Abstract
This pilot study examined the effectiveness of standard care and an empowerment intervention for abused pregnant women. Severe psychological abuse was most prevalent (42.2%) among this sample of women. Compared with women in the standard care group at the post-intervention survey, women in the empowerment group were more likely to hide money (44.6% vs. 34.3%), establish a code with family or friends (19.6% vs. 16.2%), ask neighbors to call police if violence began (6.9% vs. 1.0%), had available bank account numbers (17.1% vs. 3.1%), had valuable jewelry (8.4% vs. 3.8%), and had available a hidden bag with extra clothing (9.0% vs. 3.1%). However, there was no statistically significant difference in health-related quality of life, adoption of safety behaviors, and use of community resources between women in the two groups. Simply asking pregnant women about abuse and offering referral could potentially interrupt and prevent further abuse.
Keywords: Intimate partner violence, Pregnant women, Intervention, Peru
Introduction
Violence against women is a global public health problem. In the recent World Health Organization (WHO) multi-country study on domestic violence, lifetime prevalence of intimate partner physical violence was reported between 13% and 61%, while sexual violence was reported between 6% and 59% (Garcia-Moreno, Jansen, Ellsberg, Heise, & Watts, 2006). In addition, other studies indicate that up to 33.5% women are abused during pregnancy (Jasinski, 2004; Nasir & Hyder, 2003; Valdez-Santiago & Sanin-Aguirre, 1996; Valladares, Pena, Persson, & Hogberg, 2005).
Intimate partner violence (IPV) has been found to be associated with significant physical and psychological health consequences (Coid et al., 2003; Coker et al., 2002), mortality (Campbell et al., 2003), increased health care utilization (Lesserman, Li, Drossman, & Hu, 1998), and health care costs (Rivara et al., 2007). Furthermore, violence against pregnant women not only affects the health and well-being of the pregnant mother, but also that of the infant (Cokkinides, Coker, Sanderson, Addy, & Bethea, 1999; Parker, McFarlane, & Soeken, 1994). Abused pregnant women are at significantly greater risk of miscarriage, abruptio placentae, preterm delivery, perinatal mortality, preeclampsia, and low birthweight (Parker et al., 1994; Sanchez et al., 2008; Valladares, Ellsberg, Pena, Hogberg, & Persson, 2002). Therefore, identification of violence against pregnant women and providing specific intervention efforts targeted at them (Jasinski, 2004) should be an international health priority. In addition, pregnancy is an opportune time to offer interventions as it may be the only time a healthy woman has regular scheduled contact with health care professionals (J. McFarlane, Soeken, & Wiist, 2000).
There have been few studies on violence intervention efforts among pregnant women, and a lack of evidence-based effectiveness of such health service interventions (Nelson, Nygren, McInerney, & Klein, 2004). Only two IPV intervention studies (J. McFarlane et al., 2000; Parker, McFarlane, Soeken, Silva, & Reel, 1999) have met eligibility criteria of the third United States Preventive Services Task Force (USPSTF, 2004) on routine screening for family and IPV. These studies used an empowerment intervention that is based on an abuse prevention protocol (J. McFarlane & Parker, 1994) developed from an empowerment model (Dutton, 1992). The empowerment model is based on the premise that women experience violence because of the lack of control of their lives and the coercive control of the abuser. One way to alleviate such controlling behavior is to help women gain increased independence and control of life situations through empowerment training.
There is limited information on the prevalence of violence against pregnant women in Peru. A recent cross-sectional violence survey among 2,394 post-partum women found that the lifetime experience of any IPV (physical, psychological, or sexual abuse) was 45.1% (Perales et al., 2009). The prevalence of lifetime physical, psychological, and sexual IPV among abused women was 34.2%, 28.4% and 8.7%, respectively. Notably, 21.5% of these women reported experiencing any IPV during the current pregnancy, including 11.9% reporting any physical abuse, 15.6% reporting any psychological abuse, and 3.9% reporting any sexual abuse. These results are comparable to the findings of the recent WHO study (Garcia-Moreno et al., 2006). The high prevalence of violence among pregnant women in Peru is astounding, and reflects an urgent need for implementation of intervention efforts. Although Peru is one of the first countries in Latin America to adopt special legislation on domestic violence and established women’s police stations and one-stop centers for victims of domestic violence, implementation and practice of the laws have been difficult (Human Rights Watch, 2000). As a result, Peruvian women remain at high risk for IPV. To our knowledge, no IPV intervention studies have been conducted in Peru. As such, we utilized the standard care (abuse assessment and referral card) and empowerment (abuse assessment, referral and social worker case management) interventions in a pilot IPV intervention project among pregnant women who receive routine prenatal care in Lima, Peru. Specifically, we sought to describe the frequency and severity of physical, psychological, and sexual abuse among pregnant women, and examine the outcomes of the interventions, i.e., health-related quality of life, safety behaviors adopted by these women, and their use of community resources.
Methods
Study Design and Setting
This study design is a randomized, two-arm trial utilizing two levels of abuse intervention. The first arm, the standard care arm included an abuse assessment and a referral card. The second arm, the empowerment intervention included an abuse assessment, referral card, and social worker case management. The empowerment intervention has been widely used in studies among Hispanic, African American, and white pregnant women in the US (J. McFarlane et al., 2000; J. M. McFarlane, Groff, O’Brien, & Watson, 2006) and Chinese women in Hong Kong (Tiwari et al., 2005). Outcome measures were differences in health-related quality of life, adoption of safety behaviors, and use of community resources between the groups at postnatal interviews.
The study was conducted at the Instituto Nacional Materno Perinatal (INMP), Lima, Peru. This hospital is operated by the Peruvian government, primarily provides maternity services to low-income women residing in Lima, and is a national referral hospital for high-risk obstetric cases. Approximately 1,500 pregnant women are typically seen at INMP each month. The institutional review boards of INMP, Lima and the University of Washington, Seattle approved this study.
Interviewer Training
Study personnel included four hospital-based social workers who were trained on interviewing skills, contents of the questionnaire, safety plan development, and ethical conduct of violence research (including issues of safety and confidentiality) before the implementation of the project. Representatives from women’s organizations in Lima and a legal counsel from the Family Criminal Law Division provided information about social and legal services available to abused women. Social workers were able to offer these information to the abused women, and also refer women to these services.
