, depression, stroke location, and/or comorbid conditions as well as to stroke.22,24,26 Despite the prevalence and importance of fatigue, there is a dearth of research on post-stroke fatigue interventions. A recent systematic review27 found only two small drug trials and one self-management intervention study, none of which found a benefit of the experimental intervention over the control. Participants in a recent focus group reported that walking, water aerobics, and using assistive devices helped them cope with their fatigue after stroke,28 but we were unable find research to support these claims. Fatigue management is an important area for future research.
Participants' perceived need to improve their fitness levels is consistent with evidence of marked reduction in exercise capacity after stroke.29 It is also clear from the evidence that this impairment is amenable to physiotherapy treatment.30 In addition to referral to traditional outpatient physiotherapy programmes, in-patient therapists may recommend participation in cardiac-rehabilitation-style programmes31 or referral to community-based exercise programmes.32
Need for ongoing physiotherapy
In our study, 49% of participants identified a specific unmet need for physiotherapy 1 month after discharge from hospital. This number dropped to 30% at 1-year follow-up, but this still represents a significant proportion of individuals who felt they were not receiving the physiotherapy care they required. This proportion is greater than the 15% who expressed an unmet need for physiotherapy in a study of younger adults with chronic stroke;9 the difference may be explained by the age of participants or the chronicity of stroke.
Self-reported needs for physiotherapy may or may not reflect actual follow-up rates after discharge from hospital. We were not able to identify any reports in the literature on the actual amount of follow-up physiotherapy provided in Canada. Hunter and colleagues,5 who compared actual amount of follow-up to estimates of need for rehabilitation therapy based on incidence data, acute-care provision data, and therapy effectiveness data, estimated that only 75% of the need for rehabilitation was met after stroke; specific estimates of unmet need for physiotherapy were not provided. In the United Kingdom, Martin and colleagues33 reviewed people between 6 and 9 months after stroke and found that although 46% had some day-hospital follow-up, many reported feeling abandoned by the health care system. In a multi-country European study, physiotherapy follow-up ranged from 20% to 82% by 6 months post stroke.34 Given that a recent meta-analysis of physiotherapy efficacy studies in people at least 6 months post stroke showed a statistically significant effect size of 0.29,35 it is likely that current levels of service are not optimizing patient outcomes. Further research is needed to predict which patients will respond to therapy and to determine optimal timing and intensity of follow-up therapy.
Needs and functional status
Participants with lower acute FIM scores tended to have greater frequency of needs (see Figures 1 and 2). This finding is consistent with the work of van de Port and colleagues, who demonstrated a relationship between stroke severity and number of unmet needs.8 In our study, the FIM 41–80 group tended to have more frequent issues related to balance and fear of falling than the FIM >80 group. Participants in the FIM ≤40 group had the highest frequency of needs related to motor control and walking, but were less concerned about fitness and balance than the other two groups; these differences may reflect a hierarchy of perceived needs associated with increasing functional status. People with lower levels of function may be more concerned with achieving basic motor recovery and walking function; as they meet basic mobility milestones, they may become more active and therefore more aware of their balance impairment, risk of falls, and decreased exercise tolerance.
Needs over time
Although one might expect that needs would decrease over time, we did not see this trend in our data. This apparent stability in needs may reflect a plateau in functional recovery demonstrated by participants soon after discharge from hospital: as Table 1 shows, mean FIM score remained relatively stable over the first year following discharge. Alternatively, needs may have persisted over time because of inadequate intensity or availability of physiotherapy aimed at remediating, compensating for, or adapting to residual impairments and limitations. It is difficult to determine the reason for an apparent lack of change in need over time. Self-reports of constructs such as needs and quality of life can be influenced by multiple factors;36 according to response shift theory, one's perception of need may shift or remain stable, independent of physical status or level of function, as a result of personal changes in internal standards, values, and conceptualization of one's situation.36 Regardless of the reason for this finding, it is clear that physiotherapy-relevant patient-expressed needs persist for at least 1 year after discharge from hospital following stroke, even among people with mild acute presentation. This finding is consistent with those of previous cross-sectional studies that have identified unmet needs years after stroke.3,4,8,9 Future research should include a longitudinal study that follows individuals beyond the first year after discharge.
