Abstract
BACKGROUND
In response to increasing rates of excessive gestational weight gain (GWG) and evidence of postpartum weight retention and long-term overweight and obesity, the Institute of Medicine (IOM) revised their guidelines for GWG in 2009. Prenatal physical activity is recommended, although its role in preventing excessive GWG is unclear. We aimed to understand the association between prenatal physical activity and GWG in a longitudinal cohort.
METHODS
During a baseline survey at 34 weeks, women (n=3,006) reported their height, pre-pregnancy weight, and physical activity during pregnancy. GWG was self-reported at 1-month postpartum. Multivariable logistic regression adjusting for age, race/ethnicity, education, poverty status, marital status, gestational age at the time of delivery and smoking was used to model the association between adequate physical activity during pregnancy and exceeding the IOM recommendations for GWG.
FINDINGS
Overweight women were most likely to exceed the IOM recommendations for GWG (78.7%), followed by obese women and normal weight women (65.0% and 42.4%, respectively). The majority of women participated in some physical activity during pregnancy, with 41.2% engaging in 60–149 min and 32.1% engaging in at least 150 min of physical activity/week. In adjusted analysis, meeting the physical activity guidelines was associated with 29% (0.57–0.88) lower odds of exceeding the IOM recommendations for GWG compared with inactive women.
CONCLUSIONS
Findings of high rates of excessive GWG, especially among women with overweight and obesity, are concerning given the associated health burdens. The association of guideline-concordant physical activity with appropriate GWG suggests this is an important target for future interventions.
Introduction
The widespread adverse health and economic effects of the obesity epidemic are well described (Flegal, Carroll, Ogden, & Curtin, 2010). The majority of women of childbearing age are already overweight or obese, which elevates the risk of gestational diabetes, preeclampsia, eclampsia, cesarean delivery and macrosomic infants (Baeten, Bukusi, & Lambe, 2001; Institute of Medicine [IOM] & National Research Council [NRC], 2009). Also, nearly half of normal weight women and two-thirds of overweight and obese women are exceeding the Institute of Medicine (IOM) guidelines for appropriate gestational weight gain (GWG) during pregnancy (Chu, Callaghan, Bish, & D'Angelo, 2009; Institute of Medicine [IOM] & National Research Council [NRC], 2009; Martin et al., 2007). Excessive GWG is an important contributor to postpartum weight retention and long-term overweight and obesity; one-quarter of women with a normal pre-pregnancy body mass index (BMI) who gain more than 20 kgs during pregnancy will move up one BMI category (i.e. from normal weight to overweight) at 6 months post-partum (Nohr et al., 2008; Viswanathan et al., 2008). Even more importantly, high GWG is independently associated with poor pregnancy outcomes including premature birth, large-for-gestational age infants, lower breastfeeding initiation rates, and increased risk of cesarean delivery (Viswanathan et al., 2008).
In response to increasing rates of excessive GWG and evidence of associated negative outcomes (Viswanathan et al., 2008), the IOM revised their guidelines for GWG in 2009 (Institute of Medicine [IOM] & National Research Council [NRC], 2009). The updated guidelines for GWG are based on pre-pregnancy BMI, with lower GWG recommended for overweight and obese women compared with normal weight women. While normal weight (BMI=18.5–24.9 kg/m2) women are recommended to gain 11.5–16 kg, women who are overweight (BMI=25.0–29.9 kg/m2) are expected to limit weight gain to 7–11.5 kg (Institute of Medicine [IOM] & National Research Council [NRC], 2009). Obese women (BMI≥30.0 kg/m2) are further restricted, with recommendations to gain only 5–9 kg during pregnancy (Institute of Medicine [IOM] & National Research Council [NRC], 2009). While GWG limited to these recommended ranges has been associated with reduced maternal and infant morbidity, little is known about how modifiable prenatal behaviors influence GWG.
Describing characteristics and behaviors associated with excessive GWG may offer important clinical insights on how to limit the increasing problem of excessive weight gain during pregnancy. Identifying modifiable factors influencing GWG may provide useful targets for intervention and prevention. For example, physical activity during pregnancy is recommended by both the American Congress of Obstetricians and Gynecologists and United States Federal Guidelines, but whether prenatal physical activity has an important role in preventing excessive GWG is unclear (American College of Obstetricians and Gynecologists [ACOG], 2002; Physical Activity Guidelines Advisory Committee, 2008). In fact, the 2009 IOM report specifically recommended that studies be conducted on the effect of physical activity on weight gain during pregnancy (Institute of Medicine [IOM] & National Research Council [NRC], 2009). Subsequent studies have suggested that physical activity, both preconception and prenatal, is inversely associated with excessive GWG (Stuebe, Oken, & Gillman, 2009; Weisman, Hillemeier, Downs, Chuang, & Dyer, 2010). We hypothesize that adequate physical activity during pregnancy helps women avoid excessive GWG. This benefit may be even greater for women with overweight and obesity, given tighter restrictions on appropriate weight gain. Using a unique longitudinal cohort of women having their first child, the aim of this study was to understand the association between prenatal physical activity and GWG, using data collected at the baseline and 1-month postpartum time points.
