Abstract
Background: Urbanization is often cited as a main cause of increasing BMIs in low- and middle-income countries (LMICs), and urban residents in LMICs tend to have higher BMIs than do rural residents. However, urban-rural differences may be driven by differences in socioeconomic status (SES).
Objective: Using nationally representative data collected at 2 time points in 38 LMICs, we assessed the association between urban residence and BMI before and after adjustment for measures of individual- and household-level SES.
Design: We conducted a cross-sectional analysis of nationally representative samples of 678,471 nonpregnant women aged 15–49 y, with 225,312 women in the earlier round of surveys conducted between 1991 and 2004 and 453,159 women in the later round conducted between 1998 and 2010. We used linear and ordered multinomial analysis with a country fixed effect to obtain a pooled estimate and a country-stratified analysis.
Results: We found that mean BMI (kg/m2) in less-developed countries was generally higher within urban areas (excess BMI associated with urban residence before wealth index adjustment: 1.55; 95% CI: 1.52, 1.57). However, the urban association was attenuated after SES was accounted for (association after adjustment: 0.44; 95% CI: 0.41, 0.47). Individual- and household-level SES measures were independently and positively associated with BMI.
Conclusion: The association between urban residence and obesity in LMICs is driven largely by higher individual- and community-level SES in urban areas, which suggests that urban residence alone may not cause increased body weight in developing countries.
INTRODUCTION
In the past 2 decades, the mean BMI has increased globally, with an especially notable increase occurring in low- and middle-income countries (LMICs)4 (1–6). Obesity is a risk factor for many chronic, noncommunicable diseases, including type 2 diabetes and cardiovascular disease, and the burden of these diseases in LMICs is increasing: it is predicted that deaths from noncommunicable diseases will rise from 59% of global deaths in 2002 to 69% by 2030 (7–9).
Urbanization, or substantial population growth in urban areas of LMICs, is frequently cited as an underlying cause of the rise in global overweight. Several authors have argued that, because urban residents of LMICs are more likely to work in sedentary employment, use motorized transportation, and eat diets high in processed grains and sugars as more of the population in LMICs migrates into urban areas, mean BMIs will correspondingly increase (10–14). However, urbanization trends will have different effects on different populations within each country, which makes it impossible to generalize about the health effects of urbanization at the national or global level. Whereas several studies have identified higher mean BMI or proportion overweight in urban areas within LMICs (15–17), studies that have used the national percent urban as a predictor of BMI in LMICs have found no significant association between national urbanization and individual BMI in LMICs (18, 19). Moreover, because socioeconomic status (SES) is likely to be higher among urban residents, and because high SES is associated with a higher BMI in most LMICs (1, 20–22), it is likely that at least part of the effect of urban residence on BMI is due to the effects of individual- and community-level SES on obesity. In this analysis, we used data from 38 LMICs collected at 2 time points to measure the associations between SES, measured either as an overall wealth index or as indexes separately measuring household-level assets and community amenities, and body weight.
SUBJECTS AND METHODS
Data sources
The data for this study came from Demographic and Health Surveys (DHSs) of women of reproductive age (15–49 y) conducted at 2 separate occasions in 38 countries between 1991 and 2010 (23). To select surveys for inclusion in the analysis, we identified the earliest and latest survey from countries where ≥2 surveys had been fielded after 1990. The DHSs are household sample surveys measuring indicators of population health, maternal and child health, and nutrition (24). The target population in these DHSs included all women or ever-married women of reproductive age, with either the full sample or a subsample of women selected for anthropometric measurements.
DHSs use extensive interviewer training, standardized measurement tools and techniques, an identical core questionnaire, and instrument pretesting to ensure standardization and comparability across diverse sites and time (www.measuredhs.com/pubs/pdf/DHSG4/Recode4DHS.pdf) (25). The surveys use a multistage stratified design with probabilistic sampling, with each elementary unit having a defined probability of selection (26). Each survey was stratified by urban and rural status and by country-specific geographic or administrative regions. Detailed sampling plans are available from survey final reports at www.measuredhs.com/pubs/search/search_results.cfm?Type=5&srchTp=type&newSrch=1 (27). Response rates for the surveys are generally high, ranging between 88% and 99% of households and between 85% and 95% of women within households (28). Because the surveys collect population-representative data, and have been using a similar survey protocol for the past 20 y, the DHS is a particularly valuable data source for studying population health across lower-income countries (29–31).
Study population and sample size
The study population includes 1,028,441 women interviewed in 38 countries at 2 time points (395,695 at time 1; 632,746 at time 2). Because many surveys included anthropometric measurements on a subsample of women, 256,500 women had no measured height and weight and were excluded from the analysis. An additional 11,742 women were eligible for measurement but had missing or implausible values; these women were also excluded from analysis. Women who were pregnant at the time of the survey (n = 59,141), women who were outside the age range of 15 to 49 y (n = 3777), and women missing data on other covariates incorporated into the analysis (DHS wealth index, educational attainment, marital status) were also excluded from the analysis (n = 120). The final analytic sample used in the analyses incorporating the DHS wealth index as the primary measure of SES included 697,573 women (232,150 at time 1; 465,423 at time 2). Of these women, 19,102 were missing data on at least one housing asset or household amenity used in constructing the separate housing and amenities indexes, so the final respondent count in these analyses includes 678,471 women (225,312 at time 1; 453,159 at time 2). A flow diagram depicting the selection of the final sample is provided elsewhere (see Supplemental Figure 1 under “Supplemental data” in the online issue).
The DHS data collection procedures were approved by the Opinion Research Corporation Macro (Calverton, MD) Institutional Review Board and by the relevant body that approves research studies on human subjects in each country. Oral informed consent for the interview/survey was obtained from respondents by interviewers. The study was reviewed by Harvard School of Public Health Institutional Review Board and was considered exempt from full review because the study was based on an anonymous public use data set with no identifiable information on the survey participants.
Outcome measures
The primary outcome for this analysis was BMI among nonpregnant women aged 15–49 y. BMI was calculated as weight (in kg) divided by height (in m) squared. Weight was measured by trained investigators using a solar-powered scale with an accuracy of ±100 g, and height was measured by using an adjustable board calibrated in millimeters (25).
BMI has been chosen as the primary outcome because it provides a readily available measurement of adiposity that is comparable across countries and settings and has been found to be strongly correlated with densitometry measurements of adiposity, which are commonly used as the “gold standard” of adiposity measurement (32). BMI is a particularly useful outcome to consider because it encompasses the full spectrum of body weight, from under- to overnutrition. In addition, some evidence suggests that the risk of cardiovascular disease and all-cause mortality increase at BMI levels <25 (33–35), particularly in Asian populations (36, 37). Percentage overweight (BMI >25) and percentage underweight (BMI <18.5) were included as secondary outcomes.