Limitations
Our study has some limitations. First, we saw a large number of dropouts in the survey component of the study, which may have biased the results toward underestimation of needs. Although we present the interview results for the FIM ≤40 group, this group is under-represented in our sample, and it is likely that those who responded represent the highest-functioning element of this group; a different research approach may be needed for this segment of the population. A second limitation relates to the interview and survey tools used in this study. Because we were unable to find an existing tool that met our need for a comprehensive assessment of needs in patients with a history of stroke, we created our own semi-structured interview and survey tool; we carried out reliability testing on the survey, but it has not undergone full psychometric evaluation, which may limit the validity of our results. Lastly, although it is essential that we understand our patients' felt needs, it is important to acknowledge that not all perceived needs will be responsive to physiotherapy intervention. Data from this study are of limited use to therapists if applied in isolation. According to Straus and Sackett's definition of evidence-based practice, decisions are best made by considering the most up-to-date research-based evidence, clinician experience, and patient values.37 We propose that these values are reflected in patient-expressed needs. Therapists should consider our study findings on patient needs in the context of their own experiences, their knowledge of the literature on effectiveness and prognosis, and the expressed needs of their own individual clients.
Conclusions
In this longitudinal study, a significant proportion of participants with stroke reported a variety of unmet physiotherapy-related needs approximately 1 month, 6 months, and 1 year after discharge from hospital. All participants identified unmet needs related to motor control, mobility, and fatigue. Participants with moderate and mild acute presentation frequently expressed a need to improve higher-level mobility skills necessary for community ambulation; participants with more severe acute functional status tended to report a higher frequency of needs than those with milder acute presentation. In all groups, physiotherapy-related needs tended to stay relatively stable over the first year after discharge from hospital. Knowledge of the self-perceived needs of people with different levels of acute function after stroke should help physiotherapists to better prepare patients for effective discharge from hospital. This information should also assist health decision makers in planning appropriate community-based physiotherapy-related services after stroke.
Key Messages
What is already known on this topic
A few studies have identified the presence of unmet needs related to physical function and mobility in people with chronic stroke. Most studies are cross-sectional and have not elaborated on the specific needs identified by patients with stroke in the first year following discharge from hospital.
What this study adds
Following stroke, a significant proportion of people report a variety of unmet needs during the first year after discharge from hospital. Most commonly reported are needs related to motor control, mobility, fatigue, and access to physiotherapy. The frequency of unmet needs and barriers tends to be higher in people with lower acute functional status. Needs appear to remain stable over the first year after hospital discharge.
