Abstract
BACKGROUND
The significance of minor isolated Q waves in the resting electrocardiograms (ECGs) of apparently healthy individuals is unknown.
OBJECTIVE
To examine the association between minor isolated Q waves and incident cardiovascular disease events in the Multi-Ethnic Study of Atherosclerosis (MESA).
DESIGN
This analysis included 6551 MESA participants (38% white, 28% black, 22% Hispanic, 12% Chinese) who were free of cardiovascular disease at enrollment. Cox proportional hazards models were used to examine the association between minor isolated Q waves defined by the Minnesota ECG Classification with adjudicated incident cardiovascular events.
RESULTS
During up to 7.8 years of follow-up, 423 events occurred, with a rate of 10.7 events per 1000 person-years. A significant interaction between minor isolated Q waves and race/ethnicity was observed (P = .030). In models stratified by race/ethnicity and adjusted for demographics, socioeconomic status, common cardiovascular risk factors, and other ECG abnormalities, presence of isolated minor Q waves was significantly associated with incident cardiovascular events in Hispanics (hazard ratio [HR] 2.62; 95% confidence interval [CI], 1.42-4.82), but not in whites (HR 0.65; 95% CI, 0.32-1.33) or blacks (HR 1.46; 95% CI, 0.74-2.89). Despite the statistically significant association in the Chinese population, the small number of events precluded solid conclusions in this race/ethnicity.
CONCLUSION
The prognostic significance of minor isolated Q waves varies across races/ethnicities; they carry a high risk for future cardiovascular events in apparently healthy Hispanics, but not in whites or blacks.
Keywords: Electrocardiography, MESA, Minor isolated Q waves, Race/ethnicity
Minor isolated Q waves are common electrocardiographic findings in apparently healthy individuals.1 However, their prognostic significance as a risk factor for poor future cardiovascular outcomes is unclear. Particularly problematic are the minor isolated Q waves in inferior leads (especially in leads III and aVF), which may appear in an electrocardiogram (ECG) as an effect of the electrical orientation of the heart.1 Previous studies have reported a strong association between minor isolated ST/T abnormalities and incident cardiovascular events independent of traditional cardiovascular risk factors.2-9 In these studies, the magnitude of increased risk associated with isolated minor ST/T abnormalities was similar to that associated with smoking, diabetes, hypercholesterolemia, and hypertension.7-9 This emphasizes the potential role of minor ECG abnormalities as prognostic markers of future cardiovascular outcomes. We examined the association between minor isolated Q waves and incident cardiovascular events in the Multi-Ethnic Study of Atherosclerosis (MESA). We also examined possible interactions between minor isolated Q waves and factors that could impact their associations with incident cardiovascular events. This included examining interaction by race/ethnicity, which we found significant, and subsequently stratified the analysis by race/ethnicity.
METHODS
Study Population and Data Collection
MESA is a prospective study designed to explore the prevalence, correlates, and progression of subclinical cardiovascular disease in a population-based multi-ethnic cohort. The study objectives, design, and methods have been previously reported.10 Briefly, between July 2000 and August 2002, 6814 men and women aged 45 to 84 years and free of clinically apparent cardiovascular disease were recruited from 6 US communities: Baltimore City and Baltimore County, Maryland; Chicago, Illinois; Forsyth County, North Carolina; Los Angeles County, California; Northern Manhattan and the Bronx, New York; and St. Paul, Minnesota. Individuals with a history of physician-diagnosed myocardial infarction, angina, heart failure, atrial fibrillation, stroke, or transient ischemic attack, or who had undergone an invasive cardiovascular procedure (coronary artery bypass graft surgery, angioplasty, valve replacement, pacemaker placement, or other vascular surgeries) were excluded from participation. The institutional review boards at all participating centers approved the study, and all participants gave informed consent.
Demographics including self-reported race/ethnicity, medical history, and anthropometric, electrocardiographic, and laboratory data needed for our analysis were taken from the first examination (baseline) visit. Hypertension was defined as a systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or use of blood pressure-lowering drugs. Total cholesterol and high-density lipoprotein (HDL) cholesterol were measured from blood samples obtained after a 12-hour fast. Low-density lipoprotein (LDL) cholesterol was estimated by the Friedewald equation.11 Diabetes mellitus was defined as fasting glucose >125 mg/dL or the use of hypoglycemic medications.
