Abstract
Purpose
Impaired consciousness in epileptic seizures has a major negative impact on patient quality of life. Prior work on epileptic unconsciousness has mainly used retrospective and nonstandardized methods. Our goal was to validate and to obtain initial data using a standardized prospective testing battery.
Methods
The responsiveness in epilepsy scale (RES) was used on 52 patients during continuous video/EEG monitoring. RES begins with higher-level questions and commands, and switches adaptively to more basic sensorimotor responses depending on patient performance. RES continues after seizures and includes postictal memory testing. Scoring was conducted based on video review.
Key Findings
Testing on standardized seizure simulations yielded good intra-rater and inter-rater reliability. We captured 59 seizures from 18 patients (35% of participants) during 1420 hours of RES monitoring. RES impairment was greatest during and after tonic-clonic seizures, less in partial seizures, and minimal in auras and subclinical seizures. In partial seizures, ictal RES impairment was significantly greater if EEG changes were present. Maximum RES impairment (lowest ictal score) was also significantly correlated with long postictal recovery time, and poor postictal memory.
Significance
We found that prospective testing of responsiveness during seizures is feasible and reliable. RES impairment was related to EEG changes during seizures, as well as to postictal memory deficits and recovery time. With a larger patient sample it is hoped that this approach can identify brain networks underlying specific components of impaired consciousness in seizures. This may allow the development of improved treatments targeted at preventing dysfunction in these networks.
Keywords: Consciousness, Seizure, Behavior, Testing battery, Electroencephalography, Video/EEG monitoring
Introduction
Normal consciousness depends on the general level of arousal as well as on the collective action of numerous specific cognitive tasks. These two aspects have been termed the level and content of consciousness respectively (Plum and Posner, 1982). Epileptic seizures can invade the anatomical systems for general arousal and specific cognitive tasks, leading to impairment in both the level and content of consciousness (Cavanna and Ali, 2011; Blumenfeld and Taylor, 2003; Blumenfeld, 2009). Consequently, impairment of consciousness may cause much of the memory and cognitive function deficits, injuries, work-related disability, automobile accidents, and social stigma associated with epilepsy (Lings, 2001; Sheth et al., 2004; Jacoby et al., 2005; Wirrell, 2006; Baker et al., 2008; Smith et al., 2009). To determine whether the level or content of consciousness or both are affected during seizures would require careful and detailed behavioral testing. Interictally, cognitive impairment has been investigated extensively using neuropsychological assessment (Jones-Gotman et al., 2010; Oyegbile et al., 2004). However, the study of impairment of the level of consciousness and specific deficits in memory and cognition during the transient ictal period has been relatively neglected.
Several recent studies have begun to investigate impaired consciousness during seizures mainly based on retrospective review of nonstandardized testing with inpatient video-EEG (VEEG) monitoring (Yang et al., 2010 ; Bell et al., 1998; Inoue and Mihara, 1998; Lee et al., 2002; Lux et al., 2002; Blumenfeld et al., 2004b; Blumenfeld et al., 2004a; Guye et al., 2006; Cavanna et al., 2008; Arthuis et al., 2009; Blumenfeld et al., 2009; Englot et al., 2010), or based on outpatient testing in the case of absence seizures (Blumenfeld, 2005; Berman et al., 2009; Li et al., 2009; Bai et al., 2010). Although such studies have begun to shed light on possible cortical and subcortical mechanisms leading to ictal unconsciousness (for review see (Blumenfeld and Taylor, 2003; Blumenfeld, 2009; Cavanna and Monaco, 2009; Englot and Blumenfeld, 2009; Yu and Blumenfeld, 2009)) standardized prospective testing would allow more precise comparison of impaired functions consistently tested across seizures and across patients.
Standardized testing batteries have been useful in evaluating other relatively static disorders of consciousness, such as coma, vegetative state, and minimally conscious state (Teasdale and Jennett, 1974; Giacino et al., 2004). Advantages of these scales include the ability to reproducibly test different cognitive domains such as orientation, language, memory, and sensorimotor function. Standardized scales also more reliably distinguish the vegetative from minimally conscious state, which in some ways resemble more transient deficits observed during seizures (Blumenfeld, 2011). We now propose to develop and validate a prospective standardized “Responsiveness in Epilepsy Scale” (RES) for assessing patients during VEEG monitoring. RES was derived from the JFK Coma Recovery Scale-Revised (Giacino et al., 2004), with modifications made to enable testing within the typical 1–2 minute timeframe of seizures (Afra et al., 2008). To accomplish this, the RES is adaptive, enabling examiners to adjust the level of difficulty to optimize information gained in the minimum time.
Using this approach, we investigated the feasibility and reliability of prospective testing of responsiveness during seizures by using RES in a group of patients during VEEG monitoring. In addition, we examined the relationship between ictal and postictal impaired responsiveness as measured by RES, and also related RES impairment to other clinical features of seizures. Specifically, we analyzed the relationships between two ictal RES-outcomes (initial impairment, maximum impairment), two postictal RES-outcomes (recovery time, memory recall), and three clinical seizure-related variables (presence of EEG changes, seizure duration, side of onset). We hope that prospective standardized ictal testing can provide a valuable tool for investigating altered level and content of consciousness in epilepsy.
Methods
Subjects
Fifty-two adult or pediatric patients with epilepsy and ten normal adult controls participated in our study. Approval was obtained from the Yale Human Investigations Committee (New Haven, CT), and all subjects provided written informed consent. For patients, inclusion criteria were: 1) admission to the inpatient Yale Epilepsy Video/EEG Monitoring Unit between June, 2009 and August, 2010; 2) age 7 years or older; 3) willingness and ability to participate in simple behavioral tasks during seizures. Exclusion criteria were: 1) non-epileptic (psychiatrically-based) episodes, which have been well documented in previous studies (Ali et al., 2010; Reuber and Kurthen, 2011); 2) cognitive or motor impairment that prevented performance of the tasks.
Development of the Scale
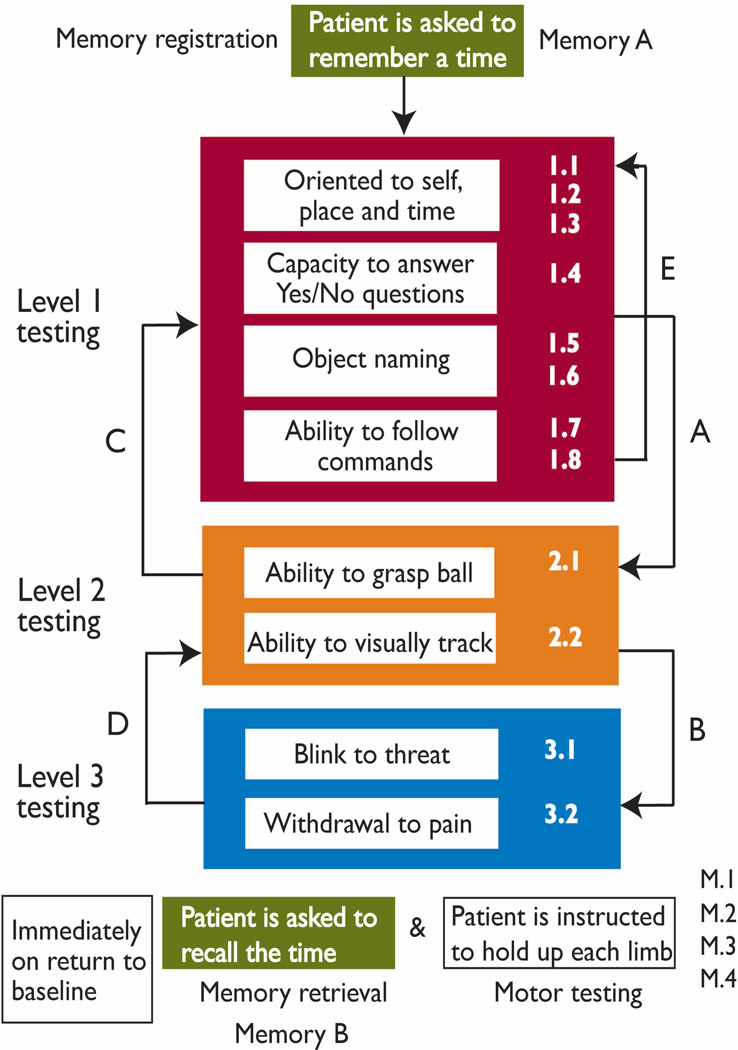
The Responsiveness in Epilepsy Scale (RES) was modified from the JFK Coma Recovery Scale-Revised used for evaluating patients with chronic disorders of consciousness (Giacino et al., 2004). Important modifications include making the scale relatively brief, to enable testing within the typical one to two minute timeframe of seizures. In addition, the RES is adaptive (Figure 1). Thus, examiners adjust the level of difficulty of testing to match the degree of impairment—the goal was to optimize information gained in the minimum time. RES is a 12-item scale consisting of three levels (Figure 1): Level 1 with eight items, Level 2 with two items, and Level 3 with two items (see Supplemental material 1, Online). Level 1 items include orientation questions, and other verbal questions and commands testing receptive and expressive language, visual processing, and motor praxis. Level 2 items include more basic sensorimotor responses and visual tracking. Level 3 items include the most basic responses to visual threat and noxious tactile stimulation. In addition to the Level 1–3 items, the RES also includes memory recall for information presented at seizure onset, as well basic post-ictal motor testing. Full details of the RES can be found in Supplemental material 1, Online.
