Abstract
A 58-year-old woman living in Reunion Island and returning from Madagascar was hospitalized for neuroinvasive encephalitis and died 1 month later. West Nile virus (WNV) infection was biologically confirmed by detection of immunoglobulin M (IgM) reactive with WNV antigens in both cerebrospinal fluid and serum, and weak neutralizing activity was also detected. A veterinary survey performed in her traveling area showed a seroprevalence of WNV of 28.7% (95% confidence interval [CI] = 21.1–36.3) in adult poultry, confirming an active circulation of the virus. Development of a severe form could be related to a weak antibody response, because the patient presented low IgM and IgG titers. This case report underlines the constant risk of emergence of West Nile in Indian Ocean territories, including Reunion Island where competent vectors are widely present during the whole year.
Background
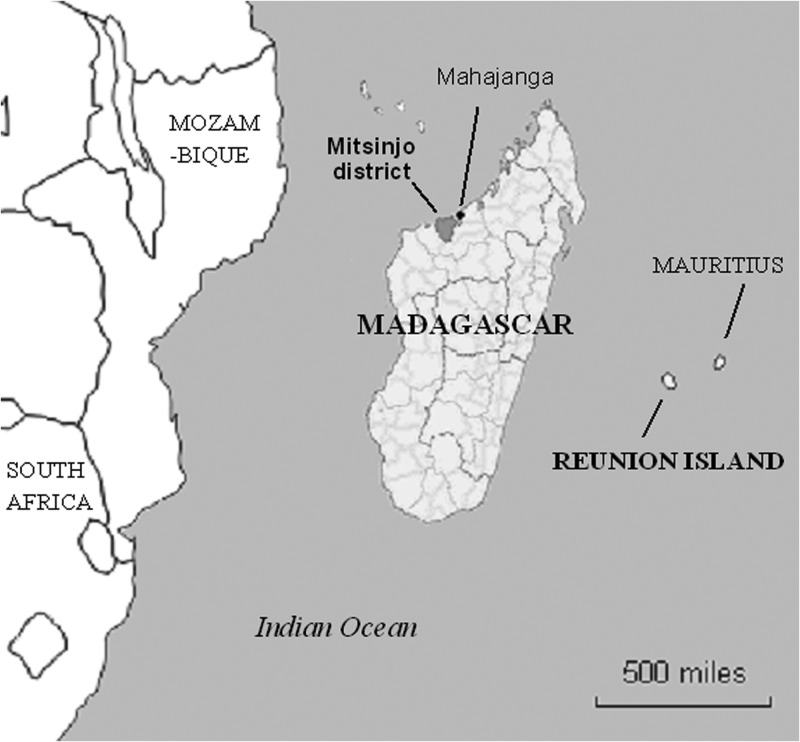
West Nile virus (WNV) is widely distributed around the world. In the Indian Ocean region, it has been responsible for a large outbreak in South Africa in 1974,1 and circulation has been documented in several territories of Africa and Asia (Kenya, South Africa, Madagascar, Thailand, India, etc.),2 although no human epidemics have been reported. In Reunion Island, a French overseas territory 700 km east of Madagascar (Figure 1), a seroprevalence study suggests that WNV might have been circulated a few decades agos,3 but no human case has been confirmed until now. Veterinary surveillance also suggests a past circulation, but is not in favor of a current one (data under publication).
Figure 1.
Localisation of Mitsinjo district (Madagascar) and Réunion Island (France).
Case Report
On May 30, 2011, a 58-year-old woman without medical history apart from a medically managed chronic hypertension living in Reunion Island developed a high fever with a temperature of 40°C. She was just returning from Madagascar where she had spent 2 weeks. Research of malaria parasites was performed by microscopy and immunochromatography and turned out negative.
The first neurological symptoms appeared on May 31, as the patient was clinically presented with encephalitis, manifested as abnormal cerebrospinal fluid (CSF) findings accompanied by confusion and acute flaccid paralysis manifested as asymmetric paralysis and peripheral motor deficits.
