Summary
Skin graft expansion techniques (mesh and micrograft) are widely used, but there is ample evidence that skin graft meshers do not provide their claimed expansion rates. Although this finding might not be new for the majority of surgeons, less is known about surgeons’ actual knowledge of expansion rates. The aim of this study was to evaluate the true expansion rates of commonly used expansion techniques with regard to claimed, achieved, and polled results. In the first part of the study, 54 surgeons were polled during an annual burns meeting regarding the most commonly used expansion techniques and expansion ratios; in the second step the true (achievable) expansion rates of the most widely used meshers and micrografts were analysed; and in third step, a poll involving 40 surgeons was conducted to estimate the true expansion rates of the most frequently used skin expansion techniques. The skin meshers (1:1.5 / 1:3) did not achieve their claimed values: (1:1.5) 84.7% of the claimed expansion (mean ± SD: 1:1.27 ± 0.15) and (1:3) 53.1% of the 1:3 (1:1.59 ± 0.15) mesher. The use of the micrografting technique resulted in 99.8% of the 1:3 (1:2.99 ± 0.09), 93.6% of the 1:4 (1:3.74 ± 0.12) and 93.8% of the 1:6 (1:5.63 ± 0.12) claimed expansion rates, respectively. In general the surgeons overestimated the achievable expansion rates. In general the achieved expansion rate was lower than the estimated and claimed expansion rates. The micrografting technique provided reliable and valid expansion rates compared to the skin meshers. We recommend using the micrograft technique when large expansion ratios are required, for example in severe extensive burns.
Keywords: skin transplantation, skin graft, mesh, micrografting, Meek’s technique
Abstract
Les techniques pour l’extension des greffes cutanées (en filet ou microgreffes) sont largement utilisées, mais il est amplement prouvé que les greffes cutanées en filet ne correspondent aux taux d’expansion réclamés. Il est bien possible que cette constatation ne constitue pas rien de nouveau pour les chirurgiens, mais nous savons encore moins des connaissances réelles des chirurgiens pour ce qui concerne cette matière. Le but de cette étude était d’évaluer l’exact taux d’expansion des techniques d’expansion couramment utilisées à l’égard des résultats revendiqués, réalisés et soumis à sondage. Dans la première partie de l’étude, 54 chirurgiens ont été interrogés lors d’une réunion annuelle des brûlologues sur les techniques d’expansion les plus utilisées et les rapports d’expansion. Dans la deuxième étape, les taux effectifs d’extension (possibles) des greffes en filet et les microgreffes les plus utilisés ont été analysés. Dans la troisième étape, un sondage auprès de 40 chirurgiens a été réalisé pour évaluer les taux effectifs des techniques d’expansion cutanée les plus utilisées. Les greffes en filet évaluées (1 : 1,5 / 1:3) en effet n’atteignaient pas les valeurs revendiquées: 1:1,5 = 84,7% de l’expansion revendiquée (moyenne ± écart-type = 1:1.27 ± 0,15) et 1:3 = 53,1% du mesher 1:3 (1:1.59 ± 0,15). L’utilisation de la technique de la microgreffe a produit des taux revendiqués d’expansion de 99,8% dans le cas de 1:3 (1:2,99 ± 0,09), de 93,6% dans le cas de 1:4 (1:3,74 ± 0,12) et de 93,8% dans le cas de 1:6 (1:5.63 ± 0,12). En général, les chirurgiens ont surestimé les taux d’expansion réalisables. Ainsi, toutes choses considérées, le taux d’expansion effectivement réalisé était inférieur aux divers taux d’expansion estimés et revendiqués. Les microgreffes montraient des taux d’expansion fiables et valides par rapport aux greffes en filet. Les Auteurs recommandent l’utilisation de la technique de la microgreffe quand il faut obtenir un rapport d’expansion élevé, par exemple dans le cas de brûlures graves de grande extension.
Introduction
Skin graft expansion is widely used in plastic surgery and related fields, but there is ample evidence in the literature that mesh devices do not provide the expansion rates as advertised.1,2 While for the majority of surgeons using skin expansion devices in their daily practice this finding may be nothing new, less is known about surgeons’ actual knowledge of expansion rates. In a previous report, we considered the difference in expansion rates of the widely used 1:3 expansion device.3-5 Since there are no reports on other expansion rates (1:1.5, 1:4, 1:6, 1:9) or on the respective estimates among surgeons, we conducted the present study.
