Abstract
National survey data suggest that new mothers have high prevalences of alcohol and illicit drug use. Depression correlates with substance use, and new mothers with postpartum depression (PPD) may be at high risk for substance use. Understanding postpartum substance use and its relationship to PPD can inform future research and intervention. A literature search was conducted resulting in 12 studies published from 1999–2012 examining postpartum alcohol use, drug use, or combined postpartum depression and substance use. Postpartum alcohol (prevalence range 30.1%−49%) and drug use (4.5%–8.5%) were lower than use among not pregnant, not postpartum women (41.5%–57.5%; 7.6%–10.6%, respectively) but higher than use among pregnant women (5.4%–11.6%; 3.7%–4.3%, respectively). Correlates of postpartum problem drinking were being unemployed, unmarried, and a cigarette smoker. Prevalence of drug use was highest among white new mothers, followed by Blacks and Hispanics, but Black new mothers appeared at greater risk of drug use. No identified studies examined correlates of postpartum drug use beyond race/ethnicity. Postpartum depressive symptoms were prevalent among postpartum substance users and those with a substance use history (19.7%–46%). The postpartum period is a critical time. Prevalent substance use and the scarcity of studies warrant research to identify means to reduce maternal substance use.
Keywords: alcohol, depression, drug use, postpartum
Introduction
National survey data from 2002–2003 showed that 14.9% of postpartum women (child aged <1 year) who were aged 15–44 years reported binge alcohol use, and 8.5% reported use of illicit or nonmedical drugs in the past month (SAMHSA 2005a). While lower than prevalences among not pregnant, not postpartum women aged 15–44 years (23.8%; 10.6%, respectively), these prevalences were higher than those of pregnant women aged 15–44 years (4.1%; 4.3%, respectively) and similar to or higher than those reported for women in a prior national survey of the general population, which included women aged 12 years or older regardless of pregnancy or parenting status (15.1% ; 6.4%, respectively) (SAMHSA 2003; SAMHSA 2005b). The initial decrease in illicit drug and binge alcohol use during pregnancy followed by an increase in use similar to that of women in the general population suggests that women who stop illicit drug and binge alcohol use in pregnancy only pause their use, and that this is a missed prevention opportunity. Postpartum alcohol and drug use may have serious consequences because they can limit a mother’s ability to stay emotionally connected to her infant, adjust to his or her rhythms and behaviors, and anticipate or follow his or her development (Pajulo et al. 2012). Women who also used substances prenatally faced added difficulties in infants’ potentially limited ability to regulate wakefulness, sleep, or distress due to in-utero exposure (Pajulo et al. 2012). Depression significantly correlates with substance use and disorders via multiple processes (e.g., self-medication) (Wu, Kouzis, and Leaf 1999; Lazareck et al. 2012). Women with postpartum depression (PPD) may be at greater risk for substance use compared with women without. PPD is a subtype of major depression that probably affects up to 14.5% of mothers in its peak period, or the first three months postpartum (APA 2000; Gavin et al. 2005). Little research has examined the relationship between PPD and substance use (Ross and Dennis 2009), but women with depression in pregnancy may be more likely to consume alcohol than those without (Flynn and Chermack 2008; Marcus 2009), and pregnant women who drink have elevated odds of experiencing PPD (Marcus 2009). Maternal alcohol and drug abuse can contribute to child neglect, abuse, and the number of children in foster care (VanDeMark et al. 2005; Morton and Konrad 2009; Pajulo et al. 2012). Children of depressed mothers are at increased risk of neglect and abuse (Burke 2003). Because the postpartum period is a transitional one when new behaviors are established and old behaviors abandoned, it is a critical time to intervene (Fleming et al. 2008). Understanding this time as one of unique vulnerability may also be critical to improving maternal abstinence, particularly among women with alcohol or drug use problems (Rutherford et al. 2011). Understanding the extent and specific patterns of substance use as well as its relationship with PPD could inform risk factor research and designs of targeted interventions to prevent or reduce substance use related problems and consequences. To facilitate research on postpartum substance use and its relationship to PPD, we reviewed the empirical evidence on alcohol and illicit drug use among postpartum women and research on combined substance use and PPD, concluding with a discussion of areas of needed research and suggestions for future studies. Due to extant reviews on postpartum tobacco use and substance use while breastfeeding (Fang et al. 2004; Giglia and Binns 2006; Forest 2009; Giglia 2010), we focused this review on alcohol use and illicit or nonmedical drug use.
Materials and Methods
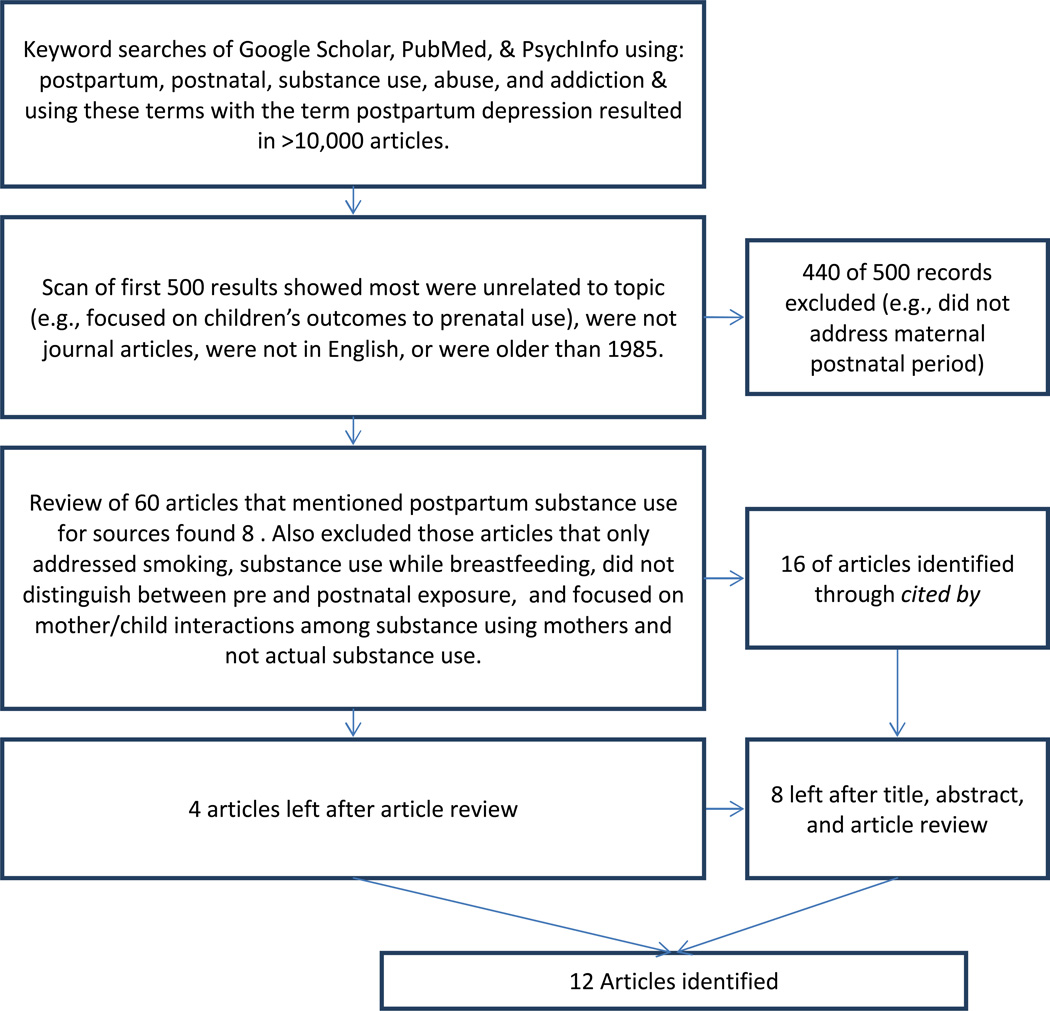
