ABSTRACT
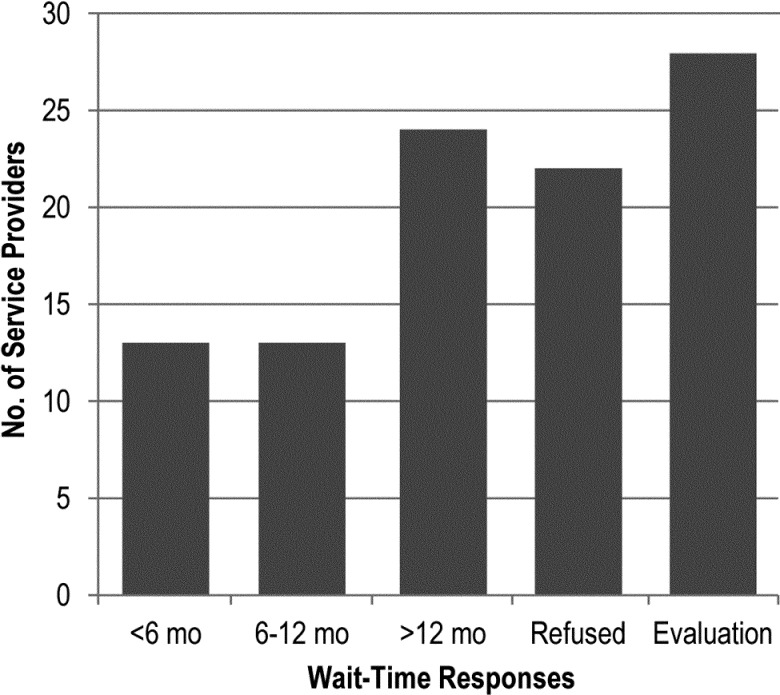
Purpose: Although arthritis is the leading cause of pain and disability in Canada, and physical therapy (PT) and occupational therapy (OT) are beneficial both for chronic osteoarthritis (OA) and for inflammatory arthritis such as rheumatoid arthritis (RA), there appear to be problems with access to such services. The aim of this study was to document wait times from referral by physician to consultation with PT or OT in the public health care system for people with arthritis in Quebec, Canada. Method: Appointments were requested by telephone, using hypothetical case scenarios; wait times were defined as the time between initial request and appointment date. Descriptive statistics were used to examine the wait times in relation to diagnosis, service provider and geographic area. Results: For both scenarios (OA and RA) combined, 13% were offered an appointment within 6 months, 13% offered given an appointment within 6–12 months, 24% were told they would need to wait longer than 12 months, and 22% were refused services. The remaining 28% were told they would require an evaluation appointment for functional assessment before being given an appointment for therapy. No difference was found between RA and OA diagnoses. Conclusions: Our study suggests that most people with arthritis living in the province of Quebec are not receiving publicly accessible PT or OT intervention in a timely manner.
Key Words: arthritis, health services accessibility, rehabilitation
RÉSUMÉ
Objet : Même si l'arthrite constitue la principale cause de douleur et d'incapacité au Canada et si la physiothérapie (PT) et l'ergothérapie (ET) sont bénéfiques à la fois contre l'arthrose chronique (AC) et l'arthrite inflammatoire comme la polyarthrite rhumatoïde (PR), il semble y avoir des problèmes d'accès à ces services. Cette étude visait à documenter les temps d'attente entre la référence par le médecin et la consultation en PT ou ET dans le système public de soins de santé pour les personnes atteintes d'arthrite au Québec, Canada. Méthode : On a demandé des rendez-vous par téléphone en utilisant des scénarios de cas hypothétiques. Les temps d'attente ont été définis comme le temps écoulé entre la demande initiale et la date du rendez-vous. Nous avons utilisé des statistiques descriptives pour analyser les temps d'attente par rapport au diagnostic, au fournisseur de service et à la région géographique. Résultats : Pour les deux scénarios (AC et PR) combinés, 13 % ont reçu un rendez-vous dans les six mois, 13 %, en six à 12 mois, on a dit à 24 % qu'ils devraient attendre plus de 12 mois et l'on a refusé des services dans 22 % des cas. Dans les 28 % de cas restants, on a dit que la personne en cause aurait besoin d'un rendez-vous d'évaluation fonctionnelle avant d'obtenir un rendez-vous de traitement. On n'a constaté aucune différence entre les diagnostics de PR et d'AC. Conclusions : Notre étude indique que la plupart des personnes qui vivent avec l'arthrite dans la province de Québec ne reçoivent pas en temps opportun de services publics de PT ou d'ET.
