Abstract
Perinatal depression is a prevalent and detrimental condition. Determining modifiable factors associated with it would identify opportunities for prevention. This paper: 1) identifies depressive symptom trajectories and heterogeneity in those trajectories during pregnancy through the first year postpartum, and 2) examines the association between unintended pregnancy and depressive symptoms. Depressive symptoms (BDI-II) were collected from low-income Hispanic immigrants (n= 215) 5 times from early pregnancy to 12 months postpartum. The sample was at high-risk for perinatal depression and recruited from two prenatal care settings. Growth mixture modeling (GMM) was used to identify distinct trajectories of depressive symptoms over the perinatal period. Multinomial logistic regression was then conducted to examine the association between unintended pregnancy (reported at baseline) and the depression trajectory patterns. Three distinct trajectory patterns of depressive symptoms were identified: high during pregnancy, but low postpartum (“Pregnancy High”: 9.8%); borderline during pregnancy, with a postpartum increase (“Postpartum High”: 10.2%); and low throughout pregnancy and postpartum (“Perinatal Low”: 80.0%). Unintended pregnancy was not associated with the “Pregnancy High” pattern, but was associated with a marginally significant nearly 4-fold increase in risk of the “Postpartum High” pattern in depressive symptoms (RRR= 3.95, p<0.10). Family planning is a potential strategy for the prevention of postpartum depression. Women who report unintended pregnancies during prenatal care must be educated of their increased risk, even if they do not exhibit antenatal depressive symptoms. Routine depression screening should occur postpartum and referral to culturally appropriate treatment should follow positive screening results.
Keywords: Depression, Pregnancy, Hispanic, Latina, Growth mixture modeling
Background
Perinatal Depression
Major depression in the perinatal period (pregnancy through 12 months postpartum) is one of the most common health problems experienced by new mothers, with a 10–15% prevalence (Gavin et al., 2005; O'Hara & Swain, 1996). There are several known risk factors for perinatal and postpartum depression, including a prior history of psychopathology, stressful life events, poor social support, low relationship quality, and pregnancy/obstetric complications (Cooper & Murray, 1998; O'Hara, 1997). Prevalence is estimated to be higher among low-income women (Bennett, Einarson, Taddio, Koren, & Einarson, 2004; Hobfoll, Ritter, Lavin, Hulsizer, & Cameron, 1995; Holzman et al., 2006). The literature is mixed regarding ethnic disparities in postpartum depression between Hispanic and non-Hispanic white women, with some studies finding lower perinatal depression prevalence among Hispanics (Segre, Losch, & O'Hara, 2006), others finding higher depressive symptoms among Hispanics (Howell, Mora, Horowitz, & Leventhal, 2005; Rich-Edwards et al., 2006), and still other studies finding no differences by ethnicity (Yonkers et al., 2001).
There is considerable heterogeneity in the onset (prenatal or postpartum) and duration of perinatal depression, which has implications for preventive and treatment interventions as well as when and who should screen women (Henshaw & Elliott, 2005; Yonkers et al., 2001). Longitudinal studies during the perinatal period are important for examining these differences and informing decisions about when screening and interventions would be most effective and for which groups of women. Interventions for the prevention (versus screening and treatment) of perinatal depression have been the topic of recent studies (Austin, 2003; Lara, Navarro, & Navarrete, 2010; Le, Perry, & Stuart, in press; Zlotnick, Miller, Pearlstein, Howard, & Sweeney, 2006). The identification of modifiable risk factors (such as pregnancy intention) that precede and are associated with perinatal depression would offer another possible entry point for prevention.
Unintended Pregnancy
Population-based surveys, such as the National Survey of Family Growth, routinely measure pregnancy intention, operationalized as whether a woman wanted to get pregnant at the time of conception (intended), later (mistimed) or not at all (unwanted). A pregnancy is conventionally defined as unintended if the woman reports it was either mistimed or unwanted. Nearly half of all pregnancies in the U.S. are unintended, with the highest rates among young women, unmarried women, cohabiting women, lower income women, less educated women, and Black and Hispanic women (Finer & Henshaw, 2006). Unintended pregnancy rates among poor Hispanic women are more than 3 times higher than the national average (Finer & Henshaw, 2006).
Unintended pregnancy has been associated with perinatal depression in cross-sectional studies (Barber, Axinn, & Thornton, 1999; Lau & Keung, 2007; Nakku, Nakasi, & Mirembe, 2006; Orr & Miller, 1997), but no known longitudinal studies exist in which temporality can be determined (i.e., Does unintended pregnancy lead to perinatal depression, or are depressed women more likely to have an unintended pregnancy?). There are plausible hypotheses for the association in both directions. In the first case, an unintended pregnancy could lead to depression via the stress associated with the unexpectedness of the situation, deciding whether to terminate the pregnancy and determining how a child will fit into a life context of a woman who was, by definition, not prepared for a child, for situational, emotional, and/or financial reasons. On the other hand, it is possible the association occurs in the other direction, where a woman who is already depressed is more likely to experience an unintended pregnancy, likely mediated by birth control use behaviors. It is plausible that depressed women are less likely to be able to maintain a consistent birth control method, for example, forgetting to take a daily pill, being unable to make and attend monthly appointments for birth control injections, or lacking the self-efficacy to negotiate condom use at each sex episode. Establishing directionality and causality of this association would require data on pregnancy intention and repeated measures of depressive symptoms beginning prior to the pregnancy and continuing through the postpartum period.
Whether depression is a precursor to or an outcome of unintended pregnancy is important knowledge for clinicians and public health professionals in terms of designing prevention strategies. If depression is a precursor to unintended pregnancy, it implies a need for identifying depressed women prior to pregnancy during routine gynecological care; these women could be offered contraceptive counseling that stresses the impact of mental health on family planning, contraceptive use and other health behaviors. If depression is a consequence of unintended pregnancy, it implies a need for mental health screening and counseling of women presenting in prenatal care with unintended pregnancies and an increased emphasis on family planning as a strategy to prevent perinatal depression.
