Abstract
Objective
This study tested whether the quality of the patient-rated working alliance, measured early in treatment, predicted subsequent symptom reduction in chronically depressed patients. Secondarily, the study assessed whether the relationship between early alliance and response to treatment differed between patients receiving Cognitive Behavioral Analysis System of Psychotherapy (CBASP) versus Brief Supportive Psychotherapy (BSP).
Method
395 adults (57% female; Mage = 46; 91% Caucasian) who met criteria for chronic depression and did not fully remit during a 12-week algorithm-based, open-label pharmacotherapy trial were randomized to receive either 16–20 sessions of CBASP or BSP in addition to continued, algorithm-based antidepressant medication. Of these, 224 patients completed the Working Alliance Inventory-Short Form at weeks 2 or 4 of treatment. Blind raters assessed depressive symptoms at two-week intervals across treatment using the Hamilton Rating Scale for Depression. Linear mixed models tested the association between early alliance and subsequent symptom ratings while accounting for early symptom change.
Results
A more positive early working alliance was associated with lower subsequent symptom ratings in both the CBASP and BSP, F(1, 1236) =62.48, p<.001. In addition, the interaction between alliance and psychotherapy type was significant, such that alliance quality was more strongly associated with symptom ratings among those in the CBASP treatment group, F(1,1234) = 8.31, p =.004.
Conclusions
The present results support the role of the therapeutic alliance as a predictor of outcome across dissimilar treatments for chronic depression. Contrary to expectations, the therapeutic alliance was more strongly related to outcome in CBASP, the more directive of the two therapies.
Keywords: alliance, depression, psychotherapy outcome, REVAMP
Considerable evidence associates the therapeutic alliance with psychotherapy outcome for a wide range of diagnoses and populations (Castonguay, Constantino, & Holtforth, 2006). A recent meta-analysis of 190 independent alliance-outcome association studies (Horvath, Del Re, Flückinger, & Symonds, 2011) reported a modest but significant relationship between alliance quality and outcome (weighted r = .28, p < .0001, CI.95 = .25 to .30). Nonetheless, methodological problems in the extant literature on the alliance-outcome association limit the conclusions that can be drawn.
A key issue is the direction of the alliance-outcome link. A significant association between alliance and treatment outcome may arise because the experience of a good therapeutic alliance generates symptom change, because symptom change positively influences one’s perception of the alliance, or because the two variables mutually influence one another (Barber, Connolly, Crits-Christoph, Gladis, & Siqueland, 2000). As Feeley and colleagues (1999) noted, existing studies on the alliance-outcome relationship have generally been observational rather than experimental. Observational studies allow inference of causal implications only if certain conditions are met, a crucial one being temporal precedence between the process (e.g., alliance) and outcome (e.g. symptom severity) variables (DeRubeis & Feeley, 1990; Feeley et al., 1999). To support the hypothesis that a good therapeutic alliance mediates therapy outcome, the alliance must be shown to predict outcome at a subsequent time point, while accounting for change on the outcome variable prior to alliance measurement (Kraemer, Wilson, Fairburn, & Agras, 2002).
Few studies meet these criteria (Barber, 2009). Reports on the relationship between the alliance and outcome have been limited by: 1) Correlating the alliance assessed at time point A with subsequent outcome at post-treatment without accounting for the possibility that some of the predicted change had already occurred prior to time point A; and 2) Correlating improvement in the outcome variable from pre- to post-treatment with an average of alliance scores across the course of treatment (Barber, Khalsa, & Sharpless, 2010; Feeley et al., 1999; Klein et al., 2003; Kraemer et al., 2002).
Among the relatively small number of studies that have investigated the temporal nature of the association between alliance and outcome in patients with depression, results are inconsistent. We are aware of three studies that have examined whether alliance predicts subsequent outcome without controlling for change in symptoms prior to the alliance assessment; none of these demonstrated a significant alliance-outcome link. DeRubeis and Feeley (1990) reported that alliance at treatment week two did not predict subsequent residual change in depression severity in a small sample of 25 patients diagnosed with major depressive disorder (MDD) who received cognitive therapy (CT). Interestingly, this study found the converse, that prior change in depressive symptoms predicted quality of the alliance measured during treatment weeks 7–9 and 10–12. In another small study of 25 patients with MDD receiving CT, Feeley, DeRubeis and Gelfand (1999) again found that week two alliance did not predict subsequent symptom change; this report did not replicate the earlier converse finding that symptom change predicted later alliance (DeRubeis & Feeley, 1990). A study of 60 patients with MDD treated with CT examined the association between repeated measures of the alliance and session-to-session symptom improvement across the first five sessions of treatment (Strunk, Brotman, & DeRubeis, 2010). The alliance did not predict inter-session reductions in symptoms, but prior symptom change did predict subsequent alliance strength (Strunk et al., 2010). These investigators did not examine outcome beyond five weeks.
Four studies conducted with depressed patients examined whether alliance predicts subsequent outcome, while also controlling for change in outcome prior to measuring the alliance. This reflects the most stringent test of the temporal associations between alliance and symptom change. In a study of 54 elderly patients with MDD who received either brief dynamic therapy, behavior therapy, or CT, Gaston et al. (1991) reported that the relationship between alliance and outcome across all three treatments was not significant. Three other studies found that alliance quality predicted subsequent change in symptoms when accounting for symptom change prior to alliance assessment. In a study involving 367 chronically depressed patients treated with either cognitive behavioral analysis system of psychotherapy (CBASP) or CBASP plus medication, the alliance significantly predicted subsequent change in depressive symptoms while controlling for prior symptom change and other patient characteristics with the potential to influence the alliance (Klein et al., 2003); neither early level of symptoms nor early change in symptoms predicted the subsequent level or course of the alliance. In a study of 45 patients with MDD treated with an alliance-enhancing therapy (Crits-Christoph et al., 2006), after controlling for early change in symptoms, early alliance predicted change in depression scores from baseline to end of treatment (Crits-Christoph, Gibbons, Hamilton, Ring-Kurtz, & Gallop, 2011). These investigators also measured alliance later in treatment and found that an average of alliance assessments conducted at sessions 3–9 had an even stronger relationship with outcome than the early alliance (Crits-Christoph et al., 2011), though this association did not control for previous symptom change. Finally, Webb and colleagues (2011) examined the alliance in 105 depressed patients treated with CT in two separate randomized controlled trials. An observer-rated version of early alliance was used and was found to significantly predict outcome.
The inconsistent findings of studies that have reported on the relation between alliance and subsequent symptom change (with or without control for early symptom change) may be related to a) the model of psychotherapy used, and b) failure to examine specific dimensions of the alliance. Although the data are mixed (Hatcher & Gillaspy, 2006), theory suggests that the alliance is comprised of different components, specifically tasks, goals, and the therapist-patient emotional bond (Bordin, 1979). Different psychotherapy models may evoke different alliance types, expressed through different scoring patterns on alliance dimensions (Hatcher & Gillaspy, 2006). Webb et al. (2011) reported that symptom change in patients who received CT was related to an alliance factor assessing agreement on goals and tasks, but not to the therapist-patient bond factor.
All but one of the previously cited studies involved only a single treatment, precluding comparison of alliance effects across treatments. In the one study that involved more than one psychotherapy model, the sample size was too small to adequately examine potential differences (Gaston et al., 1991). Thus, no studies examining the alliance-outcome relationship in depressed patients have reported on between-treatment differences in dimensions of the alliance.
