Abstract
Drug treatment services of varying types have been scaled up in China over the past decade. Yet, barriers to treatment remain among the population of drug users in China. In this paper, we use a person-centered approach to examine external barriers to drug treatment among a sample of Chinese drug users. Specifically, we used a latent class analysis to determine a typology of external barriers to treatment among a sample of 262 drug users. The results of the analyses suggest three-classes of drug users with respect to their perceptions of external barriers to treatment – Major Barriers, Low Barriers, and Systems-level Barriers – indicating that drug users are a heterogeneous population on this matter. Age and types of drugs used were predictors of class membership. In this regard, different tactics must be utilized in order to successfully reach this wide ranging group of individuals.
1. Introduction
Given the size of China's population, its rapid social and economic transformation, and its proximity to key locales of drug cultivation within the region, there has been increasing concern with the escalation of drug problems in China. Official statistics indicate that there has been significant growth in the number of officially registered drug users – users documented by the government – in China over the past two decades; the growth of this part of the population has climbed from 220,000 in 1991 to over 1.2 million by 2008 (Huang et al., 2011). Yet, as in many countries, these records remain an underestimate of the hidden population of drug users. Despite the difficulty of estimating the size of the Chinese drug using population, experts agree that drug use has increased considerably in China since the introduction of social and economic reforms during the late 1980′s (Huang et al., 2011).
With the growing number of drug users in China, the Chinese system has scaled up drug treatment considerably over the past decade. Many of the options available to those who are drug dependent include medical treatment modalities common in Western nations, including opiate substitution therapies such as methadone and buprenorphine, opiate antagonists such as naltrexone, and non-opiate agents such as clonidine and lofexidine (Tang and Hao, 2007). In addition, there are options from traditional Chinese medicine, such as acupuncture and herbal remedy blends, available through the formal health care sector. Further, while still growing, psychosocial dimensions of therapeutic intervention for drug dependency are increasingly common in China. The substance abuse treatment system in China is still undergoing a period of development, especially as the infrastructure expands to meet the needs of those dependent on non-opiate substances. While heroin remains a primary drug of dependence in China, other drugs – such as methamphetamine – have grown increasingly common in recent years (Huang et al, 2011).
Although increasingly medicalized, drug treatment in China has continued to function in a punitive fashion. Considerable differences remain between voluntary substance abuse programs, which are run by health departments and physicians, and compulsory substance abuse treatment, which is administered by the criminal justice sector (Tang and Hao, 2007). Further, even among physicians and health care professionals, attitudes towards drug users and drug treatment have been slow to change (Tang et al., 2005). Yet, despite its pace, the nature of drug treatment in China continues its transformation. Greater emphasis on relapse prevention and behavioral change has advanced, including the establishment of residential therapeutic communities (Tang & Hao, 2007). Thus, substance abuse treatment in China has become more hospitable to drug users themselves over the past two decades.
In spite of improvements in substance abuse treatment programs and the emergence of diverse treatment modalities, many drug users in China remain wary about entering drug treatment. These concerns are not unique to Chinese drug users. Even in Western nations where substance abuse treatment programs provide many options and quality care, heavy drug users express reservations about entering drug treatment (Rapp et al., 2006). Aside from individual reservations, such as the perception of drug use as unproblematic, drug users often cite factors beyond their own locus of control as reasons to avoid drug treatment (Xu et al., 2008). Such external barriers may serve as critical impediments to drug dependent individuals' readiness to change and perceived efficacy.
Barriers to substance abuse treatment serve as obstacles in the already difficult pathway to recovery from drug dependence. Examples of barriers to drug treatment include economic costs (both with regard to the cost of treatment and the potential inability to provide for dependents during treatment), hurdles inherent in the health care system, characteristics of treatment programs available, impediments of geography, and incompatibility of treatment with other obligations and responsibilities, among other factors. While socio-psychological factors underlying the transition to treatment are no doubt crucial (DiClemente et al., 2004), external barriers may further impede pathways to drug treatment even for those who are ready to engage in such programs.
