Abstract
Though significant data exist highlighting the extent of health disparities there is limited data specifically on dermatologic health disparities. Melanoma and nonmelanoma skin cancer outcomes are poorer for ethnic minorities, people of low socioeconomic status, less educated, elderly, and uninsured. Recent reports indicate that atopic dermatitis is more prevalent among ethnic minorities; however it is unclear if morbidity is also increased in these populations. Given the current dermatology workforce shortage, the increased patient load may have an adverse effect on dermatologic care access. Additional concerns include the state of dermatologic training, insufficient research involving ethnic minorities, and a lack of investigations of dermatologic health disparities. As the U.S. demographics shift to become more racially diverse, the need to address and reduce dermatologic health disparities will increase.
Keywords: health disparities, dermatology, education, workforce, atopic dermatitis, skin cancer, research
Health disparity refers to “a chain of events signified by a difference in: 1) environment, 2: access to, utilization of, and quality of care, 3: health status, or 4) a particular health outcome that deserves scrutiny.”1 Disparities can be broad and across a variety of demographic variables including, but not limited to, race, age, sex, education, and health insurance status. The 2010 U.S. Department of Health and Human Services National Healthcare Disparities Report confirms substantial health care-related barriers. The report identified access to and quality of care as inadequate, particularly for ethnic minorities and persons with low income.2 Over the 8 years that the Agency for Healthcare Research and Quality (AHRQ) has reported on the status of health care quality and disparities, they have observed that, though quality of care is improving, access to care and the state of health disparities are not.2 In collaboration with the AHQR, the Institute of Medicine Committee on Future Directions for the National Healthcare Quality and Disparities Reports identified eight national priority areas to address including population health, safety and access. Evidence of health disparities across race, ethnicity, and socioeconomic status was demonstrated for all eight priorities areas.
The paucity of and great need for data on epidemiology, natural history, clinical presentation, complications, and treatment of specific skin diseases in people of color has also been highlighted recently in the dermatologic literature.3 According to a recent report, “empiric evidence regarding access to and use of dermatologic care services [in minority populations] is scant.”4
Race and ethnicity
Race is a poorly defined term that, at times, is used interchangeably with the term ethnicity. Practically, race is a political and social construct more than a biologic phenomenon.5 In contrast, ethnicity refers to “ … large groups of people classed according to common racial, national, tribal, religious, linguistic, or cultural origin or background.”6 Despite the complexities of defining race and ethnicity, health disparities between those who define themselves as white compared to others clearly exist. Since 1974 the number of office visits to dermatologists nearly doubled (from 18 million to 36 million by 2000) and the majority of patients seen by dermatologists are white (92%)—whereas this number for non-dermatologists is 84%.7 The reasons for lower dermatologic care utilization by racial minorities are unclear. For this appraisal of dermatologic health disparities, skin cancer and atopic dermatitis were selected for review as each is relatively common, and the association with health disparities has been examined for both diagnoses. Clearly there are many other skin diseases seen by both dermatologists and nondermatologists including acne, rosacea, psoriasis, and many others, but there are little to no data on dermatologic health disparities related to those conditions. Other topics addressed in this review include health reform and the dermatologic workforce, dermatologic education, and research.
Skin Cancer
Skin cancer morbidity and mortality are disproportionally higher in blacks, Hispanics, and people of low SES.8-12 Melanoma is more common in non-Hispanic whites and people of high socioeconomic status (SES)13, yet blacks, Hispanics, people of low SES13-14, and older age persons often present with more advanced disease or have increased mortality.8-10, 15-16 The 5-year melanoma survival is 74.1% for blacks compared to 92.9% for whites.16 Nonmelanoma skin cancer (NMSC) in blacks is uncommon with an incidence of 3.4 per 100,000.17 Despite the lower incidence of NMSC in ethnic minorities, blacks as a whole, present with later stage or more aggressive squamous cell carcinomas.9 The less educated tend to have lower SC screening rates and more often have poor or inaccurate perceptions of their skin cancer risk.18-19 Like the less educated, ethnic minorities, the elderly, and people with lower income may be more likely to have inaccurate skin cancer risk perceptions.19 Lack of insurance and increased age also negatively impact skin cancer outcomes.14, 20
Atopic Dermatitis (AD)
The incidence of childhood eczema in the United States is approximately 10.7%.21 Large scale reports estimate the prevalence is between 8.3% and 18.1%21-23 and it may be increasing.24-25 Black race or multiracial background was significantly correlates with eczema prevalence. 21 Similarly, black and Asian children are more often seen for the diagnosis of AD than white children25-26, suggesting increased prevalence or severity of this disorder among these racial minorities. Just as increased SES is associated with higher rates of melanoma13-14, greater than high school education by a household member is significantly associated with the increased prevalence of eczema.21 It is unclear if, like skin cancer, the morbidity of atopic dermatitis is increased with decreased SES. Beyond race, urban setting, health insurance status, single mother household, and smaller family size, are also associated with increased risk of childhood eczema.21 Presence of eczema appears to be significantly greater in the insured that the uninsured21; however, one consideration is that those without insurance are often without health care access as well and thus are not diagnosed leading to prevalence data that in all probability is an underestimate.
