Abstract
Oxidation of low-density lipoprotein (LDL) has a key role in atherogenesis. Among the different models of oxidation that have been studied, the one using myeloperoxidase (MPO) is thought to be more physiopathologically relevant. Apolipoprotein B-100 is the unique protein of LDL and is the major target of MPO. Furthermore, MPO rapidly adsorbs at the surface of LDL, promoting oxidation of amino acid residues and formation of oxidized lipoproteins that are commonly named Mox-LDL. The latter is not recognized by the LDL receptor and is accumulated by macrophages. In the context of atherogenesis, Mox-LDL accumulates in macrophages leading to foam cell formation. Furthermore, Mox-LDL seems to have specific effects and triggers inflammation. Indeed, those oxidized lipoproteins activate endothelial cells and monocytes/macrophages and induce proinflammatory molecules such as TNFα and IL-8. Mox-LDL may also inhibit fibrinolysis mediated via endothelial cells and consecutively increase the risk of thrombus formation. Finally, Mox-LDL has been involved in the physiopathology of several diseases linked to atherosclerosis such as kidney failure and consequent hemodialysis therapy, erectile dysfunction, and sleep restriction. All these issues show that the investigations of MPO-dependent LDL oxidation are of importance to better understand the inflammatory context of atherosclerosis.
1. Introduction
Atherosclerosis is an inflammatory process involving vascular cells, monocytes, T lymphocytes, proinflammatory cytokines, chemoattractant cytokines (chemokines), and growth factors [1–3]. Specific arterial regions are favorable to atherosclerosis development [4], and these areas have been linked to shear stress abnormalities [5]. More recently, it was shown in apoE−/− mice that smooth muscle cells display a different transcriptome at locations where atherogenesis is prone even before the development of the lesion [6]. The accumulation of foam cells in intima leads to primary lesions characterized by fatty streaks in the artery wall and by thickening of the wall. Early lesions are found in the aorta of healthy 10-year-old children, in coronary arteries of 20-year-old adults, and later in cerebral arteries [7]. These lesions can naturally disappear without causing any disorder to the patient or progress of advanced lesions with smooth muscle cell migration and proliferation, foam cell accumulation, and can even lead to plaque rupture and thrombus formation.
Among the factors associated with this process, modification and particularly oxidation of low-density lipoproteins (LDLs) have been of major interest since Steinberg et al. showed that native LDL does not accumulate in macrophages, whereas modified lipoprotein does [8, 9]. However, the exact mechanisms of LDL oxidation are still not completely understood, and researchers continue to argue about them [10]. Several mechanisms have been described including reactive oxygen species (ROS) produced by endothelial cells and monocytes/macrophages [11], metal ions [12], lipoxygenase [13], or myeloperoxidase [14, 15]. Each oxidative mechanism of lipoprotein is characterized by targeting either lipid, protein, or both moieties [8].
Highly oxidized LDL (ox-LDL) cannot bind to the LDL receptor and is taken up by monocytes which transform into macrophages. Indeed, these cells express scavenger receptors such as (SR) such as CD36, SR-A, SR-B1, and LOX-1 at their surface, which bind ox-LDL and enable scavenger receptor-mediated endocytosis [16]. This reaction is the best way for removing excess of ox-LDL in the arterial wall. Conversely, this process could worsen, and ox-LDL continues to accumulate in the subendothelial space. Macrophages continue to engulf the modified lipoproteins and evolve to a state where high quantities of lipids are intracellularly accumulated leading to foam cell formation [17]. Resistance of ox-LDL to acidic lysosomal proteolysis via cathepsins has also been observed [18]. The latter phenomenon increases the risk of LDL accumulation in macrophages and therefore foam cell formation. Foam cells themselves have a proinflammatory effect by producing cytokines and growth factors such as interleukins (IL) 1β and -8, interferon-γ, tumor-necrosis factor-α (TNFα), and macrophage colony stimulating factor (M-CSF).
Ox-LDL is widely described as a key component of atherogenesis and triggers the inflammatory processes of the disease. Ox-LDL induces a number of potentially proatherogenic activities such as the production of proinflammatory cytokines and chemokines by monocytes, endothelial cells, and smooth muscle cells in vitro [19, 20]. In this paper, we focused on a particular and frequent LDL oxidation mechanism involving myeloperoxidase (MPO). MPO is an important enzyme of neutrophils which combat pathogen invasion in the body. Indeed, MPO catalyzes the production of oxidative reagents which damage pathogens and aid in their elimination. Unfortunately, in chronic inflammation syndromes, MPO is also released into the extracellular space due to neutrophil activation where MPO-derived oxidants can in turn cause tissue damage. One of the targeted components is LDL, leading to MPO-dependent oxidized LDL, commonly named Mox-LDL.
In this paper, we first review LDL, apolipoprotein B-100, the unique protein of LDL, and its oxidation sensitive components. MPO and its enzymatic mechanism are then briefly described. Following this, modifications of LDL are discussed with particular focus on MPO-dependent oxidation mechanisms and the specificity of MPO to modify LDL. In vitro experiments on inflammation involving Mox-LDL are then addressed. In this section, we will show that Mox-LDL has a key role in triggering the inflammatory response during atherogenesis and has effects on monocytes, macrophages, and endothelial cells and that those effects are different than LDL modified by other systems. Finally, clinical aspects of Mox-LDL are illustrated, focusing on several conditions such as atherosclerosis, erectile dysfunction, dialysis, nonalcoholic fatty liver disease, and sleep disorders.
2. Low-Density Lipoprotein and Apolipoprotein B-100
LDL is one of the major carriers of cholesterol in the human body and plays a role in cholesterol metabolism, as well as other lipoproteins such as high-density, intermediate-density, or very-low-density lipoproteins. LDL is generally considered to be a spherical particle of about 22 nm in diameter [21]. It includes two major groups of compounds: (i) lipids and (ii) protein representing 80% and 20% of total lipoprotein weight, respectively.
The lipid moiety contains approximately 3000 molecules including cholesterol esters mainly but also free cholesterol, phospholipids, and triglycerides. In LDL, lipids are separated into two parts: (i) a monolayer of phospholipids and free cholesterol at the surface and (ii) a core majorly composed of cholesterol esters but also free cholesterol and triglycerides.
The protein moiety of LDL includes a unique protein which is an exception among lipoproteins. This protein is apolipoprotein B-100 (apoB-100) and was completely sequenced for the first time in 1986 by several labs thanks to genetic investigations [22–25]. Mature apoB-100 consists of 4536 amino acid residues with 19 putative N-glycosylation sites making it one of the largest monomeric proteins in the human body with a molecular mass estimated to be 550 kDa. ApoB-100 is usually divided into 5 domains as first described by Yang et al. in 1989 [26] and later summarized by Segrest et al. [27]. This division of apoB-100 follows α- and β-domain characteristics. The consensus structure is as follows: NH2-βα1-β1-α2-β2-α3-COOH. ApoB-100 is distributed both at the surface and in the core of the lipoprotein where the NH2-βα1 domain (the first 1000 residues) is generally described as being a highly hydrophilic domain located outside the particle. Although the latter domain is hydrophilic, apoB-100 has several hydrophobic segments which enable strong interactions with lipids (core and surface lipids) and stabilize the lipoprotein structure.
ApoB-100 is also a key player in LDL recognition and binding to the LDL receptor, which is present at the surface of most human cells. When LDL binds to the receptor, uptake occurs followed by degradation of the lipoprotein and release of cholesterol for the cell's needs. Modifications to the apoB-100 structure can lead to decrease in affinity or even the inability of LDL to bind the receptor [28, 29]. More than 50 variants are currently described in UniProt Database, many with no effect on LDL function although others have harmful properties resulting in hypercholesterolemia and its deleterious effects. It is also assumed that a receptor-binding site is present at the surface of apoB-100. Many studies have tried to determine the exact binding site, but it is still controversial [22, 30–33]. The sequence between residues 3345 and 3381 would include the receptor-binding site and sometimes the 3359–3369 segment is mentioned [28], but it should be kept in mind that mutations on apoB-100 close to this binding site also disrupt the ability of LDL to bind to LDL receptor (e.g., R3500Q mutation which is the major cause of familial defective apoB-100 disease). Finally, oxidized apoB-100 also has a decreased affinity for the LDL receptor.
The characteristics of apoB-100 make its analysis a very complex and difficult task. Since its sequencing in 1986, apoB-100 has been the subject of several studies to elucidate its exact structure [27, 34–37]. In 1989, Yang et al. used a specific methodology to distinguish segments of the protein which are hydrophobic from those which are hydrophilic [38]. This approach is useful for prediction and supposition of segments which could be more sensitive to post-translational modifications (PTMs).
The best experimental procedures to study the modifications that occur to apoB-100 are those that utilize mass spectrometers (MS/MS or MSn) [39]. Indeed, many of these instruments have a high-resolution mass analyzer coupled to the ability to fragment the peptides in order to sequence them. Such instruments include quadrupole-time of flight (QToF) mass spectrometers which can detect peptide and PTMs with high accuracy which can be coupled to separation techniques such as liquid chromatography. This represents a powerful strategy to discover PTMs on proteins.
Another strategy has been recently described to analyze modifications of apoB-100 taking advantage of known modifications and their specific product ions to monitor PTMs by LC-MS/MS [40]. However, the huge sequence of apoB-100 also makes it important to optimize all parameters of the analysis. For this purpose, we developed and optimized an LC-MS/MS method capable of recovering up to 80% of apoB-100, and we have shown that this is required to detect the maximum of PTMs currently achievable (4 times more modifications were recovered thanks to the optimized protocol) [41].
In summary, LDL and apoB-100 investigations are important to understand their implications in the processes of disease. However, LDL/apoB-100 complexity make these studies particularly difficult, but recent improvements in instrumentation, such as those for mass spectrometry, are very helpful. In the following paragraphs, we principally discuss MPO-dependent oxidation of LDL and its roles in inflammation in vitro as well as in vivo.
3. Myeloperoxidase and MPO/H2O2/Halide System
MPO is a key enzyme in innate immunity and defense against pathogens [42]. Hereinafter, we will describe the major points of interest of MPO devoted to LDL oxidation and inflammation. For reviews on molecular mechanisms as well as physiological and physiopathological aspects of MPO, see Klebanoff [43], Davies [44], Davies et al. [45], and van der Veen et al. [46]. MPO expression is limited to myeloid cells, and its synthesis in neutrophils starts at the promyelocyte stage and terminates at the beginning of the myelocyte stage. Mature MPO is packed in azurophilic granules of neutrophils and accounts for 5% of the total dry cell weight, making MPO the major protein of neutrophils. It is also present in monocytes but to a lesser extent [47, 48].
MPO is a hemeglycoprotein with a mass of 140–155 kDa [49]. Its biosynthesis is a complex process including proteolytic events, heme and glycan additions, and a final dimerization step [50, 51]. Briefly, nascent MPO, called preproMPO, undergoes a first proteolytic event and N-glycan addition to make apoproMPO in the endoplasmic reticulum. The latter lacks the hememoiety which is then inserted due to the activity of chaperones (calreticulin and calnexin) which interact with MPO oligosaccharides. This forms proMPO which leaves the endoplasmic reticulum and travels to the Golgi apparatus and granules where MPO undergoes several new proteolytic events. The final monomer of MPO consists of a light chain of 106 residues and a heavy chain of 467 residues. The two chains are linked by a disulfide bond and also via the heme group. In the mature form, MPO is a dimer of two monomers linked by a disulfide bond on position cysteine 369 of each heavy chain. Each monomer is enzymatically active and can produce oxidants. MPO also contains a calcium binding site contributing to the stabilization of the structure. N-glycans play a key role in protein synthesis and also in enzymatic activity as recently shown by our experiments [52]. Furthermore, MPO is a highly cationic protein with a pI ≈ 11 enabling its binding to electronegative surfaces such as endothelial wall, lipoprotein, or proteoglycans [53, 54].
In the azurophilic granules, MPO is kept in an inactive state as long as the neutrophil is not activated and hydrogen peroxide (H2O2) is absent [43]. After phagocytosis, activation of neutrophils leads to the release of the contents of the azurophilic granules (including MPO) into phagosomes and to the assembly of the NADPH oxidase enzyme complex (NOX2) that produces superoxide radicals (O2 •−). This radical is highly reactive and unstable and is rapidly converted into H2O2 spontaneously or by the action of superoxide dismutase. H2O2, which has a lower oxidation potential, can reach the ingested pathogen and contributes to its destruction by oxidizing vital molecules [55]. However, the reactivity of H2O2 alone does not produce optimal antimicrobial efficacy.
Using H2O2 and chloride ion (Cl−), MPO produces a more powerful oxidant molecule, namely, hypochlorous acid (HOCl). MPO can also use other (pseudo-) halide anions including Br−, I−, and SCN− to give the corresponding hypo- (pseudo-) halogenous oxidants (Figure 1). The first reaction of MPO is its oxidation by H2O2 to give Compound I. In the halogenation cycle, MPO is then reduced back to its native form in a two-electron reaction. The latter enables the generation of hypo- (pseudo-) halogenous acid. Although Cl− has the lowest reactivity to MPO among (pseudo-) halide anions [56], it is considered to be the major physiological substrate of MPO due to its high in vivo concentration [57–60]. HOCl is a strong oxidant, and it is thought to be more efficient than H2O2 in killing pathogens [61]. HOCl effectively attacks biomolecules of the ingested pathogen resulting in the death of pathogen in the phagosome.
Figure 1.
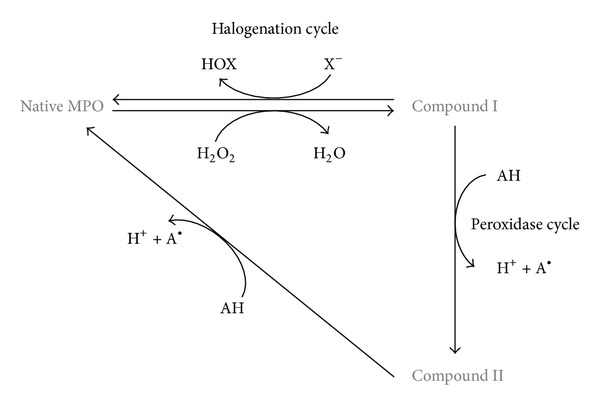
Scheme of the interconversion between different oxidized states of myeloperoxidase. The first reaction is the oxidation of native MPO to Compound I by a two-electron reaction. In the halogenation cycle, Compound I is backconverted to native MPO, and a two-electron oxidation of (pseudo-) halide generates hypo- (pseudo-) halogenous acid. In the peroxidase cycle, Compound I can oxidize an electron donor via 1-electron process transforming Compound I to Compound II and the electron donor to a radical product. Compound II can be reduced to native MPO by using 1 electron from other electron donors.