Physiotherapy Canada 2013; 65(3);204–214; doi:10.3138/ptc.2012-14
References
- 1.Heart and Stroke Foundation. Stroke statistics [Internet] Ottawa: Heart and Stroke Foundation of Canada; c2011. [cited 2011 Dec 2]. [updated 2011 Nov]. Available from: http://www.heartandstroke.com/site/c.ikIQLcMWJtE/b.3483991/k.34A8/Statistics.htm. [Google Scholar]
- 2.Kapral MK, Hall R, Stamplecoski M, et al. Registry of the Canadian Stroke Network: report on the 2008/09 Ontario Stroke Audit [Internet] Toronto: Institute for Clinical Evaluative Sciences; 2011. [cited 2011 Dec 2]. Available from: http://www.ices.on.ca/webpage.cfm?site_id=1&org_id=31&morg_id=0&gsec_id=0&item_id=6730. [Google Scholar]
- 3.Vincent C, Deaudelin I, Robichaud L, et al. BRAD group. Rehabilitation needs for older adults with stroke living at home: perceptions of four populations. BMC Geriatr. 2007;7(1):20. doi: 10.1186/1471-2318-7-20. http://dx.doi.org/10.1186/1471-2318-7-20. Medline:17697322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Talbot LR, Viscogliosi C, Desrosiers J, et al. Identification of rehabilitation needs after a stroke: an exploratory study. Health Qual Life Outcomes. 2004;2(1):53. doi: 10.1186/1477-7525-2-53. http://dx.doi.org/10.1186/1477-7525-2-53. Medline:15383147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hunter DJ, Grant HJ, Purdue MP, et al. An epidemiologically-based needs assessment for stroke services. Chronic Dis Can. 2004;25(3-4):138–46. Medline:15841854. [PubMed] [Google Scholar]
- 6.Pierce LL, Gordon Finn M, Steiner V. Families dealing with stroke desire information about self-care needs. Rehabil Nurs. 2004;29(1):14–7. doi: 10.1002/j.2048-7940.2004.tb00294.x. http://dx.doi.org/10.1002/j.2048-7940.2004.tb00294.x. Medline:14727471. [DOI] [PubMed] [Google Scholar]
- 7.Boter H, Rinkel GJE, de Haan RJ HESTIA Study Group. Outreach nurse support after stroke: a descriptive study on patients' and carers' needs, and applied nursing interventions. Clin Rehabil. 2004;18(2):156–63. doi: 10.1191/0269215504cr713oa. http://dx.doi.org/10.1191/0269215504cr713oa. Medline:15053124. [DOI] [PubMed] [Google Scholar]
- 8.van de Port IGL, van den Bos GA, Voorendt M, et al. Identification of risk factors related to perceived unmet demands in patients with chronic stroke. Disabil Rehabil. 2007;29(24):1841–6. doi: 10.1080/09638280601129157. http://dx.doi.org/10.1080/09638280601129157. Medline:17852229. [DOI] [PubMed] [Google Scholar]
- 9.Kersten P, Low JTS, Ashburn A, et al. The unmet needs of young people who have had a stroke: results of a national UK survey. Disabil Rehabil. 2002;24(16):860–6. doi: 10.1080/09638280210142167. http://dx.doi.org/10.1080/09638280210142167. Medline:12450462. [DOI] [PubMed] [Google Scholar]
- 10.Henderson A, Milburn D, Everingham K. Where to from here: patients of a day hospital rehabilitation programme perceived needs following stroke. Contemp Nurse. 1998;7(4):211–6. doi: 10.5172/conu.1998.7.4.211. http://dx.doi.org/10.5172/conu.1998.7.4.211. Medline:10095503. [DOI] [PubMed] [Google Scholar]
- 11.Lui MHL, MacKenzie AE. Chinese elderly patients' perceptions of their rehabilitation needs following a stroke. J Adv Nurs. 1999;30(2):391–400. doi: 10.1046/j.1365-2648.1999.01087.x. http://dx.doi.org/10.1046/j.1365-2648.1999.01087.x. Medline:10457241. [DOI] [PubMed] [Google Scholar]