Rapp et al. (2006) developed the Barriers to Treatment Inventory (BTI) to assess both the internal and external barriers to treatment among substance abusers. Xu et al. (2008) used confirmatory factor analysis (CFA) models to assess the factorial structure of the external barriers of the BTI among a sample of American drug users. Their results confirmed four domains of external barriers to drug treatment: time conflicts, treatment accessibility, entry difficulty, and financial problems. We extend this work through the application of a person-centered approach to study the typology of external barriers to drug treatment in China.
Given the growth of drug problems in China over the past two decades and the recent scaling up of medicalized forms of drug treatment, it remains imperative to assess the needs of the large population of drug users in China. In this study, we use Latent Class Analysis (LCA) to identify possible distinct latent classes/groups in Chinese drug users, such that individuals within a class are more similar than those between classes, in regard to barriers that impede the utilization of substance abuse treatment programs. Different from the variable-centered analytical approaches (e.g., ANOVA, multiple regression, multilevel models, and structural equation models) that focus on relations among variables and assume a homogeneous population, LCA is one of the mixture models that are person-centered analytic approaches to model population heterogeneity and identify distinct subpopulations a priori unknown (Clogg 1995; Collins & Lanza 2010; McCutcheon 1987; Muthén 2001, 2002; Magidson & Vermunt 2004). In this regard, we assess typologies of external barriers to better understand approaches that will facilitate the utilization of these services in China by drug using individuals. The identification of subgroups of individuals who perceive external barriers in similar ways may allow for targeted approaches for engagement.
2. Methods
2.1 Sampling
Our analytic sample consisted of 262 subjects recruited at intake from three drug rehabilitation centers in central China. All subjects met the Diagnostic and Statistical Manual-IV-TR (American Psychiatric Association, 2000) criteria for substance abuse based on intake assessment. Subjects met the following inclusion criteria: (a) at least 18 years of age, (b) not diagnosed with schizophrenia or any other psychotic disorder, and (c) had the capacity to understand and consent to research. Those diagnosed only with alcohol abuse or dependence were not eligible. All data received were obtained through self-report by drug users eligible for the study.
Study participants were informed that the survey would take approximately 20-30 minutes to complete and that they were free to withdraw at any stage. Issues of confidentiality and anonymity were discussed during consent procedures. The subjects were encouraged to answer the questionnaire independently and to not discuss their answers with others. All surveys received were anonymous, thus enhancing the privacy and confidentiality of the subjects.
2.2 Measures
Demographic information: The first section of the survey gathered basic demographic information on gender, age, education, marital status and annual income. Substance use: The substance use measures generated basic information consisting of drugs used, duration of use (in months), dose per use, and mode of administration. Measures of external barriers to drug treatment: Three Barriers to Treatment Inventory (BTI) domains of external barriers (i.e., time conflicts, accessibility, and entry difficulty) with a total of seven items (i.e., specific external barriers) were measured among the sample of drug users. The participants were asked to indicate how much each type of barrier influenced their perception of access to treatment services. Each specific external barrier was measured on a 5-point scale (1-strongly disagree, 2-disagree, 3-neutral, 4-agree, and 5-strongly agree). In this study, a response of Agree or Strongly Agree was coded 1, indicating perceiving such a barrier; otherwise 0, indicating no such barrier. The BTI scale was translated into Chinese using the back translation method and then pilot-tested prior to being used in this study.
2.3 Participants
A total of 262 subjects from three centers in Changsha, Hunan were included in our analyses out of 268 individuals recruited for this study over a period of five months. Three subjects voluntarily withdrew from the study and three patients' survey responses for the outcomes of interest were found unreliable or contained too much missing data. Thus, these six subjects were excluded from the final analytic sample of 262 drug users. Within the sample, the most common drug problem experienced by the users was heroin dependence (47.3%), and other drug problems related to methamphetamine (38.5%), ketamine (13.4%), pethidine (0.4%), and buprenorphine (0.4%).