Methods
Study Design
Data for these analyses are from the First Baby Study (blinded by WHI editors for peer review), which is a longitudinal cohort study of women having a first, singleton birth. The First Baby Study was approved by the Institutional Review Board [name of IRB blinded by WHI editors for peer review]. The primary purpose of the parent project is to investigate the association between mode of first delivery (vaginal vs. cesarean) and subsequent childbearing. Participants were recruited with flyers between January 2009 and April 2011 from numerous locations, such as hospitals, obstetricians’ offices and clinics, and targeted mailings to potentially eligible women obtained from marketing lists. Women were eligible to participate if they were residents of Pennsylvania, aged 18 to 35 at the time of the baseline interview, nulliparous, currently pregnant with a singleton pregnancy, and able to speak/read English or Spanish. Details regarding recruitment are described elsewhere ([reference blinded by WHI editors for peer review]). The majority of participants delivered at 7 hospitals, although women delivered at a total of 69 hospitals throughout the State. Participants of the First Baby Study completed the baseline telephone interview during the third trimester (≥34 weeks gestation), and will continue to be followed with subsequent telephone interviews until 3 years postpartum.
A total of 3,006 women were recruited, consented, and completed both the baseline interview and 1-month postpartum interview and comprise the sample for the current analysis. Since the characteristics and risks associated with pre-pregnancy weight and GWG differ significantly for underweight women, the 100 women who were underweight (BMI <18.5 kg/m2) prior to pregnancy were excluded from this analysis. We also excluded 118 women who delivered prior to 37 weeks gestation, since the IOM recommendations are intended for women with full-term gestations. Finally, 21 women did not provide information on height, pre-pregnancy weight or GWG. The final analytic sample, therefore, consisted of 2,767 women (i.e., 91% of the recruited cohort).
Definition of variables
Gestational weight gain
Using self-reported height and pre-pregnancy weight collected during the baseline survey, women were classified into pre-pregnancy body mass index (BMI) categories as follows: normal weight (BMI 18.5 – 24.9 kg/m2), overweight (BMI 25.0 – 29.9 kg/m2), and obese (BMI ≥30.0 kg/m2). During the 1-month postpartum survey, women self-reported how much weight they gained during pregnancy. Using the IOM recommendations for GWG defined above (Institute of Medicine [IOM] & National Research Council [NRC], 2009), women were then categorized as exceeding or not exceeding the recommended GWG for their respective pre-pregnancy BMI category. GWG was analyzed both as a continuous variable (in kg) and as a dichotomized variable (exceeding or not exceeding IOM recommendations).
Physical activity during pregnancy
In the baseline survey, women were given a definition for regular physical activity based on the US Department of Health and Human Services (USDHHS) guidelines (i.e., at least 150 minutes of moderate-intensity physical activity, such as brisk walking, hiking or bicycling, per week) (Physical Activity Guidelines Advisory Committee, 2008), and then asked how many days per week and minutes per day they were engaging in regular physical activity since becoming pregnant. A 3-level variable describing physical activity during pregnancy was created, defined as inactive (< 60 min/week), minimally active (60 – 149 min/week) and active (150 min/week or more). Women were also asked the type of physical activity they engaged in during pregnancy.
Covariates
Covariates were self-reported during the baseline telephone interview and were chosen to reflect variables that have been demonstrated in the literature to be associated with GWG (Institute of Medicine [IOM] & National Research Council [NRC], 2009). Sociodemographic variables included age group (18–24, 25–29, 30–36 years), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, Asian, or other), education (high school degree or less, some college or technical school, or college graduate or higher), poverty status (poverty, near poverty, or not poverty), and marital status (married, partnered/living together, partnered/not living together, or not partnered). We also included continuous variable to indicate gestational age at the time of delivery (in weeks) and a variable to indicate if women were smoking daily during pregnancy, which has been shown to be associated with lower GWG (Furuno, Gallicchio, & Sexton, 2004).