Independent variables
Urban residence and SES, as measured by household wealth, are the primary predictors in this analysis. Urban residents were defined as respondents living in an urban area as defined by the national census or statistical bureau in each country at the time the survey was conducted. The primary measure of SES was an index of household assets comparing the wealth of respondents within countries using data on the assets available within households. The index was calculated by using principal components analysis: z scores for each variable measuring a household's assets and utilities were developed, principal components analysis was conducted on these standardized variable to identify the principal component underlying asset ownership, and the values of the indicator variables were multiplied by the factor loadings for each household and summed to produce a standardized household index value with a mean of 0 and an SD of 1. This standardized score was then divided into quintiles for each country (38–40).
Whereas this overall wealth index has been shown to be a reliable and valid proxy for household expenditures data (41), it also has a documented urban bias. The assets measured in this index, particularly those measuring housing quality or amenities, are more commonly available for urban residents, which makes it less likely to identify relatively poor urban respondents or relatively wealthy rural respondents (40, 42). Moreover, the availability of urban infrastructure may be considered a measure of community-level SES, which may affect health through different mechanisms from individual- or household SES (43). For these reasons, we have conducted additional analyses by using separate asset indexes for housing amenities and household goods. We identified housing amenities as items that were substantially more common in urban areas (prevalence difference of 40% in more than half of the surveys) or may be provided as public infrastructure in urban areas. The amenities index includes improved sanitation, piped drinking water, electricity, and highest-quality flooring material. A similar measure of housing quality was constructed by using survey data from Ghana and was found to be internally consistent and have construct validity (44). The household goods index includes items that are found in both rural and urban areas, including radio, television, refrigerator, bicycle, motorcycle, or car.
Additional covariates include age, educational attainment, and marital status. Age was calculated in years and entered into all models in 10-y age groups. Education was specified as a woman having no education or incomplete primary education, completed primary education, or having some secondary or higher schooling. Marital status was entered as a binary variable, with ever-married also including widowed, divorced, and cohabiting women.
Analysis
In the primary analysis, linear regression was used to estimate the associations between urban residence and BMI and between urban residence, SES, and BMI. Three sets of analyses were conducted. First, a pooled analysis of all countries within each time group was used to estimate the overall urban association. This analysis was adjusted for country by using a fixed effect. Second, a country-stratified analysis was used to estimate the urban association within each country. Finally, an analysis pooled across country but stratified by DHS wealth group was used to estimate the differential associations between urban residence and BMI across wealth groups. In the secondary analysis, pooled and country-stratified ordered multinomial analyses were conducted by using over- and underweight as the outcomes of interest. A generalized estimating equation was used to account for the clustered sampling design of the DHS data. All analyses were conducted by using Stata 11.1 SE (45).
RESULTS
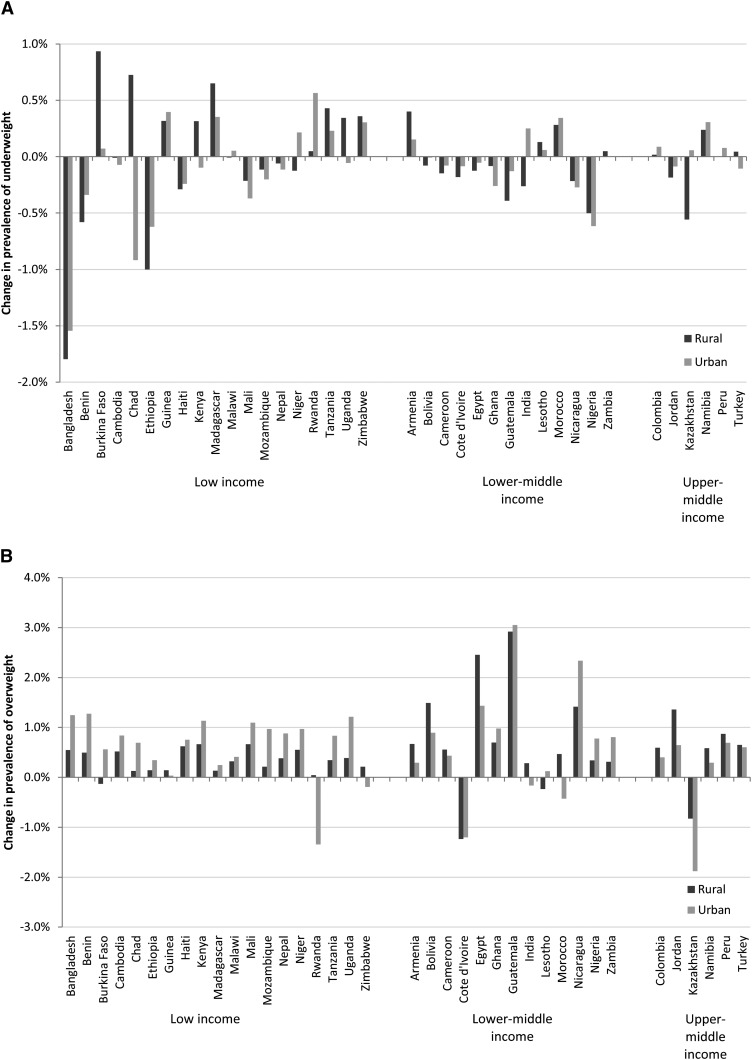
Mean BMI was higher in urban areas across most countries in both time periods (see Supplemental Table 1 under “Supplemental data” in the online issue), with exceptions in Armenia 2000 (time 1), Kazakhstan 1999 (time 2), and Colombia 2010 (time 2). The prevalence of overweight was higher in urban than in rural areas in nearly all countries (37 of 38 in time 1; 36 of 38 in time 2), and overweight increased between time periods in urban areas in 31 of 38 countries (see Supplemental Table 2 under “Supplemental data” in the online issue). Overweight was increasing more quickly in urban areas than in rural areas of lower-income countries such as Bangladesh and Uganda, but increasing more quickly among rural areas compared with urban areas of upper-middle-income countries, such as Jordan and Peru. The prevalence of underweight increased among urban residents in 16 of 38 countries, which suggests that these overall positive trends in BMI may be masking urban inequalities in some countries (Figure 1).
FIGURE 1.
Average annual change in percentage underweight (A) and overweight (B) in urban and rural areas in 38 countries. n = 697,573. National income groups were taken from the World Bank (46).