Multiple studies have shown that breastfeeding is associated with a reduced risk of atopic dermatitis, as well as a variety of other ailments (e.g., asthma, obesity, childhood leukemia, and diabetes).27-28 As a result, the American Academy of Pediatrics29 and the U.S. Surgeon General30 have all established recommendations to increase breastfeeding initiation and duration. The current level of breastfeeding costs the U.S. an estimated excess of 13 billion dollars annually28 in preventable health care costs and death. This is particularly true in populations in which disparities in health care are most prevalent, including blacks, younger women, less educated, and lower income women.31-32 Such disparities may help to explain the increased risk of AD among some racial minorities, but conflicts with the increased rate of AD in high SES children.
Health care reform and the dermatology workforce
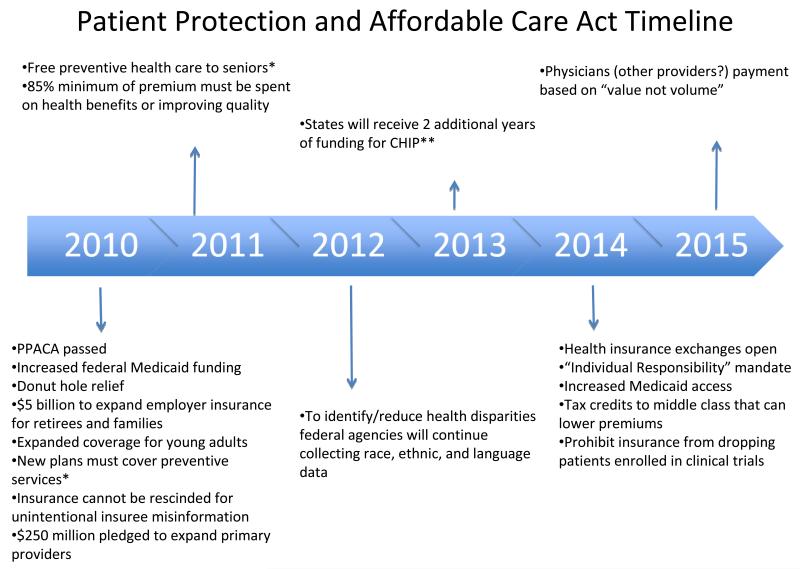
The Patient Protection and Affordability of Care Act and the Reconciliation Act was passed and signed into law in March 2010. (Figure 1) Despite the varied and polarized opinions on the legislation, it is clear that some of the measures would improve health disparities. Recent figures indicate that there are more than 50 million (16.7%) uninsured persons in the U.S. and this number has been increasing since 2000.33 Ten percent of those uninsured are children (7.5 million).33 Of insured, 30.6% are covered by government programs such as Medicare (43.4 million) and Medicaid (47.8 million).33 The U.S. economy loses $207 billion each year as a result of the poorer health and decreased lifespan of uninsured, and in 2008, $43 billion was spent on the uncompensated health care of the uninsured.34 A major goal of the health care reform act is to increase insurance coverage to nearly all Americans, thereby providing cost-sharing leading to lower overall premiums. By 2014, the individual mandate for health insurance purchase by most Americans will be enforced and at that time health insurance exchanges will open. It is estimated that the number of uninsured nonelderly people will decline to 21 million within 2 years of this mandate.35 The majority of the nonelderly persons remaining uninsured will be unauthorized immigrants (approximately 30%) and those eligible for, but not enrolled in Medicaid (approximately 25%).36 The specific effects of this legislation on dermatologic health disparities are not known. The dramatic increase in insured patients would likely lead to a shift in care of previously uninsured patients from emergency rooms and urgent care centers to primary and specialty care offices. To address the increased need, the legislation dedicated $250 million to expand the primary care workforce.37 This will help to some extent; however, some specialties--including dermatology—already have a shortage of providers. According to the 2009 American Academy of Dermatology (AAD) practice profile survey38, 38% of dermatologists report that there is a shortage of dermatologists in their community. This shortage was greatest in rural settings. Nearly one-third of survey respondents indicated that they were actively looking for another