Abstract
Objective
Although a variety of intervention methods have been used to promote Pap test screening among ethnic minority women in the US, the effectiveness of such interventions is unclear. We performed a meta-analysis to examine the overall effectiveness of these interventions in increasing Pap test use by ethnic minority women in the US.
Methods
A search of databases (MEDLINE, Cumulative Index to Nursing and Allied Health Literature, PsycINFO, and Science Citation Index-Expanded) and review articles for articles published between 1984 and April 2009 identified 18 randomized and nonrandomized controlled trials. The primary study outcome was the difference in the proportion of Pap tests between the treatment and comparison groups.
Results
The pooled mean weighted effect size (d) for the 18 studies was 0.158 (95% confidence interval [CI]=0.100, 0.215), indicating that the interventions were effective in improving Pap test use among ethnic minority women. Among the intervention types, access enhancement yielded the largest effect size (0.253 [95% CI=0.110, 0.397]), followed by community education (0.167 [95% CI=0.057, 0.278]) and individual counseling or letters (0.132 [95% CI=0.069, 0.195]). Combined intervention effects were significant for studies targeting Asian (0.177 [95% CI=0.098, 0.256]) and African American women (0.146 [95% CI=0.028, 0.265]), but not Hispanic women (0.116 [95% CI=−0.008, 0.240]).
Conclusions
Pap test use among ethnic minority women is most likely to increase when access-enhancing strategies are combined. Further research is needed to determine whether more tightly controlled trials of such interventions might reveal an improved rate of cervical cancer screening in Hispanic women as well.
Keywords: Pap test, ethnic minority, women, meta-analysis
INTRODUCTION
Ethnic minority women in the U.S. experience cervical cancer-related health disparities, defined by the Trans-Department of Health and Human Services Cancer Health Disparities Progress Review Group as “differences in the incidence, prevalence, mortality, and burden of cancer and related adverse health conditions that exist among specific population groups in the U.S. [1].” Data from the Surveillance, Epidemiology and End Results Program of the National Cancer Institute have revealed that the highest age-adjusted incidence rate of cervical cancer occurs among Vietnamese American women (43 per 100,000), followed by Korean American women (15 per 100,000); by comparison, the incidence rate is 8.1 per 100,000 in the general U.S. population [2]. Furthermore, ethnic minority women in the U.S. generally experience more severe cases of cervical cancer as a result of delayed diagnosis [3–5].
Regular screening is accepted as a critical strategy for the early detection and timely treatment of cervical cancer [6,7] The U.S. Preventive Services Task Force [6] recommends Pap tests for women within 3 years of onset of sexual activity or beginning at age 21 (whichever comes first), and screening at least every 3 years until age 64 (for age 65 and older, screening is advised only among symptomatic women and for those who have had recent abnormal results). Although the prevalence of recent Pap test use (i.e., within the past 3 years) has increased during the past two decades, a significant gap in compliance with these recommendations still exists in some groups. For example, data from the 2005 U.S. National Health Interview Surveys [8] indicated that Asian Americans were least likely to have had a recent Pap test and White women were most likely (65.8% vs. 81.4%). In the survey [8], the prevalence of recent Pap test use was particularly low among women with no health insurance (61.4%) and recent immigrants (66.8%).
Although many studies have focused on promoting cervical cancer screening among ethnic minority women, there has been no clear consensus about how best to increase cervical cancer screening among those groups of women who are disproportionately affected by cervical cancer. The National Breast and Cervical Cancer Early Detection Program (NBCCEDP), administered by the Centers for Disease Control and Prevention (CDC), has been one of key cervical cancer screening programs for women at high risk—especially poor, low-income, racial and ethnic minority women—providing no-cost breast and cervical cancer screening to eligible women. Previous meta-analyses have been conducted with regard to interventions designed to improve cervical cancer screening [9–14]: One analysis considered interventions directed at physicians only [10]; two dealt with reminders for physicians and/or patients [11, 13]; two included interventions in various forms but without any information about the target populations [9, 14]; and one included office-based interventions only and did not specify the intervention methods used [12]. Hence, no previous analyses have been specifically targeted at ethnic minority women, nor have these analyses identified culturally tailored or other intervention approaches that are most effective for groups of women who are traditionally associated with a lower use of Pap tests.
Identification of effective intervention strategies could help to reduce barriers to early detection of cervical cancer among ethnic minority women. Our goal was to fill the gap in the current literature by conducting an analysis of research studies that specifically focused on ethnic minority women in the U.S. In particular, the objectives of our meta-analysis were: (1) to describe intervention approaches used for ethnic minority (i.e., Asian American, Black, and Hispanic) women to improve their cervical cancer screening behavior, and (2) to determine the effectiveness of particular types of interventions in these groups of women.
METHODS
Identification and Selection of Studies
We identified potential studies to be included in this review by electronic searches of databases and hand searches from reference collections. Four databases (MEDLINE, the Cumulative Index to Nursing & Allied Health Literature [CINAHL], PsycINFO, and Science Citation Index-Expanded) were searched using combinations of the key words “Asian,” “African or Black,” “Hispanic or Latino,” “cervical cancer screening,” “Pap smear or Pap test,” “experimental studies,” “interventions,” or “intervention studies.” The literature search was limited to articles published between 1984 and April 2009 in the English language; international studies were not included because our focus was on interventions to improve cervical cancer screening among ethnic minority women in the U.S.