Study Sample and Procedure
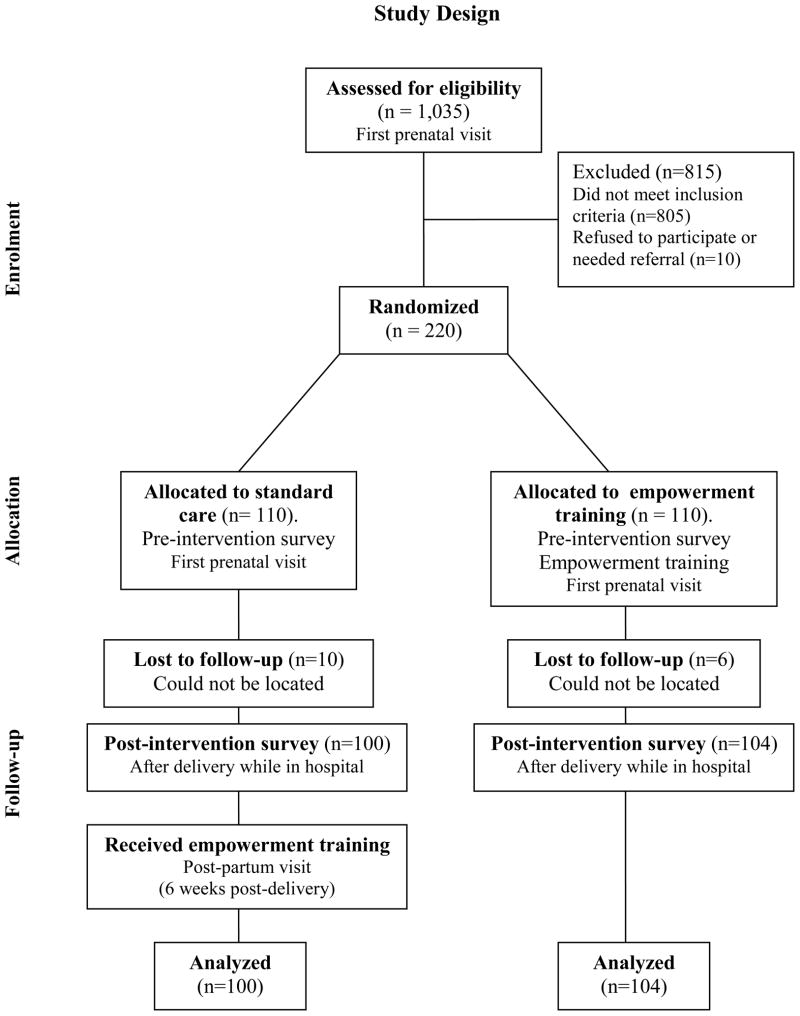
Prenatal care patients (between 12 and 26 weeks gestation) attending care at the INMP were screened for IPV by trained social workers using the modified Abuse Assessment Screen (AAS) (J. McFarlane & Parker, 1994). Participant recruitment occurred between January 9 and July 26, 2007. Test-retest reliability of the AAS was established at 0.97 and criteria-related validity was established against national survey instruments (Soeken, McFarlane, & Parker, 1998). Women were asked whether a former or current partner had pushed, shoved, slapped, hit, kicked or otherwise physically hurt them, or forced them into sexual activities in the past 12 months. Women who responded ‘yes’ to one of the questions on the modified AAS were eligible for entry into the study. Only women who spoke and understood Spanish, screened positive for IPV in the past 12 months, and who were between the ages of 18 and 45 years were included in the study. A total of 1,035 pregnant women were screened for abuse, 230 women screened positive, eight refused to participate, and two requested referral for psychological support and were excluded from the study. Thus, we enrolled 220 abused women, with 110 women randomly assigned to each intervention arm. Assignments to study arm was done using a randomized block design at recruitment (Figure 1). Sixteen women (7.3%) were lost to follow-up.
Figure 1.
Women were given an explanation of the study purpose, protocol, and follow-up schedule. All study material including consent form were translated into Spanish using backward and forward methods. Social workers administered informed consent and verbally administered interview questionnaires using the Conflict Tactics Scale-Revised (CTS2) (M.A. Straus, Hamby, Boney-McCoy, & Sugarman, 1996), the Short Form Health Survey (SF-36) (Ware, Snow, & Kosinski, 1993), a modified Safety Behavior Checklist (J. McFarlane & Parker, 1994), and a community resource use assessment. All in-person interviews were conducted in private, in a room. To minimize participant burden, women could stop the interview at any point with the option to continue the interview within a one- or two-day period, and were offered a small meal after the interview. Follow-up post-intervention interviews were conducted during the week when women were still in the hospital following delivery, and were conducted in a private interview room or in their single hospital room. To eliminate participant bias, the post-intervention interviewer was different from the pre-intervention interviewer.
Measures
The CTS2 (M.A. Straus et al., 1996) was used to measure the type, frequency, and severity of partner violence. It is comprised of 39 items with five scales that measure the magnitude of physical assault (e.g., slapping, kicking, or beating), psychological aggression (e.g., yelling/screaming or threatening), injury (e.g., bruises or needing a doctor as a result of a fight), sexual aggression (e.g., coercing or forcing a partner to have sex), and use of negotiation (e.g., expressing opinions) to resolve conflict by partners. The 39 items in the CTS2 are categorized as minor or severe within each scale. A description of items that are included in the minor and severe categories for each scale is provided in the Conflict Tactics Scale Handbook (Straus, Hamby, & Warren, 2003). Participants were asked to rate whether a behavior had never occurred, occurred once, twice, 3–5, 6–10, 11–20, or more than 20 times in the past year, or had occurred, but not in the past year. Chronicity refers to the frequency with which behaviors endorsed on the CTS2 have been reported by a respondent over the course of the prior year (Straus et al., 2003). For this study, reliability of CTS2 scales as measured by Cronbach’s α were 0.84 (physical assault), 0.38 (injury), 0.75 (sexual coercion), and 0.75 (psychological aggression). The CTS2 has the advantage of enhanced content validity and reliability, increased clarity and specificity and additional items for the psychological aggression scale (Straus et al., 1996). CTS2 has also been used among Spanish-speaking participants (Bonomi, Holt, Thompson, & Martin, 2005; Connelly, Newton, & Aarons, 2005).
The SF-36 was used to assess quality of life of the abused woman (Ware et al., 1993). This survey consists of 36 items with one item measuring health transition, and 35 items categorized within eight scales, including physical functioning, role limitation due to physical and emotional health problems, bodily pain, general health, vitality, social functioning, and mental health. Scores for items within each scale were summed and transformed to a standardized range (0 to 100). Higher scale scores indicated better health-related quality of life. The reliability (Cronbach’s α) of SF-36 scales in the present study are as follow: 0.87 (physical functioning), 0.75 (role-physical), 0.76 (bodily pain), 0.63 (general health), 0.63 (vitality), 0.83 (social functioning), 0.49 (role-emotional), and 0.78 (mental health).