Figure 1.
Responsiveness in epilepsy scale (RES) adaptive testing procedure. At seizure onset, patient is asked to remember the time (Memory A, memory registration). Level 1 testing then begins (Items 1.1 through 1.8). A. If the patient scores less than 3 points on any two consecutive items on Level 1 then proceed to Level 2. Otherwise continue through Level 1 and repeat (E). B. If the patient scores less than 2 points on ALL items in Level 2 then proceed to Level 3. Otherwise proceed back to Level 1 (D). C. After completing Level 3 proceed back to Level 2. D. If the patient scores 2 or better on ANY Level 2 items then proceed back to Level 1. E. Level 1 is repeated through the postictal period until all responses have returned to baseline. Then the patient is asked to recall the time (Memory B, memory retrieval) and motor testing is performed in each limb. For full details of the RES protocol and scoring see Supplementary data 1, Online.
Reliability testing
Ten healthy subjects with no history of neurological illness were recruited to measure how different examiners and raters influence the results of the scale. Each normal subject was told to simulate two types of seizures for about one minute each: a “simple partial” seizure without impaired consciousness, and a “complex partial” seizure with impaired consciousness. Normal subjects were laboratory or clinical personnel familiar with typical seizure manifestations. Each subject simulated each seizure type twice—the first set to one examiner and the second set to another (total of four seizures per subject). RES was administered to all subjects by two trained examiners (LY, PK) who examined subjects separately. The two examiners then rated each of the seizures independently by video footage. The seizure type was not disclosed to either examiner.
We further tested reliability by selecting a total of 20 video recordings of real epileptic seizures from 10 different patients in which level 1 and level 2 testing had been performed. Two raters (CE, XH) viewed each seizure twice and scored them independently. Intra-rater reliability and inter-rater reliability were determined for all seizures. Intra-rater reliability was calculated by comparing an individual rater’s scores for the two times they viewed each seizure. On the other hand, inter-rater reliability was calculated by comparing the results of both raters for each seizure.
RES Examiners
RES examiners were mainly undergraduate premedical student volunteers. To maintain consistency, all examiners met weekly to practice RES on seizures simulated by other members of the research team. Simulated seizures typically resembled simple partial, complex partial, or generalized seizures. Mistakes made by the examiner were identified and corrected by other team members. Prior to performing testing on each patient, examiners were informed about the patients’ typical seizure manifestations by members of the clinical team. Examiners also previewed up to three of the patient’s typical seizures on video if available. A team of six to eight examiners participated during any given semester, with a total of 16 examiners participating throughout the course of the study. Examiners sat in four-hour shifts at patients’ bedsides on the inpatient video/EEG monitoring unit during waking hours, from 6am until 11pm. Seizures arising from sleep were not investigated in this study since consciousness is already altered at seizure onset.
Data collection
Continuous video and EEG data were acquired from scalp or intracranial electrodes in all patients using a standard clinical video/EEG monitoring system (Bio-Logic, Knoxville, TN, USA). Patients typically remained in the hospital for 1–2 weeks to await spontaneous seizures, often during a period of medication tapering. The research team did not participate in the clinical team’s decisions about induction of seizures, including sleep deprivation, photic stimulation, hyperventilation, and withholding of medications.
RES examiners observed patients at their bedside whenever possible and interacted with patients in order to detect clinical seizure onset. In addition, they monitored each patient’s EEG recordings through the in-room video monitors to detect electrographic seizure onset. A bag with items used in RES testing (watch, pen, tennis ball, hand mirror, reflex hammer; see Supplemental material 1, Online) was maintained at bedside for all participating patients. RES was committed to memory by all examiners through frequent practice sessions, and administered without referring to written notes. Baseline testing (see Supplemental material 1, Online) took place during a period without ictal activity. Administration of RES began immediately upon detection of seizure onset and was repeated throughout the ictal and postictal periods until patients returned to their baseline level of performance (Figure 1). The interictal memory test was administered at least 6 hours after a seizure was captured with RES.
VEEG clinical analysis
All patients’ EEGs and video/behavioral recordings were reviewed by neurologists specializing in epilepsy at our institution. Video/EEG data were reviewed using Ceegraph vision software (7.15.06.i06 Model 811 Rev 223 A). Seizure onset time was defined by the earliest time with behavioral or electrographic evidence of a seizure, and offset time was defined as the latest time with such evidence. Events were classified as subclinical seizures, auras, partial seizures, or generalized tonic–clonic seizures. Partial seizures and generalized seizures were classified according to the criteria established by the International League Against Epilepsy (ILAE, 1981, 1989). Subclinical seizures were defined as events with epileptiform activity on EEG that progressed in either frequency or location in a characteristic ictal pattern but had no clinical signs or symptoms (Sperling and OConnor, 1990). Auras were defined as seizure warnings reported by patients verbally or by pressing the event button with no other overt behavioral symptoms. Other clinical data (Supplementary material 2, Online) were obtained from the patient medical records.
RES scoring
Performance on RES was scored based on review of video recordings and the agreement of two reviewers, one of whom was the examiner. Video recordings of RES were analyzed within 24 hours of seizure capture. Timing of all test items and responses was determined relative to seizure onset and termination, and separate analyses were performed for the ictal and postictal periods. The time of each item was defined as the time when administration of that item was completed. The time of each RES level (Levels 1–3) was defined as the time when the response to the last item on each level was completed.
Item scores were normalized such that the score of each item was divided by the total score possible for that item on a scale from 0 to 1. A composite RES “consciousness score” was also calculated at the time point at which each level was completed. This provided a graded measure of overall impairment at different times. The consciousness score was also measured on a scale from 0 to 1. To calculate the consciousness score, the raw score for each level was first calculated as Raw level score = total points for all items on that level/maximum possible points for that level. The raw level score was then weighted by the number of items for each level, and added to the minimum possible score for that level.
| [Eqn. 1] |
Thus, since there were 12 items total, the Level 1 (8 items) weight was 8/12, Level 2 (2 items) weight was 2/12, and Level 3 (2 items) weight was 2/12. Level 1 minimum score was 4/12 (equivalent to perfect score on Levels 2 and 3), the Level 2 minimum score was 2/12 (perfect score on Level 3), and the Level 3 minimum score was 0/12.