2.4 Statistical Analysis
Latent class analysis (LCA) was used to analyze a typology of external barriers to drug treatment among 262 drug users. Similar to the traditional cluster analysis techniques, the objective of LCA is to identify unobserved subgroups in the target population comprised of similar individuals. In other words, we sought to cluster individuals on the basis of perceived external barriers to drug treatment. Unlike the traditional cluster analysis, however, LCA is a model-based approach to clustering. It identifies subgroups based on posterior class membership probabilities rather than somewhat ad hoc dissimilarity measures such as Euclidean distance. The general probability model underlying LCA allows for formal statistical procedures for determining the number of latent classes, and more interpretable results stated in terms of probabilities.
The LCA modeling process involved several steps. First, we fit a series of LCA models with increasing number of latent classes and the optimal number of classes was determined by comparing k-class model with (k-1)-class model iteratively. Information criterion indices (e.g., AIC, BIC, and ABIC), Lo-Mendell-Rubin likelihood ratio (LMR LR) test (Lo, Mendell, & Rubin 2001), adjusted LMR LR (ALMR LR) test, and bootstrap likelihood ratio test (BLRT; McLachlan 1987; McLachlan & Peel 2000) were used for model comparison or selection of the optimal number of latent classes. Once the number of classes was identified, observations are assigned into their most likely latent classes on the basis of the estimated posterior probabilities for the observations, and the quality of membership classification was assessed via average posterior probabilities and the entropy statistic (Muthén & Muthén, 1998-2010). Next, we assessed the latent class probabilities (i.e., latent class prevalence rates) and the conditional probabilities of endorsing specific categories of the observed items in a given latent class. The latent classes are defined based on the estimated conditional probabilities. Finally, we examined the relationships of the latent class membership with individual characteristics, such as gender, age, education, marital status, income, primary drug use, and duration of the primary drug use in a multinomial logit model. The statistical program Mplus (Muthén & Muthén, 1998-2010) was used for modeling.
3. Results
Table 1 provides the characteristics of the sample of 262 drug users with complete data. As is typical of studies of drug users in China, the sample was primarily male (86%) and of the Han majority (86%). Their ages ranged from 18 to 50 years with mean age of 31.71 years (SD = 7.16). The sample had a fairly even distribution of married (55%) to unmarried (45%) individuals as well as those with at least a high school diploma (48%) to those with less than a high school diploma (52%). A considerable majority (85%) earned less than 20,000 Chinese Yuan within the previous year (<$3,150 USD). In addition, in accordance with recent drug trends, almost half used methamphetamine (“ice”) as their primary drug (47%), while the remainder (53%) utilized another drug as their primary drug, often heroin. The average duration of the use of their primary drug was seven and a half years (Mean = 90 months, SD = 63.1).
Table 1. Sample characteristics (N=262).
| Variable | n (%) |
|---|---|
| Gender | |
| Female | 36 (13.74) |
| Male | 226 (86.26) |
| Marital Status | |
| Unmarried | 119 (45.42) |
| Married | 143 (54.58) |
| Education | |
| <High School | 137 (52.29) |
| High School+ | 125 (47.71) |
| Annual Income | |
| <¥20,000 | 202 (85.11) |
| ¥20,000+ | 39 (14.89) |
| Age Group | |
| <30 | 105 (40.08) |
| 30+ | 157 (59.92) |
| Primary Drug Use | 138 (52.67) |
| Other Drug | 124 (47.33) |
| Ice | |
| Duration of Primary Drug Use1 | Mean: 90.21 (SD: 63.10) |
Note.
Measured in months since initiation of using the primary drug.
We present descriptive assessments of the external barriers in Table 2. With regard to time conflicts, 61.1% agreed they had other things to do and 60.3% agreed that drug treatment does not fit their schedule. With respect to accessibility, 56.9% agreed they were too far away, 83.2% agreed they did not know where to go, and 93.9% agreed they perceived difficulty getting to treatment. For entry difficulty, 74.4% agreed that waiting lists would be too long and 87.8% agreed there were too many steps.