Statistical Analysis
Frequencies of the study variables were determined. GWG (in kg) was compared between the normal weight, overweight, and obese women using ANOVA (Tukey procedure) for multiple comparisons. Bivariate analyses assessed the association between adequate physical activity and exceeding the IOM recommendations for GWG, using chi-square tests. Bivariate associations between the other independent variables and exceeding GWG recommendations were also performed, using chi-square tests or t-tests for continuous variables. We then used multivariable logistic regression to model the association between adequate physical activity during pregnancy and exceeding the IOM recommendations for GWG (Institute of Medicine [IOM] & National Research Council [NRC], 2009), controlling for the covariates described above. All analyses were performed using SAS Version 9.3 (SAS Institute, Inc., Cary, N.C.).
Results
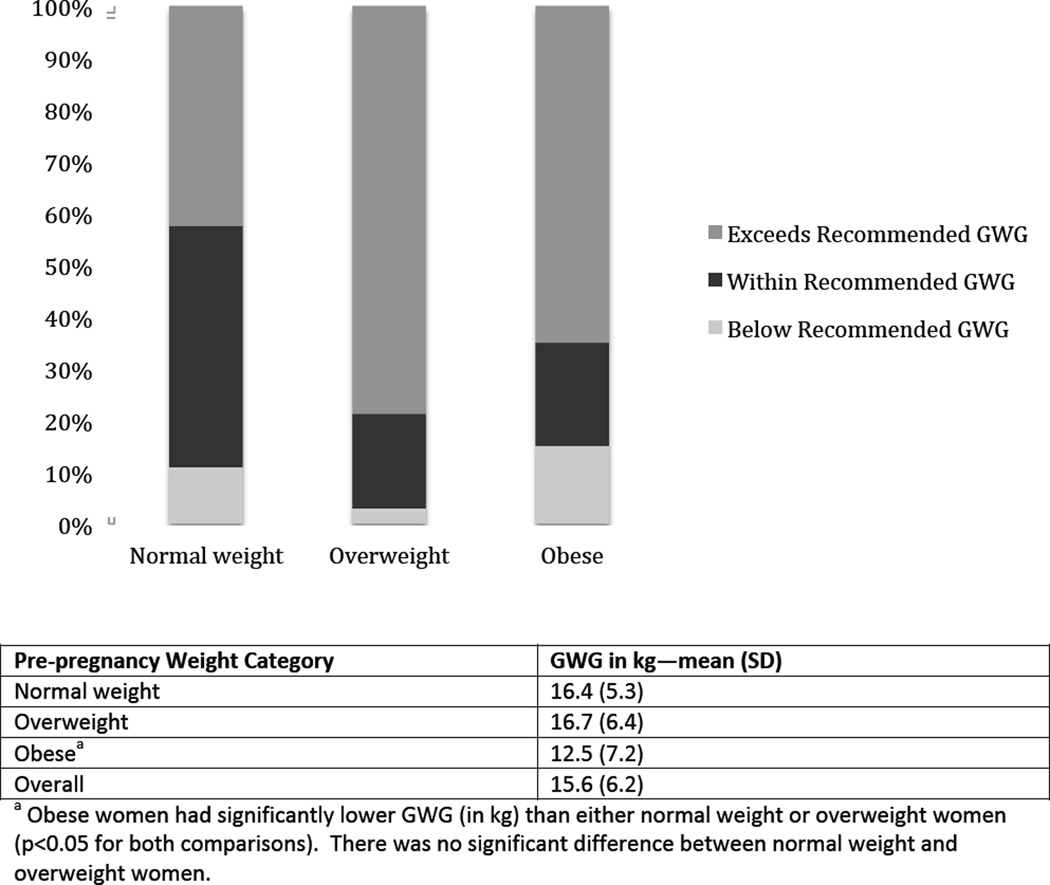
As shown in Table 1, almost half of the First Baby Study participants were either overweight or obese prior to pregnancy (22.9% and 21.5%, respectively). Overall, the majority of women (55.6%) gained more weight during pregnancy than recommended by the IOM guidelines for GWG, as shown in the top panel of the Figure. As shown in the bottom panel of the Figure, the mean GWG was 15.6 kg (SD 6.2). Obese women gained significantly less weight (in kg) than each of the other weight categories (p<0.05), but there was no statistical difference in GWG between the normal weight and overweight women. Overweight women were most likely to exceed the IOM recommendations for GWG (78.7%), followed by obese women and normal weight women (65.0% and 42.4%, respectively).
Table 1.
