Abstract
Background
Because the use of procalcitonin has been advocated as a marker of bacterial infection, this study was carried out to determine the usefulness of serum PCT as an early marker to decide upon intervention for urinary tract infection.
Methods
The subjects were 68 patients with urinary tract infection (UTI) in whom we measured serum procalcitonin concentration at the start of treatment.
Results
There were 47 patients with nonobstructed UTI and 21 with obstructed UTI. All patients with obstructed UTI were subjected to intervention. There were significant differences in procalcitonin, white blood cells, and creatinine levels between patients with nonobstructed and obstructed UTI (P < 0.05).
Conclusion
Although this retrospective study comprised a small number of patients, we found that procalcitonin was a useful marker to decide upon urinary intervention.
Keywords: procalcitonin, intervention, urinary tract infection, urology
Introduction
Urinary tract infections (UTIs) represent a major and common illness. UTIs can also progress to become a serious health concern, with the urinary tract representing the most common source of bacteria in women aged 65 years and older.1,2 For community-dwelling, cognitively intact older women, diagnosis of UTI requires genitourinary symptoms plus significant bacteriuria established by urine culture.3
C-reactive protein is an acute-phase protein produced by the liver in response to tissue injury or infection. However, the C-reactive protein level can also be very high in nonseptic states, eg, postoperatively and in the presence of inflammatory disease.4,5 On the other hand, a definite correlation between infection and change in C-reactive protein has not been documented as yet.
Procalcitonin is a 13 kDa 116-amino acid prohormone of calcitonin. In 1993, Assicot et al6 reported increased procalcitonin concentrations in patients with sepsis and infection. Further clinical studies indicated that bacterial inflammation and sepsis, but not viral infections or autoimmune disorders, could induce high concentrations of serum procalcitonin.6–10
UTI in some cases can progress to urosepsis, for which the treatment options include urinary intervention. No biomarkers to determine whether a urinary intervention is indicated are currently available. The primary goal of the present study was to evaluate the indication for urinary intervention based on the serum procalcitonin level.
Materials and methods
From August 2011 to December 2012, 68 patients with UTI had their procalcitonin levels measured and were evaluated for severity of UTI at our hospital. All patients provided a urine sample for culture before treatment with antibiotics. Serum procalcitonin was determined using a procalcitonin assay (Elecsys Brahms, Thermo Fisher Scientific Inc, Waltham, MA, USA). This electrochemiluminescence immunoassay is intended for use on Elecsys and Cobas E analyzers.11
A procalcitonin level ≥0.50 ng/mL indicates a systemic infection (sepsis), whereas a procalcitonin level ≥2.0 ng/mL indicates that there might be a systemic infection (sepsis), although various conditions are known to elevate procalcitonin as well. It is important to note that a systemic inflammatory response is almost inclusively due to severe bacterial sepsis or septic shock.12
Leukocyte counts were measured using Cellpack (II) and Stromatolyser-FB (II) and platelet counts were measured by Cellpack (II) and Sesheath (II). C-reactive protein was measured using Nanoia® CRP, and creatinine was measured using a Creatinine test kit (Pure Auto S CRE-L; Daiichi-kagaku, Tokyo, Japan).
Urinary intervention was performed immediately in patients with urosepsis (including those with hydronephrosis or urolithiasis) requiring hospitalization at their initial visit, those who were at risk of death from UTI, and those who required urinary intervention (eg, nephrostomy, ureteral stent) on the basis of their clinical course.
Comparisons between groups were performed using the Mann–Whitney U test and Kruskal–Wallis nonparametric analysis of variance. Differences at P < 0.05 were considered to be statistically significant. Receiver operating characteristic analysis was performed to evaluate the ability of procalcitonin to discriminate between the groups.
Results
The mean age of the patients was 65.5 (23–93) years, and there were 40 men and 28 women. There were 58 patients with acute pyelonephritis, 37 without resistant organ acute pyelonephritis, and 21 with obstructed UTI, seven with acute prostatitis, and three with acute epididymitis.