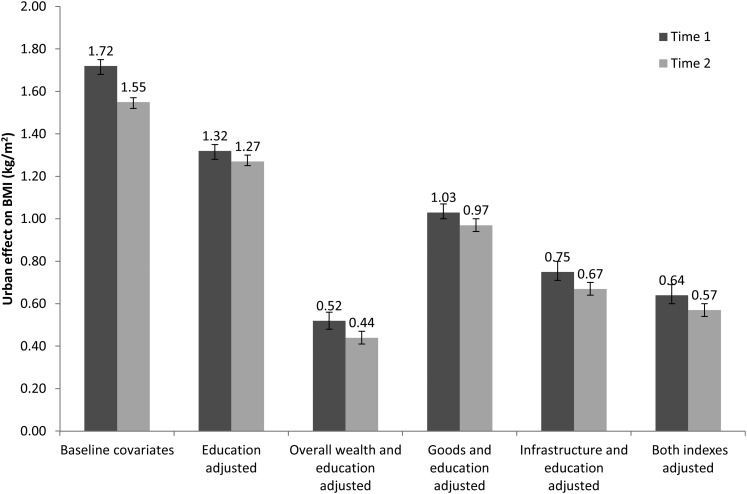
After adjustment for marital status, age, and country only, urban residents had a BMI that was 1.72 higher (95% CI: 1.68, 1.75) than that of rural residents in time 1; this urban association decreased to 1.55 (95% CI: 1.52, 1.57) in time 2. The association between urban residence and BMI decreased somewhat when educational attainment was also included in the model, to 1.32 (95% CI: 1.28, 1.35) at time 1 and 1.27 (95% CI: 1.25, 1.3) at time 2, and decreased substantially when both educational attainment and the full assets index were included in the model, to 0.52 (95% CI: 0.48, 0.56) at time 1 and to 0.44 (95% CI: 0.41, 0.47) at time 2 (Figure 2 and see Supplemental Table 3 under “Supplemental data” in the online issue). Adjustment for the household goods index decreased the strength of the urban association slightly, to 1.02 at time 1 and to 0.97 at time 2, whereas adjustment for the housing amenities decreased the strength of this association more noticeably, to 0.75 at time 1 and to 0.67 at time 2 (Figure 2 and see Supplemental Table 4 under “Supplemental data” in the online issue). In the secondary analysis, the prevalence of underweight among urban residents was lower than the prevalence among rural residents after adjustment for educational attainment, marital status, and age [adjusted prevalence ratio (APR) at time 1: 0.64 (95% CI: 0.62, 0.66); at time 2: 0.69 (95% CI: 0.68, 0.71)] but was higher after adjustment for overall wealth index at time 2 [APR at time 1: 0.99 (95% CI: 0.96, 1.03); at time 2: 1.03 (95% CI: 1, 1.07)] (see Supplemental Table 5 under “Supplemental data” in the online issue). Urban residents had a higher prevalence of overweight after adjustment for SES across both time periods [APR at time 1: 1.39 (95% CI: 1.35, 1.44); at time 2: 1.32 (95% CI: 1.3, 1.35)] (see Supplemental Table 6 under “Supplemental data” in the online issue).
FIGURE 2.
Urban association with BMI before and after adjustment for education and assets indexes. Associations were calculated by using multilevel linear models and were additionally adjusted for age (10-y groups; fixed effect), marital status (fixed effect), country (random effect), region within country (random effect), and primary sampling unit (random effect). Error bars represent 95% CIs. n = 697,573 for analyses that excluded housing amenities and household assets and 678,471 for analyses that included housing amenities and household assets.
The association between SES and BMI, whether measured by using the full assets index, the household amenities index, or the housing attributes index, remained positive across all models, with women in the highest overall wealth group had a BMI that was 2.15 higher (95% CI: 2.09, 2.21) at time 1 and 2.39 higher (95% CI: 2.34, 2.44) at time 2. SES was also positively associated with overweight across all models [APR at time 2: 3.28 (95% CI: 3.17, 3.39)] and was negatively associated with underweight across models [APR at time 2: 0.46 (95% CI: 0.44, 0.48)]. When the separate measures of housing amenities and household goods were considered, each measure was independently associated with BMI, although the association of housing amenities with BMI was somewhat higher (1.02 for the highest tertile of household goods at time 2 compared with 1.25 for the highest tertile of housing amenities.)
In country-stratified analyses, the excess BMI associated with urban residence ranged from 3.26 in Niger in 1998 (time 1) to −0.27 in Armenia in 2000 (time 1) (Table 1). Adjustment for overall wealth index attenuated the urban association in nearly all countries and time periods (37 of 38 countries at time 1; 36 of 38 at time 2). Within countries, the trend in the urban association was mixed, with 15 of 38 countries seeing an increase in the size of the association between urban residence and BMI after adjustment for the overall wealth index. This increased most in Burkina Faso (average increase of 0.151 per year between 1993 and 2003) and decreased most in Rwanda (average decrease of −0.14 per year between 2000 and 2005).
TABLE 1.