The timecourse of impairment during seizures was depicted by consciousness scores on each consecutive level over time (e.g. see Figure 3). We also determined the lowest ictal consciousness score for each seizure. The time of the lowest ictal consciousness score was measured from seizure onset; if the lowest score was the same for two or more data points these timepoints were averaged. The time required to recover to baseline RES scores, termed “recovery time,” was defined as the time between seizure offset and the completion of RES Level 1 with an unscaled total Level 1 score within 2 points of interictal baseline (see Supplemental material 1, Online).
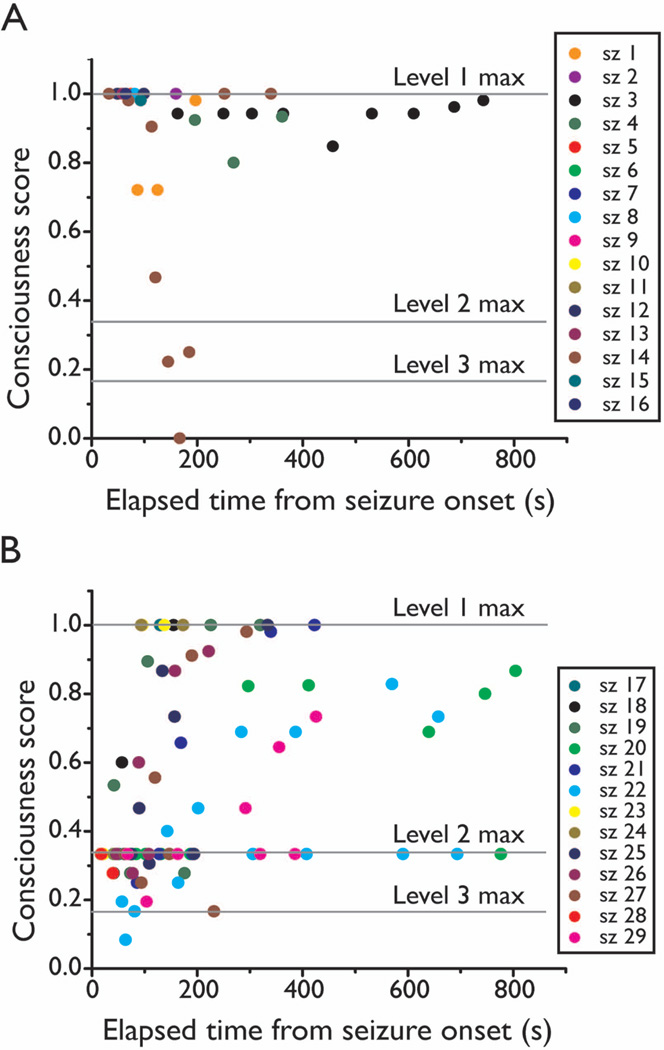
Figure 3.
RES consciousness score time courses for partial seizures without or with initial impairment. A. Seizures with Item 1.1 score = 5 (no initial impairment, total 16 seizures). Scores tended to remain relatively high throughout seizures (aside from seizure 14 which showed a delayed dip). B. Seizures with item 1.1 score = 0 (severe initial impairment, total 13 seizures). Seizures tended to show more severe persistent impairment at later times as well. Each color represents data points from one seizure. Level 1 max = maximum possible consciousness score on Level 1, calculated as (8/8)*(8/12) + 4/12 = 1 (see Eqn. 1 in Methods); Level 2 max = maximum possible consciousness score on Level 2, calculated as (2/2)*(2/12) + 2/12 = 0.333; Level 3 max = maximum possible conciousness score on Level 3, calculated as (2/2)*(2/12) + 0/12 = 0.167.
Statistical analysis
Kappa values were calculated to determine inter-rater, intra-rater and inter-examiner reliability across test items for each RES level. The chi-square test was used to examine group differences for proportions. A two-tailed t-test or analysis of variance (ANOVA) with post-hoc Tukey was used depending on whether one set or multiple variables were being tested. Spearman’s or Pearson’s correlation were used depending on whether variables were nominal or continuous. Values are reported as mean + SEM. All statistical results were calculated using SPSS 16.0.0 for Windows (SPSS Inc., Chicago, IL, U.S.A.) with a significance threshold P<0.05.
Because more than one seizure often occurred per patient (see Table 1) an important consideration was whether to pool or select data from within each patient before performing group analyses. However, since we often found the level of responsiveness to be very different among seizures within the same patient, we felt it was more appropriate to include all seizures as separate data points in group analyses. We also repeated all statistical analyses by first pooling the average results within each patient for each seizure type where feasibleand then treating each patient as an individual data point, yielding results that were nearly identical and similarly statistically significant to the analyses treating each seizure separately (see Supplemental material 3, Online).
Table 1.
Number of seizures (and patients) tested for each RES item
| RES items |
Ictal | RES items |
Postictal | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sub | Aura | Partial | GTC | Total | Sub | Aura | Partial | GTC | Total | ||
| Total | 1(1) | 4(3) | 36(14) | 4(4) | 45(17) | Total | 2(1) | 11(5) | 41(14) | 5(5) | 59(18) |
| MemA | 1(1) | 3(3) | 34(12) | 4(4) | 42(15) | MemB | 2(1) | 10(5) | 33(12) | 5(5) | 50(16) |
| L1.1 | 1(1) | 4(3) | 35(12) | 4(4) | 44(15) | L1.1 | 2(1) | 8(5) | 15(8) | 4(4) | 29(12) |
| L1.2 | 0 | 3(3) | 29(12) | 4(4) | 36(15) | L1.2 | 2(1) | 10(5) | 24(11) | 4(4) | 41(14) |
| L1.3 | 0 | 2(2) | 17(8) | 2(2) | 21(11) | L1.3 | 2(1) | 9(5) | 21(9) | 1(1) | 34(11) |
| L1.4 | 0 | 3(3) | 8(3) | 1(1) | 12(7) | L1.4 | 2(1) | 10(5) | 21(9) | 1(1) | 35(12) |
| L1.5 | 0 | 3(3) | 5(3) | 0 | 8(6) | L1.5 | 2(1) | 11(5) | 30(10) | 1(1) | 45(13) |
| L1.6 | 0 | 3(3) | 3(2) | 0 | 6(5) | L1.6 | 2(1) | 11(5) | 30(9) | 1(1) | 45(11) |
| L1.7 | 0 | 2(2) | 3(2) | 0 | 5(4) | L1.7 | 2(1) | 10(4) | 30(9) | 1(1) | 44(13) |
| L1.8 | 0 | 2(2) | 3(2) | 0 | 5(4) | L1.8 | 2(1) | 10(4) | 30(9) | 1(1) | 44(10) |
| L2.1 | 0 | 0 | 16(9) | 4 (4) | 20(12) | L2.1 | 0 | 1(1) | 10(8) | 5(5) | 16(12) |
| L2.2 | 0 | 0 | 13(8) | 3 (3) | 16(10) | L2.2 | 0 | 1(1) | 12(9) | 4(4) | 17(11) |
| L3.1 | 0 | 0 | 2(2) | 4 (4) | 6(6) | L3.1 | 0 | 0 | 3(3) | 3(3) | 6(6) |
| L3.2 | 0 | 0 | 0 | 3 (3) | 3(3) | L3.2 | 0 | 0 | 3(3) | 1(1) | 4(4) |
| M 1.1 | 2(1) | 9(5) | 33(12) | 5(5) | 49(9) | ||||||
| M 1.2 | 2(1) | 9(5) | 33(12) | 5(5) | 49(9) | ||||||
| M 2.1 | 2(1) | 9(5) | 33(12) | 5(5) | 49(9) | ||||||
| M 2.2 | 2(1) | 9(5) | 33(12) | 5(5) | 49(9) | ||||||
Number of seizures (patients) are shown. Sub=subclinical seizure, Partial=partial seizure, GTC=generalized tonic-clonic seizure. MemA= Memory A, MemB=Memory B, L=level, M =motor. Note that some seizures only had postictal data (because RES started too late), but any seizures that had ictal data also had postictal data.