dermatologist to join their practice.38 The average wait time for new patients was 33.9 days and, for established patients was 17.9 days.38 These results are similar to the previous surveys done in 2007, 2005, and 2002. These shortages are despite the fact that a majority of dermatologists’ patient care time is dedicated to medical dermatology (67.1%) with only 25.1% on non-cosmetic surgical dermatology, and 7.8% on cosmetics.38 The anticipated increase in insured patients coupled with a lack of funding to expand the dermatology workforce may only worsen the current shortage. In order for dermatologists to provide a sufficient amount of dermatologic care, innovative methods to prevent excessive patient wait times and lack of access to dermatologic care are needed.
Figure 1.
Major provisions of the Patient Protection and Affordability Care Act. Data from timeline available at:www.healthcare.gov.37 Key: *This does not include skin cancer exams. **Child health insurance program
Dermatology education and health disparities
A variety of studies have found that U.S. medical students are exposed to very little dermatology in comparison to other clinical specialties. U.S. medical students receive an average of is between 16 and 22 hours of dermatologic training—less than 1% of their undergraduate medical education.39-41 Consequently, fewer than 40% of primary care residents feel that their medical school curriculum adequately prepared them to manage common skin conditions.42 Similarly, a recent survey of United Kingdom students found that the majority (55.7%) believed that their undergraduate medical education did not provide adequate education in dermatology.43
In a recent U.S. survey, 47% of dermatologists and dermatology residents reported that their medical training (medical school and/or residency) was inadequate in training them on skin conditions in blacks.44 Those who felt their training in this area was lacking identified the need for greater exposure to black patients and training materials.44 These findings highlight the need to expose dermatology residents to a diverse patient population as well as provide them with the didactics, textbooks and peer-reviewed literature necessary to prepare them to address special considerations in skin of color to prevent disparities in quality of care.
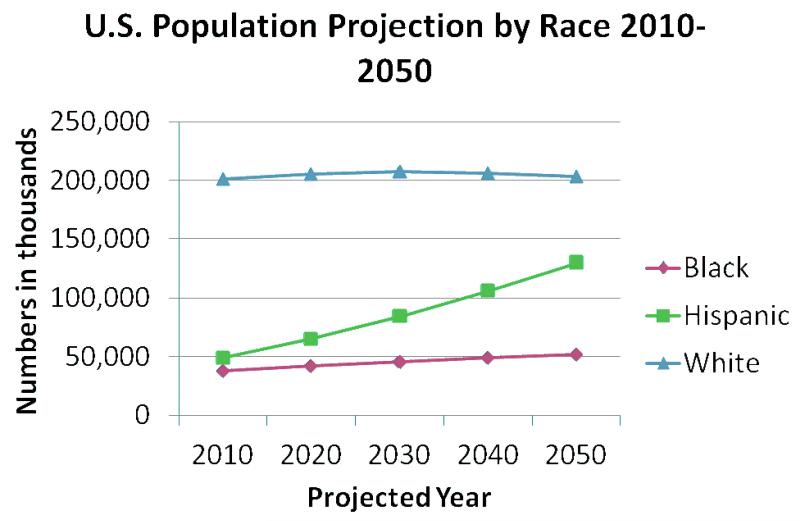
There is little research on the adequacy of current dermatologic training to produce dermatologists with cross cultural competence, confidence, and skill in treating patients from diverse backgrounds. A pubmed search of the terms dermatology, residency, and education reveals just 1 manuscript since 2000 that addresses residency training and ethnic skin. In that study45, 52.4% of chief residents and 65.9% of program directors surveyed reported that their residency provided lectures or didactics integrating ethnic skin into the curriculum. This and the knowledge of the growing ethnic minority proportion of the U.S. population (Figure 2) underscore the need for a vigorous assessment of medical education to ensure dermatologists are adequately prepared to provide quality care to patients of diverse racial and ethnic backgrounds.