All MESA participants with good quality baseline ECG data were eligible for inclusion in this analysis. We excluded 103 participants with missing or poor quality ECGs. Further, and in addition to the ECG exclusion criteria for enrollment in MESA (atrial fibrillation, complete atrioventricular block, pacemaker), we excluded 155 participants with ECG evidence of major Q waves or myocardial infarction, 3 participants with second-degree atrioventricular block, one participant with atrial flutter, and one participant with Wolff-Parkinson-White syndrome. Because major intraventricular conduction defects (QRS ≥120 ms) suppress reading the ECGs for minor Q by Minnesota ECG Classification (ie, minor isolated Q will be considered as not present), we did not exclude participants with major intraventricular conduction defects, but we adjusted for it in the full model. After all exclusions (n = 263), 6551 participants remained and were included in the analysis.
Electrocardiography
Standard 12-lead ECG was digitally acquired using a GE MAC 1200 electrocardiograph (GE Healthcare, Milwaukee, Wis) at 10 mm/mV calibration and speed of 25 mm/s. ECG reading was performed centrally at the Epidemiological Cardiology Research (EPICARE) center, Wake Forest School of Medicine, Winston Salem, NC. All ECGs were initially inspected visually for technical errors and inadequate quality before being automatically processed using GE 12-SL Marquette Version 2001 (GE Healthcare). ECG abnormalities were classified and coded using the Minnesota ECG Classification.12 Minor isolated Q waves were defined as Minnesota Codes 1.3.X that are not codeable as myocardial infarction and in the absence of any other major Q waves. All minor Q waves defined by Minnesota Code 1.3.X were <0.04 seconds in duration. Minor ST/T abnormalities were defined as Minnesota Codes 4.3, 4.4, 5.3, or 5.4, while major ST/T abnormalities were defined as Minnesota Codes 4.1, 4.2, 5.1, or 5.2. Abnormal QRS axis was defined as any QRS axis that does not fall between +90° to −30°. Cornell voltage criteria were used to define left ventricular hypertrophy (ECG-LVH).13
Ascertainment of Cardiovascular Events
Cardiovascular events were adjudicated by an adjudication committee that included cardiologists, physician epidemiologists, and neurologists. A detailed description of the cardiovascular event adjudication process has already been published.14 For the purposes of this study, we used a composite outcome of fatal and nonfatal cardiovascular events. This included myocardial infarction, resuscitated cardiac arrest, definite angina, probable angina (if followed by revascularization), percutaneous transluminal coronary angioplasty, coronary stent, coronary atherectomy, coronary bypass graft, coronary or other revascularization, congestive heart failure, coronary heart disease death, and other atherosclerotic or cardiovascular death such as sudden cardiac death or out-of-hospital death believed to be a complication of cardiovascular disease.
Statistical Analysis
The prevalence of minor Q waves stratified by key demographics and common cardiovascular risk factors that could affect presence of Q wave (sex, race/ethnicity, age, diabetes, and hypertension) was calculated and compared among strata.
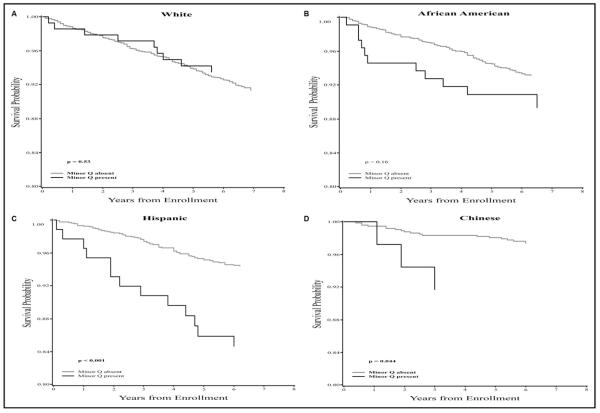
Log-rank tests were used to evaluate the bivariate association between minor isolated Q waves and incident cardiovascular events for the overall sample and by race/ethnicity. Kaplan-Meier plots were generated to graphically describe the probability of event-free survival over time.
