Summary
Burn care providers are usually challenged by multiple complications during the management of acute burns. One of the most common complications worldwide is renal failure. This article reviews the various aspects of renal failure management in burn patients. Two different types of renal failures develop in these patients. The different aetiological factors, incidence, suspected prognosis, ways of diagnosing, as well as prevention methods, and the most accepted treatment modalities are all discussed. A good understanding and an effective assessment of the problem help to reduce both morbidity and mortality in burn management.
Keywords: burn, renal failure, nephrotoxic
Abstract
Tous ceux qui s’occupent de soigner les patients brûlés doivent affronter le problème des nombreuses complications qui se présentent au cours de la gestion des brûlures graves. Une des complications les plus courantes dans tout le monde est l’insuffisance rénale. Cet article passe en revue les différents aspects de la gestion de l’insuffisance rénale chez les patients brûlés. Il y a deux types d’insuffisance rénales qui se développent dans cette catégorie des patients. Les Auteurs considèrent les divers facteurs étiologiques, l’incidence, les pronostics et les moyens de diagnostic, ainsi que des méthodes de prévention et les modalités de traitement les plus acceptées. Une bonne compréhension et une évaluation efficace du problème aident à réduire la morbidité et la mortalité dans la gestion des brûlures.
Introduction
Acute renal failure is one of the major complications of burns and it is accompanied by a high mortality rate. Most renal failures occur either immediately after the injury or at a later period when sepsis develops. Owing to recent advances in cardiovascular management, acute renal failure has become a much less frequent complication than in the past; renal failure itself is no longer life-threatening because haemodialysis is available. Late-onset renal failure is usually the consequence of sepsis and is often associated with other organ failure. Two major mechanisms are involved in the pathophysiological changes in the kidney: filtration failure and tubular dysfunction caused by various factors and interacting with each other.1
The renal failure that occurs in extensively burned patients is usually associated with failure or dysfunction of other organs in a form of multiple organ dysfunction syndrome which adversely influences the prognosis. Acute renal failure occurring immediately after burns is mostly due to reduced cardiac output, which is mainly caused by fluid loss. This is usually caused by delayed or inadequate fluid resuscitation but may also result from substantial muscle breakdown or haemolysis. It is usually reversible.2
Reduced urine output despite adequate fluid administration is usually the first sign of acute renal failure. This will be followed by a rise in serum creatinine and urea concentrations. Early renal support (haemodialysis or haemofiltration) will control serum electrolytes and accommodate the large volumes of nutritional supplementation required in a major burn.3
Causes
Fluid shift and hypovolaemia
Increased vascular permeability causes extensive fluid shift manifested as both local and generalized oedema. This results in hypovolaemia and centralization of circulation, inducing oliguria early after burns. Sodium retention in collagen fibres and sodium-potassium pump impairment also participate in giving rise to generalized oedema. Excess free water given in this period lowers the tonicity of plasma, which also results in renal oedema, followed by acute renal failure.4
Myocardial depression
Besides the decrease in circulatory volume and plasma tonicity, myocardial depression due to a presumed myocardial depressant factor, tumour necrosis factor and/or oxygen free radicals, causes a reduction of renal flow and is followed by tubular necrosis.5
Stress-related hormones
Burn stress and the associated circulatory derangement induce elevated levels of catecholamines, angiotensin II, aldosterone, and vasopressin. These hormonal changes cause vasoconstriction and fluid retention as well as alteration of regional blood flow, especially in the kidney. On the other hand, plasma atrial natriuretic polypeptide (ANP) levels are elevated for sustained periods after burns. ANP counterbalances the actions of the stress-related hormones through vasodilatation and natriuresis. Excessively high levels of stress-related hormones and/or impairment of ANP secretion may participate in reducing renal function.6
Inflammatory mediators