Characteristics of First Baby Study participants by Gestational Weight Gain (GWG), N= 2,767.
| Factor/Variable Name | Total | Exceeded Recommended GWG N=1,538 (55.6%) |
Did Not Exceed Recommended GWG N=1,229 (44.4%) |
p-value | |
|---|---|---|---|---|---|
| Physical activity during pregnancy | <0.01 | ||||
| Inactive (<60 min/wk) | 741(26.8) | 444(28.9) | 297(24.2) | ||
| Minimally active (60–149 min/wk) | 1139(41.2) | 657(42.7) | 482(39.2) | ||
| Active (≥150 min/wk) | 887(32.1) | 437(28.4) | 450(36.6) | ||
| Prepregnancy weight category | <0.01 | ||||
| Normal weight | 1537(55.5) | 651(42.3) | 886(72.1) | ||
| Overweight | 635(22.9) | 500(32.5) | 135(11) | ||
| Obese | 595(21.5) | 387(25.2) | 208(16.9) | ||
| Age group—years | 0.98 | ||||
| 18–24 | 704(25.4) | 389(25.3) | 315(25.6) | ||
| 25–29 | 1106(40) | 617(40.1) | 489(39.8) | ||
| 30–36 | 957(34.6) | 532(34.6) | 425(34.6) | ||
| Race/Ethnicity | 0.02 | ||||
| White | 2313(83.6) | 1301(84.6) | 1012(82.3) | ||
| Black | 200(7.2) | 113(7.3) | 87(7.1) | ||
| Hispanic | 151(5.5) | 78(5.1) | 73(5.9) | ||
| Asian | 54(2) | 18(1.2) | 36(2.9) | ||
| Other | 49(1.8) | 28(1.8) | 21(1.7) | ||
| Education | <0.01 | ||||
| High school degree or less | 440(15.9) | 259(16.8) | 181(14.7) | ||
| Some college | 743(26.9) | 441(28.7) | 302(24.6) | ||
| College degree or higher | 1584(57.2) | 838(54.5) | 746(60.7) | ||
| Poverty Status | 0.96 | ||||
| Poverty | 223(8.6) | 125(8.6) | 98(8.5) | ||
| Near Poverty | 224(8.6) | 127(8.7) | 97(8.4) | ||
| Not Poverty | 2157(82.8) | 1201(82.7) | 956(83.1) | ||
| Marital Status | 0.03 | ||||
| Married | 1962(70.9) | 1057(68.8) | 905(73.6) | ||
| Living with partner | 494(17.9) | 299(19.5) | 195(15.9) | ||
| Not living with partner | 173(6.3) | 100(6.5) | 73(5.9) | ||
| Not partnered | 137(5) | 81(5.3) | 56(4.6) | ||
| Gestational age at delivery, weeks—mean (SD) | 39.4 (1.1) | 39.5 (1.2) | 39.4 (1.1) | 0.34 | |
| Smokes Daily | <0.01 | ||||
| Yes | 102(3.7) | 70(4.6) | 32(2.6) | ||
| No | 2665(96.3) | 1468(95.4) | 1197(97.4) | ||
Figure.
Proportions of women who are below, within, and exceed IOM recommended Gestational Weight Gain (GWG), by pre-pregnancy weight category, N=2,767.
The majority of the women participated in at least some physical activity during pregnancy, with 41.2% engaging in 60–149 min and 32.1% engaging in at least 150 min of physical activity/week, although 26.8% engaged in less than 60 minutes of physical activity/week. The most common physical activity women reported engaging in was walking, with 81.6% reporting walking slowly and 60.0% reporting brisk walking. Smaller percentages of women reported swimming (18.9%), dancing (11.8%), participating in prenatal exercise classes (11.0%), and jogging (8.2%) during pregnancy (data not shown). Women who were inactive (< 60 min/week), minimally active (60 – 149 min/week) and active (150 min/week or more) gained a mean of 16.2 (SD 6.9), 15.6 (SD 6.0), and 15.2 (SD 5.9) kg, respectively; the difference in mean weight gain between the inactive and active women was statistically significant (p<0.05). Physical activity level was also associated with exceeding/not exceeding the IOM GWG recommendations by weight category—as shown in Table 1, physical activity level was associated with not exceeding recommended GWG (p<0.01) in bivariate analysis. Women who were active were more likely to gain the recommended weight (51%) than those who were minimally active (43%) or inactive (40%). When examined within each BMI category, women who were active were less likely to have excessive GWG compared to women who were inactive, although results were not statistically significant. There was no interaction between BMI category and physical activity. Other significant bivariate predictors of exceeding GWG recommendations included lower educational attainment and smoking daily during pregnancy. Race/ethnicity was also significantly associated with GWG, with Asian women less likely to exceed GWG recommendations.
