Abstract
INTRODUCTION
Epidermoid cysts, also called atheromas, are frequently observed. These cysts originate mostly in the pilosebaceous apparatus but rarely in areas without hair, such as the palm and sole. The mechanism of their development has been reported to be epidermal inclusion secondary to trauma or human papillomavirus (HPV)-60 infection. We report the patient who developed an epidermoid cyst in the palm without any known cause.
PRESENTATION OF CASE
A 93-year-old male noticed a mass in the left palm 3 years earlier, was diagnosed with an epidermoid cyst based on incisional biopsy, and underwent incision drainage several times during the 3-year period. However, since the cyst spontaneously ruptured and was infected, debridement and resection of the cyst were performed. The postoperative course was favorable, without signs of infection. The pathological diagnosis of the resected specimen was an epidermoid cyst.
DISCUSSION
This case was a rare epidermoid cyst originating in an area without hair, and there was neither a clear history of injury nor findings strongly suggesting HPV-60 infection. Causes other than repeated loading on the palm could not be considered for epidermal inclusion. To our knowledge, this case is the largest reported epidermoid cyst.
CONCLUSION
Epidermoid cysts are frequently observed, but their development in areas without hair is rare, and its mechanism has not been clarified. The association between this cyst and trauma or HPV is clear. However, repeated loading on areas such as the palm that tend to undergo chronic loading can also be a cause, as in this patient.
Keywords: Epidermoid cyst, Large, Atheroma, Palm
1. Introduction
Epidermoid cysts are included in atheromas as epithelial cysts.1 They originate mostly in the pilosebaceous apparatus and relatively rarely in areas without hair, such as the palm and sole. The mechanism of the development of these cysts is considered to be epidermal inclusion secondary to trauma or human papillomavirus (HPV) infection.1–12 We report a patient who developed a large epidermoid cyst in an area without hair without any known cause, and was successfully treated surgically.
2. Presentation of case
The patient was a 93-year-old male with a history of cerebral and myocardial infarction. When he visited our hospital, his general condition was favorable. He noticed a mass in the left palm without any known cause, such as trauma, 3 years earlier. There was neither tenderness in the mass area nor neurological symptoms of the fingers. The mass was elastic and soft, and there were no findings suggesting its adhesion to subcutaneous tissue. Since the mass was 5 cm in diameter, the possibility of a malignant tumor was also considered at the first consultation, and diagnosis was entrusted to an institution specializing in tumors (Shizuoka Cancer Center). As a result of incisional biopsy, no tumor cells were observed, only keratinized tissue was identified, and a diagnosis of an epidermoid cyst was made (Fig. 1). Subsequently, incision/drainage was performed several times, but recurrence repeated. The mass slightly increased (7 cm × 7 cm) and spontaneously ruptured (Fig. 2A and B). No motor impairment of the fingers was observed, but slight numbness of the thumb was present as a neurological finding. Plain X-ray examination showed a mass with decreased radiolucency in the thenar (Fig. 2C), while MRI revealed a well-delineated mass showing a low intensity area on T1-weighted images and a high intensity area on T2-weighted images in the thenar muscles (Fig. 2D and E).
Fig. 1.
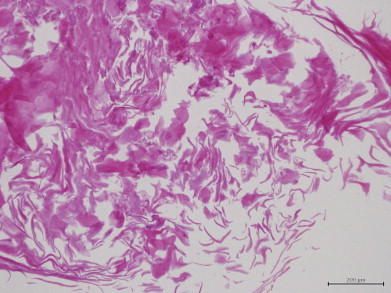
Findings on incisional biopsy (hematoxylin–eosin staining; scale, 200 μm). No tumor cells were observed, and only keratinized tissue was present.
Fig. 2.

Preoperative findings (A) and (B) the mass was 7 cm × 7 cm in size and had spontaneously ruptured. (C) Plain X-ray examination showed a mass with decreased radiolucency in the thenar. (D) and (E) MRI showed a well-delineated mass with a low intensity area on T1-weighted images and a high intensity area on T2-weighted images in the thenar muscles.
Based on these findings, a diagnosis of an epidermoid cyst was made, and the mass was resected. The cyst contained a malodorous yellowish white porridge-like material with blood (Fig. 3A). The mass was encapsulated and present in the thenar muscles, and showed no adhesion to the surrounding tissue (Fig. 3B). The capsule was detached and resected (Fig. 3C), and the deep flexor tendon was confirmed, but no clear contamination was observed.
Fig. 3.