Figure 2.
This displays the projections of the U.S. population by race with the resident population numbers represented in thousands. Thus the projected white population in 2050 is approximately 200 million citizens.59
Disparities in research
It is well known that racial and ethnic minorities have been historically underrepresented in medical research.46-48 This may be a reflection of study recruitment49, minorities’ disinterest or distrust48, 50, lack of access48, or other factors. Limited minority participation in research studies may affect the applicability of clinical trial results, potentially leading to detrimental patient outcomes. Given this research disparity, Congress enacted the National Institutes of Health (NIH) Revitalization Act of 1993, PL 103-4351, which mandated that both women and racial minorities be represented in clinical research. The NIH defines clinical research as:
(1) Patient-oriented research. Patient-oriented research includes: (a) mechanisms of human disease, (b) therapeutic interventions, (c) clinical trials, and (d) development of new technologies; (2) Epidemiologic and behavioral studies; and (3) Outcomes research and health services research.51
Consistent with this, a review of the literature reveals a steady increase in dermatologic clinical studies involving ethnic minorities. In contrast, there remains a scarcity of robust basic dermatologic research examining skin of color.3
There is little evidence on how health disparities affect dermatologic research. A systematic review of the literature failed to identify any research citing specific barriers to subject participation in dermatologic research.48 A study analyzing survey responses of black and white parents of pediatric dermatology patients and found that black parents had significantly less trust for the medical research community (p = 0.03), were three times more likely to believe their child would be treated like a guinea pig” if they participated in research (p = 0.03), and were significantly less likely to enroll their children in a clinical study in the setting of being cared for by an established provider (p = 0.0001).52 They also found that black parents had less exposure to research advertisements.52 Despite these findings, their study found that black parents were as likely as white parents to enroll their children in low-risk research studies. This is consistent with data on pediatric cancer clinical trials, in which minority children are proportionately represented.53 With such limited data, however, it is clear that additional studies are needed to determine what and how health disparities challenge dermatologic research so that barriers minority participation may be targeted and overcome.
Conclusion
As a dermatologic community, our work is cut out for us. Healthcare disparities in dermatology clearly exist, but need better definition in order to be properly addressed. There is inadequate epidemiologic data on dermatologic health disparities and the current data are effectively limited to the diagnoses of skin cancer and atopic dermatitis or eczema. Ample room exists to further explore the extent and nature of these and other inequities across a spectrum of dermatologic diseases. In addition, a variety of health disparities exist beyond those detailed in this manuscript, including those secondary to culture or language barriers, additional socioeconomic barriers (transportation, education and literacy), age, disability, differential treatment, and outcomes. Potential solutions that merit further exploration include patient navigators, patient centered medical homes, professional translators, child care, and literacy assistance, among others.54
Addressing the need for further health disparities research is an identified priority of National Institute of Arthritis and Musculoskeletal and Skin Disease3, but this has not yet been fully recognized by the dermatologic research community. Increasingly, U.S. institutions are establishing minority health research centers with goals focused on reducing health disparities. These range from enhancing minority health research infrastructure and training skilled minority health researchers to providing patient and community-focused programs to directly eliminate inequities.55-56 Such efforts present an opportunity for dermatologic researchers and providers to fill in the major gaps in current knowledge and literature by establishing health disparity focused careers within supportive academic environments.
Increased research as well as collaboration between dermatologic organizations that aim to eliminate healthcare disparities will help dermatologists to develop united and clear set goals. Recently the AAD created the Access to Dermatologic Care Task Force (ATDCTF) with the goal “to raise awareness among dermatologists of health disparities affecting populations identified by but not exclusive to race/ethnicity, socioeconomic status, geography, gender, age, and disability status and to develop policies that increase access for these groups to dermatologic services.”57 The ATDCTF also serves as the link between the AAD and other physician organizations focused on reducing healthcare inequities, such as the American Medical Association (AMA). The AMA Commission to End Health Disparities focuses on collaboration to “increase awareness among physicians and health professionals; use evidence-based and other strategies; and advocate for action, including governmental, to eliminate disparities in health care and strengthen the health care system.”58 Through increased research, awareness, education, outreach, and public policy, dermatologic and general health disparities can be decreased resulting in improved health for all Americans.