In the absence of data on depression pre-conception, growth mixture modeling (GMM) is a useful method for examining the heterogeneity of perinatal depression, as it can identify different longitudinal trajectory patterns (e.g., increasing, decreasing, consistently high or low) of a repeated measure (in this case depressive symptom levels; Muthen, 2004). GMM can also be used to identify significant predictors and outcomes of a particular trajectory pattern. If women with unintended pregnancies demonstrate a stronger increase in depressive symptoms over the course of the perinatal period, relative to those with intended pregnancies, this would provide some evidence for the depression-as-consequence hypothesis. However, if women with unintended pregnancies demonstrate chronically high or decreasing depression, relative to women with intended pregnancies, there is no support for that hypothesis. Therefore, the aims of this paper are: 1) to determine depressive symptom trajectories and heterogeneity in these trajectories during pregnancy through the first year postpartum, and 2) to examine the association between unintended pregnancy and depressive symptoms. We take advantage of an existing sample of Hispanic immigrant women at higher risk for perinatal depression so that there would be sufficient women with elevated depressive symptoms to identify different trajectories and their association with pregnancy intendedness.
Methods
Sample
This secondary analysis uses data from Mamás y Bebés: Proyecto del Estado de Ánimo y la Salud /Mothers and Babies: Mood and Health Project, a randomized controlled trial of a preventive intervention for perinatal depression (Le et al., in press). The study was approved by the George Washington University IRB and women provided informed consent prior to randomization. At baseline, a total of 217 low-income pregnant Hispanic women were enrolled in the prevention trial and randomized to either usual prenatal care or prenatal care plus an eight-week cognitive behavioral therapy class to prevent perinatal depression. Participants were recruited from two prenatal care clinics serving low-income clients in an urban setting. Women were eligible for enrollment if they were 18–35 years old, Hispanic, no more than 24 weeks gestation, and at high risk for major depressive episode in the perinatal period (i.e., CES-D≥16 during pregnancy and/or a history of major depression; Le, Muñoz, Soto, Delucchi, & Ippen, 2004), but not currently depressed. Women were excluded if they reported smoking, drinking alcohol or using illicit drugs. Additionally, they were excluded and referred for treatment if they met clinical criteria for major depression or other major mental disorders, and/or had other significant psychosocial problems (e.g., homelessness). While it is important to study the differences in depressive symptoms between U.S.- and foreign-born Hispanics, the parent sample included only 2 U.S.-born women, making analyses by immigrant status impossible. The 2 U.S.-born women were excluded from this analysis to create a more culturally homogenous sample of immigrants.
Data on participants’ mental health were gathered at two time points in pregnancy (pre and post intervention; mean=18 and 28 weeks gestation) and three follow-ups at 6 weeks, 4 months, and 12 months postpartum. Depressive symptoms differed significantly between the intervention and control groups only at time 2, the post-intervention time point, but no other times at follow-up (Le et al., in press). For this secondary analysis, intervention and control groups were analyzed together; however, to ensure that the current analysis is not affected by the use of intervention data, randomization status was controlled for in all multivariate models. The present secondary data analysis was approved by the Johns Hopkins School of Public Health IRB and includes only foreign-born participants (n= 215).
Measures
Dependent variable: At each of the 5 study visits over the perinatal period, participants were screened for depressive symptoms using the Spanish-language Beck Depression Inventory-II (BDI-II; Beck, Steer, Ball, & Ranieri, 1996), a 21-item self-report instrument that measures severity of depressive symptoms during the prior two-weeks. Scores greater than 13 are considered to be ‘depressive’ (14–19: mild, 20–28 moderate, 29–63: severe symptoms; Beck, Steer, & Brown, 1996). However, because the BDI-II includes questions about somatic symptoms that are normally seen in pregnant women (e.g., loss of energy, changes in appetite, tiredness), researchers recommend increasing this cut-off to 16 when measuring depressive symptoms in pregnancy (Holcomb, Stone, Lustman, Gavard, & Mostello, 1996; Salamero, Marcos, Gutierrez, & Rebull, 1994). We follow that recommendation here. The BDI-II, like its precursor the BDI, is a widely used measure in community and ethnically diverse samples, including Hispanic samples, with good psychometric properties (Beck, Steer, & Garbin, 1988; Bonicatto, Dew, & Soria, 1998; Penley, Wiebe, & Nwosu, 2003; Wiebe & Penley, 2005).
Independent variable: Pregnancy intention was measured at baseline (≤24 weeks gestation; mean = 18 weeks gestation) using a question derived from the National Survey of Family Growth: “In regard to your pregnancy, which of the following would you say? I was trying to get pregnant, I wanted to get pregnant but not at the present time, or I did not want to get pregnant” (translated from Spanish). The response categories correspond to the typically defined categories of intended, mistimed, and unwanted pregnancy, respectively. Descriptive statistics are presented by these 3 response options. However, to maximize statistical power in the analyses presented here, mistimed and unwanted pregnancies were collapsed into a single unintended category, as is commonly done (Santelli et al., 2003). Covariates: Demographic and social characteristics measured at baseline and adjusted for in multivariate models were chosen based on associations identified in prior literature. These variables included: maternal education, parity, years in the U.S., health insurance status, social support, lifetime history of physical or sexual abuse, and lifetime history of major depression. Social support was measured using a modified version of the Social Support Apgar (SSA; Norwood, 1996), which was developed specifically for use during pregnancy. This scale assesses social support along various domains (adaptation, partnership, growth, affection, resolve) and providers (baby’s father, mother, father, other family, friends, others). Scores are summed, with greater scores indicating more social support. Internal reliability was high in three psychometric studies (Cronbach’s α’s ranged from 0.88 to 0.93), and social support was shown to be negatively associated with life stress (Norwood, 1996). In the present sample, internal reliability of the SSA was similarly high (Cronbach’s α = 0.94). Because social support was highly correlated with marital/partner status, marital status was excluded from the multivariate models. Over two-thirds of the sample was either married or cohabiting with a partner.
Analysis
Analysis occurred in two stages. First, we used growth mixture modeling (GMM) to identify distinct patterns (“latent classes”) in depressive symptom trajectories during the perinatal period. GMM was fitted with Mplus version 5.2 software (Muthen & Muthen, 2007). Models with 1 to 5 classes were tested, and the most appropriate model was selected based on the lowest information criteria (BIC and ABIC), a high entropy (close to 1.0), a statistically significant bootstrapped likelihood ratio test, and no classes consisting of less than 5% of the sample (Muthen, 2004). Model fit statistics indicated that a quadratic model was more appropriate than a linear model and thus all models were fitted with a quadratic term for time. Once the final GMM was fitted, each individual participant was assigned to the depression class that their unique symptom trajectory had the highest probability of matching.