On June 4, a CSF examination showed a red blood cell count of 3/mL, white blood cells of 77/mL, comprising 80% lymphocytes, 140 mg/dL protein level, and a normal glucose level. All the criteria for encephalitis were present, i.e., fever > 38°C, neurological signs, and pleocytosis and elevated protein in the CSF (white blood cell count of ≥ 4 cells mm3 or protein level of ≥ 40 mg/dL). Predominance of lymphocytes and negative bacterial culture in the CSF were strongly in favor of a viral etiology but polymerase chain reaction (PCR) studies of her CSF for chikungunya, enterovirus, dengue, West Nile (WN), and herpes viruses were all negative. A serology was also performed for dengue virus (DENV), chikungunya virus, and Rift Valley fever virus and all the results were negative. Presence of immunoglobulin M (IgM) against WNV antigens was documented in both CSF and serum samples using in-house IgM antibody capture-enzyme-linked immunosorbent assay (MAC-ELISA) developed by the French National Reference Center for Arboviruses. In-house indirect IgG ELISA turned out negative. In a late sample drawn at J30 after onset of disease (i.e., 24 days after the early one), in-house MAC-ELISA and indirect IgG ELISA still indicated the presence of IgM and revealed a weak IgG seroconversion. Seroneutralization tests4 also detected a weak level of antibodies with neutralizing activity (50% plaque reduction neutralization test = 20) against WNV.
The patient's condition began to clinically deteriorate 1 week after admission with periods of agitation and confusion and an increase in hyperthermia. She was transferred to a neurology intensive care unit and intubated; her Glasgow coma score was six. Thereafter, there was a partial and gradual improvement of her neurological status (Glasgow score = 11) with slight regression of peripheral motor deficit and confusion but persistent hypotonia and marked asthenia. She died on June 30th of cardiogenic shock after deep and prolonged bradycardia.
Epidemiological and veterinary investigations
The WNV is maintained in nature by a cycle involving mosquitoes and birds, which are presumed to be the most important amplifying hosts.2 Research conducted in Madagascar since 1975 revealed the persistence of an endemic circulation of the WNV in Madagascar.5,6 The patient returned from the province of Mitsinjo, located on the northwest coast of Madagascar (70 km from Mahajanga, Figure 1), where she had spent 15 days from May 14–30, 2011 for hunting; and we precisely found the presence of the virus in that area of Madagascar in August 2009 through the AnimalRisk project.7 Indeed, a survey on animal population was undertaken in several districts recognized as migratory bird spots. A total of 136 blood samples were collected in Mitsinjo, from randomly selected adult poultry: goose (Anser anser), duck (Cairina moscata), chicken (Gallus gallus domesticus), and wild turkey (Meleagris gallopavo). Each serum sample was systematically tested for prE WNV-specific IgG by using a commercial ELISA (competitive ELISA kit, Id-Vet, Montpellier, France) and submitted to plaque reduction neutralization because antibody cross-reactions with others flaviviruses may be encountered. Of the 136 poultry studied, 39 were positive for WNV antibodies, for a seroprevalence of 28.7% (95% confidence interval [CI] = 21.1–36.3). In 1982, 40 WNV strains had also been isolated in Culicidae from Ampijoroa, a town close to Mahajanga; vectors in this province with a dry tropical climate belong to Aedes (Ae. albocephalus, Ae. aegypti, Ae. circumluteolus, Ae. madagascariensis), Anopheles sp. and Culex triaeniorhynchus.8 Furthermore, a seroprevalence survey conducted in 1999 suggested endemic human transmission of WNV in this area, because 10.6% of the children from Mahajanga 15 years of age or less had anti-WNV IgG.9
Conclusions