In the adjusted analysis (Table 2), meeting the physical activity guidelines during pregnancy was associated with 29% lower odds of exceeding the IOM recommendations for GWG compared with inactive women. Women who were minimally active (60 – 149 min/week) had the same odds of exceeding GWG recommendations as inactive women. Overweight and obese women had increased odds of exceeding GWG recommendations compared to women with normal weight women (5.11 and 2.35, respectively). Women who were 30–36 years old (compared with women 18–24), women who were not college graduates (compared to college graduates), and unmarried women living with their partners were also significantly more likely to exceed the GWG recommendations. Asian women had significantly lower odds of exceeding the GWG recommendations.
Table 2.
Logistic regression modeling exceeding GWG recommendations, N=2,603.
| Factor/Variable Name | Exceeds GWG recommendations Adjusted OR (95% CI) | |
|---|---|---|
| Physical activity during pregnancy | ||
| Inactive (<60 min/wk) | Reference | |
| Minimally active (60–149 min/wk) | 0.97 (0.79–1.2) | |
| Active (≥150 min/wk) | 0.71(0.57–0.88) | |
| Prepregnancy weight category | ||
| Normal weight | Reference | |
| Overweight | 5.11 (4.08–6.4) | |
| Obese | 2.35 (1.91–2.89) | |
| Age group—years | ||
| 18–24 | Reference | |
| 25–29 | 1.28 (0.96–1.7) | |
| 30–36 | 1.45 (1.07–1.96) | |
| Race/Ethnicity | ||
| White | Reference | |
| Black | 0.86 (0.58–1.27) | |
| Hispanic | 0.68 (0.45–1.02) | |
| Asian | 0.51 (0.27–0.96) | |
| Other | 1.02 (0.55–1.88) | |
| Education | ||
| High school degree or less | 1.46 (1.05–2.03) | |
| Some college | 1.23 (0.98–1.53) | |
| College degree or higher | Reference | |
| Poverty Status | ||
| Poverty | 0.85 (0.6–1.2) | |
| Near Poverty | 0.86 (0.62–1.19) | |
| Not Poverty | Reference | |
| Marital Status | ||
| Married | Reference | |
| Living with partner | 1.48 (1.13–1.94) | |
| Not living with partner | 1.37 (0.88–2.14) | |
| Not partnered | 1.46 (0.91–2.34) | |
| Gestational age at delivery, weeks—mean (SD) | 1.02 (0.95–1.1) | |
| Smokes Daily | ||
| Yes | 1.49 (0.9–2.49) | |
| No | Reference | |
Discussion
Our main finding was that greater than 150 minutes per week of physical activity during pregnancy, in concordance with national guidelines (Physical Activity Guidelines Advisory Committee, 2008), was associated with 29% lower odds of exceeding GWG recommendations. Interestingly, lower levels of physical activity (60–149 minutes per week) were not protective against excessive GWG. Several studies, including randomized controlled trials, have demonstrated the inverse relationship between exercise and GWG, supporting the role of IOM recommendations that prenatal care providers offer counseling on physical activity (Institute of Medicine [IOM] & National Research Council [NRC], 2009; Phelan, 2010; Stuebe et al., 2009). For example, Stuebe and colleagues (2009) demonstrated that vigorous physical activity in the second trimester resulted in a 24% lower odds of exceeding GWG. Unfortunately, pregnancy is a time of decreased physical activity for most women (Pereira et al., 2007). Pregnancy may serve as an ideal time for prenatal care providers to target weight control and healthful activities such as meeting physical activity guidelines, given its characterization as a “teachable moment” (Phelan, 2010). However, our current understanding of prenatal provider counseling patterns suggests more than one-third of women do not receive any advice regarding GWG (Ferrari & Siega-Riz, 2012; Stotland et al., 2005). Further, pregnant women who do receive counseling may not be advised to meet federal guidelines for physical activity, as a recent survey found that greater than one-quarter of obstetricians did not believe moderate intensity exercise was beneficial (Evenson & Pompeii, 2010). Our study findings highlight the importance of meeting the physical activity guidelines to moderate GWG and suggest that healthcare providers encourage their prenatal patients to meet the guidelines and emphasize that engaging in only “some activity” may not be sufficient to control GWG.