Table 2. Descriptive statistics of external barriers (N=262).
| Items# | n (%) |
|---|---|
| Time Conflict | |
|
|
|
| Have things to do at home | |
| Agree/Strongly Agree | 160 (61.1) |
| Otherwise1 | 102 (38.9) |
| Does not fit my time schedule | |
| Agree/Strongly Agree | 158 (60.3) |
| Otherwise1 | 104 (39.7) |
| Treatment Accessibility | |
|
|
|
| Moving too far away | |
| Agree/Strongly Agree | 149 (56.9) |
| Otherwise1 | 113 (43.1) |
| Do not know where to go | |
| Agree/Strongly Agree | 218 (83.2) |
| Otherwise1 | 44 (16.8) |
| Difficult getting to and from treatment | |
| Agree/Strongly Agree | 246 (93.9) |
| Otherwise1 | 16 (6.1) |
| Entry Difficulty | |
|
|
|
| Waiting list too long | |
| Agree/Strongly Agree | 195 (74.4) |
| Otherwise | 67 (25.6) |
| Too many steps | |
| Agree/Strongly Agree | 230 (87.8) |
| Otherwise1 | 32 (12.2) |
Note.
Responses to each barrier item were measures on a five-point scale:
Strongly disagree;
2-Disagree; 3-Neutral; 4-Agree; and 5-Strongly agree. In this study, a response of Agree or Strongly Agree was coded 1, otherwise 0.
Model fit indices/statistics for LCA models with different number of latent classes are shown in Table 3. The information criterion indices (e.g., AIC, BIC, and ABIC) have much larger values in the single class model than those in the 2-class model, and the p-values of the statistical tests (e.g., LMR LR, ALMR LR, and BLRT) were all statistically significant in the 2-class model. This indicates that the target population is heterogeneous in regard to the external barrier measures. While AIC and ABIC are smaller, BIC is slightly larger in the 3-class model, compared those in the 2-class model; however, all statistical tests reject a 2-class model in favor of the 3-class model. By increasing the number of latent classes from 3 to 4, all the three information criterion indices somewhat increased. Although LMR LR and ALMR LR tests in the 4-class model were statistically significant with p-values of 0.0128 and 0.0141, respectively, the more important bootstrap likelihood ratio test BLRT had an insignificant p-value of 0.5000, indicating that we cannot reject the 3-class model. As such, we are in favor of the 3-class model.
Table 3. Comparisons of LCA Models with different number of latent classes (n=262).
| Model | AIC | BIC | ABIC | LMR LR p-value | ALMR LR p-value | BLRT p-value |
|---|---|---|---|---|---|---|
| 1-Class LCA | 1924.54 | 1949.52 | 1927.33 | - | - | - |
| 2- Class LCA | 1716.07 | 1769.60 | 1722.04 | <0.0001 | <0.0001 | <0.0001 |
| 3- Class LCA | 1694.94 | 1777.01 | 1704.09 | 0.0001 | 0.0002 | <0.0001 |
| 4- Class LCA | 1697.21 | 1807.83 | 1709.55 | 0.0128 | 0.0141 | 0.5000 |
Note.
Not applicable.
AIC: Akaike information criterion
BIC: Bayesian information criterion
ABIC: Sample-size adjusted Bayesian information criterion
LMR LR: Lo-Mendell-Rubin LR test
ALMR LR: Adjusted Lo-Mendell-Rubin LR test
BLRT: Bootstrap likelihood ratio test
The 3-class model has a high Entropy statistic (0.85), indicating a good quality of latent class classification (Ramaswamy et al, 1993; Clark, 2010). The average individual posterior probabilities for being correctly assigned to latent classes 1, 2, and 3 are 0.98, 0.93, and 0.85, respectively (i.e., the diagonal figures in Table 4), which are much higher than the typical cutoff point of 0.70 (Nagin, 2005).