Mots clés : accessibilité aux services de santé, arthrite, réadaptation
Arthritis accounts for almost one-third of the total cost of musculoskeletal diseases in Canada, and its greatest economic burden is attributed to long-term disability.1 People living with arthritis experience pain, impaired physical function, and reduced quality of life, particularly with respect to their social, psychological, and financial well-being. More than 4.2 million Canadians live with some form of arthritis; in 2000, according to data issued by the Public Health Agency of Canada in 2010, the economic burden of this disease was estimated to be $6.4 billion in direct (hospital care, drugs, physician billing, and additional health care expenditure) and indirect (lost productivity, injury, morbidity and mortality) costs.1 Arthritis is a serious economic and health burden to our society.
There are several types of arthritic conditions. The two main types of arthritis are rheumatoid arthritis (RA) and osteoarthritis (OA). Rehabilitation services such as physical and occupational therapy are beneficial for both.1–4 People with OA are often managed by their primary care provider with pain medication and referred to physical therapy (PT) and occupational therapy (OT).1 Recommendations for assessment and treatment of RA include pharmacologic management under the supervision of a rheumatologist; referral to PT and OT should be considered for patients who have ongoing inflammation or joint damage.5 Physical and occupational therapists provide various treatments (including education, exercise instruction, joint protection, prescription of assistive devices, and introduction of self-management programmes) that are beneficial to people with arthritis.2–4 The main goals of PT and OT intervention are to decrease pain, prevent deformity, preserve or improve function, and promote participation in activities of daily living (ADL) as well as both vocational and leisure activities.6–8 The effectiveness of PT and OT interventions has been demonstrated;8–10 however, access to services is limited.11,12 This is especially problematic in view of the increasing prevalence of chronic arthritis and the economic burden associated with these disabling diseases.1
Although they did not document actual wait times to receive services, Beatty and colleagues reported that of the 32.2% of patients with arthritis (RA or OA) who felt they needed rehabilitation services (including PT, OT, and assistive devices), only 58.3% actually received these services.11 Another study reported similar results: of the 39% of patients with arthritis (RA or OA) who felt they needed rehabilitation services, including PT and OT, only 61% received them.12
Patient-related factors may be associated with use of PT and OT. For example, Sadhu and colleagues found that RA patients with lower socio-economic status (SES) received less allied health care (including PT and OT) than patients with higher SES.13 Greater severity and longer duration of the condition, as well as insurance status and ability to pay for services, were associated with referral to PT for patients with spine disorders.14
In Quebec, medical care is delivered in the context of a publicly funded health care system, but PT and OT services are covered by the provincial health insurance plan only when delivered by hospitals, rehabilitation centres, and community health centres (which offer care to homebound people). It has been reported that in Ontario, most physiotherapists and some occupational therapists work in private clinics15 where patients either pay out of pocket for services or have supplemental insurance (often offered by their employer) that covers a certain number of therapy sessions.
PT and OT play an important role in preventing and managing symptoms associated with OA and RA, and these interventions can potentially keep people independent longer by promoting activity and participation through a wide variety of treatments.16,17 With more people requiring arthritis care,18 the demands on PT and OT will undoubtedly increase. Further, the availability of publicly ensured PT and OT services (in this case, those covered by the provincial universal health insurance board, the Régie de l'assurance maladie du Québec or RAMQ) has decreased in Canada over the past two decades, presenting barriers to access especially for those who do not have supplementary health insurance.19
The main goals of our study were to document wait times from referral by physician to consultation in PT or OT in the public system for people with arthritis and to explore whether these wait times differed depending on diagnosis (RA vs. OA), service provider (hospital vs. community health centre vs. rehabilitation centre), and geographic area (cities with a school of rehabilitation vs. the rest of the province). We also described any methods of prioritization used in providing appointments.