Cox proportional hazards analysis was used to assess the association between baseline minor isolated Q waves with incident cardiovascular events. Interactions between sex, race/ethnicity, age, ST/T abnormalities, and abnormal QRS axis with minor isolated Q waves for incident cardiovascular events were initially examined. Because of a significant interaction by race/ethnicity (P = .030), multivariable race/ethnicity-stratified models were created with incremental adjustment for demographics (age and sex), socioeconomic status (education and income), common cardiovascular risk factors (body mass index, systolic blood pressure, blood pressure-lowering drugs, diabetes, total cholesterol, lipid-lowering drugs, smoking status), and other ECG abnormalities (ECG-LVH, abnormal QRS axis, ST/T abnormalities and intraventricular conduction defects). Event time was defined as the number of days from baseline until the first cardiovascular event or censored at the last available MESA visit or noncardiovascular death if event-free. Because individuals with ECG abnormalities suggestive of myocardialischemia/infarction may be more likely to undergo evaluation for coronary artery disease, and might therefore be more likely to undergo revascularization, we reran the analysis after excluding coronary revascularization from the endpoint. Statistical analysis was performed using SAS version 9.2.2 (SAS Institute, Cary, NC).
RESULTS
In the 6551 participants included in this analysis, the mean age was approximately 62 years, with 54% females, 38% whites, 28% blacks, 22% Hispanics, and 12% Chinese. Table 1 shows the characteristics of our analysis population stratified by race/ethnicity. Compared to other races/ethnicities, the Chinese population had lower smoking rates, lower LDL cholesterol, lower prevalence of hypertension, and smaller body mass index. On the other hand, whites had lower prevalence of diabetes and higher levels of HDL cholesterol, while blacks had lower triglyceride levels. Generally, the Hispanic population had higher LDL cholesterol and triglycerides levels but lower HDL cholesterol (Table 1).
Table 1.
Baseline Characteristics of the Study Population
| Characteristics | White n = 2507 |
African American n = 1822 |
Hispanic n = 1447 |
Chinese n = 775 |
P-Value |
|---|---|---|---|---|---|
| Age (years) | 62.49 ± 10.21 | 62.07 ± 10.04 | 61.2 ± 10.32 | 62.28 ± 10.32 | .002 |
| Females | 1320 (52.7) | 1026 (56.3) | 754 (52.1) | 407 (52.5) | .047 |
| Smoker | |||||
| Never | 1105 (44.2) | 821 (45.4) | 786 (54.3) | 586 (75.7) | <.001 |
| Former | 1109 (44.3) | 664 (36.7) | 462 (31.9) | 143 (18.5) | <.001 |
| Current | 288 (11.5) | 323 (17.9) | 199 (13.8) | 45 (5.8) | <.001 |
| Total cholesterol (mg/dL) | 195.85 ± 34.93 | 189.99 ± 36.14 | 197.92 ± 37.61 | 192.92 ± 31.45 | <.001 |
| LDL cholesterol (mg/dL) | 117.16 ± 30.09 | 116.64 ± 32.98 | 119.6 ± 32.91 | 115.32 ± 28.92 | .01 |
| HDL cholesterol (mg/dL) | 52.4 ± 15.69 | 52.53 ± 15.25 | 47.76 ± 13.09 | 49.63 ± 12.65 | <.001 |
| Triglycerides (mg/dL) | 132.81 ± 90.62 | 104.85 ± 68.94 | 156.04 ± 101.2 | 142.76 ± 84.91 | <.001 |
| Body mass index (kg/m2) | 27.73 ± 5.07 | 30.21 ± 5.87 | 29.42 ± 5.09 | 23.95 ± 3.3 | <.001 |
| Hypertension | 957 (38.2) | 1079 (59.2) | 594 (41.1) | 286 (36.9) | <.001 |
| Systolic blood pressure | 123.4 (20.4) | 131.52 (21.5) | 126.6 (21.8) | 124.53 (21.6) | <.001 |
| Diastolic blood pressure | 70.23 (10.0) | 74.37 (10.2) | 71.48 (10.1) | 71.89 (10.3) | <.001 |
| Diabetes mellitus | 148 (5.9) | 313 (17.3) | 253 (17.5) | 102 (13.2) | <.001 |
| QRS axis | 20.97 ± 32.53 | 15.95 ± 30.17 | 15.21 ± 29.51 | 31.54 ± 31.7 | <.001 |
| Abnormal QRS axis | 177 (7.1) | 125 (6.86) | 87 (6.01) | 31 (4) | .016 |
| Left ventricular hypertrophy | 146 (5.8) | 112 (6.2) | 77 (5.3) | 46 (5.9) | .79 |
| ST/T abnormalities | |||||
| Any ST/T abnormalities | 261 (10.4) | 343 (18.8) | 202 (14.0) | 91 (11.7) | <.001 |
| Minor ST/T abnormalities | 224 (8.9) | 315 (17.3) | 188 (13.0) | 77 (9.9) | <.001 |
| Major ST/T abnormalities | 76 (3.0) | 112 (6.2) | 47 (3.3) | 33 (4.3) | <.001 |
HDL = high-density lipoprotein;LDL = low-density lipoprotein.