It is worth noting that MPO also has a peroxidase cycle in which electron donors can be oxidized and native MPO is regenerated in a two-step reaction (via the formation of Compound II: see Figure 1).
Due to its powerful oxidation products, MPO would be required to give the neutrophil optimum antimicrobial activity. Although neutrophils retain normal phagocytosis activity when MPO is inhibited or deficient, they cannot kill all types of ingested pathogens [62].
Despite its key role in host defense, MPO has also been involved in pathologic states. Indeed, during chronic inflammation or acute oxidative stress, MPO is released into the extracellular space where oxidants can be produced and host tissues damaged. Among biomolecular targets of MPO, LDL has been pointed out, and MPO is considered to be a major contributor of ox-LDL generation in vivo [8]. Moreover, clinical studies have highlighted serum MPO levels as a prognosis factor in patients with acute coronary syndromes or chest pain. These data support the necessity to understand the in vivo impact of Mox-LDL [63, 64], resulting from the reaction of MPO in the presence of LDL.
4. Modification of LDL, Myeloperoxidase, and Mox-LDL
4.1. Introduction
One of the primary steps of atherogenesis is the activation of the immune and vasculature systems leading to endothelial dysfunction and infiltration of immune cells and LDL into the vascular wall. This also leads to an oxidative burst and production of reactive oxygen species (ROS). The latter play a key role in the disease by inducing LDL modification (oxidation) resulting in the accumulation of lipids in macrophages, and the formation of foam cells and atherosclerotic plaques. LDL can be subjected to a variety of PTMs [40] among which oxidation [12, 14, 65], glycation [66, 67], and glycosylation [68, 69] are described. The oxidation mechanism is described from here on, focusing on MPO-dependent oxidation.
4.2. Oxidation of LDL
Increased plasma cholesterol level is a well-documented proatherogenic factor, and hypocholesterolemic therapy is the only approved pharmacological treatment. However, around 50% of patients experiencing a cardiovascular event have a normal level of cholesterol. This fact leads researchers and physicians to consider that the quality of lipoproteins might be more important than the quantity. In this context, it is largely admitted that the modifications of lipoproteins, particularly LDL and HDL, are of major importance in the development of atherosclerosis. This was first highlighted by Steinberg et al. who observed that native LDL is not extensively taken up by macrophages and does not lead to foam cell formation even though modified lipoproteins accumulate in these cells [9, 16]. Among the modifications, oxidation of LDL has certainly been the most studied for the last number of decades, and many studies have described the presence of ox-LDL in atheromatous lesions [14, 70–72].
Several mechanisms of oxidation exist involving metal cations as well as many different enzyme systems such as lipoxygenase, myeloperoxidase, xanthine oxidase, and NADPH oxidase. See Yoshida and Kisugi 2010 [10] for a review on major mechanisms of LDL oxidation. Numerous oxidants preferentially target the lipid moiety (i.e., Cu2+, lipoxygenases, and RNS; [72–74]), whereas others target the protein moiety of lipoproteins (HOCl and MPO; [59, 75]). From here on, we summarize some of the mechanisms involved in LDL oxidation, starting with an introduction to metal cation- and lipoxygenase-dependent LDL oxidation, followed by a complete description of the MPO-dependent process.
4.2.1. Oxidation of LDL by Metal Cations and Lipoxygenases
The exact process of oxidation of LDL in vivo is controversial. Since the discovery of the impact of LDL oxidation in atherosclerosis, metal ion-dependent oxidation of LDL has been extensively used for in vitro experiments. Iron (Fe3+) and copper (Cu2+) are the two major metal ions described to catalyze LDL oxidation. Copper had sometimes been preferred due to its ability to bind to apoB-100 and form a complex with it [12]. However, copper cations seem to target the lipid moiety of LDL and not apoB-100 [76]. Recently, Kriško et al. studied the impact of Cu2+ on the apoB-100 structure and observed conformational modifications early in the oxidation process, principally in β-sheet regions [77]. Metal ion-dependent oxidation mechanisms assume a high concentration of cations at the site of oxidation, a subject which is controversial [10]. Nevertheless, Stadler et al. quantified both copper- and iron-free cations using a technique that did not release transition metals from proteins during the reaction mechanism [78]. Furthermore, in this study, the authors showed an increase in both copper and iron levels in the intima of lesions compared with healthy controls. In addition, they correlated the iron levels, but not copper levels, with cholesterol levels. Whereas these cations are present, their implication in atherosclerosis remains a point of contention. Indeed, studies have sometimes positively correlated metal ion levels with cardiovascular risk, whereas others have negatively correlated them [79]. Nevertheless, epidemiological studies as well as in vitro experiments with iron agree on its potential impact on atherogenesis, whereas copper might be ambiguous [80–82].
Lipoxygenase-dependent LDL oxidation is also a contentious hypothesis because they are intracellular enzymes. However, 15-lipoxygenase mRNA and protein, as well as epitopes of ox-LDL, have been colocalized in human lesions [83, 84]. Lipoxygenase could migrate from the cytoplasm to the membrane surface of macrophages where LDL could be oxidized without phagocytosis/endocytosis of the lipoprotein. Lipoxygenases would be able to promote lipid peroxidation either directly by action on LDL lipids or indirectly by triggering ROS formation and subsequent LDL oxidation [10].
Several groups, like ours, have thus focused their research on the MPO-dependent mechanism of LDL oxidation which might be more physiologically relevant than the copper-dependent oxidation of LDL.
4.2.2. Oxidation of LDL by Myeloperoxidase
Background. The first evidence of MPO implication in atherogenesis was highlighted in 1994 by Daugherty et al. when they observed that MPO was expressed in atherosclerotic lesions [65]. Since then, many clues have arisen such as the fact that fingerprints for in vivo modification by the MPO/H2O2/Cl− system of apoB-100 were observed by immunohistological analyses [15] and later confirmed by gas chromatography-mass spectrometry [85, 86]. Other reports also showed that MPO deficiency or low plasma levels of MPO decrease cardiovascular risk in patients [87, 88] strengthening the case that MPO is a key element for oxidative damages in atherosclerosis.
Targets of MPO on LDL and Products of Oxidation. It is important to keep in mind that HOCl is the most abundant product of MPO in vivo, and traces of HOCl-modified epitopes have been found in acute and chronic vascular inflammatory diseases such as atherosclerosis [14, 89]. MPO produces HOCl by the enzymatic system MPO/H2O2/Cl−. However, to facilitate the experimental scheme, HOCl reactant is commonly used instead of the enzymatic system.
Modification of LDL by HOCl has been studied by different groups, and Malle et al. have recently reviewed the effects of that reactant on LDL [90]. From these works, it clearly appeared that the protein moiety apoB-100 is the major target of HOCl although the production of hydroperoxides, chlorohydrins, chlorinated sterols or fatty acids, and lysophospholipids has also been described in the presence of HOCl [76, 91, 92]. These lipid oxidations occur in strict reaction conditions such as an acidic pH (3–5) and with a large excess of reactant.
Specificity of MPO to Oxidize LDL. As mentioned above, HOCl added as a reactant has been usually used to mimic the MPO/H2O2/Cl− system. However, this model may not be a perfect model to mimic MPO action on LDL/apoB-100. The main reason for this is the fact that MPO rapidly adsorbs at the surface of LDL and seems to have a strong interaction with the protein moiety of LDL [93, 94]. This adsorption phenomenon is due to the cationic characteristic of MPO, and it has been described on lipoproteins and also on endothelial cells [95]. LDL-MPO bound was first shown by Carr et al. who observed a coprecipitation of apoB-100-containing lipoproteins and MPO. The authors demonstrated that lipoprotein-deficient plasma did not permit MPO precipitation, whereas a dose-dependent MPO precipitation was observed by addition of LDL [93]. More recently, Sokolov et al. studied the specificity of MPO to bind different lipoproteins and concluded that MPO binds LDL more avidly and more specifically than HDL [94]. They also demonstrated that ceruloplasmin, which is a human plasmatic protein and a physiological MPO inhibitor [96], is able to inhibit MPO activity when HDL is present but not in the presence of LDL. The same group then studied the binding site for MPO on apoB-100 [97]. The authors predicted that MPO should bind to the NH2-βα1 domain of apoB-100 because this domain is exposed on the outside of the lipoprotein. Furthermore, because of the cationic property of MPO, these authors speculated that the MPO binding site on apoB-100 may not include any positively charged residues (lysine or Arginine) but at the opposite include negatively charged ones (aspartic or glutamic acid). They therefore proposed that MPO might bind one of the three following apoB-100 sites: 1EEEMLEN7, 53VELEVPQ59, or 445EQIQDDCTGDED456. They synthesized these three peptides and studied their affinity for MPO. Only the 445EQIQDDCTGDED456 peptide was able to form a complex with MPO, and the authors concluded that it might be the binding site of MPO on apoB-100. However, experiments should be performed to confirm this binding site. Experiments with site-specific mutations on apoB-100 to disable MPO-LDL complex formation would be a good experimental procedure, in this respect and this has previously been done to reveal the binding site of MPO on apolipoprotein A-I of HDL [98]. Furthermore, Carr et al. described MPO : LDL ratio of 3 : 1, whereas Sokolov et al. found a ratio of 1 : 1. The study of MPO-LDL interactions and LDL oxidation by MPO thus remains a challenge for the future.
Oxidation of LDL by MPO-Dependent Species other than Hypochlorous Acid. Whereas HOCl is the major oxidant formed by MPO, others might also be produced in vivo. Among them, tyrosyl radical, nitrogen dioxide, hypobromous acid, cyanate, and hypothiocyanous acid are often mentioned as potential species that may target LDL.
Tyrosine is a substrate of MPO, and tyrosyl radical can be produced via the one-electron reaction of the peroxidase cycle. The latter rapidly oxidizes lipids and also forms di-tyrosine residues in proteins, and protein-bound dityrosine residues have been identified in atherosclerotic lesions [99].
Nitration of LDL has been also studied in several works. Recently, Hamilton et al. have shown that LDL nitration leads to unfolded protein and deleterious effects [100]. These authors studied the phenomenon using Sin-1 as a peroxynitrite generator for protein nitration, and MPO has also been used as a catalyzer of nitration [101–103]. However, MPO mediates protein nitration via the formation of nitrogen dioxide (NO2 −) from nitric oxide [104, 105].
MPO can also produce hypobromous and hypothiocyanous acids via the halogenous cycle. The former would be a minor product of MPO activity [49], but several studies have been performed on its reactivity on lipoproteins [106]. The latter work concluded that hypobromous acid attacks both lipid and protein moieties, but it has less deleterious effects than hypochlorous acid. On the other hand, hypothiocyanous formation might be present in vivo to a larger extent; however, there are no clear data showing definitive alteration produced by this species [59]. However, cyanate (−OCN), a product of decomposition of hypothiocyanous acid, reacts with the terminal amino group of lysine, forming a carbamylated residue, also named homocitrulline. MPO can also use thiocyanate (−SCN) and produce −OCN [107]. MPO might therefore indirectly result in protein carbamylation, and this phenomenon was observed in lesions and lipoproteins [107, 108]. It is also worth noting that −SCN concentration may change the efficiency of MPO to produce HOCl [59]. These data illustrate how complex the process of LDL oxidation is in vivo, and the latter should be the subject of future experiments.
4.2.3. Localization of LDL Oxidation by Myeloperoxidase
The consensus model of atherogenesis describes the first step of the disease as migration of native LDL from plasma to the subendothelial space where it can be oxidized [17]. However, the mechanism and localization of in vivo LDL oxidation is still not fully understood. The model of early LDL oxidation in the circulation is often ruled out by the fact that blood contains lots of antioxidant molecules. It is further thought that the presence of ox-LDL in the plasma is due to backdiffusion from lesions. However, evidence has recently emerged to strengthen the possibility of LDL oxidation in the circulation. Our group has shown that LDL can be oxidized at the surface of activated endothelial cells in the presence of MPO. Circulating MPO is indeed known to adsorb on LDL and also on endothelium where this oxidation process could happen when the cells are activated and NADPH oxidase complex produces O2 •−. To this end, in vitro experiments were performed using endothelial cells (Ea.hy926) which were incubated for 24 h in the presence of native LDL, MPO, and angiotensin II, a modulator of O2 •− production by the NADPH oxidase complex. Mox-LDL production was monitored using a specific Mox-LDL antibody [109] and increased dependently of MPO and LDL concentrations. These data showed that LDL oxidation is possibly not restricted to intima. The plasma level of Mox-LDL is potentially a marker of plasma MPO activity in the field of cardiovascular disease. In this context, we showed that patients exposed to hemodialysis therapy due to kidney failure have higher blood levels of Mox-LDL, and this could be linked to their high cardiovascular risk [110].
To summarize, Figure 2 illustrates a revised scheme of the LDL oxidation by MPO in atherogenesis taking into account the model of oxidation in the circulation.
Figure 2.
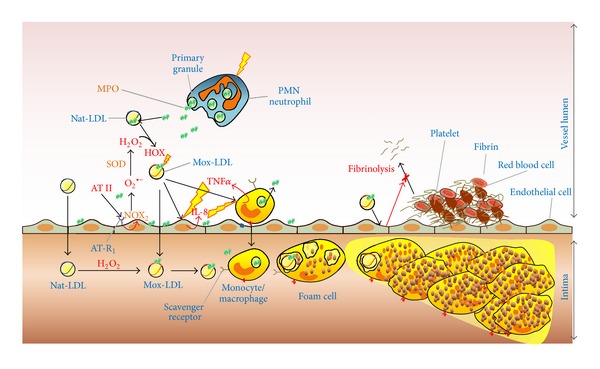
Role of myeloperoxidase and Mox-LDL in triggering inflammation and atherosclerosis plaque formation. Activation of neutrophils and monocytes leads to MPO release in the extracellular space, that is, the circulation. Due to its cationic properties, free MPO rapidly adsorbs at the surface of endothelial cells or native LDL (Nat-LDL). Angiotensin II (AT II) activates endothelial cells via angiotensin receptor 1 (AT-R1), which in turn produces superoxide anion (O2 •−) via the NADPH oxidase complex, (NOX2). O2 •− is rapidly transformed into hydrogen peroxide (H2O2) spontaneously or by the enzyme superoxide dismutase (SOD). Nat-LDL can be so directly oxidized by MPO/H2O2/chloride system in the circulation and form the so-called Mox-LDL. The latter can in turn pass through the endothelium (due to endothelial dysfunction) to the subendothelial space where it will be recognized by macrophages and eliminated. Accumulation of oxidized lipoproteins leads to foam cell formation and lipid accumulation in the subendothelial space. Nat-LDL, can also directly pass through the endothelial wall where they are oxidized by MPO in the subendothelial space. Finally, LDL oxidized by myeloperoxidase (Mox-LDL) activates endothelial cells and induces interleukine-8 (IL-8) secretion by these cells. Mox-LDL effects on monocyte are similar and activate tumor-necrosis factor-α (TNFα) secretion by these cells. In turn, IL-8 and TNFα activate monocytes and endothelial cells, respectively. Mox-LDL also inhibits fibrinolysis process via endothelial cell interaction.