Searches of Google Scholar, PsychInfo, and PubMed using variations of keywords postpartum, postnatal, substance use, abuse, addiction, and PPD, without language or date restrictions, identified over 10,000 articles (Figure 1). A title scan of the first 500 results showed the most relevant articles appeared first, based on the number and frequency of keywords in each article, but most articles related to prenatal drug use and child outcomes with little or no mention of the maternal postpartum period (i.e., up to two years following the birth of a child). Of the first 500 results, we eliminated those that did not mention the maternal postnatal period, were not in English, were older than 1985, or were not journal articles (n=440). Additional exclusion criteria were a focus on substance use while breastfeeding, smoking, mother/child interaction among substance-using mothers and not actual substance use, and failure to distinguish between pre and postnatal use (n=52). From the remaining articles, we downloaded relevant-looking sources, and used the cited by feature of Google Scholar to find additional articles. With the exception of one article that also addressed PPD, articles on adolescent mothers have been reported elsewhere (Chapman and Wu 2013). Twelve studies published from 1999–2012 met our review criteria and were included in this review. Six studied alcohol by postpartum status, discussed first. Two examined illicit drug use, discussed second. We then reviewed six studies that discussed PPD and substance use in combination to examine whether and how PPD might contribute to substance use and concluded with implications and suggestions for future research.
Figure 1.
Summary of the literature search and inclusion
Results
Alcohol
Five cross-sectional studies published from 2007–2011 examined postpartum alcohol use (Table 1). Three used large samples (n≥8,706) and provided prevalences of alcohol use for postpartum women (Laborde and Mair 2011; Muhuri and Gfroerer 2009; Jagodzinski and Fleming 2007a). Two analyzed subsamples (≤381) identified from larger studies (Fleming et al. 2008; Jagodzinski and Fleming 2007b). An additional study examined prenatal and postpartum alcohol use, following women from pregnancy through six to ten weeks postpartum in New Zealand (McLeod et al., 2002). None of the studies reported on substance use disorders. Only two addressed postpartum depression (Fleming et al. 2008; Jagodzinski and Fleming 2007b).
Table 1.
Studies related to postpartum alcohol use
| Authors | Year | Sample N |
Race/ Ethnicity |
Data source & Study Design |
Pregnancy Status & Drinking Prevalence |
Additional Findings |
|---|---|---|---|---|---|---|
| Laborde & Mair (2011) | 1997–2008 | 28,537 (3,448 new mothers) | New Mothers 34.8% White, 46.4% Hispanic, 5.9% Black, 12% Other | CA Women’s Health Survey | Not Pregnant 52.5% Any**; 11.7% Binge Drink; 5.8% Binge Drink >1 |
Variables Positively Associated with: Any Drinking = Working Part-Time (OR=1.31, CI 0.97–1.77), Smoking (OR=1.61, CI 1.14–2.26); Drinking Frequency= Higher Income >$75k (OR=2.84, CI 0.86–9.43); Binge Drinking = Never Married (Ref), >$75k (OR=1.59, CI 1.26–2.00); Binge Drinking >2 times = Never Married (N/A), >$75k (OR= 1.37 CI=1.03–1.38), Ever Smoke (OR=4.20 CI 3.63–4.86), Self Employed (OR=3.34 CI 1.00–11.06), Unemployed (OR=2.31, CI 1.01–5.26) |
| Cross Sectional | ||||||
| Pregnant N/A | ||||||
| Postpartum 36.7% Any*; 8.4% Frequently**; 5.6% Binge Drink; 2.9% Binge Drink >1 | ||||||
|
Variables negatively associated with: Any Drinking = Tech. School or Some College (OR=0.68, CI 0.50–0.93), College or Post Grad. (OR=0.71, CI= 0.51–0.97); Binge Drinking & Binge Drinking >2 times= Aged 41–48 (OR=0.41, CI 0.35–0.49), Married (Ref); |
||||||
| Muhuri & Gfroerer (2009) | 2002–2006 | 94,483 | 63.8% White, 13.5% Black, 15.2% Hispanic, 7.2% Other | National Survey on Drug Use and Health | Not Pregnant 57.4% Any*; 25.8% Binge Drink | Pregnant & postpartum women had lower odds of drinking than not pregnant/not postpartum women. Variables Positively Associated with Alcohol Use while Pregnant*: white (OR=0.07, CI 0.06–0.09), Black (OR=0.11, CI 0.07–0.15), Hispanic (OR=0.08, CI 0.05–0.13); Variables Positively Associated with Alcohol Use while Postpartum*: white (OR= 0.73, CI 0.68–0.78), Black (OR=0.82, CI 0.71–0.95), Hispanic (OR= 0.78, CI 0.66–0.91) |
| Cross Sectional | Pregnant 10.5% Any*; 3.2% Binge Drink; | |||||
| Postpartum 49% Any*; 17.1% Binge Drink | ||||||
| Fleming et al., (2008) | 2002–2005 | 235 | 81% White, 7.2% Native American, 6.8% Black, | Wisconsin Women Cross | All women in the study were at risk drinkers | There was a high prevalence (38.7%) of depression. |
| 2.5% Hispanic | Sectional | |||||
| Jagodzinski & Fleming (2007a) | July 2002 – April 2005 | 8,706 | 81% White, 6.5% Hispanic, 5% Black, 3% Asian, 2% Native American | ≥ 18 years old, college educated, married women in WI | Not Pregnant 27.6% ≤ 1*** 13.6% >1–3***; 10.0% >3-<7***; 7.2%≥7***, |
Variables Positively Associated with Postpartum Risky Drinking: Pre Pregnancy Problem Drinking (OR=5.8, CI 4.6–7.2), Score as misusing alcohol on alcohol assessment (OR 4.2, CI 2.3–7.7), Smoking (OR=2.5, CI 2.1–3.0), Being Single (OR=1.5, CI 1.2–1.8); Variables Negatively Associated with Postpartum Risky Drinking: Breastfeeding (OR=0.3, CI 0.2–0.3), Black (OR=0.6, CI 0.4–0.8), aged >35 years (OR=0.7, CI 0.5–0.9), Not in Labor Force (OR=0.7, CI 0.6–0.9). |
| Cross Sectional | Pregnant 5.1 % ≤ 1***; 0.2% >1–3***; 0.06% >3-<7***; 0.02%≥7***; | |||||
| Postpartum 30.1% ≤ 1***; 8.2% >1–3***; 4.0% >3-<7***; 1.5%≥7***; | ||||||
| Jagodzinski & Fleming (2007b) | July 2002 – April 2005 | 381 | 87% White, 5.5% multiracial, 3.9% other, 3.7% as Black | Frequent drinkers from sample above | Postpartum 18% Problem drinking ≥ 2x a month; 5% ≥ 7 drinks a week; 15% Both |
Variables Positively Associated with Postpartum Risky Drinking: Risky Drinking Partner (OR=2.6, CI 1.5–4.5), Unemployed (OR= 3.0, CI 1.2–7.7), Smoke while Pregnant (OR=1.9, CI 1.0–3.5), Drink while Pregnant (OR=4.8, CI 2.2–10.6); Variables Negatively Associated with Postpartum Risky Drinking: Breastfeeding (OR=0.3, CI 0.2–0.5) |
| Cross Sectional | ||||||
| McLeod et al., (2002) | N/A | 665 | New Zealand (n=66 or 10% Maori) | Women registered for prenatal care | Pregnant 3.9% ≥ 3***; |
Variables Positively Associated with Postpartum Drinking: Tertiary education (OR=1.46, CI 1.02–2.08) Variable Negatively Associated with Postpartum Drinking: Community Service Card Holder (OR 0.44, CI 0.27–0.73) |
| Postpartum 16.4% ≥ 3*** | Prospective to 6–10 weeks postpartum | |||||