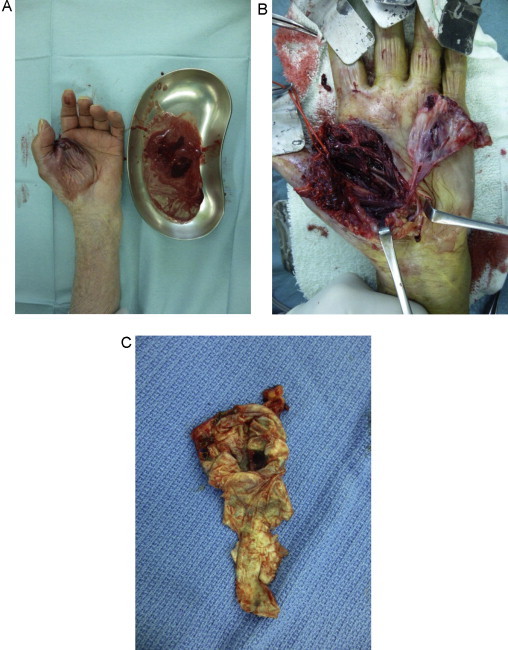
Surgical findings (A) the mass contained a malodorous yellowish white porridge-like material with blood. (B) The mass was encapsulated and present in the thenar muscles, and showed no adhesion to the surrounding tissue. (C) The resected capsule.
Histopathological examination showed a stratified squamous epithelium structure similar to that of the skin and a clear granular layer. There was no abnormal proliferation of cells suggesting malignancy. Neither eccrine glands nor hair tissue structures were confirmed in any cross-section. In the cyst cavity, only floating keratinized tissue was observed, and foreign-body reactions were absent (Fig. 4; Table 1).
Fig. 4.
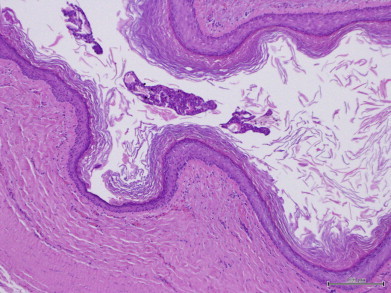
Histopathological findings (hematoxylin–eosin staining; scale, 100 μm). A squamous cell epithelium structure and a clear granular layer were present. In the cyst cavity, only floating keratinized tissue was observed. There was no abnormal cell proliferation suggesting malignancy.
Table 1.
Reported cases of epidermoid cysts in the hand.
| No. | Author | Age | Sex | Affected site | Cause | Size (mm) | Treatment | Recurrence |
|---|---|---|---|---|---|---|---|---|
| 1 | Henry (2009) | 59 | M | Finger | Skin graft | 7.5 | Resection | – |
| 2 | De Giorgi (2006) | 62 | M | Palm | Repeated loading | 20 | Resection | ? |
| 3 | Haga (2005) | 57 | M | Finger | Verruca | 10 | Resection | ? |
| 4 | Yokogawa (2002) | 65 | F | Palm | Unknown | Small, multiple | Resection | ? |
| 5 | Ward (1985) | 33 | M | Palm | Repeated loading | ? | Resection | – |
| 6 | 16 | M | Palm | Repeated loading | ? | Resection | – | |
| 7 | Ikegami (2003) | 77 | F | Finger | Trauma (Crush) | 15 × 20 | Resection | – |
| 8 | Vergles (2009) | 54 | F | Finger | Idiopathic | 2 | Resection | – |
| 9 | Hung (2012) | 16 | F | Finger | Idiopathic | 11 | Resection | – |
| 10 | Baran (1988) | 45 | F | Finger | Trauma (Crush) | ? | Resection | – |
| 11 | 19 | F | Finger | Trauma (Crush) | ? | Resection | – |
M, male; F, female.
His postoperative course was favorable. There were neither signs of infection nor motor impairment of the fingers 6 months after the operation. The numbness of the thumb preoperatively observed improved.
3. Discussion
In diagnosis, epidermoid cysts should be differentiated first from trichilemmal cysts as benign tumors classified as atheromas. Differentiation from trichilemmal cysts is difficult based on clinical findings, but is possible based on histopathological findings. Trichilemmal cysts show specific keratinization without a granular layer, called trichilemmal keratinization.1,6 Since a clear granular layer was histopathologically confirmed in this patient (Fig. 4), a trichilemmal cyst was excluded.
In recent years, the cause of epidermoid cysts originating in areas without hair has been considered to be epidermal inclusion secondary to trauma or HPV infection.1–12 Concerning the types of trauma, crush injuries have often been reported.1,2,9 In addition, cases after skin transplantation6 or cryotherapy for a wart5 have been reported. There have also been cases due to repeated physical loading on the area,3,11 and many cases with an unknown cause.7,10,12 Lincoski et al. investigated epidermoid cysts in the hand, and reported that 83% of the patients were female, and a history of trauma was present in 48% or all patients.8 Our patient also had no clear history of trauma or treatment.
Concerning HPV infection, cases secondary to HPV-60 infection have been reported.5,12 In such cases, the characteristic histopathological findings are vacuolated cells and keratohyalin granules.12 Recent studies have suggested the involvement of eccrine glands, leading to the theory that epidermoid metaplasia of eccrine glands occurs due to HPV infection.4,5,12 We did not perform virus examination to evaluate the possible association between HPV infection and this case. However, since histological examination did not confirm vacuolated cells, keratohyalin granules, or eccrine glands, their association was unlikely.