Average estimated difference in BMI between urban and rural residents before and after adjustment for socioeconomic status, by country1
| Urban residence |
Urban residence + overall wealth |
Urban residence + amenities and household goods |
|||||||
| Survey | Year | Association | 95% CI | Association | 95% CI | No. of subjects | Association | 95% CI | No. of subjects |
| Armenia | 2000 | −0.27 | (−0.56, 0.03) | −0.65 | (−1.02, −0.29) | 5981 | −0.38 | (−0.71, −0.06) | 5903 |
| Armenia | 2005 | 0.01 | (−0.32, 0.34) | −0.33 | (−0.7, 0.03) | 6067 | 0.06 | (−0.31, 0.43) | 5831 |
| Bangladesh | 1996 | 1.09 | (0.75, 1.44) | 0.4 | (0.04, 0.76) | 4045 | 0.53 | (0.17, 0.88) | 3938 |
| Bangladesh | 2007 | 1.55 | (1.3, 1.81) | 0.56 | (0.34, 0.77) | 10,106 | 0.72 | (0.5, 0.94) | 9923 |
| Benin | 1996 | 0.64 | (0.22, 1.07) | −0.09 | (−0.53, 0.35) | 2330 | 0.29 | (−0.13, 0.7) | 2242 |
| Benin | 2006 | 1.37 | (1.11, 1.63) | 0.37 | (0.15, 0.59) | 14,883 | 0.65 | (0.42, 0.89) | 14,665 |
| Bolivia | 1994 | 1.22 | (0.85, 1.58) | 0.32 | (−0.12, 0.76) | 2346 | 0.43 | (−0.01, 0.87) | 2272 |
| Bolivia | 2008 | 0.98 | (0.78, 1.19) | −0.36 | (−0.64, −0.09) | 15,539 | 0.5 | (0.26, 0.73) | 15,126 |
| Burkina Faso | 1993 | 1.18 | (0.9, 1.45) | 0.36 | (−0.08, 0.79) | 3467 | 0.42 | (0.04, 0.8) | 3366 |
| Burkina Faso | 2003 | 2.69 | (2.34, 3.05) | 1.44 | (1.07, 1.82) | 10,996 | 1.5 | (1.1, 1.9) | 10,821 |
| Cambodia | 2000 | 0.76 | (0.54, 0.99) | 0.29 | (0.06, 0.52) | 6911 | 0.37 | (0.13, 0.61) | 6555 |
| Cambodia | 2005 | 0.82 | (0.59, 1.06) | 0.15 | (−0.06, 0.36) | 7845 | 0.28 | (0.07, 0.49) | 7759 |
| Cameroon | 1998 | 1.3 | (0.76, 1.84) | 0.35 | (−0.28, 0.97) | 1661 | 0.31 | (−0.31, 0.93) | 1607 |
| Cameroon | 2004 | 1.54 | (1.21, 1.88) | 0.64 | (0.25, 1.03) | 4646 | 0.56 | (0.17, 0.95) | 4448 |
| Chad | 1996 | 1.62 | (1.26, 1.98) | 0.86 | (0.41, 1.32) | 2952 | 0.97 | (0.53, 1.4) | 2871 |
| Chad | 2004 | 0.65 | (0.27, 1.02) | 0.01 | (−0.48, 0.5) | 3709 | 0.46 | (0.06, 0.87) | 3646 |
| Colombia | 1995 | 0.36 | (0, 0.72) | −0.45 | (−0.92, 0.01) | 3319 | 0.14 | (−0.23, 0.52) | 3248 |
| Colombia | 2010 | 0.02 | (−0.1, 0.14) | −0.09 | (−0.25, 0.08) | 43,950 | −0.01 | (−0.14, 0.12) | 43,563 |
| Cote d'Ivoire | 1994 | 1.91 | (1.4, 2.41) | 0.41 | (−0.15, 0.98) | 2740 | 1.11 | (0.55, 1.67) | 2683 |
| Cote d'Ivoire | 1998–1999 | 1.51 | (1.2, 1.83) | 0.81 | (0.46, 1.16) | 3146 | 0.99 | (0.62, 1.35) | 3069 |
| Egypt | 1995 | 2.2 | (1.81, 2.58) | 1.02 | (0.63, 1.41) | 6777 | 1.53 | (1.14, 1.93) | 6032 |
| Egypt | 2008 | 0.64 | (0.37, 0.91) | −0.11 | (−0.4, 0.17) | 14,840 | 0.63 | (0.35, 0.9) | 14,516 |
| Ethiopia | 2000 | 1.74 | (1.51, 1.98) | 1.13 | (0.83, 1.44) | 13,906 | 1.02 | (0.71, 1.32) | 13,653 |
| Ethiopia | 2005 | 1.72 | (1.43, 2.01) | 1.07 | (0.73, 1.41) | 6127 | 0.59 | (0.21, 0.96) | 6050 |
| Ghana | 1993 | 1.66 | (1.17, 2.15) | 0.68 | (0.08, 1.28) | 1781 | 0.52 | (−0.13, 1.18) | 1763 |
| Ghana | 2008 | 2.1 | (1.75, 2.46) | 0.52 | (0.14, 0.9) | 4450 | 0.97 | (0.58, 1.36) | 4386 |
| Guatemala | 1995 | 1.44 | (1.1, 1.77) | 0.55 | (0.24, 0.87) | 5015 | 0.67 | (0.34, 0.99) | 4924 |
| Guatemala | 1998–1999 | 1.34 | (0.78, 1.9) | 0.25 | (−0.33, 0.82) | 2398 | 0.66 | (0.07, 1.24) | 2353 |
| Guinea | 1999 | 1.54 | (1.2, 1.88) | 0.67 | (0.23, 1.1) | 3347 | 0.86 | (0.43, 1.3) | 3184 |
| Guinea | 2005 | 1.78 | (1.44, 2.13) | 1.19 | (0.74, 1.63) | 3574 | 1.52 | (1.08, 1.97) | 3464 |
| Haiti | 1994–1995 | 1.04 | (0.65, 1.42) | 0.04 | (−0.37, 0.45) | 1902 | 0.21 | (−0.2, 0.63) | 1834 |
| Haiti | 2005–2006 | 1.5 | (1.18, 1.82) | 0.25 | (−0.11, 0.62) | 4935 | 0.64 | (0.28, 1) | 4862 |
| India | 1998 | 1.59 | (1.46, 1.72) | 0.59 | (0.48, 0.71) | 76,616 | 0.68 | (0.56, 0.8) | 74,928 |
| India | 2005 | 1.45 | (1.36, 1.54) | 0.55 | (0.46, 0.63) | 113,063 | 0.63 | (0.54, 0.72) | 110,987 |
| Jordan | 1997 | 0.95 | (0.35, 1.55) | 0.79 | (0.19, 1.4) | 3082 | 0.93 | (0.31, 1.54) | 2994 |
| Jordan | 2007 | 0.06 | (−0.37, 0.48) | 0.09 | (−0.34, 0.51) | 4527 | −0.03 | (−0.46, 0.41) | 4426 |
| Kazakhstan | 1995 | 0.07 | (−0.47, 0.62) | −0.18 | (−0.8, 0.43) | 3538 | −0.03 | (−0.66, 0.61) | 3436 |