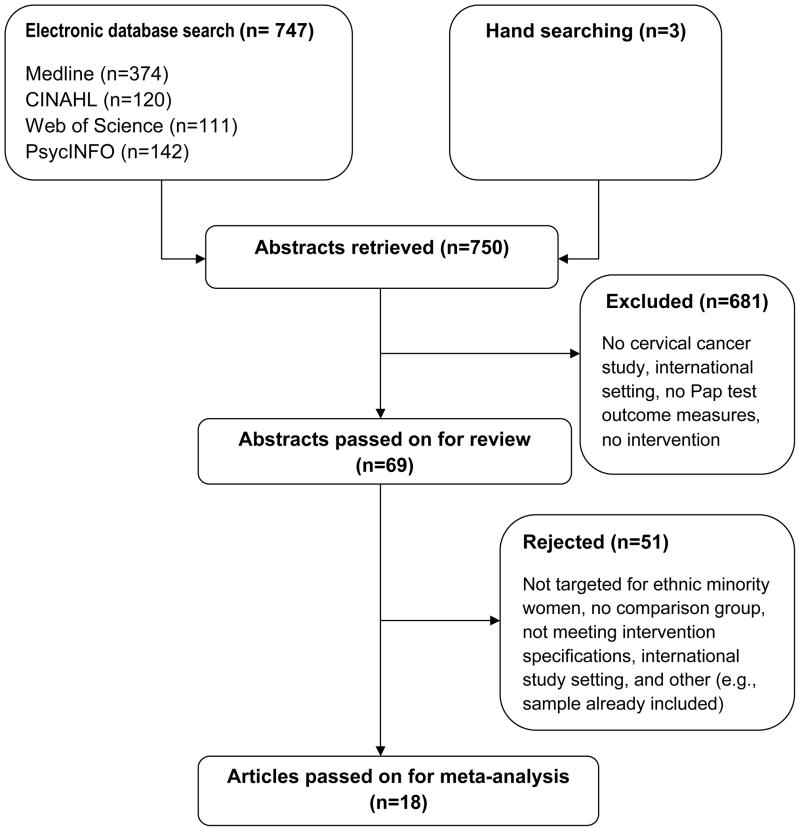
Figure 1 summarizes our study selection process. Our electronic searches yielded a combined total of 747 titles and abstracts for initial screening; our hand searches of references yielded three additional studies. Reference sections of prior systematic reviews [9, 11–14] were also screened. Interventions exclusively aimed at health professionals were not included, since they have been considered in previous reviews [9–12]. Assessment of relevant studies for inclusion was conducted by two independent raters.
Figure 1.
Flow chart of the literature search and selection process
Of these 750 studies identified, 681 were excluded in our initial screening. The remaining 69 full-text articles were reviewed for eligibility on the basis of the following criteria: (1) the study aimed to increase the use of Pap tests among asymptomatic women, either exclusively or in addition to other health behaviors; (2) Asian American, Black, or Hispanic women, together or alone, represented >40% of the total sample; (3) the study outcomes were based on a woman’s adherence to Pap tests; and (4) the study used an experimental or quasi-experimental design. Of the 69 studies, 51 were excluded: In 7 studies, ethnic minority women did not represent >40% of the entire population, or the ethnicity of the study population was unclear; 17 did not clearly specify an intervention component or did not have a comparison group; 20 had an international study setting; and 7 reported on the same sample as another that was already included. As a result, a total of 18 studies were included in our meta-analysis.
Extracted Information
The outcomes were study-specific adherence rates as defined by each study. This allowed us to include a wider range of studies, since some studies recorded receipt of a Pap test, according to screening guidelines, or receipt of an initial Pap test. The following information was coded: first author; year; study design; setting; sample (% ethnic minority women) and sample size; type of intervention; intervention period, time to outcome measure (months); the method of outcome ascertainment; proportion of Pap tests for the treatment and comparison groups; theory; comparison group (no intervention, minimal intervention/usual care, or other non-cervical cancer intervention); cultural strategies used, if any; and study quality.
Adopting the typology used in a previous review of cancer screening interventions [15], we categorized interventions according to five intervention components. Each type of intervention component was defined as follows.
Individual-directed interventions
This type of intervention is given on an individual basis to provide information on benefits of screening, while motivating participants to seek screening. Examples include one-on-one counseling (in-person or by telephone), tailored and non-tailored letters or reminders (printed or verbal).
Access-enhancing interventions
Access-enhancing strategies promote cancer screening by reducing financial (e.g., reduced-cost or free Pap tests), structural (e.g., mobile vans or transportation), or linguistic barriers (e.g., making appointments, language translation) that hamper access to screening services.
Peer navigator-related interventions
Peer leaders or lay health advisors in the target community provide necessary support, follow-up, or referral to help minority women obtain screening tests.
Community education
Community education through small group workshops or seminars is usually conducted by health professionals or by trained educators in a variety of settings (e.g., health fairs, churches). Participants are informed and encouraged to receive a screening test in a group setting.
Mass media
Mass media interventions using television, newspapers, radio, or magazines are designed to increase awareness about cervical cancer and screening at the community level. It is more common that this approach is combined with other interventions (e.g., small group seminars, financial incentives, peer navigator support) than used alone.
Likewise, cultural strategies were categorized into three types and defined as follows:
Involving community members
A collaborative research process involving members of the target community allows researchers to employ local knowledge in the understanding of health problems and in the design of interventions. It is assumed that this approach offers better opportunities to improve the health and well being of these communities.
Culturally matched materials
Incorporating culture-specific values and attitudes into health promotion tools and other educational materials can enhance participant understanding and satisfaction with the intervention program. Examples include culturally relevant graphics, stories, adages, or language adaptations.
Matched intervention deliveries
Participants from different backgrounds may prefer to receive intervention from individuals of their own race, ethnicity, or language group. This cultural strategy involves the delivery of interventions using ethnically and/or linguistically matched or local people to deliver the interventions.
We used meta-analysis techniques to calculate the effect size of each intervention type across multiple studies. For three studies that compared two or more treatment groups to one comparison group [16–18], the intervention with the most components (i.e., highest dose) was considered. We used the “Research and Quality Scoring Method” by Sackett and Haynes [19], the Jadad scale [20], and the items published by Cho and Bero [21] to rate the quality of each study (Table 1). The range of total quality scores was 0 to 9. Studies with scores 0–5 were considered to be low quality and those with scores 6–9 were considered to be high quality. Two raters independently coded variables using Microsoft Excel. Discrepancies were identified and resolved by discussion among team members. To assess the coding agreement between the two raters, Cohen’s κ was calculated using SPSS version 15. The average kappa was 0.812, reflecting substantial agreement between the raters.
Table 1.
Study quality ratings
| Item | Score |
|---|---|
| Study design | 0 = Non-randomized, quasi-experimental design |
| 1 = Randomized experiment | |
| Outcome measure | 0 = Pap test is self-reported |
| 1 = Pap test is confirmed by claims data or chart review | |
| Clarity of outcome | 0 = No definition of study outcome (Pap test adherence) |
| 1 = Clearly defined Pap test adherence | |
| Information on withdrawal or dropout rate | 0 = Not discussed |
| 1 = The number and the reasons for withdrawals in each group are stated | |
| Research question | 0 = Not clear |
| 1 = Clearly stated | |
| Participants in sample | 0 = Unclear |
| 1 = Clearly described | |
| Participant inclusion/exclusion criteria | 0 = Unclear |
| 1 = Specified | |
| Type of facility where the study was conducted | 0 = Unclear |
| 1 = Clearly stated | |
| Sample size justification | 0 = Unclear/not provided |
| 1 = Sufficiently described and justified before the study |
Meta-Analysis
We used STATA (StataCorp LP, College Station, TX) to conduct the data analyses. Since our primary focus was on differences in post-intervention screening rates between the intervention and comparison groups, we chose to use a raw-score metric to define the effect size. This approach has been recommended because of its ease of interpretation and utility for public policy and clinical purposes [15, 22]. Specifically, we calculated an effect size (d) for each study using the difference in the post-intervention adherence rates between the intervention and comparison groups (pi and pc, respectively). In studies reporting odds ratios instead of proportions [16, 23], post-intervention Pap test rates were calculated based on either the reported proportion in the comparison group or in the intervention group. Using the meta command in Stata, which weights d by the inverse of the estimated study variance in fixed effect models, an overall mean weighted effect size was computed for the 18 studies included in the analysis. In addition, 95% confidence intervals (CIs) were estimated for each effect size. For the effect size of d = pi − pc, the study variance was defined as pi (1 − pi)/ni + pc (1 − pc)/nc where ni and nc are the number of subjects in the intervention and comparison groups, respectively [24]. We performed a test for heterogeneity of the intervention effects based on the DerSimonian and Laird [24] Q-statistic. When the results were significant, a random effects model was used to accommodate this heterogeneity by pooling the effect sizes across studies [24]. This process was repeated to calculate d for the various subgroup analyses.