Any use in past 30 days
drinking >4 days in the past 30 days
drinks per week
Aggregate data from the 2006–2007 National Surveys on Drug Use and Health (NSDUH) showed a prevalence rate of any past-month alcohol use (42.1%) among postpartum mothers (child aged ≤ 1 year) (SAMHSA 2008). Prevalence of any past-month alcohol use was 54% among non-pregnant, non-postpartum women and 11.6% among pregnant women (SAMHSA 2008). The 2006–2007 NSDUH data also showed that older, better-educated, higher-income women drank less per occasion when compared to younger, less-educated, lower-income women (e.g., high school graduate: pregnant 2.6 drinks, postpartum 2.9 drinks, non-pregnant/non-postpartum 3.4 drinks vs. college graduate: pregnant 1.6 drinks, postpartum 1.7 drinks, non-pregnant/non-postpartum 2.2 drinks) (SAMHSA 2008).
Laborde and Mair (2011) analyzed data from the 1997–2008 California Women’s Health Surveys (CWHS) and compared alcohol use among new mothers (children aged < 1 year, n=3,448) with other women. New mothers were less likely to drink any alcohol in the past month (36.7% vs. 52.5%, respectively), drink frequently (drink > 4 days in the past month; 8.4% vs. 17.1%, respectively), binge drink (5.6% vs. 11.7%, respectively), or binge drink more than once (2.9% vs. 5.8%, respectively). Results of adjusted logistic regression model controlling for race, age, education, income, employment, marital status, and cigarette smoking status indicated that higher income was associated with drinking frequency, while never having married correlated with binge drinking, and never having married, ever having smoked, being self-employed, and being unemployed were associated with binge drinking more than two times. Older age (aged 41–48 years) and being married were negatively associated with binge drinking and binge drinking more than once. Using the 2002–2006 NSDUH data, Muhuri and Gfroerer (2009) also found prevalent past-month alcohol use (49%) and binge drinking (≥ 5 drinks per occasion, 17.1%) among women with children aged ≤ 2 years. While these prevalences were lower than estimates among non-pregnant, non-postpartum women (57.5% and 25.8%, respectively), they were considerably higher than prevalences among pregnant women (10.5%, alcohol use; 3.2%, binge drinking). When controlling for maternal age, marital status, education, and family income, results showed that pregnant and postpartum white, Black, and Hispanic women had lower odds of drinking compared with women of the same race who were neither pregnant nor postpartum. White women had the highest prevalence of any alcohol use, followed by Black and Hispanic women. Although the prevalence in Black and Hispanic women did not differ, compared with all of the women whose data were analyzed, a greater proportion of pregnant and parenting women were younger, Hispanic, and married; the majority of neither pregnant nor parenting women were unmarried.
Jagodzinski and Fleming (2007a) surveyed 8,706 predominantly white (81%), married (73.1%), employed (67.5%), multiparious (54.1%), breastfeeding (58.4%) women (aged >18 years) with some college (70%) seen for postpartum care at 35 Wisconsin clinics from July 2002 to April 2005. The prevalence of any past-month alcohol use among postpartum women was 30.1%, with 1.5% reporting ≥ 7 drinks per week. This was lower than that of women’s reported pre-pregnancy drinking (41.5% any use and 7.2% ≥ 7 drinks per week) but higher than prenatal use (5.4% any drinking and 0.02 ≥ 7 drinks per week). Results of an adjusted logistic regression model controlling for age, race, education, marital status, number of children, breastfeeding, postpartum cigarette smoking, and employment status indicated that postpartum risky drinkers (≥ 7 drinks per week and ≥ 4 drinks in one day in the past 30 days; 12%) were less likely than non-risky drinkers to be Black (vs. white), to have breastfed in the past seven days, to be aged > 35 years, and to be outside the labor force. Correlates of risky drinking were risky drinking before pregnancy, scoring as at risk or having a current problem on an alcohol misuse assessment, smoking cigarettes after birth, and being single.
In a continuation of this research, Jagodzinksi and Fleming (2007b) analyzed the survey responses of 381 frequent drinkers (>7 drinks per week) before pregnancy. They found that 37.8% were risky drinkers postpartum. Of the 381 women, 16% reported depressive symptoms. The prevalence rose to 35.9% among low risk alcohol users and to 47.5% among at risk drinkers, but depressive symptoms did not correlate with at risk alcohol use. Controlling for age, race, education, marital status, employment status, number of children, breastfeeding status, and depressive symptoms, correlates of risky drinking were having a risky drinking partner, being unemployed, smoking cigarettes while pregnant, and knowingly drinking while pregnant. Women who breastfed were less likely than women who did not breastfeed to report risky drinking (odds ratio [OR] = 0.3, 95% confidence interval [CI]: 0.2–0.5). Fleming et al. (2008) further analyzed characteristics of 235 women identified as postpartum risky drinkers from the original 8,706 and found that these 235 postpartum risky drinkers were similar to the original 8,706 postpartum participants in that they were predominantly white (81% vs. 81%, respectively) and employed (66% vs. 67%, respectively). The 235 postpartum risky drinkers differed slightly from the 8,706 in that fewer had attended college (63% vs. 70%) and more were married or lived with a partner (82% vs. 73%, respectively). They differed substantially in that fewer breastfed their infants (27.7% vs. 58.4%, respectively) and more smoked cigarettes (53.2% vs. 13%, respectively). Women in the subsample also had a high prevalence of depressive symptoms (38.7%). These were the only studies that assessed depressive symptoms.