The present study examined the relationship between early alliance and subsequent change in depressive symptoms in two distinct psychotherapies, namely CBASP or Brief Supportive Psychotherapy (BSP), while accounting for prior symptom change in a single patient population, consisting of chronically depressed patients. Chronically depressed patients may present unique difficulties in developing and maintaining productive therapeutic alliances. McCullough (2000) has argued that the chronically depressed patient is distinguished by preoperational thinking (Piaget, 1926, 1967) involving features such as egocentric views of the self and others, impaired empathy, and lack of responsiveness to corrective feedback. Although interpersonal difficulties such as social skills deficits and interpersonal dependency are characteristic of depressed patients in general (Joiner & Timmons, 2009), the chronically depressed patient, according to McCullough, is unique in his failure to understand the relationship between thinking, behavior and environmental consequences. In turn, this results in a lack of effective agency, and a wariness of interpersonal engagement (Constantino et al., 2008). The interpersonal style of the chronically depressed patient, according to McCullough, manifests as either hostile detachment or excessive submissiveness. In a test of McCullough’s theory, based upon data gathered in several samples using the Impact Message Inventory (Kiesler & Schmidt, 1993), Constantino et al. (2008) found that chronically depressed patients, compared with an acutely depressed sample, had significantly greater hostile and lower friendly-dominant impacts on their therapists. Compared to a normative comparison group, chronically depressed patient impacts were significantly more hostile and hostile-submissive, and significantly less friendly dominant.
Our primary hypothesis was that a stronger early therapeutic alliance would predict a significantly greater treatment response both for patients receiving CBASP and for patients receiving BSP. For CBASP, this hypothesis stemmed from previous findings reported by Klein et al. (2003). For BSP, the expectation of an alliance-outcome association is consistent with the model’s putative focus on “common factors,” including the therapeutic alliance (Markowitz, Manber, & Rosen, 2008). As Markowitz et al. (2008) noted, while all psychotherapies use common factors, “they…do so to differing degrees.” (p. 71) Given BSP’s emphasis on the therapeutic alliance and its de-emphasis of the procedural interventions characteristic of CBASP and other structured psychotherapy models, we further hypothesized that the magnitude of the alliance-outcome correlation would be greater in BSP than CBASP. Additional aims were to explore whether CBASP and BSP differed in alliance development and, if so, whether the two models were associated with differences in the dimensions of early alliance. Based on the findings of Strunk et al. (2010) and DeRubeis and Feeley (1990), we also aimed to evaluate the complementary hypothesis that early symptom reduction would predict therapeutic alliance rating across treatment.
Method
Design
The current study reports data from phase 2 of the REVAMP trial. The REVAMP trial design has been described in detail elsewhere (Kocsis et al., 2009). Briefly, it comprised two phases. In the nonrandomized phase 1, all participants received algorithm-driven antidepressant medication. Those who did not achieve remission [defined as at least a 60% reduction in Hamilton Rating Scale for Depression score (HAM-D) (Hamilton, 1960), a 24-item total HAM-D score of 7 or less, and not meeting DSM-IV-TR criteria for MDD over 2 consecutive visits during weeks 6 through 12] continued to phase 2, in which they were randomly assigned to receive CBASP + antidepressant medication (ADM), BSP + ADM, or ADM only. Phase 2 findings revealed no differences between the three conditions in remission, partial response or change in HAM-D scores. Among all participants, remission was achieved in 15%, and partial response in 22.5% (Kocsis et al., 2009). Secondary mixed model analyses revealed significantly lower mean HAM-D scores in the CBASP versus BSP comparison (p=.04), although the two groups did not differ in rate of change.
Participants
Participants were outpatients, age 18–75, recruited at eight separate sites. IRB committees at each site approved the study. All patients met DSM-IV-TR criteria (American Psychiatric Association, 2000) for current MDD as determined by the Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P) (First, Spitzer, Gibbon, & Williams, 1996). All patients had experienced the current MDD episode for a minimum of 4 weeks and all had experienced depressive symptoms for at least two years without remission, thus meeting criteria for chronic MDD, recurrent MDD with incomplete inter-episode recovery, or “double depression” (current MDD episode with antecedent dysthymic disorder). In addition, participants scored at least 20 on the 24-item HAM-D (Hamilton, 1960) at baseline and spoke English.
Exclusion criteria were current diagnosis of any psychotic disorder, dementia, or antisocial, schizotypal or severe borderline personality disorder; current primary diagnosis of posttraumatic stress disorder, anorexia, bulimia, or obsessive-compulsive disorder; history of bipolar disorder; previous CBASP treatment; previous nonresponse to four or more steps of pharmacotherapy algorithm; unwillingness to terminate other psychiatric treatment during the study; pregnancy; serious unstable medical illness; and current alcohol or substance dependence (except nicotine dependence) that required detoxification. Participants with alcohol and substance abuse were not excluded if they agreed to participate in Alcoholics Anonymous or chemical dependence counseling and to implement a sobriety plan while participating in the study.
Pharmacotherapy
All patients received concomitant algorithm-based pharmacotherapy. The pharmacotherapy algorithm (Klein et al., 2009; Kocsis et al., 2009) was based on other empirically derived regimens including the STAR*D study (Fava et al., 2003). The study medications included sertraline, escitalopram, bupropion XL, venlafaxine XR, mirtazapine, and lithium. Prior treatment history determined choice of initial medication; treatment naïve patients began on sertraline. Minimum and maximum doses, speed of dosage escalation, and trial lengths after each change were specified by the protocol.
Participants were evaluated every two weeks. Participants who were intolerant to a medication during the first four weeks of phase 1 could move to the next option in the sequence. Pharmacotherapists followed the Fawcett et al. (1987) manual from the National Institute of Mental Health Treatment of Depression Collaborative Research Program (NIMH TDCRP) (Elkin et al., 1989) to ensure minimal psychotherapeutic intervention.
Cognitive Behavioral Analysis System of Psychotherapy (CBASP)
CBASP is a manualized, time-limited, cognitive-behavioral intervention designed specifically for patients suffering from chronic depression (McCullough, 2000). A primary assumption of CBASP is that chronically depressed patients fail to understand the relationships among their own thoughts, behaviors, and environmental consequences. Situational analysis, a core CBASP procedure, is a social problem-solving algorithm designed to modify maladaptive thoughts and behaviors and enhance awareness of the consequences of one’s own thoughts and behaviors (Arnow, 2005; McCullough, 2000). Patients are asked to track distressing interpersonal situations between sessions using the Coping Style Questionnaire (McCullough, 2000). During situational analysis, the patient and therapist examine the associations among thoughts, behaviors, and actual and desired outcomes in specific interpersonal encounters. CBASP focuses on examining discrepancies between actual and desired outcomes, and on how thinking and behavior need to change in order to increase the likelihood of achieving the desired outcome. If the desired outcome is unrealistic, the therapist works with the patient to formulate a more achievable goal. CBASP therapists formulate transference hypotheses at the beginning of treatment and implement explicit procedures for addressing interactions within the therapeutic relationship that are inconsistent with the patient’s relationship expectations (McCullough, 2000) with the goal of teaching the patient the situational specificity of others’ reactions to their behavior.
CBASP emphasizes the importance of “disciplined personal involvement” (McCullough, 2000) on the part of the psychotherapist in promoting a sound therapeutic alliance. This requires the therapist’s willingness to productively make use of both positive and negative reactions to the patient. Positive reactions were often contrasted with the responses of significant others in the patient’s history. For instance, a therapist’s willingness to accept a patient’s angry response might be contrasted with the habitual response of significant others in the patient’s history (e.g., “What are the implications both for our relationship and for your relationship with others of my willingness to accept and take seriously your anger toward me?”). When the therapist has negative responses toward a patient, procedures included verbalizing the response, identifying the specific behavioral precipitant and its impact on the therapist, and using the interaction to improve the patient’s understanding of his interpersonal impact on the therapist and on others.