Values are expressed as mean ± SD or number (%).
Minor isolated Q wave was present in 377 (5.8%) of the participants. Table 2 shows the prevalence of minor isolated Q waves in any of the 3 ECG lead groups (anterior, lateral, and inferior) and in each lead group stratified by age, sex, race/ethnicity, hypertension, and diabetes. There was no statistically significant difference in the prevalence of minor isolated Q waves in any ECG lead group between males and females or among races/ethnicities. On the other hand, older age and individuals with hypertension were more likely to have minor isolated Q waves in any ECG lead group. Individuals with diabetes had a higher prevalence of minor isolated Q waves in any ECG lead group, but the difference was marginally significant. Notably, females had more minor isolated Q waves in the anterior ECG lead group, while individuals with diabetes and hypertension had these minor isolated waves more in the inferior ECG lead group.
Table 2.
Baseline Prevalence of Minor Isolated Q Waves by ECG Lead Group
| Any Lead Group % (n) |
P-Value | Anterior Lead Group* % (n) |
P-Value | Lateral Lead Group† % (n) |
P-Value | Inferior Lead Group‡ % (n) |
P-Value | |
|---|---|---|---|---|---|---|---|---|
| Age (years) | ||||||||
| < 50 (n = 1053) | 4.8 (51) | .038 | 1.3 (14) | .12 | 1.1 (12) | .79 | 2.8 (29) | .07 |
| 51-60 (n = 1957) | 5.0 (98) | 0.6 (12) | 1.2 (24) | 3.3 (65) | ||||
| > 60 (n = 3541) | 6.4 (228) | 1.0 (36) | 1.4 (49) | 4.2 (147) | ||||
| Sex | ||||||||
| Females (n = 3507) | 5.6 (198) | .68 | 1.2 (41) | .046 | 1.3 (44) | .74 | 3.3 (117) | .11 |
| Males (n = 3044) | 5.9 (179) | 0.7 (21) | 1.3 (41) | 4.1 (124) | ||||
| Race/ethnicity | ||||||||
| White (n = 2507) | 5.6 (141) | .54 | 1.0 (26) | .06 | 1.6 (40) | .12 | 3.3 (82) | .07 |
| African American (n = 1822) | 6.2 (112) | 1.3 (24) | 1.4 (26) | 3.5 (63) | ||||
| Hispanic (n = 1447) | 6.0 (87) | 0.4 (6) | 1.0 (14) | 4.8 (70) | ||||
| Chinese (n = 775) | 4.8 (37) | 0.8 (6) | 0.6 (5) | 3.3 (26) | ||||
| Diabetes status | ||||||||
| Without diabetes (n = 5735) | 5.5 (317) | .05 | 1.0 (55) | .77 | 1.4 (78) | .23 | 3.4 (193) | .001 |
| With diabetes (n = 816) | 7.2 (59) | 0.9 (7) | 0.9 (7) | 5.8 (47) | ||||
| Hypertension | ||||||||
| Without hypertension (n = 3635) |
5.0 (183) | .005 | 0.9 (31) | .38 | 1.2 (45) | .63 | 3.1 (114) | .009 |
| With hypertension (n = 2916) |
6.7 (194) | 1.1 (31) | 1.4 (40) | 4.4 (127) |
ECG = electrocardiogram.
Leads V1-V5.
Leads I, aVL, V6.
Leads II, III, aVF.
During up to 7.8 years of follow-up (median 6.5 years), 423 cardiovascular events occurred. Overall, the event rate in the study participants with minor isolated Q waves was significantly higher than the event rate in those without minor isolated Q waves (P = .012) (Table 3). A significant interaction between presence of minor isolated Q waves and race/ethnicity for prediction of cardiovascular events was observed (P = .030). No significant interaction was observed for sex, age, abnormal ST/T abnormalities, or QRS axis.