- 12.Moreland JD, Depaul VG, Dehueck AL, et al. Needs assessment of individuals with stroke after discharge from hospital stratified by acute Functional Independence Measure score. Disabil Rehabil. 2009;31(26):2185–95. doi: 10.3109/09638280902951846. http://dx.doi.org/10.3109/09638280902951846. Medline:19903128. [DOI] [PubMed] [Google Scholar]
- 13.Rothman J, Gant LM. Approaches and methods of community intervention. In: Johnson DE, Meiller LR, Miller LC, et al., editors. Needs assessment: theory and methods. Ames (IA): Iowa State University Press; 1987. [Google Scholar]
- 14.Hamilton BB, Laughlin JA, Fiedler RC, et al. Interrater reliability of the 7-level Functional Independence Measure (FIM) Scand J Rehabil Med. 1994;26(3):115–9. Medline:7801060. [PubMed] [Google Scholar]
- 15.Ween JE, Alexander MP, D'Esposito M, et al. Factors predictive of stroke outcome in a rehabilitation setting. Neurology. 1996;47(2):388–92. doi: 10.1212/wnl.47.2.388. http://dx.doi.org/10.1212/WNL.47.2.388. Medline:8757009. [DOI] [PubMed] [Google Scholar]
- 16.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74. http://dx.doi.org/10.2307/2529310. Medline:843571. [PubMed] [Google Scholar]
- 17.Strupek CD. Analyzing indicators and using the analysis. In: Nardi DA, Petr JM, editors. Community health and wellness needs assessment: a step-by-step guide. New York: Thomson Delmar Learning; 2003. pp. 224–5. [Google Scholar]
- 18.Geyh S, Cieza A, Schouten J, et al. ICF core sets for stroke. J Rehabil Med. 2004;(44 Suppl):135–41. doi: 10.1080/16501960410016776. http://dx.doi.org/10.1080/16501960410016776. Medline:15370761. [DOI] [PubMed] [Google Scholar]
- 19.Shumway-Cook A, Patla AE, Stewart A, et al. Environmental demands associated with community mobility in older adults with and without mobility disabilities. Phys Ther. 2002;82(7):670–81. Medline:12088464. [PubMed] [Google Scholar]
- 20.Lord SE, McPherson K, McNaughton HK, et al. Community ambulation after stroke: how important and obtainable is it and what measures appear predictive? Arch Phys Med Rehabil. 2004;85(2):234–9. doi: 10.1016/j.apmr.2003.05.002. http://dx.doi.org/10.1016/j.apmr.2003.05.002. Medline:14966707. [DOI] [PubMed] [Google Scholar]
- 21.Buurke JH, Nene AV, Kwakkel G, et al. Recovery of gait after stroke: what changes? Neurorehabil Neural Repair. 2008;22(6):676–83. doi: 10.1177/1545968308317972. http://dx.doi.org/10.1177/1545968308317972. Medline:18971383. [DOI] [PubMed] [Google Scholar]
- 22.Lerdal A, Bakken LN, Kouwenhoven SE, et al. Poststroke fatigue—a review. J Pain Symptom Manage. 2009;38(6):928–49. doi: 10.1016/j.jpainsymman.2009.04.028. http://dx.doi.org/10.1016/j.jpainsymman.2009.04.028. Medline:19811888. [DOI] [PubMed] [Google Scholar]
- 23.van Eijsden HM, van de Port IGL, Visser-Meily JMA, et al. Poststroke fatigue: who is at risk for an increase in fatigue? Stroke Res Treat. 2012;2012:863978. doi: 10.1155/2012/863978. http://dx.doi.org/10.1155/2012/863978. Medline:22028989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lerdal A, Bakken LN, Rasmussen EF, et al. Physical impairment, depressive symptoms and pre-stroke fatigue are related to fatigue in the acute phase after stroke. Disabil Rehabil. 2011;33(4):334–42. doi: 10.3109/09638288.2010.490867. http://dx.doi.org/10.3109/09638288.2010.490867. Medline:20521900. [DOI] [PubMed] [Google Scholar]
- 25.Winward C, Sackley C, Metha Z, et al. A population-based study of the prevalence of fatigue after transient ischemic attack and minor stroke. Stroke. 2009;40(3):757–61. doi: 10.1161/STROKEAHA.108.527101. http://dx.doi.org/10.1161/STROKEAHA.108.527101. Medline:19131658. [DOI] [PubMed] [Google Scholar]