5. Impacts of Mox-LDL on Inflammation: In Vitro Experiments
As mentioned previously in this paper, Mox-LDL is very specific and differs from LDL oxidized by Cu2+. In this context, monoclonal antibodies against Mox-LDL were developed for immunochemical studies. In our research group, several antibodies were generated by immunizing mice and collecting and analyzing clones. Four antibodies were specific for Mox-LDL and did not crossreact with Cu-LDL, LDL oxidized by H2O2, or albumin oxidized by the MPO system. Three of these antibodies recognize the protein moiety of LDL (AG948, EB2E9, and EB2G3), and one (14A2G6) is dependent on the presence of the lipid moiety. Furthermore, the three protein-sensitive antibodies appear to be conformation dependent [109]. These antibodies react with atherosclerotic plaques showing that they can be used for immunohistochemistry studies. Other monoclonal antibodies against Mox-LDL have also been developed by other groups [14].
A large number of transcription factors have been observed to be activated by ox-LDL [111], and many of them have particular impacts on the inflammatory effect of atherosclerosis. In the following paragraphs, we report the major effects observed on monocytes, macrophages, and endothelial cells with a particular interest on Mox-LDL induction.
5.1. Effects of Mox-LDL on Monocytes/Macrophages
Atherosclerosis is a complex process involving inflammatory and oxidative stress pathways [112]. Ox-LDL is involved in monocyte/macrophage activation and in the inflammatory response [113]. Monocytes are one of the first cells that reach the site of inflammation such as in nascent atherosclerotic lesions. When activated, this cell type expresses leukocyte adhesion molecules [114], and it also produces ROS and RNS, partly due to MPO activity, and causes the transformation of LDL into a high-uptake form for macrophages [115–117]. Cu-LDL has the capacity to activate monocytes and increases expression of peroxisome proliferator-activated receptor-γ (PPAR-γ), a regulator of cell proliferation, inflammation, monocyte/macrophage differentiation, and CD36 scavenger receptor expression at the cell surface [118, 119]. In 2005, Westendorf et al. have shown that HOCl-LDL has the same proinflammatory properties in vitro [120].
As with Cu-LDL [18], HOCl-LDL inhibits lysosomal proteases (e.g., cathepsin B), but the mechanism was identified as dependent on the chloramine content of apoB-100 and oxidized residues that are not present in Cu-LDL [121]. This protease inhibition contributes to lipid accumulation in macrophages and to foam cell transformation.
Furthermore, both Cu- and HOCl-LDL are potent inducers of caspase-dependent apoptosis as shown by Vicca et al. [122] on THP-1 monocytes cell. However, macrophage-differentiated cells seemed to be resistant to apoptosis in these experiments. Nevertheless, this effect is compatible with the idea that macrophages have a prolonged survival and boost atherogenesis.
Considering the literature of LDL oxidation and cell inflammatory processes, studies of ox-LDL effects on monocytes/macrophages have been mainly performed using Cu-LDL, whereas HOCl-LDL and MPO-LDL are more rarely used. We recently investigated Mox-LDL impacts on a THP-1 cell line and observed an intriguing result [123]. Incubation of Mox-LDL with THP-1 cells during 4 h increased 2-folds the secretion of TNFα (a key regulator of the synthesis of acute-phase proteins (i.e., fibrinogen, factor VIII) that are linked to atherogenesis [124]), whereas no increase was detected for native LDL or native and Mox-albumin. These data highlighted the specificity of Mox-LDL as MPO-oxidized proteins did not induce TNFα production. TNFα is itself an activator of other cells such as endothelial cells where it induces among other things the expression of VCAM-1 [125]. We will return to discuss this activation later in this paper in the context of endothelial cell activation by Mox-LDL.
More recently, macrophage reactivity to ox-LDL was investigated by comparing Mox-LDL and Cu-LDL on RAW264.7 cells [126]. This cell line is usually used for metabolic studies with the advantage of interaction with ox-LDL and to induce foam cell formation [127–130]. Cells were incubated with native and ox-LDL for 48 h before analysis. The first set of experiments highlighted that accumulation of lipids is higher in the presence of Mox-LDL than Cu-LDL (Figure 1 of [126]). The same trend was confirmed with macrophages derived from peripheral blood mononuclear cells (PBMCs) differentiated by macrophage-colony stimulating factor. In a second set of experiments, ROS production was explored by monitoring fluorescence of dichloro-dihydro-fluorescein when RAW264.7 and PBMC-derived macrophages were exposed to ox-LDL. Whereas both Mox- and Cu-LDL significantly increased ROS accumulation in RAW264.7, only Mox-LDL seemed to increase this accumulation in PBMC-derived macrophages (Figure 2 of [126]).
In order to combat an excess of ROS, cells have developed several mechanisms. In this context, NF-E2-related factor 2 (Nrf2) is a transcription factor which is upregulated when ROS is increased. In redox homeostatic conditions, Nrf2 is inactive and kept in the cytoplasm bound with a Keap1/Rbx1/Cul3 complex, which promotes its ubiquitination and subsequent degradation by the 26S proteasome. When activated, Nrf2 binds DNA at the “antioxidant response element” and regulates the expression of protective genes. The regulatory subunit of glutamate-cysteine ligase (Gclm) and hemeoxygenase-1 (HO-1) are two examples of Nrf2-regulated genes [131]. Glcm is the limiting component of glutathione production, a strong in vivo antioxidant, and HO-1 is responsible for hemedegradation in cells, decreasing potential oxidant formation by heme-enzymes. In the same study, Calay et al. [126] showed that Mox-LDL and Cu-LDL result in overexpression of Gclm and HO-1 induction by Nrf2-dependent activation. However, Mox-LDL triggered a stronger response than Cu-LDL. In addition, Trolox, a well-known water-soluble antioxidant able to quench ROS production, was added to experimental batches in order to confirm that Nrf2 was induced by ROS accumulation. Addition of Trolox led to reduced Nrf2 expression. However, while ROS production was totally inhibited by Trolox, Gclm and HO-1 expression was still higher than basal level, suggesting the implication of other pathways in their overexpression. RNA interference approaches targeting Nrf2 gave the same result of partial abolition of Gclm and HO-1 expression and confirmed the hypothesis that transcription factors other than Nrf2 are implicated in the antioxidant response of macrophages.
Differences observed between Cu- and Mox-LDL could be explained by the fact that their ROS induction is mediated by different pathways. ROS production via NADPH oxidase is activated by both ox-LDL, but only Mox-LDL induced the production of ROS by cytosolic phospholipase A2. This was illustrated by quantifying ROS production in the presence of methylarachidonylfluorophosphonate, an inhibitor of cytosolic phospholipase A2. A 43% decrease was observed in ROS production induced by Mox-LDL where no decrease was observed for Cu-LDL.
Interestingly, when Mox-LDL was generated by a stronger MPO-dependent oxidative process, which is capable of extending the oxidation of LDL to the lipid moiety, the ROS production was decreased but remained higher than Cu-LDL induction. These data suggest that lipid peroxidation levels of ox-LDL could be inversely correlated to ROS production in macrophages.
In summary, Mox-LDL induces ROS production, lipid accumulation, and antioxidant responses in macrophages as with other ox-LDL but by using a different pathway than Cu-LDL. However, Mox-LDL seems to induce a higher responsiveness in monocytes/macrophages than ox-LDL and might be more atherogenic.
5.2. Effects of Mox-LDL on Endothelial Cells
Endothelial dysfunction is potentially the first event of atherosclerosis development. It is still not totally understood why this occurs and when these lesions start, but evidence has been claimed many times. Endothelial permeability is increased at the site of lesions and favors LDL penetration into the artery wall. Furthermore, ox-LDL mediates endothelial dysfunction and is considered as a key event in the initiation of arterial lesions [132].
Endothelial cells also express scavenger receptor (SR) at their surface and can interact with ox-LDL. However, the main SR expressed on endothelial cells is LOX-1, the specific lectin-like endothelial receptor for ox-LDL. However, CD36 and SR-B1 have also been localized at the endothelial cell surface [133]. HOCl-LDL is internalized by CD36 and SR-B1 [134], while the receptor(s) which recognize(s) Mox-LDL and enable(s) endocytosis remain(s) to be documented for monocytes, macrophages, and endothelial cells. The presence of scavenger receptors at the surface of endothelial cells could lead to endocytosis of Mox-LDL. However, endothelial cells are not able to accumulate lipids when incubated with ox-LDL. Nevertheless, Mox-LDL activates endothelial cells, as well as monocytes/macrophages.
Cu-LDL but not native LDL is able to induce interleukin-8 (IL-8) production by endothelial cells [135]. IL-8 belongs to the C-X-C subgroup of chemokines and is a multifunctional cytokine involved in numerous biological processes including atherosclerosis. IL-8 acts as a chemoattractant to inflammatory cells and also to smooth muscle cells and is involved in the migration of the latter in the intima. Furthermore, IL-8 activates monocytes and/or macrophages and up-regulates their production of TNFα. HOCl-LDL induction of IL-8 was also demonstrated but only in monocytes [136].
In order to assess whether Mox-LDL is also an inducer of IL-8 production by endothelial cells, our group performed an experiment where Mox-LDL was incubated with EAhy926 endothelial cells for 48 h [123]. This cell line is a reliable model for studying vascular inflammation, leukocyte-endothelial interactions, and metabolic impacts of ox-LDL [135]. IL-8 was measured in the supernatant, and a dose-dependent response was observed. No response was detected with native LDL and native or Mox-albumin (control experiments). The specificity of Mox-LDL was also confirmed by the absence of a Mox-albumin effect.
With the capability of Mox-LDL to trigger both monocytes and endothelial cells, it appeared that a cycle could be present. Indeed, Mox-LDL activated both monocytes and endothelial cells which secrete TNFα and IL-8 respectively. The latter activates endothelial cells and monocytes/macrophages leading (i) to ROS production, (ii) to MPO release in the extracellular matrix, and (iii) so potentially to new Mox-LDL.
5.3. Mox-LDL and Fibrinolysis
Coagulation and fibrinolysis are continuously in balance at the surface of the endothelial cell wall. These cells contribute to fibrinolysis by secreting tissue-plasminogen activator (t-PA), urokinase-plasminogen activator (u-PA), and plasminogen activator inhibitor-1 (PAI-1), three fibrinolysis regulators, or by expressing specific receptors which bind these fibrinolysis factors [137]. Enhancement of fibrin generation gives a prothrombotic environment on the endothelial cell surface, and fibrin induces the production of IL-8 by endothelial cells. In this context, a dysfunctional fibrinolysis process was reported to be a factor in atherogenesis, complementary to ox-LDL [138]. This was first mentioned as a key factor in 1998 by Sueishi et al. [139] and Mayerl et al. [140], and a recent clinical study from our group further confirmed it [141]. However, until 2012, the interplay between Mox-LDL (and more generally ox-LDL), endothelial cells, and fibrinolysis had not been investigated [142]. Our group documented this intriguing subject with the aid of a device which allows us to monitor fibrinolysis in real time [143]. Briefly, fibrin formation and degradation occurs in adapted circular microcuvettes. To monitor the effect of endothelial cells (EA.hy926) on fibrinolysis taking place at their surface, cells were immobilized on collagen-coated membranes, fixed to the bottom of glass circular microcuvettes, and grown to confluence. The microcuvettes were inserted in the experimental apparatus at 37°C, the euglobuin fraction was added and clot formation started by addition of thrombin. TNFα was used as a positive control as it is known to have antifibrinolytic activity. To test the system, a 24 h TNFα treatment of endothelial cells was performed and effectively showed an increase in fibrinolysis time. Monitoring of native and Mox-LDL showed that Mox-LDL at concentrations of 10 and 50 μg/mL also increased the time of fibrinolysis unlike native lipoprotein, confirming again that Mox-LDL has a physiopathological effect on atherogenesis. Nevertheless, higher concentrations of Mox-LDL (100 μg/mL) showed a decreased effect.
PAI-1, t-PA, annexin II (a t-PA receptor), and uPAR secretion were also analyzed in this study, but there was no effect of native or Mox-LDL. However, as TNFα increased t-PA and PAI-1 in smooth muscle cells, it is suggested that other pathways/factors are involved in fibrinolysis modulation. This raises the question whether the receptor and signal transduction pathways activated by Mox-LDL and TNFα are different. With a view to clarify the underlying bio-molecular mechanism, scavenger receptor interactions with Mox-LDL were investigated. Previous data described LOX-1 binding to ox-LDL and mediating effects in endothelial cells. However, our first investigations by neutralization of this receptor using antibodies did not impact IL-8 production induced by Mox-LDL, disproving this pathway [142]. Hence, future research on scavenger receptor is required to extend the understanding of Mox-LDL effects on endothelial cells.
In summary, Mox-LDL disturbs fibrinolysis but in a different pathway than the t-PA- and PAI-1 dependent pathways. Future investigations are needed to solve the mechanism by which Mox-LDL is involved in this pathological process.
5.4. Summary of In Vitro Effects of Mox-LDL
It appears that Mox-LDL plays a crucial role in lipid accumulation in macrophages/foam cells and also in the whole proinflammatory process linked to atherosclerosis lesion development. Figure 2 summarizes the different aspects and effects of MPO/Mox-LDL in the circulation/intima including effects on endothelial cells, monocytes/macrophages, and fibrinolysis. Mox-LDL generates a vicious circle effect, prevents resolution of the nascent lesion, triggers oxidative stress and lipid accumulation in the subendothelial space, and inhibits normal fibrinolysis.