Table 3.
Incidence Rate of Cardiovascular Events in Participants with and without Minor Isolated Q Waves
| Incident Rate per 1000 Person-year |
||||
|---|---|---|---|---|
| Overall | Without Minor Q Waves |
With Minor Q Waves |
Rate Ratio (95% CI) |
|
| All population | 10.7 | 10.4 | 16.1 | 1.55 (1.10-2.17) |
| White | 12.7 | 12.8 | 10.4 | 0.81 (0.41-1.57) |
| Black | 11.3 | 11.0 | 16.9 | 1.54 (0.82-2.86) |
| Hispanic | 9.9 | 8.8 | 26.3 | 2.96 (1.64-5.34) |
| Chinese | 4.6 | 4.2 | 13.6 | 3.24 (0.96-10.94) |
CI = confidence interval.
The Figure shows the event-free survival curves of participants with and without minor isolated Q waves in the study population stratified by race/ethnicity. As shown, minor isolated Q waves were associated with higher risk of cardiovascular disease in Hispanics (log-rank P-value <.001) but not in whites or blacks. Similarly, in a Cox proportional hazard model adjusted for demographics and socioeconomic status, minor isolated Q waves in Hispanics were associated with almost 3 times higher risk of incident cardiovascular events (HR 2.80; 95% CI, 1.54-5.07). On the other hand, presence of minor isolated Q waves in whites and blacks did not confer any statistically significant increase in cardiovascular risk (HR 0.74; 95% CI 0.36-1.50) in whites, and HR 1.58; 95% CI, 0.82-3.03) in African Americans. This pattern of associations persisted after further adjustment for cardiovascular disease risk factors and other ECG abnormalities (Table 4). The small number of events (n = 22) in the Chinese population precluded solid conclusions in this race/ethnicity.
Figure.
Kaplan-Meier survival curves for incident cardiovascular events in MESA participants with and without minor isolated Q waves stratified by race/ethnicity (MESA study 2000-2008). *P value for log-rank test.
Table 4.
Multivariable Hazard Ratios (HR) and 95% Confidence Intervals (CI) for Incident Cardiovascular Events Associated with Presence of Minor Isolated Q Waves Stratified by Race/Ethnicity
| Model 1* HR (95% CI) |
Model 2† HR (95% CI) |
|
|---|---|---|
| White | 0.68 (0.33-1.34) | 0.65 (0.32-1.33) |
| Black | 1.59 (0.82-3.01) | 1.46 (0.74-2.89) |
| Hispanic | 2.57 (1.41-4.69) | 2.62 (1.42-4.82) |
The Chinese group was excluded from multivariable analysis because of its small number of events.
Model 1: Demographic variables (age and sex), socioeconomic status (education and income), and cardiovascular disease risk factors (body mass index, total cholesterol, lipid-lowering drugs, smoking status, systolic blood pressure, blood pressure lowering drugs, diabetes).
Model 2: Variables in Model 1 plus other electrocardiographic abnormalities (abnormal QRS axis, ST/T abnormalities, left ventricular hypertrophy, and intraventricular conduction defects).
Similar results were obtained after excluding coronary revascularization from the end point (Supplemental Table 1, online).
DISCUSSION
We showed that minor isolated Q waves are fairly common in the ECGs of individuals free of cardiovascular disease. Although there was no significant difference in the prevalence of minor isolated Q waves among races/ethnicities, the prognostic significance was different. As shown, after adjusting for demographics, socioeconomic status, cardiovascular disease risk factors, and ECG abnormalities, presence of minor isolated Q waves was strongly associated with incident cardiovascular events in Hispanics, but not in whites or blacks.
Lack of prognostic significance of minor isolated Q waves in whites and blacks supports the current practice that considers these minor ECG findings as nonpathological.12,15,16 On the other hand, our findings in Hispanics raise concerns about the appropriateness of applying the current standards of ECG interpretation to races/ethnicities other than whites and blacks. If our results were replicated in other cohorts, changing our interpretation of routine ECG to consider the racial/ethnic differences in the prognostic significance of minor isolated Q waves may be warranted.