Acknowledgments
Funding: Dr. Buster was supported by an NIH T32 grant.
Abbreviations and Acronyms
- (AHRQ)
Agency for Healthcare Research and Quality
- (SES)
socioeconomic status
- (NMSC)
Nonmelanoma skin cancer
- (AD)
atopic dermatitis
- (AAD)
American Academy of Dermatology
- (NIH)
National Institutes of Health
- (ATDCTF)
Access to Dermatologic Care Task Force
- (AMA)
American Medical Associationx
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosures: The authors have nothing to disclose.
References
- 1.Carter-Pokras O, Baquet C. What is a “health disparity”? Public Health Rep. 2002 Sep-Oct;117(5):426–434. doi: 10.1093/phr/117.5.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agency for Healthcare Research and Quality [Accessed May 1, 2011];National Healthcare Disparities Report. 2010 http://www.ahrq.gov/qual/nhdr10/nhdr10.pdf.
- 3.Taylor SC, Kelly AP, Dupree NE, Kimball AB, Lawrence RC. Health disparities in arthritis and musculoskeletal and skin diseases-the dermatology session: National Institute of Arthritis and Musculoskeletal and Skin Diseases, Bethesda, Maryland, December 15-16, 2000. J Am Acad Dermatol. 2002 Nov;47(5):770–773. doi: 10.1067/mjd.2002.124691. [DOI] [PubMed] [Google Scholar]
- 4.McMichael AJ, Jackson S. Issues in dermatologic health care delivery in minority populations. Dermatol Clin. 2000 Apr;18(2):229–233. viii. doi: 10.1016/s0733-8635(05)70168-6. [DOI] [PubMed] [Google Scholar]
- 5.Bigby M. Epidemiology of cutaneous disease. In: Kelly AP, Taylor SC, editors. Dermatology for skin of color. McGraw Hill Medical; New York: 2009. [Google Scholar]
- 6.Rapp SR, Feldman SR, Graham G, Fleischer AB, Brenes G, Dailey M. The Acne Quality of Life Index (Acne-QOLI): development and validation of a brief instrument. Am J Clin Dermatol. 2006;7(3):185–192. doi: 10.2165/00128071-200607030-00005. [DOI] [PubMed] [Google Scholar]
- 7.Stern RS. Dermatologists and office-based care of dermatologic disease in the 21st century. J Investig Dermatol Symp Proc. 2004 Mar;9(2):126–130. doi: 10.1046/j.1087-0024.2003.09108.x. [DOI] [PubMed] [Google Scholar]
- 8.Wingo PA, Bolden S, Tong T, Parker SL, Martin LM, Heath CW., Jr. Cancer statistics for African Americans, 1996. CA Cancer J Clin. 1996 Mar-Apr;46(2):113–125. doi: 10.3322/canjclin.46.2.113. [DOI] [PubMed] [Google Scholar]
- 9.Gloster HM, Jr., Neal K. Skin cancer in skin of color. J Am Acad Dermatol. 2006 Nov;55(5):741–760. doi: 10.1016/j.jaad.2005.08.063. quiz 761-744. [DOI] [PubMed] [Google Scholar]
- 10.Weinstock MA. Nonmelanoma skin cancer mortality in the United States, 1969 through 1988. Arch Dermatol. 1993 Oct;129(10):1286–1290. [PubMed] [Google Scholar]
- 11.Geller AC, Miller DR, Lew RA, Clapp RW, Wenneker MB, Koh HK. Cutaneous melanoma mortality among the socioeconomically disadvantaged in Massachusetts. Am J Public Health. 1996 Apr;86(4):538–543. doi: 10.2105/ajph.86.4.538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reyes-Ortiz CA, Goodwin JS, Freeman JL, Kuo YF. Socioeconomic status and survival in older patients with melanoma. J Am Geriatr Soc. 2006 Nov;54(11):1758–1764. doi: 10.1111/j.1532-5415.2006.00943.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Linos E, Swetter SM, Cockburn MG, Colditz GA, Clarke CA. Increasing burden of melanoma in the United States. J Invest Dermatol. 2009 Jul;129(7):1666–1674. doi: 10.1038/jid.2008.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roetzheim RG, Pal N, Tennant C, et al. Effects of health insurance and race on early detection of cancer. J Natl Cancer Inst. 1999 Aug 18;91(16):1409–1415. doi: 10.1093/jnci/91.16.1409. [DOI] [PubMed] [Google Scholar]