Methods
Our cross-sectional study took place in Quebec, Canada. To determine the wait time from referral by a physician to PT or OT consultation, we developed two referral scenarios with input from two physiotherapists, two occupational therapists, two rheumatologists, and two family physicians. The referral scenarios, based on a 55-year-old woman, were created to be as realistic as possible:
Diagnosed RA: “55-year-old female with RA suffering from severe pain and swelling of hands and feet. Morning stiffness of 1 hour. ESR (erythrocyte sedimentation rate): 22, CRP (C-reactive protein): 30, RF (rheumatoid factor): 68. Please assess.”
Diagnosed OA: “55-year-old female with OA suffering from chronic pain in right knee ×5 years, no swelling. Please assess.”
The scenarios were used to request appointments for PT and OT consultation in all publicly accessible (non-private) PT and OT hospital-based departments, community health centres, and rehabilitation centres in Quebec. Wait times were calculated as the number of days between the initial request and the appointment date given (PT or OT) and were further categorized into five groups: within 6 months, 6–12 months, >12 months, refused, and evaluation appointment.
A single research assistant contacted all service providers in our sample between April 2010 and June 2010 to request an appointment based on the referral scenarios. There are two potential ways for a referring physician to arrange a rehabilitation consultation in Quebec: either the referring doctor's office calls to arrange the appointment or sends a referral letter by fax or by mail; or the referring doctor may give the referral letter to the patient and ask him or her to call to arrange the appointment (with the understanding that the patient will bring the referral sheet on the day of the appointment). For our study, the research assistant called each service provider, assuming the role of a patient with one of the prepared referral scenarios. The two scenarios were used in random order, determined by flipping a coin, over a period of 3 months. A standardized script was used to request the appointment while also obtaining information about the type of service provider (hospital, community health centre, or rehabilitation centre). When the research assistant could not provide certain information (valid health insurance number, local address, local telephone number) or, in some cases, when an appointment date was not given over the telephone (i.e., if the receptionist said that the “patient” would be called back with an appointment date or that the office needed to receive the referral before booking an appointment), the research assistant inquired about the estimated wait time and the steps required to obtain an appointment. If she succeeded in booking an appointment, it was subsequently cancelled within 24 hours.
Descriptive statistics were used to examine the wait times by diagnosis, service provider, and geographic area. Inferential statistics (chi-square tests) were also used, with the level of significance set at p<0.05. The administrative regions containing a school of rehabilitation with both PT and OT programmes were Montreal, Estrie (Sherbrooke), and Capitale-National (Quebec City).
Ethics approval was obtained from the Université de Montréal and McGill University.
Results
Of the 100 public PT and OT service providers serving the adult outpatient population of Quebec, 12% are hospital teaching centres, 74% are community health centres (i.e., community hospitals or Health and Social Service Centres, CSSS) and 14% are rehabilitation centres for people with physical impairments and disabilities. Approximately one-fifth (21%) of these service providers are located in the administrative region of Montreal, the largest city in the province and home to two schools of rehabilitation (at McGill University and Université de Montréal).
For both scenarios (OA and RA) combined, 13% of calls resulted in an appointment within 6 months, 13% within 6–12 months, and 24% within >12 months; in 22% of cases, services were refused (see Figure 1). In the remaining 28% of cases, the research assistant was told that she would require an evaluation appointment for functional assessment before being given an appointment. Reasons given for refusal of services were that the service provider accepted only patients referred internally by their institution (36%); accepted only postoperative or trauma patients (27%); did not accept clients with a diagnosis of RA or OA (18%); was not accepting new patients at the time the request was made (10%); or accepted only patients aged ≥65 years (9%). When an appointment was refused or a long wait time was given, the receptionist often suggested that the “patient” seek private PT and OT services.
Figure 1.
Wait-time responses for rehabilitation services in Quebec
<6 mo=appointment scheduled within 6 months; 6–12 mo=appointment scheduled within 6–12 months; >12 mo=told to wait more than 12 months for an appointment; Refused=services refused; Evaluation=evaluation based on a functional assessment before an appointment could be given.