In the second stage of analysis, multinomial logistic regressions were performed using depression class as a categorical outcome variable and unintended pregnancy as the primary independent variable of interest. Three models were run, where model 1 was an unadjusted analysis, model 2 controlled for demographic variables (maternal education, parity, years in the U.S., and health insurance status as a proxy for socioeconomic status), and model 3 controlled for demographics plus psychosocial factors (social support, history of depression, and history of physical and/or sexual abuse). Covariates were identified a priori based on previous research on depression and unintended pregnancy, as discussed in the introduction. Where there were sets of potential confounders that were highly correlated (e.g., parity and maternal age; marital/partner status and social support), only one variable was included in the model. Models 2 and 3 also controlled for randomization to the intervention that was a part of the parent study.
Results
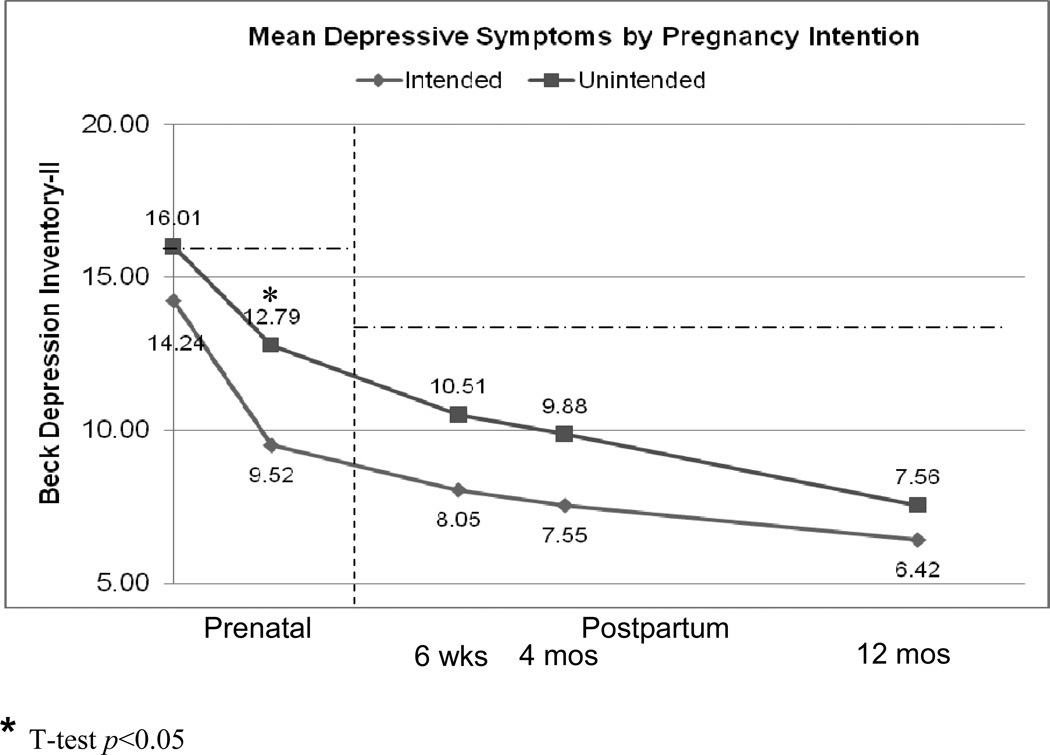
The sample consisted of 215 young (M = 25.4 years, SD = 4.6), recent immigrant women (M = 4.1 years in the U.S., SD = 4.3), predominantly from Central America (54.9% from El Salvador, 22.8% other Central American). Most were married (16.7%) or cohabiting with an unmarried partner (47.4%) and had little formal education (M = 8.9 years, SD = 4.1). For 41.4%, this was a first pregnancy and for just over a quarter (26.5%), it was a third or higher order pregnancy. Two-thirds (66.4%) of the sample reported having health insurance: most commonly D.C. Health Care Alliance, a public means-tested insurance program for Washington, D.C. residents. Two-thirds of women reported that their current pregnancy was unintended (37% mistimed and 28% unwanted). Table 1 depicts these demographic characteristics by pregnancy intendedness. Mean depressive symptom scores at each of the five data collection points were below the risk cutoff and showed a decreasing trend over the course of the perinatal period; Figure 1 shows the overall mean depressive symptom scores by reported pregnancy intention.
Table 1.