Many mediators, including cytokines (TNF, IL-1, etc.), eicosanoids (prostaglandins [PGs], thromboxane, leukotrienes), and platelet-aggregating (activating) factor (PAF) are produced or released in the early post-burn period. They act variably to increase vascular permeability and to induce tissue damage. These mediators are also involved in the development of disseminated intravascular coagulation, in which microthrombi are formed in the capillaries of the glomeruli and renal tubule. Vasodilator PGE2 is a specific PG in the kidney and works to counteract the above vasoconstrictor substances, but its production is inhibited in the early phase of burns. Similar inflammatory changes occur when a burn patient develops sepsis in the late period.7
Nephrotoxic agents
Antibiotics, such as aminoglycoside and certain cephalosporins, are known to be nephrotoxic. Acute or chronic intoxication with alcohol, barbiturates, chlorpromazine, toluene, and paint thinner have been reported as possible associated agents inducing renal failure in burn patients. In some of these patients, early resuscitation therapy was delayed.8
Denaturated proteins (pigmenturia)
Free haemoglobin released from degraded red blood cells by heat is conjugated by haptoglobin and transferred to the liver. When a large amount of free haemoglobin is produced in extensive third-degree burns, unconjugated free haemoglobin passes through the glomeruli and is excreted in the urine. This may cause degenerative changes in the tubular cells, occlusion of the renal tubules by the formation of haemoglobin casts, and eventually renal failure, especially when combined with dehydration, acidosis, shock, or endotoxaemia. The free haemoglobin absorbed by tubular epithelium is degraded into globin and haem; the latter may induce tubular damage by generating oxygen free radicals via iron ions.9
Increased serum myoglobin has also been reported in patients with destroyed muscles in deep thermal injury, electrical injury, distal ischaemia due to persistent hypotension or sustained compression, high fever, and drug-induced myolysis. These proteins can be aetiological factors of acute renal failure in the first one or two days after injury.10
Respiratory dysfunction
Associated respiratory dysfunction adversely affects renal function because of reduced oxygen supply to the kidney. Reduced cardiac output caused by mechanical ventilation with continuous positive airway pressure modes decreases renal blood flow.11
Incidence
Ten to thirty per cent of burn patients are reported to suffer from renal failure, depending on the criteria used to define renal failure and on the patient population. Generally, the more severely burned the patients are, the higher the incidence of renal failure.12
Prognosis
The prognosis of burn patients with acute renal failure is usually unfavourable. Mortality rates of 73-100% have been reported.13 In patients in whom serum creatinine increased to a level greater than 1.5 mg/dl above initial values in the absence of shock, the mortality rate was 72.7%, which was much higher than among patients without renal dysfunction (16.6%).14
Diagnosis
Urinary output is the key parameter in evaluating both renal function and the patient’s circulatory state. Generally, a urine volume of 0.8-1.0 ml/kg/h reflects adequate perfusion pressure. In an oliguric state, however, it must be determined whether the reduced urine volume is due to functional renal (or pre-renal) failure or to organic (or renal) failure. Prolonged functional renal failure is often observed before organic failure develops. In non-oliguric renal failure, urine volume is of no value in the diagnosis. Urine and serum osmolality and electrolyte concentrations are useful in the differential diagnosis.5
Prevention
Circulatory stabilization
Adequate fluid therapy is crucial in maintaining renal function. Monitoring by urine output or Swan-Ganz catheterization and thermodilution cardiac output determination is useful in the circulatory management of severely burned patients. Albumin infusion increases plasma volume by 37% and normalizes elevated basal levels of aldosterone and plasma renin activity.15
Monitoring renal function
Early diagnosis of renal failure is very important. To evaluate renal failure, monitoring of glomerular and tubular functions, of persistent proteinuria, and of urinary tubule enzymes is recommended in addition to taking measurements of urine volume, blood urea nitrogen, and serum creatinine.16
Creatinine clearance reflects the glomerular filtration rate (GFR), and is useful in evaluating the prognosis in renal dysfunction. Increased serum concentrations of B2- microglobulin reflect a decreased GFR. Free water clearance (CH2O) is a useful parameter for the early diagnosis of renal failure. CH2O falls to nearly zero before organic renal failure is established.16