6. Clinical Aspects of Mox-LDL
6.1. Introduction
For a long time, ox-LDL and MPO have been accepted as cardiovascular risk factors and have been largely documented in the literature by in vivo experiments or clinical studies [17, 63, 144–146]. However, only a small number of studies have investigated LDL modified by the MPO/H2O2/chloride system (Mox-LDL). Our group has contributed to this, and we observed that Mox-LDL is present in atherosclerotic lesions [109]. We have already discussed numerous Mox-LDL effects in atherosclerosis plaque formation in this paper and this subject is not further discussed here. Nevertheless, cardiovascular diseases are linked, notably in relation to atherosclerosis development, to several pathologies such as kidney failure/end stage renal disease, sleep restriction, erectile dysfunction, or chronic obstructive pulmonary disease. Evidences have been growing for Mox-LDL implications in these pathologies, and they are summarized in the following paragraphs.
6.2. Mox-LDL, Kidney Failure, and Hemodialysis
Kidney failure and subsequent uremia has been linked to chronic inflammation and cardiovascular disease [147]. It has also been proposed that hemodialysis triggers inflammation as a result of exposure of blood to the bioincompatible system stimulating monocyte and macrophage cells [148, 149]. These processes induce proinflammatory oxidative stress responses, and MPO has been implicated in the development of cardiovascular and chronic kidney diseases [88, 150, 151]. MPO also directly targets kidneys through HOCl production [152, 153].
Wu et al. reported [154] that MPO concentration could serve as a marker of oxidative stress during hemodialysis, and Himmelfarb et al. [155] showed that MPO concentration increases during hemodialysis sessions. We also recently contributed to MPO investigations in the context of hemodialysis therapy [156]. In this paper, MPO activity was monitored using the SIEFED (specific immunoextraction followed by enzymatic detection) method developed previously by Franck et al. [157]. We further developed a total protein hydrolysis method assisted by microwave and coupled to LC-MS analyses devoted to the monitoring of protein-bound 3-chlorotyrosine and homocitrulline. In this work, it was observed in 15 patients that an increase of plasma MPO, levels during the hemodialysis, is accompanied (i) by a direct increase of MPO activity and, more interestingly, (ii) by a direct MPO-dependent oxidation of plasma proteins.
Previously, we had shown that Mox-LDL levels in blood are increased during hemodialysis [110]. Together with the recent results, these data highlight that MPO induces direct protein oxidation and potentially targets LDL. Indeed, MPO avidly interacts and adsorbs at the surface of LDL and triggers apoB-100 oxidation with an impact on the cardiovascular risk of the patients [156]. Furthermore, these data strengthen the model of the MPO-dependent oxidation of LDL in the circulation as a contributive mechanism of atherosclerosis. The latter process is also illustrated in Figure 2.
6.3. Mox-LDL and Sleep Restriction
Nowadays, people are more and more sleep deprived due to work pressure and requirement (i.e., shift schedules or extension of hours), family demands, or our 24/7-week lifestyle [158]. According to the 2009 National Sleep Foundation Survey, 20% of Americans sleep less than 6 h per night during the week [159]. This modification of sleep duration is not of minor consequence to our health. Sleep deprivation is harmful and can lead to problems in metabolism [160], immune [161], or cardiovascular systems [162, 163].
Studying sleep-deprived individuals, van Leeuwen et al. have associated the increase of proinflammatory molecules IL-17, C-reactive protein (CRP), IL-1β, and IL-6 with cardiovascular risk [164]. Furthermore, total or severe sleep restriction alters blood cell counts with a particular increasing effect on neutrophils and granulocytes [165, 166]. Neutrophil count has even been proposed as a marker of immune recovery function of sleep [167]. An increase in MPO plasma levels was also detected after acute sleep restriction [166].
In this context, MPO and Mox-LDL levels were recently studied, together with inflammatory markers in 9 mid-twenties men for 11 consecutive days (3 baseline nights followed by 5 restricted-sleep nights (max. 5 hours of sleep) and then 3 recovery-sleep nights) [168]. Results showed that MPO was not increased during the sleep restriction but rose during the first night of recovery sleep. Whereas MPO levels peaked during the first recovery night, Mox-LDL levels were significantly higher during the first and third nights of sleep restriction but not at the recovery period. Mox-LDL/apoB-100 ratio, which expresses the fraction of modified lipoproteins in the total pool, was also statistically increased during the first night of sleep restriction. Speculating on the reason for this temporal discordance between Mox-LDL and MPO levels in blood, it appears from the literature that catecholamines are increased during sleep restriction [169] and can activate the NADPH oxidase complex at the surface of endothelial cells [170]. As a result, the O2 −• formed could be converted into H2O2 and react with MPO to form Mox-LDL.
In summary, these data show that the recovery process after sleep restriction is linked to modifications of levels of cardiovascular risk biomarkers in blood. However, future experiments are required to help understand the impact of sleep restriction on human health. Studies including more male and female individuals are also needed but are unfortunately difficult to set up and standardize.
6.4. Mox-LDL and Nonalcoholic Fatty Liver Disease
Nonalcoholic fatty liver disease (NAFLD) includes different liver disorders such as steatosis, steatohepatitis, cirrhosis, and advanced fibrosis. Furthermore, NAFLD has been associated with a high risk of cardiovascular disease (CVD) [171], obstructive sleep apnea [172], or colorectal cancer [173]. MPO has been involved in the progression of non-alcoholic steatohepatitis where neutrophil accumulation is a key component of the inflammatory process. Moreover, it has been shown that NAFLD is associated with increased levels of nitrated proteins that might partly come from MPO activity [174]. More recently, Rensen et al. reported that MPO deficiency decreases hepatic cholesterol accumulation and inflammation in mice that do not express the LDL-receptor (LDLR−/− mice) and that were fed with a high-fat diet, [175]. In these experiments, the authors also observed that, after 3 weeks of high-fat diet, MPO levels were increased in the liver of hyperlipidemic mice that expressed MPO. Furthermore, MPO activity in mouse liver was investigated by monitoring nitrotyrosine levels. The latter product is indeed, at least partially, generated by MPO during the inflammation process. These data demonstrate the important role of MPO in NAFLD, and this might be linked to the oxidation of lipoproteins and particularly of LDL by MPO.
6.5. Mox-LDL and Chronic Obstructive Pulmonary Disease
Patients with chronic obstructive pulmonary disease (COPD) have increased systemic inflammation, increased endothelial dysfunction, and changes in the oxidant/antioxidant ratio. Furthermore, these patients are at a high risk of cardiovascular disease, and 22%–50% of them will die of cardiovascular conditions [176–178]. Long-term oxygen therapy has been observed to prolong survival in hypoxemic COPD patients, but the mechanisms are not completely understood.
In this context, we hypothesized that oxygen therapy could alter systemic inflammation and oxidative stress. As a consequence, several markers, including neutrophils, Mox-LDL, and IL-8, were monitored in 11 patients before starting, after one week and after one month of oxygen therapy [179]. Neutrophils, IL-8, and Mox-LDL were all significantly decreased after one month of oxygen therapy. These data showed that oxygen breathing is favorable to reduce the oxidative stress and inflammatory state in hypoxemic patients with COPD.
At this point only, speculation could explain these observed decreases. In this way, chronic hypoxia is associated with raised sympathetic activity, activation of the renin-angiotensin system, and production of catecholamines [180]. By activating the NADPH oxidase complex, catecholamines can induce Mox-LDL formation in the circulation. Conversely, when oxygen therapy is provided, catecholamine formation is reduced, which could decrease Mox-LDL formation. Reduction of the sympathetic activity might also decrease neutrophil counts in blood and act on MPO level. Finally, IL-8 released by endothelial cells is also induced by Mox-LDL in vitro and suggests that Mox-LDL decrease could partly be explained by the reduction in IL-8 secretion.
6.6. Mox-LDL and Erectile Dysfunction
Erectile dysfunction (ED) is a vascular disorder. Indeed, erection and detumescence of the penis are hemodynamic events controlled by the relaxation and contraction, respectively, of arterial and intracavernous smooth muscle cells. Erectile function is also subject to endothelial cells and their ability to release nitric oxide (NO•). NO• is indeed the main neurotransmitter involved in erection and reacts with the enzyme guanylate cyclase that increases cyclic guanosine monophosphate and produces a cascade of events at the intracellular level. This process results in a loss of contractile tone of smooth muscle cells [181, 182].
Clinical studies have identified a link between hypercholesterolemia, atherosclerosis, and erectile dysfunction. ED has been even described as a preliminary event of future major cardiovascular outcomes and as a predictor of coronary heart disease [183–186]. Furthermore, it was reported that HOCl-LDL inhibits NO• synthesis in endothelium [187], and we previously reported effects of Mox-LDL on endothelial cells ([123] and see above: effects of Mox-LDL on endothelial cells).
On this basis, our group has performed an immunohistochemical approach to study the presence of Mox-LDL in penile tissues in patients suffering from ED [188]. Intracavernous tissue was taken from 8 patients undergoing penile implant surgery, and an antibody against Mox-LDL [109] was used to reveal the presence of MPO-dependent oxidized LDL. Among these patients, 7 were known to have vascular ED, and one patient had ED due to neurologic lesions after radical prostatectomy. In the 7 patients with vascular ED, the presence of Mox-LDL was observed, whereas no Mox-LDL was observed in the patient with ED due to prostatectomy. The latter was a good negative control and these data confirmed that, when ED is due to vascular dysfunction, LDL is oxidized and this phenomenon could trigger ED development.
In addition, careful observation of stained slides revealed that Mox-LDL is restricted to the endothelium and subendothelial space in artery, but, conversely, they are deeply diffused and intermingled between the smooth muscle fibers in the intracavernous tissues. Furthermore, Mox-LDL staining revealed the presence of Mox-LDL in the cytoplasm of endothelial cells. This confirms the endocytosis of these lipoproteins into cells.
As cyclic guanosine monophosphate (cGMP) is a key mediator in the NO•-dependent pathway of erectile function, it was hypothesized that cGMP levels could be influenced by the presence of Mox-LDL. We showed in vitro that a 48 h incubation of Mox-LDL with EA.hy926 endothelial cells induces a decrease of the level of cGMP when compared with control and native LDL [189]. In the cavernosum tissue, cGMP is naturally hydrolyzed by phosphodiesterase 5 (PDE5). Inhibition of this enzyme is considered a first-line therapy for patients with ED and helps maintain higher levels of cGMP [190–192]. Thus, Mox-LDL presence in penile tissue could be an explanation for the resistance of patients to PDE5 inhibitor therapy [189]. Conversely, PDE5 inhibitors were tested to know whether they protect or not against the proinflammatory effects of Mox-LDL on endothelial cells. For this purpose, EA.hy926 endothelial cells were incubated with Mox-LDL and available PDE5 inhibitors (sildenafil, vardenafil and tadalafil), and IL-8 production was then measured [193]. Only one of the PDE5 inhibitors (tadalafil) was shown to have a beneficial effect in vitro by significantly decreasing IL-8 production compared with the other two inhibitors. A complementary effect on endothelial cells (in addition to the relaxation) could be also produced by tadalafil. This could potentially be an interesting effect that could be considered in the future when a physician implements a chronic treatment for ED. However, clinical data are required to confirm the in vitro experiments before drawing further conclusions.
7. Concluding Remarks and Future Perspectives
In summary and conclusion, in vitro experiments and clinical studies support a key role of MPO-dependent oxidized LDL in the process of atherosclerosis and cardiovascular linked diseases. This specifically modified lipoprotein induces proinflammatory effects by stimulating TNFα and IL-8 secretion in monocytes and endothelial cells respectively. In turn, TNFα and IL-8 activate endothelial cells and monocytes, respectively, and promote MPO and ROS release leading to new Mox-LDL formation. Furthermore, Mox-LDL has exhibited inhibitory effects on fibrinolysis, a key process in the release of fibrin.
In vivo, Mox-LDL is present in atherosclerotic lesions, and its level is increased in the circulation of patients with high cardiovascular risk, such as those with kidney failure and those undergoing hemodialysis. The presence of Mox-LDL was also revealed in patients suffering from vascular erectile dysfunction, disease linked to atherosclerosis and endothelial dysfunction. In addition, increased blood levels of Mox-LDL have also been observed during sleep restriction. Mox-LDL is thus a potentially good marker of cardiovascular disorders and/or cardiovascular risk.
In contrast to other types of oxidation (e.g., by copper), MPO-dependent oxidation of LDL primarily targets the protein moiety of LDL, namely, apolipoprotein B-100. Furthermore, MPO oxidation is thought of as a more physiopathological model of LDL oxidation than that involving copper. As Mox-LDL induces much more ROS production and lipid accumulation in macrophages than Cu-LDL, Mox-LDL in particular should be considered more in biological experiments and clinical studies.
Challenges thus remain for the future, and researchers should keep working on the impact of MPO and Mox-LDL on human health. As an example, the exact receptors that enable Mox-LDL endocytosis in macrophages/monocytes and endothelial cells should be further studied. Last but not least, it has been observed that MPO specifically oxidizes apoB-100, but the exact binding sites of MPO at the surface of apoB-100 remain to be further described, as well as the residues oxidized on apoB-100. Increased understanding of the impact of Mox-LDL on the induction of proinflammatory and oxidative stress processes is also of major importance for the future.
Authors' Contribution
Cédric Delporte and Pierre Van Antwerpen equally contributed to this paper.
Acknowledgments
The authors express thanks to Dr. Jerrard Hayes (National Institute for Bioprocessing Research and Training, NIBRT, Dublin, Ireland) for his helpful advice on this paper. Cédric Delporte is a Postdoctoral Researcher of the Belgian Fund for Scientific Research (FRS-FNRS), and Luc Vanhamme is a Research Director of the Belgian Fund for Scientific Research (FRS-FNRS).
Abbreviations
- ApoB-100:
Apolipoprotein B-100
- Cu-LDL:
Low-density lipoprotein modified by reagent Cu2+
- ED:
Erectile dysfunction
- H2O2:
Hydrogen peroxide
- HOCl/OCl−:
Hypochlorous acid/hypochlorite
- HOCl-LDL:
Low-density lipoprotein modified by reagent HOCl
- IL:
Interleukin
- LDL:
Low-density lipoprotein
- M-CSF:
Macrophage colony stimulating factor
- Mox-albumin:
Albumin modified by the MPO-H2O2-chloride system
- Mox-LDL:
LDL modified by the MPO-H2O2-chloride system
- MPO:
Myeloperoxidase
- MS:
Mass spectrometry
- NADPHox:
Nicotinamide adenine dinucleotide phosphate oxidase
- Ox-LDL:
Oxidized LDL
- PTM:
post-translational modification
- RNS:
reactive nitrogen species
- ROS:
reactive oxygen species
- TNFα:
tumor-necrosis factor-α.