| Kazakhstan | 1999 | −0.25 | (−0.72, 0.21) | −0.38 | (−1.25, 0.5) | 2218 | −0.3 | (−1.06, 0.47) | 2107 |
| Kenya | 1998 | 1.28 | (0.84, 1.72) | 0.33 | (−0.1, 0.76) | 3294 | 0.75 | (0.29, 1.2) | 3144 |
| Kenya | 2008–2009 | 1.76 | (1.41, 2.1) | 0.18 | (−0.24, 0.6) | 7692 | 0.73 | (0.33, 1.13) | 7553 |
| Lesotho | 2004 | 0.96 | (0.5, 1.42) | −0.35 | (−0.83, 0.12) | 3205 | 0.33 | (−0.12, 0.79) | 3133 |
| Lesotho | 2009 | 1.38 | (0.92, 1.85) | −0.23 | (−0.73, 0.28) | 3775 | 0.49 | (0.02, 0.96) | 3610 |
| Madagascar | 1997 | 0.48 | (0.17, 0.79) | −0.01 | (−0.33, 0.32) | 2627 | 0.07 | (−0.25, 0.38) | 2594 |
| Madagascar | 2008–2009 | 0.73 | (0.49, 0.97) | −0.16 | (−0.43, 0.12) | 7674 | 0.06 | (−0.2, 0.32) | 7578 |
| Malawi | 1992 | 0.81 | (0.44, 1.18) | 0.5 | (0.09, 0.9) | 2342 | 0.52 | (0.12, 0.92) | 2307 |
| Malawi | 2010 | 1.31 | (1, 1.63) | 0.61 | (0.28, 0.95) | 6881 | 0.77 | (0.43, 1.1) | 6754 |
| Mali | 2006 | 1.1 | (0.85, 1.36) | 0.65 | (0.38, 0.93) | 4306 | 0.49 | (0.18, 0.81) | 4195 |
| Mali | 1995–1996 | 2.15 | (1.85, 2.46) | 1.04 | (0.69, 1.39) | 12,506 | 1.5 | (1.12, 1.88) | 12,135 |
| Morocco | 1992 | 2.11 | (1.59, 2.62) | 0.46 | (−0.14, 1.07) | 2890 | 0.98 | (0.34, 1.62) | 2843 |
| Morocco | 2003–2004 | 1.41 | (1.16, 1.66) | 0.18 | (−0.16, 0.52) | 15,941 | 0.82 | (0.51, 1.14) | 15,214 |
| Mozambique | 1997 | 0.98 | (0.58, 1.38) | −0.02 | (−0.41, 0.37) | 3284 | 0.25 | (−0.13, 0.64) | 3190 |
| Mozambique | 2003 | 1.74 | (1.49, 1.98) | 0.34 | (0.1, 0.57) | 10,533 | 0.69 | (0.46, 0.92) | 10,208 |
| Namibia | 1992 | 2.17 | (1.59, 2.76) | 0.67 | (0, 1.34) | 2268 | 0.62 | (−0.15, 1.39) | 2177 |
| Namibia | 2006–2007 | 1.53 | (1.26, 1.8) | 0.14 | (−0.16, 0.44) | 8962 | 0.37 | (0.06, 0.67) | 8496 |
| Nepal | 1996 | 0.35 | (−0.21, 0.9) | 0.1 | (−0.45, 0.66) | 3420 | 0.28 | (−0.24, 0.8) | 3311 |
| Nepal | 2006 | 0.67 | (0.34, 1) | −0.03 | (−0.32, 0.25) | 10,116 | 0.07 | (−0.2, 0.35) | 9857 |
| Nicaragua | 1998 | 0.91 | (0.67, 1.14) | 0.14 | (−0.1, 0.38) | 12,258 | 0.21 | (−0.03, 0.46) | 11,734 |
| Nicaragua | 2001 | 1.16 | (0.9, 1.42) | 0.08 | (−0.21, 0.38) | 11,936 | 0.26 | (−0.02, 0.54) | 11,808 |
| Niger | 1998 | 3.26 | (2.81, 3.7) | 2.09 | (1.49, 2.7) | 3947 | 2.06 | (1.4, 2.71) | 3887 |
| Niger | 2006 | 2.28 | (1.83, 2.73) | 1.04 | (0.54, 1.53) | 3454 | 1.61 | (1.08, 2.14) | 3302 |
| Nigeria | 2003 | 0.79 | (0.46, 1.11) | 0.19 | (−0.12, 0.5) | 6606 | 0.28 | (−0.03, 0.6) | 6421 |
| Nigeria | 2008 | 0.8 | (0.6, 1) | 0.03 | (−0.17, 0.24) | 28,900 | 0.18 | (−0.02, 0.38) | 27,705 |
| Peru | 1991–1992 | 1.1 | (0.82, 1.38) | 0.38 | (0.06, 0.7) | 5199 | 0.32 | (0.01, 0.64) | 5062 |
| Peru | 2004–2008 | 1.23 | (1.05, 1.4) | 0.47 | (0.27, 0.67) | 25,928 | 0.6 | (0.39, 0.82) | 23,627 |
| Rwanda | 2000 | 1.3 | (1.08, 1.51) | 0.86 | (0.58, 1.14) | 9168 | 0.76 | (0.48, 1.03) | 8,922 |
| Rwanda | 2005 | 0.6 | (0.32, 0.88) | 0.08 | (−0.19, 0.36) | 5211 | 0.07 | (−0.21, 0.35) | 5105 |
| Tanzania | 1996 | 1.36 | (0.99, 1.73) | 0.45 | (0.06, 0.84) | 3820 | 0.45 | (0.06, 0.84) | 3662 |
| Tanzania | 2004–2005 | 1.96 | (1.64, 2.27) | 0.83 | (0.53, 1.14) | 9159 | 1.09 | (0.79, 1.4) | 8948 |
| Turkey | 1993 | 0.7 | (0.25, 1.15) | 0.16 | (−0.31, 0.63) | 2417 | 0.67 | (0.05, 1.3) | 2308 |
| Turkey | 2003 | 0.7 | (0.22, 1.18) | 0.48 | (0, 0.96) | 3030 | 0.16 | (−0.39, 0.72) | 2922 |
| Uganda | 1995 | 1.28 | (0.9, 1.66) | 0.67 | (0.29, 1.04) | 3234 | 0.46 | (0.06, 0.85) | 3116 |
| Uganda | 2006 | 2.38 | (1.83, 2.94) | 1.25 | (0.62, 1.88) | 2519 | 1.22 | (0.56, 1.89) | 2465 |
| Zambia | 1996 | 1.01 | (0.74, 1.27) | 0.13 | (−0.21, 0.47) | 3902 | 0.39 | (0.05, 0.73) | 3778 |
| Zambia | 2007 | 1.55 | (1.25, 1.85) | 0.33 | (−0.04, 0.71) | 6288 | 0.56 | (0.19, 0.93) | 6024 |
| Zimbabwe | 1994 | 1.89 | (1.41, 2.37) | 0.43 | (−0.38, 1.24) | 1983 | 1.17 | (−0.16, 2.5) | 1905 |
| Zimbabwe | 2005–2006 | 1.73 | (1.5, 1.97) | 0.03 | (−0.34, 0.4) | 8163 | 0.05 | (−0.39, 0.49) | 8036 |
Associations were calculated by using multilevel linear models and were additionally adjusted for age (10-y groups; fixed effect), marital status (fixed effect), country (random effect), region within country (random effect), and primary sampling unit (random effect).