Results
Reliability
For the 20 simulated simple partial seizures, inter-rater reliability for RES Level 1 was high (same examiners) (κ = 0.90, SE = 0.03, 95% CI 0.84–0.96). Inter-examiner reliability (same raters) for Level 1 was also high (κ = 0.89, SE = 0.03, 95% CI 0.82–0.96). RES Levels 2 and 3 were not performed during simple partial seizures, in agreement with protocol (Supplementary Data 1, Online). For the 20 simulated complex partial seizures, the inter-rater reliability values were acceptable for Level 1 (κ = 1.00, SE = 0.00, 95% CI 1.00–1.00), Level 2 (κ = 0.84, SE = 0.15, 95% CI 0.54–1.00) and Level 3 (κ = 0.74, SE = 0.14, 95% CI 0.46–1.00). Likewise, the inter-examiner reliability values were also acceptable for Level 1 (κ = 1.00, SE = 0.00, 95% CI 1.00–1.00), Level 2 (κ = 0.72, SE = 0.19, 95% CI 0.35–1.00) and Level 3 (κ = 0.76, SE = 0.17, 95% CI 0.43–1.00). Of note, all raters and examiners agreed upon when the subject maintained Level 1 as well as when to proceed to Level 2 or 3.
The reliability test for the real patients’ seizures showed similar findings between and within individual raters. The intra-rater reliability for Level 1 showed almost perfect agreement (κ = 0.96, SE = 0.02, 95% CI 0.93–0.99). Likewise for the inter-rater reliability (κ = 0.85, SE = 0.02, 95% CI 0.81–0.89). Reliability tests for Level 2 also showed excellent inter-rater (κ = 0.76, SE = 0.09, 95% CI 0.59–0.94) and intra-rater (κ = 0.84, SE = 0.07, 95% CI 0.71–0.99) reliability.
Demographics of patient sample
A total of 52 subjects were recruited to this study. Subjects included 27 females (52%) and 25 males. Their mean age at the time of hospitalization was 39 years (range 10–68 years), with 49 adult subjects aged 18–68 years (94%) and 3 pediatric subjects aged 10–17 years. Subjects included 45 (87%) right-handed and 7 left-handed patients. Of the 59 subjects, seizures were captured with RES testing in 18. For these 18 subjects included in the final analysis, 11 (61%) were female while 7 were male (39%). In addition, there were 14 (78%) right-handed and 4 left-handed patients. 11 of them (61%) underwent scalp EEG alone, 1 (5.56%) underwent ictal SPECT analysis along with scalp EEG, and 5 patients (27%) underwent intracranial EEG analysis. Their mean age was 36 years at time of testing, with 18 adult and no pediatric patients.
Feasibility
A total of 59 seizures from 18 patients (35% of participants) were captured with RES. This amounts to an average of one seizure for every 23.7 hours of RES monitoring. Examiners conducted a total of 1420.3 hours of RES monitoring. The range of RES monitoring hours per patient spanned 2.5 to 158.0 hours, and the mean RES monitoring time was 27.3 hours per patient. Each patient was monitored by one to seven examiners at different times, with an average of 3.8 examiners assigned to each patient.
Overall, the average VEEG monitoring period per patient was 7.5 days, so that RES testing was performed during 15% of total VEEG monitoring time. Seizure frequency was 0.04 seizures per hour during RES, somewhat lower than the 0.08 seizures per hour during overall VEEG monitoring. Of note, RES was only performed while patients were awake and during the hours of 6am to 11pm.
Mean seizure duration during RES was 109 s (mean duration of auras was 31s, subclinical seizures 71s, partial seizures 112 s, and generalized tonic-clonic seizures 287s). The first RES question was asked a mean of 41 + 6 seconds after seizure onset. The average ictal examining time, defined as the time from beginning of the first test item to end of the last test item during seizures, was 68 s. Each seizure with ictal testing featured an average of 9.2 items. Each item took 7.3 s to complete on average.
Seizure events were classified as subclinical seizures, auras, partial seizures, or generalized tonic clonic seizures (see Methods). By far the most common events captured were partial seizures (Table 1). In a few cases RES testing did not start until seizures were already over and only postictal data were obtained (Table 1). For example, in partial seizures from 14 patients, there were 36 events with ictal data and 41 events with postictal data (5 seizures had postictal data only). Table 1 shows the total number of seizures in which data were obtained for each RES test item.
Seizure localization
Of the 18 patients whose seizures were captured with RES examination, epilepsy was localized to the left hemisphere in six patients and to the right hemisphere in seven patients. The remaining five patients had bilateral localization or were unlocalized (Supplemental material 2, Online). Seizure onset involved the temporal lobe in eight patients, frontal lobe in four, occipital lobe in two, and parietal lobe in one. Four patients underwent surgical treatment, but only short-term outcome was available at the time of the study (Supplemental material 2, Online).
Overview of performance across seizure types by RES level
As an initial step, to look at overall performance during and following seizures, we determined the number of seizures that “passed” or “failed” each RES level ictally across different seizure types (Table 2). In other words, we counted the number of seizures in which performance was sufficiently preserved to maintain Level 1 testing throughout, and seizures in which performance was impaired enough to reach Level 2, or Level 3 testing. All subclinical seizures as well as auras maintained Level 1 both ictally and postictally. Partial seizures demonstrated a more variable distribution: 58% maintained Level 1 ictally, compared with 42% that proceeded to Level 2 and 7% that proceeded to Level 3. Postictally, 81% of all partial seizures maintained Level 1, while 19% proceeded to Level 2 and 7% proceeded to Level 3. In contrast, all generalized tonic-clonic seizures proceeded to Level 2 and Level 3 ictally. Postictally, after one tonic-clonic seizure there was a quick return to Level 1, while after the remainder of tonic-clonic seizures testing continued at Level 2 and Level 3. These results suggest that, not surprisingly, patients were least impaired with subclinical seizures and auras, variably impaired with partial seizures, and most severely impaired with tonic-clonic seizures.
Table 2.
Ictal and postictal RES Level 1, 2, 3 performance by seizure type
| Ictal | Postictal | |||||||
|---|---|---|---|---|---|---|---|---|
| Sz type | No. Szs |
Maintains Level 1 |
Proceed to Level 2 |
Proceed to Level 3 |
No. Szs |
Maintains Level 1 |
Proceed to Level 2 |
Proceed to Level 3 |
| Subclin | 1 | 1 | 0 | 0 | 2 | 2 | 0 | 0 |
| Aura | 4 | 4 | 0 | 0 | 11 | 11 | 0 | 0 |
| Partial | 36 | 21 | 15 | 2 | 41 | 33 | 8 | 3 |
| GTC | 4 | 0 | 4 | 4 | 5 | 1 | 4 | 3 |
Number of seizures are shown. Number of patients were 1 for subclinical, 5 for auras, 14 for partial, and 5 for GTC seizures. Note that some seizures only had postictal data (because RES started too late), but any seizures that had ictal data also had postictal data.