Creatinine and procalcitonin levels were significantly higher in patients with obstructed acute pyelonephritis (P < 0.0001). White blood cells showed significant differences between the groups (P < 0.05). On the other hand, platelet count and C-reactive protein did not differ significantly (Table 2). The characteristics of procalcitonin measurement regarding prediction of UTI are summarized in Table 3. The areas under the receiver operating characteristic curve for procalcitonin, white blood cells, and C-reactive protein were 0.81, 0.68, and 0.56 (Figure 1). Only procalcitonin and C-reactive protein were significantly different between the groups (P < 0.0001).
Table 2.
Laboratory data for 58 patients with acute pyelonephritis
| Non obstructed UTI groups (median) | Obstructed UTI group (median) | P value | |
|---|---|---|---|
| Leukocyte count (/μL) | 11497.3 | 15685.71 | <0.05 |
| CRP (mg/dL) | 10.2 | 14.30 | Ns |
| Creatinine (mg/dL) | 1.22 | 2.37 | <0.0001 |
| Platelet (/μL) | 23.13 | 19.73 | Ns |
| PCT (mg/dL) | 1.88 | 36.67 | <0.0001 |
Abbreviations: CRP, C-reactive protein; PCT, procalcitonin; UTI, urinary tract infection; ns, not significant.
Table 3A.
Characteristics associated with the procalcitonin measurement for prediction of urinary tract infection
| Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | |
|---|---|---|---|---|
| PCT (ng/mL) | ||||
| ≥0.50 | 45.7 | 84.8 | 76.2 | 59.6 |
| ≥2.0 | 56.5 | 82.2 | 61.9 | 78.7 |
Abbreviations: PCT, procalcitonin; PPV, positive predictive value; NPV, negative predictive value.
Figure 1.
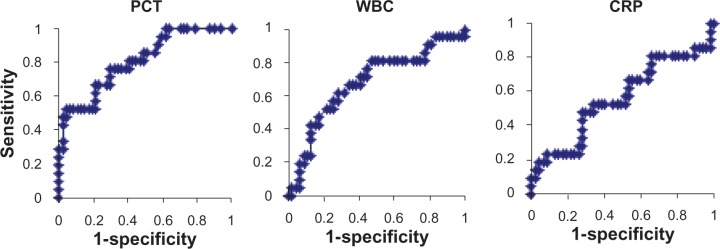
Receiver operating characteristic curves for procalcitonin, white blood cells, and C-reactive protein. The area under the curve for PCT (0.81) was significantly higher than CRP (0.56; P<0.0001).
Abbreviations: PCT, procalcitonin; CRP, C-reactive protein; WBC, white blood cells.
Discussion
UTI is a disease commonly encountered in the clinical setting. Sepsis resulting from UTI is a serious life-threatening condition. It has been reported that the mortality rate due to urosepsis is 16.1%.13 In addition, it has been reported that 78% of urosepsis is due to urinary tract obstruction.14
C-reactive protein is generally regarded as a useful marker for the diagnosis of sepsis and is used along with blood culture. However, these methods are rarely adequate for diagnosing sepsis and a test permitting more rapid and efficient diagnosis has long been necessary.
Procalcitonin is considered to be a useful marker for rapid differential diagnosis of bacterial sepsis and evaluation of its severity.15–19 The recommended treatment for urosepsis is drainage of the obstructed urinary tract to secure its patency and removal of an infected lesion if present. Any delay in providing appropriate treatment can be fatal. The results of our current study showed that all 11 patients with a procalcitonin level ≥10 ng/mL had severe bacterial urosepsis. Of these patients, five also had disseminated intravascular coagulation and eight needed relief of an obstructed urinary tract.20
According to the algorithm for management of urosepsis developed by the European Association of Urology,21 early goal-directed and empirical antibiotic therapy are recommended for patients with signs and symptoms suggestive of urosepsis. Urinary interventions are considered to be effective for the success of early goal-directed therapy.
Clinicians may hesitate to perform urinary interventions (eg, nephrostomy, ureteral stent) in elderly patients, especially those with dementia. However, some patients experience marked worsening of their general condition in as little as one day, and required emergency intervention. Previous reports have described reduced mortality with early goal-directed therapy,22 and early interventions are thought to improve outcomes. In the present study, procalcitonin levels were significantly higher in patients with obstructed UTI compared with those with nonobstructed UTI, indicating the potential of procalcitonin as a useful biomarker for early goal-directed therapy.