The reasons for the racial/ethnic differences in the prognostic significance of minor isolated Q waves are totally unclear and would be just speculations. Differences in the anthropometric measures between Hispanics and Chinese compared with whites and blacks may partially explain the observed differences in the prognostic significance of minor isolated Q waves in our study. Non-myocardial-infarction-related minor isolated Q waves can be present due to vertical position of the heart, altered ventricular conduction, ventricular enlargement, and noncoronary heart disease.17,18 Most of these nonischemic/nonpathological situations are accompanied by a vertical positioning of the heart either anatomically or electrically (axis), which in turn can enhance appearance of nonpathological Q waves that may come from the depolarization of the ventricular septum. Generally, Hispanics are shorter than whites and blacks,19 and subsequently could have a more horizontally oriented heart, which makes it less likely to be more vertical and hence less likely for the non-myocardial-infarction-related Q waves to appear. In other words, the shorter stature and horizontal heart position of Hispanics and the Chinese (compared with whites and blacks) minimize the possibility of appearance of any Q waves unless caused by myocardial injury, and hence, minor isolated Q waves in Hispanics and the Chinese reflect underlying pathology rather than a normal variant. Noteworthy, the average height of the Hispanic participants in MESA at the baseline visit was 161.9 cm, which is 7.1 cm shorter than whites and 6.5 cm shorter than blacks. Similarly, the average height of the Chinese participants was 161.5 cm, which is 7.4 cm shorter than whites and 6.8 cm shorter than blacks. Examining the relationship between minor isolated Q waves and myocardial structural abnormalities, especially myocardial scar by cardiac magnetic resonance imaging, may shed light on the pathophysiology behind minor isolated Q waves in different races/ethnicities.
In the Framingham Heart Study, diabetic patients had increased incidence of silent myocardial infarction compared with nondiabetic patients.20,21 This may explain our finding that minor isolated Q waves were more common (especially in the inferior lead group) in individuals with diabetes and hypertension, and this may be an indication of previous silent ischemic events in this high-risk population.
Studies reporting differences in ECG findings across races/ethnicities are limited, and reports on the racial/ethnic differences in the prognostic significance of these ECG findings are even more limited. A study of over 44,000 ECGs reported lower prevalence of ECG markers of coronary heart disease, atrial fibrillation, and left ventricular hypertrophy in Hispanics, compared with non-Hispanics.22 However, ECG abnormalities included in that study conferred an approximately 2-fold increase in risk of cardiovascular death, which was similar to that of the non-Hispanic subgroup. At first glance, these findings contradict our observation of no difference in the prevalence of minor isolated Q waves among races/ethnicities, and that minor isolated Q waves carry prognostic significance in Hispanics but not other races/ethnicities. However, the fact that presence of minor isolated Q waves was not considered an abnormal finding in that study may explain such contradiction. Further, Hispanic participants in that study were predominantly men (8.8% women), and were compared with non-Hispanics collectively, not individual races/ethnicities.
Hispanics reportedly have lower all-cause and cardiovascular mortality despite increased prevalence of traditional cardiovascular risk factors, which has been called the “Hispanic Paradox.”23 Nevertheless, it has been suggested that vital statistics under-ascertain minority deaths, especially in Hispanics, and that cohort studies may provide better estimates.24 In the San Antonio Heart Study,25 risk factor distributions predicted higher all-cause and cardiovascular mortality among Mexican Americans than among non-Hispanic whites. Follow-up of that cohort confirmed a mortality ratio of 1.38 for all-cause and 1.30 for cardiovascular mortality for Mexican Americans vs non-Hispanic whites.
The MESA study excluded participants with a self-reported history of cardiovascular disease, including myocardial infarction and ischemia. Hence, it may be argued that differences in access to health care might have led to including Hispanics with minor isolated Q waves that represent silent myocardial infarctions that they never know about due to less access to health care. However, the similar prevalence of minor isolated Q waves across all races/ethnicities, and adjustment for socioeconomic status, makes it less likely that our results are due to selection bias.
Our results should be read in the context of some limitations and strengths. The fewer cardiovascular events in the Chinese population limited our ability to appropriately interpret the results in this racial/ethnic group. We could not examine whether presence of minor isolated Q waves in the group with more than one ECG lead is associated with higher risk compared with one ECG lead because there were only 9 participants with minor isolated Q waves in the group with more than one lead. Our study also has several strengths. This is the first report from a well-established multi-ethnic cohort showing the racial/ethnic differences in the prognostic significance of minor isolated Q waves that are considered nonpathological by the current guidelines of ECG interpretation. Cardiovascular events in MESA were adjudicated by a committee of expert physicians, and the minor isolated Q waves were detected from standard digital ECGs that were recorded by trained technicians using an electrode locator, and were centrally read in an ECG core laboratory using standard ECG classification.