There was no difference between RA and OA diagnoses in terms of ability to obtain an appointment by phone. However, 28% of service providers offered an evaluation appointment regardless of diagnosis, which implies some type of screening or prioritization based on functional assessment as opposed to diagnosis. The wait time would therefore depend on the patient's need and would be prioritized accordingly at each service provider's discretion. When we looked at service providers who required an evaluation appointment before beginning services, we found a statistically significant difference (p=0.006) between cities with a school of rehabilitation (10%; 95% CI, 0.09–0.11) and the rest of the province (36%; 95% CI, 0.32–0.40). The majority of evaluation appointments were in community health centres (82%, p=0.07). In addition, 70 of the 100 service providers required that the referral be sent for their review before the initial consultation, regardless of the evaluation appointment.
Of the 50 service providers who gave an indication of the expected wait time, 26% offered an appointment within 6 months, 26% offered an appointment within 6–12 months, and 48% predicted a wait of >12 months. Neither diagnosis (RA vs. OA) nor type of service provider was associated with getting an earlier appointment (see Table 1). However, none of the rehabilitation centres provided an appointment within 6 months for either the RA or the OA case scenarios, whereas 13 (15%) of the 86 other PT and OT departments did so.
Table 1.
Variables Associated with Obtaining an Appointment for Physical or Occupational Therapy within 6 Months
| No. (%) |
|||
|---|---|---|---|
| Variable | <6 mo | >6 mo | p-value |
| Diagnosis | |||
| RA | 13 (26) | 37 (74) | 1.00 |
| OA | 13 (26) | 37 (74) | |
| Type of centre | |||
| Hospital | 2 (29) | 5 (71) | 0.46 |
| CHC | 11 (28) | 28 (72) | |
| Rehabilitation | 0 (0) | 4 (100) | |
| Region | |||
| Academic cities | 4 (27) | 11 (73) | 0.94 |
| Rest of the province | 9 (26) | 26 (74) | |
RA=rheumatoid arthritis; OA=osteoarthritis; CHC=community health centre.
Discussion
Improving access to health services and decreasing wait times is a priority for many governments, including Canada's. Our study found problems with access to public PT and OT services for people with arthritis (RA and OA)—specifically, long wait times and unavailability of services for this population in more than 20% of cases. Feldman and colleagues, who conducted interviews directly with patients, found that 96% of patients who felt they needed rehabilitation services received these services; however, only 26.1% of their sample perceived a need for rehabilitation services.20 Our study was based on hypothetical scenarios of patients who were presumably referred to PT and OT because of their physician's assessment of need, yet only 26% were given an appointment within 12 months of referral.
Our findings are consistent with the results of a qualitative study in Quebec that assessed therapists' perceptions regarding barriers to and facilitators of access to PT and OT for people with RA. Therapists noted that access to publicly available programmes was very limited,19 which forced patients to either pay for private services or go without. This underscores the effect of socio-economic status on access to PT and OT. In fact, the therapists believed that in many cases physicians do not even initiate a referral because they are well aware that the patient will be unable to access a therapist.19 People with higher levels of education are also more likely to perceive the need for therapy services,20–24 which may indicate increased knowledge about potential benefits.
Sandhu and colleagues have suggested that low referral rates to rehabilitation may be driven by a lack of understanding of the roles of PT and OT.25 Based on the reasons given for refusing to book an appointment, our data suggest that service providers or their administrators perceive a greater PT and OT need for patients with acute conditions (e.g., postoperative conditions, traumas, fractures, or recent hospital admissions) and older people. This conclusion is consistent Passalent and colleagues' finding that arthritis is categorized as a chronic condition and is therefore less prioritized in rehabilitation services.15 Therefore, developing patient, physician, and therapist awareness of the importance and benefits of early access to PT and OT care is extremely important. Campaigns such as the widespread effort to improve joint-replacement outcomes26 (a priority area in Quebec, as in the rest of Canada) actually have the potential to drain resources from other patient groups in need, including people living with chronic arthritis.