Finally, we estimated the interaction of the associations between wealth and urban residence on BMI. A model including the interaction between urban residence and overall wealth was run for each time period, and the P values for significance of the interaction were as follows: P = 0.01 (F[4, 3390] = 3.10) at time 1 and P = 0.001 (F[4, 8652] = 4.56) at time 2. In an analysis stratified by wealth, we found that the size of the association between urban residence and BMI generally increased with increasing wealth. The excess BMI associated with urban residence ranged from 0.14 (95% CI: −0.01, 0.29) in the poorest wealth group to 0.86 (95% CI: 0.77, 0.94) in the wealthiest group at time 1 and from 0.12 (95% CI: 0.02, 0.23) among the poorest to 0.74 (95% CI: 0.67, 0.81) among the wealthiest at time 2 (Table 2).
TABLE 2.
Adjusted associations (95% CIs) between urban residence, educational attainment, and BMI within 5 wealth groups1
| Time 1(n = 232,150) | Time 2(n = 465,423) | |
| Poorest wealth group | ||
| Urban residence | 0.14 (−0.01, 0.29) | 0.12 (0.02, 0.23) |
| Educational attainment | ||
| Completed primary | 0.19 (0.09, 0.3) | 0.23 (0.16, 0.08) |
| Secondary or higher | 0.51 (0.16, 0.86) | 0.08 (−0.09, 0.37) |
| Second wealth group | ||
| Urban residence | 0.16 (0.04, 0.28) | 0.1 (0.02, 0.17) |
| Educational attainment | ||
| Completed primary | 0.17 (0.08, 0.26) | 0.19 (0.12, −0.1) |
| Secondary or higher | 0.16 (−0.07, 0.4) | −0.1 (−0.22, 0.36) |
| Third wealth group | ||
| Urban residence | 0.3 (0.2, 0.39) | 0.23 (0.17, 0.3) |
| Educational attainment | ||
| Completed primary | 0.17 (0.08, 0.26) | 0.32 (0.26, −0.15) |
| Secondary or higher | 0.09 (−0.08, 0.25) | −0.15 (−0.25, 0.53) |
| Fourth wealth group | ||
| Urban residence | 0.34 (0.27, 0.42) | 0.35 (0.29, 0.4) |
| Educational attainment | ||
| Completed primary | 0.3 (0.22, 0.39) | 0.31 (0.24, 0.01) |
| Secondary or higher | 0.06 (−0.07, 0.19) | 0.01 (−0.08, 0.7) |
| Highest wealth group | ||
| Urban residence | 0.86 (0.77, 0.94) | 0.74 (0.67, 0.81) |
| Educational attainment | ||
| Completed primary | 0.72 (0.63, 0.82) | 0.48 (0.4, 0.44) |
| Secondary or higher | 1 (0.89, 1.11) | 0.44 (0.36, 1.02) |
Associations were calculated by using multilevel linear models and were additionally adjusted for age (10-y groups; fixed effect), marital status (fixed effect), country (random effect), region within country (random effect), and primary sampling unit (random effect).
DISCUSSION
Consistent with earlier literature, we found that the mean BMI in less-developed countries is generally higher in urban areas than in rural areas and that prevalence of overweight is similarly higher in urban areas. However, the size of the association between urban residence and BMI is substantially reduced after adjustment for household wealth index, which suggests that much of the difference between urban and rural residents is driven by the socioeconomic composition of urban areas. In multiple regression models, although we identified independent positive associations between urban residence and SES as measured by an overall wealth index on body weight, this association was attenuated after SES was accounted for, from 1.27 at time 1 to 0.44 in time 2. Moreover, the association between urban environment and BMI is highest among wealthy respondents and is near zero among the poorest. Finally, the prevalence of underweight is increasing in some urban areas, including in some middle-income countries and across all geographic regions included in the data set used.
Additionally, this analysis found independent positive associations between SES and BMI at multiple levels, including both household- and community-level measures of resource availability. Household- and community-level SES have been found to have independent, but complementary effects on a variety of maternal and child health outcomes (43); extending these findings to BMI points toward multiple pathways through which SES may affect BMI and adds to the evidence that both community context and individual resources shape body weight simultaneously. The residual association between urban residence on BMI after adjustment for SES suggests that additional city-level factors that are not captured in the community-level SES measure, such as the availability of food retail or transportation infrastructure, also affect BMI. However, more detailed studies will be needed to confirm this hypothesis.
Taken together, these findings suggest not only that urban-rural differences in BMI are driven in large part by socioeconomic differences between residents of urban-rural areas, but also that there is heterogeneity in trends in urban BMI. Increases in prevalence of underweight in some urban areas further illustrate that the problem of increased obesity is not reaching all residents of developing countries and that under nutrition remains an important issue. In light of these findings, policies addressing obesity and chronic disease in LMICs should not only measure mean levels of risk factors at a national level, but should also assess the implications of ongoing changes in diet and physical activity on health disparities, including disparities within urban areas. This conclusion fits with the suggestions of several authors discussing the effects of globalization on health, who note that these trends are likely to increase disparities in a variety of health measures, from access to health care to quality of diet (47, 48).
This study had several limitations and strengths. Because the surveys used in this analysis were conducted at different times across countries, we were unable to estimate the change in BMI across all countries for the entire survey period. Whereas we have attempted to account for the differences in the span of time included for each country by providing estimates of average annual change, care must be taken in interpreting trend results, particularly in comparing effects calculated in models with data from the first and second time periods. Additionally, this study did not incorporate any information about the length of time respondents have lived in an urban area and consequently does not account for fluctuations in health that may occur after migration to an urban area. A study of rural-to-urban migrants in India found that adiposity increased quickly after migrating into an urban environment, but then the rate of increase slowed after a decade spent in urban areas (49). This suggests that the rates of change in BMI in urban areas may also depend on historical trends in migration. Finally, in this analysis, urban residence is defined by each country, and these definitions vary widely within regions (50–52). The wealth index measures used as a proxy for SES are calculated based on assets information that is collected similarly across countries, but quintile cutoffs differ for each time period and survey (39).