References
- 1.Lind L. Circulating markers of inflammation and atherosclerosis. Atherosclerosis. 2003;169(2):203–214. doi: 10.1016/s0021-9150(03)00012-1. [DOI] [PubMed] [Google Scholar]
- 2.Noels H, Weber C. Editorial comment: catching up with important players in atherosclerosis: type i interferons and neutrophils. Current Opinion in Lipidology. 2011;22(2):144–145. doi: 10.1097/MOL.0b013e328344780b. [DOI] [PubMed] [Google Scholar]
- 3.Weber C, Noels H. Atherosclerosis: current pathogenesis and therapeutic options. Nature Medicine. 2011;17(11):1410–1422. doi: 10.1038/nm.2538. [DOI] [PubMed] [Google Scholar]
- 4.DeBakey ME, Lawrie GM, Glaeser DH. Patterns of atherosclerosis and their surgical significance. Annals of Surgery. 1985;201(2):115–131. doi: 10.1097/00000658-198502000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mazzolai L, Silacci P, Bouzourene K, Daniel F, Brunner H, Hayoz D. Tissue factor activity is upregulated in human endothelial cells exposed to oscillatory shear stress. Thrombosis and Haemostasis. 2002;87(6):1062–1068. [PubMed] [Google Scholar]
- 6.Van Assche T, Hendrickx J, Crauwels HM, et al. Transcription profiles of aortic smooth muscle cells from atherosclerosis-prone and -resistant regions in young apolipoprotein E-deficient mice before plaque development. Journal of Vascular Research. 2011;48(1):31–42. doi: 10.1159/000317398. [DOI] [PubMed] [Google Scholar]
- 7.Lusis AJ. Atherosclerosis. Nature. 2000;407(6801):233–241. doi: 10.1038/35025203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heinecke JW. Oxidants and antioxidants in the pathogenesis of atherosclerosis: implications for the oxidized low density lipoprotein hypothesis. Atherosclerosis. 1998;141(1):1–15. doi: 10.1016/s0021-9150(98)00173-7. [DOI] [PubMed] [Google Scholar]
- 9.Steinberg D, Parthasarathy S, Carew TE, Khoo JC, Witztum JL. Beyond cholesterol: modifications of low-density lipoprotein that increase its atherogenicity. The New England Journal of Medicine. 1989;320(14):915–924. doi: 10.1056/NEJM198904063201407. [DOI] [PubMed] [Google Scholar]
- 10.Yoshida H, Kisugi R. Mechanisms of LDL oxidation. Clinica Chimica Acta. 2010;411(23-24):1875–1882. doi: 10.1016/j.cca.2010.08.038. [DOI] [PubMed] [Google Scholar]
- 11.Chen K, Thomas SR, Keaney JF., Jr. Beyond LDL oxidation: ROS in vascular signal transduction. Free Radical Biology and Medicine. 2003;35(2):117–132. doi: 10.1016/s0891-5849(03)00239-9. [DOI] [PubMed] [Google Scholar]
- 12.Obama T, Kato R, Masuda Y, Takahashi K, Aiuchi T, Itabe H. Analysis of modified apolipoprotein B-100 structures formed in oxidized low-density lipoprotein using LC-MS/MS. Proteomics. 2007;7(13):2132–2141. doi: 10.1002/pmic.200700111. [DOI] [PubMed] [Google Scholar]
- 13.Sparrow CP, Parthasarathy S, Steinberg D. Enzymatic modification of low density lipoprotein by purified lipoxygenase plus phospholipase A2 mimics cell-mediated oxidative modification. Journal of Lipid Research. 1988;29(6):745–753. [PubMed] [Google Scholar]
- 14.Malle E, Waeg G, Schreiber R, Gröne EF, Sattler W, Gröne H-J. Immunohistochemical evidence for the myeloperoxidase/H2O2/halide system in human atherosclerotic lesions. Colocalization of myeloperoxidase and hypochlorite-modified proteins. European Journal of Biochemistry. 2000;267(14):4495–4503. doi: 10.1046/j.1432-1327.2000.01498.x. [DOI] [PubMed] [Google Scholar]
- 15.Hazell LJ, Arnold L, Flowers D, Waeg G, Malle E, Stocker R. Presence of hypochlorite-modified proteins in human atherosclerotic lesions. Journal of Clinical Investigation. 1996;97(6):1535–1544. doi: 10.1172/JCI118576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kruth HS, Huang W, Ishii I, Zhang W-Y. Macrophage foam cell formation with native low density lipoprotein. Journal of Biological Chemistry. 2002;277(37):34573–34580. doi: 10.1074/jbc.M205059200. [DOI] [PubMed] [Google Scholar]
- 17.Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473(7347):317–325. doi: 10.1038/nature10146. [DOI] [PubMed] [Google Scholar]
- 18.Hoff HF, Zyromski N, Armstrong D, O’Neil J. Aggregation as well as chemical modification of LDL during oxidation is responsible for poor processing in macrophages. Journal of Lipid Research. 1993;34(11):1919–1929. [PubMed] [Google Scholar]
- 19.Hansson GK. Regulation of immune mechanisms in atherosclerosis. Annals of the New York Academy of Sciences. 2001;947:157–165. [PubMed] [Google Scholar]
- 20.Hansson GK. Immune mechanisms in atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology. 2001;21:1876–1890. doi: 10.1161/hq1201.100220. [DOI] [PubMed] [Google Scholar]
- 21.Hevonoja T, Pentikäinen MO, Hyvönen MT, Kovanen PT, Ala-Korpela M. Structure of low density lipoprotein (LDL) particles: basis for understanding molecular changes in modified LDL. Biochimica et Biophysica Acta. 2000;1488(3):189–210. doi: 10.1016/s1388-1981(00)00123-2. [DOI] [PubMed] [Google Scholar]
- 22.Yang C-Y, Chen S-H, Gianturco SH. Sequence, structure, receptor-binding domains and internal repeats of human apolipoprotein B-100. Nature. 1986;323(6090):738–742. doi: 10.1038/323738a0. [DOI] [PubMed] [Google Scholar]
- 23.Knott TJ, Pease RJ, Powell LM. Complete protein sequence and identification of structural domains of human apolipoprotein B. Nature. 1986;323(6090):734–738. doi: 10.1038/323734a0. [DOI] [PubMed] [Google Scholar]
- 24.Knott TJ, Rall SC, Jr., Innerarity TL. Human apolipoprotein B: structure of carboxyl-terminal domains, sites of gene expression, and chromosomal localization. Science. 1985;230(4721):37–43. doi: 10.1126/science.2994225. [DOI] [PubMed] [Google Scholar]
- 25.Law SW, Grant SM, Higuchi K. Human liver apolipoprotein B-100 cDNA: complete nucleic acid and derived amino acid sequence. Proceedings of the National Academy of Sciences of the United States of America. 1986;83(21):8142–8146. doi: 10.1073/pnas.83.21.8142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang C-Y, Kim TW, Pao Q, et al. Structure and conformational analysis of lipid-associating peptides of apolipoprotein B-100 produced by trypsinolysis. Journal of Protein Chemistry. 1989;8(6):689–699. doi: 10.1007/BF01024895. [DOI] [PubMed] [Google Scholar]
- 27.Segrest JP, Jones MK, De Loof H, Dashti N. Structure of apolipoprotein B-100 in low density lipoproteins. Journal of Lipid Research. 2001;42(9):1346–1367. [PubMed] [Google Scholar]
- 28.Borén J, Ekström U, Ågren B, Nilsson-Ehle P, Innerarity TL. The molecular mechanism for the genetic disorder familial defective apolipoprotein B100. Journal of Biological Chemistry. 2001;276(12):9214–9218. doi: 10.1074/jbc.M008890200. [DOI] [PubMed] [Google Scholar]
- 29.Rutledge AC, Su Q, Adeli K. Apolipoprotein B100 biogenesis: a complex array of intracellular mechanisms regulating folding, stability, and lipoprotein assembly. Biochemistry and Cell Biology. 2010;88(2):251–267. doi: 10.1139/o09-168. [DOI] [PubMed] [Google Scholar]
- 30.Milne R, Theilis R, Jr., Maurice R, et al. The use of monoclonal antibodies to localize the low density lipoprotein receptor-binding domain of apolipoprotein B. Journal of Biological Chemistry. 1989;264(33):19754–19760. [PubMed] [Google Scholar]
- 31.Welty FK, Seman L, Yen FT. Purification of the apolipoprotein B-67-containing low density lipoprotein particle and its affinity for the low density lipoprotein receptor. Journal of Lipid Research. 1995;36(12):2622–2629. [PubMed] [Google Scholar]
- 32.Krul ES, Parhofer KG, Barrett PHR, Wagner RD, Schonfeld G. ApoB-75, a truncation of apolipoprotein B associated with familial hypobetalipoproteinemia: genetic and kinetic studies. Journal of Lipid Research. 1992;33(7):1037–1050. [PubMed] [Google Scholar]
- 33.Weisgraber KH. Apolipoprotein E: structure-function relationships. Advances in Protein Chemistry. 1994;45:249–302. doi: 10.1016/s0065-3233(08)60642-7. [DOI] [PubMed] [Google Scholar]
- 34.Al-Ali H, Khachfe HM. The N-terminal domain of apolipoprotein B-100: structural characterization by homology modeling. BMC Biochemistry. 2007;8, article 12 doi: 10.1186/1471-2091-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kriško A, Etchebest C. Theoretical model of human apolipoprotein B100 tertiary structure. Proteins. 2007;66(2):342–358. doi: 10.1002/prot.21229. [DOI] [PubMed] [Google Scholar]
- 36.Chen P-F, Marcel YL, Yang C-Y, et al. Primary sequence mapping of human apolipoprotein B-100 epitopes. Comparisons of trypsin accessibility and immunoreactivity and implication for apoB conformation. European Journal of Biochemistry. 1988;175(1):111–118. doi: 10.1111/j.1432-1033.1988.tb14172.x. [DOI] [PubMed] [Google Scholar]
- 37.Stocks J, Miller NE. Analysis of apolipoproteins and lipoproteins by capillary electrophoresis. Electrophoresis. 1999;20:2118–2123. doi: 10.1002/(SICI)1522-2683(19990701)20:10<2118::AID-ELPS2118>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 38.Yang C-Y, Gu Z-W, Weng S-A, et al. Structure of apolipoprotein B-100 of human low density lipoproteins. Arteriosclerosis. 1989;9(1):96–108. doi: 10.1161/01.atv.9.1.96. [DOI] [PubMed] [Google Scholar]
- 39.Thornalley PJ, Rabbani N. Detection of oxidized and glycated proteins in clinical samples using mass spectrometry—a user's perspective. Biochimica et Biophysica Acta. 2013 doi: 10.1016/j.bbagen.2013.03.025. [DOI] [PubMed] [Google Scholar]
- 40.Spickett CM, Reis A, Pitt AR. The use of narrow mass-window, high-resolution extracted product ion chromatograms for the sensitive and selective identification of protein modifications. Analytical Chemistry. 2013;85(9):4621–4627. doi: 10.1021/ac400131f. [DOI] [PubMed] [Google Scholar]
- 41.Delporte C, Van Antwerpen P, Zouaoui Boudjeltia K, et al. Optimization of apolipoprotein-B-100 sequence coverage by liquid chromatography-tandem mass spectrometry for the future study of its posttranslational modifications. Analytical Biochemistry. 2011;411(1):129–138. doi: 10.1016/j.ab.2010.11.039. [DOI] [PubMed] [Google Scholar]
- 42.Klebanoff SJ, Kettle AJ, Rosen H, Winterbourn CC, Nauseef WM. Myeloperoxidase: a front-line defender against phagocytosed microorganisms. Journal of Leukocyte Biology. 2013;93:185–198. doi: 10.1189/jlb.0712349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Klebanoff SJ. Myeloperoxidase: friend and foe. Journal of Leukocyte Biology. 2005;77(5):598–625. doi: 10.1189/jlb.1204697. [DOI] [PubMed] [Google Scholar]
- 44.Davies MJ. Myeloperoxidase-derived oxidation: mechanisms of biological damage and its prevention. Journal of Clinical Biochemistry and Nutrition. 2011;48(1):8–19. doi: 10.3164/jcbn.11-006FR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Davies MJ, Hawkins CL, Pattison DI, Rees MD. Mammalian heme peroxidases: from molecular mechanisms to health implications. Antioxidants and Redox Signaling. 2008;10(7):1199–1234. doi: 10.1089/ars.2007.1927. [DOI] [PubMed] [Google Scholar]
- 46.van der Veen BS, De Winther MPJ, Heeringa P. Myeloperoxidase: molecular mechanisms of action and their relevance to human health and disease. Antioxidants and Redox Signaling. 2009;11(11):2899–2937. doi: 10.1089/ars.2009.2538. [DOI] [PubMed] [Google Scholar]
- 47.Bainton DF, Ullyot JL, Farquhar MG. The development of neutrophilic polymorphonuclear leukocytes in human bone marrow. Journal of Experimental Medicine. 1971;134(4):907–934. doi: 10.1084/jem.134.4.907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dunn WB, Hardin JH, Spicer SS. Ultrastructural localization of myeloperoxidase in human neutrophil and rabbit heterophil and eosinophil leukocytes. Blood. 1968;32(6):935–944. [PubMed] [Google Scholar]
- 49.Furtmüller PG, Zederbauer M, Jantschko W, et al. Active site structure and catalytic mechanisms of human peroxidases. Archives of Biochemistry and Biophysics. 2006;445(2):199–213. doi: 10.1016/j.abb.2005.09.017. [DOI] [PubMed] [Google Scholar]
- 50.Banerjee S, Stampler J, Furtmüller PG, Obinger C. Conformational and thermal stability of mature dimeric human myeloperoxidase and a recombinant monomeric form from CHO cells. Biochimica et Biophysica Acta. 2011;1814(2):375–387. doi: 10.1016/j.bbapap.2010.09.015. [DOI] [PubMed] [Google Scholar]
- 51.Hansson M, Olsson I, Nauseef WM. Biosynthesis, processing, and sorting of human myeloperoxidase. Archives of Biochemistry and Biophysics. 2006;445(2):214–224. doi: 10.1016/j.abb.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 52.Van Antwerpen P, Slomianny M-C, Boudjeltia KZ, et al. Glycosylation pattern of mature dimeric leukocyte and recombinant monomeric myeloperoxidase: glycosylation is required for optimal enzymatic activity. Journal of Biological Chemistry. 2010;285(21):16351–16359. doi: 10.1074/jbc.M109.089748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fiedler TJ, Davey CA, Fenna RE. X-ray crystal structure and characterization of halide-binding sites of human myeloperoxidase at 1.8 Å resolution. Journal of Biological Chemistry. 2000;275(16):11964–11971. doi: 10.1074/jbc.275.16.11964. [DOI] [PubMed] [Google Scholar]