The excessive wait times for rehabilitation services revealed in our study reflect a need to re-evaluate supply and demand, as well as the role of therapists as leaders in prevention and education for people with rheumatic conditions. Adequate organization of publicly and privately accessible services is even more crucial, given that staff shortages in both OT27 and PT28 have been identified in the literature. Although not all public rehabilitation service providers appeared to have a formal triage system in place, more than one-quarter of those we contacted required evaluation appointments for new patients. The majority of these service providers were in the community health centre setting, which may indicate a need for prioritization in this setting, given the increasing demands for PT and OT. These evaluation appointments serve as a form of triage, both to determine the needs of each patient and to allow therapists to give patients some basic education about their condition.
We found no difference between RA and OA diagnoses when requesting an appointment by phone, nor any association between obtaining an earlier appointment and type of service provider.
Limitations
A limitation of our study was the inability to provide the personal details required by some departments, which might have expedited the initial consultation process and given us more accurate data on wait times for each scenario. In these cases, as mentioned above, we were still able to obtain an estimated wait time for the appointment date from the receptionist, but we do not know how valid these estimates were or how an evaluation appointment would have affected the wait time. Another limitation is that our study addressed only one method of obtaining PT or OT services; appointments initiated by physicians' offices might have yielded a faster response and shorter wait times than patient-initiated calls. In many community-based centres, however, the patient is required to initiate the process. Finally, our study was not able to account for differences in wait times between PT and OT, as wait times were calculated as the time between the initial request and the appointment date received, irrespective of whether the appointment was for PT or OT. Although the OA case is more likely to fall within the scope of practice of physiotherapists, and the RA case to fall within the scope of practice of occupational therapists, both patients could have benefited from the expertise of both professionals.
Conclusion
Arthritis is the leading cause of pain and physical disability in Canada and has become a major public-health challenge and economic burden.1 Because PT and OT interventions can optimize function and increase participation, we need to focus on developing strategies to ensure that referrals are completed and appointments are obtained rapidly and easily. One potential strategy is to develop a standardized model of prioritization or guidelines to ensure the timely provision of appointments. Moreover, given that people with arthritis are not always receiving prompt rehabilitation services, rehabilitation professionals can implement management strategies to decrease the impact of arthritis through education, awareness, and self-management programmes.1 Evaluating service delivery is also extremely important, as therapist shortages could be further exacerbated by the organization of these services.28
Key Messages
What is already known on this topic
Arthritis is the leading cause of pain and disability in Canada and a major public-health challenge. People with arthritis should have timely access to services in order to begin appropriate treatment and optimize health outcomes. PT and OT are beneficial for both chronic osteoarthritis and inflammatory arthritis.
What this study adds
Our findings suggest that most people with arthritis living in the province of Quebec are not receiving timely PT or OT intervention through publicly funded service providers; those requiring these services must either wait or access private services. Improved triage methods and better resource allocation are needed to optimize function and participation for this population.
Physiotherapy Canada 2013; 65(3);238–243; doi:10.3138/ptc.2011-62
References
- 1.Public Health Agency of Canada, editors; Arthritis Consumer Experts, editors; Arthritis Community Research and Evaluation Unit, editors. Life with arthritis in Canada: a personal and public health challenge. Ottawa: The Agency; 2010. [cited 2011 Feb]. Available from: http://www.phac-aspc.gc.ca/cd-mc/arthritis-arthrite/lwaic-vaaac-10/pdf/arthritis-2010-eng.pdf. [Google Scholar]
- 2.Glazier RH, Dalby DM, Badley EM, et al. Management of the early and late presentations of rheumatoid arthritis: a survey of Ontario primary care physicians. CMAJ. 1996;155(6):679–87. Medline:8823213. [PMC free article] [PubMed] [Google Scholar]
- 3.Hochberg MC, Altman RD, Brandt KD, et al. American College of Rheumatology. Guidelines for the medical management of osteoarthritis. Part II. Osteoarthritis of the knee. Arthritis Rheum. 1995;38(11):1541–6. doi: 10.1002/art.1780381104. http://dx.doi.org/10.1002/art.1780381104. Medline:7488273. [DOI] [PubMed] [Google Scholar]
- 4.American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. Arthritis Rheum. 2000;43(9):1905–15. doi: 10.1002/1529-0131(200009)43:9<1905::AID-ANR1>3.0.CO;2-P. http://dx.doi.org/10.1002/1529-0131(200009)43:9<1905::AID-ANR1>3.0.CO;2-P. Medline:11014340. [DOI] [PubMed] [Google Scholar]
- 5.British Columbia Ministry of Health. Rheumatoid arthritis: diagnosis and management. 2006. [cited 2011 Feb]. Available from: http://www.bcguidelines.ca/guideline_osteoarthritis.html.