Sample Demographics, by Pregnancy Intendedness, with χ2 Tests of Association
| Intended | Mistimed | Unwanted | Total | ||
|---|---|---|---|---|---|
| Total | n | 74 | 79 | 61 | 214 |
| Row % | 34.6 | 36.9 | 28.5 | 100.0 | |
| Age | |||||
| 18–24 | 35 | 44 | 24 | 103 | |
| 34.0 | 42.7 | 23.3 | |||
| 25–29 | 25 | 21 | 19 | 65 | |
| 38.5 | 32.3 | 29.2 | |||
| 30 or Older | 14 | 13 | 18 | 45 | |
| 31.1 | 28.9 | 40.0 | |||
| Education (years)* | |||||
| 0–8 | 27 | 22 | 31 | 80 | |
| 33.7 | 27.5 | 38.8 | |||
| 9–12 | 37 | 47 | 20 | 104 | |
| 35.6 | 45.2 | 19.2 | |||
| More than 12 | 9 | 10 | 10 | 29 | |
| 31.0 | 34.5 | 34.5 | |||
| Parity (including index birth)** | |||||
| 1st | 47 | 30 | 12 | 89 | |
| 52.8 | 33.7 | 13.5 | |||
| 2nd | 16 | 32 | 20 | 68 | |
| 23.5 | 47.1 | 29.4 | |||
| 3rd or Higher | 11 | 17 | 29 | 57 | |
| 19.3 | 29.8 | 50.9 | |||
| Years in U.S.* | |||||
| Less than 1 | 6 | 18 | 5 | 29 | |
| 20.7 | 62.1 | 17.2 | |||
| 1–4 | 40 | 33 | 32 | 105 | |
| 38.1 | 31.4 | 30.5 | |||
| 5 or More | 25 | 26 | 23 | 74 | |
| 33.8 | 35.1 | 31.1 | |||
| Insured | |||||
| Yes | 52 | 53 | 36 | 141 | |
| 36.9 | 37.6 | 25.5 | |||
| No | 21 | 26 | 25 | 72 | |
| 29.2 | 36.1 | 34.7 | |||
| Partner/Marital Status** | |||||
| Married | 23 | 6 | 6 | 35 | |
| 65.7 | 17.1 | 17.1 | |||
| Cohabiting | 36 | 40 | 26 | 102 | |
| 35.3 | 39.2 | 25.5 | |||
| Non-cohabiting | 15 | 33 | 29 | 77 | |
| 19.5 | 42.9 | 37.7 | |||
| High depressive symptoms at baseline | |||||
| Yes | 29 | 44 | 31 | 104 | |
| 27.9 | 42.3 | 29.8 | |||
| No | 44 | 35 | 28 | 107 | |
| 41.1 | 32.7 | 26.2 | |||
| History of depressive episode | |||||
| Yes | 11 | 18 | 10 | 39 | |
| 28.2 | 46.2 | 25.6 | |||
| No | 63 | 61 | 51 | 175 | |
| 36.0 | 34.9 | 29.1 | |||
χ2:
p<0.10
p<0.05
p<0.01
Figure 1. Mean Depressive Symptoms by Pregnancy Intention.
Note: Suggested depression risk cutoffs for the BDI-II are indicated in dashed lines (16 for pregnant women, 13 for the general population).
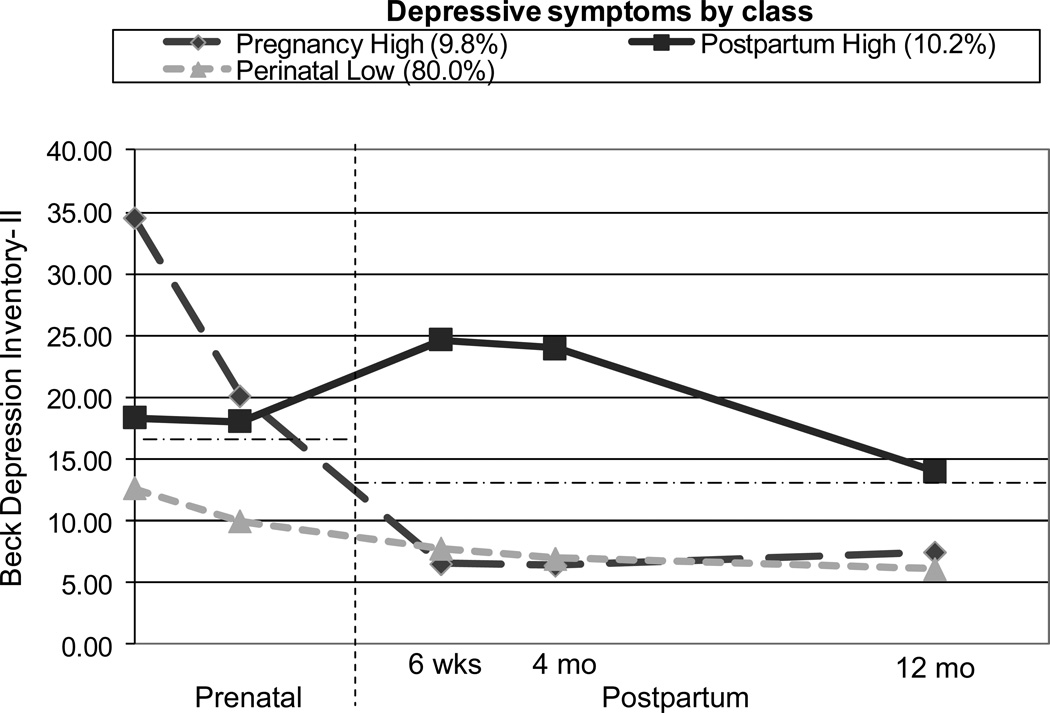
Growth mixture modeling identified three distinct depressive symptom trajectory patterns (Table 2). Individuals were generally very well classified into these groups, with half of women having a greater than 99% posterior probability of being in the class they were assigned to (median = 0.99; M = 0.94, SD = 0.12). Based on the level and timing of depressive symptoms, the 3 classes were labeled: “Pregnancy High” depression (9.8%), “Postpartum High” depression (10.2%) and “Perinatal Low” depression (80.0%). Mean values of the BDI-II for each group at each time point are graphed in Figure 2. In the “Pregnancy High” group, BDI-II scores were high at the two prenatal visits, but postpartum they dropped dramatically to a mean below the risk cutoff. The “Postpartum High” group showed prenatal BDI-II means near the risk cut-off, with a marked increase in symptoms at 6 weeks and 4 months postpartum. By 12 months postpartum, their symptoms returned to levels near the risk cut-off. Mean BDI-II levels for individuals in the “Perinatal Low” depression group never exceeded the risk cut-off during pregnancy and postpartum.
Table 2.
Choosing the Number of Classes: Growth Mixture Modeling Information Criteria
| Classes | Parameters | BIC | ABIC | Entropy | LMR LRT | BLRT |
|---|---|---|---|---|---|---|
| 1 | 11 | 5959.32 | 5924.46 | |||
| 2 | 15 | 5921.11 | 5873.57 | 0.838 | 0.011 | 0.000 |
| 3 | 19 | 5885.84 | 5825.63 | 0.860 | 0.042 | 0.000 |
| 4 | 23 | 5892.29 | 5819.41 | 0.836 | 0.745 | 0.040 |
| 5* | 27 | 5885.74 | 5800.18 | 0.839 | 0.089 | 0.000 |
Contains small class (< 5% of the sample): signifies unstable classification
BIC = Bayesian Information Criterion: lower values are better
ABIC = Sample-size Adjusted BIC: lower values are better
Entropy: measure of classification; ranges 0.00–1.00, with values closer to 1.00 being best
LMR LRT = Lo Mendell Rubenstein Likelihood Ratio Test p-value; want p<0.05
BLRT = Bootstrapped Likelihood Ratio Test p-value; want p<0.05
Figure 2. Mean Depressive Symptom Trajectories across the Perinatal Period for Each Depression Class.