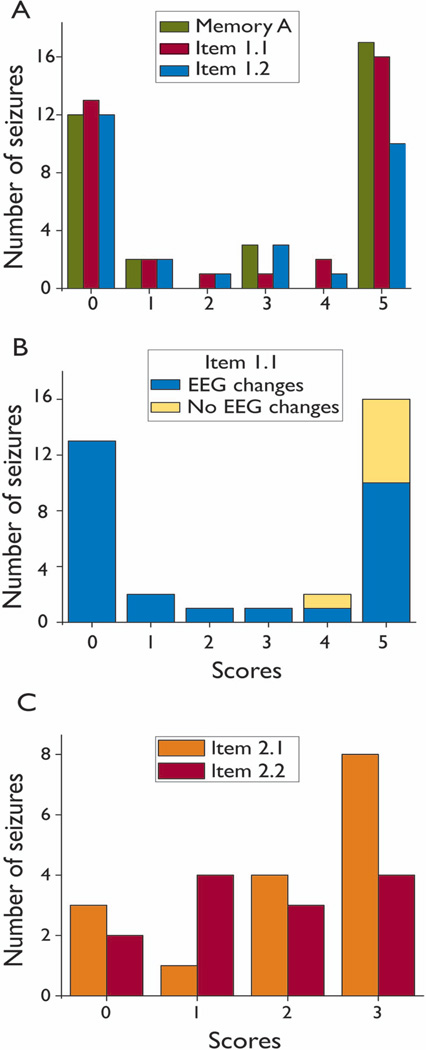
Initial ictal impairment in partial seizures
Most seizures captured by RES were partial seizures (69%) (see Table 1), so these seizures were a point of focus for data analysis. The scores of the first three items asked—Memory A, Item 1.1, and Item 1.2—exhibited a bimodal distribution (Figure 2A). For Memory A, Item 1.1, and Item 1.2, 35%, 37%, and 41% respectively of seizures received a score of 0/5, whereas 50%, 46% and 34% respectively received a score of 5/5. In addition, scores of the three items were highly correlated with each other. (Memory A vs Item 1.1, r=0.681, P<0.001; Item 1.1 vs Item 1.2, r=0.935, P<0.001; Memory A vs Item 1.2, r=0.711, P<0.001).
Figure 2.
RES initial testing scores for partial seizures are bimodally distributed, and related to EEG changes. A. Bimodal distribution of scores on initial ictal testing items. Score of 0 is worst, and 5 is best. B. EEG changes were always present for partial seizures with severe initial impairment (low score on Item 1.1, “What is your name?”), but EEG changes were sometimes absent for seizures with good initial RES scores. C. Unlike initial test scores, Item 2.1 and 2.2 scores were relatively evenly distributed (score of 0 is worst, 3 is best). For full details of the RES protocol and scoring see Supplementary data 1, Online.
Since Item 1.1 yielded the most scored data (see Table 1), we further investigated possible clinical seizure-related factors to explain divergent RES performance between Item 1.1=0 and Item 1.1=5 seizure groups. Thirteen out of 35 partial seizures that were captured by RES ictally received a score of 0/5, and 16 seizures captured ictally received a score of 5/5. The remaining six scores fell in the range of 1 to 4 out of 5 (Figure 2 B). All the partial seizures that received a score of 0 exhibited EEG changes; in contrast, of the seizures that received a score of 5, only 62.5% exhibited EEG changes. The number of seizures with and without EEG changes between Item 1.1=5 and Item 1.1=0 groups were significantly different (Chi-square = 13.07, p = 0.005). In contrast, there was no apparent relationship between impairment on Item 1.1, and either side of seizure onset, or seizure duration. Thus, of the 13 partial seizures with Item 1.1=0, four had right hemisphere onset, two had left hemisphere onset, and seven had bilateral or unknown onset. Of the 16 partial seizures with Item 1.1=5, six had right hemisphere onset, three had left hemisphere onset, and one had bilateral onset. In addition, seizure duration of the Item 1.1=0 group was 139±37.5 s (n=13), which is not significantly different compared with the Item 1.1=5 group seizure duration of 133±51.2 s (n=16).
Later ictal impairment in partial seizures
Later impairment was evaluated by two approaches: 1. Level 2 and Level 3 individual item scores, which did not yield clear relationships to clinical seizure-related variables; and 2. Minimum RES consciousness score, which was more informative. The Ictal Level 2 item scores in partial seizures are shown in Figure 2 C. Seizures with scores for Items 2.1 and 2.2, ranging from 0 to 3, were more evenly distributed, in contrast to Memory A, Item 1.1, and Item 1.2 scores (see Figure 2 A). RES Level 2 items were performed ictally in 16 partial seizures. We did not find any clear relationship between performance on Level 2 items and clinical seizure-related variables with the present data set. All partial seizures that had Level 2 testing exhibited EEG changes, so we could not relate this variable to Level 2 score. Of the seizures that were tested with Level 2 items, three seizures were localized to the left hemisphere, six to the right hemisphere (seven were bilateral), and side of onset showed no clear relationship to Level 2 scores. We also found that seizure duration was not correlated with either Item 2.1 or Item 2.2 scores. For Level 3 items, there was insufficient data (see Table 1) to investigate relationships to clinical seizure-related variables.
In a second approach to look at later impairment, we analyzed consciousness scores in all partial seizures, 36 total, that were captured ictally with RES. The lowest consciousness score was calculated for each seizure with a scaled range of zero to one. Overall, the lowest consciousness score averaged 0.59±0.06. The average time between seizure onset and lowest consciousness score was 85s±15s. We next examined the relationship between lowest consciousness score and clinical seizure-related variables for partial seizures. We found that the lowest consciousness score had a negative correlation with seizure duration (r=−0.558, p<0.001, n=36), meaning that lower consciousness score was associated with longer seizure duration. In addition, the lowest consciousness scores of seizures with EEG changes had a mean of 0.49±0.06 (n=29), which was significantly lower compared with those without EEG changes with a mean of 0.997±0.003 (n=7) (t=3.884, p<0.001, two-tailed t-test). We did not find a relationship between lowest consciousness score and hemisphere of seizure onset.
We also examined the later impairment in partial seizures in relation to initial impairment on Item 1.1. We found that seizures showing impaired function on Item 1.1 (score = 0) had a mean lowest consciousness score of 0.27 ±0.02 (n=13), significantly lower than the score of 0.90 ±0.06 (n=16) seen in seizures with initially spared function (Item 1.1 score = 5) (t=8.518, p< 0.001, two-tailed t-test). The timecourse of consciousness score changes for partial seizures confirms that seizures with initially spared performance tended to retain good performance throughout seizures (Figure 3 A), while seizures with initially impaired performance were more likely to show later impaired performance as well (Figure 3 B).
Postictal recovery time
Recovery time (interval between seizure offset and completion of RES Level 1 within 2 points of baseline) was 328 seconds on average for all seizures. Mean recovery time increases as severity of seizure type increases: 32±2.83 s for subclinical seizures, 44±29.9 s for auras, 151±371.8 s for partial seizures, and 2673±1737.8 s for GTC seizures. Recovery time was significantly correlated with the four seizure types in the order listed above (Spearman r=0.416, p=0.002). We analyzed the recovery time for partial seizures in greater detail, and did not find any significant relationships to clinical seizure-related variables including seizure duration, presence or absence of EEG changes during the seizure, and side of seizure onset. In addition, recovery time was not significantly different for seizures with initial impairment (Item 1.1=0) compared to seizures without initial impairment (Item 1.1=5). However, we found that recovery time in partial seizures had a significant negative correlation with lowest consciousness score (r=−0.504, p=0.003), meaning that recovery time was longer for seizures with more severely impaired consciousness.
