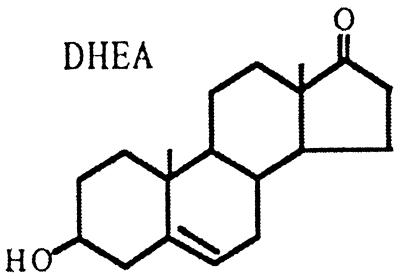
Dehydroepiandrosterone (DHEA) was isolated in urine in 1934, and DHEA 3β-sulfate (DHEAS) was identified 10 years later (1, 2). It took another decade to identify DHEA and DHEAS in peripheral blood (3, 4). More recently, fatty acid esters of DHEA, testosterone, and estradiol (5) were isolated from a variety of tissues, particularly fat (6), and their presence in circulation (5). In 1981, Corpéchot et al. (7) reported the presence of DHEA/DHEAS in the mammalian brain, but isolation of the key enzyme P450c17 required for the biosynthesis of DHEA was unsuccessful. Recently, P450c17 expression and biosynthesis of DHEA were found to interact by way of a tripartite contribution of astrocytes, oligodendrocytes, and neurons (8, 9). These neurosteroids act as an antagonist of the γ-aminobutyric acid type A receptor and as a modulator of the N-methyl-D-aspartate receptor (10) and may have sleep-inducing (rapid eye movement sleep) (11), memory-enhancing, and anxiolytic properties (see review in ref. 10).
During the past five decades, a myriad of animal experiments has suggested that DHEA is a multifunctional hormone with immunoenhancing, antidiabetic, antiobesity, anticancer, neurotropic, memory-enhancing, and antiaging effects.
The adrenals of humans and a few higher primates synthesize and secrete large amounts of DHEA and DHEAS (via sulfatransferase) that are biotransformed into biologically active androgens and estrogens in peripheral tissues. It is estimated that more than 30% of total androgen in men and over 90% of estrogen in postmenopausal women are derived from peripheral conversion of DHEA/DHEAS (12). Thus, intracellular biotransformation of DHEA to active sex steroids may bind locally to their specific intracellular nuclear receptors with minimal loss of concentration or time, an economical system to exert maximal functional activities (12).
During the past five decades, a myriad of animal experiments has suggested that DHEA is a multifunctional hormone with beneficial effects, including antiaging properties. Because a backdrop of these studies was conducted in rodents with little or no detectable circulating DHEA, it may be viewed as a pharmacological model with a naïve environment that is devoid of endogenous DHEA.
The secretion of DHEA by the human adrenal gland exhibits a pulsatile pattern with increasing frequency and amplitude at night. This pattern of DHEA synthesis and secretion by the zona reticularis is, in large measure, mediated by corticotropin (ACTH) but without the feedback regulatory function. With aging, the progressive blunting of ACTH mediates pulsatile activities, particularly the nocturnal amplification of DHEA (13), without affecting the pulsatile rhythm of cortisol (14). Although the decline of DHEAS levels persists into advanced age with a sexually dimorphic pattern, in contrast, cortisol levels in men and women show a parallel linear increase with aging (15). The age-related decline in DHEAS shows marked individual differences with a wide range of values and is under partial hereditary control. It has been suggested that DHEAS may be a measurable component of the individuality of the aging process itself (16, 17) (Scheme S1).
Scheme 1.
The biological function of DHEA and DHEAS in human aging is evolving. Mazat et al., in a recent issue of PNAS (18), advance the possibility, emerging over the past few years, that in aging men, but not in aging women, low DHEAS levels are a reliable predictor of death in smokers, even in former smokers, under 70 years of age. The population under study is a subset cohort of the PAQUID program (a prospective cohort study of elderly subjects from the southwest of France) with an 8-year follow-up in 290 subjects (119 men and 171 women). DHEAS measurements and interviews for health parameters were conducted at 1- and 8-year follow-ups. During the 7-year interval, there was a global trend of decline in DHEAS levels: 2.3% per year among men and 3.9% among women. However, in ≈30% of participants, DHEAS levels actually increased, a phenomenon also observed in another longitudinal study by Orentreich et al. (19). This evolution in DHEAS levels with time in one-third of individuals has no relationship to health parameters and is difficult to explain in the context of selective reduction of zona reticularis cell mass by 30% in aging individuals, accountable for the decline in DHEA/DHEAS synthesis and secretion (20). The possibility of a reduced metabolic clearance of DHEA/DHEAS because of subclinical functional impairment of kidneys and liver was not evaluated.