CBASP sessions occurred twice weekly during weeks 1–4 and once weekly during weeks 5–12. During weeks 5–8, up to four additional sessions could be added if a participant needed additional assistance in mastering situational analysis. Thus, total CBASP treatment ranged from 16–20 sessions.
Brief Supportive Psychotherapy (BSP)
BSP resembled client-centered (Rogers, 1951) therapy with added psychoeducation regarding chronic depression. It was designed to control for the nonspecific elements of psychotherapeutic treatment, and to provide a contrast with the more structured CBASP (Markowitz, Manber, et al., 2008). The model used in the REVAMP study was similar to that used in studies of depressed HIV-positive (Markowitz et al., 1998) dysthymic (Markowitz, Kocsis, Bleiberg, Christos, & Sacks, 2005) and chronically depressed alcohol-abuse patients (Markowitz, Kocsis, Christos, Bleiberg, & Carlin, 2008). Therapists conducting BSP used an unpublished treatment manual that drew on the principles of supportive psychotherapy (Novalis, Rojcewicz, & Peele, 1993; Pinsker, 1997) and emphasized the following “common” psychotherapeutic factors (Frank, 1963; Rogers, 1951): reflective listening, empathic therapeutic responses, evoking affect, normalizing patient feelings such as anger and sadness, imparting therapeutic hope, encouraging patients to find solutions rather than directly suggesting them, and highlighting success experiences (Markowitz, Manber, et al., 2008). Patients determined the session focus and pace, making sessions much less structured than in CBASP. Therapists elicited patients’ emotional reactions and highlighted patients’ strengths. Specific interpersonal, cognitive, behavioral, and psychodynamic interventions were prohibited (Markowitz, Manber, et al., 2008). As in CBASP, 16–20 sessions of BSP were scheduled over 12 weeks.
Forming an understanding and supportive therapeutic alliance is a primary goal of BSP. Therapists sought to achieve this by letting patients determine subject matter, listening carefully, mirroring patient affects in their own emotional responses during a session (e.g., looking sad when a patient described a sad situation or feeling), echoing their feelings (“It really hurts, doesn’t it?”), using therapeutic silence to allow feelings to build in the room to demonstrate that therapists could tolerate “noxious” patient feelings; and providing support and encouragement. In short, the alliance was fostered by helping the patient to feel that the therapist understood and empathized with him or her (Frank, 1963).
Psychotherapists
All psychotherapists were licensed and had at least two years of clinical experience after completing a Ph.D. in psychology or a psychiatric residency, or at least 5 years of experience after completing a Masters in Social Work degree. BSP therapists were comparable to CBASP therapists in type of professional degree and amount of clinical experience.
Supervision and Protocol Adherence
The developer of CBASP, James P. McCullough, Jr., PhD, trained and certified CBASP therapists and site supervisors. Similarly, John C. Markowitz, MD, trained and certified BSP therapists and site supervisors. All psychotherapy sessions were videotaped. Supervision was conducted by site supervisors who met weekly with therapists. XXX and YYY provided monthly phone supervision to the full group of site CBASP and BSP supervisors, respectively.
For both psychotherapy conditions, one or two session tapes for each therapist-patient dyad were randomly selected and rated for protocol adherence. Tapes were taken from early (session 2–6) and/or late (session 8 or later) sessions and rated in their entirety using the Collaborative Study Psychotherapy Rating Scale from the NIMH TDCRP (Elkin et al., 1989) modified to also rule out situational analysis (for BSP) and the CBASP Therapist Adherence Rating Scale (for CBASP).
Randomization
Randomization in phase 2 was stratified by site, phase 1 response status (non-response versus partial response), and medication history (failure to respond to fewer than 3 adequate medication trials including phase 1 trials, versus failure to respond to 3 or more adequate trials). The randomization allocation ratio was 2 : 2 : 1 (CBASP + ADM : BSP + ADM : ADM only). Only the CBASP + ADM and BSP + ADM treatment groups are included in the current study.
Measures and Procedure
Depressive Symptoms
Raters assessed participant depressive symptoms every two weeks using the 24-item HAM-D (Hamilton, 1960). The 24-item version was selected because it contains cognitive items characteristic of chronically depressed individuals. Raters were blind to treatment condition. Rater and therapist offices were physically separated at each site and raters began each assessment by requesting that participants not refer to psychotherapy or psychotherapists during the interview.
Global Assessment of Functioning
Trained raters assessed level of impairment due to psychiatric symptoms at baseline using the Global Assessment of Functioning Scale (GAF) (Endicott, Spitzer, Fleiss, & Cohen, 1976). The GAF is a single numerical rating designed to capture an individual’s psychological, social, and occupational functioning. Scores range from 1–100 divided into 10-point intervals, each with a set of distinguishing characteristics. The GAF has demonstrated good interrater reliability (intraclass correlation coefficient > .86) and correlated moderately with other general symptom severity measures in a sample seeking outpatient mental health treatment (Hilsenroth et al., 2000).
Therapeutic alliance
Because the current study focused on the therapeutic alliance in psychotherapy, alliance data were not collected in the medication only group. For the CBASP and BSP conditions, the patient-rated short form of the Working Alliance Inventory (WAI) (Horvath & Greenberg, 1989; Tracey & Kokotovic, 1989) was administered at 3 time points across phase 2: early (week 2 or week 4), middle (week 6) and late (week 12). Due to an administrative error, the WAI was not given at week 2 to 41 of 224 (18%) participants in this study. In these instances, the week 4 score served as the early alliance score. Patients providing alliance data at week 2 did not statistically differ from those providing data at week 4 on any baseline or outcome measure (e.g., GAF, early symptom change, overall symptom reduction).
The WAI short form is a 12-item self-report measure derived from the full 36-item WAI (Tracey & Kokotovic, 1989). It has been widely used to assess therapeutic alliance. The full WAI correlates moderately with other alliance measures (Horvath & Greenberg, 1989), and scores on both the full form (Horvath, 1994) and short form (Klein et al., 2003) have predicted psychotherapy outcome. We used the patient form because it predicts psychotherapy outcome more strongly than psychotherapist-rated assessment of the alliance (Barber et al., 1999; Constantino, Castonguay, & Schut, 2002; Horvath & Symonds, 1991). Because participants had two treating clinicians, a pharmacotherapist and a psychotherapist, the instructions clarified that the measure should be completed specifically regarding their psychotherapists.
Items are rated on a 7-point Likert scale with higher scores reflecting a stronger therapeutic alliance. Both the original and the shortened versions of the WAI have a purported two-level structure, with a general alliance factor that can be divided into three subscale scores: (1) Goals, designed to measure therapist and patient agreement on the goals for therapy; (2) Tasks, designed to measure therapist and patient agreement on how to achieve treatment goals; and (3) Bond, designed to measure the quality of the therapist-patient relationship (Tracey & Kokotovic, 1989).
Statistical Analyses
Descriptive data were calculated for the total sample and by treatment group. Between subjects descriptive variables were compared using independent samples t-tests for continuous data and chi-square analyses for categorical data. Within subjects descriptive variables were compared using paired-samples t-tests. Internal consistency of the WAI was examined by calculating Cronbach’s alpha for the early, middle and late WAI total scores.
A linear mixed model was used to test the main study hypothesis that stronger early alliance would predict greater treatment response. Fixed factors in the model included early WAI total score, treatment group, the interaction of WAI total score with treatment group, patient age, patient gender, baseline functioning (GAF), and early change in HAM-D (i.e., week 2 score minus baseline HAM-D score). For the 46 patients whose early alliance was assessed at week 4, the early change in symptoms variable was calculated using week 4 minus baseline HAM-D score. Early change in HAM-D was included based on the assumption that early response to treatment could influence both early treatment alliance and treatment outcome. Baseline GAF was included on the assumption that initial severity may correlate with response to treatment. GAF was chosen rather than baseline HAM-D because of potential multicollinearity with the change in early symptoms variable and because it incorporates a greater range of prognostically relevant information (e.g., comorbid symptomatology, functional impairment). Continuous predictor variables were mean centered and dichotomous variables were coded as 0 or 1. The dependent variable was HAM-D total score measured at Weeks 2, 4, 6, 8 and 12 of treatment (or Weeks 4,6,8 and 12 for those participants completing the WAI at Week 4). HAM-D observations were specified as a repeated measures variable based on time.