- 26.Tseng BY, Billinger SA, Gajewski BJ, et al. Exertion fatigue and chronic fatigue are two distinct constructs in people post-stroke. Stroke. 2010;41(12):2908–12. doi: 10.1161/STROKEAHA.110.596064. http://dx.doi.org/10.1161/STROKEAHA.110.596064. Medline:20947841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McGeough E, Pollock A, Smith LN, et al. Interventions for post-stroke fatigue. Cochrane Database Syst Rev. 2009;8(3):CD007030. doi: 10.1002/14651858.CD007030.pub2. http://dx.doi.org/10.1002/14651858.CD007030.pub2. Medline:19588416. [DOI] [PubMed] [Google Scholar]
- 28.Flinn NA, Stube JE. Post-stroke fatigue: qualitative study of three focus groups. Occup Ther Int. 2010;17(2):81–91. doi: 10.1002/oti.286. Medline:19787634. [DOI] [PubMed] [Google Scholar]
- 29.MacKay-Lyons MJ, Makrides L. Longitudinal changes in exercise capacity after stroke. Arch Phys Med Rehabil. 2004;85(10):1608–12. doi: 10.1016/j.apmr.2004.01.027. http://dx.doi.org/10.1016/j.apmr.2004.01.027. Medline:15468019. [DOI] [PubMed] [Google Scholar]
- 30.Pang MYC, Eng JJ, Dawson AS, et al. The use of aerobic exercise training in improving aerobic capacity in individuals with stroke: a meta-analysis. Clin Rehabil. 2006;20(2):97–111. doi: 10.1191/0269215506cr926oa. http://dx.doi.org/10.1191/0269215506cr926oa. Medline:16541930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tang A, Marzolini S, Oh P, et al. Feasibility and effects of adapted cardiac rehabilitation after stroke: a prospective trial. BMC Neurol. 2010;10(1):40. doi: 10.1186/1471-2377-10-40. http://dx.doi.org/10.1186/1471-2377-10-40. Medline:20529376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pang MYC, Eng JJ, Dawson AS, et al. A community-based fitness and mobility exercise program for older adults with chronic stroke: a randomized, controlled trial. J Am Geriatr Soc. 2005;53(10):1667–74. doi: 10.1111/j.1532-5415.2005.53521.x. http://dx.doi.org/10.1111/j.1532-5415.2005.53521.x. Medline:16181164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Martin BJ, Yip B, Hearty M, et al. Outcome, functional recovery and unmet needs following stroke: experience of patient follow up at 6 to 9 months in a newly established stroke service. Scott Med J. 2002;47(6):136–7. doi: 10.1177/003693300204700605. Medline:12616970. [DOI] [PubMed] [Google Scholar]
- 34.Putman K, De Wit L, Schupp W, et al. Variations in follow-up services after inpatient stroke rehabilitation: a multicentre study. J Rehabil Med. 2009;41(8):646–53. doi: 10.2340/16501977-0385. http://dx.doi.org/10.2340/16501977-0385. Medline:19565159. [DOI] [PubMed] [Google Scholar]
- 35.Ferrarello F, Baccini M, Rinaldi LA, et al. Efficacy of physiotherapy interventions late after stroke: a meta-analysis. J Neurol Neurosurg Psychiatry. 2011;82(2):136–43. doi: 10.1136/jnnp.2009.196428. http://dx.doi.org/10.1136/jnnp.2009.196428. Medline:20826872. [DOI] [PubMed] [Google Scholar]
- 36.Schwartz CE, Andresen EM, Nosek MA, et al. RRTC Expert Panel on Health Status Measurement. Response shift theory: important implications for measuring quality of life in people with disability. Arch Phys Med Rehabil. 2007;88(4):529–36. doi: 10.1016/j.apmr.2006.12.032. http://dx.doi.org/10.1016/j.apmr.2006.12.032. Medline:17398257. [DOI] [PubMed] [Google Scholar]
- 37.Straus SE, Sackett DL. Applying evidence to the individual patient. Ann Oncol. 1999;10(1):29–32. doi: 10.1023/a:1008308211595. http://dx.doi.org/10.1023/A:1008308211595. Medline:10076718. [DOI] [PubMed] [Google Scholar]