The majority of first-time mothers (55.6%) in our study exceeded the current IOM guidelines for GWG. These findings are comparable to other recent studies examining guideline-concordant weight gain (Ferrari & Siega-Riz, 2012; Stuebe et al., 2009). Stuebe and colleagues (2009) found 51% of women in their prospective cohort (n= 1,388) experienced excessive gestational weight gain. Ferrari and colleagues (2012) demonstrated that 78% of women in their prospective cohort (n = 1,454) had exceeded recommended weight gain. We found that while normal and overweight women gained similar amounts of weight in pregnancy, obese women gained significantly less weight in comparison. However, the mean weight gain in all three BMI categories exceeded IOM guidelines. Particularly concerning is the finding that overweight women were at significantly increased risk of excessive GWG, with greater than 5 times the odds of excessive GWG compared to normal weight women. This elevated risk is particularly concerning because excessive GWG is known to increase postpartum weight retention (Callaway et al., 2007; Linne, Dye, Barkeling, & Rossner, 2003; Linne, Dye, Barkeling, & Rossner, 2004). Therefore, higher rates of weight gain in overweight women further threatens their post-pregnancy health. As the second most preventable cause of death (Mokdad et al., 2001), obesity is a risk factor for cardiovascular disease, stroke, several types of cancer, and diabetes mellitus (Thompson, Edelsberg, Colditz, Bird, & Oster, 1999). Also of concern is the limited intervention evidence for moderating GWG among overweight and obese pregnant women. That is, while interventions have been able to modify GWG among normal weight women (Phelan et al., 2011; Polley, Wing, & Sims, 2002; Ruchat et al., 2012), few, if any, interventions have effectively moderated GWG in overweight/obese women. This remains an important area of future research.
This study has several limitations. First, participant height, weight, and GWG were obtained by self-report. However, women’s self-report of pre-pregnancy weight has been validated (Oken, Taveras, Kleinman, Rich-Edwards, & Gillman, 2007). Further, as self-report has been shown to underestimate weight when compared with objective measures, this would suggest even greater rates of excessive GWG than demonstrated (Elgar & Stewart, 2008; Stomme & Schoenborn, 2009). Another limitation is that physical activity was obtained by participant self-report, however, this methodology remains widely used despite overestimating activity when compared to objective measures (Chasan-Taber, Evenson, Sternfeld, & Kengeri, 2007). Although the physical activity questionnaire used was not validated, it parallels the Leisure-Time Exercise Questionnaire (LTEQ), a validated measure of physical activity. The LTEQ and other physical activity measures have been similarly adapted in recent years to convert metabolic equivalents (METS) to bouts and minutes of physical activity, in order to parallel the federal physical activity guidelines. An additional limitation is the potential for residual confounding not controlled for in our analysis. For example, pre-pregnancy physical activity and dietary intake were not assessed, which may predict gestational weight gain and gestational physical activity, respectively. We also did not account for the specific types or levels of physical activity in which women engaged, outside of “moderate”. However, the IOM report concluded that the evidence base remains too limited to draw conclusions for these factors (Institute of Medicine [IOM] & National Research Council [NRC], 2009). Lastly, our study is limited in its ability to generalize these results to other populations. Women in the First Baby Study were older, more likely to be White, more education, more likely to have private insurance, and less likely to smoke than the general population of women having their first, singleton birth ([referenced blinded by WHI editors]).
Our study also has important strengths. The First Baby Study is a large observational study which allows for the determination of associations limited by smaller studies. Further, the study design allowed weight and physical activity data to be obtained during pregnancy, thereby limiting participant recall bias. Our finding that guideline-concordant physical activity was associated with decreased gestational weight gain in this population further supports that real-world activity, outside of clinical interventions, is effective.
Implications for Practice and/or Policy
Our findings reveal high rates of excessive GWG, especially among women with overweight and obesity. We also demonstrated that only guideline-concordant levels of physical activity, and not less, were inversely associated with GWG. The association of guideline-concordant physical activity with appropriate GWG suggests this is an important target for future interventions. Provider-based interventions during pregnancy may be particularly relevant given pregnancy is a particularly “teachable” moment for weight control (Phelan, 2010). Appropriate GWG and physical activity should be encouraged among all pregnant women, in accordance with current guidelines (Institute of Medicine [IOM] & National Research Council [NRC], 2009), to reduce both short-term pregnancy complications and the long-term risks of overweight and obesity.
Acknowledgements
We acknowledge the support of this research by grant number R01 HD052990 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development, National Institutes of Health. Dr. Kraschnewski is supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1RR033184 and KL2RR033180. Dr. Chuang is supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K23 HD051634). Dr. Kraschnewski had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Statement
The authors report no conflict of interest.
Contributor Information
Jennifer L. Kraschnewski, Assistant Professor of Medicine and Public Health Sciences, Penn State Milton S. Hershey Medical Center, Penn State College of Medicine, 500 University Drive, H034, Hershey, PA 17033, Phone: 717-531-8161, Fax: 717-531-7726, jkraschnewski@hmc.psu.edu.
Cynthia H. Chuang, Assistant Professor of Medicine and Public Health Sciences, Penn State Milton S. Hershey Medical Center, Penn State College of Medicine, 500 University Drive, H034, Hershey, PA 17033, Phone: 717-531-8161, Fax: 717-531-7726, cchuang@hmc.psu.edu.