Table 4. Quality of latent class membership classification.
| Latent Class | Class 1 | Class 2 | Class 3 |
|---|---|---|---|
| Class 1 (n=154) | 0.98 | 0.00 | 0.02 |
| Class 2 (n=58) | 0.03 | 0.93 | 0.04 |
| Class 3 (n=50) | 0.00 | 0.15 | 0.85 |
| Entropy=0.85 | |||
Each individual was assigned to a latent class for which the individual has the largest posterior class-membership probability. Among the 262 participants in the sample, 154 of them were assigned into Class 1, 58 into Class 2, and 50 into Class 3. The corresponding latent class probabilities or class prevalence rates for Classes 1, 2, and 3 are, therefore, 0.59, 0.22, and 0.19, respectively (see the upper panel of Table 5). The estimated latent classes can be defined on the basis of the estimated probabilities of endorsing specific categories of the observed items in each class. For example, for Class 3, there was a zero probability of indicating “Agree” or “Strongly Agree” response to “Time Conflict” items. However, everyone in this class indicated “Agree” or “Strongly Agree” to questions “I do not know where to go” and “I will have difficulty getting to and from treatment.” In addition, almost everyone (98%) in this class agreed or strongly agreed that “I will have to go through too many steps to get into treatment,” and the corresponding figure is 90% for “Waiting list is too long.” Since all the barriers that the participants in Class 3 encountered had to do with “Treatment Accessibility” or “Entry Difficulty,” we define this class as “System-Level Barriers Class.” Similarly, Classes 1 and 2 can be defined as a “Major Barriers Class” and a “Low Barriers Class” (see Table 5). The patterns of estimated conditional probabilities of endorsing specific categories of the observed items are plotted by classes in Figure 1. As the curves for the “Major Barriers Class” and a “Low Barriers Class” are basically parallel, we conclude that these two classes share similar barriers, but with differing levels, while the “System-Level Barriers Class” differs from these two classes by types of barriers.
Table 5. Unconditional and Conditional Probabilities: 3-Class LCA Model (n=262).
| Item | Latent Class | ||
|---|---|---|---|
|
|
|||
| Class 1 (Major Barriers) (n= 154) | Class 2 (Low Barriers) (n=58) | Class 3 (System-Level Barriers) (n=50) | |
|
|
|||
| Latent Class Probability | |||
| 0.59 | 0.22 | 0.19 | |
|
|
|||
| Probability of Endorsing Item Category | |||
| Time Conflict | |||
|
|
|||
| Have things to do at home | |||
| Agree/Strongly Agree | 0.95 | 0.23 | 0.00 |
| Otherwise | 0.05 | 0.77 | 1.00 |
| Not fit my time schedule | |||
| Agree/Strongly Agree | 0.97 | 0.16 | 0.00 |
| Otherwise | 0.03 | 0.84 | 1.00 |
| Treatment Accessibility | |||
|
|
|||
| Moving too far away | |||
| Agree/Strongly Agree | 0.69 | 0.24 | 0.64 |
| Otherwise | 0.31 | 0.76 | 0.36 |
| Do not know where to go | |||
| Agree/Strongly Agree | 0.93 | 0.48 | 1.00 |
| Otherwise | 0.07 | 0.52 | 0.00 |
| Difficult getting to and from treatment | |||
| Agree/Strongly Agree | |||
| Otherwise | 1.00 | 0.75 | 1.00 |
| 0.00 | 0.25 | 0.00 | |
| Entry Difficulty | |||
|
|
|||
| Waiting list too long | |||
| Agree/Strongly Agree | 0.78 | 0.56 | 0.90 |
| Otherwise | 0.22 | 0.44 | 0.10 |
| Too many steps | |||
| Agree/Strongly Agree | 0.94 | 0.66 | 0.98 |
| Otherwise | 0.06 | 0.34 | 0.03 |
Figure 1.
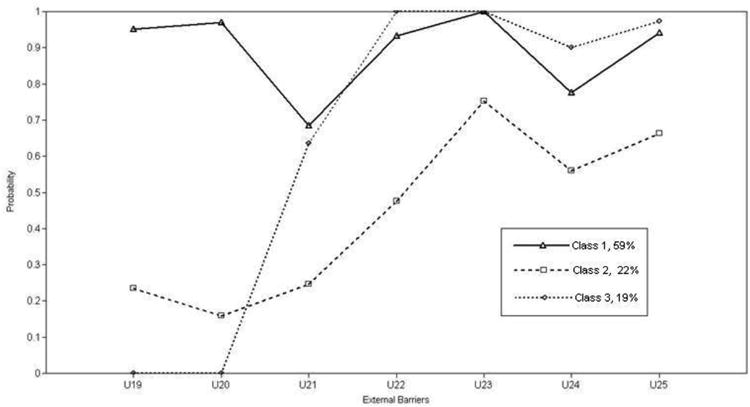
Probabilities of reporting specific external barriers to drug treatment by latent class. Note, the labels on the X-axis are variable names: U19: Have things to do at home; U20: Not fit my time schedule; U21: Moving too far away; U22: Do not know where to go; U23: Difficult getting to and from treatment; U24: Waiting list too long; U25: Too many steps.