- 54.Blair-Johnson M, Fiedler T, Fenna R. Human myeloperoxidase: structure of a cyanide complex and its interaction with bromide and thiocyanate substrates at 1.9 Å resolution. Biochemistry. 2001;40(46):13990–13997. doi: 10.1021/bi0111808. [DOI] [PubMed] [Google Scholar]
- 55.Staudinger BJ, Oberdoerster MA, Lewis PJ, Rosen H. mRNA expression profiles for Escherichia coli ingested by normal and phagocyte oxidase-deficient human neutrophils. Journal of Clinical Investigation. 2002;110(8):1151–1163. doi: 10.1172/JCI15268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zederbauer M, Furtmüller PG, Brogioni S, Jakopitsch C, Smulevich G, Obinger C. Heme to protein linkages in mammalian peroxidases: impact on spectroscopic, redox and catalytic properties. Natural Product Reports. 2007;24(3):571–584. doi: 10.1039/b604178g. [DOI] [PubMed] [Google Scholar]
- 57.Klebanoff SJ. Myeloperoxidase-halide-hydrogen peroxide antibacterial system. Journal of Bacteriology. 1968;95(6):2131–2138. doi: 10.1128/jb.95.6.2131-2138.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Klebanoff SJ. A peroxidase-mediated antimicrobial system in leukocytes. Journal of Clinical Investigation. 1967;46:p. 1078. [Google Scholar]
- 59.Pattison DI, Davies MJ, Hawkins CL. Reactions and reactivity of myeloperoxidase-derived oxidants: differential biological effects of hypochlorous and hypothiocyanous acids. Free Radical Research. 2012;46:975–995. doi: 10.3109/10715762.2012.667566. [DOI] [PubMed] [Google Scholar]
- 60.Talib J, Pattison DI, Harmer JA, Celermajer DS, Davies MJ. High plasma thiocyanate levels modulate protein damage induced by myeloperoxidase and perturb measurement of 3-chlorotyrosine. Free Radical Biology & Medicine. 2012;53:20–29. doi: 10.1016/j.freeradbiomed.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 61.Arnhold J, Flemmig J. Human myeloperoxidase in innate and acquired immunity. Archives of Biochemistry and Biophysics. 2010;500(1):92–106. doi: 10.1016/j.abb.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 62.Odell EW, Segal AW. The bactericidal effects of the respiratory burst and the myeloperoxidase system isolated in neutrophil cytoplasts. Biochimica et Biophysica Acta. 1988;971(3):266–274. doi: 10.1016/0167-4889(88)90141-3. [DOI] [PubMed] [Google Scholar]
- 63.Brennan M-L, Penn MS, Van Lente F, et al. Prognostic value of myeloperoxidase in patients with chest pain. The New England Journal of Medicine. 2003;349(17):1595–1604. doi: 10.1056/NEJMoa035003. [DOI] [PubMed] [Google Scholar]
- 64.Baldus S, Heeschen C, Meinertz T, et al. Myeloperoxidase serum levels predict risk in patients with acute coronary syndromes. Circulation. 2003;108(12):1440–1445. doi: 10.1161/01.CIR.0000090690.67322.51. [DOI] [PubMed] [Google Scholar]
- 65.Daugherty A, Dunn JL, Rateri DL, Heinecke JW. Myeloperoxidase, a catalyst for lipoprotein oxidation, is expressed in human atherosclerotic lesions. Journal of Clinical Investigation. 1994;94(1):437–444. doi: 10.1172/JCI117342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ravandi A, Kuksis A, Shaikh NA. Glucosylated glycerophosphoethanolamines are the major LDL glycation products and increase LDL susceptibility to oxidation: evidence of their presence in atherosclerotic lesions. Arteriosclerosis, Thrombosis, and Vascular Biology. 2000;20(2):467–477. doi: 10.1161/01.atv.20.2.467. [DOI] [PubMed] [Google Scholar]
- 67.Rabbani N, Chittari MV, Bodmer CW, Zehnder D, Ceriello A, Thornalley PJ. Increased glycation and oxidative damage to apolipoprotein B100 of LDL cholesterol in patients with type 2 diabetes and effect of metformin. Diabetes. 2010;59(4):1038–1045. doi: 10.2337/db09-1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tertov VV, Kaplun VV, Sobenin IA, Orekhov AN. Low-density lipoprotein modification occurring in human plasma possible mechanism of in vivo lipoprotein desialylation as a primary step of atherogenic modification. Atherosclerosis. 1998;138(1):183–195. doi: 10.1016/s0021-9150(98)00023-9. [DOI] [PubMed] [Google Scholar]
- 69.Garner B, Harvey DJ, Royle L, et al. Characterization of human apolipoprotein B100 oligosaccharides in LDL subfractions derived from normal and hyperlipidemic plasma: deficiency of α-N-acetylneuraminyllactosyl-ceramide in light and small dense LDL particles. Glycobiology. 2001;11(10):791–802. doi: 10.1093/glycob/11.10.791. [DOI] [PubMed] [Google Scholar]
- 70.O’Brien KD, Alpers CE, Hokanson JE, Wang S, Chait A. Oxidation-specific epitopes in human coronary atherosclerosis are not limited to oxidized low-density lipoprotein. Circulation. 1996;94(6):1216–1225. doi: 10.1161/01.cir.94.6.1216. [DOI] [PubMed] [Google Scholar]
- 71.Briley-Saebo KC, Cho YS, Tsimikas S. Imaging of oxidation-specific epitopes in atherosclerosis and macrophage-rich vulnerable plaques. Current Cardiovascular Imaging Reports. 2011;4:4–16. doi: 10.1007/s12410-010-9060-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Holvoet P, De Keyzer D, Jacobs DR., Jr. Oxidized LDL and the metabolic syndrome. Future Lipidology. 2008;3(6):637–649. doi: 10.2217/17460875.3.6.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Itabe H. Oxidative modification of LDL: its pathological role in atherosclerosis. Clinical Reviews in Allergy & Immunology. 2009;37(1):4–11. doi: 10.1007/s12016-008-8095-9. [DOI] [PubMed] [Google Scholar]
- 74.Greig FH, Kennedy S, Spickett CM. Physiological effects of oxidized phospholipids and their cellular signaling mechanisms in inflammation. Free Radical Biology and Medicine. 2012;52(2):266–280. doi: 10.1016/j.freeradbiomed.2011.10.481. [DOI] [PubMed] [Google Scholar]
- 75.Hawkins CL, Pattison DI, Davies MJ. Hypochlorite-induced oxidation of amino acids, peptides and proteins. Amino Acids. 2003;25(3-4):259–274. doi: 10.1007/s00726-003-0016-x. [DOI] [PubMed] [Google Scholar]
- 76.Spickett CM, Jerlich A, Panasenko OM, et al. The reactions of hypochlorous acid, the reactive oxygen species produced by myeloperoxidase, with lipids. Acta Biochimica Polonica. 2000;47(4):889–899. [PubMed] [Google Scholar]
- 77.Kriško A, Stjepanović G, Pifat G, Ruysschaert J-M, Goormaghtigh E. Detection of apolipoprotein B100 early conformational changes during oxidation. Biochimica et Biophysica Acta. 2007;1768(11):2923–2930. doi: 10.1016/j.bbamem.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 78.Stadler N, Lindner RA, Davies MJ. Direct detection and quantification of transition metal ions in human atherosclerotic plaques: evidence for the presence of elevated levels of iron and copper. Arteriosclerosis, Thrombosis, and Vascular Biology. 2004;24(5):949–954. doi: 10.1161/01.ATV.0000124892.90999.cb. [DOI] [PubMed] [Google Scholar]
- 79.Gaut JP, Heinecke JW. Mechanisms for oxidizing low-density lipoprotein: insights from patterns of oxidation products in the artery wall and from mouse models of atherosclerosis. Trends in Cardiovascular Medicine. 2001;11(3-4):103–112. doi: 10.1016/s1050-1738(01)00101-3. [DOI] [PubMed] [Google Scholar]
- 80.Sullivan JL. Do hemochromatosis mutations protect against iron-mediated atherogenesis? Circulation. 2009;2(6):652–657. doi: 10.1161/CIRCGENETICS.109.906230. [DOI] [PubMed] [Google Scholar]
- 81.Sullivan JL. Iron in arterial plaque: a modifiable risk factor for atherosclerosis. Biochimica et Biophysica Acta. 2009;1790(7):718–723. doi: 10.1016/j.bbagen.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 82.Sullivan JL, Katz SD. Iron reduction and cardiovascular outcomes. Journal of the American Medical Association. 2007;297(19):p. 2075. doi: 10.1001/jama.297.19.2075-a. [DOI] [PubMed] [Google Scholar]
- 83.Yla-Herttuala S, Rosenfeld ME, Parthasarathy S, et al. Colocalization of 15-lipoxygenase mRNA and protein with epitopes of oxidized low density lipoprotein in macrophage-rich areas of atherosclerotic lesions. Proceedings of the National Academy of Sciences of the United States of America. 1990;87(18):6959–6963. doi: 10.1073/pnas.87.18.6959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yla-Herttuala S, Rosenfeld ME, Parthasarathy S, et al. Gene expression in macrophage-rich human atherosclerotic lesions: 15-lipoxygenase and acetyl low density lipoprotein receptor messenger RNA colocalize with oxidation specific lipid-protein adducts. Journal of Clinical Investigation. 1991;87(4):1146–1152. doi: 10.1172/JCI115111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hazen SL, Crowley JR, Mueller DM, Heinecke JW. Mass spectrometric quantification of 3-chlorotyrosine in human tissues with attomole sensitivity: a sensitive and specific marker for myeloperoxidase-catalyzed chlorination at sites of inflammation. Free Radical Biology and Medicine. 1997;23(6):909–916. doi: 10.1016/s0891-5849(97)00084-1. [DOI] [PubMed] [Google Scholar]
- 86.Hazen SL, Heinecke JW. 3-Chlorotyrosine, a specific marker of myeloperoxidase-catalyzed oxidation, is markedly elevated in low density lipoprotein isolated from human atherosclerotic intima. Journal of Clinical Investigation. 1997;99(9):2075–2081. doi: 10.1172/JCI119379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zhang R, Brennan M-L, Fu X, et al. Association between myeloperoxidase levels and risk of coronary artery disease. Journal of the American Medical Association. 2001;286(17):2136–2142. doi: 10.1001/jama.286.17.2136. [DOI] [PubMed] [Google Scholar]
- 88.Kutter D, Devaquet P, Vanderstocken G, Paulus JM, Marchal V, Gothot A. Consequences of total and subtotal myeloperoxidase deficiency: risk or benefit? Acta Haematologica. 2000;104(1):10–15. doi: 10.1159/000041062. [DOI] [PubMed] [Google Scholar]
- 89.Gröne H-J, Gröne EF, Malle E. Immunohistochemical detection of hypochlorite-modified proteins in glomeruli of human membranous glomerulonephritis. Laboratory Investigation. 2002;82(1):5–14. doi: 10.1038/labinvest.3780390. [DOI] [PubMed] [Google Scholar]
- 90.Malle E, Marsche G, Arnhold J, Davies MJ. Modification of low-density lipoprotein by myeloperoxidase-derived oxidants and reagent hypochlorous acid. Biochimica et Biophysica Acta. 2006;1761(4):392–415. doi: 10.1016/j.bbalip.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 91.Jerlich A, Pitt AR, Schaur RJ, Spickett CM. Pathways of phospholipid oxidation by HOCl in human LDL detected by LC-MS. Free Radical Biology and Medicine. 2000;28(5):673–682. doi: 10.1016/s0891-5849(99)00273-7. [DOI] [PubMed] [Google Scholar]
- 92.Hazen SL, Hsu FF, Duffin K, Heinecke JW. Molecular chlorine generated by the myeloperoxidase-hydrogen peroxide- chloride system of phagocytes converts low density lipoprotein cholesterol into a family of chlorinated sterols. Journal of Biological Chemistry. 1996;271(38):23080–23088. doi: 10.1074/jbc.271.38.23080. [DOI] [PubMed] [Google Scholar]
- 93.Carr AC, Myzak MC, Stocker R, McCall MR, Frei B. Myeloperoxidase binds to low-density lipoprotein: potential implications for atherosclerosis. FEBS Letters. 2000;487(2):176–180. doi: 10.1016/s0014-5793(00)02227-4. [DOI] [PubMed] [Google Scholar]
- 94.Sokolov AV, Ageeva KV, Cherkalina OS, et al. Identification and properties of complexes formed by myeloperoxidase with lipoproteins and ceruloplasmin. Chemistry and Physics of Lipids. 2010;163(4-5):347–355. doi: 10.1016/j.chemphyslip.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 95.Daphna E-M, Michaela S, Eynat P, Irit A, Rimon S. Association of myeloperoxidase with heparin: oxidative inactivation of proteins on the surface of endothelial cells by the bound enzyme. Molecular and Cellular Biochemistry. 1998;183(1-2):55–61. doi: 10.1023/a:1006848730927. [DOI] [PubMed] [Google Scholar]
- 96.Sokolov A, Ageeva K, Pulina M, et al. Ceruloplasmin and myeloperoxidase in complex affect the enzymatic properties of each other. Free Radical Research. 2008;42(11-12):989–998. doi: 10.1080/10715760802566574. [DOI] [PubMed] [Google Scholar]
- 97.Sokolov AV, Chekanov AV, Kostevich VA, Aksenov DV, Vasilyev VB, Panasenko OM. Revealing binding sites for myeloperoxidase on the surface of human low density lipoproteins. Chemistry and Physics of Lipids. 2011;164(1):49–53. doi: 10.1016/j.chemphyslip.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 98.Zheng L, Nukuna B, Brennan M-L, et al. Apolipoprotein A-I is a selective target for myeloperoxidase-catalyzed oxidation and function impairment in subjects with cardiovascular disease. Journal of Clinical Investigation. 2004;114(4):529–541. doi: 10.1172/JCI21109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Heinecke JW. Tyrosyl radical production by myeloperoxidase: a phagocyte pathway for lipid peroxidation and dityrosine cross-linking of proteins. Toxicology. 2002;177(1):11–22. doi: 10.1016/s0300-483x(02)00192-0. [DOI] [PubMed] [Google Scholar]