McLeod et al. (2002) surveyed 665 women registered for prenatal care in Wellington, New Zealand at 20–24 and 36 weeks pregnant and at 6–10 weeks postpartum about their cigarette smoking behavior, alcohol consumption, and demographic information. McLeod et al. (2002) found that, at 20–24 weeks gestation, only 3.9% of women had consumed alcohol on ≥ 3 days in the past week. At 6–10 weeks postpartum, 16.4% had. Drinking ≥ 3 days in the past week at 6–10 weeks postpartum was positively associated with tertiary education (i.e., college or post high school vocational training). Abstinence at 6–10 weeks postpartum was positively associated with socioeconomic deprivation.
In summary, all identified studies used cross-sectional designs. Problem drinking (i.e., either binge drinking or drinking ≥ 7 drinks per week) ranged from 1.5%–8.4% among postpartum women. Postpartum prevalences were lower than those for women who were neither pregnant nor postpartum (range 7.2%–25.8%) but higher than prevalences for pregnant women (range 0.02%–3.2%). Collectively, postpartum drinkers in the U.S. were characterized by being predominately white and low-income. Correlates of postpartum problem drinking included being unmarried, smoking cigarettes, and being unemployed. Only two studies examined depressive symptoms among postpartum alcohol users.
Illicit Drugs
Two cross-sectional studies examined drug use among postpartum women (Table 2) (Fleming et al. 2008; Muhuri and Gfroerer 2009). The first used a national sample (n=94,483). The second focused on marijuana and cocaine use among postpartum women with drinking problems (n=235) (Fleming et al. 2008).
Table 2.
Studies related to postpartum illicit or nonmedical drug use
| Authors | Year | Sample, N | Race/ Ethnicity |
Data source & Study Design | Pregnancy Status & Prevalence of drug use | Associated Variables |
|---|---|---|---|---|---|---|
| Muhuri &Gfroerer (2009) | 2002–2006 | 94,483 | 63.8% White, 13.5% Black, 15.2% Hispanic, 7.2% Other | National Survey on Drug Use & Health Cross-sectional | Not Pregnant 7.3% Marijuana or Hashish*; 3.7% Marijuana ≥6 days*; 4.0% Psychotherapeutics*; 1.2% Cocaine (& Crack)*; 6.5% Polydrug use* | Whites had the highest prevalence of use followed by Hispanics and Non Hispanic Blacks except for marijuana on >6 days (no difference between whites and Blacks) & cocaine, binge alcohol, & psychotherapeutics (no difference between Blacks and Hispanics) |
| Pregnant 2.8% Marijuana or Hashish*; 1.8% Marijuana >6 days*; 1.1% Psychotherapeutics*; 0.3% Cocaine (& Crack)*; 1.4% Polydrug use* | ||||||
| Postpartum 4.6% Marijuana or Hashish*; 2.7% Marijuana >6 days*; 2.6% Psychotherapeutics*; 0.6% Cocaine (& Crack)*; 3.9% Polydrug use* | ||||||
| Fleming et al. (2008) | 2002–2005 | 235 | 81% White, 7.2% Native American, 6.8% Black, 2.5% Hispanic | At risk postpartum drinkers recruited from 15 Wisconsin counties Cross-sectional | Postpartum 17.9% Marijuana*; 2.5% Cocaine* | N/A |
Psychotherapeutics: nonmedical use of prescription drugs (opioid pain relievers, stimulants, sedatives, or tranquilizers).
Any use in past 30 days
The 2002–2003 NSDUH data showed that 8.5% of new mothers (child aged < 1year) reported past-month use of illicit or nonmedical drugs (marijuana/ hashish, cocaine/crack, inhalants, hallucinogens, heroin, or prescription psychoactive drugs [including opioid analgesics, stimulants, tranquilizers, and sedatives]) (SAMHSA 2005a), which was higher than the prevalence (4.5%) in 1999 (SAMHSA 2001). In 2002–2003, more women not pregnant or postpartum used illicit or nonmedical drugs (10.6%) than did new mothers (SAMHSA 2005a), and the prevalence of use was also higher than the prevalence (7.6%) in 1999 (SAMHSA 2001). In 2002–2003 and 1999, pregnant women had the lowest prevalences (4.3%; 3.7%, respectively) with little change in drug use among pregnant women in these years (SAMHSA 2005a; SAMHSA 2001).
Muhuri and Gfroerer (2009) investigated postpartum drug use (marijuana/hashish, cocaine, and prescription psychoactive drugs) using 2002–2006 NSDUH data. Excluding marijuana, a twofold increase in past-month drug use occurred between pregnant (1.2%) and postpartum (2.5%) women. Among women with a child aged ≤ 2 years, past-month prevalence of use of marijuana/hashish, prescription psychoactive drugs (nonmedical use), and cocaine were 4.6%, 2.6%, and 0.6%, respectively, which were lower than estimates for women who were not pregnant or postpartum (7.3%; 4%; and 1.2%, respectively), but higher than estimates for pregnant women (2.8%; 1.1%; and 0.3%, respectively). In addition, prevalence of marijuana use on ≥ 6 days was higher among new mothers (2.7%) compared with pregnant women (1.8%) as was polysubstance use, including alcohol and cigarettes (3.9%; 1.4%, respectively). After alcohol and cigarettes, marijuana (6.6%) was the substance used most often, followed by prescription psychoactive drugs (3.6%) and cocaine (1.1%).
Controlling for maternal age, marital status, education, and family income, Muhuri and Gfroerer (2009) found that women who were neither pregnant nor postpartum had increased odds for use for all substances (marijuana, prescription psychoactive drugs, and cocaine), and pregnant women had lower odds of use (p<0.001). Prevalence of use of any substance was highest for whites, regardless of pregnancy or parenting status, followed by Blacks and Hispanics. The odds of drug use were lower for white and Hispanic new mothers when compared to neither pregnant nor postpartum women of the same race (excluding marijuana use on ≥ 6 days and nonmedical prescription psychoactive drug use for Hispanic women), showing that white and Hispanic new mothers were less likely to use drugs than women neither pregnant nor postpartum of the same race. Among Black new mothers, odds of any marijuana use, marijuana use on ≥ 6 days, nonmedical prescription psychoactive drug use, and cocaine use did not differ from odds of use among Black women who were neither pregnant nor postpartum, indicating that Black new mothers were not significantly less likely to use drugs than their not pregnant and not postpartum counterparts.
In a subsample of postpartum risky drinkers (n=235), Fleming et al. (2008) found that 17.9% of women used marijuana in the past 30 days, and that 2.5% used cocaine. As discussed above, the prevalence of depressive symptoms (38.7%) in the sample was high. Fleming et al. (2008) did not include correlates of drug use.