Note: Suggested depression risk cutoffs for the BDI-II are indicated in dashed lines (16 for pregnant women, 13 for the general population).
Table 3 shows how the sample demographic characteristics differ by depression class. Women in the “Perinatal Low” depressive symptom class were significantly more likely to have an intended pregnancy, more likely to have health insurance, and more likely to be married, compared to women in the “Pregnancy High” and “Postpartum High” depressive symptom groups. Non-significant trends also imply that the “Perinatal Low” group may be more recent immigrants and less likely to have experienced abuse or a previous depressive episode, compared to the other two groups.
Table 3.
Sample Characteristics by Depressive Symptom Class (n= 215)
| Pregnancy High column % |
Postpartum High column % |
Perinatal Low column % |
|
|---|---|---|---|
| Pregnancy Intention | |||
| Intended* | 33.3 | 13.6 | 37.4 |
| Unintended* | 66.7 | 86.4 | 62.6 |
| Mistimed | 28.6 | 45.5 | 36.8 |
| Unwanted | 38.1 | 40.9 | 25.7 |
| Maternal age | |||
| 18–24 | 42.9 | 42.9 | 49.4 |
| 25–29 | 42.9 | 28.6 | 29.7 |
| 30+ | 14.3 | 28.6 | 20.9 |
| Maternal education (years) | |||
| 0–8 | 42.9 | 40.9 | 36.8 |
| 9–12 | 42.9 | 50.0 | 49.1 |
| More than 12 | 14.3 | 9.1 | 14.0 |
| Parity (including index birth) | |||
| 1st | 42.9 | 27.3 | 43.0 |
| 2nd | 28.6 | 36.4 | 32.0 |
| 3rd or higher | 28.6 | 36.4 | 25.0 |
| Years in the U.S. | |||
| Less than 1 | 10.5 | 9.5 | 14.8 |
| 1–4 | 47.4 | 42.9 | 51.5 |
| 5 or more | 42.1 | 47.6 | 33.7 |
| Health insurance* | 52.4 | 45.5 | 70.1 |
| Marital/partner status | |||
| Married* | 0.0 | 4.5 | 20.3 |
| Cohabiting | 47.6 | 36.4 | 48.8 |
| Other* | 52.4 | 59.1 | 30.8 |
| History of abuse | 28.6 | 45.5 | 20.0 |
| History of depression | 23.8 | 36.4 | 15.1 |
Wald test p<0.05
Table 4 displays the results from the 3 multinomial logistic regression models, comparing the risk of being in the “Pregnancy High” and “Postpartum High” depression trajectories versus the “Perinatal Low” depressive trajectory as a function of pregnancy intendedness. In none of the models was unintended pregnancy associated with the “Pregnancy High” pattern (top portion of Table 4). However, the risk of “Postpartum High” depressive symptoms was almost 4-fold higher among women with an unintended pregnancy than among those with an intended pregnancy in the unadjusted model (RRR=3.79, p<0.05; bottom portion of Table 4, Model 1). Only 4% of women with intended pregnancies followed the “Postpartum High” depressive symptom trajectory, compared to 14% of women with unintended pregnancies (not shown). Once adjusted for demographic factors (Model 2), women who report unintended pregnancies were over 5 times more likely to follow the “Postpartum High” depression pattern (RRR= 5.22, p<0.05), compared to women with an intended pregnancy. With the final adjustment for psychosocial factors (social support, history of depression and history of abuse; Model 3), the risk ratio remained large, but was only marginally statistically significant (RRR= 3.95, p<0.10).
Table 4.
Multinomial Logistic Regression: Impact of Unintended Pregnancy on Depression Class Membership, Compared to Perinatal Low Depression Class
| Model 1 (n= 214) RRR (95% CI) |
Model 2 (n= 206) RRR (95% CI) |
Model 3 (n= 204) RRR (95% CI) |
|
|---|---|---|---|
| Pregnancy High (vs. Perinatal Low) Depressive Symptoms | |||
| Unintended pregnancy | 1.20 (0.46, 3.12) | 0.93 (0.32, 2.69) | 0.66 (0.21, 2.05) |
| Maternal education (years) | 0.99 (0.88, 1.12) | 0.97 (0.86, 1.10) | |
| Parity (including index birth) | |||
| 1st | 1.00 | 1.00 | |
| 2nd | 0.95 (0.27, 3.26) | 1.02 (0.29, 3.60) | |
| 3rd or higher | 1.22 (0.34, 4.36) | 1.08 (0.29, 3.95) | |
| Years in the U.S. | |||
| Under 1 year | 1.00 | 1.00 | |
| 1–4 years | 1.03 (0.20, 5.34) | 0.85 (0.15, 4.68) | |
| 5 or more years | 1.51 (0.28, 8.08) | 1.06 (0.19, 5.93) | |
| Health insurance | 0.54 (0.19, 1.48) | 0.53 (0.18, 1.51) | |
| Social support (SSA) | 0.96* (0.92, 0.99) | ||
| History of depression | 0.85 (0.21, 3.39) | ||
| History of abuse | 1.32 (0.40, 4.31) | ||
| Intervention group | 1.32 (0.50, 3.49) | 1.40 (0.51, 3.87) | |
| Postpartum High (vs. Perinatal Low) Depressive Symptoms | |||
|---|---|---|---|
| Unintended pregnancy | 3.79* (1.08, 13.31) | 5.22* (1.10, 24.72) | 3.95† (0.76, 20.54) |
| Maternal education (years) | 0.96 (0.85, 1.08) | 0.93 (0.81, 1.05) | |
| Parity (including index birth) | |||
| 1st | 1.00 | 1.00 | |
| 2nd | 1.05 (0.30, 3.71) | 1.17 (0.31, 4.39) | |
| 3rd or higher | 1.40 (0.39, 5.07) | 0.91 (0.23, 3.64) | |
| Years in the U.S. | |||
| Under 1 year | 1.00 | 1.00 | |
| 1–4 years | 1.12 (0.21, 5.94) | 0.91 (0.15, 5.43) | |
| 5 or more years | 2.08 (0.39, 11.08) | 1.30 (0.22, 7.71) | |
| Health insurance | 0.29* (0.11, 0.79) | 0.26* (0.09, 0.77) | |
| Social support (SSA) | 0.97† (0.93, 1.00) | ||
| History of depression | 2.90† (0.92, 9.15) | ||
| History of abuse | 3.18* (1.07, 9.43) | ||
| Intervention group | 0.94 (0.36, 2.46) | 0.69 (0.24, 2.01) | |
p<0.05
p<0.10
Discussion
This analysis used a novel analytical technique to explore the heterogeneity of depressive symptoms in the perinatal period among a low-income, high-risk sample of Hispanic immigrants, providing evidence of three distinct patterns of perinatal depressive symptoms: “Pregnancy High” (9.8%), “Postpartum High” (10.2%), and “Perinatal Low” (80.0%). These classifications are similar to the results from the only other known GMM analysis of perinatal depression, which utilized a multiracial, low-income, urban sample (Mora et al., 2009). Mora et al. detected 5 distinct classes of depression from pregnancy to 24 months postpartum: chronic depression (7%), antenatal depression only (6%), postpartum depression only (9%), late onset depression (at 24 months; 7%), and never depressed (71%). If one examines only the first 12 months postpartum and reclassifies Mora et al.’s late onset depression (at 24 months) as never depressed in the perinatal period (first 12 months), then the prevalence of their antenatal depression (6%), postpartum depression (9%), and never/late (78%) depressed classes are remarkably similar to our “Pregnancy High” (9.8%), “Postpartum High” (10.2%), and “Perinatal Low” (80%) classes, respectively. However, in spite of the high-risk status of this sample, the present analysis did not detect a chronic depression class during the first year postpartum. This may be because women who were diagnosed with clinical depression at baseline were excluded from the study and referred to treatment. Longer term follow-up data were not collected on these subjects, so we could not assess the emergence of a late onset depression class.
