Abstract
Since infection with Helicobacter pylori has been suggested to play a pathogenic role in diabetes mellitus, we investigated whether eradication therapy for H. pylori might affect glycemic control in Japanese subjects with type 2 diabetes. A total of 72 subjects (55 males, 17 females; aged 63.7 years) with type 2 diabetes who received eradication therapy for H. pylori were included. The change of their blood glycosylated hemoglobin (A1C) levels 3 months before (−3 m) the H. pylori eradication, as well as 3 months (3 m) and 6 months (6 m) after were evaluated. Their A1C levels did not show any significant change after therapy {6.9 [0.1]% (−3 m) to 7.0 [0.1]% (3 m); P = 0.3, 7.0 [0.1] (6 m); P = 0.3}. Our findings suggest that the eradication therapy for H. pylori does not, at least profoundly, affect glycemic control in Japanese subjects with type 2 diabetes.
Keywords: helicobacter pylori, eradication, diabetes
Introduction
Recently, it has been suggested that infection with Helicobacter pylori may have a pathogenic role in diabetes mellitus.1–3 However, there is no definite evidence regarding the role of H. pylori infection that may cause insulin resistance. In the present study, we aimed to elucidate whether H. pylori deteriorates glycemic control in subjects with diabetes mellitus. To do so, we retrospectively investigated the effect of eradication therapy on H. pylori and how it might affect glycemic control in Japanese subjects with type 2 diabetes.
Subjects and Methods
The study included a total of 72 subjects with type 2 diabetes who received eradication therapy for H. pylori during 6 years from 2006 to 2011. Subjects gave their oral consent for use of their clinical data in this study. They included 55 male and 17 female subjects, aged 63.7 [standard error (SE) 1.1] years, and we checked A1C levels regularly in our division. At first, the subjects were pathologically diagnosed with H. pylori infection by upper gastrointestinal endoscopy. The eradication therapy for H. pylori was performed using oral administration of amoxicillin 1500 mg/day, clarithromycin 800 mg/day with lansoprazole 60 mg/day (n = 65) or omeprazole 40 mg/day (n = 2), or rabeprazole 40 mg/ day (n = 5) for 7 days. The eradication was evaluated by urea breath test and the subjects who failed to eradicate H. pylori were excluded. The blood glycosylated hemoglobin (A1C) levels were evaluated 3 months before (−3 m) the eradication therapy, as well as 3 months (3 m) and 6 months (6 m) after. The subjects had been treated with sulfonylureas (58.3%), alpha-glucosidase inhibitors (19.4%), biguanides (18.1%), dipeptidyl pep-tidase-4 inhibitors (9.7%), glinides (4.2%) and thiazo-lidinedione (1.4%), or with insulin (11.1.%); 27.8% of subjects did not receive any medications. An unpaired t-test was used to compare A1C levels before and after the eradication. Statistical analysis was performed with SPSS-II (SPSS Inc, Chicago, IL, USA) for WINDOWS® (Microsoft Corporation, Redmond, WA).
Results
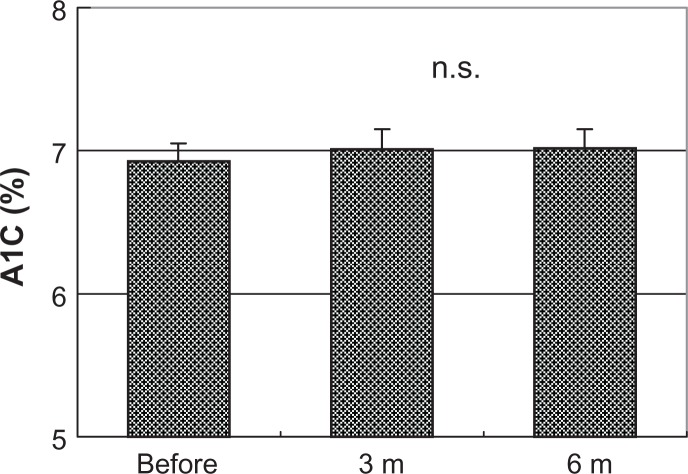
The A1C levels before and after the eradication therapy for H. pylori did not show any significant changes in subjects with type 2 diabetes {6.9 [0.1]% (−3 m) to 7.0 [0.1]% (3 m); P = 0.3, 7.0 [0.1] (6 m); P = 0.3} (Fig. 1). Scatter plotting also revealed that the A1C levels of each subject had not been changed during the study period (Fig. 2).
Figure 1.
Change in A1C levels before 3 m, as well as after 3 m and 6 m of H. pylori eradication.
Note: There was no significant change in A1C levels.
Figure 2.