We used a modified Safety Behavior Checklist with 13 items that were culturally appropriate to Peru. The original 15-item safety behavior survey was developed as part of the March of Dimes protocol (J. McFarlane & Parker, 1994). The proportion of women who adopted each safety behavior was calculated by dividing the number of women who adopted the behavior by the number of women who indicated that the behavior was applicable to them.
We used a modified community resource use assessment (J. M. McFarlane et al., 2006) to determine women’s use of seven different types of community resources to help end abuse. These resources included agencies dealing with alcohol or drug treatment, battered women’s groups, church or clergy, healthcare, legal services, police, or social services. Women were asked if they used any of the resources in the past three months prior to the pre- and post-intervention interviews.
Interventions
Standard care intervention
Women randomized to receive standard care received a wallet-size referral card listing agencies that provide IPV services to abused women (e.g., legal, social services, and law enforcement). No counseling, advocacy, education or other services were offered to women in this group at the pre-intervention interview. However, they were provided the empowerment intervention, specifically supportive counseling and education, and advice in the areas of safety, by a trained social worker at the conclusion of the study during the sixth-week postpartum visit. This one-on-one counseling session usually lasted about 30 minutes.
Empowerment intervention
In addition to receiving a referral card, women in the empowerment intervention received supportive counseling and education, and advice in the areas of safety by a trained social worker at the pre-intervention interview. This one-on-one counseling session lasted about 30 minutes. Interviewers listened empathetically to the women, and acknowledged their perceptions and feelings. Women were reminded that they are not at fault for violent incidents, and that many women report experiences of abuse. Interviewers also helped women understand the cycle of violence (Walker, 1979), and reviewed components of the safety plan including behaviors indicated in the Safety Behavior Checklist. For example, women were asked how they might secure and hide money and important documents such as birth certificates. Interviewers also provided suggestions on where to hide money or important documents, and helped women develop a code to use with family and trusted friends to signal the need for assistance and/or to mentally plan their escape when needed. Throughout the intervention session, women were asked to appraise the safety of adopting each behavior to minimize any violence that may result from the women’s participation in the study. Women were given a brochure with a 13-item safety plan to reinforce safety behaviors that were discussed during the intervention session. To make the safety plan brochure less conspicuous, other prenatal brochures on topics such as breastfeeding or nutrition were also offered to the women. In addition to the safety plan, the interviewers provided a list of community resources, such as emergency shelter, legal aid, law enforcement, and counseling, and strategies for seeking help from these resources. As part of the intervention, interviewers also offered to assist women with telephone calls to social service agencies or women’s groups who could act as advocates for abused women. At the conclusion of the empowerment intervention session, interviewers helped women determine if it was safe for her to keep the safety plan brochure and the referral card. In addition to the aforementioned protocol, each woman in the empowerment training intervention received supportive care, validation of feelings, empathetic listening, and information on what to expect when seeking help from legal resources, shelters, law enforcement, or counseling services. Women were free to discuss the pros and cons of leaving the abuser, reporting the abuser to law enforcement or applying for a protection order.
Data analysis
Data was entered into EPI INFO (Version 3.3.2), and analyzed using Statistical Package for Social Sciences (SPSS) (version 13.0, SPSS Inc., Chicago, IL, USA). Two sample t-tests and chi-square tests of mean differences with 95% confidence interval were calculated to compare the difference between the two intervention groups.
Results
Women in the intervention and standard care groups did not differ with regards to age, educational attainment, marital status, housing status, employment, and access to basic foods and medical care (Table 1). More than 50% of participants were between 20 and 29 years of age, had six or less years of education, unmarried, and unemployed. Women in both the empowerment and standard care arms reported having limited access to basic foods and medical care. Smoking during pregnancy is not a prevalent characteristic (less than 10%) in this study sample. Less than one third of the participants indicated that they consumed any alcoholic beverages during the index pregnancy. Of this sample of women, approximately 3% of those in the empowerment group indicated that they had used illicit drugs during the index pregnancy (Table 1). Between 3% and 6% of women indicated that their partners used illicit drugs, and between 30% and 40% of women indicated that their partners sometimes consumed alcohol (Table 1).
Table 1.
Selected Sociodemographic Characteristics of Participants and Partners.
| Characteristics | Intervention group | Standard care | p-valuea | ||
|---|---|---|---|---|---|
| n | Percentage | n | Percentage | ||
| Maternal age (years; mean±SD) | 104 | 25.8 ± 5.00 | 100 | 26.5 ± 5.86 | 0.386b |
| Maternal age (years) | |||||
| < 20 | 11 | 10.6 | 8 | 8.0 | 0.105 |
| 20 – 29 | 65 | 62.5 | 65 | 65.0 | |
| 30 – 34 | 23 | 22.1 | 14 | 14.0 | |
| 35 and older | 5 | 4.8 | 13 | 13.0 | |
| Education level | |||||
| More than 12 years | 37 | 35.6 | 33 | 33.0 | 0.481 |
| 7 – 12 years | 14 | 13.5 | 9 | 9.0 | |
| Less than or equal to 6 years | 53 | 51.0 | 58 | 58.0 | |
| Marital status | |||||
| Married, living with husband | 10 | 9.6 | 8 | 8.0 | 0.669 |
| Other | 93 | 89.4 | 92 | 92.0 | |
| Missing | 1 | 1.0 | 0 | 0.0 | |
| Mestizo | 88 | 84.6 | 90 | 90.0 | 0.345 |
| Home owner | 9 | 8.7 | 14 | 14.0 | 0.227 |
| Unemployed | 68 | 65.4 | 60 | 60.0 | 0.426 |
| Limited access to basic foods | 53 | 51.0 | 52 | 52.0 | 0.882 |
| Limited access to medical care | 67 | 64.4 | 64 | 64.0 | 0.950 |
| Smoked during pregnancy | 9 | 8.7 | 5 | 5.0 | 0.302 |
| Consumed alcoholic beverages during pregnancy | 30 | 28.8 | 25 | 25.0 | 0.536 |
| Used illicit drugs during pregnancy | 3 | 2.9 | 0 | 0.0 | 0.247c |
| Partner’s age (years) | |||||
| < 20 | 3 | 2.9 | 1 | 1.0 | 0.468c |
| 20 – 29 | 55 | 52.9 | 52 | 52.0 | |
| 30 – 34 | 24 | 23.1 | 31 | 31.0 | |
| 35 and older | 21 | 20.2 | 16 | 16.0 | |
| Missing | 1 | 1.0 | 0 | 0.0 | |
| Partner’s education level | |||||
| More than 12 years | 31 | 29.8 | 34 | 34.0 | 0.779 |
| 7 – 12 years | 5 | 4.8 | 6 | 6.0 | |
| Less than or equal to 6 years | 65 | 62.5 | 59 | 59.0 | |
| Missing | 3 | 2.9 | 1 | 1.0 | |
| Partner used alcohol | |||||
| Rarely | 64 | 61.5 | 58 | 58.0 | 0.663 |
| Sometimes | 39 | 37.5 | 31 | 31.0 | |
| Missing | 1 | 1.0 | 11 | 11.0 | |
| Partner used illicit drugs | |||||
| No | 88 | 84.6 | 88 | 88.0 | 0.747c |
| Yes | 4 | 3.8 | 6 | 6.0 | |
| Missing | 12 | 11.5 | 6 | 6.0 | |
Chi-square test;
Student T-test;
Fisher’s Exact Test
Compared with women in the standard care group at baseline, women in the empowerment group reported a slightly higher prevalence of minor physical assault (26.0% vs. 23.5%), minor injury (13.2% vs. 10.8%), minor sexual coercion (16.7% vs. 10.3%), and severe psychological aggression (42.2% vs. 39.2%). Women in the empowerment group had lower severe injury (2.5% vs. 3.9%), and severe sexual coercion (6.9% vs. 10.3%) when compared with women in the standard care group. Overall, severe psychological aggression was most prevalent among women in this sample, followed by minor physical assault, minor sexual coercion and minor injury (Table 2).