In summary, all identified studies employed cross-sectional designs. Only one study directly examined postpartum illicit drug use. Muhuri and Gfroerer (2009) found a higher prevalence of drug and polysubstance use among postpartum women compared with prenatal women but a lower prevalence compared with women who were neither pregnant nor postpartum. Fleming et al. (2008) compared postpartum marijuana and cocaine prevalences with results of a study investigating postpartum alcohol use and found prevalent polysubstance use (17.9% alcohol and marijuana). Muhuri and Gfroerer (2009) examined racial/ethnic variations in use and found the highest prevalence of marijuana use, nonmedical prescription psychoactive drug use, and cocaine use among whites, followed by Blacks, and then Hispanics. Of note, the odds of drug use among Black new mothers did not differ from Black women who were neither pregnant nor postpartum, which highlights a need for research to understand factors influencing their use and continuous drug use behaviors. Muhuri and Gfroerer (2009) did not include use correlates beyond race, such as income. No studies directly investigated postpartum drug use and depression, with only Fleming et al. (2008) reporting the prevalence of depressive symptoms in their sample (n=235).
Does Postpartum Depression (PPD) Contribute to Substance Use?
During its peak period (birth-3months postpartum), PPD may occur in up to 14.5% of new mothers (Gavin et al. 2007). Clinical and epidemiologic studies have shown that substance use and depressive disorders are risks for each other (e.g., depression may increase risk for later substance abuse or vice versa) (Swendsen and Merikangas 2000), and both may reduce women’s ability to care for children and negatively affect maternal and child health (Homish et al. 2004). Few studies have examined the prevalence of PPD among substance-using mothers or whether PPD influences substance use (Ross and Dennis 2009). From the studies described above, we found that Jagodzinski and Fleming (2007b) and Fleming et al. (2008) reported prevalence of depressive symptoms. The six studies that examined substance use and PPD (Table 3) were published between 1995 and 2009 and had sample sizes ≤ 595 (Homish et al. 2004; Barnet et al. 1995; Bryan et al. 1999; Pajulo et al. 2001; Salisbury et al. 2007; Wilton, Moberg, and Fleming 2009). None compared substance use prevalence among postpartum women to prevalences among pregnant or neither pregnant nor postpartum women. Three analyzed survey data from women found in hospital treatment (Homish et al. 2004; Barnet et al. 1995; Salisbury et al. 2007), two assessed rates of PPD among women in substance abuse treatment (Pajulo et al. 2001; Wilton, Moberg, and Fleming 2009), and one used a retrospective medical chart review to examine substance use and depressive symptoms among women who recently gave birth (Bryan et al. 1999).
Table 3.
Studies related to postpartum substance use and depression
| Authors | Year | Sample, N | Race/Ethnicity | Data source | Findings on Depressive Symptoms |
|---|---|---|---|---|---|
| Barnet et al. (1995) | July 1989–March 1990 | 125 eligible; 108 surveyed; 105 urine assays | 93% Black | Inner City teaching hospital adolescent pregnancy program |
At 4 Months Postpartum:
|
| Bryan et al. (1999) | 1993 | 403 | N/A | Medical Charts or women from Olmstead County, MN |
|
| Pajulo et al. (2001) | 1994–1995 | 24 (12 Control) | Finnish | Women in & not in Drug treatment |
|
| Homish et al., (2004) | 1982–1985 | 595 | 51% Black; 49% White | Urban Hospital Prenatal Clinic |
Variables that Increased Odds of Postpartum Substance Use and Depressive Symptoms Comorbidity in Any Trimester:
|
In Addition:
|
|||||
| Salisbury et al. (2007) | Not Provided | 385 Cocaine Users & 668 Non users | 80% Black; 13% White; 7% Other | 4 National Institute of Child Health and Human Development Neonatal Research Network sites |
|
| Wilton et al. (2009) | 2002–2005 | 235 | 81% White, 7.2% Native American, 6.8% Black, 2.5% Hispanic | Women from 15 Wisconsin counties |
6 Month Follow-Up:
|
In a longitudinal cohort study, Barnet et al. (1995) surveyed 108 predominantly Black (93%) new adolescent mothers aged 12–18 years (mean 16.3 + 1.3 years) at two and four months postpartum who were enrolled in an inner-city teaching hospital adolescent pregnancy program from July 1989 to March 1990. Controlling for age, girls at four months postpartum who reported any alcohol use since delivery were more likely than nonusers of alcohol to have high depressive symptom scores on the Center for Epidemiological Studies of Depression-Children’s Scale (46% users vs. 24% nonusers, p = 0.02). Girls who reported any alcohol or illicit drug use since delivery were also more likely than nonusers of alcohol or drugs to report stress (62% vs. 43%, p = 0.04). Girls who reported any alcohol or illicit drug use since delivery were marginally more likely than nonusers to report a need for social support at four months postpartum (62% users vs. 44% nonusers, p = 0.07). Of note, the odds of any alcohol or illicit drug use at four months postpartum were 3.3 times higher for those with high depressive symptom scores compared to those lower scores (p = 0.02); the odds increased to 6.7 times greater among girls with high depressive symptom scores who also smoked cigarettes (p < 0.001).
Bryan et al. (1999) analyzed retrospectively collected data from the medical charts of 403 Minnesota women who gave birth in 1993 and found that, of the 3.7% of the women who displayed depressive symptoms, 20% had a history of substance abuse. This prevalence was much higher than the 4.6% of new mothers without depressive symptoms and a substance abuse history. Prevalence of prenatal drug use was also much higher among those with PPD symptoms (46.7%) when compared to those without (16.5%). In a longitudinal study, Pajulo et al. (2001) used the Edinburgh Postnatal Depression Scale to identify postpartum depression (score >12 or possible PPD and in need of intervention) in a sample of 12 new Finnish mothers being treated for substance abuse from 1994–1995 and compared it to 12 women without a history of substance abuse. Rates of PPD symptoms were higher among women in treatment (25% vs. 8% at 3 months; 42% vs. 8% at six months); however, the small sample size made it impossible to include in-depth analyses.
In a longitudinal study, Homish et al., (2004) examined concurrent alcohol use and depressive symptoms (defined by Center for Epidemiologic Studies-Depression Scale with a cut-point 16) among 595 Black (51%) and white (49%) women of low socioeconomic status recruited at an urban hospital prenatal clinic from 1982 to 1985. In models controlling for race, employment, marital status, social support, cigarette use, depressive symptoms, and binge drinking, the results revealed that postpartum alcohol use was positively associated with depressive symptoms, cigarette use, and binge drinking in any of the three trimesters. Additional correlates included being unmarried in the second trimester and experiencing anxiety in the third. In another longitudinal study, Salisbury et al. (2007) used the Addiction Survey Index (ASI) to assess 385 new mothers who used cocaine prenatally and 668 demographically matched new mothers who did not at one month postpartum. Depression was determined as a serious depression lasting ≥ 2 weeks in the past 30 days and a score of ≥ 3 for psychological problems on the ASI. Depressive symptoms were prevalent among the 385 women who used cocaine (19.7%). Additionally, prenatal cocaine users with depressive symptoms were significantly more likely than those without depressive symptoms to report postpartum cocaine use (26.3% vs. 14.3%).