- 100.Hamilton RT, Asatryan L, Nilsen JT, et al. LDL protein nitration: implication for LDL protein unfolding. Archives of Biochemistry and Biophysics. 2008;479(1):1–14. doi: 10.1016/j.abb.2008.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nicholls SJ, Hazen SL. Myeloperoxidase, modified lipoproteins, and atherogenesis. Journal of Lipid Research. 2009;50:S346–S351. doi: 10.1194/jlr.R800086-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Nicholls SJ, Hazen SL. Myeloperoxidase and cardiovascular disease. Arteriosclerosis, Thrombosis, and Vascular Biology. 2005;25(6):1102–1111. doi: 10.1161/01.ATV.0000163262.83456.6d. [DOI] [PubMed] [Google Scholar]
- 103.Baldus S, Heitzer T, Eiserich JP, et al. Myeloperoxidase enhances nitric oxide catabolism during myocardial ischemia and reperfusion. Free Radical Biology and Medicine. 2004;37(6):902–911. doi: 10.1016/j.freeradbiomed.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 104.Baldus S, Eiserich JP, Mani A, et al. Endothelial transcytosis of myeloperoxidase confers specificity to vascular ECM proteins as targets of tyrosine nitration. Journal of Clinical Investigation. 2001;108(12):1759–1770. doi: 10.1172/JCI12617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Arnhold J, Monzani E, Furtmüller PG, Zederbauer M, Casella L, Obinger C. Kinetics and thermodynamics of halide and nitrite oxidation by mammalian heme peroxidases. European Journal of Inorganic Chemistry. 2006;(19):3801–3811. [Google Scholar]
- 106.Carr AC, Decker EA, Park Y, Frei B. Comparison of low-density lipoprotein modification by myeloperoxidase-derived hypochlorous and hypobromous acids. Free Radical Biology and Medicine. 2001;31(1):62–72. doi: 10.1016/s0891-5849(01)00552-4. [DOI] [PubMed] [Google Scholar]
- 107.Wang Z, Nicholls SJ, Rodriguez ER, et al. Protein carbamylation links inflammation, smoking, uremia and atherogenesis. Nature Medicine. 2007;13(10):1176–1184. doi: 10.1038/nm1637. [DOI] [PubMed] [Google Scholar]
- 108.Holzer M, Gauster M, Pfeifer T, et al. Protein carbamylation renders high-density lipoprotein dysfunctional. Antioxidants and Redox Signaling. 2011;14(12):2337–2346. doi: 10.1089/ars.2010.3640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Moguilevsky N, Zouaoui Boudjeltia K, Babar S, et al. Monoclonal antibodies against LDL progressively oxidized by myeloperoxidase react with ApoB-100 protein moiety and human atherosclerotic lesions. Biochemical and Biophysical Research Communications. 2004;323(4):1223–1228. doi: 10.1016/j.bbrc.2004.08.220. [DOI] [PubMed] [Google Scholar]
- 110.Vaes M, Zouaoui Boudjeltia K, Van Antwerpen P, et al. Poster Abstract: XIV International Symposium on Atherosclerosis, Th-P15:146 Low-density lipoprotein oxidation by myeloperoxidase occurs in the blood circulation during hemodialysis. Atherosclerosis Supplements. 2006;7:p. 525. [Google Scholar]
- 111.Mazière C, Mazière J-C. Activation of transcription factors and gene expression by oxidized low-density lipoprotein. Free Radical Biology and Medicine. 2009;46(2):127–137. doi: 10.1016/j.freeradbiomed.2008.10.024. [DOI] [PubMed] [Google Scholar]
- 112.Popolo A, Autore G, Pinto A, Marzocco S. Oxidative stress in patients with cardiovascular disease and chronic renal failure. Free Radical Research. 2013;47(5):346–356. doi: 10.3109/10715762.2013.779373. [DOI] [PubMed] [Google Scholar]
- 113.Chen T, Huang Z, Wang L, et al. MicroRNA-125a-5p partly regulates the inflammatory response, lipid uptake, and ORP9 expression in oxLDL-stimulated monocyte/macrophages. Cardiovascular Research. 2009;83(1):131–139. doi: 10.1093/cvr/cvp121. [DOI] [PubMed] [Google Scholar]
- 114.Moore KJ, Tabas I. Macrophages in the pathogenesis of atherosclerosis. Cell. 2011;145(3):341–355. doi: 10.1016/j.cell.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hazell LJ, Stocker R. Oxidation of low-density lipoprotein with hypochlorite causes transformation of the lipoprotein into a high-uptake form for macrophages. Biochemical Journal. 1993;290(1):165–172. doi: 10.1042/bj2900165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Podrez EA, Febbraio M, Sheibani N, et al. Macrophage scavenger receptor CD36 is the major receptor for LDL modified by monocyte-generated reactive nitrogen species. Journal of Clinical Investigation. 2000;105(10):1095–1108. doi: 10.1172/JCI8574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Podrez EA, Schmitt D, Hoff HF, Hazen SL. Myeloperoxidase-generated reactive nitrogen species convert LDL into an atherogenic form in vitro. Journal of Clinical Investigation. 1999;103(11):1547–1560. doi: 10.1172/JCI5549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Nagy L, Tontonoz P, Alvarez JGA, Chen H, Evans RM. Oxidized LDL regulates macrophage gene expression through ligand activation of PPARγ . Cell. 1998;93(2):229–240. doi: 10.1016/s0092-8674(00)81574-3. [DOI] [PubMed] [Google Scholar]
- 119.Tontonoz P, Nagy L, Alvarez JGA, Thomazy VA, Evans RM. PPARγ promotes monocyte/macrophage differentiation and uptake of oxidized LDL. Cell. 1998;93(2):241–252. doi: 10.1016/s0092-8674(00)81575-5. [DOI] [PubMed] [Google Scholar]
- 120.Westendorf T, Graessler J, Kopprasch S. Hypochlorite-oxidized low-density lipoprotein upregulates CD36 and PPARγ mRNA expression and modulates SR-BI gene expression in murine macrophages. Molecular and Cellular Biochemistry. 2005;277(1-2):143–152. doi: 10.1007/s11010-005-5873-z. [DOI] [PubMed] [Google Scholar]
- 121.Carr AC. Hypochlorous acid-modified low-density lipoprotein inactivates the lysosomal protease cathepsin B: Protection by ascorbic and lipoic acids. Redox Report. 2001;6(6):343–349. doi: 10.1179/135100001101536526. [DOI] [PubMed] [Google Scholar]
- 122.Vicca S, Hennequin C, Nguyen-Khoa T, et al. Caspase-dependent apoptosis in THP-1 cells exposed to oxidized low-density lipoproteins. Biochemical and Biophysical Research Communications. 2000;273(3):948–954. doi: 10.1006/bbrc.2000.3017. [DOI] [PubMed] [Google Scholar]
- 123.Boudjeltia KZ, Legssyer I, Van Antwerpen P, et al. Triggering of inflammatory response by myeloperoxidase-oxidized LDL. Biochemistry and Cell Biology. 2006;84(5):805–812. doi: 10.1139/o06-061. [DOI] [PubMed] [Google Scholar]
- 124.Baumann H, Gauldie J. The acute phase response. Immunology Today. 1994;15(2):74–80. doi: 10.1016/0167-5699(94)90137-6. [DOI] [PubMed] [Google Scholar]
- 125.Chen X-L, Varner SE, Rao AS, et al. Laminar flow induction of antioxidant response element-mediated genes in endothelial cells: a novel anti-inflammatory mechanism. Journal of Biological Chemistry. 2003;278(2):703–711. doi: 10.1074/jbc.M203161200. [DOI] [PubMed] [Google Scholar]
- 126.Calay D, Rousseau A, Mattart L, et al. Copper and myeloperoxidase-modified LDLs activate Nrf2 through different pathways of ros production in macrophages. Antioxidants and Redox Signaling. 2010;13(10):1491–1502. doi: 10.1089/ars.2009.2971. [DOI] [PubMed] [Google Scholar]
- 127.Akiba S, Yoneda Y, Ohno S, Nemoto M, Sato T. Oxidized LDL activates phospholipase A2 to supply fatty acids required for cholesterol esterification. Journal of Lipid Research. 2003;44(9):1676–1685. doi: 10.1194/jlr.M300012-JLR200. [DOI] [PubMed] [Google Scholar]
- 128.Bea F, Hudson FN, Chait A, Kavanagh TJ, Rosenfeld ME. Induction of glutathione synthesis in macrophages by oxidized low-density lipoproteins is mediated by consensus antioxidant response elements. Circulation Research. 2003;92(4):386–393. doi: 10.1161/01.RES.0000059561.65545.16. [DOI] [PubMed] [Google Scholar]
- 129.Maruyama A, Tsukamoto S, Nishikawa K, et al. Nrf2 regulates the alternative first exons of CD36 in macrophages through specific antioxidant response elements. Archives of Biochemistry and Biophysics. 2008;477(1):139–145. doi: 10.1016/j.abb.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 130.Liu Q, Dai Z, Liu Z, et al. Oxidized low-density lipoprotein activates adipophilin through ERK1/2 signal pathway in RAW264.7 cells. Acta Biochimica et Biophysica Sinica. 2010;42(9):635–645. doi: 10.1093/abbs/gmq070. [DOI] [PubMed] [Google Scholar]
- 131.Kensler TW, Wakabayashi N, Biswal S. Cell survival responses to environmental stresses via the Keap1-Nrf2-ARE pathway. Annual Review of Pharmacology and Toxicology. 2007;47:89–116. doi: 10.1146/annurev.pharmtox.46.120604.141046. [DOI] [PubMed] [Google Scholar]
- 132.Pennathur S, Heinecke JW. Oxidative stress and endothelial dysfunction in vascular disease. Current Diabetes Reports. 2007;7(4):257–264. doi: 10.1007/s11892-007-0041-3. [DOI] [PubMed] [Google Scholar]
- 133.Adachi H, Tsujimoto M. Endothelial scavenger receptors. Progress in Lipid Research. 2006;45(5):379–404. doi: 10.1016/j.plipres.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 134.Marsche G, Zimmermann R, Horiuchi S, Tandon NN, Sattler W, Malle E. Class B scavenger receptors CD36 and SR-BI are receptors for hypochlorite-modified low density lipoprotein. Journal of Biological Chemistry. 2003;278(48):47562–47570. doi: 10.1074/jbc.M308428200. [DOI] [PubMed] [Google Scholar]
- 135.Claise C, Edeas M, Chalas J, et al. Oxidized low-density lipoprotein induces the production of interleukin-8 by endothelial cells. FEBS Letters. 1996;398(2-3):223–227. doi: 10.1016/s0014-5793(96)01255-0. [DOI] [PubMed] [Google Scholar]
- 136.Woenckhaus C, Kaufmann A, Bußfeld D, Gemsa D, Sprenger H, Gröne H-J. Hypochlorite-modified LDL: chemotactic potential and chemokine induction in human monocytes. Clinical Immunology and Immunopathology. 1998;86(1):27–33. doi: 10.1006/clin.1997.4453. [DOI] [PubMed] [Google Scholar]
- 137.Cesarman-Maus G, Hajjar KA. Molecular mechanisms of fibrinolysis. British Journal of Haematology. 2005;129(3):307–321. doi: 10.1111/j.1365-2141.2005.05444.x. [DOI] [PubMed] [Google Scholar]
- 138.Astrup T. The biological significance of fibrinolysis. The Lancet. 1956;268(6942):565–568. doi: 10.1016/s0140-6736(56)92048-7. [DOI] [PubMed] [Google Scholar]
- 139.Sueishi K, Ichikawa K, Kato K, Nakagawa K, Chen Y-X. Atherosclerosis: coagulation and fibrinolysis. Seminars in Thrombosis and Hemostasis. 1998;24(3):255–260. doi: 10.1055/s-2007-995851. [DOI] [PubMed] [Google Scholar]
- 140.Mayerl C, Lukasser M, Sedivy R, Niederegger H, Seiler R, Wick G. Atherosclerosis research from past to present—on the track of two pathologists with opposing views, Carl von Rokitansky and Rudolf Virchow. Virchows Archiv. 2006;449(1):96–103. doi: 10.1007/s00428-006-0176-7. [DOI] [PubMed] [Google Scholar]
- 141.Zouaoui Boudjeltia K, Guillaume M, Henuzet C, et al. Fibrinolysis and cardiovascular risk factors: association with fibrinogen, lipids, and monocyte count. European Journal of Internal Medicine. 2006;17(2):102–108. doi: 10.1016/j.ejim.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 142.Zouaoui Boudjeltia K, Daher J, Van Antwerpen P, et al. Exposure of endothelial cells to physiological levels of myeloperoxidase-modified LDL delays pericellular fibrinolysis. PLoS ONE. 2012;7 doi: 10.1371/journal.pone.0038810.e38810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Boudjeltia KZ, Cauchie P, Remacle C, et al. A new device for measurement of fibrin clot lysis: application to the euglobulin clot lysis time. BMC Biotechnology. 2002;2(1, article 8) doi: 10.1186/1472-6750-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Strobel NA, Fassett RG, Marsh SA, Coombes JS. Oxidative stress biomarkers as predictors of cardiovascular disease. International Journal of Cardiology. 2011;147(2):191–201. doi: 10.1016/j.ijcard.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 145.Tsimikas S, Miller YI. Oxidative modification of lipoproteins: mechanisms, role in inflammation and potential clinical applications in cardiovascular disease. Current Pharmaceutical Design. 2011;17(1):27–37. doi: 10.2174/138161211795049831. [DOI] [PubMed] [Google Scholar]
- 146.Brennan M-L, Gaur A, Pahuja A, Lusis AJ, Reynolds WF. Mice lacking myeloperoxidase are more susceptible to experimental autoimmune encephalomyelitis. Journal of Neuroimmunology. 2001;112(1-2):97–105. doi: 10.1016/s0165-5728(00)00392-1. [DOI] [PubMed] [Google Scholar]
- 147.Himmelfarb J, Ikizler TA. Medical progress: hemodialysis. The New England Journal of Medicine. 2010;363(19):1833–1845. doi: 10.1056/NEJMra0902710. [DOI] [PubMed] [Google Scholar]
- 148.Libetta C, Sepe V, Esposito P, Galli F, Dal Canton A. Oxidative stress and inflammation: implications in uremia and hemodialysis. Clinical Biochemistry. 2011;44(14-15):1189–1198. doi: 10.1016/j.clinbiochem.2011.06.988. [DOI] [PubMed] [Google Scholar]