- 15.Byrd KM, Wilson DC, Hoyler SS, Peck GL. Advanced presentation of melanoma in African Americans. J Am Acad Dermatol. 2004 Jan;50(1):21–24. doi: 10.1016/s0190-9622(03)02091-7. discussion 142-143. [DOI] [PubMed] [Google Scholar]
- 16.Altekruse SFKC, Krapcho M, Neyman N, Aminou R, Waldron W, Ruhl J, Howlader N, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Cronin K, Chen HS, Feuer EJ, Stinchcomb DG, Edwards BK, (U.S.). NCI, editors. SEER Cancer Statistics Review, 1975-2007. Bethesda, MD: 2010. [Google Scholar]
- 17.Scotto J, Fears TR, Fraumeni JF. Incidence of non-melanoma skin cancer in the United States. U.S. Dept. of Health and Human Services, National Institutes of Health; Bethesda, MD: 1983. NIH Pub. no. 83-2433. [Google Scholar]
- 18.Coups EJ, Geller AC, Weinstock MA, Heckman CJ, Manne SL. Prevalence and correlates of skin cancer screening among middle-aged and older white adults in the United States. Am J Med. 2010 May;123(5):439–445. doi: 10.1016/j.amjmed.2009.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buster KJ, You Z, Fouad M, Elmets CA. [Accepted May 10, 2011];Skin cancer risk perceptions: A comparison across ethnicity, age, education, gender, and income. J Am Acad Dermatol. doi: 10.1016/j.jaad.2011.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bilimoria KY, Balch CM, Wayne JD, et al. Health care system and socioeconomic factors associated with variance in use of sentinel lymph node biopsy for melanoma in the United States. J Clin Oncol. 2009 Apr 10;27(11):1857–1863. doi: 10.1200/JCO.2008.18.7567. [DOI] [PubMed] [Google Scholar]
- 21.Shaw TE, Currie GP, Koudelka CW, Simpson EL. Eczema prevalence in the United States: data from the 2003 National Survey of Children’s Health. J Invest Dermatol. 2011 Jan;131(1):67–73. doi: 10.1038/jid.2010.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Asher MI, Montefort S, Bjorksten B, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006 Aug 26;368(9537):733–743. doi: 10.1016/S0140-6736(06)69283-0. [DOI] [PubMed] [Google Scholar]
- 23.The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet. 1998 Apr 25;351(9111):1225–1232. [PubMed] [Google Scholar]
- 24.Laughter D, Istvan JA, Tofte SJ, Hanifin JM. The prevalence of atopic dermatitis in Oregon schoolchildren. J Am Acad Dermatol. 2000 Oct;43(4):649–655. doi: 10.1067/mjd.2000.107773. [DOI] [PubMed] [Google Scholar]
- 25.Horii KA, Simon SD, Liu DY, Sharma V. Atopic dermatitis in children in the United States, 1997-2004: visit trends, patient and provider characteristics, and prescribing patterns. Pediatrics. 2007 Sep;120(3):e527–534. doi: 10.1542/peds.2007-0289. [DOI] [PubMed] [Google Scholar]
- 26.Janumpally SR, Feldman SR, Gupta AK, Fleischer AB., Jr. In the United States, blacks and Asian/Pacific Islanders are more likely than whites to seek medical care for atopic dermatitis. Arch Dermatol. 2002 May;138(5):634–637. doi: 10.1001/archderm.138.5.634. [DOI] [PubMed] [Google Scholar]
- 27.Ip S, Chung M, Raman G, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep) 2007 Apr;(153):1–186. [PMC free article] [PubMed] [Google Scholar]
- 28.Bartick M, Reinhold A. The burden of suboptimal breastfeeding in the United States: a pediatric cost analysis. Pediatrics. 2010 May;125(5):e1048–1056. doi: 10.1542/peds.2009-1616. [DOI] [PubMed] [Google Scholar]