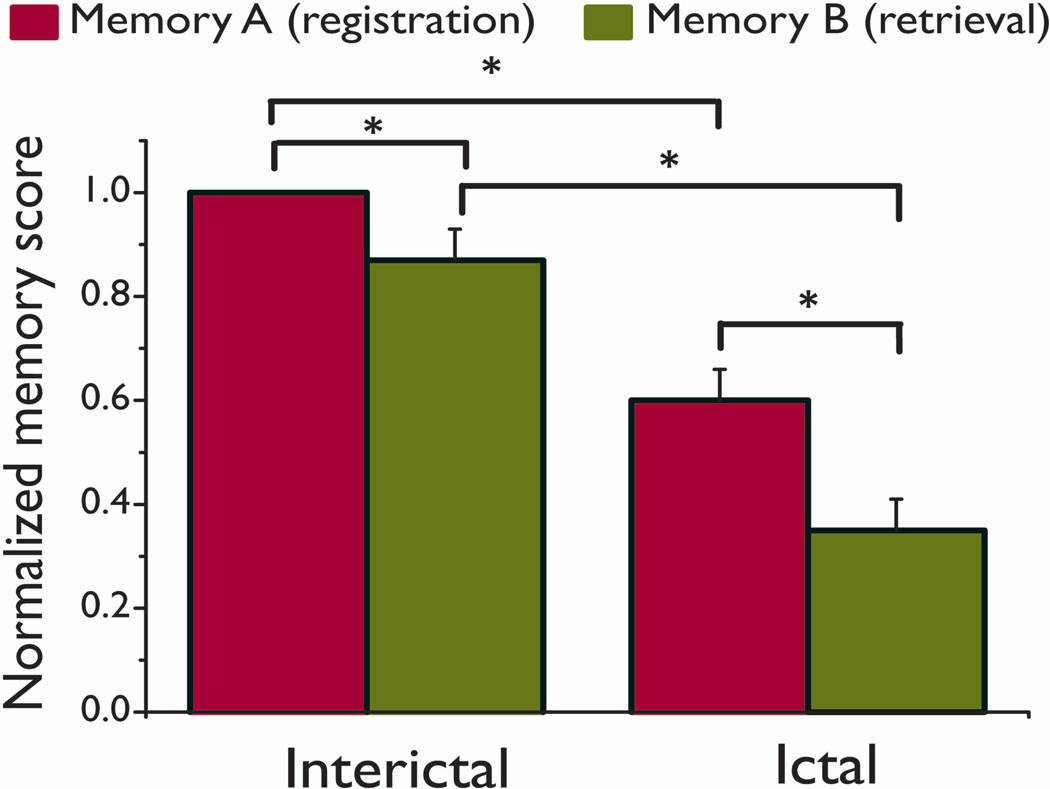
RES memory performance
For analysis of memory performance we focused on ictal memory registration (Memory A) and postictal memory recall (Memory B). In addition, baseline interictal Memory A and B scores were obtained for all patients at the same intervals as the ictal testing. Baseline interictal registration (Memory A) scores of 1.00 ±0.00 were somewhat higher than recall (Memory B) scores of 0.87±0.06 (t=2.214, p=0.047, two-tailed paired t-test) even though no seizure had occurred in the interim (Figure 4). Ictal Memory A was obtained on average 37 s after seizure onset, and with a mean score of 0.60±0.06 was significantly lower than interictal Memory A (t=3.029, p=0.01, two-tailed paired t-test) (Figure 4). Postictal Memory B was obtained an average of 128 seconds after Memory A was asked (74 seconds after seizure offset). Mean postictal Memory B score of 0.35±0.06 was significantly lower than both ictal Memory A (t=3.737, p<0.001, two-tailed paired t-test), and interictal Memory B (t=3.464, p=0.006, two-tailed paired t-test) (Figure 4). In addition, the drop in memory score between registration and retrieval (Memory A minus Memory B) was significantly higher during seizures (0.70±0.20) than during the interictal period (0.20± 0.15; t=2.828, p<0.05, two-tailed paired t-test).
Figure 4.
Memory registration and retrieval during the interictal and ictal periods. Interictal Memory A (registration) scores were marginally higher than Memory B (retrieval) scores even though no seizure had occurred in the interim (t=2.214, p=0.047, two-tailed paired t-test). Ictal Memory A (registration) scores were significantly lower than interictal Memory A (t=3.029, p= 0.01). In addition, postictal Memory B (retrieval, labeled here as “Ictal”) scores were significantly lower than both ictal Memory A (t=3.737, p<0.001) and interictal Memory B (t=3.464, p = 0.006). * p < 0.05. Values shown are mean ± SEM.
We next investigated whether memory performance for partial seizures was related to either initial or later ictal impairment on RES. Ictal Memory A scores for seizures with initial severe impairment on RES (Item 1.1=0) averaged 0.26±0.11; this was lower than Memory A scores for seizures with Item 1.1=5, which had average scores of 0.91±0.07 (t=5.312, p<0.001, two-tailed t-test). There was a trend for worse postictal Memory B scores in seizures with Item 1.1=0 (0.20+0.11) compared to those without initial ictal impairment (0.47+0.13) although this did not reach statistical significance (t=1.49, p=0.15, two-tailed t-test). On the other hand, we found that lowest ictal consciousness score and postictal Memory B were significantly correlated (r=0.506, p=0.004).
Clinical seizure-related variables including seizure duration, presence of ictal EEG changes, and side of seizure onset were not related to either Memory A or Memory B scores. In addition, the time between seizure end and postictal Memory B administration did not correlate with postictal Memory B scores (r=−0.291, p=0.133).
Postictal motor score performance
Postictal motor testing was performed as an ancillary measure of patient impairment following seizures. During baseline testing, only Patient 11 demonstrated motor impairment, with left-sided weakness due to a previous stroke (see Supplemental material 1, Online). Mean time from seizure end to onset of motor testing including all seizures was 295 + 95 s. In general, very few patients showed deficits during postictal motor testing. Compared with baseline scores, subclinical seizures and auras had perfect postictal motor scores. Of the patients with partial seizures, one patient (Patient 11, mentioned above) could not hold up the left arm and left leg, and Patient 18 could not hold up the right arm because another seizure started at that point. Of the patients with generalized tonic-clonic seizures, one patient (Patient 4) could not hold up the left arm and left leg due to postictal paralysis.
Discussion
We found that the RES was reliable and feasible for prospective behavioral testing during seizures, and yielded some interesting initial results. RES impairment was related to seizure type, with poorest performance in generalized tonic-clonic seizures, minimal impairment in auras and subclinical seizures, and intermediate performance in partial seizures. Partial seizures were analyzed in greater detail. We found that initial impairment on RES had a bimodal distribution. Seizures with severe initial impairment were more likely to have later impairment as well, while those without initial impairment usually continued without impairment at later times. Both initial and later impairment on RES were greater in partial seizures showing EEG changes compared to seizures without EEG changes. Postictal recovery time and memory deficits were both correlated with the magnitude of the lowest RES score during seizures.
These findings suggest that partial seizures can usually be separated cleanly into those with or without RES impairment, corresponding to the traditional “complex partial” and “simple partial” categories, with distinct clinical and electrographic features. RES-impaired (complex partial) seizures all showed EEG changes while only about half of RES-spared (simple partial) seizures showed changes on EEG. Seizures with lowest RES scores had more prolonged postictal recovery times, and more severe postictal memory deficits.
Several recent studies have used nonstandardized behavioral testing with inpatient VEEG (Yang et al., 2010 ; Bell et al., 1998; Inoue and Mihara, 1998; Lee et al., 2002; Lux et al., 2002; Blumenfeld et al., 2004b; Blumenfeld et al., 2004a; Guye et al., 2006; Cavanna et al., 2008; Arthuis et al., 2009; Blumenfeld et al., 2009; Englot et al., 2010),or outpatient testing of absence seizures (Blumenfeld, 2005; Berman et al., 2009; Li et al., 2009; Bai et al., 2010). Based on this work, it appears that impaired consciousness is related to abnormal activity in the upper brainstem/diencephalic arousal systems as well as in the association cortex (Blumenfeld and Taylor, 2003; Blumenfeld, 2009; Cavanna and Monaco, 2009; Englot and Blumenfeld, 2009; Englot et al., 2009; Yu and Blumenfeld, 2009; Blumenfeld, 2011). However, in order to differentiate impairment of specific domains of the content of consciousness, such as orientation, language, memory, and sensorimotor function, along with impairment in the overall level of behavioral arousal, more detailed testing is needed in a larger patient sample. Our goal in developing the RES (Figure 1) is to evaluate these specific domains in the ictal and postictal periods, and ultimately to relate deficits to physiological dysfunction in specific cortical-subcortical networks. In this manner the anatomical and physiological basis of impaired content and level of consciousness during seizures can be examined in detail.