Table 2.
Prevalence and 95% Confidence Intervals for CTS2 Abuse Scales (at baseline).
| Intervention group (n=104) | Standard care (n=100) | |||
|---|---|---|---|---|
|
| ||||
| Prevalence (%) | 95% confidence interval | Prevalence (%) | 95% confidence interval | |
| Physical assault | ||||
| Minora | 26.0 | 19.9, 32.0 | 23.5 | 17.7, 29.4 |
| Severeb | 23.0 | 17.2, 28.8 | 23.0 | 17.2, 28.8 |
| Injury | ||||
| Minor | 13.2 | 8.6, 17.9 | 10.8 | 6.5, 15.1 |
| Severe | 2.5 | 0.3, 4.6 | 3.9 | 1.3, 6.6 |
| Sexual coercion | ||||
| Minor | 16.7 | 11.5, 21.8 | 10.3 | 6.1, 14.5 |
| Severe | 6.9 | 3.4, 10.3 | 10.3 | 6.1, 14.5 |
| Psychological aggression | ||||
| Minor | 7.4 | 3.8, 10.9 | 8.8 | 4.9, 12.7 |
| Severe | 42.2 | 35.4, 48.9 | 39.2 | 32.5, 45.9 |
Minor only, without endorsement of any severe items;
Severe, with or without endorsement of any minor items.
Women in the empowerment group (mean = 31.21, SD = 47.72) had greater mean chronicity of severe sexual coercion when compared with women in the standard care group (mean = 18.05, SD = 32.83) (Table 3). However, there was no statistically significant difference between women in the empowerment group and the standard care group in relation to mean chronicity of physical assault, injury, sexual coercion, and psychological aggression in the 12 months prior to baseline interview.
Table 3.
Chronicity of Abuse in the Past 12 Months, CTS2 (at baseline)
| Intervention group | Standard care | Group difference | 95% confidence interval | t-test p-value | |||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| n | Mean | Standard deviation | n | Mean | Standard deviation | ||||
| Physical assault | |||||||||
| Minora | 53 | 4.94 | 6.65 | 48 | 5.29 | 7.18 | −0.35 | (−3.08, 2.38) | 0.801 |
| Severeb | 47 | 41.09 | 47.42 | 47 | 43.47 | 54.6 | −2.38 | (−23.33, 18.57) | 0.822 |
| Injury | |||||||||
| Minor | 27 | 4.59 | 7.48 | 22 | 5.23 | 11.26 | −0.63 | (−6.04, 4.77) | 0.814 |
| Severe | 5 | 13.4 | 22.72 | 8 | 13.50 | 12.83 | −0.1 | (−21.56, 21.36) | 0.992 |
| Sexual coercion | |||||||||
| Minor | 34 | 8.94 | 11.9 | 21 | 5.38 | 7.05 | 3.56 | (−2.20, 9.32) | 0.220 |
| Severe | 14 | 31.21 | 47.72 | 21 | 18.05 | 32.83 | 13.17 | (−14.47, 40.81) | 0.340 |
| Psychological aggression | |||||||||
| Minor | 15 | 16.73 | 16.56 | 18 | 18.83 | 23.1 | −2.1 | (−16.65, 12.45) | 0.770 |
| Severe | 86 | 47.98 | 40.08 | 80 | 46.44 | 39.71 | 1.54 | (−10.70, 13.78) | 0.804 |
Minor only, without endorsement of any severe items;
Severe, with or without endorsement of any minor items.
Women in both groups had higher scores for physical functioning, role-physical and emotional scales, bodily pain, vitality, and social functioning at the post-intervention interview. Overall, there was no statistically significant difference in the mean difference of frequency scores between baseline and post-intervention data among the two groups of women (Table 4).
Table 4.
SF-36 Mean Frequency Scores for Women Randomized to Empowerment Intervention and Standard Care groups.
| Intervention group (n=104) | Standard care group (n=100) | Between group difference (95% CI) | t-test p-value | |
|---|---|---|---|---|
|
| ||||
| Difference between baseline and post-intervention mean frequency score (SD) | Difference between baseline and post-intervention mean frequency score (SD) | |||
| Physical functioning | −15.67 (28.35) | −15.70 (25.06) | 0.03 (−7.37, 7.42) | 0.994 |
| Role-Physical | −15.14 (38.23) | −11.25 (31.26) | −3.89 (−13.56, 5.77) | 0.428 |
| Bodily pain | −7.40 (28.33) | −7.90 (24.28) | 0.50 (−6.80, 7.79) | 0.893 |
| General health | 5.30 (15.62) | 4.74 (14.67) | 0.56 (−3.63, 4.74) | 0.793 |
| Vitality | −0.19 (22.34) | −3.65 (22.06) | 3.46 (−2.67, 9.59) | 0.268 |
| Social functioning | −0.36 (34.94) | −3.50 (37.06) | 3.14 (−6.80, 13.08) | 0.534 |
| Role-Emotional | −6.41 (47.16) | −4.00 (34.91) | −2.41 (−13.90, 9.08) | 0.680 |
| Mental health | 2.50 (20.95) | −2.04 (19.61) | 4.54 (−1.07, 10.15) | 0.112 |
We examined change in the prevalence of women who adopted safety behaviors between the pre- and post-intervention interviews. There was an increase in the number of women (1.8% to 30.3%) who adopted safety behaviors for eight of the 13 behaviors in the intervention arm. This was contrasted by an increase of 0.5% and 11.2% of women who adopted safety behaviors in four of the 13 safety behaviors in the standard care arm (results not shown). Compared with women in the standard care group, more women in the empowerment group hid money (44.6% vs. 34.3%; p-value 0.144), established a code with family or friends (19.6% vs. 16.2%; p-value=0.525), asked neighbors to call police if violence begins (6.9% vs. 1.0%; p-value=0.065), had available bank account numbers (17.1% vs. 3.1%; p-value=0.108), had available valuable jewelry (8.4% vs. 3.8%; p-value=0.330), and had available a hidden bag with extra clothing (9.0% vs. 3.1%; p-value=0.135) at the post-intervention interview (Table 5). However, these findings were not statistically significant.