We estimated the effects of individual characteristics on the latent class membership from a multinomial logit model, in which we treated the System-Level Barriers Class as the reference group, and the results are shown in Table 6. Drug users aged 30 or older were less likely to be classified in other latent classes (Major Barriers Class and Low Barriers Class): for the older age group, the odds of being in Major Barriers Class and Low Barriers Class were only 0.36 and 0.24, respectively, of the corresponding odds for the young age group.
Table 6. Selected results of latent multinomial logit model: predictors of latent class membership (n=262)1.
| Variable | Latent Class1 | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Class 3 (System-Level Barriers) (n=48)2 | Class 1 (Major Barriers) (n=155) | Class 2 (Low Barriers) (n=59) | ||||
|
|
||||||
| Odds Ratio | (95% C.I.) | Odds Ratio | (95% C.I.) | Odds Ratio | (95% C.I.) | |
| Gender | ||||||
| Female | - | - | - | - | - | - |
| Male | - | - | 0.67 | (0.16, 2.90) | 0.87 | (0.12, 6.09) |
| Married Status | ||||||
| Not Married | - | - | - | - | - | - |
| Married | - | - | 0.84 | (0.37, 1.94) | 1.19 | (0.36, 3.99) |
| Age Group | ||||||
| <30 | - | - | - | - | - | - |
| 30+ | - | - | 0.36 | (0.14, 0.92) | 0.24 | (0.07, 0.82) |
| Education | ||||||
| <High School | - | - | - | - | - | - |
| High School+ | - | - | 0.85 | (0.36, 1.99) | 1.97 | (0.53, 7.37) |
| Annual Income | ||||||
| <¥20,000 | - | - | - | - | - | - |
| ¥20,000+ | - | - | 0.72 | (0.24, 2.20) | 1.83 | (0.46, 7.25) |
| Primary Use Drug | ||||||
| Other Drug | - | - | - | - | - | - |
| Ice | - | - | 3.40 | (1.06, 10.90) | 2.80 | (0.56, 14.08) |
| Duration of Primary Drug Use (months)3 | - | - | 1.00 | (0.99, 1.00) | 1.00 | (1.00, 1.01) |
Note:
When covariates were included into the model, latent class membership classification remained almost unchanged with only two cases moved from Class 3 to Classes 1 and 2, respectively.
Class 3 (i.e., System-level Barriers Class) was treated as the reference group.
Duration of primary drug use was recoded as deviation from overall mean.
Compared to other drug users, those whose primary drug was methamphetamine were much more likely to be in the Major Barriers class; the odds ratio was 3.4. Other measures of individual characteristics, such as gender, marital status, education, annual income, and duration of primary drug use, did not show a significant effect on the latent class membership.
4. Discussion
Drug use remains a growing problem in China and drug treatment services have changed over time in response (Huang et al., 2011; Tang & Hao, 2007). The results described above highlight the external barriers to drug treatment among Chinese drug users. A majority of the sample reported many external barriers. Systems-level barriers were common in this population: 93.9% reporting “difficult getting to and from treatment;” 87.8% reporting “too many steps to get into treatment;” and 83.9% reporting they “do not know where to go” (see Table 2). In this regard, a focus on reducing the systems level barriers to drug treatment would benefit a wide range of drug users in China. Policies directed at facilitating treatment accessibility and highlighting access points for drug treatment would be of considerable importance, and indeed the recent scale up of numerous drug treatment modalities in China are an important step in this direction.