Because the outcome and all predictors were measured simultaneously, the estimated associations provide evidence of the patterning of high BMI, but should not be interpreted in causal terms. In addition, these findings are based on the experiences of women and cannot be generalized to men. However, reviews of the association between SES and body weight in high-income countries have found that the inverse association between SES and weight first appeared among women (1, 20), and evidence from developing countries suggests that both rural women and men are likely to weigh less than their urban counterparts (2). This makes it unlikely that the positive socioeconomic gradient found in this study is driven by sex differences in the direction of this association and suggests that the urban-rural gradients would likely be similar if data from both sexes were used. Finally, several authors have found that risk of obesity-related diseases increases at lower BMI levels in Asian populations (53, 54). Whereas few studies have assessed the health effect of different BMI levels in African populations, studies of African Americans have shown that, for a given BMI level, African Americans tend to have lower adiposity than do their white counterparts (55). Although this literature questions the relevance of a BMI cutoff as a measure of disease risk across the diverse population included in this study, these cutoffs are widely used for studying weight status in populations. Consequently, we have reported models with both individual-level BMI and weight-group status (underweight, normal weight, and overweight) as outcomes.
The strengths of this analysis include the number and variety of countries included in the analysis, the incorporation of multiple years of nationally representative data, and the use of multiple measures of SES, including both an overall measure and a measure disaggregating household- and community-level assets. Previous analyses of the effect of urban residence on body weight have focused on a single country (2, 15, 16, 38, 56) or have investigated associations between obesity and SES within urban areas only (57–59). The results presented above incorporate multiple years of nationally representative data from a diverse array of LMICs, which adds to the literature a broader understanding of the effects of both urban residence and SES on body weight. Additionally, the analysis incorporates multiple measures of SES, including both an overall wealth index and separate measures of availability of urban infrastructure and household goods, which account for the primarily urban distribution of many of the items typically included in overall wealth indexes and provide a more nuanced analysis of the way SES works across multiple levels to affect health.
In summary, this analysis found a positive and independent association between urban residence and BMI, which suggests that in LMICs such differences are largely explained by household and community SES. In most LMICs, mean BMI is highest among wealthy urban residents, but high BMI has not extended to rural populations or the urban poor, where underweight is increasing in some countries. These findings indicate that the focus of research on global obesity should not be on global factors alone, but on how these factors interact with local and individual attributes to shape health and health disparities.
Supplementary Material
Acknowledgments
We acknowledge the support of Macro International, Inc (Calverton, MD), for providing access to the various Demographic and Health Surveys.
The authors’ responsibilities were as follows—MN and SVS: conceptualized the study, designed the analysis, and co-wrote the manuscript; MN: conducted the analysis; and SG and IK: contributed to the conceptualization and interpretation of results. No conflicts of interest were reported.
Footnotes
Abbreviations used: APR, adjusted prevalence ratio; DHS, Demographic and Health Survey; LMICs, low- and middle-income countries; SES, socioeconomic status.
REFERENCES
- 1.Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychol Bull 1989;105:260–75 [DOI] [PubMed] [Google Scholar]
- 2.Prentice AM. The emerging epidemic of obesity in developing countries. Int J Epidemiol 2006;35:93–9 [DOI] [PubMed] [Google Scholar]
- 3.Hossain P, Kawar B, El Nahas M. Obesity and diabetes in the developing world—a growing challenge. N Engl J Med 2007;356:213–5 [DOI] [PubMed] [Google Scholar]
- 4.Kelly T, Yang W, Chen CS, Reynolds K, He J. Global burden of obesity in 2005 and projections to 2030. Int J Obes (Lond) 2008;32:1431–7 [DOI] [PubMed] [Google Scholar]
- 5.Wang H, Du S, Zhai F, Popkin BM. Trends in the distribution of body mass index among Chinese adults, aged 20-45 years (1989-2000). Int J Obes (Lond) 2007;31:272–8 [DOI] [PubMed] [Google Scholar]
- 6.Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, Singh GM, Gutierrez HR, Lu Y, Bahalim AN. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9· 1 million participants. Lancet 2011;377:557–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006;367:1747–57 [DOI] [PubMed] [Google Scholar]
- 8.WHO Global burden of disease: 2004 update. Geneva, Switzerland: WHO, 2008 [Google Scholar]
- 9.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006;3:e442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. WHO. Obesity: preventing and managing the global epidemic. World Health Organ Tech Rep Ser 2000;894. [PubMed]
- 11.Popkin BM. Urbanization, lifestyle changes and the nutrition transition. World Dev 1999;27:1905–16 [Google Scholar]
- 12.Monteiro CA, Conde WL, Popkin BM. The burden of disease from undernutrition and overnutrition in countries undergoing rapid nutrition transition: a view from Brazil. Am J Public Health 2004;94:433–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Popkin BM. The nutrition transition and obesity in the developing world. J Nutr 2001;131:871S–3S [DOI] [PubMed] [Google Scholar]
- 14.Popkin BM. Technology, transport, globalization and the nutrition transition food policy. Food Policy 2006;31:554–69 [Google Scholar]
- 15.Dearth-Wesley T, Wang H, Popkin B. Under-and overnutrition dynamics in Chinese children and adults (1991–2004). Eur J Clin Nutr 2008;62:1302–7 [DOI] [PubMed] [Google Scholar]
- 16.Monteiro CA, D'A Benicio MH, Conde WL, Popkin BM. Shifting obesity trends in Brazil. Eur J Clin Nutr 2000;54:342–6 [DOI] [PubMed] [Google Scholar]
- 17.Martorell R, Khan LK, Hughes ML, Grummer-Strawn LM. Obesity in women from developing countries. Eur J Clin Nutr 2000;54:247–52 [DOI] [PubMed] [Google Scholar]
- 18.Rabin BA, Boehmer TK, Brownson RC. Cross-national comparison of environmental and policy correlates of obesity in Europe. Eur J Public Health 2007;17:53–61 [DOI] [PubMed] [Google Scholar]
- 19.Nandi A, Sweet E, Kawachi I, Heymann J, Galea S. “Economic development, urbanization, FDI, trade liberalization, and patterns of under- and overweight in low- and middle-income countries: a multilevel analysis of 81,000 adults in 23 countries.'.
- 20.McLaren L. Socioeconomic status and obesity. Epidemiol Rev 2007;29:29–48 [DOI] [PubMed] [Google Scholar]
- 21.Neuman M, Subramanian S, Finlay J, Davey Smith G. The poor stay thinner: stable socioeconomic gradients in body mass index among women in lower and middle income countries. Am J Clin Nutr 2011;94:1348–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Subramanian SV, Perkins JM, Ozaltin E, Davey Smith G. Weight of nations: a socioeconomic analysis of women in low- to middle-income countries. Am J Clin Nutr 2011;93:413–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Macro International Inc Demographic and health surveys. Calverton, MD: Macro International Inc, 2010 [Google Scholar]
- 24.Rutstein SO, Rojas G. Guide to DHS statistics. Calverton, MD: ORC Macro, 2003 [Google Scholar]
- 25. Macro ORC. Demographic and Health Survey interviewer's manual. Calverton, MD: ORC Macro, 2006.