Table 5.
Descriptive Statistics for Safety Behavior That were Adopted by Participants at Post-intervention.
| Safety behavior | Intervention group | Standard care group | Chi-square p-value | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| n | Yes | % | n | Yes | % | ||
| Hid money | 101 | 45 | 44.6 | 96 | 33 | 34.3 | 0.144 |
| Hid extra set of house and car keys | 101 | 49 | 48.5 | 98 | 48 | 49.0 | 0.948 |
| Established signal with family or friends | 102 | 20 | 19.6 | 99 | 16 | 16.2 | 0.524 |
| Asked neighbors to call police if violence begins | 101 | 7 | 6.9 | 100 | 1 | 1.0 | 0.065 |
| Available social security numbers (self, partner, children) | 37 | 20 | 54.1 | 34 | 20 | 58.8 | 0.686 |
| Available rent receipts | 48 | 15 | 31.3 | 49 | 19 | 38.8 | 0.437 |
| Available birth certificates (self and children) | 98 | 74 | 75.5 | 91 | 68 | 74.7 | 0.901 |
| Available ID or driver’s license (self and children) | 104 | 96 | 92.3 | 100 | 92 | 92.0 | 0.935 |
| Available bank account numbers | 35 | 6 | 17.1 | 32 | 1 | 3.1 | 0.108 |
| Available marriage certificate | 15 | 7 | 46.7 | 19 | 11 | 57.9 | 0.515 |
| Available valuable jewelry | 83 | 7 | 8.4 | 78 | 3 | 3.8 | 0.330 |
| Available important phone numbers (e.g., police, ambulance, hospital) | 104 | 65 | 62.5 | 100 | 60 | 60.0 | 0.714 |
| Available hidden bag with extra clothing | 100 | 9 | 9.0 | 96 | 3 | 3.1 | 0.135 |
Both groups of women were more likely to seek help from the church and the police than from other community resources (Table 6). There was no statistically significant difference in the type of community resource accessed by the two groups of women at post-intervention.
Table 6.
Community Resource Use for the Three Months Prior to Pre- and Post-intervention Surveys
| Intervention group (n=104) | Standard care group (n=100) | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Pre-intervention | Post-intervention | Pre-intervention | Post-intervention | |||||
|
| ||||||||
| n | % | n | % | n | % | n | % | |
| Alcohol or drug abuse treatment center | 1 | 0.96 | 0 | 0 | 2 | 2.00 | 0 | 0 |
| Battered women’s organization | 1 | 0.96 | 1 | 0.96 | 1 | 1.00 | 1 | 1.00 |
| Church | 4 | 3.85 | 2 | 1.92 | 8 | 8.00 | 1 | 1.00 |
| Healthcare center | 3 | 2.88 | 0 | 0 | 2 | 2.00 | 1 | 1.00 |
| Legal | 2 | 1.92 | 2 | 1.92 | 3 | 3.00 | 3 | 3.00 |
| Police | 6 | 5.77 | 1 | 0.96 | 7 | 7.00 | 4 | 4.00 |
| Social services organization | 3 | 2.88 | 2 | 1.92 | 2 | 2.00 | 2 | 2.00 |
Discussion
This report is the first to our knowledge to pilot the use of an empowerment intervention that includes a discussion of safety planning with abused pregnant women in Peru. This project highlighted the feasibility of conducting an IPV intervention with follow-up among abused Peruvian women. We documented good success in participation (95.7%) and follow-up (92.7%) rates. Approximately 90% of the women in this study are of Mestizo race. This distribution is representative of the distribution of racial groups in the Lima region. Thirteen of the 16 women lost of follow-up were Mestizos. There is no differential in the race of women lost to follow-up between the two study arms. Our study is limited by sample size and duration of follow-up. Despite the lack of statistically significant findings, our study is broadly in agreement with results of prior studies (J. McFarlane, Parker, Soeken, Silva, & Reel, 1998; J. M. McFarlane et al., 2006) with regards to adoption of safety behaviors. We do not have post-intervention abuse information, but several investigators have reported a reduction in violence during the first postnatal year when an empowerment intervention was offered to women during pregnancy (Parker et al., 1999; Tiwari et al., 2005).
There has only been a small number of intervention studies that have targeted pregnant women. These interventions have ranged from providing abused women with a referral card listing community resources to unlimited counseling and advocacy by mentors (J. McFarlane & Gondolf, 1998; J. McFarlane et al., 2000; J. McFarlane & Wiist, 1997; J. M. McFarlane et al., 2006; Tiwari et al., 2005). Use of intervention methods that include supportive counseling, advocacy, and empowerment of women have been shown to be effective in reducing violence, increasing the adoption of safety behavior and use of community resources (J. McFarlane et al., 2000; J. M. McFarlane et al., 2006; Parker et al., 1999; Tiwari et al., 2005). Other investigators (J. McFarlane et al., 2000; J. M. McFarlane et al., 2006) have reported that just asking pregnant women about abuse may in and of itself be the most effective intervention. This is because disclosure of abuse by women and the corresponding validation of the women’s feelings helps women know that abuse is common and that their feelings are valued.
The goal of empowering abused women, to help them gain better control of their lives can be a means for reducing abuse. However, it is important to consider that abused women are a heterogeneous group with differences in histories of oppression and family structure. As a result, there is not one intervention plan that fits all. Kasturirangan (2008) reviewed the use of empowerment in the context of violence intervention programs, and suggested that empowerment needs to be viewed as a process and abused women at different stages in the continuum of empowerment. Within the empowerment process, abused women should be engaged in defining goals and actions. Goals and actions of the women should be shaped by their own values that are rooted in individual personality and culture, and would depend on the stage that they are at in the continuum of empowerment. Women, however, may need counseling support in setting goals. When women have determined goals, they can then identify appropriate and available resources needed to achieve those goals. Depending on the type of goals, intervention programs may be able to offer further support by providing transportation, childcare, counseling, shelter, or peer support groups. A critical characteristic of violence intervention programs is that programs need to be flexible, value self-determination of women and distributive justice (Kasturirangan, 2008). Future studies may explore further the use of empowerment training for different forms of IPV and the types of interventions that would be appropriate for men who are perpetrators of IPV in Peru.