Wilton et al. (2009) conducted a longitudinal study to examine the effect of a brief alcohol intervention on PPD among 235 postpartum alcohol users, originally recruited as part of the Fleming et al. (2008) study conducted from 2002–2005. A large proportion (38.7%) of postpartum alcohol users indicated a high level of depressive symptoms on the Edinburgh Postnatal Depression Scale (>9 or at risk of depression) at six months postpartum. Wilton et al. (2009) found that, while alcohol use at baseline or six-month follow up was not associated with depressive symptoms, the level of depressive symptoms was significantly reduced among those who received the intervention compared to those who did not (p<0.001).
Taken together, these identified studies focused on predominantly poor or socially marginalized populations (e.g., adolescent mothers) who may have high rates of depression generally. They tended to examine PPD symptoms among women identified as using substances postpartum or with a substance use history, including prenatal use, and found prevalent PPD symptoms among these women (range 19.7%–46%). Women who had high depressive symptom scores were also more likely than those with lower scores to engage in alcohol or illicit drug use (Barnet et al. 1995; Salisbury et al. 2007), and an alcohol intervention reduced depressive scores among postpartum women (Wilton, Moberg, and Fleming 2009). None of the studies, however, provided substance use prevalences for women with PPD.
Discussion
Comparisons of substance use prevalences among postpartum, pregnant, and neither pregnant nor postpartum women consistently showed that pregnant women had lowest prevalences, followed by new mothers. Prevalence of alcohol use among postpartum women with a child aged <1 year ranged from 36.7% to 49%, lower than prevalences among neither pregnant nor postpartum women (52.5%–57.4%) and higher than those among pregnant women (10.4%–11.6%). Similar results were found for women with children aged ≤ 2 years, for binge drinking, and for drinking frequently (Table 1). Illicit drug use prevalences showed a similar pattern (i.e., women with a child aged <1 year range 4.5%–8.5%; women neither pregnant nor postpartum range 7.6%–10.6%, and pregnant women range 3.7%–4.3%), which repeated for women with a child aged ≤ 2 and polysubstance use (Table 2). However, data were lacking on prevalences and correlates of alcohol or drug use disorders among postpartum women. Given prevalent rates of substance use by postpartum women, future research examining the prevalences and correlates of alcohol and drug use disorders is warranted for this population. Identified studies on substance use prevalence used cross-sectional designs, impeding the ability to make temporal inference. Additionally, data are scarce about the prevalence of postpartum women seeking or finding treatment and the characteristics of women in treatment. Such research is needed to inform intervention efforts by identifying gaps in receipt of treatment, the women least likely to seek help, and the women most in need of assistance.
We have found two articles examining a possible relationship between breastfeeding and alcohol use (Jagodzinski and Fleming 2007a and 2007b). Fleming et al. (2008) reported breastfeeding prevalence in a subsample of risky drinkers (n=235), who had a lower prevalence of breastfeeding than the rate for women in the original sample (n=8,706; 27.7% vs. 58.4, respectively). Findings suggest that breastfeeding may be protective against problem drinking, which corresponds to the findings from studies on alcohol use and breastfeeding (Giglia and Binns 2006). However, studies on breastfeeding also found that, when compared to nursing mothers and women who never nursed, women who weaned early (before three months) drank most often and reported the most binge drinking (Giglia and Binns, 2006), suggesting that the relationship between alcohol use and breastfeeding is complex and needs further investigation. If breastfeeding is protective or women at greater risk for early weaning are also at greater risk for problem drinking, it may be beneficial to incorporate substance related counseling into lactation support. None of the studies that examined illicit drug use identified for this review directly explored the influence of breastfeeding on drug use, so it is unclear whether breastfeeding may be protective against drug use. Overall, findings from this review suggest that women with PPD are more likely to use substances than new mothers without PPD (Barnet et al. 1995; Salisbury et al. 2007). Postpartum substance users and women with a history of substance use had higher PPD prevalences (19.7%–46%) compared to women not using or without such a history. Extant studies provide the rationale for research using large, representative samples to characterize better substance use patterns and associated family, contextual, and mental health factors that may influence continued substance use, reduction in use, and treatment seeking for substance use problems among postpartum women and subgroups with PPD. PPD and substance use may influence each other, resulting in adverse consequences. Longitudinal data are needed to understand their interactive effects and temporal associations in order to inform designs of targeted interventions to reduce consequences and improve women’s health status and parenting skills. The prevalent rates of substance use among postpartum women and identified associations between depressive symptoms and substance use suggest that depression assessment and intervention should be part of prenatal and postpartum care among substance-using women. Additionally, white race was positively associated with postpartum alcohol use (Laborde and Mair 2011; Jagodzinski and Fleming 2007a), and white women had higher prevalences of postpartum alcohol and drug use than Hispanic women (Muhuri and Gfroerer 2009). Although Black women did not differ from white women in their odds of drug use, the lack of differences in odds of drug use between Black new mothers and Black women who were neither pregnant nor postpartum suggests a greater likelihood of continuous drug use through pregnancy into the postpartum period among Black women when compared to white and Hispanic women (Muhuri and Gfroerer 2009). Further, studies reviewed here have not considered engagement in prenatal care. Future research could examine the relations between use of prenatal care and substance use prevention strategies, including age and racial/ethnic differences in barriers to receiving prenatal care and substance use status. Low income was also positively associated with postpartum alcohol use (Laborde and Mair 2011; SAMHSA 2008), as was being young (Muhuri and Gfroerer 2009), unemployed (Laborde and Mair 2011; Jagodzinski and Fleming 2007a), and cigarette smoking either before or after pregnancy (Laborde and Mair 2011; Jagodzinski and Fleming 2007a; Jagodzinski and Fleming 2007b). This review also found that correlates of postpartum drug use beyond race have not been systematically investigated.
Extant findings have not elucidated relationships between socioeconomic status and alcohol or drug use among postpartum women, but similarities in alcohol use correlates (e.g., being white, young) with those found among pregnant and neither pregnant nor postpartum women suggest the relations of environmental factors to substance use in this population (Darrow et al. 1992; Leight et al. 2010). Differences in perception about risk or approval of substance use could diminish women’s ability to self-recognize when they have a postpartum substance use problem, as they may assume their use is normal and acceptable. This finding, combined with the higher prevalence of postpartum substance use when compared to rates in pregnancy, represents missed treatment and intervention opportunities. To inform targeted intervention and treatment efforts, there is a need to better characterize risk factors for postpartum substance use and psychiatric characteristics of postpartum substance users by substance type (e.g., alcohol vs. illicit drugs) and patterns of use (e.g., initiation vs. resumption). Such factors, characteristics, and patterns could be used to develop clinically useful screening questions or tools and train core care providers (e.g., neonate nurses, pediatricians; see Fleming et al. 2008) to identify and assist women in need.