CONCLUSIONS
We showed that presence of minor isolated Q waves in the ECG of individuals free of cardiovascular disease carries a high risk of future cardiovascular events in Hispanics, but not in whites or blacks. Clinicians may need to be more aware of the possible consequences of minor Q waves in Hispanic populations.
Supplementary Material
Supplemental Table 1 Multivariable Hazard Ratios (HR) and 95% Confidence Intervals (CI) for Incident Cardiovascular Events (Excluding Coronary Revascularization) Associated with Presence of Minor Isolated Q Waves Stratified by Race/Ethnicity
CLINICAL SIGNIFICANCE.
The prognostic significance of minor isolated Q waves in the resting 12-lead electrocardiogram varies across races/ethnicities; they carry a high risk for future cardiovascular events in apparently healthy Hispanics but not in whites or blacks.
Interpretation of minor isolated Q waves in Hispanics should consider possible association of this common ECG abnormality with future cardiovascular events.
ACKNOWLEDGMENT
The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Funding: The Multi-Ethnic Study of Atherosclerosis (MESA) study was supported by contracts N01-HC-95159 through N01-HC-95169 from the National Heart, Lung and Blood Institute.
Footnotes
Conflict of Interest: None.
Authorship: All authors had role in writing the manuscript and access to the data.
References
- 1.Chou TC. Electrocardiography in Clinical Practice. 4th ed Saunders; Philadelphia: 1996. Normal and abnormal electrocardiograms in adults; pp. 3–22. [Google Scholar]
- 2.Kumar A, Lloyd-Jones DM. Clinical significance of minor nonspecific ST-segment and T-wave abnormalities in asymptomatic subjects: a systematic review. Cardiol Rev. 2007;15(3):133–142. doi: 10.1097/01.crd.0000249382.65955.14. [DOI] [PubMed] [Google Scholar]
- 3.The pooling project research group Relationship of blood pressure, serum cholesterol, smoking habit, relative weight and ECG abnormalities to incidence of major coronary events: final report of the pooling project. J Chronic Dis. 1978;31(4):201–306. doi: 10.1016/0021-9681(78)90073-5. [DOI] [PubMed] [Google Scholar]
- 4.Daviglus ML, Liao Y, Greenland P, et al. Association of nonspecific minor ST-T abnormalities with cardiovascular mortality: the Chicago Western Electric Study. JAMA. 1999;281(6):530–536. doi: 10.1001/jama.281.6.530. [DOI] [PubMed] [Google Scholar]
- 5.De Bacquer D, Martins Pereira LS, De Backer G, et al. The predictive value of electrocardiographic abnormalities for total and cardiovascular disease mortality in men and women. Eur Heart J. 1994;15(12):1604–1610. doi: 10.1093/oxfordjournals.eurheartj.a060441. [DOI] [PubMed] [Google Scholar]
- 6.Greenland P, Xie X, Liu K, et al. Impact of minor electrocardiographic ST-segment and/or T-wave abnormalities on cardiovascular mortality during long-term follow-up. Am J Cardiol. 2003;91(9):1068–1074. doi: 10.1016/s0002-9149(03)00150-4. [DOI] [PubMed] [Google Scholar]
- 7.Kannel WB, Anderson K, McGee DL, et al. Nonspecific electrocardiographic abnormality as a predictor of coronary heart disease: the Framingham Study. Am Heart J. 1987;113(2 Pt 1):370–376. doi: 10.1016/0002-8703(87)90280-8. [DOI] [PubMed] [Google Scholar]
- 8.Kumar A, Prineas RJ, Arnold AM, et al. Prevalence, prognosis, and implications of isolated minor nonspecific ST-segment and T-wave abnormalities in older adults: Cardiovascular Health Study. Circulation. 2008;118(25):2790–2796. doi: 10.1161/CIRCULATIONAHA.108.772541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prineas RJ, Grandits G, Rautaharju PM, et al. Long-term prognostic significance of isolated minor electrocardiographic T-wave abnormalities in middle-aged men free of clinical cardiovascular disease (The Multiple Risk Factor Intervention Trial [MRFIT]) Am J Cardiol. 2002;90(12):1391–1395. doi: 10.1016/s0002-9149(02)02881-3. [DOI] [PubMed] [Google Scholar]