We acknowledge that while providing abused women with 30-minute counseling and case management, such as that used in this study is very beneficial, it may not be a feasible option in a resource-limited setting that has high IPV risk like Lima. Building the physical infrastructure and human capacity to provide abused women with intensive case-management are likely to be daunting tasks. Based on our experiences working with abused women in Lima, Peru, we expect that a combination of intervention methods that include screening, counseling and advocacy by both healthcare professionals and community outreach workers may empower abused women to seek help and subsequently, reduce IPV in Peru. There needs to be concerted efforts by both public and private organizations to collaborate and pool resources to reduce IPV in Peru. In addition, laws and policies related to IPV that are in place, have not been fully implemented and enforced (Sagot, 2005). An important initial step would be to implement and evaluate existing policies related to IPV; enforced laws designed to protect abused women; as well as design, monitor and evaluate IPV intervention programs for their efficacy in meeting the needs of affected women and family members.
Results from this study differed from those reported of abused Chinese women in Hong Kong (Tiwari et al., 2005). Tiwari et al. (2005) found that the abused women who received the empowerment intervention had improved emotional and physical well-being (role-physical and role-emotional in the SF-36). One difference that was noted in the Hong Kong study was the use empathetic understanding in addition to the empowerment model. The use of empathetic understanding proved to be effective in helping women who experienced psychological abuse. In addition, we did not assess depression as an independent psychological outcome in this study. Although women in Hong Kong and Peru experience a high prevalence of psychological abuse (Perales et al., 2009; Tiwari et al., 2005), we expect that there would be differences in exposure to and coping mechanisms of psychologic stress, and types and extent of social support in these two study populations, thus leading to different outcomes.
Several studies have documented an increase in the adoption of safety behaviors following an intervention that discussed safety behaviors (J. McFarlane et al., 2004; Parker et al., 1999). Even though there was no statistically significant difference in the adoption of safety behavior between the two groups of women, there was a general trend of greater numbers of women in the intervention arm adopting safety behaviors. All the safety behaviors required planning and forethought. Abused women may not have thought of these actions as safety behavior. But, a discussion of these behaviors may have prompted the women to consider how adopting these behaviors may affect their safety, and the benefit of adopting such actions.
Community resource use during the three months prior to pre-intervention and post-intervention interviews was low in this study. The absence of a distinct difference in the use of community groups between the two arms may be attributed to the fact that both groups were offered a referral card that listed several organizations that provide services to abused women in Lima. Despite devastating effects of abuse on women’s lives, studies suggest that many women do not seek help (Du Mont, Forte, Cohen, Hyman, & Romans, 2005; Henning & Klesges, 2002). A cross-sectional survey on lifetime and during pregnancy abuse in Lima, Peru, found that abused women do not seek help. Some prominent reasons include the acceptance of violence as a way of life and the presence of fear of retaliation from the perpetrator (unpublished results). These attitudes are consistent with findings by Garcia-Moreno et al. (2005). It is known that many individual, interpersonal and sociocultural factors along with severity of abuse influence women’s decision to seek help (Liang, Goodman, Tummala-Narra, & Weintraub, 2005; J. McFarlane, Soeken, Reel, Parker, & Silva, 1997). Some investigators found that abused women if they sought help, were more likely to seek help from informal sources (e.g., relatives, friends, neighbors), rather than formal sources (e.g., battered women organizations, police, legal aid) (Coker, Derrick, Lumpkin, Aldrich, & Oldendick, 2000; West, Kantor, & Jasinski, 1998). In this study, we only asked women if they used formal sources of help, and did not ask about informal sources of help. Women in Peru who have sought help from formal sources have experienced a lack of response from the police or found the justice system to be ineffective (Sagot, 2005). Furthermore, domestic violence is often not deemed serious enough to warrant punishment of perpetrators (Human Rights Watch, 2000). As a result, informal help may be seen as a major source of assistance to abused women as well as a pathway to more formal types of help from health, criminal justice, and social service system (Kaukinen, 2002). Alternatively, abused women may turn to formal services for help only when informal contacts fail to provide the help needed (Dutton, 1996). It is important to realize that even if abused women decided to seek help from formal sources, they must know that services exist and perceive the services to be helpful. In addition, the services must be accessible to them both in locality and cost. Little is known about abuse women’s help-seeking behavior in Peru. More research needs to be conducted to understand abused women’s perceived benefits of case management, and formal and informal community resources.
We were not able to determine whether the lack of help-seeking behavior in this sample of women was due to a decrease in abuse during pregnancy, or whether women simply lack the physical and emotional capacity to deal with or respond to the abuse when pregnant. It may be that a pregnant woman’s priority is to get through the pregnancy first, and then manage or deal with the abuse after the birth of the infant, unless there was an immediate threat to her life and that of the unborn child.
Results from this study must be interpreted within the context of several limitations. First, it was not possible to assign abused women to a true no-treatment control group because it would be unethical. Furthermore, results from past IPV intervention studies (cMFarlane et al., 2004; J. McFarlane et al., 2000; Parker et al., 1999) indicate that simply asking pregnant women about abuse and offering referral does increase her sensitivity to the topic, and often motivates her to increase health-seeking behavior, which indirectly is an intervention in and of itself. Second, we only conducted one post-intervention assessment with the participants of this study. There might not have been sufficient time for women to consider and adopt safety behaviors, or seek help between the first and the second interview. Future studies should include a longer follow-up period during post-partum. In addition, we do not have information on the severity of abuse during pregnancy, which could influence a woman’s decision to adopt safety behaviors or seek help. Third, a common criticism of the CTS is that it counts acts of violence, without accounting for the context in which the violence occurs (M.A. Straus, 1990). In addition, the measurement relies on self-reports, which are subject to recall errors. Fourth, one CTS2 scale (injury) and three SF-36 scales (general health, vitality and role-emotional) had Cronbach’s α <0.70. Thus, these scales are likely to have had low internal consistency in this sample of Peruvian women. The SF-36 may not be the most appropriate instrument to be used in this population. A quality of life instrument may perhaps, be more appropriate. Fifth, the small sample size and single site may limit generalizability of the findings. Future studies should consider using a larger and more diverse population of pregnant women. Finally, the women’s current and former intimate partners would have played a key role in the abusive relationship. However, they were not included in this study. The reported outcomes only reflected the women’s efforts in reducing IPV without taking the partner’s actions into account. Future studies could also consider including men in intervention programs.
Conclusions
This pilot project demonstrated the feasibility of conducting a follow-up intervention study among abused women in Lima, Peru. Women in the empowerment training group tended to adopt more safety behaviors when compared with women in the standard care group. Although there were no statistically significant findings, our study is broadly in agreement with results of prior empowerment intervention studies with regards to adoption of safety behaviors (J. McFarlane et al., 1998; J. M. McFarlane et al., 2006). Asking pregnant women about abuse and offering referral could potentially interrupt and prevent further IPV. We expect that a combination of formal and informal network of resources and support may help reduce IPV in Lima, Peru.