To the best of our knowledge, the present study is the first to apply a person-centered approach to analyze external barriers to drug treatment among Chinese drug users. Our findings provide evidence that the drug using population in China is a heterogeneous population in regard to perceptions of external barriers to drug treatment. The sample of drug users under study were classified into three distinctive classes: major barriers; low barriers; and system-level barriers. A majority of the sample (59%) could be classified in the major barriers to drug treatment class. This further highlights the extent to which Chinese drug users widely perceive significant obstacles to treatment entry that are beyond their locus of control. The numerous obstacles in the lives of these individuals may be further exacerbating personal barriers to drug treatment. Yet, the diminution of the external barriers described in this study through effective policy may enable greater opportunity for those who are drug dependent and desire to access treatment.
Approximately one-fifth (19%) of the participants did not indicate they had time conflict barriers, yet almost everyone in this class reported system-level barriers. In this regard, there may be a sizable population of drug users who are otherwise amenable to drug treatment, in that they perceive availability for it within their own life, but find the structural impediments to treatment entry remain too problematic. Such a population may be most easily channeled toward proper access with proper policies in place.
The class indicating low barriers may be the most difficult to assist via policy changes. Many of these individuals may perceive greater personal barriers to substance abuse treatment instead of external barriers. Thus, outreach efforts and effective engagement, perhaps through harm reduction work with this population, may serve as the most prominent means to effect change the lives of these users and to ensure their health and well-being.
Age group and primary drug used had significant effects on latent class membership. Older drug users were more likely to be in system-level barriers class. In this regard, older individuals were less likely to perceive impediments to their time to be an issue with entry into drug treatment, yet still perceived system-level problems. Thus, older individuals may benefit most significantly from policies that facilitate ease of access to drug treatment.
People using methamphetamine as their primary drug were more likely to be in the major barriers class than in the system-level barriers class. In this regard, methamphetamine users were most likely to perceive a wider range of barriers outside their locus of control. Some of these perceptions may relate to the relatively recent introduction of methamphetamine to Chinese drug markets. The perceived external barriers may pertain specifically to accessing treatment beneficial to non-opiate users. In this regard, the significant scale up of opiate substitution therapies and other treatment modalities for opiate users in China may exclude the needs of those developing problems with other drugs (Yin et al., 2010).
Beyond age and primary drug type, there were no other characteristics that located individuals into particular classes. This finding is important as it indicates that neither education nor income is a significant influence in how drug users perceive external barriers to drug treatment. Additionally, as it has been shown that women in Western nations express unique barriers to drug treatment (e.g. Greenfield et al., 2007), it is interesting that female drug users did not differentially locate into a particular class. Yet, caution must be urged in the consideration of how gender influences entry into drug treatment in China given the relatively small number of women in this sample.
4.1 Limitations
While our findings provide important information about the perceived external barriers to drug treatment among drug users in China, we must consider some of the limitations. First, the sample is a convenience sample drawn from individuals referred to drug treatment. Thus, these individuals may have resolved some of the issues related to external barriers to drug treatment and represent a certain group of drug users. Yet, this would suggest that the hidden population of drug users may find even more significant barriers to drug treatment than those reported by the sample. In addition, the self-report nature of the survey may lead to some biases, particularly those related to social desirability. While this remains a concern for many studies of substance abuse, that these individuals had been referred to evaluation for treatment suggests that they have reduced incentive to misrepresent themselves in their survey responses. Finally, the study was conducted in a provincial capital city in central China, and may not represent the perceptions of barriers to treatment in other regions within China. Despite these limitations, the results reported provide important information on the perception of external barriers to treatment among drug users in China.