- 6.Fransen M, Crosbie J, Edmonds J. Physical therapy is effective for patients with osteoarthritis of the knee: a randomized controlled clinical trial. J Rheumatol. 2001;28(1):156–64. Medline:11196518. [PubMed] [Google Scholar]
- 7.Hammond A, Young A, Kidao R. A randomised controlled trial of occupational therapy for people with early rheumatoid arthritis. Ann Rheum Dis. 2004;63(1):23–30. doi: 10.1136/ard.2002.001511. http://dx.doi.org/10.1136/ard.2002.001511. Medline:14672887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li LC, Iversen MD. Outcomes of patients with rheumatoid arthritis receiving rehabilitation. Curr Opin Rheumatol. 2005;17(2):172–6. doi: 10.1097/01.bor.0000151401.11028.88. http://dx.doi.org/10.1097/01.bor.0000151401.11028.88. Medline:15711231. [DOI] [PubMed] [Google Scholar]
- 9.Buckwalter JA, Stanish WD, Rosier RN, et al. The increasing need for nonoperative treatment of patients with osteoarthritis. Clin Orthop Relat Res. 2001;385(385):36–45. doi: 10.1097/00003086-200104000-00008. http://dx.doi.org/10.1097/00003086-200104000-00008. Medline:11302324. [DOI] [PubMed] [Google Scholar]
- 10.Lineker SC, Bell MJ, Wilkins AL, et al. Improvements following short term home based physical therapy are maintained at one year in people with moderate to severe rheumatoid arthritis. J Rheumatol. 2001;28(1):165–8. Medline:11196519. [PubMed] [Google Scholar]
- 11.Beatty PW, Hagglund KJ, Neri MT, et al. Access to health care services among people with chronic or disabling conditions: patterns and predictors. Arch Phys Med Rehabil. 2003;84(10):1417–25. doi: 10.1016/s0003-9993(03)00268-5. http://dx.doi.org/10.1016/S0003-9993(03)00268-5. Medline:14586907. [DOI] [PubMed] [Google Scholar]
- 12.Hagglund KJ, Clark MJ, Hilton SA, et al. Access to healthcare services among persons with osteoarthritis and rheumatoid arthritis. Am J Phys Med Rehabil. 2005;84(9):702–11. doi: 10.1097/01.phm.0000167618.84726.33. http://dx.doi.org/10.1097/01.phm.0000167618.84726.33. Medline:16141749. [DOI] [PubMed] [Google Scholar]
- 13.Berkanovic E, Hurwicz ML. Rheumatoid arthritis and comorbidity. J Rheumatol. 1990;17(7):888–92. Medline:2213754. [PubMed] [Google Scholar]
- 14.Aletaha D, Neogi T, Silman AJ, et al. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62(9):2569–81. doi: 10.1002/art.27584. http://dx.doi.org/10.1002/art.27584. Medline:20872595. [DOI] [PubMed] [Google Scholar]
- 15.Passalent LA, Landry MD, Cott CA. Wait times for publicly funded outpatient and community physiotherapy and occupational therapy services: implications for the increasing number of persons with chronic conditions in ontario, Canada. Physiother Can. 2009;61(1):5–14. doi: 10.3138/physio.61.1.5. http://dx.doi.org/10.3138/physio.61.1.5. Medline:20145747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.European Bone and Joint Health Strategies Project. European action towards better musculoskeletal health: a public health strategy to reduce the burden of musculoskeletal conditions. Lund (Sweden): The Bone and Joint Decade, Department of Orthopedics, University Hospital; 2004. [cited 2011 Feb]. Available from: http://ec.europa.eu/health/ph_projects/2000/promotion/fp_promotion_2000_frep_15_en.pdf. [Google Scholar]