Acknowledgments
Special thanks to all the women who participated in this study. We are very grateful to the contributions of our team, Nely Ojeda, Silvia Tacuri, Sara Vilca, Maria Luisa Jimenéz, Susana Chavéz, and Gina Yañez. This research was supported by the Bill and Melinda Gates Foundation and by an award from the National Institutes of Health, Center for Minority Health and Health Disparities (T37-MD001449).
Contributor Information
Swee May Cripe, University of Washington.
Sixto Sanchez, Gineco Obstetra, Epidémiólogo, Hospital Nacional Dos de Mayo and Universidad San Martin de Porres, Lima, Peru.
Elena Sanchez, Proyectos Salud & Consultores, E.I.R.L., Lima, Peru.
Beatriz Ayala Quintanilla, Instituto Nacional de Salud, Lima, Peru.
Christian Hernández Alarcon, Fiscal Provisional Adjunto Superior de la 8va. Fiscala Superior de Lima, Peru.
Bizu Gelaye, University of Washington.
Michelle A. Williams, University of Washington
References
- Bonomi AE, Holt VL, Thompson RS, Martin DP. Ascertainment of intimate partner violence in women seeking legal protection. American Journal of Preventive Medicine. 2005;28(1):52–58. doi: 10.1016/j.amepre.2004.09.011. [DOI] [PubMed] [Google Scholar]
- Campbell J, Webster D, Koziol-McLain J, Block C, Campbell D, Curry MA, et al. Risk factors for femicide in abusive relationships: results from a multisite case control study. American Journal of Public Health. 2003;93(7):1089–1097. doi: 10.2105/ajph.93.7.1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coid J, Petruckevitch A, Chung WS, Richardson J, Moorey S, Cotter S, et al. Sexual violence against adult women primary care attenders in east London. British Journal of General Practice. 2003;53(496):858–862. [PMC free article] [PubMed] [Google Scholar]
- Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, et al. Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine. 2002;23(4):260–268. doi: 10.1016/s0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- Coker AL, Derrick C, Lumpkin JL, Aldrich TE, Oldendick R. Help-seeking for intimate partner violence and forced sex in South Carolina. American Journal of Preventive Medicine. 2000;19(4):316–320. doi: 10.1016/s0749-3797(00)00239-7. [DOI] [PubMed] [Google Scholar]
- Cokkinides VE, Coker AL, Sanderson M, Addy C, Bethea L. Physical violence during pregnancy: maternal complications and birth outcomes. Obstetrics and Gynecology. 1999;93(5 Pt 1):661–666. doi: 10.1016/s0029-7844(98)00486-4. [DOI] [PubMed] [Google Scholar]
- Connelly CD, Newton RR, Aarons GA. A psychometric examination of English and Spanish versions of the Revised Conflict Tactics Scales. Journal of Interpersonal Violence. 2005;20(12):1560–1579. doi: 10.1177/0886260505280341. [DOI] [PubMed] [Google Scholar]
- Du Mont J, Forte T, Cohen MM, Hyman I, Romans S. Changing help-seeking rates for intimate partner violence in Canada. Women and Health. 2005;41(1):1–19. doi: 10.1300/J013v41n01_01. [DOI] [PubMed] [Google Scholar]
- Dutton M. Empowering and healing the battered women. New York: Springer-Verlag; 1992. [Google Scholar]
- Dutton M. Impact of evidence concerning battering and its effects in criminal trials involving battered women. Washington, DC: National Law Center, George Washington University; 1996. [Google Scholar]
- Garcia-Moreno C, Heise L, Jansen HA, Ellsberg M, Watts C. Public health. Violence against women. Science. 2005;310(5752):1282–1283. doi: 10.1126/science.1121400. [DOI] [PubMed] [Google Scholar]
- Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. Lancet. 2006;368(9543):1260–1269. doi: 10.1016/S0140-6736(06)69523-8. [DOI] [PubMed] [Google Scholar]
- Henning KR, Klesges LM. Utilization of counseling and supportive services by female victims of domestic abuse. Violence and Victims. 2002;17(5):623–636. doi: 10.1891/vivi.17.5.623.33714. [DOI] [PubMed] [Google Scholar]
- Human Rights Watch. [Assessed on March 1, 2007];HRW memorandum on Peru’s Law of Protection from Family Violence. 2000 http://www.hrw.org/backgrounder/wrd/peru-women.htm.
- Jasinski JL. Pregnancy and domestic violence: a review of the literature. Trauma Violence Abuse. 2004;5(1):47–64. doi: 10.1177/1524838003259322. [DOI] [PubMed] [Google Scholar]
- Kasturirangan A. Empowerment and programs designed to address domestic violence. Violence Against Women. 2008;14(12):1465–1475. doi: 10.1177/1077801208325188. [DOI] [PubMed] [Google Scholar]
- Kaukinen C. The help-seeking of women violence crime victims: Findings from the Canadian violence against women survey. International Journal of Sociology and Social Policy. 2002;22(7–8):5–44. [Google Scholar]
- Lesserman J, Li Z, Drossman DA, Hu YJB. Selected symptoms associated with sexual and physical abuse history among female patients with gastrointestinal disorders: The impact in subsequent healthcare visits. Psychological Medicine. 1998;28(2):417–425. doi: 10.1017/s0033291797006508. [DOI] [PubMed] [Google Scholar]
- Liang B, Goodman L, Tummala-Narra P, Weintraub S. A theoretical framework for understanding help-seeking processes among survivors of intimate partner violence. American Journal of Community Psychology. 2005;36(1–2):71–84. doi: 10.1007/s10464-005-6233-6. [DOI] [PubMed] [Google Scholar]
- McFarlane J, Gondolf E. Preventing abuse during pregnancy: a clinical protocol. MCN; American Journal of Maternal Child Nursing. 1998;23(1):22–26. doi: 10.1097/00005721-199801000-00005. quiz 27. [DOI] [PubMed] [Google Scholar]
- McFarlane J, Malecha A, Gist J, Watson K, Batten E, Hall I, et al. Increasing the safety-promoting behaviors of abused women. American Journal of Nursing. 2004;104(3):40–50. doi: 10.1097/00000446-200403000-00019. quiz 50-41. [DOI] [PubMed] [Google Scholar]
- McFarlane J, Parker B. Abuse during pregnancy: A protocol for prevention and intervention. New York: National March of Dimes Education Foundation; 1994. [Google Scholar]