- 10.Bild DE, Bluemke DA, Burke GL, et al. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol. 2002;156(9):871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 11.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502. [PubMed] [Google Scholar]
- 12.Prineas RJ, Crow R, Blackburn HW. The Minnesota Code Manual of Electrocardiographic Findings: Standards and Procedures for Measurement and Classification. J. Wright; Boston, MA: 1982. [Google Scholar]
- 13.Devereux RB, Casale PN, Eisenberg RR, et al. Electrocardiographic detection of left ventricular hypertrophy using echocardiographic determination of left ventricular mass as the reference standard. Comparison of standard criteria, computer diagnosis and physician interpretation. J Am Coll Cardiol. 1984;3(1):82–87. doi: 10.1016/s0735-1097(84)80433-7. [DOI] [PubMed] [Google Scholar]
- 14.Bluemke DA, Kronmal RA, Lima JA, et al. The relationship of left ventricular mass and geometry to incident cardiovascular events: The MESA (Multi-ethnic Study of Atherosclerosis) study. J Am Coll Cardiol. 2008;52(25):2148–2155. doi: 10.1016/j.jacc.2008.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thygesen K, Alpert JS, White HD, et al. Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. Circulation. 2007;116(22):2634–2653. doi: 10.1161/CIRCULATIONAHA.107.187397. [DOI] [PubMed] [Google Scholar]
- 16.Luepker RV, Apple FS, Christenson RH, et al. Case definitions for acute coronary heart disease in epidemiology and clinical research studies. A statement from the AHA Council on Epidemiology and Prevention; AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation. 2003;108:2543–2549. doi: 10.1161/01.CIR.0000100560.46946.EA. [DOI] [PubMed] [Google Scholar]
- 17.Goldberger AL. Normal and noninfarct Q waves. Cardiol Clin. 1987;5(3):357–366. [PubMed] [Google Scholar]
- 18.Chou TC. Pseudo-infarction (noninfarction Q waves) Cardiovasc Clin. 1973;5(3):199–218. [PubMed] [Google Scholar]
- 19.Carroll JF, Chiapa AL, Rodriquez M, et al. Visceral fat, waist circumference, and BMI: impact of race/ethnicity. Obesity (Silver Spring) 2008;16(3):600–607. doi: 10.1038/oby.2007.92. [DOI] [PubMed] [Google Scholar]
- 20.Margolis JR, Kannel WS, Feinleib M, et al. Clinical features of unrecognized myocardial infarction: silent and asymptomatic: eighteen-year follow-up study: the Framingham Study. Am J Cardiol. 1973;32(1):1–7. doi: 10.1016/s0002-9149(73)80079-7. [DOI] [PubMed] [Google Scholar]
- 21.Kannel WB, Abbott RD. Incidence and prognosis of unrecognized myocardial infarction: an update on the Framingham Study. N Engl J Med. 1984;311(18):1144–1147. doi: 10.1056/NEJM198411013111802. [DOI] [PubMed] [Google Scholar]
- 22.Perez MV, Yaw TS, Myers J, et al. Prognostic value of the computerized ECG in Hispanics. Clin Cardiol. 2007;30(4):189–194. doi: 10.1002/clc.20053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lerman-Garber I, Villa AR, Caballero E. Diabetes and cardiovascular disease. Is there a true Hispanic paradox? Rev Invest Clin. 2004;56(3):282–296. [PubMed] [Google Scholar]
- 24.Stern MP, Wei M. Do Mexican Americans really have low rates of cardiovascular disease? Prev Med. 1999;29(6 Pt 2):S90–S95. doi: 10.1006/pmed.1998.0464. [DOI] [PubMed] [Google Scholar]
- 25.Mitchell BD, Hazuda HP, Haffner SM, et al. Myocardial infarction in Mexican-Americans and non-Hispanic whites. The San Antonio Heart Study. Circulation. 1991;83(1):45–51. doi: 10.1161/01.cir.83.1.45. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1 Multivariable Hazard Ratios (HR) and 95% Confidence Intervals (CI) for Incident Cardiovascular Events (Excluding Coronary Revascularization) Associated with Presence of Minor Isolated Q Waves Stratified by Race/Ethnicity