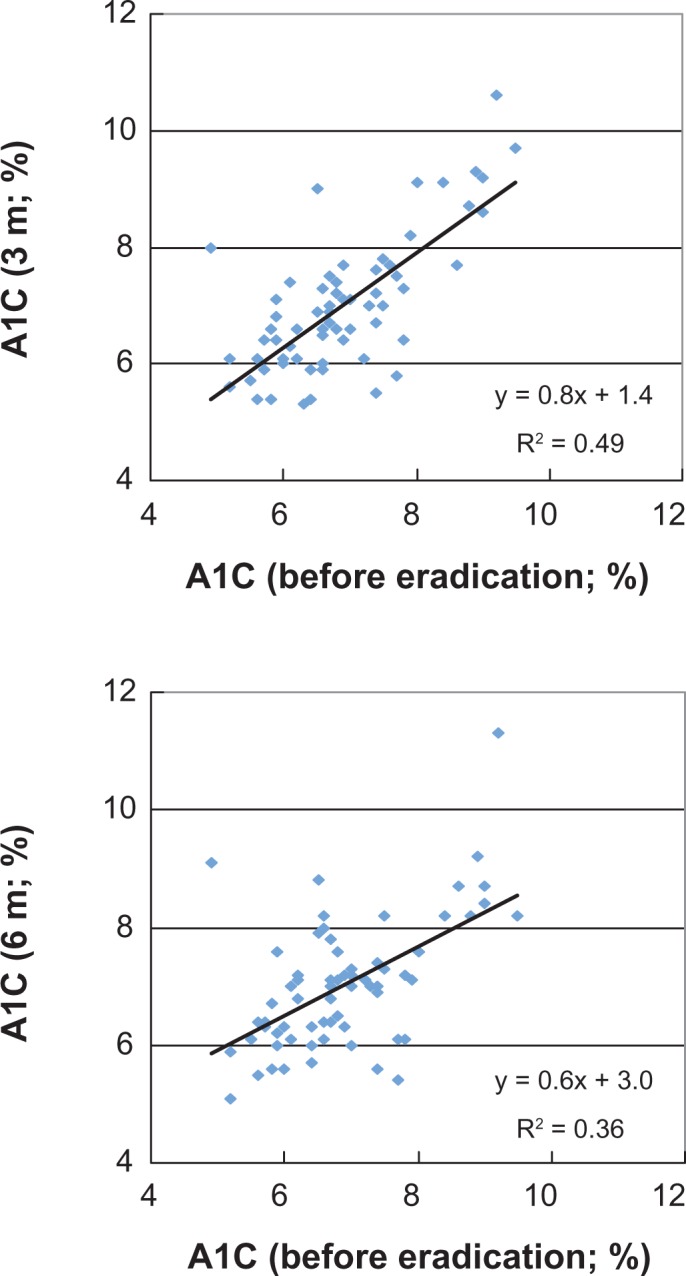
Scatter plotting of each A1C level before and after H. pylori eradication (upper: 3 m before and 3 m after the eradication; lower: before 3 m and 6 m after the eradication).
Note: A1C levels did not show significant changes before and after the eradication.
Discussion
Infection with H. pylori has been recently suggested to be associated with an increased rate of diabetes mellitus.2 A previous report found that H. pylori infection might be associated with insulin-dependent diabetes mellitus.1 A case report from Japan has also suggested that the eradication of H. pylori may result in the amelioration of insulin resistance in a patient with type B insulin resistance, (ie, insulin receptor autoantibodies).3 However, another case report from Japan indicated that the eradication of H. pylori might trigger the onset of type 1 diabetes.4
Although our study is limited by the fact that it is a retrospective analysis from one center with a small number of subjects, the present findings suggest that eradication therapy for H. pylori does not, at least profoundly, affect glycemic control in Japanese subjects with type 2 diabetes. Further investigation is needed to determine whether autoantibodies against insulin or islet cells possibly triggered by H. pylori infection might be an irreversible process.
Conclusion
The eradication therapy for H. pylori does not seem to affect glycemic control in Japanese subjects with type 2 diabetes.
Footnotes
Author Contributions
Conceived and designed the experiments: YW, YH, HK. Analyzed the data: YW, JF. Wrote the first draft of the manuscript: YW, YH, HK. Contributed to the writing of the manuscript: YW, YH, YK, SH, KF, HT, AM, HI, JF, HK. Agree with manuscript results and conclusions: YW, YH, YK, SH, KF, HT, AM, HI, JF, HK. Jointly developed the structure and arguments for the paper: YW, YH, YK, SH, KF, HT, AM, HI, JF, HK. Made critical revisions and approved final version: YW, YH, YK, SH, KF, HT, AM, HI, JF, HK. All authors reviewed and approved of the final manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Kitano hospital received research grant from Merck Sharp and Dohme (MSD) Japan, Novo nordisk Pharma, Elli Lilly and Company Japan, Mitsubishi Tanabe Pharma Bohringer-Ingelheim, and Astellas Pharma.
Competing Interests
Author(s) disclose no potential conflicts of interest.
Disclosures and Ethics
This manuscript has been read and approved by all authors. The authors have read and confirmed their agreement with the ICMJE authorship and conflict of interest criteria. The authors have also confirmed that this article is unique and not under consideration or published in any other publication, and that they have permission from rights holders to reproduce any copyrighted material. Any disclosures are made in this section. The external blind peer reviewers report no conflicts of interest.
References
- 1.de Luis DA, de la Calle H, Roy G, et al. Helicobacter pylori infection and insulin-dependent diabetes mellitus. Diabetes Res Clin Pract. 1998;39(2):143–6. doi: 10.1016/s0168-8227(97)00127-7. [DOI] [PubMed] [Google Scholar]
- 2.Jeon CY, Haan MN, Cheng C, et al. Helicobacter pylori infection is associated with an increased rate of diabetes. Diabetes Care. 2012;35(3):520–5. doi: 10.2337/dc11-1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Imai J, Yamada T, Saito T, et al. Eradication of insulin resistance. Lancet. 2009;374(9685):264. doi: 10.1016/S0140-6736(09)60872-2. [DOI] [PubMed] [Google Scholar]
- 4.Tada A, Komiya N, Shimada A, Katsuki T, Oikawa Y, Itoh H. Eradication of Helicobacter pylori may trigger onset of type 1 diabetes: a case report. Ann N Y Acad Sci. 2008;1150:208–9. doi: 10.1196/annals.1447.001. [DOI] [PubMed] [Google Scholar]