- 29.Gartner LM, Morton J, Lawrence RA, et al. Breastfeeding and the use of human milk. Pediatrics. 2005 Feb;115(2):496–506. doi: 10.1542/peds.2004-2491. [DOI] [PubMed] [Google Scholar]
- 30.Office of the Surgeon General [Accessed May 15, 2011];The Surgeon General’s Call to Action to Support Breastfeeding 2011. http://www.surgeongeneral.gov/topics/breastfeeding/factsheet.html. [PubMed]
- 31.Nommsen-Rivers LA, Chantry CJ, Cohen RJ, Dewey KG. Comfort with the idea of formula feeding helps explain ethnic disparity in breastfeeding intentions among expectant first-time mothers. Breastfeed Med. 2010 Feb;5(1):25–33. doi: 10.1089/bfm.2009.0052. [DOI] [PubMed] [Google Scholar]
- 32.Ahluwalia IB, Morrow B, Hsia J, Grummer-Strawn LM. Who is breast-feeding? Recent trends from the pregnancy risk assessment and monitoring system. J Pediatr. 2003 May;142(5):486–491. doi: 10.1067/mpd.2003.199. [DOI] [PubMed] [Google Scholar]
- 33.DeNavas-Walt CPB, Smith JC. In: Income, poverty, and health insurance coverage in the United States: 2009. Bureau USC, editor. U.S. Government Printing Office; Washington, DC: 2010. pp. 22–24. [Google Scholar]
- 34.Office of the Legislative Counsel. http://docs.house.gov/energycommerce/ppacacon.pdf [Accessed May 2, 2011];Compilation of patient protection and affordable care act. http://docs.house.gov/energycommerce/ppacacon.pdf
- 35.Congressional Budget Office [Accessed May 2, 2011];Estimate of the Effects of the Insurance Coverage Provisions Contained in the Patient Protection and Affordable Care Act (Public Law 111-148) and the Health Care and Education Reconciliation Act of 2010 (P.L. 111-152) 2011 Mar; http://www.cbo.gov/budget/factsheets/2011b/HealthInsuranceProvisions.pdf.
- 36.Elmendorf D. [Accessed May 2, 2011];CBO’s analysis of the major health care legislation enacted in March 2010. 2011 Mar 30; http://www.cbo.gov/ftpdocs/121xx/doc12119/03-30-HealthCareLegislation.pdf.
- 37. Healthcare.gov [Accessed April 12, 2011];Understand the law. Healthcare.gov http://www.healthcare.gov.
- 38.Kostecki J. Dermatology practice profile survey 2009 report. American Academy of Dermatology Association; 2009. Database provided to authors. [Google Scholar]
- 39.McCleskey PE, Gilson RT, DeVillez RL. Medical Student Core Curriculum in Dermatology Survey. J Am Acad Dermatol. 2009 Jul;61(1):30–35. e34. doi: 10.1016/j.jaad.2008.10.066. [DOI] [PubMed] [Google Scholar]
- 40.Knable A, Hood AF, Pearson TG. Undergraduate medical education in dermatology: report from the AAD Interdisciplinary Education Committee, Subcommittee on Undergraduate Medical Education. J Am Acad Dermatol. 1997 Mar;36(3 Pt 1):467–470. doi: 10.1016/s0190-9622(97)80227-7. [DOI] [PubMed] [Google Scholar]
- 41.Ramsay DL, Mayer F. National survey of undergraduate dermatologic medical education. Arch Dermatol. 1985 Dec;121(12):1529–1530. [PubMed] [Google Scholar]
- 42.Hansra NK, O’Sullivan P, Chen CL, Berger TG. Medical school dermatology curriculum: are we adequately preparing primary care physicians? J Am Acad Dermatol. 2009 Jul;61(1):23–29. e21. doi: 10.1016/j.jaad.2008.11.912. [DOI] [PubMed] [Google Scholar]
- 43.Chiang YZ, Tan KT, Chiang YN, Burge SM, Griffiths CE, Verbov JL. Evaluation of educational methods in dermatology and confidence levels: a national survey of UK medical students. Int J Dermatol. 2011 Feb;50(2):198–202. doi: 10.1111/j.1365-4632.2010.04664.x. [DOI] [PubMed] [Google Scholar]
- 44.Buster KJ, Yang L, Elmets CA. Are dermatologists confident in treating skin disease in African-Americans?; J Invest Dermatol Meeting Abstracts; 2011; abstract 235. [Google Scholar]