Sensitivity analyses were conducted to determine whether the results were affected by potentially influential studies (i.e., those with a large sample size or extreme effect size) or study quality. Using a leave-one-out approach, we re-estimated the overall d after removing the potentially influential studies one at a time. We also compared the overall d for studies of high and low quality. Additional analyses were done to assess and adjust for any publication bias. Publication bias refers to a bias that can result from the selective publication of positive findings [25]; if the published literature is more likely to include trials showing positive effects of interventions and if equally valid trials showing no or negative effects are unpublished, systematic reviews of the literature would be biased. A funnel plot [25] was constructed, with a symmetric, inverted funnel being taken to represent an absence of publication bias. We also calculated Rosenthal’s fail-safe N, which is an estimate of the number of studies having no effect that would be needed to reduce the overall effect size in the meta-analysis from significant to nonsignificant [26]. A fail-safe N that was greater than a cutoff value would suggest that there was no evidence of publication bias.
RESULTS
Description of the studies included in the meta-analysis
The 18 studies reporting quantifiable outcomes included in the effect size calculations [16–18, 23, 27–40] are presented in Table 2. The final sample included a total of 13,407 women, with the smaller studies [27, 31, 32] involving about 100 to 200 women and the largest study [38] including > 2,000 women in its sample. In four studies [16, 29, 35, 39], the sample was predominantly African American; in three studies [30, 32, 40], it was Hispanic; in eight studies, Asian (Vietnamese [28, 33, 34, 36, 38], Korean [31, 37], or Chinese[18]); in one study, native American [23]; and in two studies [17, 27], a combination of African American and Hispanic women. Half of the studies [16–18, 23, 27, 29, 30, 36, 40] used a randomized experimental study design, and 13 studies [18, 23, 28, 29, 31–34, 36–40] were conducted in a community setting.
Table 2.
Characteristics of included studies targeting increases in Pap tests among ethnic minority women
| 1st author, yr* | Study designa |
Setting | Sample size |
Sampleb (%minority) |
Intervention | Comparison groupc |
Outcome measured |
Outcome monthe |
Theoryf | Tailored | Cultural strategyg |
Quality rating |
Post-intervention screening rates |
Effect size |
95% CI | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | |||||||||||||||
| Batal, 200027 | R | Health care | 197 | AF (21%), H (52.3%) | Pap test offered in an urgent care clinic | Usual | O | 6 | None | No | None | 8 | 84.7% | 29% | 56% | (0.44, 0.67) |
| Bird, 199828 | NR | Community | 717 | A (100%) | Lay health workers, small group education | No | O | Not available | None | No | Matched material, matched delivery | 8 | 66% | 42% | 24% | (0.17, 0.31) |
| Burack, 199816 | R | Health care | 1,924 | AF (95%) | Reminder letters | No | O | Not available | None | No | None | 9 | 32% | 27.7%† | 4% | (0.00, 0.08) |
| Campbell, 200229 | R | Community | 538 | AF (59.2%) | Computer-tailored magazine, natural helpers | Other | S | 18 | SCT, SSM | Yes | Member | 7 | 75% | 73% | 2% | (−0.05, 0.09) |
| Dietrich, 200630 | R | Health care | 1,390 | H (62.8%, used Spanish as primary language) | Telephone counseling | Usual | O | 18 | None | No | Matched material | 8 | 78% | 70% | 8% | (0.03, 0.13) |
| Dignan, 199623 | R | Community | 540 | NA (100%) | Individual health education | No | S | 6 | HBM, PPM, SET, MHCM, CBCF, SL | No | Matched material, matched delivery | 8 | 79.3%† | 65.1% | 14% | (0.07, 0.22) |
| Fang, 200731 | NR | Community | 102 | A (100%) | Small group education, navigation service | Minimal | S | 6 | HBM, SCT | No | Matched material, matched delivery | 6 | 82.7% | 22% | 61% | (0.45, 0.76) |
| Fernandez-Esquer, 200332 | NR | Community | 195 | H (100%) | Peer volunteer campaign, mass media | No | S | Not available | DIT | No | Matched material, matched delivery | 6 | 36% | 44% | −8% | (−0.22, 0.06) |
| Jenkins, 199933 | NR | Community | 876 | A (100%) | Media education | No | S | 24 | TTM | No | Matched material | 6 | 47.7% | 37% | 11% | (0.04, 0.17) |
| Jibaja-Weiss, 200317 | R | Health care | 959 | AF (41.9%), H (40.3%) | Personalized tailored letters | No | O | 12 | HBM | Yes | Matched material | 7 | 43.9% | 39.9% | 4% | (−0.02, 0.10) |
| Lam, 200334 | NR | Community | 373 | A (100%) | Media education, lay health workers | Minimal | S | Not available | PPM | No | Matched material, matched delivery | 3 | 76.9% | 72.8% | 4% | (−0.05, 0.13) |
| Mandelblatt, 199335 | NR | Health care | 319 | AF (89.3%) | Screening offered at primary care clinics | Usual | O | Not available | None | No | None | 8 | 56.9% | 18.2% | 39% | (0.29, 0.48) |
| Mock, 200736 | R | Community | 911 | A (100%) | Lay health workers, media education | Minimal | S | 3.5 | None | No | Matched material, matched delivery | 5 | 67.3% | 55.7% | 12% | (0.05, 0.18) |
| Moskowitz, 200737 | NR | Community | 876 | A (100%) | Small group education, financial incentives, media campaign | No | S | Not available | PPM | No | Matched material, matched delivery | 6 | 66.9% | 65.1% | 2% | (−0.04, 0.08) |
| Nguyen, 200638 | NR | Community | 2,009 | A (100%) | Media campaign, lay health workers, small group education, navigation, reminder letter | No | S | Not available | PM | No | Matched material, matched delivery | 3 | 70.4% | 53.1% | 17% | (0.13, 0.21) |
| Paskett, 199939 | NR | Community | 302 | AF (78.5%) | Lay health educators, one-on-one education, targeted mailing, mass media, monthly classes in housing community | No | S | 36 | HBM, PPM, SL | No | Matched material, matched delivery | 5 | 87% | 60% | 27% | (0.17, 0.37) |
| Taylor, 200218 | R | Community | 263 | A (100%) | Outreach workers, transportation assistance, telephone counseling | Usual | O | 6 | None | No | Matched material, matched delivery | 7 | 39% | 15% | 24% | (0.14, 0.34) |
| Thompson, 200640 | R | Community | 916 | H (100%) | Community education, free screening, lay health workers, individual discussion | No | S | 30 | CO | No | Member, matched material, matched delivery | 8 | 94.2% | 93.7% | < 1% | (−0.03, 0.04) |
Superscript refers to numbers in the reference list.