Glomerular dysfunction is associated with increased renal excretion of higher molecular weight proteins, and tubular dysfunction is associated with increased excretion of lower molecular weight proteins (<60000 Daltons) due to tubular impairment of reabsorption and/or degradation of these proteins. In some burn patients, a transient glomerular lesion may cause albuminuria immediately after the burn, followed by increased excretion of higher molecular weight proteins, such as α1-acid glycoprotein, α1-antichymotrypsin, and γ-glutamyltransferase (GT), around 5 days after the burn. There is no correlation, however, between proteinuria and the development of renal dysfunction. 17
Haptoglobin administration
Haptoglobin combines specifically with free haemoglobin, forming a conjugate, which is metabolized in the liver. In extensive third-degree burns, haptoglobin administration is useful in preventing or decreasing haemoglobinuria. It was approved for clinical use in Japan in 1985. Haptoglobin preparations must be administered immediately after burns when haemoglobulinaemia is anticipated or trace haemoglobulinaemia is detected. Alkalinizing urine by administering sodium bicarbonate and increasing urine output by massive fluid loading or diuretics prevent haemoglobin precipitation in the tubules, but may not prevent the possible toxic effects of haemoglobin on tubular cells.1
Other measures to prevent renal failure
Correction of hypoxia and acidosis are important measures in preventing the development of renal failure. Anticoagulation therapy, such as antithrombin III and heparin, is indicated in the hypercoagulatory state. More importantly, early excision of deep second- and third-degree burns followed by immediate grafting decreases the incidence of renal failure, which develops in sepsis.18
Management
Fluid balance
If haemodialysis is not indicated, it is necessary to determine urine volume, insensible water loss, and gastrointestinal fluid loss. Fluid overload should be avoided in order to prevent pulmonary oedema and heart failure. In burn patients with extensive raw surfaces, fluid loss through the wound is not accurately assessed. Central venous pressure and/or pulmonary capillary wedge pressure monitoring is recommended.5
Diuretics
Diuretics are indicated in pre-renal oliguria but not in established organic renal failure. Intravenous furosemide (20-80 mg/day) is given to maintain urine output when oliguria continues in spite of adequate fluid replacement.19
Management of hyperkalaemia
Serum potassium levels above 6.0 mEq/l and/or abnormal ECG (tenting of the T wave, flattening of the P wave, and widened QRS complex) are indications of the need for immediate treatment. Intravenous administration of 500 ml of 10% dextrose with 1-20 units of regular insulin will lower the serum potassium level by approximately 2mEq/l.12
Haemodialysis
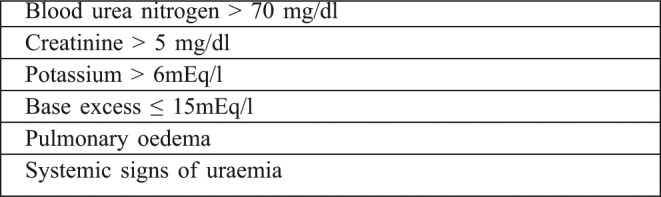
Early and frequent haemodialysis (HD) is recommended. The criteria for the introduction of HD to treat acute renal failure in burn patients are listed in Table I. Although HD is most effective in the management of renal failure, it is sometimes difficult to ensure stable circulation. Also, in extensive burns, bleeding through wounds may be a problem due to owing to the use of anticoagulants. In hypotensive patients, albumin or blood should be transfused prior to HD. To remove excess water and circulating toxic substances other than creatinine and urea, continuous haemofiltration can be combined with HD.20
Table I. Criteria for haemodialysis.
Nutritional support
In burn patients, energy requirements are high, and adequate nutritional support is critical to the outcome. Renal failure itself does not increase the metabolic rate, but the stress causing renal failure may induce a hypermetabolic state.5
Conclusion
There are many reasons for believing that the survivors of moderate and serious burn injuries received appropriate management with general condition monitoring and support, in addition to local burn wound care. Renal failure as a common complication with deleterious consequences is one of the most important issues in burn management. In this systematic review, we highlighted the magnitude of the problem together with possible methods of prevention and treatment. In burn victims, if renal failure is effectively predicted and promptly managed, there will be a significant reduction in morbidity and overall mortality, especially in severe burn injuries.