Our present patient sample does not yet allow this detailed analysis. For example, impairment on Level 1 (Figure 1) could represent deficits in the level of consciousness, or more focal language dysfunction; further analysis in a larger patient sample of the simpler, less language dependant items (yes/no questions) on Level 1, and Levels 2–3 may ultimately enable deficits in the level vs. content of consciousness to be distinguished. In addition, we found that in agreement with past work (Gastaut and Broughton, 1972; Devinsky et al., 1988), partial seizures with impaired responsiveness more often exhibit EEG changes. However, we did not have sufficient data to analyze the type or location of EEG changes, as has been done in recent retrospective studies (Arthuis et al., 2009; Englot et al., 2010). Variability from seizure to seizure within individual patients also complicates the analysis, and ideally this work should be extended to a larger sample where both within-patient and between-patient variability could be more fully investigated. Further work in a larger sample using RES or similar prospective standardized testing along with techniques such as high density intracranial EEG and ictal SPECT has the potential to reveal fundamental mechanisms of ictal unconsciousness.
The adaptive nature of the RES testing procedure (Figure 1) was intended to optimize information obtained in the shortest time possible. However, in practice this requires much training and skill of personnel. It is important to note that the current version of the RES was performed by highly motivated and trained premedical students in the setting of a specialized epilepsy video/EEG monitoring unit. It is possible that the current version of the RES may not be feasible or practical in other settings without further modifications, In addition, some items (such as Level 3) were not often used, providing little data in the current patient sample (see Table 1). We found that nine RES items on average were completed per seizure. Therefore, it may be advantageous to modify the RES in future work, focusing on about nine of the highest yield items presented repeatedly in a non-adaptive manner throughout the ictal and postical periods.
In conclusion, we found that prospective evaluation of patient behavior during seizures is feasible and reliable using the RES if substantial concerted effort and training are performed. Detailed ictal and postictal testing of this kind can be helpful for distinguishing seizures with and without impaired consciousness. This may greatly enhance further investigations aimed at correlating altered physiology and anatomy with behavior in patients with epilepsy.
Supplementary Material
Acknowledgements
We thank Xiaoxiao Bai for helpful comments on the manuscript. This work was supported by The Patrick and Catherine Weldon Donaghue Medical Research Foundation, and by the Betsy and Jonathan Blattmachr family. Li Yang was supported by the China Scholarship Council.
Footnotes
Disclosure of Conflicts of Interest
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
None of the authors has any conflict of interest to disclose.
References
- Afra P, Jouny CC, Bergey GK. Duration of complex partial seizures: an intracranial EEG study. Epilepsia. 2008;49:677–684. doi: 10.1111/j.1528-1167.2007.01420.x. [DOI] [PubMed] [Google Scholar]
- Ali F, Rickards H, Bagary M, Greenhill L, McCorry D, Cavanna AE. Ictal consciousness in epilepsy and nonepileptic attack disorder. Epilepsy Behav. 2010;19:522–525. doi: 10.1016/j.yebeh.2010.08.014. [DOI] [PubMed] [Google Scholar]
- Arthuis M, Valton L, Regis J, Chauvel P, Wendling F, Naccache L, Bernard C, Bartolomei F. Impaired consciousness during temporal lobe seizures is related to increased long-distance cortical-subcortical synchronization. Brain. 2009;132:2091–2101. doi: 10.1093/brain/awp086. [DOI] [PubMed] [Google Scholar]
- Bai X, Vestal M, Berman R, Negishi M, Spann M, Vega C, Desalvo M, Novotny EJ, Constable RT, Blumenfeld H. Dynamic time course of typical childhood absence seizures: EEG, behavior, and functional magnetic resonance imaging. J of Neurosci. 2010;30:5884–5893. doi: 10.1523/JNEUROSCI.5101-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker GA, Hargis E, Hsih MM, Mounfield H, Arzimanoglou A, Glauser T, Pellock J, Lund S. Perceived impact of epilepsy in teenagers and young adults: an international survey. Epilepsy Behav. 2008;12:395–401. doi: 10.1016/j.yebeh.2007.11.001. [DOI] [PubMed] [Google Scholar]
- Bell WL, Park YD, Thompson EA, Radtke RA. Ictal cognitive assessment of partial seizures and pseudoseizures. Arch of Neurol. 1998;55:1456–1459. doi: 10.1001/archneur.55.11.1456. [DOI] [PubMed] [Google Scholar]
- Berman R, Negishi M, Vestal M, Spann M, Chung M, Bai X, Purcaro M, Motelow JE, Dix-Cooper L, Enev M, Novotny EJ, Constable RT, Blumenfeld H. Simultaneous EEG, fMRI, and behavioral testing in typical childhood absence seizures. 2009 doi: 10.1111/j.1528-1167.2010.02652.x. In review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenfeld H, Taylor J. Why do seizures cause loss of consciousness? Neuroscientist. 2003;9:301–310. doi: 10.1177/1073858403255624. [DOI] [PubMed] [Google Scholar]
- Blumenfeld H, Rivera M, McNally KA, Davis K, Spencer DD, Spencer SS. Ictal neocortical slowing in temporal lobe epilepsy. Neurology. 2004a;63:1015–1021. doi: 10.1212/01.wnl.0000141086.91077.cd. [DOI] [PubMed] [Google Scholar]
- Blumenfeld H, McNally KA, Vanderhill SD, Paige AL, Chung R, Davis K, Norden AD, Stokking R, Studholme C, Novotny EJ, Zubal IG, Spencer SS. Positive and negative network correlations in temporal lobe epilepsy. Cereb Cortex. 2004b;14:892–902. doi: 10.1093/cercor/bhh048. [DOI] [PubMed] [Google Scholar]
- Blumenfeld H. Consciousness and epilepsy: why are patients with absence seizures absent? Prog Brain Res. 2005;150:271–286. doi: 10.1016/S0079-6123(05)50020-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenfeld H, Varghese G, Purcaro MJ, Motelow JE, Enev M, McNally KA, Levin AR, Hirsch LJ, Tikofsky R, Zubal IG, Spencer SS, Paige AL. Cortical and subcortical networks in human secondarily generalized tonic-clonic seizures. Brain. 2009;132:999–1012. doi: 10.1093/brain/awp028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenfeld H. Epilepsy and consciousness. In: Laureys S, Tononi G, editors. The Neurology of Consciousness: Cognitive Neuroscience and Neuropathology. New York: Academic Press; 2009. pp. 15–30. [Google Scholar]