Danielle Symons Downs, Associate Professor of Kinesiology and Obstetrics and Gynecology, 268Q Recreation Building, The Pennsylvania State University, University Park, PA 16802, Phone: 814-863-0456, Fax: 814-865-1275, dsd11@psu.edu.
Carol S. Weisman, Associate Dean for Faculty Affairs, Distinguished Professor of Public Health Sciences and Obstetrics and Gynecology, Penn State College of Medicine, 600 Centerview Drive, A210, Hershey, PA 17033, Phone: 717-531-6690, Fax: 717-531-5779, cweisman@psu.edu.
Eric L. McCamant, Resident 1, Medicine Resident, Penn State College of Medicine, 500 University Drive, H034, Hershey, PA 17033, Phone: 717-531-8161, Fax: 717-531-7726, emccamant@hmc.psu.edu.
Kesha Baptiste-Roberts, Assistant Professor of Nursing, Penn State College of Medicine, 600 Centerview Drive, A110, Hershey, PA 17033, Phone: 717-531-4211, Fax: 717-531-5339, kab50@psu.edu.
Junjia Zhu, Assistant Professor, Division of Biostatistics and Bioinformatics, Department of Public Health Sciences, Penn State College of Medicine, 600 Centerview Drive, A210, Hershey, PA 17033, Phone: 717-531-1509, Fax: 717-531-5779, jxz203@psu.edu.
Kristen H. Kjerulff, Professor of Public Health Sciences and Obstretics and Gynecology, Penn State College of Medicine, 600 Centerview Drive, A210, Hershey, PA 17033, Phone: 717-531-7178, Fax: 717-531-5779, khk2@psu.edu.
References
- ACOG committee opinion. Exercise during pregnancy and the postpartum period. Number 267, January 2002. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 2002;77(1):79–81. doi: 10.1016/s0020-7292(02)80004-2. [DOI] [PubMed] [Google Scholar]
- Baeten JM, Bukusi EA, Lambe M. Pregnancy complications and outcomes among overweight and obese nulliparous women. Am J Public Health. 2001;91(3):436–440. doi: 10.2105/ajph.91.3.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaway LK, McIntyre HD, O'Callaghan M, Williams GM, Najman JM, Lawlor DA. The association of hypertensive disorders of pregnancy with weight gain over the subsequent 21 years: findings from a prospective cohort study. Am J Epidem. 2007;166(4):421–428. doi: 10.1093/aje/kwm099. [DOI] [PubMed] [Google Scholar]
- Chasan-Taber L, Evenson KR, Sternfeld B, Kengeri S. Assessment of recreational physical activity during pregnancy in epidemiologic studies of birthweight and length of gestation: methodologic aspects. Women Health. 2007;45(4):85–107. doi: 10.1300/J013v45n04_05. [DOI] [PubMed] [Google Scholar]
- Chu SY, Callaghan WM, Bish CL, D’Angelo D. Gestational weight gain by body mass index among US women delivering live births, 2004–2005: fueling future obesity. Am J Obstet Gynecol. 2009;200(3):271, e1–e7. doi: 10.1016/j.ajog.2008.09.879. [DOI] [PubMed] [Google Scholar]
- Elgar FJ, Stewart JM. Validity of self-report screening for overweight and obesity. Evidence from the Canadian Community Health Survey. Can J Public Health. 2008;99(5):423–427. doi: 10.1007/BF03405254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evenson KR, Pompeii LA. Obstetrician practice patterns and recommendations for physical activity during pregnancy. J Womens Health (Larchmt) 2010;19(9):1733–1740. doi: 10.1089/jwh.2009.1833. [DOI] [PubMed] [Google Scholar]
- Ferrari RM, Siega-Riz AM. Provider Advice About Pregnancy Weight Gain and Adequacy of Weight Gain. Matern Child Health J. 2012 doi: 10.1007/s10995-012-0969-z. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- Furuno JP, Gallicchio L, Sexton M. Cigarette smoking and low maternal weight gain in Medicaid-eligible pregnant women. J Womens Health (Larchmt) 2004;13(7):770–777. doi: 10.1089/jwh.2004.13.770. [DOI] [PubMed] [Google Scholar]
- IOM (Institute of Medicine), NRC (National Research Council) Weight Gain During Pregnancy: Reexamining the Guidelines. Washington, DC: 2009. [reference blinded by WHI editors for peer review] [Google Scholar]
- Linne Y, Dye L, Barkeling B, Rossner S. Weight development over time in parous women--the SPAWN study--15 years follow-up. Int J Obes Relat Metab Disord. 2003;27(12):1516–1522. doi: 10.1038/sj.ijo.0802441. [DOI] [PubMed] [Google Scholar]