We reported here a fatal WNV infection in a 58-year-old woman. Despite the documented IgM positivity and IgG seroconversion, infection by another virus should not be totally excluded because cross-reactions between flaviviruses have been extensively described.10 Regarding the negative reverse transcription-PCR (RT-PCR) in both CSF and serum, WNV genetic material can be detected in CSF in < 50% of patients who present with acute meningoencephalitis, and viral loads begin to decrease before or concurrent with IgM development.11 Post-mortem samples could have been useful for virus isolation but unfortunately they could not be performed. An autochthonous infection in Reunion Island is also technically possible, as incubation periods for flaviviruses might exceed 2 weeks. However, to our knowledge, the only other flavivirus likely to be circulating in Madagascar and Reunion Island is DENV, and no transmission was observed in 2011 despite an active surveillance in both countries. Furthermore, DENV RT-PCR and serologies were all negative for the patient. Regarding place of infection, although WNV might have been circulating in Reunion Island several decades ago,3 no confirmed human case has been reported until now and no recent animal infection has been confirmed despite an active surveillance. In view of these elements, diagnosis of a WNV infection imported from Madagascar seems more than probable based on several converging arguments: an IgG seroconversion with a neutralizing activity; the presence of the virus in the area visited by the patient; a very compatible clinical syndrome; and negative results for DENV, which is assumed to be the only other flavivirus likely to circulate in Reunion Island and Madagascar.
Because the patient had traveled in an area where both mosquitoes and birds were found to be infected, and where human transmission is thought to be endemic, the circumstances of the infection were rapidly assumed. Reunion Island belongs to a regional network for epidemiological surveillance and health alert management coordinated by the Indian Ocean Commission (SEGA network), an intergovernmental organization also including Madagascar, Comoros, Mauritius, and Seychelles. All the information about this case was shared as part of this network, so that the Malagasy's surveillance unit could realize an active case research in the indicated area. Since May 15 to the end of the year, there has been neither suspected nor confirmed cases reported, suggesting that the transmission was sporadic.
Neuroinvasive forms of WNV infection represent < 1% of WNV-infected persons.12 Acute flaccid paralysis is also uncommon, but can occur without associated meningitis or encephalitis. It has been described as having a poor long-term outcome, and the fast—but slight—regression of peripheral motor deficit presented by the patient is not usual.13 The patient's only chronic condition that could be related to severity of the disease was hypertension, which has been described as a risk factor for developing a neuroinvasive form of WNV infection,14 even when treated.15
Although it was not the first human West Nile infection documented in Madagascar, the occurrence of this fatal infection underlines the constant risk of emergence of the disease in Indian Ocean territories. Indeed, many islands serve as landing points between Africa and Asia for numerous migratory birds, which constitute a major reservoir for flaviviruses. Once the virus is introduced, three competent vectors widely present during the whole year because of the tropical climate can facilitate its dissemination whatever the season: Culex quinquefasciatus, already shown as responsible for urban transmission cycles of WNV,16 is present in the whole urban areas of Reunion Island; and Culex tritaeniorhynchus and Culex unnivatus, which have been thought to be involved in transmission in Pakistan17 and South Africa,1 are also present in the island to a smaller extent. Although vector competence is influenced by many extrinsic and intrinsic factors, the risk of an outbreak of WNV has therefore to be considered. As a reminder, the introduction of chikungunya virus through an infected traveler returning from Madagascar in Reunion Island, where the population was totally naive, led to the greatest outbreak ever described: between March 2005 and December 2006, 266,000 persons were infected among 780,000 inhabitants.18
This case also raises the need for collaboration between neighboring countries, especially when exposed to similar risks of emergence. Indeed, timely and transparent sharing of information at an international level can be crucial to limit the risk of spread of infectious diseases. The existence of strong links between Reunion Island and Madagascar through the SEGA network allowed this sharing, and complementary investigations were immediately undertaken to detect any spread of the disease.
ACKNOWLEDGMENTS
We are grateful to Caroline Garnier for her help in data collection and to Marc Grandadam for biological analyses.