- 26.Macro International Inc Sampling manual. Calverton, MD: ORC Macro, 1996 [Google Scholar]
- 27.MEASURE DHS. Available from: http://www.measuredhs.com/pubs/search/search_results.cfm?Type=5&srchTp=type&newSrch=1 (cited 18 June 2011)
- 28.Vaessen M, Thiam M, Le T. The Demographic and Health Surveys. Household sample surveys in developing and transition countries. New York, NY: United Nations Statistical Division, 2005 [Google Scholar]
- 29.Wirth ME, Delamonica E, Sacks E, Balk D, Storeygard A, Minujin A. Monitoring health equity in the MDGs: a practical guide. New York, NY: CIESIN/UNICEF, 2006 [Google Scholar]
- 30.Vaessen M. The potential of the Demographic and Health Surveys (DHS) for the evaluation and monitoring of maternal and child health indicators. : Khlat M, Demographic evaluation of health programs. Paris, France: CICRED/UNFPA, 1996 [Google Scholar]
- 31.Pullum T. An assessment of the quality of data on health and nutrition in the DHS surveys, 1998-2003. Calverton, MD: Macro International Inc, 2008 [Google Scholar]
- 32.Willett W. Nutritional epidemiology. 2nd ed New York, NY: Oxford University Press, 1998 [Google Scholar]
- 33.Willett WC, Manson JE, Stampfer MJ, Colditz GA, Rosner B, Speizer FE, Hennekens CH. Weight, weight change, and coronary heart disease in women. Risk within the 'normal’ weight range. JAMA 1995;273:461–5 [DOI] [PubMed] [Google Scholar]
- 34.Freedman DM, Ron E, Ballard-Barbash R, Doody MM, Linet MS. Body mass index and all-cause mortality in a nationwide US cohort. Int J Obes (Lond) 2006;30:822–9 [DOI] [PubMed] [Google Scholar]
- 35.Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE, Hennekens CH, Speizer FE. Body weight and mortality among women. N Engl J Med 1995;333:677–85 [DOI] [PubMed] [Google Scholar]
- 36.Hu FB. Obesity epidemiology. New York, NY: Oxford University Press, 2008 [Google Scholar]
- 37.WHO Expert Consultation Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157–63 [DOI] [PubMed] [Google Scholar]
- 38.Gwatkin DR, Rutstein SO, Johnson K, Pande R, Wagstaff A. Socioeconomic differences in health, nutrition, and population in India. Washington, DC: The World Bank, 2000 [Google Scholar]
- 39.Rutstein SO, Johnson K. The DHS wealth index. Calverton, MD: ORC Macro, 2004 [Google Scholar]
- 40.Rutstein SO. The DHS Wealth Index: approaches for rural and urban areas. Washington, DC: Macro International Inc, 2008 [Google Scholar]
- 41.Filmer D, Pritchett L. Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography 2001;38:115–32 [DOI] [PubMed] [Google Scholar]
- 42.Speizer I, Luseno W. Measuring and interpreting urban fertility and family planning indicators by wealth in two South Asian countries. Chapel Hill, NC: Measure Evaluation and the University of North Carolina at Chapel Hill, 2010 [Google Scholar]
- 43.Fotso JC, Kuate-Defo B. Measuring socioeconomic status in health research in developing countries: should we be focusing on households, communities or both? Soc Indic Res 2005;72:189–237 [Google Scholar]
- 44.Fiadzo ED, Houston JE, Godwin DD. Estimating housing quality for poverty and development policy analysis: CWIQ in Ghana. Soc Indic Res 2001;53:137–62 [Google Scholar]
- 45.StataCorp Stata Statistical software: release 11. College Station, TX: StataCorp LP, 2009 [Google Scholar]
- 46.World Bank. Available from: http://data.worldbank.org/country (cited 22 June 2011)
- 47.Blouin C, Chopra M, van der Hoeven R. Trade and social determinants of health. Lancet 2009;373:502–7 [DOI] [PubMed] [Google Scholar]
- 48.Cornia GA, Rossignoli S, Tiberti L. Globalisation and health: impact pathways and recent evidence. Santa Cruz, CA: CGIAR (Consultative Group on International Agricultural Research), 2007 [Google Scholar]
- 49.Ebrahim S, Kinra S, Bowen L, Andersen E, Ben-Shlomo Y, Lyngdoh T, Ramakrishnan L, Ahuja RC, Joshi P, Das SM, et al. The effect of rural-to-urban migration on obesity and diabetes in India: a cross-sectional study. PLoS Med 2010;7:e1000268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vlahov D, Galea S. Urbanization, urbanicity, and health. J Urban Health 2002;79:S1–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.United Nations Population Division World urbanization prospects: the 2001 revision. New York, NY: United Nations, 2002 [Google Scholar]
- 52.United Nations Statistics Division. Available from: http://unstats.un.org/unsd/demographic/sconcerns/densurb/densurbmethods.htm (cited 9 June 2011)
- 53.Snehalatha C, Viswanathan V, Ramachandran A. Cutoff values for normal anthropometric variables in asian Indian adults. Diabetes Care 2003;26:1380–4 [DOI] [PubMed] [Google Scholar]
- 54.Zheng W, McLerran DF, Rolland B, Zhang X, Inoue M, Matsuo K, He J, Gupta PC, Ramadas K, Tsugane S, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med 2011;364:719–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wagner DR, Heyward VH. Measures of body composition in blacks and whites: a comparative review. Am J Clin Nutr 2000;71:1392–402 [DOI] [PubMed] [Google Scholar]
- 56.Subramanian SV, Smith GD. Patterns, distribution, and determinants of under- and overnutrition: a population-based study of women in India. Am J Clin Nutr 2006;84:633–40 [DOI] [PubMed] [Google Scholar]
- 57.Fezeu L, Minkoulou E, Balkau B, Kengne AP, Awah P, Unwin N, Alberti GK, Mbanya JC. Association between socioeconomic status and adiposity in urban Cameroon. Int J Epidemiol 2006;35:105–11 [DOI] [PubMed] [Google Scholar]
- 58.Case A, Menendez A. Sex differences in obesity rates in poor countries: evidence from South Africa. Econ Hum Biol 2009;7:271–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dahly DL, Gordon-Larsen P, Popkin BM, Kaufman JS, Adair LS. Associations between multiple indicators of socioeconomic status and obesity in young adult Filipinos vary by gender, urbanicity, and indicator used. J Nutr 2010;140:366–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.