Although marijuana was the drug used most often by postpartum women, newer studies on illicit and nonmedical drug use using more recently collected data are needed to account for current drug use trends. In particular, nonmedical use or abuse of prescription opioids are epidemic (CDC 2012), the nation’s fastest growing drug problem (e.g., admissions to emergency department, overdose mortalities), and the second most prevalent drug use disorder after marijuana use disorders (Wu et al., 2011; Wu et al., 2012). Women are also at greater risk than men for opioid abuse and psychiatric comorbidities (e.g., major depression) (Green et al. 2009; Wu et al., 2010), and opioids are often prescribed to help women with obstetric related pain (Madadi, Ross, and Hayden 2009).
The postpartum period is one of lifestyle and biological change. Many women struggle to adapt and cope to this new phase of their lives. It is possible that all women with a history of substance misuse should receive psychological assessments and intervention as needed during prenatal and postpartum care. Their needs must be properly assessed and identified to be effectively addressed. Research on prevalence and correlates of substance use behaviors and PPD thus can provide useful information to aid providers in distinguishing those in need and providing them with appropriate help. Evidence indicates that treatment for postpartum women should include children, be gender-specific, build self-efficacy, and integrate infant and early-childhood parent training (Bowie 2004; Grella 2008; Suchman et al. 2011). However, due to a lack of research data to gauge women’s mental and behavioral health needs and to guide gender- or race-specific intervention programs, treatment for postpartum women is not always available, gender-specific, or comprehensive (ABM 2009). Maternal substance abuse can contribute to child abuse or neglect (VanDeMark et al. 2005; Morton and Konrad 2009). Abused children are further at risk for substance abuse as adults, and cycles of abuse can become generational (Dunn et al. 2002). Women who quit substances in pregnancy have the best of intentions and deserve help in maintaining abstinence, which can improve their, their children’s, and possibly their grand children’s long-term health and psychological outcomes.
Acknowledgements
The authors have received research support from the U.S. National Institute on Drug Abuse of the National Institutes of Health (R33DA027503, R01DA019623, and R01DA019901; PI: Li-Tzy Wu). The sponsoring agency had no further role in the writing of this paper or the decision to submit the paper for publication. The opinions expressed in this paper are solely those of the authors.
Footnotes
Disclosures: None
Works Cited
- Academy of Breastfeeding Medicine Protocol Committee [ABM] ABM clinical protocol #21: Guidelines for breastfeeding and the drug dependant woman. Breastfeed Med. 2009;4:225–228. doi: 10.1089/bfm.2009.9987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association [APA] Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Barnet B, Duggan AK, Wilson MD, Joffe A. Association between postpartum substance use and depressive symptoms, stress, and social support in adolescent mothers. Pediatrics. 1995;96:659–666. [PubMed] [Google Scholar]
- Bowie BH. Interventions to improve interactions between drug abusing mothers and their drug-exposed infants: A review of the research literature. J Addict Nurs. 2004;15:153–161. [Google Scholar]
- Bryan TL, Georgiopoulos AM, Harms RW, Huxsahl JE, Larson DR, Yawn BP. Incidence of postpartum depression in Olmstead County, Minnesota. A population based retrospective study. J Reprod Med. 1999;44:351–358. [PubMed] [Google Scholar]
- Burke L. The impact of maternal depression on familial relationships. Int Rev Psychiatry. 2003;15:243–255. doi: 10.1080/0954026031000136866. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC] CDC grand rounds: prescription drug overdoses - a U.S. epidemic. Morb Mortal Wkly Rep. 2012;61:10–13. [PubMed] [Google Scholar]
- Chapman SL, Wu LT. Substance use among adolescent mothers: A review. Child Youth Serv Rev. 2013 doi: 10.1016/j.childyouth.2013.02.004. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darrow SL, Russell M, Cooper ML, Mudar PJ, Frone MR. Sociodemographic correlates of alcohol consumption among African-American and white women. Women Health. 1992;18:35–51. doi: 10.1300/J013v18n04_03. [DOI] [PubMed] [Google Scholar]
- Dunn MG, Tarter RE, Mezzich AC, Vanyokov M, Kirisci L, Kirillova G. Origins and consequences of child neglect in substance abuse families. Clin Psychol Rev. 2002;22:1063–1090. doi: 10.1016/s0272-7358(02)00132-0. [DOI] [PubMed] [Google Scholar]
- Fang WL, Goldstein AO, Butzen AY, Hartsock A, Hartmann KE, Helton M, Lohr JA. Smoking cessation in pregnancy: A review of postpartum relapse prevention strategies. J Am Board Fam Pract. 2004;17:264–275. doi: 10.3122/jabfm.17.4.264. [DOI] [PubMed] [Google Scholar]
- Fleming MF, Lund MR, Wilton G, Landry M, Scheets D. The Healthy Moms Study: The efficacy of brief alcohol intervention in postpartum women. Alcohol Clin Exp Res. 2008;32:1600–1606. doi: 10.1111/j.1530-0277.2008.00738.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn HA, Chermack ST. Prenatal alcohol use: the role of lifetime problems with alcohol, drugs, depression, and violence. J Stud Alcohol Drugs. 2008;69:500–509. doi: 10.15288/jsad.2008.69.500. [DOI] [PubMed] [Google Scholar]
- Forest S. Preventing postpartum smoking relapse: An opportunity for neonatal nurses. Adv Neonatal Care. 2009;9:148–155. doi: 10.1097/ANC.0b013e3181a68afd. [DOI] [PubMed] [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: A systematic review of prevalence and incidence. Obstet Gynecol. 2005;106:1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- Giglia R. Alcohol and lactation: An updated systematic review. Nutr Diet. 2010;67:237–243. [Google Scholar]
- Giglia R, Binns C. Alcohol and lactation: A systematic review. Nutr Diet. 2006;63:103–116. [Google Scholar]
- Green TC, Grimes Serrano JM, Licari A, Budman SH, Butler SF. Women who abuse prescription opioids: Findings from the Addiction Severity Index-Multimedia Version Connect Prescription Opioid Database. Drug Alcohol Depend. 2009;103:65–73. doi: 10.1016/j.drugalcdep.2009.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE. From generic to gender responsive treatment: Changes in social policies, treatment services, and outcomes of women in substance abuse treatment. J Psychoactive Drugs. 2008;(Suppl5):327–343. doi: 10.1080/02791072.2008.10400661. [DOI] [PubMed] [Google Scholar]
- Homish GG, Cornelius JR, Richardson GA, Day NL. Antenatal risk factors associated with postpartum comorbid alcohol use and depressive symptomatology. Alcohol Clin Exp Res. 2004;28:1242–1248. doi: 10.1097/01.alc.0000134217.43967.97. [DOI] [PubMed] [Google Scholar]