Our findings also fit within the current epidemiological understanding of perinatal depression. Evidence from meta-analyses estimates the postpartum depression prevalence to be 10–15%, with a best guess of 13% in the general population (Gavin et al., 2005; O'Hara & Swain, 1996). This figure is drawn from studies that use clinical diagnoses of depression. In this analysis, we used mean BDI-II trends to identify distinct depression classes, rather than clinically diagnosing individual patients; however, our estimates of postpartum depression “prevalence” (10.2% fall into the “Postpartum High” class) are relatively similar to the epidemiological findings from clinical studies and meta-analyses. The figure of 10.2% provides some evidence that the GMM classifications are meaningful, yet they should not be used as a clinical depression prevalence estimate for this population.
Logistic regression models demonstrated that unintended pregnancy was not associated with depressive symptoms that are high only during pregnancy; however, it led to a marginally significant three- to four-fold increase in postpartum high depressive symptoms, compared to women who reported intended pregnancies. These analyses lend support to the hypothesis that unintended pregnancy leads to perinatal depression, rather than depression preceding the unintended pregnancy as potentially mediated by inconsistent contraceptive use. Previous research has demonstrated a cross-sectional association between unintended pregnancy and perinatal depression, but temporality cannot be established from cross-sectional studies (Barber et al., 1999; Lau & Keung, 2007; Nakku et al., 2006; Orr & Miller, 1997). One other known study has attempted to determine the temporal relationship between unintended pregnancy and postpartum depression (Najman, Morrison, Williams, Andersen, & Keeping, 1991). The cohort study of over 8,000 pregnant women in Brisbane, Australia found that women who reported unintended pregnancies at baseline had greater than double the risk of depression at 6 months postpartum (adj. RR= 2.4, 95% CI: 1.5, 3.9), a result similar to ours. However, in a secondary analysis of that study that excluded women who had mental health problems at baseline (n unspecified), the adjusted relative risk of depression was no longer statistically significant (adj. RR= 1.6, CI: 0.8, 3.2), suggesting that depression may precede unintended pregnancy. In our study, all of the women were at high-risk for depression (but not depressed) at baseline, with either high depressive symptoms and/or a history of major depression.
The vulnerability-stress model of psychosocial risk (Zubin & Spring, 1977) gives theoretical grounding to the evidence that unintended pregnancy increases women’s risk of perinatal depression. This model is not a new way of conceptualizing mental health risk; however, it was recently outlined as a useful framework in postpartum depression (Bernazzani et al., 2005). This model identifies three domains of risk and protection that affect either environmental or psychological vulnerability for depression: stressful life events, social support and maternal feelings/adaptation. All three domains are potentially affected by an unintended pregnancy. Pregnancy itself can be considered a stressful life event and unintended pregnancy even more so. By definition, an unintended pregnancy is unexpected. It raises significant questions of whether or not to terminate the pregnancy and/or requires planning and preparation for the baby’s birth. Additionally, the unintended pregnancy may have occurred as the result of a stressful period that led the woman or couple to be inconsistent with contraceptive use.
Social support and relationship factors may be affected by an unintended pregnancy if the woman’s feelings about the pregnancy differ from her partner’s, family’s, or friends’ feelings. In many cases the pregnancy may be intended by one member of a couple and unintended by the other. This discordance may cause disagreements about whether or not to continue the pregnancy, or arguments about finances or other aspects related to having a(nother) child.
Maternal feelings, attitudes toward the pregnancy and transition to motherhood may also differ by pregnancy intention. A woman who is planning to and wants to become pregnant may have more positive and/or less ambivalent feelings about the pregnancy and be quicker to adapt to a new social role than a woman with an unintended pregnancy.
Hispanic immigrant women may experience unique stressors when faced with an unintended pregnancy. Qualitative interviews with participants of this study and other recent Hispanic immigrants highlight some of these unique stressors (Christensen, 2010). Many Hispanic immigrants (both women and men) come to the U.S. to work and send money home to family in their home countries. Becoming unexpectedly pregnant, especially shortly after immigration, is likely to hinder these goals. For a majority of low-income Hispanic immigrants, abortion is not a culturally acceptable option. It is difficult to continue working, especially low-wage, service sector jobs, through pregnancy and after childbirth. There are limited affordable childcare options and many immigrant women do not have access to an informal childcare network of family and neighbors that likely would be available to them in their home countries. As such, an unintended pregnancy can upend a woman’s goals she had for herself upon immigration.