In human aging, the reduction of adrenal androgen secretion is accompanied by a host of neuroendocrine–metabolic dysfunctions that include decline in the growth hormone (GH)-insulin-like growth factor I (GH-IGF-I) system (21), thyroid function (22), and immune competence (23), fragmentation of sleep (11), and neuronal loss. The data presented by Mazat et al. (18) reaffirm the variability of DHEAS levels and gender differences. The absence of effects of low DHEAS levels on mortality in women is contrasted to a high relative risk (RR) of death in aging men with low DHEAS levels (RR = 1.9, P < 0.007) but even higher RR of death in men under 70 years of age (RR = 6.5, P = 0.003). Against this background, the RR of death is much higher in smokers with low DHEAS levels than in nonsmokers with high DHEAS levels (RR = 6.7, P = 0.001). Thus, Mazat et al. concluded that low DHEAS levels are a reliable predictor of death in male smokers. However, several studies cited have shown smokers are associated with high instead of the low DHEAS levels observed in the present study—an intriguing puzzle! Nonetheless, the cohort sample (290) of aging subjects is relatively small to address issues of mortality.
The selection by death or survival bias is best illustrated in studies conducted in centenarians. Ravaglia et al. (24) reported that, among the oldest men, those with the highest functional status had the highest DHEAS levels, and individuals with poor functioning levels had the lowest DHEAS levels. Thus, DHEAS has a strong interrelation with functional activities observed in 75 healthy people 90–106 years old. Another study in healthy centenarians (25) has found plasma IGF-I/IGF-binding protein 3 (IGFBP3) molar ratios are greater than in aged subjects, suggesting increased bioavailable IGF-I might improve insulin action and plasma lipid profiles in centenarians. Studies in aged populations (55–80 years) showed free IGF-I levels do not decline with age and are even higher in individuals above 70 years old. It was proposed that high free IGF-I levels in older persons may be the consequence of selective survival in the cohort (26). Moreover, high fasting free IGF-I levels are associated with a decreased risk of cardiovascular disease (27), whereas low free IGF-I and high IGFBP-1 are associated with a decreased quality of health but not physical disability in the elderly (28).
DHEAS has also been shown to induce peroxisome gene expression mediated through the activation of peroxisome proliferator-activated receptor (PPAR)α, as reported by Peters et al. (29). DHEA and α-Adiol are both inactive in this regard, suggesting the importance of 3β-sulfate may be required for structural confirmation for PPARα (29, 30). Thus, DHEAS may serve as an important endogenous regulator of hepatic PPARα-mediated pathways thereby maintain lipid homeostasis and prevent decline in cellular PPARα expression in normal aging. The administration of DHEAS to aging animals elicits a number of biologic changes that are mediated through a process involving PPARα activation with reversal of the dysregulated cytokines, particularly IL-6 (29). In humans, James et al. (31) and Straub et al. (23) have provided evidence that serum levels of IL-6 increase with age and that serum DHEAS levels are negatively correlated with serum IL-6 concentrations in both aging men and women. The maximal effective dose of DHEA is in the range for immunomodulation (23). Thus, the increase in IL-6 production during the process of aging might be related to diminished DHEAS secretion, which, in turn, may be a significant cofactor for the manifestation of inflammatory and age-related diseases, including bone loss (30).
Replacement of DHEA in aging populations by using different doses, durations, routes, time of day of administration, and endpoints has generated results that are favorable in most studies (11, 32–35) but not in others (36, 37). The report by Yen et al. (38) specified that DHEA be taken before bedtime to simulate the circadian rise of DHEA secretion at night. Another issue is relatively normal values for endogenous DHEA levels in some aging individuals: beneficial effects by exogenous DHEA may not be clinically evident. In this regard, Arlt et al. have demonstrated that DHEA administration (50 mg/day) induced an impressive improvement in well-being, depression score, and sexual interest in women with adrenal insufficiency and very low endogenous DHEA levels (39). Beneficial effects of DHEA have been found in immune function in controlled studies in postmenopausal women (40) and in systemic lupus erythematosus (41). Night-time DHEA administration targeted to individuals with low DHEAS levels would likely afford maximal benefits, e.g., improved quality of sleep and increase in muscle strength (32, 35). As proposed by Mazat et al. (18), the cessation of smoking and the supplementation of low DHEA levels may be a most sound approach to reducing mortality in male smokers. Interestingly, an increase in IGF-I levels in response to oral DHEA treatment (50 and 100 mg/day) was observed in several of our studies (not accompanied by changes in GH secretion). Although the mechanism(s) for the increase in IGF-I is unclear (38), the beneficial effects of IGF-I in aging subjects are evident according to several studies cited above.
Footnotes
See companion article on page 8145 in issue 14 of volume 98.