The expansion rate of skin grafts depends on the quality and sharpness of blades, surgical technique, thickness of skin grafts, elastic recoil, and the presence of residual unmeshed skin (hindering further expansion).6 After transplantation to the wound bed, meshed skin grafting resembles - at least in part - healing by secondary intention. Apart from the actual expansion ratio used, the resulting time-to-healing in vivo is related to the timing and depth of surgical debridement, wound bed quality, the microbiological environment, and associated complications.7,8
Although Meek’s technique and other related micrografting techniques9 have been around for some time, only recently has their clinical application undergone a revival. This has allowed the use of even small skin remnants, with reliable expansion ratios.10-14
In this study, we aimed to expand on previous findings and verify the expansion rates of various expansion carriers using either a mesher or a micrografting device, and to analyse the estimates of expansion rates among surgeons in a poll.
Materials and methods
As a first step we conducted a survey among 54 burn surgeons in order to evaluate the most widely used skin expansion techniques and their respective expansion ratios. Data were collected by use of an anonymous written questionnaire including staff grade, mesh and micrografting device.
In the second step of the study, we used a carrier-based mesher [(DermacarriersTM II in combination with (Zimmer, Dover, Ohia, USA)] for mesh expansion (1:1.5 and 1:3) and the Meek Micrograft Gauze (Humeca B.V., Enschede, The Netherlands) for micrograft expansion (1:3, 1:4, and 1:6). One experienced surgeon harvested skin grafts from the anterior thigh with a dermatome (Air-Dermatome, Zimmer, Dover, Ohia, USA), which was set at the 10 mark. Meshed skin graft surface area was measured before and after expansion. A total of 21 skin grafts were used per mesh expansion (1:1.5 and 1:3). Micrografting expansion rates (1:3, 1:4 and 1:6) were directly assessed on the micrografting gauzes before and after unfolding on a flat surface. The details of the micrografting technique were described in a previous work.10 A total of seven micrografting gauzes were assessed per expansion (1:3, 1:4, and 1:6). A standard SI ruler was used to measure length and width, and the surface area was calculated afterwards.
In the second survey, 40 surgeons were polled during an annual burn meeting for their estimation of expansion rates. Data collected by the use of an anonymous written questionnaire included staff grade, mesh and micrografting device used, estimation of respective expansion rates, and indications for use of either technique.
Throughout this report, the term “achieved” expansion rate refers to the technical results and “estimated” to the polling results. Claimed, achieved and estimated expansion rates are presented in a descriptive fashion below. When comparing two groups, expansion rates were analysed using the Mann-Whitney rank sum test. If more than two groups were tested, Kruskal-Wallis was followed by Dunn’s testing method for multiple comparisons. Post-testing was only performed in cases of statistical significance, and p below 0.05 was considered statistically significant (GraphPad Prism software, La Jolla, California, USA).
Results
In the first part of the study, involving 54 participants, the most used mesh expansion rate was 1:1,5 (92% of all surgeons), followed by 1:3 (82%), 1:1 (23%), 1:6 (16%), 1:4 (13%), 1:2 (10%), and 1:9 (0%); 92% of participants used carrier-based meshers; 50% of all surgeons used the Meek technique; and the most used expansion rate was 1:6 (41% of all surgeons), followed by 1:4 (38%), 1:3 (13%), and 1:9 (6%).
The achieved expansion rates of the skin meshers differed from claimed values: the 1:1.5 carrier attained a 1:1.27 ± 0.15 (± SD / 84.7%) expansion, while the 1:3 mesher attained a 1:1.59 ± 0.15 expansion, representing only 53.1% of claimed values. Unfolding of the micrografting gauzes resulted respectively in 99.8% of the 1:3 expansions (1:2.99 ± 0.09), 93.6% of the 1:4 expansions (1:3.74 ± 0.12), and 93.8% of the 1:6 expansions (1:5.63 ± 0.12) (Table I). There was a statistically significant difference between the achieved 1:3 mesh (1:1.59 ± 0.15) and the 1:3 micrografting (1:2.99 ± 0.09) expansion rates (p = 0.0001) (Table I).
Table I. Expansion rates: claimed, achieved (clinical results, grey-shaded), and estimated (polling results).