4.2 Conclusions
External barriers to drug treatment remain a concern within China in spite of the recent expansion of various drug treatment modalities. Chinese drug users are a heterogeneous population with regard to their perceptions of barriers to treatment beyond their own locus of control. The three subgroups identified perceive these external barriers in different ways and may benefit from targeted approaches to engage them in drug treatment. In this regard, different tactics must be utilized in order to successfully reach this wide ranging group of individuals. Both policies aimed at expanding access to drug treatment further as well as outreach directed towards informing drug users about treatment access points and engaging them in other efforts to promote health and well-being are necessary in order to facilitate the utilization of drug treatment services in China.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and statistical manual of psychiatric disorders. 4th. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Clark SL. Mixture modeling with behavioral data Doctoral dissertation. University of California; Los Angeles: 2010. [Google Scholar]
- Clogg CC. Latent class models. In: Arminger G, Clogg CC, Sobel ME, editors. Handbook of Statistical Modeling for the Social and Behavioral Sciences. Plenum Press; New York: 1995. pp. 311–359. [Google Scholar]
- Collins LM, Lanza ST. Latent Class and Latent Transition Analysis: With Applications in the Social, Behavioural, and Health Sciences. New York: Wiley; 2010. [Google Scholar]
- DiClemente CC, Schlundt D, Gemmell L. Readiness and stages of change in addiction treatment. The American Journal on Addictions. 2004;13:103–119. doi: 10.1080/10550490490435777. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, McHugh RK, Lincoln M, Hien D, Miele GM. Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug and Alcohol Dependence. 86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang K, Zhang L, Liu J. Drug problems in contemporary China: A profile of Chinese drug users in a metropolitan area. International Journal of Drug Policy. 2011;22:128–132. doi: 10.1016/j.drugpo.2010.09.010. [DOI] [PubMed] [Google Scholar]
- Lo Y, Mendell N, Rubin D. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- Magidson J, Vermunt J. Latent class models. In: Kaplan D, editor. The SAGE Handbook of Quantitative Methodology for the Social Sciences. Sage Publications; Thousand Oaks, CA: 2004. pp. 345–368. [Google Scholar]
- McCutcheon AL. Latent Class Analysis Quantitative Applications in the Social Sciences Series No 64. Thousand Oaks, California: Sage Publications; 1987. [Google Scholar]
- McLachlan G, Peel D. Finite mixture models. New York: John Wiley & Sons; 2000. [Google Scholar]
- Muthén B. Latent variable mixture modeling. In: Marcoulides GA, Schumacker RE, editors. New Developments and Techniques in Structural Equation Modeling. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. pp. 1–33. [Google Scholar]
- Muthén B. Beyond SEM: General latent variable modeling. Behaviormetrika. 2002;29:81–117. [Google Scholar]
- Muthén L, Muthén B. Mplus User's Guide. Sixth. Los Angeles, CA: Muthén & & Muthén; 1998-2010. [Google Scholar]
- Nagin DS. Group-based modeling of development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Ramaswamy V, DeSarbo W, Reibstein D, Robinson W. The empirical pooling approach for estimating marketing mix elasticities with PIMS data. Marketing Sci. 1993;12:103–124. [Google Scholar]
- Rapp RC, Xu J, Carr CA, Lane DT, Wang J, Carlson RG. Treatment barriers identified by substance abusers following assessment at a centralized intake unit. J Subst Abuse Treat. 2006;30:227–235. doi: 10.1016/j.jsat.2006.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang YL, Wiste A, Mao PX, Hou YZ. Attitudes, knowledge, and perceptions of Chinese doctors towards drug abuse. J of Subst Abuse Treat. 2005;29:215–220. doi: 10.1016/j.jsat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Tang YL, Hao W. Improving drug addiction treatment in China. Addiction. 2007;102:1057–1063. doi: 10.1111/j.1360-0443.2007.01849.x. [DOI] [PubMed] [Google Scholar]
- Xu J, Rapp RC, Wang J, Carlson RG. The multidimensional structure of external barriers to substance abuse treatment and its invariance across gender, ethnicity, and age. Substance Abuse. 2008;29:43–54. doi: 10.1300/J465v29n01_06. [DOI] [PubMed] [Google Scholar]
- Yin, et al. Scaling up the national methadone maintenance treatment program in China: achievements and challenges. Int J Epidemiol (2010) 2010;39(suppl 2):ii29–ii37. doi: 10.1093/ije/dyq210. [DOI] [PMC free article] [PubMed] [Google Scholar]