A similar linear mixed model was used to test whether early HAM-D symptom reduction predicted subsequent alliance. This model also tested whether CBASP + ADM and BSP + ADM treatment groups differed in development of the alliance. Centered values for early symptom change, treatment group, the interaction of early symptom change with treatment group, GAF and patient age and dichotomous values for patient gender were entered as fixed factors. The dependent variable was WAI total score at Weeks 2 (or 4), 6 and 12. Mixed model analyses were conducted using the MIXED procedure in SPSS. An alpha of .05 was used for defining statistical significance in all analyses.
Effect size is reported as Cohen’s d. The Cohen’s d statistic can be calculated from any statistical analysis that yields a t statistic via the equation d = t(2/n)1/2 (Dunlap, Cortina, Vaslow, & Burke, 1996). Additionally, for comparison with studies reporting effects as r values, the t statistic can be utilized to generate r via the equation r = [t2/(t2 + df)]1/2.
Results
Descriptive Characteristics
Sample demographics appear in Table 1. There were no statistically significant differences between the two treatment groups on baseline variables. Two hundred participants were randomized to CBASP + ADM and 195 were randomized to BSP + ADM. Of these, data on the variables of interest were available for 111 participants in CBASP + ADM (56% of total CBASP +ADM sample) and 113 participants in BSP + ADM (58% of total BSP +ADM sample). Patients in the current study sample did not differ from participants in the larger study on any parameter (see Table 1).
Table 1.
Characteristics of Study Participants
| CBASP + ADM | BSP + ADM | |
|---|---|---|
| N | 111 | 113 |
| Age, M(SD) | 45.6 (11.3) | 47.4 (11.2) |
| Gender, % Female | 54.1 | 53.1 |
| Ethnicity, % | ||
| African American | 3.6 | 3.5 |
| Caucasian | 92.8 | 89.4 |
| Other | 3.6 | 7.1 |
| Hispanic ethnicity,1 % | ||
| Yes | 9.0 | 5.3 |
| No | 88.3 | 93.8 |
| Education in years, M (SD) | 16 (3) | 15 (3) |
| Marital Status, % | ||
| Divorced, widowed or separated | 24.3 | 29.2 |
| Married or cohabitating | 41.4 | 47.8 |
| Never married | 34.2 | 23.0 |
| GAF, M (SD) | 54 (9) | 54 (7) |
| Current Comorbid Anxiety, % | 36.9 | 38.9 |
| Alcohol Abuse or Dependence, % | 3.6 | 1.8 |
| Phase II Baseline HAM-D, M (SD) | 18.7 (7.8) | 19.5 (8.5) |
Percentages do not total 100 due to missing data
Mean HAM-D scores across treatment appear in Figure 1. Consistent with findings of the main outcome study (Kocsis et al., 2009), HAM-D scores decreased in both groups during the 12-week trial (BSP + ADM: mean change from baseline = −6.7, SD = 7.3, paired t = 9.3, df = 103, p < .001; CBASP + ADM: mean change from baseline = −7.3, SD = 7.0, paired t = 10.7, df = 106, p < .001). Mean WAI scores, measured during the early (week 2 or 4), middle (week 6) and late phases (week 12) of the study appear in Figure 2. WAI scores increased significantly during the course of the study in both the BSP + ADM and CBASP + ADM groups (BSP + ADM: M = +5.4, SD = 9.0, t= 5.9, df = 98, p < .001; CBASP + ADM: M = +3.5, SD = 10.2, t = 3.4, df = 93, p <.001). Internal consistency of the WAI was high at each time point (Cronbach’s alpha = .90, .90 and .93 for Weeks 2, 6 and 12, respectively).
Figure 1.
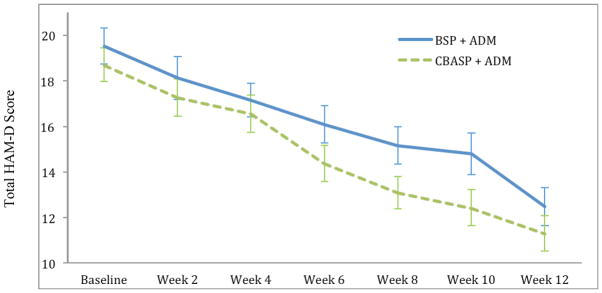
Mean HAM-D scores across the 12-week study
Note: Error bars represent Standard Error of the Mean. Group means did not statistically differ at baseline (p = .44), Week 2 (p = .49), Week 4 (p = .58), Week 6 (p = .13) or Week 12 (p = .30). Those in CBASP + ADM showed lower mean HAM-D scores than those in BSP + ADM at Week 10, p = .05; M(SD)BSP = 14.80(9.44); M(SD)CBASP = 12.41(8.12).There was a trend for those in CBASP + ADM to show lower mean HAM-D scores at Week 8 (p = .06). BSP = Brief Supportive Therapy. CBASP = Cognitive Behavioral Analysis System of Psychotherapy. ADM = Antidepressant Medication. HAM-D = Hamilton Rating Scale for Depression.
Figure 2.
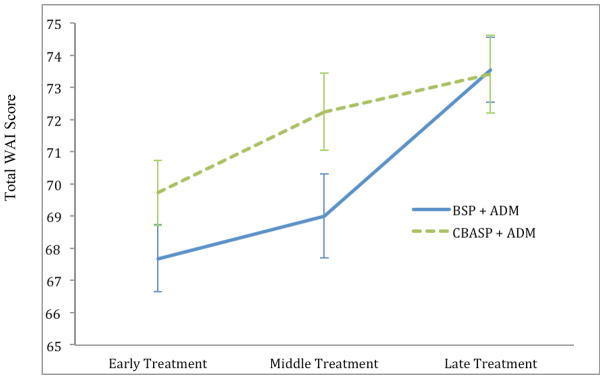
Scores Across Treatment On the Working Alliance Inventory
Note: Error bars represent Standard Error of the Mean. Early treatment n = 113 in BSP + ADM and 111 in CBASP + ADM; Middle treatment n = 73 in BSP + ADM and 63 in CBASP + ADM; Late treatment n = 99 in BSP + ADM and 94 in CBASP + ADM. BSP = Brief Supportive Therapy. CBASP = Cognitive Behavioral Analysis System of Psychotherapy. ADM = Antidepressant Medication. WAI = Working Alliance Inventory.
Prediction of Symptom Outcome From Early Therapeutic Working Alliance
The mixed model analysis testing the primary hypothesis showed, as predicted, that higher early working alliance scores were significantly associated with lower subsequent HAM-D scores across treatment, F(1, 1236) = 62.48, p < .001. Parameter estimates appear in Table 2. The interaction of treatment group x alliance was also significant; however the direction was contrary to prediction, indicating that the association between alliance and subsequent symptom reduction was stronger among those in CBASP + ADM when compared to those in BSP + ADM, F(1,1234) = 8.31, p = .004. Greater reduction in HAM-D scores in the initial weeks of treatment significantly predicted lower subsequent HAM-D scores, F(1,1233) = 40.57, p < .001, as did higher baseline level of functioning as measured by the GAF, F(1,1218) = 84.85, p < .001, and CBASP treatment group, F(1,1237) = 4.19, p = .04 although treatment groups did not significantly differ at the study endpoint. Age and gender were not predictive of HAM-D symptom reduction.