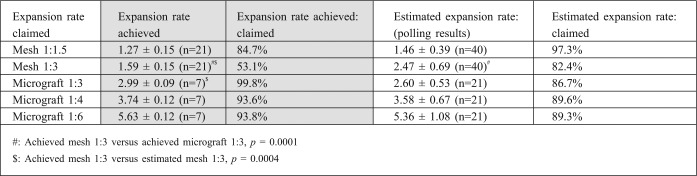
All 40 participants polled in the third part were familiar with mesh skin expansion devices. The expected mesh expansion rates represented respectively 97.3% of the 1:1.5 (1:1.46 ± 0.39) claimed values and 82.4% of those of 1:3 (1:2.47 ± 0.69). The same holds true for the estimated ratios for the micrografting technique, which represented respectively 86.7% of the 1:3 (1:2.60 ± 0.53) claimed rates, 89.6% of the 1:4 claimed rates (1:3.58 ± 0.67), and 89.3% of the 1:6 (1:5.36 ± 1.08) (Table I). The participants familiar with the MEEK technique mainly based their indication for the use of one technique or the other either on the expansion rate (12/21 = 57.1%), % TBSA (6/21 = 28.6%) or on a combination of both (3/21 = 14.3%). All participants overestimated the achievable 1:3 expansion rates by 55%, and this finding was statistically significant (p = 0.0004) (Table I).
Discussion
When comparing skin expansion rates, it is essential to exclude biasing factors resulting from surgical technique and the presenting wound bed (uneven three-dimensional surfaces, locations, debridement, wound moistness). Accordingly, only one experienced surgeon (L.P.K.) harvested skin grafts from a uniform location, and measurements were immediately performed before and after skin expansion. The initial study design contained seven measurements for each group. Owing to the differences observed between claimed and achieved expansion rates for mesh grafts, we repeated the setup in order to verify our findings on different charges of the disposable mesh carriers in two additional measurements. With previous results for mesh skin expansions confirmed, we would like to conclude by declaring that over the past two decades no technical modifications have been made1 and the mathematical predictions for the expansion rates of mesh devices have been reserved for theoretical considerations.2 This also confirmed the overestimation of the expansion rates by 55% when using the widely used 1:3 mesh device.3 Knowledge about the achievable expansion rate is important when planning an operation. Although the differences in expansion rates may be less relevant for small surface areas, they become more evident when addressing large ones. Since meshed skin grafts become even more unreliable beyond 1:6 expansions15 and achieved only 53.1% of the claimed 1:3 value in our study with 1.59 ± 0.15 expansion rates, micrografting seems to be a worthwhile alternative. This is important when we require large expansion rates since expansion with the tested micrografting technique resulted in reliable rates ranging between 86.5% and 99.8% of the claimed ratios.
Choosing the appropriate expansion device may in the future help to economize donor sites,16 and is especially important in large burns where scarce donor sites should be reserved for coverage of full-thickness regions.12 In elderly patients, donor sites should be reduced to a minimum, thus reducing the (additional) total wound surface area and the commonly associated complications in this age group.17
Our results could be useful when planning an operation involving skin graft coverage of large surface areas, with its defining of more accurate cut-off values for the use of either technique. In our clinical experience the use of micrografting delivers the best results when expansions of 1:3 and above are required.12
Only 50% of all surgeons were micrograft users: one possible explanation for this may be related to the more labour-intensive setup required for micrografting compared to the mesh technique. Our results confirm the benefits of using micrografting techniques, notably because the expansion rates achieved have been shown to be reliable, almost reflecting the claimed ratios. Nonetheless, further studies are necessary to examine contraction rates and the aesthetic long-term outcome of mesh versus micrografting techniques in the future.
Conclusion
To conclude, we would like to recall a comment made by one of the survey participants who after completion of the questionnaire described the object of the poll as a “widely known old fact”, although this knowledge may in fact not be so omnipresent after all. In general, achieved expansion rates are lower than estimated and claimed expansion rates. Micrografting yields expansion ratios close to claimed rates, unlike overestimated skin meshers. If we require large expansion rates, we should therefore opt in favour of micrografting techniques.
Acknowledgments
Conference presentations. This paper won an award for the best poster presentation at the Sixteenth Congress of the International Confederation for Plastic Reconstructive and Aesthetic Surgery (IPRAS), Vancouver, Canada, May 2011. It was also presented at the Burn Conference of the German-speaking countries (DAV), Mayrhofen, Austria, January 2013.