- McFarlane J, Parker B, Soeken K, Silva C, Reel S. Safety behaviors of abused women after an intervention during pregnancy. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 1998;27(1):64–69. doi: 10.1111/j.1552-6909.1998.tb02592.x. [DOI] [PubMed] [Google Scholar]
- McFarlane J, Soeken K, Reel S, Parker B, Silva C. Resource use by abused women following an intervention program: associated severity of abuse and reports of abuse ending. Public Health Nursing. 1997;14(4):244–250. doi: 10.1111/j.1525-1446.1997.tb00297.x. [DOI] [PubMed] [Google Scholar]
- McFarlane J, Soeken K, Wiist W. An evaluation of interventions to decrease intimate partner violence to pregnant women. Public Health Nursing. 2000;17(6):443–451. doi: 10.1046/j.1525-1446.2000.00443.x. [DOI] [PubMed] [Google Scholar]
- McFarlane J, Wiist W. Preventing abuse to pregnant women: implementation of a “mentor mother” advocacy model. Journal of Community Health Nursing. 1997;14(4):237–249. doi: 10.1207/s15327655jchn1404_3. [DOI] [PubMed] [Google Scholar]
- McFarlane JM, Groff JY, O’Brien JA, Watson K. Secondary prevention of intimate partner violence: a randomized controlled trial. Nursing Research. 2006;55(1):52–61. doi: 10.1097/00006199-200601000-00007. [DOI] [PubMed] [Google Scholar]
- Nasir K, Hyder AA. Violence against pregnant women in developing countries: review of evidence. European Journal of Public Health. 2003;13(2):105–107. doi: 10.1093/eurpub/13.2.105. [DOI] [PubMed] [Google Scholar]
- Nelson HD, Nygren P, McInerney Y, Klein J. Screening women and elderly adults for family and intimate partner violence: a review of the evidence for the U. S. Preventive Services Task Force. Annals of Internal Medicine. 2004;140(5):387–396. doi: 10.7326/0003-4819-140-5-200403020-00015. [DOI] [PubMed] [Google Scholar]
- Parker B, McFarlane J, Soeken K. Abuse during pregnancy: effects on maternal complications and birth weight in adult and teenage women. Obstetrics and Gynecology. 1994;84(3):323–328. [PubMed] [Google Scholar]
- Parker B, McFarlane J, Soeken K, Silva C, Reel S. Testing an intervention to prevent further abuse to pregnant women. Research in Nursing and Health. 1999;22(1):59–66. doi: 10.1002/(sici)1098-240x(199902)22:1<59::aid-nur7>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Perales MT, Cripe SM, Lam N, Sanchez SE, Sanchez E, Williams MA. Prevalence, types, and pattern of intimate partner violence among pregnant women in Lima, Peru. Violence Against Women. 2009;15(2):224–250. doi: 10.1177/1077801208329387. [DOI] [PubMed] [Google Scholar]
- Rivara FP, Anderson ML, Fishman P, Bonomi AE, Reid RJ, Carrell D, et al. Healthcare utilization and costs for women with a history of intimate partner violence. American Journal of Preventive Medicine. 2007;32(2):89–96. doi: 10.1016/j.amepre.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Sagot M. The critical path of women affected by family violence in Latin America: case studies from 10 countries. Violence Against Women. 2005;11(10):1292–1318. doi: 10.1177/1077801205280189. [DOI] [PubMed] [Google Scholar]
- Sanchez SE, Qiu C, Perales MT, Lam N, Garcia P, Williams MA. Intimate partner violence (IPV) and preeclampsia among Peruvian women. European Journal of Obstetrics, Gynecology, and Reproductive Biology. 2008;137(1):50–55. doi: 10.1016/j.ejogrb.2007.05.013. [DOI] [PubMed] [Google Scholar]
- Soeken K, McFarlane J, Parker B. The abuse assessment screen. A clinical instrument to measure frequency, severity, and perpetrator of abuse against women. In: Campbell JC, editor. Empowering survivors of abuse: Health care for battered women and their children. Thousand Oaks, CA: Sage; 1998. pp. 195–203. [Google Scholar]
- Straus MA. The Conflict Tactics Scales and its critics: an evaluation and new data on validity and reliability. In: Straus MA, Gelles J, editors. Physical Violence in American Families: Risk Factors and Adaptations to Violence in 8,145 Families. New Brunswick, NJ: Transaction Publishers; 1990. pp. 51–73. [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised Conflict Tactics Scales (CTS2): development and preliminary psychometric data. Journal of Family Issues. 1996;17:283–316. [Google Scholar]
- Straus MA, Hamby SL, Warren WL. The Conflict Tactics Scales Handbook. Los Angeles: Western Psychological Services; 2003. [Google Scholar]
- Tiwari A, Leung WC, Leung TW, Humphreys J, Parker B, Ho PC. A randomised controlled trial of empowerment training for Chinese abused pregnant women in Hong Kong. British Journal of Obstetrics and Gynaecology. 2005;112(9):1249–1256. doi: 10.1111/j.1471-0528.2005.00709.x. [DOI] [PubMed] [Google Scholar]
- USPSTF. Screening for Family and Intimate Partner Violence: Recommendation Statement. United States Preventive Services Task Force. Annals of Internal Medicine. 2004;140(5):382–386. doi: 10.7326/0003-4819-140-5-200403020-00014. [DOI] [PubMed] [Google Scholar]
- Valdez-Santiago R, Sanin-Aguirre LH. Domestic violence during pregnancy and its relationship with birth weight. Salud Publica de Mexico. 1996;38(5):352–362. [PubMed] [Google Scholar]
- Valladares E, Ellsberg M, Pena R, Hogberg U, Persson LA. Physical partner abuse during pregnancy: a risk factor for low birth weight in Nicaragua. Obstetrics and Gynecology. 2002;100(4):700–705. doi: 10.1016/s0029-7844(02)02093-8. [DOI] [PubMed] [Google Scholar]
- Valladares E, Pena R, Persson LA, Hogberg U. Violence against pregnant women: prevalence and characteristics. A population-based study in Nicaragua. British Journal of Obstetrics and Gynaecology. 2005;112(9):1243–1248. doi: 10.1111/j.1471-0528.2005.00621.x. [DOI] [PubMed] [Google Scholar]
- Walker L. The battered woman. New York: Harper and Rowe; 1979. [Google Scholar]
- Ware JE, Snow KK, Kosinski M. SF-36 Health Survey - Manual and Interpretation Guide. Boston, MA: The Health Institute; 1993. [Google Scholar]
- West CM, Kantor GK, Jasinski JL. Sociodemographic predictors and cultural barriers to help-seeking behavior by Latina and Anglo American battered women. Violence and Victims. 1998;13(4):361–375. [PubMed] [Google Scholar]