Since the cyst size was large in this patient, there was a possibility of malignant transformation. The differential diagnosis includes basal cell carcinoma, cell carcinoma, and Bowen's disease, although their incidences are very low. In the presence of these diseases, abnormal cell proliferation specific to malignant findings is observed. Differentiation is performed by confirming palisading or destruction of the basement membrane. In this patient, histopathological examination showed no clear cell proliferation, excluding malignant transformation. Based on these findings, repeated loading on the palm for many years may have been involved in this case, although the cause of the cyst was unknown.
We performed surgery for this patient for a number of reasons. First, spontaneous rupture increased the risk of infection. Another reason was the possibility of malignant transformation since repeated recurrence was observed. The other reason was difficulty in radical surgery, considering his age (93 years), even if malignant transformation was present. Thus, we selected simple resection.
4. Conclusion
Epidermoid cysts are frequently observed, but their development in areas without hair is rare, and its mechanism has not been clarified. The association between this cyst and trauma or HPV is clear. However, repeated loading on areas such as the palm that tend to undergo chronic loading can also be a cause, as in this patient. To our knowledge, this case is the largest reported epidermoid cyst.
Conflict of interest statement
None.
Funding
No funds were received in support of this study.
Consent
Written informed consent was obtained from patient's parents for publication of this case report and accompanying images. A copy of the written consents are available for review by Editor-in-Chief of this journal on request.
Author contributions
All authors have contributed significantly, and that all authors are in agreement with the content of the manuscript.
Motoshi Gomi, Kiyohito Naito and Osamu Obayashi performed operation and ward management; Kiyohito Naito and Osamu Obayashi diagnosed; and Motoshi Gomi and Kiyohito Naito wrote the paper.
References
- 1.Ikegami T., Kameyama M., Orikasa H., Yamazaki K. Trichilemmal cyst in the pulp of the index finger: a case report. Hand Surgery. 2003;8:253–255. doi: 10.1142/s0218810403001765. [DOI] [PubMed] [Google Scholar]
- 2.Baran R., Broutart J.C. Epidermoid cyst of the thumb presenting as pincer nail. Journal of American Academy of Dermatology. 1988;19:143–144. doi: 10.1016/s0190-9622(88)80236-6. [DOI] [PubMed] [Google Scholar]
- 3.De Giorgi V., Sestini S., Nardini P., Lotti T. Palmoplantar cysts: sebaceous or epidermoid cysts. Journal of the European Academy of Dermatology and Venereology. 2006;20:1026–1027. doi: 10.1111/j.1468-3083.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- 4.Egawa K., Kitasato H., Ono T. A palmar epidermoid cyst, showing histological features suggestive of eccrine duct origin, developing after a bee-sting. British Journal of Dermatology. 2000;143:469–470. doi: 10.1046/j.1365-2133.2000.03697.x. [DOI] [PubMed] [Google Scholar]
- 5.Haga T., Okuyama R., Tagami H., Egawa K., Aiba S. Demonstration of human papillomavirus type 60 in an epidermoid cyst developing in the finger pulp of the thumb. Dermatology. 2005;211:296–297. doi: 10.1159/000087029. [DOI] [PubMed] [Google Scholar]
- 6.Henry F.P., Healy C.E., O’Broin E. Epidermoid cyst post dermofasciectomy. Journal of Plastic, Reconstructive Aesthetic Surgery. 2010;63:e44–e45. doi: 10.1016/j.bjps.2009.05.019. [DOI] [PubMed] [Google Scholar]
- 7.Hung T., Yang A., Binder S.W., Barnhill R.L. Cutaneous ciliated cyst on the finger: a cutaneous mullerian cyst. American Journal of Dermatopathology. 2012;34:335–338. doi: 10.1097/DAD.0b013e3182330550. [DOI] [PubMed] [Google Scholar]
- 8.Lincoski C.J., Bush D.C., Millon S.J. Epidermoid cysts in the hand. Journal of Hand Surgery (European Volume) 2009;34:792–796. doi: 10.1177/1753193409347509. [DOI] [PubMed] [Google Scholar]
- 9.Saint Onge R.A., Jackson I.T. An uncommon sequel to thumb trauma: epidermoid cyst. Hand. 1977;9:52–56. doi: 10.1016/s0072-968x(77)80032-6. [DOI] [PubMed] [Google Scholar]
- 10.Vergles D., Horzic M., Cupurdija K., Lackovic Z., Vergles J.M. Epidermoid cyst on top of the left arm thumb. American Journal of Dermatopathology. 2009;31:723–724. doi: 10.1097/DAD.0b013e31818d0bec. [DOI] [PubMed] [Google Scholar]
- 11.Ward W.A., Labosky D.A. Ruptured epidermal inclusion cyst of the palm presenting as collar-button abscess. Journal of Hand Surgery (American Volume) 1985;10:899–901. doi: 10.1016/s0363-5023(85)80170-2. [DOI] [PubMed] [Google Scholar]
- 12.Yokogawa M., Egawa K., Dabanaka K., Wada E., Miyoshi K., Ikeda M., Honda Y., Kitasato H., Kodama H. Multiple palmar epidermoid cysts. Dermatology. 2002;205:398–400. doi: 10.1159/000066419. [DOI] [PubMed] [Google Scholar]