Knowing that unintended pregnancy is a precursor to many cases of perinatal depression provides another opportunity for interventions to prevent depression. Those concerned with maternal mental health should look further upstream to the context of the pregnancy and whether it was planned, mistimed, or unwanted. In addition, prevention programs designed to modify cognitive patterns with cognitive behavioral therapy, for example, might be best targeted to groups of pregnant women who are already at increased risk for depression, such as those who reported unintended pregnancies.
This study is limited in its generalizability. The unique sample consisted of low-income Hispanic immigrants who were at increased risk of perinatal depression. The patterns of perinatal depression and their association with unintended pregnancy may not be replicated in lower risk populations or in other racial/ethnic populations. The measures of depression in this study are self-reported depressive symptoms, rather than clinical diagnoses. In addition, growth mixture modeling (GMM) shows only the mean trends, and individuals vary in how closely they follow the trend. It is important to remember that there is individual variability within each depression class, which means, for example, that some women assigned to the “Perinatal Low” depressive symptom class may have actually exhibited depressive symptoms that cross the risk threshold at one time point or another. By assigning women to one and only one depression class, we do not capture this variability in our regression models; however, as mentioned in the results section, our GMM model classified women very well.
This paper also presents many strengths, including that pregnancy intendedness was measured early in pregnancy to limit recall bias, and depressive symptoms were measured at 5 points across pregnancy and the postpartum period. This allows some establishment of temporal relationships. In addition, although the high-risk, convenience sample limits generalizability, Hispanic immigrant women are a growing demographic that is at increased risk for unintended pregnancy and possibly for perinatal depression, and should be considered a priority study population.
Establishing the temporal relationship between unintended pregnancy and perinatal depression has important clinical and public health implications for communication messaging and the timing of and responsibility for depression screening. Because this analysis was conducted with a sample of high-risk Hispanic immigrants, more research must be done to determine if these associations are similar in other populations of women. If current findings are replicated , prenatal care providers should inform women who report unintended pregnancy of their increased risk of postpartum depression, provide them with information on the symptoms and treatment options, even if they demonstrate no or low depressive symptoms prenatally. Additionally, health care providers who interact with postpartum women (including their own primary care providers and their children’s pediatricians) should be prepared to offer the proper mental health referrals to women who demonstrate need and if possible, screen new mothers for depression in the months following birth.
Acknowledgments
Dr. Christensen completed this research for her doctoral dissertation at The Johns Hopkins Bloomberg School of Public Health and is currently employed by Mathematica Policy Research. Funding for this study was provided by grant R40 MC 02497 from the Maternal and Child Health Bureau (Title V, Social Security Act), Health Resources and Services Administration, Department of Health and Human Services (PI: Le). Dr. Christensen’s time was supported by a dissertation grant (1R36DP001880-01) from the Centers for Disease Control and Prevention. Dr. Stuart’s time was partially supported by Award K25MH083846 from the National Institute of Mental Health.
Contributor Information
Anna L. Christensen, Health Researcher, Mathematica Policy Research.
Elizabeth A. Stuart, Assistant Professor, Departments of Mental Health and Biostatistics, Johns Hopkins Bloomberg School of Public Health.
Deborah F. Perry, Research Associate Professor, Center for Child and Human Development, Georgetown University.
Huynh-Nhu Le, Associate Professor, Department of Psychology, George Washington University.
References
- Austin MP. Targeted group antenatal prevention of postnatal depression: A review. Acta Psychiatrica Scandinavica. 2003;107:244–250. doi: 10.1034/j.1600-0447.2003.00086.x. [DOI] [PubMed] [Google Scholar]
- Barber JS, Axinn WG, Thornton A. Unwanted childbearing, health, and mother-child relationships. Journal of Health and Social Behavior. 1999;40:231–257. [PubMed] [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri W. Comparison of beck depression inventories -IA and -II in psychiatric outpatients. Journal of Personality Assessment. 1996;67:588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory -II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: Systematic review. Obstetrics and Gynecology. 2004;103:698–709. doi: 10.1097/01.AOG.0000116689.75396.5f. [DOI] [PubMed] [Google Scholar]
- Bernazzani O, Marks MN, Bifulco A, Siddle K, Asten P, Conroy S. Assessing psychosocial risk in pregnant/postpartum women using the Contextual Assessment of Maternity Experience (CAME)-- Recent life adversity, social support and maternal feelings. Social Psychiatry and Psychiatric Epidemiology. 2005;40:497–508. doi: 10.1007/s00127-005-0917-y. [DOI] [PubMed] [Google Scholar]
- Bonicatto S, Dew AM, Soria JJ. Analysis of the psychometric properties of the Spanish version of the Beck Depression Inventory in Argentina. Psychiatry Research. 1998;79:277–285. doi: 10.1016/s0165-1781(98)00047-x. [DOI] [PubMed] [Google Scholar]
- Christensen AL. Unintended Pregnancy among Hispanic Immigrants in Washington, D.C.: The Cultural Context, Correlates and Mental Health Consequences. 2010. Doctoral Dissertation; UMI No. 3407703. [Google Scholar]