- Blumenfeld H. Epilepsy and the Consciousness System: Mechanisms and Clinical Impact of a Transient Vegetative State. Neurology Clinics. 2011 doi: 10.1016/j.ncl.2011.07.014. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanna AE, Ali F. Epilepsy: The quintessential pathology of consciousness. Behav Neurol. 2011;24:3–10. doi: 10.3233/BEN-2011-0311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanna AE, Monaco F. Brain mechanisms of altered conscious states during epileptic seizures. Nat Rev Neurol. 2009;5:267–276. doi: 10.1038/nrneurol.2009.38. [DOI] [PubMed] [Google Scholar]
- Cavanna AE, Mula M, Servo S, Strigaro G, Tota G, Barbagli D, Collimedaglia L, Viana M, Cantello R, Monaco F. Measuring the level and content of consciousness during epileptic seizures: the Ictal Consciousness Inventory. Epilepsy Behav. 2008;13:184–188. doi: 10.1016/j.yebeh.2008.01.009. [DOI] [PubMed] [Google Scholar]
- Devinsky O, Kelley K, Porter RJ, Theodore WH. Clinical and electroencephalographic features of simple partial seizures. Neurology. 1988;38:1347–1352. doi: 10.1212/wnl.38.9.1347. [DOI] [PubMed] [Google Scholar]
- Englot DJ, Blumenfeld H. Consciousness and epilepsy: why are complex-partial seizures complex? Prog Brain Res. 2009;177:147–170. doi: 10.1016/S0079-6123(09)17711-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Englot DJ, Modi B, Mishra AM, DeSalvo M, Hyder F, Blumenfeld H. Cortical deactivation induced by subcortical network dysfunction in limbic seizures. J Neurosci. 2009;29:13006–13018. doi: 10.1523/JNEUROSCI.3846-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Englot DJ, Yang L, Hamid H, Danielson N, Bai X, Marfeo A, Yu L, Gordon A, Purcaro MJ, Motelow JE, Agarwal R, Ellens DJ, Golomb JD, Shamy MCF, Zhang H, Carlson C, Doyle W, Devinsky O, Vives K, Spencer DD, Spencer SS, Schevon C, Zaveri HP, Blumenfeld H. Impaired consciousness in temporal lobe seizures: role of cortical slow activity. Brain. 2010;133:3764–77. doi: 10.1093/brain/awq316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gastaut H, Broughton R. Epileptic Seizures, Clinical and Electrographic Features, Diagnosis and Treatment. Springfield: Charles C Thomas Pub Ltd; 1972. [Google Scholar]
- Giacino JT, Kalmar K, Whyte J. The JFK Coma Recovery Scale-Revised: measurement characteristics and diagnostic utility. Arch Phys Med Rehabil. 2004;85:2020–2029. doi: 10.1016/j.apmr.2004.02.033. [DOI] [PubMed] [Google Scholar]
- Guye M, Regis J, Tamura M, Wendling F, McGonigal A, Chauvel P, Bartolomei F. The role of corticothalamic coupling in human temporal lobe epilepsy. Brain. 2006;129:1917–28. doi: 10.1093/brain/awl151. [DOI] [PubMed] [Google Scholar]
- ILAE Proposal for revised clinical and electroencephalographic classification of epileptic seizures. From the Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia. 1981;22:489–501. doi: 10.1111/j.1528-1157.1981.tb06159.x. [DOI] [PubMed] [Google Scholar]
- ILAE Proposal for revised classification of epilepsies and epileptic syndromes. Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia. 1989;30:389–399. doi: 10.1111/j.1528-1157.1989.tb05316.x. [DOI] [PubMed] [Google Scholar]
- Inoue Y, Mihara T. Awareness and responsiveness during partial seizures. Epilepsia. 1998;39:7–10. doi: 10.1111/j.1528-1157.1998.tb05142.x. [DOI] [PubMed] [Google Scholar]
- Jacoby A, Snape D, Baker GA. Epilepsy and social identity: the stigma of a chronic neurological disorder. Lancet Neurol. 2005;4:171–178. doi: 10.1016/S1474-4422(05)01014-8. [DOI] [PubMed] [Google Scholar]
- Jones-Gotman M, Smith ML, Risse GL, Westerveld M, Swanson SJ, Giovagnoli AR, Lee T, Mader-Joaquim MJ, Piazzini A. The contribution of neuropsychology to diagnostic assessment in epilepsy. Epilepsy Behav. 2010;18:3–12. doi: 10.1016/j.yebeh.2010.02.019. [DOI] [PubMed] [Google Scholar]
- Lee KH, Meador KJ, Park YD, King DW, Murro AM, Pillai JJ, Kaminski RJ. Pathophysiology of altered consciousness during seizures: Subtraction SPECT study. Neurology. 2002;59:841–846. doi: 10.1212/wnl.59.6.841. [DOI] [PubMed] [Google Scholar]
- Li Q, Luo C, Yang T, Yao Z, He L, Liu L, Xu H, Gong Q, Yao D, Zhou D. EEG-fMRI study on the interictal and ictal generalized spike-wave discharges in patients with childhood absence epilepsy. Epilepsy Res. 2009;87:160–168. doi: 10.1016/j.eplepsyres.2009.08.018. [DOI] [PubMed] [Google Scholar]
- Lings S. Increased driving accident frequency in Danish patients with epilepsy. Neurology. 2001;57:435–439. doi: 10.1212/wnl.57.3.435. [DOI] [PubMed] [Google Scholar]
- Lux S, Kurthen M, Helmstaedter C, Hartje W, Reuber M, Elger CE. The localizing value of ictal consciousness and its constituent functions: a video-EEG study in patients with focal epilepsy. Brain. 2002;125:2691–2698. doi: 10.1093/brain/awf276. [DOI] [PubMed] [Google Scholar]
- Oyegbile TO, Dow C, Jones J, Bell B, Rutecki P, Sheth R, Seidenberg M, Hermann BP. The nature and course of neuropsychological morbidity in chronic temporal lobe epilepsy. Neurology. 2004;62:1736–1742. doi: 10.1212/01.wnl.0000125186.04867.34. [DOI] [PubMed] [Google Scholar]
- Plum F, Posner JB. The diagnosis of stupor and coma. USA: Oxford University Press; 1982. [Google Scholar]
- Reuber M, Kurthen M. Consciousness in nonepileptic attack disorder. Behav Neurol. 2011;24:95–106. doi: 10.3233/BEN-2011-0315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheth SG, Krauss G, Krumholz A, Li G. Mortality in epilepsy: driving fatalities vs other causes of death in patients with epilepsy. Neurology. 2004;63:1002–1007. doi: 10.1212/01.wnl.0000138590.00074.9a. [DOI] [PubMed] [Google Scholar]
- Smith G, Ferguson PL, Saunders LL, Wagner JL, Wannamaker BB, Selassie AW. Psychosocial factors associated with stigma in adults with epilepsy. Epilepsy Behav. 2009;16:484–490. doi: 10.1016/j.yebeh.2009.08.028. [DOI] [PubMed] [Google Scholar]
- Sperling MR, OConnor MJ. Auras and Subclinical Seizures: Characteristics and Prognostic Significance. Ann Neurology. 1990;28:320–328. doi: 10.1002/ana.410280304. [DOI] [PubMed] [Google Scholar]
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- Wirrell EC. Epilepsy-related injuries. Epilepsia. 2006;47:79–86. doi: 10.1111/j.1528-1167.2006.00666.x. [DOI] [PubMed] [Google Scholar]
- Yang L, Morland TB, Schmits K, Rawson E, Narasimhan P, Motelow JE, Purcaro MJ, Peng K, Raouf S, Desalvo MN, Oh T, Wilkerson J, Bod J, Srinivasan A, Kurashvili P, Anaya J, Manza P, Danielson N, Ransom CB, Huh L, Elrich S, Padin-Rosado J, Naidu Y, Detyniecki K, Hamid H, Farooque P, Astur R, Xiao B, Duckrow RB, Blumenfeld H. A prospective study of loss of consciousness in epilepsy using virtual reality driving simulation and other video games. Epilepsy Behav. 2010;18:238–246. doi: 10.1016/j.yebeh.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L, Blumenfeld H. Theories of impaired consciousness in epilepsy. Ann N Y Acad Sci. 2009;1157:48–60. doi: 10.1111/j.1749-6632.2009.04472.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.