References
- 1.Butemandt A, Dannenbaum H. Z Physiol Chem. 1934;229:192–195. [Google Scholar]
- 2.Munson P L, Gallagher T F, Koch F C. J Biol Chem. 1944;152:67–77. [Google Scholar]
- 3.Baulieu E E. J Clin Endocrinol Metab. 1960;20:900–904. doi: 10.1210/jcem-20-6-900. [DOI] [PubMed] [Google Scholar]
- 4.Migeon C J, Plager J E. J Biol Chem. 1954;209:767–772. [PubMed] [Google Scholar]
- 5.Bélanger A, Candas B, Dupont A, Cusan L, Diamond P, Gomez J L, Labrie F. J Clin Endocrinol Metab. 1994;79:1086–1090. doi: 10.1210/jcem.79.4.7962278. [DOI] [PubMed] [Google Scholar]
- 6.Albert D H, Ponticorvo L, Lieberman S. J Biol Chem. 1980;255:10618–10623. [PubMed] [Google Scholar]
- 7.Corpéchot C, Robel P, Axelson M, Sjövall J, Baulieu E E. Proc Natl Acad Sci USA. 1981;78:4704–4707. doi: 10.1073/pnas.78.8.4704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zwain I H, Yen S S C. Endocrinology. 1999;140:880–887. doi: 10.1210/endo.140.2.6528. [DOI] [PubMed] [Google Scholar]
- 9.Zwain I H, Yen S S C. Endocrinology. 1999;140:3843–3852. doi: 10.1210/endo.140.8.6907. [DOI] [PubMed] [Google Scholar]
- 10.Baulieu E E. Recent Prog Horm Res. 1997;52:1–32. [PubMed] [Google Scholar]
- 11.Friess E, Trachsel L, Guldner J, Schier T, Steiger A, Holsboer F. Am J Physiol. 1995;268:E107–E113. doi: 10.1152/ajpendo.1995.268.1.E107. [DOI] [PubMed] [Google Scholar]
- 12.Labrie F, Belanger A, Simard J, Luu-The V, Labrie C. Dehydroepiandrosterone (DHEA) and Aging. Vol. 774. New York: New York Academy of Sci-ences; 1995. pp. 16–28. [DOI] [PubMed] [Google Scholar]
- 13.Liu C H, Laughlin G A, Fischer U G, Yen S S C. J Clin Endocrinol Metab. 1990;71:900–906. doi: 10.1210/jcem-71-4-900. [DOI] [PubMed] [Google Scholar]
- 14.Van Cauter E, Leproult R, Kupfer D J. J Clin Endocrinol Metab. 1996;81:2468–2473. doi: 10.1210/jcem.81.7.8675562. [DOI] [PubMed] [Google Scholar]
- 15.Laughlin G A, Barrett-Connor E. J Clin Endocrinol Metab. 2000;85:3561–3568. doi: 10.1210/jcem.85.10.6861. [DOI] [PubMed] [Google Scholar]
- 16.Rotter J I, Wong F L, Lifrak E T, Parker L N. Metabolism. 1985;34:731–736. doi: 10.1016/0026-0495(85)90023-x. [DOI] [PubMed] [Google Scholar]
- 17.Thomas G, Frenoy N, Legrain S, Sebag-Lanoe R, Baulieu E E, Debuire B. J Clin Endocrinol Metab. 1994;79:1273–1276. doi: 10.1210/jcem.79.5.7962319. [DOI] [PubMed] [Google Scholar]
- 18.Mazat L, Lafont S, Berr C, Debuire B, Tessier J-F, Dartigues J-F, Baulieu E-E. Proc Natl Acad Sci USA. 2001;98:8145–8150. doi: 10.1073/pnas.121177998. . (First Published June 26, 2001; 10.1073/pnas.121177998) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Orentreich N, Brind J L, Vogelman J H, Andres R, Baldwin H. J Clin Endocrinol Metab. 1992;75:1002–1004. doi: 10.1210/jcem.75.4.1400863. [DOI] [PubMed] [Google Scholar]
- 20.Parker C R, Jr, Mixon R L, Brissie R M, Grizzle W E. J Clin Endocrinol Metab. 1997;82:3898–3901. doi: 10.1210/jcem.82.11.4507. [DOI] [PubMed] [Google Scholar]
- 21.Corpas E, Harman S M, Blackman M R. Endocr Rev. 1993;14:20–39. doi: 10.1210/edrv-14-1-20. [DOI] [PubMed] [Google Scholar]
- 22.Mariotti S, Barbesino G, Caturegli P, Bartalena L, Sansoni P, Fagnoni F, Monti D, Fagiolo U, Franceschi C, Pinchera A. J Clin Endocrinol Metab. 1993;77:1130–1134. doi: 10.1210/jcem.77.5.8077303. [DOI] [PubMed] [Google Scholar]