- Cooper PJ, Murray L. Postnatal depression. BMJ (Clinical Research Ed.) 1998;316:1884–1886. doi: 10.1136/bmj.316.7148.1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspectives on Sexual and Reproductive Health. 2006;38:90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: A systematic review of prevalence and incidence. Obstetrics and Gynecology. 2005;106:1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- Henshaw C, Elliott S. Screening for Perinatal Depression. London: Jessica Kingsley Publishers; 2005. [Google Scholar]
- Hobfoll SE, Ritter C, Lavin J, Hulsizer MR, Cameron RP. Depression prevalence and incidence among inner-city pregnant and postpartum women. Journal of Consulting and Clinical Psychology. 1995;63:445–453. doi: 10.1037//0022-006x.63.3.445. [DOI] [PubMed] [Google Scholar]
- Holcomb WL, Jr., Stone LS, Lustman PJ, Gavard JA, Mostello DJ. Screening for depression in pregnancy: Characteristics of the Beck Depression Inventory. Obstetrics and Gynecology. 1996;88:1021–1025. doi: 10.1016/s0029-7844(96)00329-8. [DOI] [PubMed] [Google Scholar]
- Holzman C, Eyster J, Tiedje LB, Roman LA, Seagull E, Rahbar MH. A life course perspective on depressive symptoms in mid-pregnancy. Maternal and Child Health Journal. 2006;10:127–138. doi: 10.1007/s10995-005-0044-0. [DOI] [PubMed] [Google Scholar]
- Howell EA, Mora PA, Horowitz CR, Leventhal H. Racial and ethnic differences in factors associated with early postpartum depressive symptoms. Obstetrics and Gynecology. 2005;105:1442–1450. doi: 10.1097/01.AOG.0000164050.34126.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara MA, Navarro C, Navarrete L. Outcome results of a psycho-educational intervention in pregnancy to prevent PPD: A randomized control trial. Journal of Affective Disorders. 2010;122:109–117. doi: 10.1016/j.jad.2009.06.024. [DOI] [PubMed] [Google Scholar]
- Lau Y, Keung DW. Correlates of depressive symptomatology during the second trimester of pregnancy among Hong Kong Chinese. Social Science & Medicine (1982) 2007;64:1802–1811. doi: 10.1016/j.socscimed.2007.01.001. [DOI] [PubMed] [Google Scholar]
- Le HN, Perry DF, Stuart EA. Randomized controlled trial of a preventive intervention for perinatal depression in high-risk Latinas. Journal of Consulting and Clinical Psychology. doi: 10.1037/a0022492. in press. [DOI] [PubMed] [Google Scholar]
- Le HN, Muñoz RF, Soto JA, Delucchi KL, Ippen CG. Identifying risk for onset of major depressive episodes in low-income Latinas during pregnancy and postpartum. Hispanic Journal of Behavioral Sciences. 2004;26:463–482. [Google Scholar]
- Mora PA, Bennett IM, Elo IT, Mathew L, Coyne JC, Culhane JF. Distinct trajectories of perinatal depressive symptomatology: Evidence from growth mixture modeling. American Journal of Epidemiology. 2009;169:24–32. doi: 10.1093/aje/kwn283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen BO. Latent variable analysis: Growth mixture modelling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of Quantitative Methodology for the Social Sciences. Newbury Park, CA: Sage Publications; 2004. pp. 345–368. [Google Scholar]
- Muthen LK, & Muthen BO. Mplus Users Guide. Los Angeles, CA: Muthen & Muthen; 2007. [Google Scholar]
- Najman JM, Morrison J, Williams G, Andersen M, Keeping JD. The mental health of women 6 months after they give birth to an unwanted baby: A longitudinal study. Social Science & Medicine. 1991;32:241–247. doi: 10.1016/0277-9536(91)90100-q. [DOI] [PubMed] [Google Scholar]
- Nakku JE, Nakasi G, Mirembe F. Postpartum major depression at six weeks in primary health care: Prevalence and associated factors. African Health Sciences. 2006;6:207–214. doi: 10.5555/afhs.2006.6.4.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norwood SL. The Social Support Apgar: Instrument development and testing. Research in Nursing & Health. 1996;19:143–152. doi: 10.1002/(SICI)1098-240X(199604)19:2<143::AID-NUR6>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- O'Hara MW. The nature of postpartum depressive disorders. In: Cooper PJ, editor. Postpartum Depression and Child Development. New York: The Guilford Press; 1997. [Google Scholar]
- O'Hara MW, Swain AM. Rates and risk of postpartum depression: A meta-analysis. International Review of Psychiatry. 1996;8:37. [Google Scholar]
- Orr ST, Miller CA. Unintended pregnancy and the psychosocial well-being of pregnant women. Women's Health Issues: Official Publication of the Jacobs Institute of Women's Health. 1997;7:38–46. doi: 10.1016/s1049-3867(96)00017-5. [DOI] [PubMed] [Google Scholar]
- Penley JA, Wiebe JS, Nwosu A. Psychometric properties of the Spanish Beck Depression Inventory-II in a medical sample. Psychological Assessment. 2003;15:569–577. doi: 10.1037/1040-3590.15.4.569. [DOI] [PubMed] [Google Scholar]
- Rich-Edwards JW, Kleinman K, Abrams A, Harlow BL, McLaughlin TJ, Joffe H, Gillman MW. Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. Journal of Epidemiology and Community Health. 2006;60:221–227. doi: 10.1136/jech.2005.039370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salamero M, Marcos T, Gutierrez F, Rebull E. Factorial study of the BDI in pregnant women. Psychological Medicine. 1994;24:1031–1035. doi: 10.1017/s0033291700029111. [DOI] [PubMed] [Google Scholar]
- Santelli J, Rochat R, Hatfield-Timajchy K, Gilbert BC, Curtis K, Cabral R, Hirsch JS, Schieve L. the Unintended Pregnancy Working Group The measurement and meaning of unintended pregnancy. Perspectives on Sexual and Reproductive Health. 2003;35:94–101. doi: 10.1363/3509403. [DOI] [PubMed] [Google Scholar]
- Segre LS, Losch MS, O'Hara MW. Brief Report: Race/ethnicity and perinatal depressed mood. Journal of Reproductive and Infant Psychology. 2006;24:99–106. [Google Scholar]
- Wiebe JS, Penley JA. A psychometric comparison of the Beck Depression Inventory-II in English and Spanish. Psychological Assessment. 2005;17:481–485. doi: 10.1037/1040-3590.17.4.481. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Miller IW, Pearlstein T, Howard M, Sweeney P. A preventive intervention for pregnant women on public assistance at risk for postpartum depression. American Journal of Psychiatry. 2006;163:1443–1445. doi: 10.1176/appi.ajp.163.8.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zubin J, Spring B. Vulnerability - a new view of schizophrenia. Journal of Abnormal Psychology, 86. 1977:103–124. doi: 10.1037//0021-843x.86.2.103. [DOI] [PubMed] [Google Scholar]