Estimated from odds ratio using baseline Pap test rates and sample size information.
Study design: NR – non-randomized quasi-experimental design, R – randomized experiment
Sample: A – Asian, AF – African American, NA – Native American, H – Hispanic
Comparison group: No – no intervention, Usual – usual care, Minimal – minimal intervention, Other – some other non-cervical intervention
Outcome measure: O – objective measure (e.g., medical record reviews, claims data), S – self-report
Outcome months: Time to outcome measure
Theory: HBM – Health Belief Model, PPM – Precede-Proceed Model, SL – Social Learning theory, TTM – Transtheoretical Model of Change, SCT – Social cognitive theory, SSM – Social Support Model, SET – Self-efficacy Theory, MHCM – Minority Health Communication Model, CBCF – Communication-Behavior Change Framework, DIT – Diffusion of Innovation Theory, PM – Pathways Model, CO – Community Organization Model
Cultural strategies: Member – involving members of the target community, Matched material – including culturally matched promotional or other material, Matched delivery – using ethnically matched or local people to deliver the intervention
The most commonly applied intervention approaches were (1) individually directed print materials and counseling [16–18, 23, 29, 30, 35, 38–40], and (2) peer navigator-related interventions [18, 28, 29, 32, 34, 36–40]. For the comparison group, most studies [16–18, 23, 27, 28, 30, 32, 33, 35, 37–40] provided no intervention or usual care; three studies [31, 34, 36] offered only minimal intervention; and in one study [29], other active non-cervical intervention (e.g., education on midlife issues, parenting, flu shots) was provided. Self-report [23, 29, 31–34, 36–40] was used more often than medical records [16–18, 27, 28, 30, 35] for outcome measurement. Seven studies [16, 18, 27, 28, 30, 35, 36] did not indicate any theoretical approach. For theoretically-based studies [17, 23, 29, 31–34, 37–40], the Health Belief Model was the most frequently used theory, alone or in combination with other theories [17, 23, 31, 39]. Two studies [17, 29] included personalized tailored letters and magazine attuned to the characteristics of each woman (e.g., age, current health behaviors, place of employment) in order to provide personalized feedback and strategies for healthy behavioral changes. Fifteen [17, 18, 23, 28–34, 36–40] of the 18 studies reported some form of cultural approach, with nearly every study adopting more than one strategy. Both culturally matched intervention materials and intervention deliveries using ethnically matched or local people were commonly used. Two studies [29, 40] involved members of the target community as a way of increasing the cultural sensitivity of their interventions.
Effects of interventions on the use of Pap tests at follow-up
The overall d for the 18 studies [16–18, 23, 27–40] was 0.158 (95% CI=0.100, 0.215), indicating that the interventions were effective in increasing Pap test use among ethnic minority women (Table 3). Access-enhancing interventions [18, 27, 31, 37, 38, 40] increased compliance with cervical cancer screening to a greater extent than did other types of interventions, and yielded the largest effect size (d=0.253, 95% CI=0.110, 0.397). Interventions using community education [28, 31, 32, 37–40] had the next largest effect size (d=0.167, 95% CI=0.057, 0.278), followed by individually directed interventions [16–18, 23, 29, 30, 35, 38–40] (d=0.132, 95% CI=0.069, 0.195) and mass media approaches [33, 34, 36–39] (d=0.119, 95% CI=0.055, 0.183) or peer navigators [18, 28, 29, 32, 34, 36–40] (d=0.106, 95% CI=0.039, 0.173).
Table 3.
Estimated effect sizes with 95% CIs
| Element | Category | No. studies | Effect size (95% CI) |
|---|---|---|---|
| Overall | 18 | 0.158 (0.100, 0.215) | |
| Intervention type*† | Individual-directed16–18, 23, 29, 30, 35, 38–40 | 10 | 0.132 (0.069, 0.195) |
| Access-enhancing18, 27, 31, 37, 38, 40 | 6 | 0.253 (0.110, 0.397) | |
| Peer navigator-related18, 28, 29, 32, 34, 36–40 | 10 | 0.106 (0.039, 0.173) | |
| Community education-related28, 31, 32, 37–40 | 7 | 0.167 (0.057, 0.278) | |
| Mass media-related33, 34, 36–39 | 6 | 0.119 (0.055, 0.183) | |
| Setting | Health care16, 17, 27, 30, 35 | 5 | 0.212 (0.071, 0.353) |
| Community18, 23, 28, 29, 31–34, 36–40 | 13 | 0.138 (0.074, 0.202) | |
| Cultural strategies* | Culturally matched materials17, 18, 23, 28, 30–34, 36–40 | 14 | 0.134 (0.077, 0.190) |
| Matched intervention deliveries18, 23, 28, 31, 32, 34, 36–40 | 11 | 0.153 (0.078, 0.229) | |
| Used multiple cultural strategies18, 23, 28, 31, 32, 34, 36–40 | 11 | 0.153 (0.078, 0.229) | |
| Used single cultural strategy17, 29, 30, 33 | 4 | 0.066 (0.031, 0.101) | |
| Ethnic groups‡ | African16, 17, 29, 35, 39 | 5 | 0.146 (0.028, 0.265) |
| Asian18, 28, 31, 33, 34, 36–38 | 8 | 0.177 (0.098, 0.256) | |
| Hispanic17, 27, 30, 32, 40 | 5 | 0.116 (−0.008, 0.240) | |
| Quality | High (6–9)16–18, 23, 27–33, 35, 37, 40 | 14 | 0.162 (0.091, 0.232) |
| Low (0–5)34, 36, 38, 39 | 4 | 0.148 (0.075, 0.222) |
Studies may be classified as using more than one type of intervention or cultural strategies
Type of intervention:
Individual-directed – counseling (in-person, telephone), letters, reminders;
Access-enhancing – facilitated scheduling, mobile vans, vouchers, reduced-cost or free
Pap tests, language translation;
Peer navigator-related – peer leaders or lay health advisors;
Community education-related – community workshops, seminars;
Mass media-related – awareness campaign
Included studies in which the specified ethnic group accounted for >40% of the total sample