References
- 1.Peeters R, Hubens A. The mesh skin graft - true expansion rate. Burns. 1988;14:239–40. doi: 10.1016/0305-4179(88)90047-2. [DOI] [PubMed] [Google Scholar]
- 2.Vandeput J, Nelissen M, Tanner JC, et al. A review of skin meshers. Burns. 1995;21:364–70. doi: 10.1016/0305-4179(94)00008-5. [DOI] [PubMed] [Google Scholar]
- 3.Lumenta DB, Kamolz LP, Keck M, et al. Comparison of meshed versus Meek micrografted skin expansion rate: Claimed, achieved, and polled results. Plast Reconstr Surg. 2011;128:40–41e. doi: 10.1097/PRS.0b013e318217463a. [DOI] [PubMed] [Google Scholar]
- 4.Lumenta DB, Kamolz LP, Keck M, et al. Skin expansion rates and its results by the use of mesh and micrografting techniques. . 43rd Annual Meeting of the American Burn Association, Chicago, J Burn Care Res. 2011;32:S155. [Google Scholar]
- 5.Kamolz LP, Lumenta DB, Parvizi D. The real expansion rates of Mesh and Meek: . 31. Jahrestagung der Deutschsprachigen Arbeitsgemeinschaft für Verbrennungsbehandlung, ; Mayrhofen. 2013. www.dav2013.de. [Google Scholar]
- 6.Vandeput JJ, Tanner JC, Boswick J. Implementation of parameters in the expansion ratio of mesh skin grafts. Plast Reconstr Surg. 1997;100:653–6. doi: 10.1097/00006534-199709000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Fifer TD, Pieper D, Hawtof D. Contraction rates of meshed, nonexpanded split-thickness skin grafts versus split-thickness sheet grafts. Ann Plast Surg. 1993;31:162–3. doi: 10.1097/00000637-199308000-00015. [DOI] [PubMed] [Google Scholar]
- 8.el Hadidy M, Tesauro P, Cavallini M. Contraction and growth of deep burn wounds covered by non-meshed and meshed splitthickness skin grafts in humans. Burns. 1994;20:226–8. doi: 10.1016/0305-4179(94)90187-2. [DOI] [PubMed] [Google Scholar]
- 9.Meek CP. Microdermagrafting: The Meek Technic. Hosp Top. 1965;43:114–6. doi: 10.1080/00185868.1965.9954511. [DOI] [PubMed] [Google Scholar]
- 10.Hsieh CS, Schuong JY, Huang WS. Five years’ experience of the modified Meek technique in the management of extensive burns. Burns. 2008;34:350–4. doi: 10.1016/j.burns.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Kreis RW, Mackie DP, Vloemans AW. Widely expanded postage stamp skin grafts using a modified Meek technique in combination with an allograft overlay. Burns. 1993;19:142–5. doi: 10.1016/0305-4179(93)90038-a. [DOI] [PubMed] [Google Scholar]
- 12.Lumenta DB, Kamolz LP, Frey M. Adult burn patients with more than 60% TBSA involved-Meek and other techniques to overcome restricted skin harvest availability - the Viennese Concept. J Burn Care Res. 2009;30:231–42. doi: 10.1097/BCR.0b013e318198a2d6. [DOI] [PubMed] [Google Scholar]
- 13.Raff T, Hartmann B, Wagner H. Experience with the modified Meek technique. Acta Chir Plast. 1996;38:142–6. [PubMed] [Google Scholar]
- 14.Zermani RG, Zarabini A, Trivisonno A. Micrografting in the treatment of severely burned patients. Burns. 1997;23:604–7. doi: 10.1016/s0305-4179(97)00032-6. [DOI] [PubMed] [Google Scholar]
- 15.Kreis RW, Mackie DP, Hermans RR. Expansion techniques for skin grafts: Comparison between mesh and Meek island (sandwich-) grafts. Burns. 1994;20:S39–42. doi: 10.1016/0305-4179(94)90088-4. [DOI] [PubMed] [Google Scholar]
- 16.Erba P, Ogawa R, Vyas R. The reconstructive matrix: A new paradigm in reconstructive plastic surgery. Plast Reconstr Surg. 2010;126:492–8. doi: 10.1097/PRS.0b013e3181de232b. [DOI] [PubMed] [Google Scholar]
- 17.Keck M, Lumenta DB, Andel H. Burn treatment in the elderly. Burns. 2009;35:1071–9. doi: 10.1016/j.burns.2009.03.004. [DOI] [PubMed] [Google Scholar]