Footnotes
Authors' addresses: Sophie Larrieu and Elise Brottet, Cellule Interrégionale d'Épidémiologie Océan Indien (Cire OI), Institut de Veille Sanitaire, Saint Denis, La Réunion, France, E-mails: sophie.larrieu@ars.sante.fr and Elise.brottet@ars.sante.fr. Eric Cardinale and Matthieu Roger, CIRAD-UMR, Saint Denis, Réunion, Centre de Recherche et de Veille de l'Océan Indien - Santé Animale, Saint Denis, Réunion, E-mails: eric.cardinale@cirad.fr and roger.matthieu@cirad.fr. Philippe Ocquidant, Centre Hospitalier Réunion, Groupe Hospitalier Sud Réunion (GHSR) - Neuroréanimation, Saint Pierre, Réunion, E-mail: philippe.ocquidant@chr-reunion.fr. Richard Lepec, Commission de l'Océan Indien - (COI), Quatre Bornes, Mauritius, E-mail: richard.lepec@coi-ioc.org. Hélène Delatte, Institut de Recherche et de Développement - Entomologie, Marseille, France, E-mail: Helene.delatte@ird.fr. Guillaume Camuset, Centre Hospitalier Réunion, Groupe Hospitalier Sud Réunion (GHSR) - Maladies Infectieuses, Saint Pierre, Réunion, E-mail: guillaume.camuset@chr-reunion.fr. Philippe Desprès, Institut Pasteur - CNR des Arbovirus, Paris, France, E-mail: philippe.despres@ip.fr. Cyril Charlin, Centre Hospitalier Réunion, Groupe Hospitalier Sud Réunion (GHSR) - Neurologie, Saint Pierre Réunion, E-mail: cyril.charlin@chr-reunion.fr. Alain Michault, Centre Hospitalier Réunion, Groupe Hospitalier Sud Réunion (GHSR) - Laboratoire de Bactériologie-Parasitologie-Virologie-Hygiène Saint Pierre, Réunion, E-mail: alain.michault@chr-reunion.fr.
References
- 1.Jupp PG. The ecology of West Nile virus in South Africa and the occurrence of outbreaks in humans. Ann N Y Acad Sci. 2001;951:143–152. doi: 10.1111/j.1749-6632.2001.tb02692.x. [DOI] [PubMed] [Google Scholar]
- 2.Hayes EB, Komar N, Nasci RS, Montgomery SP, O'Leary DR, Campbell GL. Epidemiology and transmission dynamics of West Nile virus disease. Emerg Infect Dis. 2005;11:1167–1173. doi: 10.3201/eid1108.050289a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kles V, Michault A, Rodhain F, Mevel F, Chastel C. A serological survey regarding Flaviviridae infections on the island of Réunion (1971–1989) Bull Soc Pathol Exot. 1994;87:71–76. [PubMed] [Google Scholar]
- 4.Maeda A, Maeda J. Review of diagnostic plaque reduction neutralization tests for flavivirus infection. Vet J. 2013;195:33–40. doi: 10.1016/j.tvjl.2012.08.019. [DOI] [PubMed] [Google Scholar]
- 5.Rousset D, Andrianarivelo MR. Viruses. In: Goodman SM, Benstead JP, editors. The Natural History of Madagascar. Chicago, IL: The University of Chicago Press; 2003. pp. 165–178. [Google Scholar]
- 6.Morvan J, Chin LH, Fontenille D, Rakotoarivony I, Coulanges P. Prevalence of antibodies to West Nile virus in youngsters from 5 to 20 years old in Madagascar. Bull Soc Pathol Exot. 1991;84:225–234. [PubMed] [Google Scholar]
- 7.Cardinale E, Roger M, Elissa N, Faharoudine A, Girard S, Halifa M, Jaumally MR, Héraud JM, Lalaonirina BA, Laurette S, Lasnes L, Licciardi S, Maquart M, Melanie J, Meenowa D, Olive MM, Rakotoharinome CE, Rakotondravao M, Ravaomanana J. Le réseau régional AnimalRisk dans l'Océan Indien. Bulletin Épidémiologique de l'Anses 2011 [Google Scholar]