Table 3 also shows the ways in which the interventions were delivered. Interventions delivered in health care settings [16, 17, 27, 30, 35] were more effective than those in community settings [18, 23, 28, 29, 31–34, 36–40] (d=0.212 [95% CI=0.071, 0.353] vs. 0.138 [95% CI=0.074, 0.202], respectively). We also examined whether different cultural strategies influenced the effect size found. Interventions using culturally matched materials [17, 18, 23, 28, 30–34, 36–40] (d=0.134, 95% CI=0.077, 0.190) and ethnically matched intervention deliveries [18, 23, 28, 31, 32, 34, 36–40] (d=0.153, 95% CI=0.078, 0.229) were both effective in significantly improving Pap test screening. We did not calculate the effect size for two studies [29, 40] involving members of the target community as a cultural strategy because the numbers were too small to permit subgroup analysis. Using two or more cultural strategies [18, 23, 28, 31, 32, 34, 36–40] resulted in a larger effect size (d=0.153, 95% CI=0.078, 0.229) than did using a single cultural strategy (d=0.066, 95% CI=0.031, 0.101) [17, 29, 30, 33]. Combined intervention effects were examined for each ethnic group (for those studies in which the specified ethnic group represented >40% of the sample). The effect size point estimates were significant for African American [16, 17, 29, 35, 39] (d=0.146, 95% CI=0.028, 0.265) and Asian women [18, 28, 31, 33, 34, 36–38] (d=0.177, 95% CI=0.098, 0.256). The interventions involving Hispanic women [17, 27, 30, 32, 40] yielded a positive effect size of 0.116 but the lower bound of the 95% CI was negative (95% CI=−0.008, 0.240), suggesting no effect of the interventions on Pap test use in these women. Finally, we estimated d for the high-quality vs. low-quality studies (quality rating 6–9 vs. 0–5). The effect size for the studies of high quality [16–18, 23, 27–33, 35, 37, 40] was 0.162 (95% CI=0.091, 0.232), while the effect size for the low-quality studies [34, 36, 38, 39] was 0.148 (95% CI=0.075, 0.222).
Sensitivity Analyses
We conducted sensitivity analyses to assess the effect of potentially influential studies that had much larger effect sizes than those of the other studies [27, 31, 35]. Removing Fang et al. [31] resulted in an effect size of 0.137 (95% CI=0.082, 0.191) for the remaining studies. When Batal et al. [27] was removed, the effect size for the other 17 studies was 0.135 (95% CI=0.083, 0.187). Without the study by Mandelblatt et al. [35], the effect size for the remaining studies was 0.144 (95% CI=0.088, 0.200). The overall effect size was also maintained when the largest study (n=2,009 [38]) was removed. Without this study, the overall effect size was 0.157 (95% CI = 0.096, 0.219). Likewise, when the next largest study was removed (n=1,924 [16]), the overall effect size increased slightly, from d=0.158 (95% CI=0.100, 0.215) to d=0.166 (95% CI=0.103, 0.229).
Publication Bias
We also assessed the likelihood of publication bias. The funnel plot appeared slightly asymmetrical (not shown): studies with the largest effect sizes [27, 31] had the smallest sample sizes (i.e., the largest standard errors). The fail-safe analysis, however, indicated that 1,189 nonsignificant studies would have to be added to the database before the pooled effect size of these interventions to promote Pap tests among traditionally non-adherent ethnic minority women would no longer be significant at the 0.05 significance level (cutoff=100), indicating our results were fairly robust.
DISCUSSION
The 18 studies of interventions to increase Pap test use among ethnic minority women demonstrated that improvement can be achieved (an average increase of 15.8%) through various methods. In particular, our meta-analysis indicated that the highest level of benefit could be achieved by the use of access-enhancing interventions (an increase of 25.3% in cervical cancer screening), followed by intervention approaches involving community education (a 16.7% increase), and individual counseling, letters, or reminders (a 13.2% increase).
Although our results cannot be directly compared to those of other meta-analyses because of differences in study selection criteria and intervention typology, our findings are similar to those of Stone et al. [9] who reported that financial incentives (i.e., reductions in payment, direct compensation to patients) were the strongest patient-targeted intervention approach. Access to care has been documented as the strongest socioeconomic correlate of cancer screening [41]. Given that ethnic minority women are less likely than their white counterparts to have health insurance (69.7% vs. 87%) [42], incorporating access-enhancing features would be particularly important when an intervention is designed to improve Pap test screening among ethnic minority women.
Even though interventions utilizing peer navigators were among the most frequently employed intervention approaches in our analysis, they were associated with a smaller effect size (10.6%) when compared to other intervention types. We are unaware of any previous meta-analyses that have examined peer navigator-related interventions as part of intervention typology for cervical cancer screening. Inadequate descriptions of peer navigator training and monitoring in the interventions make it difficult to explain why this approach was not as effective as others. It is notable, however, that all of the studies using peer navigators were conducted in a community setting, with the majority being nonrandomized trials. Several researchers [43, 44] have cautioned that without sufficient monitoring, the utility of peer navigator intervention is unclear because the content and frequency of interactions between the peer navigator and the participant can vary widely, at the discretion of the peer navigator. These results seem to point to the importance of rigorous peer navigator training and monitoring plans when a community-based intervention trial using peer navigators is designed.
In our analysis, studies conducted in a health care setting such as a health maintenance organization, urgent care clinic, or community health center produced a bigger effect size than did community-based studies. In a health care setting, women are likely to have the benefit of increased contact with medical providers, one of the strongest motivators for cancer screening [45]. These women might have experienced fewer barriers to cervical cancer screening because they received personalized reminders [16, 17], in-person or telephone counseling [30, 35], or an offering of instant screening at the clinic [27]. Nevertheless, the relatively small effect size difference of about 7% between the health care and community settings suggests additional cues and support that may be necessary to promote Pap test use among ethnic minority women. Conducting trials in community settings could be challenging since tightly controlled studies are not always feasible. In fact, all four studies with low quality ratings were conducted in a community setting and often involved a non-randomized study design. Researchers have reported ethical concerns about traditional randomized controlled trials because control groups do not necessarily benefit from study participation [46]. Future intervention research should incorporate more diverse study designs as alternatives to this traditional approach (e.g., attention control or waiting list designs), which may yield better outcomes while ensuring that the benefits of the research are given to all participants in the trial [47].