- 45.Nijhawan RI, Jacob SE, Woolery-Lloyd H. Skin of color education in dermatology residency programs: does residency training reflect the changing demographics of the United States? J Am Acad Dermatol. 2008 Oct;59(4):615–618. doi: 10.1016/j.jaad.2008.06.024. [DOI] [PubMed] [Google Scholar]
- 46.Adams-Campbell LL, Ahaghotu C, Gaskins M, et al. Enrollment of African Americans onto clinical treatment trials: study design barriers. J Clin Oncol. 2004 Feb 15;22(4):730–734. doi: 10.1200/JCO.2004.03.160. [DOI] [PubMed] [Google Scholar]
- 47.Advani AS, Atkeson B, Brown CL, et al. Barriers to the participation of African-American patients with cancer in clinical trials: a pilot study. Cancer. 2003 Mar 15;97(6):1499–1506. doi: 10.1002/cncr.11213. [DOI] [PubMed] [Google Scholar]
- 48.Spears CR, Nolan BV, O’Neill JL, Arcury TA, Grzywacz JG, Feldman SR. Recruiting underserved populations to dermatologic research: a systematic review. Int J Dermatol. 2011 Apr;50(4):385–395. doi: 10.1111/j.1365-4632.2010.04813.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Roberson NL. Clinical trial participation. Viewpoints from racial/ethnic groups. Cancer. 1994 Nov;74(9 Suppl):2687–91. doi: 10.1002/1097-0142(19941101)74:9+<2687::aid-cncr2820741817>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 50.Corbie-Smith G, Thomas SB, Williams MV, Moody-Ayers S. Attitudes and beliefs of African Americans toward participation in medical research. J Gen Intern Med. 1999 Sep;14(9):537–546. doi: 10.1046/j.1525-1497.1999.07048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.U.S. Department of Health and Human Services [Accessed May 10, 2011];NIH Policy and Guidelines on The Inclusion of Women and Minorities as Subjects in Clinical Research. http://grants.nih.gov/grants/funding/women_min/guidelines_amended_10_2001.htm.
- 52.Shaw MG, Morrell DS, Corbie-Smith GM, Goldsmith LA. Perceptions of pediatric clinical research among African American and Caucasian parents. J Natl Med Assoc. 2009 Sep;101(9):900–907. doi: 10.1016/s0027-9684(15)31037-3. [DOI] [PubMed] [Google Scholar]
- 53.Bleyer WA, Tejeda HA, Murphy SB, Brawley OW, Smith MA, Ungerleider RS. Equal participation of minority patients in U.S. national pediatric cancer clinical trials. J Pediatr Hematol Oncol. 1997 Sep-Oct;19(5):423–427. doi: 10.1097/00043426-199709000-00003. [DOI] [PubMed] [Google Scholar]
- 54.Sauaia A, Dellavalle RP. Health care inequities: an introduction for dermatology providers. Dermatol Clin. 2009 Apr;27(2):103–107. v. doi: 10.1016/j.det.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.University of Alabama at Birmingham Minority Health and Health Disparities Research Center [Accessed on May 1, 2011]; http://mhrc.dopm.uab.edu/
- 56.Temple University School of Medicine Center for Minority Health and Health Disparities [Accessed on May 14, 2011]; http://www.temple.edu/medicine/departments_centers/research/minority_health.htm.
- 57.American Academy of Dermatology Access to Dermatologic Care Task Force [Accesed May 14, 2011]; http://www.aad.org/forms/cctf/default.aspx.
- 58.American Medical Association Commission ot End Health Care Disparities [Accessed May 14, 2011]; http://www.ama-assn.org/ama/pub/physician-resources/public-health/eliminating-health-disparities/commission-end-health-care-disparities.page.
- 59.U.S. Census Bureau [Accessed April 21, 2011];U.S. Population Projections. http://www.census.gov/population/www/projections/downloadablefiles.html.