- Jagodzinski T, Fleming MF. Postpartum and alcohol-related factors associated with the relapse of risky drinking. J Stud Alcohol Drugs. 2007a;68:879–885. doi: 10.15288/jsad.2007.68.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagodzinski T, Fleming MF. Correlates of postpartum alcohol use. Wis Med J. 2007b;106:319–325. [PubMed] [Google Scholar]
- Laborde ND, Mair C. Alcohol use patterns among postpartum women. Matern Child Health J. 2011 doi: 10.1007/s10995-011-0925-3. epub ahead of print: http://www.springerlink.com/content/43613w8382748275/ [DOI] [PMC free article] [PubMed]
- Lazareck S, Robinson JA, Crum RM, Mojtabai R, Sareen J, Bolton JM. A longitudinal investigation of the role of self-medication in the development of comorbid mood and drug use disorders: findings from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) J Clin Psychiatry. 2012;73:e588–e593. doi: 10.4088/JCP.11m07345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leight KL, Fitelson EM, Weston CA, Wisner KL. Childbirth and Mental Disorders. Int Rev Psychiatry. 2010;22:453–471. doi: 10.3109/09540261.2010.514600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madadi P, Ross CJD, Hayden MR. Pharmacogenetics of neonatal opioid toxicity following maternal use of codeine during breastfeeding: A case-control study. Clin Pharmacol Ther. 2009;85:31–35. doi: 10.1038/clpt.2008.157. [DOI] [PubMed] [Google Scholar]
- Marcus SM. Depression during pregnancy: Rates, risks and consequences. The Canadian Journal of Clinical Pharmacology. 2009;16:e15–e22. [PubMed] [Google Scholar]
- McLeod D, Pullon S, Cookson T, Comford E. Factors influencing alcohol consumption during pregnancy and after giving birth. The New Zealand Medical Journal. 2002;115:1–7. [PubMed] [Google Scholar]
- Morton J, Konrad SC. Introducing a caring/relational framework for building relationships with addicted mothers. J Obstet Gynecol Neonatal Nurs. 2009;38:206–213. doi: 10.1111/j.1552-6909.2009.01006.x. [DOI] [PubMed] [Google Scholar]
- Muhuri PK, Gfroerer JC. Substance use among women: Associations with pregnancy, parenting, and race/ethnicity. Matern Child Health J. 2009;13:376–385. doi: 10.1007/s10995-008-0375-8. [DOI] [PubMed] [Google Scholar]
- Pajulo M, Pyykkonen N, Kalland M, Helenius H, Punamaki R-L, Suchman N. Substance-abusing mothers in residential treatment with their babies: Importance of pre-and postnatal maternal reflective functioning. Infant Ment Health J. 2012;33:70–81. doi: 10.1002/imhj.20342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pajulo M, Savonlahti E, Sourander A, Ahlqvist S, Helenius H, Piha J. An early report on the mother-baby interactive capacity of substance-abusing mothers. J Subst Abuse Treat. 2001;20:143–151. doi: 10.1016/s0740-5472(00)00161-6. [DOI] [PubMed] [Google Scholar]
- Ross LE, Dennis C-L. The prevalence of postpartum depression among women with substance use, and abuse history or chronic illness: A systematic review. J Womens Health. 2009;18:475–486. doi: 10.1089/jwh.2008.0953. [DOI] [PubMed] [Google Scholar]
- Rutherford H, Williams SK, Moy S, Mayes LC, Johns JM. Disruption of maternal parenting circuitry by addictive process: Rewiring of reward and stress systems. Front Psychiatry. 2011;2:1–17. doi: 10.3389/fpsyt.2011.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salisbury AL, Lester BM, Seifer R, LaGasse L, Bauer CR, Shankaran S, Bada H, Wright LL, Liu J, Poole K. Prenatal cocaine use and maternal depression: Effects on infant neurobehavior. Neurotoxicol Teratol. 2007;29:331–340. doi: 10.1016/j.ntt.2006.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration [SAMHSA] The NHSDA Report, Pregnancy and Illicit Drug Use. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2001. [Google Scholar]
- Substance Abuse and Mental Health Services Administration [SAMHSA] Results from the 2002 National Survey on Drug Use and Health: Summary of National Finding. (DHHS Publication No. SMA 03–3836, NHSDA Series H-22) Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2003. [Google Scholar]
- Substance Abuse and Mental Health Services Administration [SAMHSA] The NHSDA Report, Substance Use during Pregnancy: 2002 and 2003 Update. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2005a. [Google Scholar]
- Substance Abuse and Mental Health Services Administration [SAMHSA] The NSDUH Report. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Study; 2005b. [Google Scholar]
- Substance Abuse and Mental Health Services Administration [SAMHSA] Alcohol use among pregnant and recent mothers: 2002 to 2007. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2008. [Google Scholar]
- Suchman NE, Decoste C, McMahon TJ, Rounsaville B, Mayes L. The mothers and toddlers program, an attachment-based parenting intervention for substance-using women: Results at 6-week follow-up in a randomized clinical pilot. Infant Ment Health. 2011;32:427–449. doi: 10.1002/imhj.20303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swendsen JD, Merikangas KR. The comorbidity of depression and substance use disorders. Clin Psychol Rev. 2000;20:173–189. doi: 10.1016/s0272-7358(99)00026-4. [DOI] [PubMed] [Google Scholar]
- VanDeMark NR, Russell LA, O’Keefe M, Finkelstein N, Noether CD, Gampel JC. Children of mothers with histories of substance abuse, mental illness, and trauma. J Community Psychol. 2005;33:445–459. [Google Scholar]
- Wilton G, Moberg DP, Fleming MF. The effect of brief alcohol intervention on postpartum depression. Am J Matern Child Nurs. 2009;34:297–302. doi: 10.1097/01.NMC.0000360422.06486.c4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Kouzis AC, Leaf PJ. Influence of comorbid alcohol and psychiatric disorders on utilization of mental health services in the National Comorbidity Survey. Am J Psychiatry. 1999;156:1230–1236. doi: 10.1176/ajp.156.8.1230. [DOI] [PubMed] [Google Scholar]
- Wu LT, Woody GE, Yang C, Blazer DG. Subtypes of nonmedical opioid users: results from the national epidemiologic survey on alcohol and related conditions. Drug Alcohol Depend. 2010;112:69–80. doi: 10.1016/j.drugalcdep.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Woody GE, Yang C, Pan JJ, Blazer DG. Racial/ethnic variations in substance-related disorders among adolescents in the United States. Arch Gen Psychiatry. 2011;68:1176–1185. doi: 10.1001/archgenpsychiatry.2011.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Swartz MS, Wu Z, Mannelli P, Yang C, Blazer DG. Alcohol and drug use disorders among adults in emergency department settings in the United States. Ann Emerg Med. 2012;60:172–180. e5. doi: 10.1016/j.annemergmed.2012.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]