Incorporating cultural strategies significantly improved cervical cancer screening among ethnic minority women. In particular, multiple cultural strategies were more effective than single strategies for increasing Pap test use. Making direct comparisons with previous meta-analyses is impossible, since none of them specifically evaluated cultural strategies as part of their intervention typology. Of the 18 studies we analyzed, there were only two in which members of the target community were involved as a means of making the intervention more culturally sensitive and suited to the needs of the community. Studies have shown that acknowledging and integrating the values and preferences of the target community are important for successful interventions, particularly when the intervention is designed for hard-to-reach ethnic minority groups [48, 49]. Future meta-analysis is needed as more empirical evidence is accumulated in this regard.
Studies including populations of >40% African American or Asian American women yielded similar effect sizes, although the effect size for Asian American women was slightly larger; however, interventions involving populations of >40% Hispanic women were not associated with a significant increase in Pap test use (p=0.068). While no published analysis of intervention effects for this specific ethnic group is available, the lack of efficacy that we observed may relate to the fact that three of the five studies [17, 30, 40] had a large sample size (approaching 1,000 or more), with a small or no intervention effect. Authors of the studies cited the following as potential reasons for the limited intervention effect: possible contamination between the intervention and control communities, the fact that the dose of the intervention was spread across a wide population base, or the low educational status of the target population. Researchers are likely to face a less controlled situation as the scale of a trial increases. The lack of any significant positive effect in these studies supports the need for more tightly controlled trials to improve the efficacy of interventions targeting Hispanic women. Better monitoring of intervention fidelity would be critical to maintaining study quality. As Thompson et al. [40] have pointed out, researchers may need to consider using a smaller number of participants to maximize the resources available or consider reducing the number of intervention components to concentrate the resources in a stronger dose. In addition, more tailored, culturally aligned interventions to address low literacy among Hispanic women should be considered as alternative strategies [50, 51]. For example, storytelling was found to be an effective approach for promoting intent to obtain colorectal cancer screening, compared to a risk tool-based intervention (i.e., providing information about risk factors) among Hispanic women [52].
A limitation of our analysis is the heterogeneity found in the quality and quantity of data reported in the 18 studies. In an attempt to address this issue, we have provided effect size estimates separately for high- versus low-quality studies. The effect size calculated from groups consisting of only a small number of studies (in some cases, only four to six studies) should be considered as preliminary evidence and not as definitive estimates of these studies. There were two studies recruiting both African American and Hispanic women [17, 27]. Our ethnic subgroup analyses used the pooled proportions (i.e., each study’s effect sizes were combined over all ethnicities). Ideally, one would include only African American women from each study in the subgroup analysis (and similarly for the other ethnicities). However, few papers report the ethnicity specific results. If the African American and Hispanic women had drastically different effect sizes, combining estimates in the studies might have the effect of “muddling” the true effect, which would lead to wider confidence intervals. We looked at sensitivity analyses to see if removing any of the studies with mixed ethnicity samples would drastically change the results, which was not the case for the two mentioned above. Any paper that does not have an ethnically homogeneous sample should report ethnic specific results for more accurate estimation of ethnic-specific effect sizes. Another possible limitation is publication bias, a phenomenon that can lead to an inaccurate estimation of effect sizes by excluding unpublished data. However, some researchers [53] have reported the absence of any differences related to the inclusion or exclusion of unpublished studies. As is frequently the case in meta-analysis, 11 out of 18 studies included in the analysis used multiple intervention components, making it difficult to tease out the effect of an individual approach. Future research using study designs that permit within-study comparisons of specific intervention components (e.g., factorial designs) is needed to examine which intervention component, together or alone, has the greatest impact [15]. Finally, we did not include studies conducted outside the U.S. because our focus was on ethnic minority women in the U.S., who face unique cultural and linguistic challenges. Therefore, our findings may not be generalizable to ethnic minority women in other countries.
CONCLUSION
The results indicate that the most effective approach for increasing the use of Pap tests among ethnic minority women in the U.S. involves the use of access-enhancing strategies. Future interventions targeting ethnic minority women should also benefit from multiple, rather than single, cultural strategies. At this point, it is unclear whether a cultural strategy involving members of the target community can significantly increase Pap test use among these groups of women, given the insufficient number of studies using this method. While interventions based on social networks, such as the use of peer navigators, have been popular, the effect size obtained for this approach was smaller than those for other approaches. Future research using this approach should include rigorous training of peer navigators and a well-designed monitoring plan. Finally, additional, tightly-controlled studies are needed to improve the efficacy of cervical cancer screening interventions involving ethnic minority women, particularly Hispanic women.
Acknowledgments
This study was supported, in part, by a grant from the National Cancer Institute (R01 CA129060). Editorial support was provided by the Johns Hopkins University School of Nursing Center for Collaborative Intervention Research. Funding for the Center is provided by the National Institute of Nursing Research P30 NRO 8995. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
References
*Indicates studies included in this meta-analysis.