- 17.Bartlett SJBC, Maricic MJ, Iversen MD, et al. Clinical care in the rheumatic diseases. 3rd ed. Atlanta: Association of Rheumatology Health Professionals, American College of Rheumatology; 2006. [Google Scholar]
- 18.Arthritis Alliance of Canada. The impact of arthritis in Canada: today and over the next 30 years. The Alliance; 2011. [cited 2011 Feb]. Available from: http://www.arthritisalliance.ca/docs/20111022_2200_impact_of_arthritis.pdf. [Google Scholar]
- 19.Bernatsky S, Feldman D, De Civita M, et al. Optimal care for rheumatoid arthritis: a focus group study. Clin Rheumatol. 2010;29(6):645–57. doi: 10.1007/s10067-010-1383-9. http://dx.doi.org/10.1007/s10067-010-1383-9. Medline:20127397. [DOI] [PubMed] [Google Scholar]
- 20.Feldman DE, Bernatsky S, Lévesque JF, et al. Access and perceived need for physical and occupational therapy in chronic arthritis. Disabil Rehabil. 2010;32(22):1827–32. doi: 10.3109/09638281003734417. http://dx.doi.org/10.3109/09638281003734417. Medline:20345251. [DOI] [PubMed] [Google Scholar]
- 21.Freburger JK, Carey TS, Holmes GM. Physician referrals to physical therapists for the treatment of spine disorders. Spine J. 2005;5(5):530–41. doi: 10.1016/j.spinee.2005.03.008. http://dx.doi.org/10.1016/j.spinee.2005.03.008. Medline:16153582. [DOI] [PubMed] [Google Scholar]
- 22.Freburger JK, Carey TS, Holmes GM. Management of back and neck pain: who seeks care from physical therapists? Phys Ther. 2005;85(9):872–86. Medline:16117598. [PubMed] [Google Scholar]
- 23.Jacobi CE, Mol GD, Boshuizen HC, et al. Impact of socioeconomic status on the course of rheumatoid arthritis and on related use of health care services. Arthritis Rheum. 2003;49(4):567–73. doi: 10.1002/art.11200. http://dx.doi.org/10.1002/art.11200. Medline:12910565. [DOI] [PubMed] [Google Scholar]
- 24.Jacobi CE, Triemstra M, Rupp I, et al. Health care utilization among rheumatoid arthritis patients referred to a rheumatology center: unequal needs, unequal care? Arthritis Rheum. 2001;45(4):324–30. doi: 10.1002/1529-0131(200108)45:4<324::AID-ART344>3.0.CO;2-1. http://dx.doi.org/10.1002/1529-0131(200108)45:4<324::AID-ART344>3.0.CO;2-1. Medline:11501719. [DOI] [PubMed] [Google Scholar]
- 25.Sandhu RS, Treharne GJ, Justice EA, et al. West Midlands Rheumatology Services and Training Committee. Accessibility and quality of secondary care rheumatology services for people with inflammatory arthritis: a regional survey. Clin Med. 2007;7(6):579–84. doi: 10.7861/clinmedicine.7-6-579. http://dx.doi.org/10.7861/clinmedicine.7-6-579. Medline:18193705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Health Canada. First minister's meeting on the future of health care 2004—A 10-year plan to strengthen health care. Ottawa: Health Canada; 2004. [cited 2011 Jun 6]. Available from: http://www.hc-sc.gc.ca/hcs-sss/delivery-prestation/fptcollab/2004-fmm-rpm/index-eng.php. [Google Scholar]
- 27.von Zweck C. The occupational therapy workforce in Canada: a review of available data. Occup Ther Now. 2008;10(2):3–6. [Google Scholar]
- 28.Québec, Ministère de la santé et des services sociaux. Document de consultation. The Ministry; 2006. [cited 2011 Nov]. Garantir l'accès: un défi d'équité, d'efficience et de qualité. Available from: http://publications.msss.gouv.qc.ca/acrobat/f/documentation/2005/05-721-01.pdf. [Google Scholar]