Table 2.
Mixed Model Parameter Estimates for the Prediction of HAM-D Symptom Reduction Across Treatment (n = 224)
| Estimate | SE | t | Significance | 95% CI Lower |
95% CI Upper |
d | |
|---|---|---|---|---|---|---|---|
| Intercept1 | 14.72 | .39 | 38.05 | p <.001 | 13.96 | 15.48 | 3.60 |
| Gender | −.30 | .46 | .65 | p =.52 | −1.20 | .60 | .06 |
| Age | −.04 | .02 | 1.65 | p =.10 | .01 | −.07 | .16 |
| Baseline GAF | −.27 | .03 | 9.21 | p < .001 | −.32 | −.21 | .87 |
| Early alliance | −.23 | .03 | 7.48 | p <.001 | −.29 | −.17 | .71 |
| Early symptom change | .21 | .03 | 6.37 | p <.001 | −.14 | .28 | .60 |
| Treatment group | .93 | .46 | 2.05 | p =.04 | −1.79 | −.01 | .19 |
| Alliance X Treatment group | .12 | .04 | 2.88 | p = .004 | .04 | .21 | .27 |
Note:
Intercept reflects estimated mean HAM-D score across all time points.
Gender reference group = male. Treatment group reference group = CBASP + ADM. GAF = Global Assessment of Functioning.
In order to further assess the finding that the association between alliance and HAM-D symptom reduction was stronger in CBASP + ADM than in BSP + ADM, additional mixed models analyses were run separately for each treatment group. The models were similar to the main analysis except that treatment group and the interaction of early alliance rating with treatment group were removed as fixed factors. As in the combined model, significant predictors for both treatment groups were baseline GAF, early alliance and early HAM-D symptom change. In addition, there was a trend for younger age to predict greater HAM-D symptom reduction in BSP + ADM, F(1, 609) = 3.72, p = .05. Parameter estimates appear in Tables 3a and 3b. Among those in CBASP + ADM, the estimated effect of early working alliance on HAM-D symptom reduction across treatment was −.22 compared to −.11 in BSP + ADM. Thus, over the course of treatment, those in CBASP + ADM showed an average HAM-D point decrease of 1.32 for each additional point increase on the WAI whereas those in BSP + ADM showed an average HAM-D decrease of .66 for each additional point increase on the WAI. Cohen’s d for early working alliance was 1.00 in CBASP + ADM compared to .48 in BSP + ADM.
Table 3a.
Mixed Model Parameter Estimates for the Prediction of HAM-D Symptom Reduction Across Treatment Among Patients Receiving CBASP + ADM (n = 111)
| Estimate | SE | t | Significance | 95% CI Lower |
95% CI Upper |
d | |
|---|---|---|---|---|---|---|---|
| Intercept1 | 14.43 | .45 | 34.16 | p < .001 | 14.93 | 16.71 | 4.59 |
| Female Gender | −.06 | .62 | .11 | p = .91 | −1.29 | 1.14 | .01 |
| Age | .01 | .03 | .45 | p = .66 | −.04 | .07 | .06 |
| Baseline GAF | −.25 | .04 | −6.80 | p <.001 | −.32 | −.17 | .91 |
| Early alliance | −.22 | .03 | −7.48 | P < .001 | −.28 | −.16 | 1.00 |
| Early symptom change | .14 | .05 | 3.01 | p = .003 | .05 | .22 | .40 |
Note:
Intercept reflects estimated mean HAM-D score across all time points.
Gender reference group = male. GAF = Global Assessment of Functioning.
Table 3b.
Mixed Model Parameter Estimates for the Prediction of HAM-D Symptom Reduction Across Treatment Among Patients Receiving BSP + ADM (n = 113)
| Estimate | SE | t | Significance | 95% CI Lower |
95% CI Upper |
d | |
|---|---|---|---|---|---|---|---|
| Intercept1 | 15.81 | .45 | 34.85 | p < .001 | 14.93 | 16.71 | 4.63 |
| Female Gender | −.54 | .68 | −.79 | p = .43 | −1.87 | .79 | .11 |
| Age | .06 | .03 | 1.93 | p = .05 | .00 | .12 | .26 |
| Baseline GAF | −.30 | .05 | −6.39 | p < .001 | −.40 | −.21 | .85 |
| Early alliance | −.11 | .03 | −3.58 | p < .001 | −.17 | −.05 | .48 |
| Early symptom change | .29 | .05 | 5.73 | p < .001 | .19 | .38 | .76 |
Note:
Intercept reflects estimated mean HAM-D score across all time points.
Gender reference group = male. GAF = Global Assessment of Functioning.
Prediction of Therapeutic Working Alliance From Early Symptom Reduction
In the mixed model analysis evaluating whether treatment group or early symptom reduction predicted average alliance over treatment, early change in HAM-D did not predict mean therapeutic alliance ratings across treatment as a main effect, F(545) = 1.48, p = .23, or interact with treatment group to predict alliance, F(1,545) = .02, p=.90. Treatment group was predictive of therapeutic alliance such that mean alliance ratings across treatment were higher among those in CBASP + ADM when compared to those in BSP + ADM, F(1,543) = 4.10, p = .04. Parameter estimates indicated that, on average, those in CBASP + ADM showed mean alliance ratings that that were an average of 1.86 points higher on the WAI than those in BSP + ADM. Older age was predictive of stronger alliance, F(1,544) = 10.94, p<.001 and there was a trend for women to show higher alliance ratings than men, F(1,543) = 3.09, p = .08. Baseline GAF did not predict mean alliance, F(1,543) = .85, p=.36.
Treatment Group Differences in Therapeutic Working Alliance Ratings
In order to explore treatment group differences in the alliance-outcome relationship, bivariate Pearson correlations between early alliance and HAM-D total scores at all time points were computed for each treatment group. Correlations appear in Table 4. Among patients who received CBASP + ADM, early alliance accounted for 4.4% to 12.3% of the total variance in depressive symptoms between Weeks 4 and 12. Among patients receiving BSP + ADM, early alliance was not significantly correlated with symptom ratings except at Week 6 where it explained 5.3% of the variance in depressive symptom on the HAM-D.
Table 4.
Bivariate Correlations Between Alliance and HAM-D Total Scores
| HAM-D Total Score
|
|||||||
|---|---|---|---|---|---|---|---|
| Baseline | Week 2 | Week 4 | Week 6 | Week 8 | Week 10 | Week 12 | |
| WAI total in CBASP + ADM | −.23* | −.10 | −.35** | −.32** | −.23* | −.35** | −.21* |
| WAI total in BSP + ADM | −.15 | −.16 | −.11 | −.23* | −.14 | −.10 | −.13 |
Note: ns range from 111-63 in CBASP + ADM because of missing data. ns range from 113-73 in BSP + ADM because of missing data. WAI = Working Alliance Inventory. HAM-D = Hamilton Rating Scale for Depression.
p< .05,
p < .01
An additional exploratory analysis was conducted to identify whether particular aspects of the alliance differed between the groups. A one-way ANOVA was used to compare mean early alliance subscale scores on the WAI (Tracey & Kokotovic, 1989) between those in the CBASP + ADM and BSP + ADM subgroups. There were no significant differences in the bond subscale between the two treatment groups, F(1,220) = .01, p = .94. However, compared to those in BSP + ADM, those in CBASP + ADM showed higher mean ratings on tasks, F(1,220) = 6.22, p<.05, M(SD)BSP = 21.65(4.54), M(SD)CBASP = 23.05(3.80), and goals subscales of the WAI, F(1,216) = 4.31, p<.05, M(SD)BSP = 22.54(4.04), M(SD)CBASP = 23.62(3.59).