- 1.Trans-HHS Cancer Health Disparities Progress Review Group. Making cancer health disparities history. 2009 [Google Scholar]
- 2.Miller BA, Kolonel LN, Bernstein L, Young JL, Jr, Swanson GM, West D, Key CR, Liff JM, Glover CS, Alexander GA, et al. Racial/ethnic patterns of cancer in the United States 1988–1992. National Cancer Institute; Bethesda, MD: 1996. NIH Publication No. 96-4104. [Google Scholar]
- 3.Mills PK, Yang RC, Riordan D. Cancer incidence in the Hmong in California, 1988–2000. Cancer. 2005;104:2969–74. doi: 10.1002/cncr.21525. [DOI] [PubMed] [Google Scholar]
- 4.Carey P, Gjerdingen DK. Follow-up of abnormal Papanicolaou smears among women of different races. J Fam Pract. 1993;37:583–7. [PubMed] [Google Scholar]
- 5.Do TQN. The incidence and prevalence of cervical cancer in Vietnamese women (1993–1995): An analysis of SEER reported cases. Virginia Commonwealth University; Richmond, VA: 2005. [Google Scholar]
- 6.U S. Preventive Services Task Force. Screening for cervical cancer: Recommendations and rationale. 2003;67:1759–66. [PubMed] [Google Scholar]
- 7.American Cancer Society. Cancer prevention & early detection facts and figures. American Cancer Society; Atlanta, GA: 2008. [Google Scholar]
- 8.National Center for Health Statistics. Health, United States, 2006 with chartbook on trends in the health of Americans. National Center for Health Statistics, Centers for Disease Control and Prevention; Hyattsville, MD: 2006. [Google Scholar]
- 9.Stone EG, Morton SC, Hulscher ME, Maglione MA, Roth EA, Grimshaw JM, Mittman BS, Rubenstein LV, Rubenstein LZ, Shekelle PG. Interventions that increase use of adult immunization and cancer screening services: a meta-analysis. Ann Intern Med. 2002;136:641–51. doi: 10.7326/0003-4819-136-9-200205070-00006. [DOI] [PubMed] [Google Scholar]
- 10.Austin SM, Balas EA, Mitchell JA, Ewigman BG. Effect of physician reminders on preventive care: meta-analysis of randomized clinical trials. Proc Annu Symp Comput Appl Med Care. 1994:121–4. [PMC free article] [PubMed] [Google Scholar]
- 11.Shea S, DuMouchel W, Bahamonde L. A meta-analysis of 16 randomized controlled trials to evaluate computer-based clinical reminder systems for preventive care in the ambulatory setting. J Am Med Inform Assoc. 1996;3:399–409. doi: 10.1136/jamia.1996.97084513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Snell JL, Buck EL. Increasing cancer screening: a meta-analysis. Prev Med. 1996;25:702–7. doi: 10.1006/pmed.1996.0109. [DOI] [PubMed] [Google Scholar]
- 13.Tseng DS, Cox E, Plane MB, Hla KM. Efficacy of patient letter reminders on cervical cancer screening: a meta-analysis. J Gen Intern Med. 2001;16:563–8. doi: 10.1046/j.1525-1497.2001.016008567.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Forbes C, Jepson R, Martin-Hirsch P. Interventions targeted at women to encourage the uptake of cervical screening. Cochrane Database Syst Rev. 2002;(3):CD002834. doi: 10.1002/14651858.CD002834. [DOI] [PubMed] [Google Scholar]
- 15.Legler J, Meissner HI, Coyne C, Breen N, Chollette V, Rimer BK. The effectiveness of interventions to promote mammography among women with historically lower rates of screening. Cancer Epidemiol Biomarkers Prev. 2002;11:59–71. [PubMed] [Google Scholar]
- *16.Burack RC, Gimotty PA, George J, McBride S, Moncrease A, Simon MS, Dews P, Coombs J. How reminders given to patients and physicians affected Pap smear use in a health maintenance organization: results of a randomized controlled trial. Cancer. 1998;82:2391–400. doi: 10.1002/(sici)1097-0142(19980615)82:12<2391::aid-cncr13>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- *17.Jibaja-Weiss ML, Volk RJ, Kingery P, Smith QW, Holcomb JD. Tailored messages for breast and cervical cancer screening of low-income and minority women using medical records data. Patient Educ Couns. 2003;50:123–32. doi: 10.1016/s0738-3991(02)00119-2. [DOI] [PubMed] [Google Scholar]
- *18.Taylor VM, Hislop TG, Jackson JC, Tu SP, Yasui Y, Schwartz SM, Teh C, Kuniyuki A, Acorda E, Marchand A, Thompson B. A randomized controlled trial of interventions to promote cervical cancer screening among Chinese women in North America. J Natl Cancer Inst. 2002;94:670–7. doi: 10.1093/jnci/94.9.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sackett DL, Haynes RB. Compliance with therapeutic regimens. 1976 [Google Scholar]
- 20.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 21.Cho MK, Bero LA. Instruments for assessing the quality of drug studies published in the medical literature. JAMA. 1994;272:101–4. [PubMed] [Google Scholar]
- 22.Greenland S. Invited commentary: a critical look at some popular meta-analytic methods. Am J Epidemiol. 1994;140:290–6. doi: 10.1093/oxfordjournals.aje.a117248. [DOI] [PubMed] [Google Scholar]
- *23.Dignan M, Michielutte R, Blinson K, Wells HB, Case LD, Sharp P, Davis S, Konen J, McQuellon RP. Effectiveness of health education to increase screening for cervical cancer among eastern-band Cherokee Indian women in North Carolina. J Natl Cancer Inst. 1996;88 :1670–6. doi: 10.1093/jnci/88.22.1670. [DOI] [PubMed] [Google Scholar]
- 24.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 25.Light RJ, Pillemer DB. Summing up: The science of reviewing research. Harvard University Press; Cambridge, MA: 1984. [Google Scholar]
- 26.Rosenthal R. Meta-analysis procedures for social research. Sage; Beverly Hills, CA: 1984. [Google Scholar]
- *27.Batal H, Biggerstaff S, Dunn T, Mehler PS. Cervical cancer screening in the urgent care setting. J Gen Intern Med. 2000;15:389–94. doi: 10.1046/j.1525-1497.2000.08001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *28.Bird JA, McPhee SJ, Ha NT, Le B, Davis T, Jenkins CN. Opening pathways to cancer screening for Vietnamese-American women: lay health workers hold a key. Prev Med. 1998;27:821–9. doi: 10.1006/pmed.1998.0365. [DOI] [PubMed] [Google Scholar]
- *29.Campbell MK, Tessaro I, DeVellis B, Benedict S, Kelsey K, Belton L, Sanhueza A. Effects of a tailored health promotion program for female blue-collar workers: health works for women. Prev Med. 2002;34:313–23. doi: 10.1006/pmed.2001.0988. [DOI] [PubMed] [Google Scholar]