- 149.Borawski J. Myeloperoxidase as a marker of hemodialysis biocompatibility and oxidative stress: the underestimated modifying effects of heparin. American Journal of Kidney Diseases. 2006;47(1):37–41. doi: 10.1053/j.ajkd.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 150.Nikpoor B, Turecki G, Fournier C, Théroux P, Rouleau GA. A functional myeloperoxidase polymorphic variant is associated with coronary artery disease in French-Canadians. American Heart Journal. 2001;142(2):336–339. doi: 10.1067/mhj.2001.116769. [DOI] [PubMed] [Google Scholar]
- 151.Malle E, Buch T, Grone H-J. Myeloperoxidase in kidney disease. Kidney International. 2003;64(6):1956–1967. doi: 10.1046/j.1523-1755.2003.00336.x. [DOI] [PubMed] [Google Scholar]
- 152.Hillegass LM, Griswold DE, Brickson B, Albrightson-Winslow C. Assessment of myeloperoxidase activity in whole rat kidney. Journal of Pharmacological Methods. 1990;24(4):285–295. doi: 10.1016/0160-5402(90)90013-b. [DOI] [PubMed] [Google Scholar]
- 153.Rutgers A, Heeringa P, Kooman JP, Van Der Sande FM, Tervaert JWC. Peripheral blood myeloperoxidase activity increases during hemodialysis. Kidney International. 2003;64(2):p. 760. doi: 10.1046/j.1523-1755.2003.00139.x. [DOI] [PubMed] [Google Scholar]
- 154.Wu C-C, Chen J-S, Wu W-M, et al. Myeloperoxidase serves as a marker of oxidative stress during single haemodialysis session using two different biocompatible dialysis membranes. Nephrology Dialysis Transplantation. 2005;20:1134–1139. doi: 10.1093/ndt/gfh764. [DOI] [PubMed] [Google Scholar]
- 155.Himmelfarb J, McMenamin ME, Loseto G, Heinecke JW. Myeloperoxidase-catalyzed 3-chlorotyrosine formation in dialysis patients. Free Radical Biology and Medicine. 2001;31(10):1163–1169. doi: 10.1016/s0891-5849(01)00697-9. [DOI] [PubMed] [Google Scholar]
- 156.Delporte C, Franck T, Noyon C, et al. Simultaneous measurement of protein-bound 3-chlorotyrosine and homocitrulline by LC-MS/MS after hydrolysis assisted by microwave: application to the study of myeloperoxidase activity during hemodialysis. Talanta. 2012;99:603–609. doi: 10.1016/j.talanta.2012.06.044. [DOI] [PubMed] [Google Scholar]
- 157.Franck T, Kohnen S, Boudjeltia KZ, et al. A new easy method for specific measurement of active myeloperoxidase in human biological fluids and tissue extracts. Talanta. 2009;80(2):723–729. doi: 10.1016/j.talanta.2009.07.052. [DOI] [PubMed] [Google Scholar]
- 158.Wehrens SM, Hampton SM, Kerkhofs M, Skene DJ. Mood, alertness, and performance in response to sleep deprivation and recovery sleep in experienced shiftworkers versus non-shiftworkers. Chronobiology International. 2012;29:537–548. doi: 10.3109/07420528.2012.675258. [DOI] [PubMed] [Google Scholar]
- 159.Kerkhofs M, Boudjeltia KZ. From total sleep deprivation to cardiovascular disease: a key role for the immune system? Sleep. 2012;35:895–896. doi: 10.5665/sleep.1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Spiegel K, Tasali E, Leproult R, Van Cauter E. Effects of poor and short sleep on glucose metabolism and obesity risk. Nature Reviews Endocrinology. 2009;5(5):253–261. doi: 10.1038/nrendo.2009.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Faraut B, Boudjeltia KZ, Vanhamme L, Kerkhofs M. Immune, inflammatory and cardiovascular consequences of sleep restriction and recovery. Sleep Medicine Reviews. 2012;16(2):137–149. doi: 10.1016/j.smrv.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 162.Nagai M, Hoshide S, Kario K. Sleep duration as a risk factor for cardiovascular disease—a review of the recent literature. Current Cardiology Reviews. 2010;6(1):54–61. doi: 10.2174/157340310790231635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. Journal of Sleep Research. 2009;18(2):148–158. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 164.van Leeuwen WMA, Lehto M, Karisola P, et al. Sleep restriction increases the risk of developing cardiovascular diseases by augmenting proinflammatory responses through IL-17 and CRP. PLoS ONE. 2009;4(2) doi: 10.1371/journal.pone.0004589.e4589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ackermann K, Revell VL, Lao O, Rombouts EJ, Skene DJ, Kayser M. Diurnal rhythms in blood cell populations and the effect of acute sleep deprivation in healthy young men. Sleep. 2012;35:933–940. doi: 10.5665/sleep.1954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Faraut B, Boudjeltia KZ, Dyzma M, et al. Benefits of napping and an extended duration of recovery sleep on alertness and immune cells after acute sleep restriction. Brain, Behavior, and Immunity. 2011;25(1):16–24. doi: 10.1016/j.bbi.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 167.Lange T, Born J. The immune recovery function of sleep—tracked by neutrophil counts. Brain, Behavior, and Immunity. 2011;25(1):14–15. doi: 10.1016/j.bbi.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 168.Boudjeltia K, Faraut B, Esposito MJ, et al. Temporal dissociation between myeloperoxidase (MPO)-modified LDL and MPO elevations during chronic sleep restriction and recovery in healthy young men. PLoS ONE. 2011;6(11) doi: 10.1371/journal.pone.0028230.e28230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Irwin M, Thompson J, Miller C, Gillin JC, Ziegler M. Effects of sleep and sleep deprivation on catecholamine and interleukin-2 levels in humans: clinical implications. Journal of Clinical Endocrinology and Metabolism. 1999;84(6):1979–1985. doi: 10.1210/jcem.84.6.5788. [DOI] [PubMed] [Google Scholar]
- 170.Bleeke T, Zhang H, Madamanchi N, Patterson C, Faber JE. Catecholamine-induced vascular wall growth is dependent on generation of reactive oxygen species. Circulation Research. 2004;94(1):37–45. doi: 10.1161/01.RES.0000109412.80157.7D. [DOI] [PubMed] [Google Scholar]
- 171.Ahmed MH, Barakat S, Almobarak AO. Nonalcoholic fatty liver disease and cardiovascular disease: has the time come for cardiologists to be hepatologists? Journal of Obesity. 2012;2012:9 pages. doi: 10.1155/2012/483135.483135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Musso G, Cassader M, Olivetti C, Rosina F, Carbone G, Gambino R. Association of obstructive sleep apnoea with the presence and severity of non-alcoholic fatty liver disease. A systematic review and meta-analysis. Obesity Reviews. 2013;14:417–431. doi: 10.1111/obr.12020. [DOI] [PubMed] [Google Scholar]
- 173.Muhidin SO, Magan AA, Osman KA, Syed S, Ahmed MH. The relationship between nonalcoholic fatty liver disease and colorectal cancer: the future challenges and outcomes of the metabolic syndrome. Journal of Obesity. 2012;2012 doi: 10.1155/2012/637538.637538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Rensen SS, Slaats Y, Nijhuis J, et al. Increased hepatic myeloperoxidase activity in obese subjects with nonalcoholic steatohepatitis. American Journal of Pathology. 2009;175(4):1473–1482. doi: 10.2353/ajpath.2009.080999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Rensen SS, Bieghs V, Xanthoulea S, et al. Neutrophil-derived myeloperoxidase aggravates non-alcoholic steatohepatitis in low-density lipoprotein receptor-deficient mice. PLoS ONE. 2012;7 doi: 10.1371/journal.pone.0052411.e52411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Sin DD, Paul Man SF. Why are patients with chronic obstructive pulmonary disease at increased risk of cardiovascular diseases? The potential role of systemic inflammation in chronic obstructive pulmonary disease. Circulation. 2003;107(11):1514–1519. doi: 10.1161/01.cir.0000056767.69054.b3. [DOI] [PubMed] [Google Scholar]
- 177.Mannino DM, Buist AS, Petty TL, Enright PL, Redd SC. Lung function and mortality in the United States: data from the First National Health and Nutrition Examination Survey follow up study. Thorax. 2003;58(5):388–393. doi: 10.1136/thorax.58.5.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.McGarvey LP, John M, Anderson JA, Zvarich M, Wise RA. Ascertainment of cause-specific mortality in COPD: operations of the TORCH Clinical Endpoint Committee. Thorax. 2007;62(5):411–415. doi: 10.1136/thx.2006.072348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Zouaoui Boudjeltia K, Tragas G, Babar S, et al. Effects of oxygen therapy on systemic inflammation and myeloperoxidase modified LDL in hypoxemic COPD patients. Atherosclerosis. 2009;205(2):360–362. doi: 10.1016/j.atherosclerosis.2009.01.028. [DOI] [PubMed] [Google Scholar]
- 180.Bratel T, Wennlund A, Carlström K. Impact of hypoxaemia on neuroendocrine function and catecholamine secretion in chronic obstructive pulmonary disease (COPD). Effects of long-term oxygen treatment. Respiratory Medicine. 2000;94(12):1221–1228. doi: 10.1053/rmed.2000.0953. [DOI] [PubMed] [Google Scholar]
- 181.Christ GJ, Lue T. Physiology and biochemistry of erections. Endocrine. 2004;23(2-3):93–100. doi: 10.1385/ENDO:23:2-3:093. [DOI] [PubMed] [Google Scholar]
- 182.Kirby M, Jackson G, Simonsen U. Endothelial dysfunction links erectile dysfunction to heart disease. International Journal of Clinical Practice. 2005;59(2):225–229. doi: 10.1111/j.1742-1241.2005.00453.x. [DOI] [PubMed] [Google Scholar]
- 183.Saltzman EA, Guay AT, Jacobson J. Improvement in erectile function in men with organic erectile dysfunction by correction of elevated cholesterol levels: a clinical observation. The Journal of Urology. 2004;172(1):255–258. doi: 10.1097/01.ju.0000132368.10458.66. [DOI] [PubMed] [Google Scholar]
- 184.Roumeguère T, Wespes E, Carpentier Y, Hoffmann P, Schulman CC. Erectile dysfunction is associated with a high prevalence of hyperlipidemia and coronary heart disease risk. European Urology. 2003;44(3):355–359. doi: 10.1016/s0302-2838(03)00306-3. [DOI] [PubMed] [Google Scholar]
- 185.Ponholzer A, Temml C, Obermayr R, Wehrberger C, Madersbacher S. Is erectile dysfunction an indicator for increased risk of coronary heart disease and stroke? European Urology. 2005;48(3):512–518. doi: 10.1016/j.eururo.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 186.Vlachopoulos C, Rokkas K, Ioakeimidis N, et al. Prevalence of asymptomatic coronary artery disease in men with vasculogenic erectile dysfunction: a prospective angiographic study. European Urology. 2005;48(6):996–1003. doi: 10.1016/j.eururo.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 187.Nuszkowski A, Gräbner R, Marsche G, Unbehaun A, Malle E, Heller R. Hypochlorite-modified low density lipoprotein inhibits nitric oxide synthesis in endothelial cells via an intracellular dislocalization of endothelial nitric-oxide synthase. Journal of Biological Chemistry. 2001;276(17):14212–14221. doi: 10.1074/jbc.M007659200. [DOI] [PubMed] [Google Scholar]
- 188.Zouaoui Boudjeltia K, Roumeguere T, Delree P, et al. Presence of LDL modified by myeloperoxidase in the penis in patients with vascular erectile dysfunction: a Preliminary Study. European Urology. 2007;51(1):262–269. doi: 10.1016/j.eururo.2006.08.040. [DOI] [PubMed] [Google Scholar]
- 189.Roumeguère T, Boudjeltia KZ, Vanhaeverbeek M. Effect of LDL modified by myeloperoxidase-H2O2-Cl- system on intracellular cyclic guanosine monophosphate level of endothelial cells: a link to erectile dysfunction? European Urology. 2009;55(3):754–755. doi: 10.1016/j.eururo.2008.09.038. [DOI] [PubMed] [Google Scholar]
- 190.Perimenis P, Roumeguere T, Heidler H, Roos E, Belger M, Schmitt H. Evaluation of patient expectations and treatment satisfaction after 1-year Tadalafil therapy for erectile dysfunction: the DETECT study. Journal of Sexual Medicine. 2009;6(1):257–267. doi: 10.1111/j.1743-6109.2008.01027.x. [DOI] [PubMed] [Google Scholar]
- 191.Roumeguère T, Verheyden B, Arver S, Bitton A, Belger M, Schmitt H. Therapeutic response after first month of tadalafil treatment predicts 12 months treatment continuation in patients with erectile dysfunction: results from the DETECT study. Journal of Sexual Medicine. 2008;5(7):1708–1719. doi: 10.1111/j.1743-6109.2008.00790.x. [DOI] [PubMed] [Google Scholar]
- 192.Verheyden B, Roumeguère T, Bitton A, Belger M, Schmitt H. Effects of 12-month tadalafil therapy for erectile dysfunction on couple relationships: results from the DETECT study. Journal of Sexual Medicine. 2009;6(12):3458–3468. doi: 10.1111/j.1743-6109.2009.01527.x. [DOI] [PubMed] [Google Scholar]
- 193.Roumeguère T, Zouaoui Boudjeltia K, Babar S, et al. Effects of phosphodiesterase inhibitors on the inflammatory response of endothelial cells stimulated by myeloperoxidase-modified low-density lipoprotein or tumor necrosis factor alpha. European Urology. 2010;57(3):522–529. doi: 10.1016/j.eururo.2009.01.030. [DOI] [PubMed] [Google Scholar]