Discussion
We examined the association between early psychotherapeutic alliance and subsequent symptom change across treatment in a large sample of chronically depressed patients receiving two different psychotherapy models, CBASP or BSP, combined with ADM. We also tested an alternative explanation for the relationship between the alliance and outcome, namely that early symptom change predicts subsequent alliance. Additionally, we tested whether patients in these two treatments differed in alliance development and in dimensions of the alliance early in treatment.
Consistent with the primary hypothesis, in both the CBASP + ADM and BSP + ADM conditions, early alliance significantly predicted subsequent depressive symptom ratings. Furthermore, we observed these relationships after accounting for the variance in outcome associated with baseline functioning and symptom change occurring prior to the alliance assessment. Our findings on the alliance-outcome association in CBASP replicate those of Klein et al. (2003), who found that alliance predicted subsequent depressive symptoms, controlling for change prior to alliance assessment among chronically depressed patients receiving CBASP + ADM as well among patients receiving only CBASP. We know of no findings testing the relationship between alliance and outcome in patients receiving BSP, alone or with antidepressant(s), but our findings appear consistent with the conceptualization of BSP as a “common factors” treatment (Markowitz, Manber, et al., 2008) emphasizing features that are shared across different models of psychotherapy including the therapeutic alliance.
In the combined mixed model involving the full study sample, early alliance, baseline GAF, treatment arm, early change in depressive symptoms and the interaction of treatment arm with early alliance all significantly predicted outcome. In the models that evaluated these variables separately for patients randomized to BSP + ADM and CBASP + ADM, early symptom change, early alliance and GAF continued to predict in both conditions.
While we had hypothesized that the alliance would predict outcome in both BSP and CBASP, the role of the therapeutic alliance presumably functions differently in these two models. In contrasting the alliance in CBT-oriented therapies with other models, Castonguay and colleagues (2010) noted that CBT models rely on specific techniques that produce change “on their own” (p. 154), whereas other psychotherapy models may conceptualize the alliance as “a change mechanism itself” (p. 154). That the alliance predicted outcome in both of these models provides evidence of its critical role across different approaches to psychotherapy.
We hypothesized that the magnitude of the alliance-outcome association would be greater in the BSP than the CBASP group. This hypothesis was not supported. In fact, while we did find a significant alliance X treatment interaction, the association between the alliance and HAM-D ratings was significantly higher among patients receiving CBASP compared to BSP. We also found evidence that participants in the CBASP condition rated alliance as stronger across treatment than those in BSP.
Because BSP is conceptualized as a “common factors” treatment (Markowitz, Manber, et al., 2008) emphasizing features that are shared across different models of psychotherapy including the therapeutic alliance, we were surprised by both of these findings. In examining WAI subscale scores of early alliance ratings, we found no differences between BSP and CBASP groups on the bond subscale. However, CBASP patients rated the task and goal subscale items more highly than those in the BSP condition. One explanation for these findings is that compared with those in the nondirective BSP, the structural features of CBASP (e.g., situational analysis, a rationale regarding its putative benefits, between-session homework tasks) enhanced the patients’ sense that the treatment procedures would be helpful and that their goals for treatment were aligned with those of their therapists. In general, the task and goal dimensions of the therapeutic alliance may be amplified in a structured treatment emphasizing specific procedures, compared with a less structured one. Our findings are consistent with those of (Webb et al., 2011) who reported that the relationship between the WAI (observer-rated) and depression symptom reduction in CT was significantly related to a factor comprising patient-therapist agreement on goals and tasks, but not to a factor assessing affective bond between patient and therapist.
The possibility that clear within-session procedures may promote a stronger therapeutic alliance when compared with the nondirective therapies was discussed almost two decades ago (Raue & Goldfried, 1994) and is consistent with two subsequent studies, which found higher alliance levels in CBT than psychodynamic-interpersonal therapy (Raue, Castonguay, & Goldfried, 1993; Raue, Goldfried, & Barkham, 1997). Bedi and colleagues (2005) found that from the patient perspective, techniques addressing symptoms were more important in facilitating the therapeutic alliance than actions specifically aimed at alliance development. More frequent (e.g., session by session) alliance measures would help to determine whether the pattern of differences in the alliance that we observed across the two treatments would replicate.
Interestingly, and consistent with others’ findings (Barber et al., 2001), alliance scores significantly increased in linear fashion over the 12-week treatment in both groups. We found no evidence of a V-shaped pattern, reflecting a strong early alliance, followed by rupture and repair, which has been found in some studies to be associated with superior outcome (Stiles et al., 2004; Strauss et al., 2006). However, we only assessed the alliance at three time points and we cannot rule out the possibility that more frequent assessment might have revealed such a pattern. Although alliances improved over the course of treatment, symptom change prior to assessment of the early alliance did not predict subsequent alliance ratings, suggesting that alliance ratings were not attributable to early symptom change. Even so, patients’ experience of the therapeutic alliance may be strengthened by improvement in depression across later stages of treatment, by increased familiarity and contact with the therapist, or both. Both the total scores and the change observed over the course of treatment are similar to those reported by Klein et al. (2003) in a previous investigation of the alliance-outcome relationship in chronically depressed patients using the WAI short form.
Little attention has been paid to the relative size of alliance effects in predicting outcome across studies. We found Cohen’s d’s of 1.00 for CBASP +ADM and .48 for BSP + ADM. Effect sizes can also be presented as an r statistic. Crits-Christoph and colleagues (2011) recently demonstrated that effects of alliance on treatment outcome are consistently larger when aggregated across multiple observations. These authors found r values of .32, .38, and .41 when predicting outcome in psychotherapy for depression from alliance scores aggregated across sessions 3–6, 4–7, and 5–8 respectively. While Crits-Cristoph et al. (2011) assessed alliance across multiple treatment modalities, Gaston, Marmar, Gallagher, and Thompson (1991) isolated independent effects of alliance on outcome in behavior therapy, cognitive therapy, and brief psychodynamic therapy. These authors reported rs between early treatment alliance and outcome of .56, .48, and .42 across the three modalities respectively. Translating to r-values, we found effects of alliance on outcome of .58 and .32 in CBASP and BSP. Thus, our findings are consistent with previously published work.
Given that alliance scores increased as HAM-D scores decreased, we examined whether early symptom change predicted alliance ratings over the course of treatment and did not find a relationship. This finding is consistent with those of Klein et al. (2003), Barber et al. (2000), and Feeley, DeRubeis and Gelfand (1999), but not with two other studies (DeRubeis & Feeley, 1990; Strunk et al., 2010). Differences between our findings and those of Strunk et al. (2010) may reflect considerable differences in analytic strategies. We examined the relationship between early change and later alliance, whereas Strunk et al. (2010) focused on only the first five therapist-patient encounters. Among other differences, our sample consisted entirely of chronically depressed patients and all of our participants received concomitant pharmacotherapy. That early alliance predicted subsequent symptom ratings yet early symptom change did not predict later alliance, suggests that the observed increases in alliance across the study are not merely a consequence of patients’ decreased depression. The patient’s perception of their relationship with their therapist does not appear to be attributable to improved mood.