- *30.Dietrich AJ, Tobin JN, Cassells A, Robinson CM, Greene MA, Sox CH, Beach ML, DuHamel KN, Younge RG. Telephone care management to improve cancer screening among low-income women: a randomized, controlled trial. Ann Intern Med. 2006;144:563–71. doi: 10.7326/0003-4819-144-8-200604180-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *31.Fang CY, Ma GX, Tan Y, Chi N. A multifaceted intervention to increase cervical cancer screening among underserved Korean women. Cancer Epidemiol Biomarkers Prev. 2007;16:1298–302. doi: 10.1158/1055-9965.EPI-07-0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *32.Fernandez-Esquer ME, Espinoza P, Torres I, Ramirez AG, McAlister AL. A su salud: a quasi-experimental study among Mexican American women. Am J Health Behav. 2003;27:536–45. doi: 10.5993/ajhb.27.5.5. [DOI] [PubMed] [Google Scholar]
- *33.Jenkins CN, McPhee SJ, Bird JA, Pham GQ, Nguyen BH, Nguyen T, Lai KQ, Wong C, Davis TB. Effect of a media-led education campaign on breast and cervical cancer screening among Vietnamese-American women. Prev Med. 1999;28:395–406. doi: 10.1006/pmed.1998.0444. [DOI] [PubMed] [Google Scholar]
- *34.Lam TK, McPhee SJ, Mock J, Wong C, Doan HT, Nguyen T, Lai KQ, Ha-Iaconis T, Luong TN. Encouraging Vietnamese-American women to obtain Pap tests through lay health worker outreach and media education. J Gen Intern Med. 2003;18:516–24. doi: 10.1046/j.1525-1497.2003.21043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *35.Mandelblatt J, Traxler M, Lakin P, Thomas L, Chauhan P, Matseoane S, Kanetsky P. A nurse practitioner intervention to increase breast and cervical cancer screening for poor, elderly black women. The Harlem Study Team. J Gen Intern Med. 1993;8:173–8. doi: 10.1007/BF02599260. [DOI] [PubMed] [Google Scholar]
- *36.Mock J, McPhee SJ, Nguyen T, Wong C, Doan H, Lai KQ, Nguyen KH, Nguyen TT, Bui-Tong N. Effective lay health worker outreach and media-based education for promoting cervical cancer screening among Vietnamese American women. Am J Public Health. 2007;97 :1693–700. doi: 10.2105/AJPH.2006.086470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *37.Moskowitz JM, Kazinets G, Wong JM, Tager IB. “Health is strength”: a community health education program to improve breast and cervical cancer screening among Korean American Women in Alameda County, California. Cancer Detect Prev. 2007;31:173–83. doi: 10.1016/j.cdp.2007.02.002. [DOI] [PubMed] [Google Scholar]
- *38.Nguyen TT, McPhee SJ, Bui-Tong N, Luong TN, Ha-Iaconis T, Nguyen T, Wong C, Lai KQ, Lam H. Community-based participatory research increases cervical cancer screening among Vietnamese-Americans. J Health Care Poor Underserved. 2006;17:31–54. doi: 10.1353/hpu.2006.0091. [DOI] [PubMed] [Google Scholar]
- *39.Paskett ED, Tatum CM, D’Agostino R, Jr, Rushing J, Velez R, Michielutte R, Dignan M. Community-based interventions to improve breast and cervical cancer screening: results of the Forsyth County Cancer Screening (FoCaS) Project. Cancer Epidemiol Biomarkers Prev. 1999;8:453–9. [PubMed] [Google Scholar]
- *40.Thompson B, Coronado G, Chen L, Islas I. Celebremos la salud! a community randomized trial of cancer prevention (United States) Cancer Causes Control. 2006;17:733–46. doi: 10.1007/s10552-006-0006-x. [DOI] [PubMed] [Google Scholar]
- 41.Rakowski W, Meissner H, Vernon SW, Breen N, Rimer B, Clark MA. Correlates of repeat and recent mammography for women ages 45 to 75 in the 2002 to 2003 Health Information National Trends Survey (HINTS 2003) Cancer Epidemiol Biomarkers Prev. 2006;15:2093–101. doi: 10.1158/1055-9965.EPI-06-0301. [DOI] [PubMed] [Google Scholar]
- 42.Town RJ, Wholey DR, Feldman RD, Burns LR. Hospital consolidation and racial/income disparities in health insurance coverage. Health Aff (Millwood) 2007;26:1170–80. doi: 10.1377/hlthaff.26.4.1170. [DOI] [PubMed] [Google Scholar]
- 43.Suarez L, Roche RA, Pulley LV, Weiss NS, Goldman D, Simpson DM. Why a peer intervention program for Mexican-American women failed to modify the secular trend in cancer screening. Am J Prev Med. 1997;13:411–7. [PubMed] [Google Scholar]
- 44.Wasserman M, Bender D, Lee SY. Use of preventive maternal and child health services by Latina women: a review of published intervention studies. Med Care Res Rev. 2007;64:4–45. doi: 10.1177/1077558706296238. [DOI] [PubMed] [Google Scholar]
- 45.Rauscher GH, Hawley ST, Earp JA. Baseline predictors of initiation vs. maintenance of regular mammography use among rural women. Prev Med. 2005;40:822–30. doi: 10.1016/j.ypmed.2004.09.029. [DOI] [PubMed] [Google Scholar]
- 46.Learmonth AM. Utilizing research in practice and generating evidence from practice. Health Educ Res. 2000;15:743–56. doi: 10.1093/her/15.6.743. [DOI] [PubMed] [Google Scholar]
- 47.Corbie-Smith G, Ammerman AS, Katz ML, St George DM, Blumenthal C, Washington C, Weathers B, Keyserling TC, Switzer B. Trust, benefit, satisfaction, and burden: a randomized controlled trial to reduce cancer risk through African-American churches. J Gen Intern Med. 2003;18:531–41. doi: 10.1046/j.1525-1497.2003.21061.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Metzler MM, Higgins DL, Beeker CG, Freudenberg N, Lantz PM, Senturia KD, Eisinger AA, Viruell-Fuentes EA, Gheisar B, Palermo AG, Softley D. Addressing urban health in Detroit, New York City, and Seattle through community-based participatory research partnerships. Am J Public Health. 2003;93:803–11. doi: 10.2105/ajph.93.5.803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schulz AJ, Israel BA, Parker EA, Lockett M, Hill Y, Wills R. The East Side Village Health Worker Partnership: integrating research with action to reduce health disparities. Public Health Rep. 2001;116:548–57. doi: 10.1016/S0033-3549(04)50087-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Garbers S, Chiasson MA. Inadequate functional health literacy in Spanish as a barrier to cervical cancer screening among immigrant Latinas in New York City. Prev Chronic Dis. 2004;1:A07. [PMC free article] [PubMed] [Google Scholar]
- 51.Natale-Pereira A, Marks J, Vega M, Mouzon D, Hudson SV, Salas-Lopez D. Barriers and facilitators for colorectal cancer screening practices in the Latino community: perspectives from community leaders. Cancer Control. 2008;15:157–65. doi: 10.1177/107327480801500208. [DOI] [PubMed] [Google Scholar]
- 52.Larkey LK, Lopez AM, Minnal A, Gonzalez J. Storytelling for promoting colorectal cancer screening among underserved Latina women: a randomized pilot study. Cancer Control. 2009;16:79–87. doi: 10.1177/107327480901600112. [DOI] [PubMed] [Google Scholar]
- 53.Conn VS, Valentine JC, Cooper HM, Rantz MJ. Grey literature in meta-analyses. Nurs Res. 2003;52:256–61. doi: 10.1097/00006199-200307000-00008. [DOI] [PubMed] [Google Scholar]