- 23.Straub R H, Konecna L, Hrach S, Rothe G, Kreutz M, Schölmerich J, Falk W, Lang B. J Clin Endocrinol Metab. 1998;83:2012–2017. doi: 10.1210/jcem.83.6.4876. [DOI] [PubMed] [Google Scholar]
- 24.Ravaglia G, Forti P, Maioli F, Boschi F, Bernardi M, Pratelli L, Pizzoferrato A, Gasbarrini G. J Clin Endocrinol Metab. 1996;81:1173–1178. doi: 10.1210/jcem.81.3.8772596. [DOI] [PubMed] [Google Scholar]
- 25.Paolisso G, Ammendola S, Del Buono A, Gambardella A, Riondino M, Tagliamonte M R, Rizzo M R, Carella C, Varricchio M. J Clin Endocrinol Metab. 1997;82:2204–2209. doi: 10.1210/jcem.82.7.4087. [DOI] [PubMed] [Google Scholar]
- 26.Janssen J A, Stolk R P, Pols H A, Grobbee D E, de Jong F H, Lamberts S W. Clin Endocrinol (Oxford) 1998;48:471–478. doi: 10.1046/j.1365-2265.1998.00300.x. [DOI] [PubMed] [Google Scholar]
- 27.Janssen J A, Stolk R P, Pols H A, Grobbee D E, Lamberts S W. Arterioscler Thromb Vasc Biol. 1998;18:277–282. doi: 10.1161/01.atv.18.2.277. [DOI] [PubMed] [Google Scholar]
- 28.Janssen J A, Stolk R P, Pols H A, Grobbee D E, Lamberts S W. Gerontology. 1998;44:277–280. doi: 10.1159/000022026. [DOI] [PubMed] [Google Scholar]
- 29.Peters J M, Zhou Y C, Ram P A, Lee S S, Gonzalez F J, Waxman D J. Mol Pharmacol. 1996;50:67–74. [PubMed] [Google Scholar]
- 30.Poynter M E, Daynes R A. J Biol Chem. 1998;273:32833–32841. doi: 10.1074/jbc.273.49.32833. [DOI] [PubMed] [Google Scholar]
- 31.James K, Premchand N, Skibinska A, Skibinski G, Nicol M, Mason J I. Mech Ageing Dev. 1997;93:15–24. doi: 10.1016/s0047-6374(96)01807-6. [DOI] [PubMed] [Google Scholar]
- 32.Morales A J, Nolan J J, Nelson J C, Yen S S C. J Clin Endocrinol Metab. 1994;78:1360–1367. doi: 10.1210/jcem.78.6.7515387. [DOI] [PubMed] [Google Scholar]
- 33.Diamond P, Cusan L, Gomez J L, Bélanger A, Labrie F. J Endocrinol. 1996;150:S43–S50. [PubMed] [Google Scholar]
- 34.Labrie F, Diamond P, Cusan L, Gomez J L, Bélanger A, Candas B. J Clin Endocrinol Metab. 1997;82:3498–3505. doi: 10.1210/jcem.82.10.4306. [DOI] [PubMed] [Google Scholar]
- 35.Morales A J, Haubrich R H, Hwang J Y, Asakura H, Yen S S C. Clin Endocrinol (Oxford) 1998;49:421–432. doi: 10.1046/j.1365-2265.1998.00507.x. [DOI] [PubMed] [Google Scholar]
- 36.Kudielka B M, Hellhammer J, Hellhammer D H, Wolf O T, Pirke K M, Varadi E, Pilz J, Kirschbaum C. J Clin Endocrinol Metab. 1998;83:1756–1761. doi: 10.1210/jcem.83.5.4758. [DOI] [PubMed] [Google Scholar]
- 37.Wolf O T, Köster B, Kirschbaum C, Pietrowsky R, Kern W, Hellhammer D H, Born J, Fehm H L. Biol Psychiatry. 1997;42:845–848. doi: 10.1016/s0006-3223(97)00323-5. [DOI] [PubMed] [Google Scholar]
- 38.Yen S S C, Morales A J, Khorram O. Ann NY Acad Sci. 1995;774:128–142. doi: 10.1111/j.1749-6632.1995.tb17377.x. [DOI] [PubMed] [Google Scholar]
- 39.Arlt W, Callies F, van Vlijmen J C, Koehler I, Reincke M, Bidlingmaier M, Huebler D, Oettel M, Ernst M, Schulte H M, Allolio B. N Engl J Med. 1999;341:1013–1020. doi: 10.1056/NEJM199909303411401. [DOI] [PubMed] [Google Scholar]
- 40.Casson P, Andersen R, Herrod H, Stentz F, Straughn A, Abraham G, Buster J. Am J Obstet Gynecol. 1993;169:1536–1539. doi: 10.1016/0002-9378(93)90431-h. [DOI] [PubMed] [Google Scholar]
- 41.van Vollenhoven R F, Park J L, Genovese M C, West J P, McGuire J L. Lupus. 1999;8:181–187. doi: 10.1191/096120399678847588. [DOI] [PubMed] [Google Scholar]