Our study had several limitations that may limit generalizability. First, all patients received psychotherapy in the context of a randomized clinical trial with several unique characteristics. They were initially recruited for an open pharmacotherapy trial from which only partial or non-responders to medication were randomized to BSP + ADM or CBASP + ADM. Thus, patients may have been somewhat more discouraged compared with those participating in trials that do not select for non- or partial response. In addition, many of these patients may not have been initially seeking psychotherapy, or conversely, were seeking psychotherapy and had to wait to receive it. Second, both BSP and CBASP were limited to 12 weeks. Third, all patients received concomitant pharmacotherapy; the extent to which these findings apply to settings where psychotherapy is provided alone is unclear. Klein et al. (2003) found that, among chronically depressed patients receiving CBASP alone or CBASP combined with pharmacotherapy, alliances were stronger in the combined condition, but the relationship between the alliance and outcome was similar in both conditions (Klein et al., 2003). Additionally, the extent of cooperation, collegiality, supervision and accountability among psychopharmacologists and psychotherapists under clinical trial conditions may differ from community settings. Fourth, some study patients were omitted due to missing data. The current sample comprises approximately 57% of the total number of patients randomized to the two psychotherapy arms of the study (Kocsis et al., 2009). Although we observed no differences between patients whom we included versus those who lacked alliance data, we cannot rule out differences beyond those that were formally assessed. Finally, since there were no significant differences in the primary efficacy measures between the three treatment groups (Kocsis et al., 2009), it could be argued that the significant reductions in depression observed in all three conditions were attributable to the effects of medication. However, we assume that between-group and within-group change are independent. That is, even when mean levels of between-group change are similar, the predictors of change and their magnitude of effects may differ in each group. Conversely, it is possible that levels of change may be significantly different between groups, and yet within-group predictors of change may be similar. Moreover, the working alliance was not assessed in patients receiving medication only, and thus we can neither rule out nor support the possibility that it was a significant predictor of the changes observed in that group.
The above limitations notwithstanding, our study had numerous strengths. These include the randomized design; adequate sample size for testing the study hypotheses; ability to compare the therapeutic alliance-outcome relationship in two psychotherapies with different assumptions regarding the role of the alliance; careful assessment of patients; use of blinded raters; and use of experienced therapists.
To conclude, we found that alliance quality significantly predicted subsequent change in depressive symptoms among patients receiving CBASP and BSP (combined with ADM). The strength of the relationship between the alliance and outcome was significantly greater in CBASP, a more structured psychotherapy compared to BSP. Nonetheless, that early therapeutic alliance significantly predicted subsequent symptom ratings in two dissimilar psychotherapy models after accounting for early improvement in symptoms underscores its consistent and important role in the process of change.
Contributor Information
Bruce A. Arnow, Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine
Dana Steidtmann, Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine.
Christine Blasey, Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine
Rachel Manber, Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine
Michael J. Constantino, Department of Psychology, University of Massachusetts Amherst
Daniel N. Klein, Department of Psychology, State University of New York at Stony Brook
John C. Markowitz, Columbia University/New York State Psychiatric Institute
Barbara O. Rothbaum, Department of Psychiatry, Emory University School of Medicine
Michael E. Thase, Department of Psychiatry, University of Pennsylvania School of Medicine
Aaron J. Fisher, Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine
James H. Kocsis, Department of Psychiatry, Weill Medical College of Cornell University
References
- American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder (revision) American Journal of Psychiatry. 2000;157(4 suppl):1–45. [PubMed] [Google Scholar]
- Arnow BA. Cognitive behavioral analysis system of psychotherapy for chronic depression. Cognitive and Behavioral Practice. 2005;12:6–16. [Google Scholar]
- Barber JP. Toward a working through of some core conflicts in psychotherapy research. Psychotherapy Research. 2009;19(1):1–12. doi: 10.1080/10503300802609680. [DOI] [PubMed] [Google Scholar]
- Barber JP, Connolly MB, Crits-Christoph P, Gladis L, Siqueland L. Alliance predicts patients’ outcome beyond in-treatment change in symptoms. Journal of Consulting and Clinical Psychology. 2000;68(6):1027–1032. doi: 10.1037//0022-006x.68.6.1027. [DOI] [PubMed] [Google Scholar]
- Barber JP, Khalsa SR, Sharpless BA. The validity of the alliance as a predictor of psychotherapy outcome. In: Muran JC, Barber JP, editors. The therapeutic alliance: An evidence-based guide to practice. New York: The Guilford Press; 2010. pp. 29–43. [Google Scholar]
- Barber JP, Luborsky L, Crits-Christoph P, Thase ME, Weiss R, Frank A, et al. Therapeutic alliance as a predictor of outcome in treatment of cocaine dependence. Psychotherapy Research. 1999;9:54–73. [Google Scholar]
- Barber JP, Luborsky L, Gallop R, Crits-Christoph P, Frank A, Weiss RD, Siqueland L. Therapeutic alliance as a predictor of outcome and retention in the national institute on drug abuse collaborative cocaine treatment study. Journal of Consulting and Clinical Psychology. 2001;69(1):119–124. doi: 10.1037//0022-006x.69.1.119. [DOI] [PubMed] [Google Scholar]
- Bedi RP, Davis MD, Williams M. Critical incidents in the formation of the therapeutic alliance from the client’s perspective. Psychotherapy: Theory, Research, Practice, Training. 2005;42(3):311–323. [Google Scholar]
- Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research & Practice. 1979;16(3):252–260. doi: 10.1037/h0085885. [DOI] [Google Scholar]
- Castonguay LG, Constantino MJ, Holtforth MG. The working alliance: Where are we and where should we go? Psychotherapy: Theory, Research, Practice, Training. 2006;43(3):271–279. doi: 10.1037/0033-3204.43.3.271. [DOI] [PubMed] [Google Scholar]
- Castonguay LG, Constantino MJ, McAleavey AA, Goldfried MR. The therapeutic alliance in cognitive-behavioral therapy. In: Muran JC, Barber JP, editors. The therapeutic alliance: An evidence-based guide to practice. New York: The Guilford Press; 2010. [Google Scholar]
- Constantino MJ, Castonguay LG, Schut AJ. The working alliance: A flagship for the “scientist-practitioner” model in psychotherapy. In: Tryon GS, editor. Counseling based on process research: Applying what we know. Boston: Allyn & Bacon; 2002. pp. 81–131. [Google Scholar]
- Constantino MJ, Marnell ME, Haile AJ, Kanther-Sista SN, Wolman K, Zappert L, Arnow B. Integrative cognitive therapy for depression: A randomized pilot comparison. Psychotherapy Theory, Research, Practice, Training. 2008;45(2):122–134. doi: 10.1037/0033-3204.45.2.122. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Connolly Gibbons MB, Crits-Christoph K, Narducci J, Schamberger M, Gallop R. Can therapists be trained to improve their alliances? A preliminary study of alliance-fostering psychotherapy. Psychotherapy Research. 2006;16(3):268–281. [Google Scholar]
- Crits-Christoph P, Gibbons MB, Hamilton J, Ring-Kurtz S, Gallop R. The dependability of alliance assessments: The alliance-outcome correlation is larger than you might think. Journal of Consulting and Clinical Psychology. 2011;79(3):267–278. doi: 10.1037/a0023668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeRubeis RJ, Feeley M. Determinants of change in cognitive therapy for depression. Cognitive Therapy and Research. 1990;14(5):469–482. [Google Scholar]
- Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;1(2):170–177. [Google Scholar]
- Elkin I, Shea MT, Watkins JT, Imber SD, Sotsky SM, Collins JF, Parloff MB. National institute of mental health treatment of depression collaborative research program. General effectiveness of treatments. Archives of General Psychiatry. 1989;46(11):971–982. doi: 10.1001/archpsyc.1989.01810110013002. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Archives of General Psychiatry. 1976;33(6):766–771. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- Fava M, Rush AJ, Trivedi MH, Nierenberg AA, Thase ME, Sackeim HA, Kupfer DJ. Background and rationale for the sequenced treatment alternatives to relieve depression (star*d) study. Psychiatric Clinics of North America. 2003;26(2):457, 494, x. doi: 10.1016/s0193-953x(02)00107-7. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Epstein P, Fiester SJ, Elkin I, Autry JH. Clinical management--imipramine/placebo administration manual. Nimh treatment of depression collaborative research program. Psychopharmacology Bulletin. 1987;23(2):309–324. [PubMed] [Google Scholar]
- Feeley M, DeRubeis RJ, Gelfand LA. The temporal relation of adherence and alliance to symptom change in cognitive therapy for depression. Journal of Consulting and Clinical Psychology. 1999;67(4):578–582. doi: 10.1037//0022-006x.67.4.578. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RLO, Gibbon M, Williams JBW. The structured clinical interview for dsm-iv axis i disorders. New York: Biometrices Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- Frank JD. Persuasion and healing. Oxford: Schocken; 1963. [Google Scholar]
- Gaston L, Marmar CR, Gallagher D, Thompson LW. Alliance prediction of outcome beyond in-treatment symptomatic change as psychotherapy processes. Psychotherapy Research. 1991;1:104–113. [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry. 1960;23:56–61. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher RL, Gillaspy JA. Development and validation of a revised short version of the working alliance inventory. Psychotherapy Research. 2006;16(1):12–25. [Google Scholar]
- Hilsenroth MJ, Ackerman SJ, Blagys MD, Baumann BD, Baity MR, Smith SR, Holdwick DJ., Jr Reliability and validity of dsm-iv axis v. American Journal of Psychiatry. 2000;157(11):1858–1863. doi: 10.1176/appi.ajp.157.11.1858. [DOI] [PubMed] [Google Scholar]
- Horvath AO. Research on the alliance. In: Horvath AO, Greenberg LS, editors. The working alliance: Theory, research, and practice. New York: Wiley; 1994. pp. 259–286. [Google Scholar]
- Horvath AO, Del Re AC, Flückinger C, Symonds D. Alliance in individual psychotherapy. In: Norcross JC, editor. Psychotherapy relationships that work: Evidence-based responsiveness. 2. New York: Oxford University Press; 2011. pp. 25–69. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. Development and validation of the working alliance inventory. Journal of Counseling Psychology. 1989;36:223–233. [Google Scholar]
- Horvath AO, Symonds BD. Relation between working alliance and outcome in psychotherapy. Journal of Counseling Psychology. 1991;38:139–149. [Google Scholar]
- Joiner TE, Timmons KA. Depression in its interpersonal context. In: Gotlib IH, Hammen CL, editors. Handbook of depression. 2. New York, NY: The Guilford Press; 2009. [Google Scholar]
- Kiesler DJ, Schmidt JA. The impact message inventory: Form iia octant scale version. Redwood City, CA: Mind Garden; 1993. [Google Scholar]
- Klein DN, Arnow BA, Barkin JL, Dowling F, Kocsis JH, Leon AC, Wisniewski SR. Early adversity in chronic depression: Clinical correlates and response to pharmacotherapy. Depression and Anxiety. 2009;26(8):701–710. doi: 10.1002/da.20577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Schwartz JE, Santiago NJ, Vivian D, Vocisano C, Castonguay LG, Keller MB. Therapeutic alliance in depression treatment: Controlling for prior change and patient characteristics. Journal of Consulting and Clinical Psychology. 2003;71(6):997–1006. doi: 10.1037/0022-006X.71.6.997. [DOI] [PubMed] [Google Scholar]
- Kocsis JH, Gelenberg AJ, Rothbaum BO, Klein DN, Trivedi MH, Manber R, Thase ME. Cognitive behavioral analysis system of psychotherapy and brief supportive psychotherapy for augmentation of antidepressant nonresponse in chronic depression: The revamp trial. Archives of General Psychiatry. 2009;66(11):1178–1188. doi: 10.1001/archgenpsychiatry.2009.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59(10):877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Kocsis JH, Bleiberg KL, Christos PJ, Sacks MH. A comparative trial of psychotherapy and pharmacotherapy for “pure” dysthymic patients. Journal of Affective Disorders. 2005;89:167–175. doi: 10.1016/j.jad.2005.10.001. [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Kocsis JH, Christos P, Bleiberg K, Carlin A. Pilot study of interpersonal psychotherapy versus supportive psychotherapy for dysthymic patients with secondary alcohol abuse of dependence. The Journal of Nervous and Mental Disease. 2008;196(6):468–474. doi: 10.1097/NMD.0b013e31817738f1. [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Kocsis JH, Fishman B, Spielman LA, Jacobsberg LB, Frances AJ, Perry SW. Treatment of hiv-positive patients with depressive symptoms. Archives of General Psychiatry. 1998;55:452–457. doi: 10.1001/archpsyc.55.5.452. [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Manber R, Rosen P. Therapists’ responses to training in brief supportive psychotherapy. American Journal of Psychotherapy. 2008;62(1):67–81. doi: 10.1176/appi.psychotherapy.2008.62.1.67. [DOI] [PubMed] [Google Scholar]
- McCullough JP. Treatment for chronic depression: Cognitive behavioral analysis system of psychotherapy. New York: Guilford Press; 2000. [DOI] [PubMed] [Google Scholar]
- Novalis PN, Rojcewicz SJ, Peele R. Clinical manual of supportive psychotherapy. Washington, DC: American Psychiatric Press; 1993. [Google Scholar]
- Piaget J. The language and thought of the child. New York, NY: Harcourt, Brace; 1926. [Google Scholar]
- Piaget J. In: Six psychological studies. Elkind d., editor. New York, NY: Random House; 1967. [Google Scholar]
- Pinsker H. A primer of supportive psychotherapy. Hillsdale, NJ: The Analytic Press; 1997. [Google Scholar]
- Raue PJ, Castonguay LG, Goldfried MR. The working alliance: A comparison of two therapies. Psychotherapy Research. 1993;3(3):197–207. [Google Scholar]
- Raue PJ, Goldfried MR. The therapeutic alliance in cognitive-behavior therapy. In: Horvath AO, Greenberg LS, editors. The working alliance: Theory, research, and practice. New York: John Wiley & Sons, Inc; 1994. pp. 131–150. [Google Scholar]
- Raue PJ, Goldfried MR, Barkham M. The therapeutic alliance in psychodynamic-interpersonal and cognitive-behavioral therapy. Journal of Consulting and Clinical Psychology. 1997;65(4):582–587. doi: 10.1037//0022-006x.65.4.582. [DOI] [PubMed] [Google Scholar]
- Rogers CR. Client-centered therapy. Boston, MA: Houghton Mifflin; 1951. [Google Scholar]
- Stiles WB, Glick MJ, Osatuke K, Hardy GE, Shapiro DA, Agnew-Davies R, et al. Patterns of alliance development and the rupture-repair hypothesis: Are productive relationships u-shaped or v-shaped? Journal of Counseling Psychology. 2004;51:81–92. [Google Scholar]
- Strauss JL, Hayes AM, Johnson SL, Newman CR, Brown GK, Barber JP, et al. Early alliance, alliance ruptures, and symptom change in a non-randomized trial of cognitive therapy for avoidant and obsessive-compulsive personality disorders. Journal of Consulting and Clinical Psychology. 2006;74:337–345. doi: 10.1037/0022-006X.74.2.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strunk DR, Brotman MA, DeRubeis RJ. The process of change in cognitive therapy for depression: Predictors of early inter-session symptom gains. Behavior Research and Therapy. 2010;48(7):599–606. doi: 10.1016/j.brat.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracey TJ, Kokotovic A. Factor structure of the working alliance inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1989;1:207–210. [Google Scholar]
- Webb CA, DeRubeis RJ, Amsterdam JD, Shelton RC, Hollon SD, Dimidjian S. Two aspects of the therapeutic alliance: Differential relations with depressive symptom change. Journal of Consulting and Clinical Psychology. 2011;79(3):279–283. doi: 10.1037/a0023252. [DOI] [PMC free article] [PubMed] [Google Scholar]