References
- 1.Aikawa J, Wakabayashi G, Ueda M, et al. Regulation of renal function in thermal injury. J Trauma. 1990;30:174–8. doi: 10.1097/00005373-199012001-00035. [DOI] [PubMed] [Google Scholar]
- 2.Pruitt B. Protection from excessive resuscitation: Pushing the pendulum back. J Trauma. 2000;49:567–73. doi: 10.1097/00005373-200009000-00030. [DOI] [PubMed] [Google Scholar]
- 3.Ansermino M, Hemsley C. Intensive care management and control of infection in burned patients. BMJ. 2004;329:220–3. doi: 10.1136/bmj.329.7459.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hauben D. Invited comment on acute renal failure in burned patients. Burns. 1988;14:113–4. doi: 10.1016/0305-4179(88)90214-8. [DOI] [PubMed] [Google Scholar]
- 5. Herndon, D , editor. “Total Burn Care”. (ed.) W.B. Saunders; London: 2003. Renal failure in burn patients. pp. 393–8. [Google Scholar]
- 6.Sharar S, Heimbach D, Green M, et al. Effects of body surface thermal injury on apparent renal and cutaneous blood flow in goats. J Burn Care Rehabil. 1988;9:26–31. doi: 10.1097/00004630-198801000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Kowal-Vern A, Walenga J, Sharp-Pucci M, et al. Postburn edema and related changes in interleukin-2, leukocytes, platelet activation, endothelin-1, and C1 esterase inhibitor. J Burn Care Rehabil. 1997;18:99–102. doi: 10.1097/00004630-199703000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Sawada Y, Momma S, Takamizawa A, et al. Survival from acute renal failure after severe burns. Burns. 1994;11:143–7. doi: 10.1016/0305-4179(84)90139-6. [DOI] [PubMed] [Google Scholar]
- 9.Yoshioka T, Sugimoto T, Ukai T, et al. Haptoglobin therapy for possible prevention of renal failure following thermal injury: A clinical study. J Trauma. 1985;25:281–7. doi: 10.1097/00005373-198504000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Cynober l, Guechot J, Bétourné C, et al. Rhabdomyolysis and acute renal failure in a patient with thermal injury. Int Care Med. 1986;12:159–60. doi: 10.1007/BF00254933. [DOI] [PubMed] [Google Scholar]
- 11.Bulger E, Jurkovich G, Gentilello L, et al. Current clinical options for the treatment and management of acute respiratory distress syndrome. J Trauma. 2000;48:562–72. doi: 10.1097/00005373-200003000-00037. [DOI] [PubMed] [Google Scholar]
- 12.Holm C, Holbrand E, von Donnersmarck G, et al. Acute renal failure in severely burned patients. Burns. 1999;25:171–8. doi: 10.1016/s0305-4179(98)00144-2. [DOI] [PubMed] [Google Scholar]
- 13.Schiavon M, Dilandro D, Baldo M, et al. A study of renal damage in seriously burned patients. Burns. 1988;14:107–14. doi: 10.1016/0305-4179(88)90213-6. [DOI] [PubMed] [Google Scholar]
- 14.Chrysopoulo M, Jeschke M, Dziewulski P, et al. Acute renal dysfunction in severely burned adults. J Trauma. 1999;46:141–4. doi: 10.1097/00005373-199901000-00024. [DOI] [PubMed] [Google Scholar]
- 15.Kevin K, Juncos L, Wolf S, et al. Continuous renal replacement therapy improves survival in severely burned military casualties with acute kidney injury. J Trauma. 2008;64:S179–87. doi: 10.1097/TA.0b013e3181608676. [DOI] [PubMed] [Google Scholar]
- 16. Herndon, D , editor. “Total Burn Care”. (ed.) W.B. Saunders; London: 2003. A: Epidemiological, demographic, and outcome characteristics of burn injury. pp. 16–30. [Google Scholar]
- 17.Shakespeare P, Coombes E, Hambleton J, et al. Proteinuria after burn injury. Ann Clin Biochem. 1981;18:535–60. doi: 10.1177/000456328101800606. [DOI] [PubMed] [Google Scholar]
- 18.Walsh M, Miller S, Kagen L, et al. Myoglubinemia in severely burned patients: Correlation with severity and survival. J Trauma. 1982;22:6–10. [PubMed] [Google Scholar]
- 19.Belba M, Belba G. Acute renal failure in severe burns. Conclusions after analyses of deaths during 1998. Ann Burns Fire Disasters. 2000;13:124–9. [Google Scholar]
- 20.Leblanc M, Thibeault Y, Quérin S, et al. Continuous and haemodiafiltration for acute renal failure in severely burned patients. Burns. 1997;23:160–5. doi: 10.1016/s0305-4179(96)00085-x. [DOI] [PubMed] [Google Scholar]