- 8.Longchamp C, Migliani R, Ratsitorahina M, Rabarijaona LP, Ramarokoto CE, Rakoto Andrianarivelo M, Rousset D. Persistance d'une circulation endémique du virus West Nile à Madagascar. Arch Inst Pasteur Madagascar. 2003;69:33–36. [PubMed] [Google Scholar]
- 9.Fontenille D, Rodhain F, Digoutte JP, Mathiot C, Morvan J, Coulange P. Transmission cycles of the West Nile virus in Madagascar, Indian Ocean. Ann Soc Belg Med Trop. 1989;69:233–243. [PubMed] [Google Scholar]
- 10.Monath TP, Heinz FX. Flaviviruses. In: Fields BN, Knipe DM, Howley PM, editors. Fields Virology. Philadelphia, PA: Lippincott Raven; 1996. pp. 961–1034. Third edition. [Google Scholar]
- 11.Busch MP, Kleinman SH, Tobler LH, Kamel HT, Norris PJ, Walsh I, Matud JL, Prince HE, Lanciotti RS, Wright DJ, Linnen JM, Caglioti S. Virus and antibody dynamics in acute West Nile virus infection. J Infect Dis. 2008;198:984–993. doi: 10.1086/591467. [DOI] [PubMed] [Google Scholar]
- 12.Hayes EB, Sejvar JJ, Zaki SR, Lanciotti RS, Bode AV, Campbell GL. Virology, pathology, and clinical manifestations of West Nile virus disease. Emerg Infect Dis. 2005;11:1174–1179. doi: 10.3201/eid1108.050289b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sejvar JJ, Haddad MB, Tierney BC, Campbell GL, Marfin AA, Van Gerpen JA, Fleischauer A, Leis AA, Stokic DS, Petersen LR. Neurologic manifestations and outcome of West Nile virus infection. JAMA. 2003;290:511–515. doi: 10.1001/jama.290.4.511. [DOI] [PubMed] [Google Scholar]
- 14.Jean CM, Honarmand S, Louie JK, Glaser CA. Risk factors for West Nile virus neuroinvasive disease, California, 2005. Emerg Infect Dis. 2007;13:1918–1920. doi: 10.3201/eid1312.061265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murray K, Baraniuk S, Resnick M, Arafat R, Kilborn C, Cain K, Shallenberger R, York TL, Martinez D, Hellums JS, Hellums D, Malkoff M, Elgawley N, McNeely W, Khuwaja SA, Tesh RB. Risk factors for encephalitis and death from West Nile virus infection. Epidemiol Infect. 2006;134:1325–1332. doi: 10.1017/S0950268806006339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Molaei G, Cummings RF, Su T, Armstrong PM, Williams GA, Cheng ML, Webb JP, Andreadis TG. Vector-host interactions governing epidemiology of West Nile virus in southern California. Am J Trop Med Hyg. 2010;83:1269–1282. doi: 10.4269/ajtmh.2010.10-0392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Akhter R, Hayes CG, Baqar S, Reisen WK. West Nile virus in Pakistan. III. Comparative vector capability of Culex tritaeniorhynchus and eight other species of mosquitoes. Trans R Soc Trop Med Hyg. 1982;76:449–453. doi: 10.1016/0035-9203(82)90132-8. [DOI] [PubMed] [Google Scholar]
- 18.Renault P, Solet JL, Sissoko D, Balleydier E, Larrieu S, Filleul L, Lassalle C, Thiria J, Rachou E, de Valk H, Ilef D, Ledrans M, Quatresous I, Quenel P, Pierre V. A major epidemic of chikungunya virus infection on Reunion Island, France, 2005–2006. Am J Trop Med Hyg. 2007;77:727–731. [PubMed] [Google Scholar]