The superior value of the procalcitonin level in diagnosis of sepsis when compared with C-reactive protein has already been reported.23,24 In a study comparing PCT with CRP, the diagnostic sensitivity was 77%, specificity was 79%, and the receiver operating characteristic was 85%. Although our study contained a very small number of subjects, our results were similar to those of a large scale meta-analysis.18 Procalcitonin can be a useful biomarker warranting routine measurement when determining whether urinary intervention is indicated.
In conclusion, by comparing two groups of patients, we identified a significantly higher value for procalcitonin in patients with obstructed UTI. As a result, we suggest that the procalcitonin level could be used as a potential bio-marker for the clinician to make a rapid decision regarding whether to proceed to urinary intervention in patients with obstructed UTI.
Table 1.
Patient characteristics
| Non obstructed UTI groups | Obstructed UTI groups | |
|---|---|---|
| Number | 47 | 21 |
| Male/female | 29/18 | 11/10 |
| Age (mean) | 61.3 | 75.1 |
| UTI | ||
| acute pyelonephritis | 37 | 21 |
| acute prostatitis | 7 | 0 |
| acute epididymitis | 3 | 0 |
Abbreviation: UTI, urinary tract infection.
Table 3B.
Procalcitonin ≥0.50 ng/mL
| Non obstructed UTI groups | Obstructed UTI groups | Total | |
|---|---|---|---|
| Positive | 16 | 5 | 21 |
| Negative | 19 | 28 | 47 |
| Total | 35 | 33 | 68 |
Abbreviation: UTI, urinary tract infection.
Table 3C.
Procalcitonin ≥2.0 ng/mL
| Non obstructed UTI groups | Obstructed UTI groups | Total | |
|---|---|---|---|
| Positive | 13 | 8 | 21 |
| Negative | 10 | 37 | 47 |
| Total | 23 | 45 | 68 |
Abbreviation: UTI, urinary tract infection.
Footnotes
Disclosure
The authors declare that they have no conflict of interest in this work.
References
- 1.Leibovici L, Pitlik SD, Konisberger H, Drucker Bloodstream infections in patients older than eighty years. Age Ageing. 1993;22(6):431–442. doi: 10.1093/ageing/22.6.431. [DOI] [PubMed] [Google Scholar]
- 2.Lark RL, Saint S, Chenoweth C, Zemencuk JK, Lipsky BA, Plorde JJ. Four-year prospective evaluation of community-acquired bacteremia: epidemiology, microbiology, and patient outcome. Diagn Microbiol Infect Dis. 2001;41(1–2):15–22. doi: 10.1016/s0732-8893(01)00284-x. [DOI] [PubMed] [Google Scholar]
- 3.Juthani-Mehta M. Asymptomatic bacteriuria and urinary tract infection in older adults. Clin Geriatr Med. 2007;23(3):585–594. doi: 10.1016/j.cger.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 4.Oberhofer D, Juras J, Pavicic AM, Rancic Zuric I, Rumenjak V. Comparison of C-reactive protein and procalcitonin as predictors of postoperative infectious complications after elective colorectal surgery. Croat Med J. 2012;53(6):612–619. doi: 10.3325/cmj.2012.53.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ludwig M, Kummel C, Schroeder-Printzen I, Ringert RH, Weidner W. Evaluation of seminal plasma parameters in patients with chronic prostatitis or leukocytospermia. Andrologia. 1998;30(Suppl 1):41–47. doi: 10.1111/j.1439-0272.1998.tb02825.x. [DOI] [PubMed] [Google Scholar]