- Linne Y, Dye L, Barkeling B, Rossner S. Long-term weight development in women: a 15-year follow-up of the effects of pregnancy. Obes Res. 2004;12(7):1166–1178. doi: 10.1038/oby.2004.146. [DOI] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S, Munson ML. Births: final data for 2005. Natl Vital Stat Rep. 2007;56(6):1–103. [PubMed] [Google Scholar]
- Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, Marks JS. Prevalence of obesity, diabetes, and obesity-related health risk factors. JAMA. 2001;289(1):76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- Nohr EA, Vaeth M, Baker JL, Sorensen T, Olsen J, Rasmussen KM. Combined associations of prepregnancy body mass index and gestational weight gain with the outcome of pregnancy. Am J Clin Nutr. 2008;87(6):1750–1759. doi: 10.1093/ajcn/87.6.1750. [DOI] [PubMed] [Google Scholar]
- Oken E, Taveras EM, Kleinman KP, Rich-Edwards JW, Gillman MW. Gestational weight gain and child adiposity at age 3 years. Am J Obstet Gynecol. 2007;196(4):322, e1–e8. doi: 10.1016/j.ajog.2006.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira MA, Rifas-Shiman SL, Kleinman KP, Rich-Edwards JW, Peterson KE, Gillman MW. Predictors of change in physical activity during and after pregnancy: Project Viva. Am J Prev Med. 2007;32(4):312–319. doi: 10.1016/j.amepre.2006.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan S. Pregnancy: a "teachable moment" for weight control and obesity prevention. Am J Obstet Gynecol. 2010;202(2):135, e1–e8. doi: 10.1016/j.ajog.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan S, Phipps MG, Abrams B, Darroch F, Schaffner A, Wing RR. Randomized trial of a behavioral intervention to prevent excessive gestational weight gain: the Fit for Delivery Study. Am J Clin Nutr. 2011;93(4):772–779. doi: 10.3945/ajcn.110.005306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report. Washington, DC: U.S. Department of Health and Human Services; 2008. [DOI] [PubMed] [Google Scholar]
- Polley BA, Wing RR, Sims CJ. Randomized controlled trial to prevent excessive weight gain in pregnant women. Int J Obes Relat Metab Disord. 2002;26(11):1494–1502. doi: 10.1038/sj.ijo.0802130. [DOI] [PubMed] [Google Scholar]
- Ruchat SM, Davenport MH, Giroux I, Hillier M, Batada A, Sopper MM, Hammond JM, Mottola MF. Nutrition and Exercise Reduce Excessive Weight Gain in Normal-Weight Pregnant Women. Med Sci Sports Exerc. 2012;44(8):1419–1426. doi: 10.1249/MSS.0b013e31825365f1. [DOI] [PubMed] [Google Scholar]
- Stommel M, Schoenborn CA. Accuracy and usefulness of BMI measures based on self-reported weight and height: findings from the NHANES & NHIS 2001–2006. BMC Public Health. 2009;9:421. doi: 10.1186/1471-2458-9-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stotland NE, Haas JS, Brawarsky P, Jackson RA, Fuentes-Afflick E, Escobar GJ. Body mass index, provider advice, and target gestational weight gain. Obstet Gynecol. 2005;105(3):633–638. doi: 10.1097/01.AOG.0000152349.84025.35. [DOI] [PubMed] [Google Scholar]
- Stuebe AM, Oken E, Gillman MW. Associations of diet and physical activity during pregnancy with risk for excessive gestational weight gain. Am J Obstet Gynecol. 2009;201(1):58, e1–e8. doi: 10.1016/j.ajog.2009.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson D, Edelsberg J, Colditz GA, Bird AP, Oster G. Lifetime health and economic consequences of obesity. Arch Intern Med. 1999;159(18):2177–2183. doi: 10.1001/archinte.159.18.2177. [DOI] [PubMed] [Google Scholar]
- Viswanathan M, Siega-Riz AM, Moos MK, Deierlein A, Mumford S, Knaack J, Thieda P, Lux LJ, Lohr KN. Outcomes of maternal weight gain. Evid Rep Technol Assess (Full Rep) 2008;168:1–223. [PMC free article] [PubMed] [Google Scholar]
- Weisman CS, Hillemeier MM, Downs DS, Chuang CH, Dyer AM. Preconception predictors of weight gain during pregnancy: prospective findings from the Central Pennsylvania Women's Health Study. Womens Health Issues. 2010;20(2):126–132. doi: 10.1016/j.whi.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]