- 6.Assicot M, Gendrel D, Carsin H, et al. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993;341(8844):515–518. doi: 10.1016/0140-6736(93)90277-N. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gendrel D, Raymond J, Coste J, et al. Comparison of procalcitonin with C-reactive protein, interleukin 6 and interferon-alpha for differentiation of bacterial vs viral infections. Pediatr Infect Dis. 1999;18(10):875–881. doi: 10.1097/00006454-199910000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Delevaux I, Andre M, Colombier M, et al. Can procalcitonin measurement help in differentiating between bacterial infection and other kinds of inflammatory processes? Ann Rheum Dis. 2003;62(4):337–340. doi: 10.1136/ard.62.4.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gendrel D, Bohuon C. Procalcitonin in pediatrics for differentiation of bacterial and viral infections. Intensive Care Med. 2000;(Suppl 2):S178–S181. doi: 10.1007/BF02900734. [DOI] [PubMed] [Google Scholar]
- 10.Ugarte H, Silva E, Mercan D, De Mendonca A, Vincent JL. Procalcitonin used as a marker of infection in the intensive care unit. Crit Care Med. 1999;27(3):498–504. doi: 10.1097/00003246-199903000-00024. [DOI] [PubMed] [Google Scholar]
- 11.Meisner M. Procalcitonin (PCT) – A New Innovative Infection Parameter. Biochemical and Clinical Aspects. New York, NY: Thieme; 2000. [Google Scholar]
- 12.Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644–1655. doi: 10.1378/chest.101.6.1644. [DOI] [PubMed] [Google Scholar]
- 13.Ackermann RJ, Monroe PW. Bacteremic urinary tract infection in older people. J Am Geriatr Soc. 1996;44(8):927–933. doi: 10.1111/j.1532-5415.1996.tb01862.x. [DOI] [PubMed] [Google Scholar]
- 14.Wagenlehner FM, Pilatz A, Naber KG, Weider W. Therapeutic challenges of urosepsis. Eur J Clin Invest. 2008;38(Suppl 2):45–49. doi: 10.1111/j.1365-2362.2008.02008.x. [DOI] [PubMed] [Google Scholar]
- 15.Aikawa N, Fujishima S, Endo S, et al. Multicenter prospective study of procalcitonin as an indicator of sepsis. J Infect Chemother. 2005;11(3):152–159. doi: 10.1007/s10156-005-0388-9. [DOI] [PubMed] [Google Scholar]
- 16.Muller B, Becker KL, Schachinger H, et al. Calcitonin precursors are reliable markers of sepsis in a medical intensive care unit. Crit Care Med. 2000;28(4):977–983. doi: 10.1097/00003246-200004000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Yukioka H, Yoshida G, Kurita S, Kato N. Plasma procalcitonin in sepsis and organ failure. Ann Acad Med Singapore. 2001;30(5):528–531. [PubMed] [Google Scholar]
- 18.Wacker C, Prkno A, Brunkhorst FM, Schlattmann P. Procalcitonin as a diagnostic marker for sepsis: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13(5):426–435. doi: 10.1016/S1473-3099(12)70323-7. [DOI] [PubMed] [Google Scholar]
- 19.Mitsuma SF, Mansour MK, Dekker JP, et al. Promising new assays and technologies for the diagnosis and management of infectious disease. Clin Infect Dis. 2013;56(7):996–1002. doi: 10.1093/cid/cis1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sugimoto K, Adomi S, Koike H, Esa A. Procalcitonin as an indicator of urosepsis. Res Rep Urol. 2013;5:77–80. doi: 10.2147/RRU.S42711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grabe M, Bjerklund-Johansen TE, Carler JM, et al. Sepsis syndrome in urology (urosepsis): guidelines on urological infections Available from: http://www.uroweb.org/gls/pdf/15_Urological_Infections.pdfAccessed June 15, 2013
- 22.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 23.Tang BM, Eslick GD, Craig JC, McLean AS. Accuracy of procalcitonin for sepsis diagnosis in critically ill patients: systematic review and meta-analysis. Lancet Infect Dis. 2007;7(3):210–217. doi: 10.1016/S1473-3099(07)70052-X. [DOI] [PubMed] [Google Scholar]
- 24.Uzzan B, Cohen R, Nicolas P, et al. Procalcitonin as a diagnostic test for sepsis in critically ill adults and after surgery or trauma: a systematic review and meta-analysis. Crit Care Med. 2006;34(7):1996–2003. doi: 10.1097/01.CCM.0000226413.54364.36. [DOI] [PubMed] [Google Scholar]


