Abstract
Background
Prior studies find no effect of baseline income on response to contingency management (CM) interventions. However, income among substance disordered patients is variable, particularly at treatment entry. This study investigated the impact of during-treatment income, a more proximal estimate of economic resources at the time that CM is in effect, on response to standard treatment or the standard treatment plus CM.
Method
These secondary analyses included 418 cocaine dependent participants initiating community intensive outpatient treatment. We examined whether differences were present in pretreatment and during-treatment overall income, as well as specific income sources. We then conducted a series of regression models to investigate the impact of during-treatment income on treatment outcome.
Results
Participants’ during-treatment income was significantly lower compared to pretreatment income, and this difference was largely attributable to decreases in earned income, illegal income, and support from friends and family. Neither the main effect of income, nor the interaction of income and treatment condition, was significantly associated with treatment outcome. CM, however, was a significant predictor of improved treatment outcome relative to standard treatment. Income sources and some demographic characteristics were also significant predictors of outcomes; public assistance income was associated with improved outcomes and illegal income was associated with poorer outcomes.
Conclusions
These results suggest that substance abusers benefit from CM regardless of their income level, and these data add to the growing literature supporting the generalizability of CM across a variety of patient characteristics.
Keywords: socio-economic status, income, substance abuse treatment, contingency management, patient characteristics, treatment outcome
1. INTRODUCTION
In contingency management (CM) interventions, patients earn reinforcers for attaining verified target behaviors such as abstinence or treatment attendance. Meta-analyses suggest CM is effective for the treatment of a variety of substance use disorders (Lussier et al., 2006; Prendergast et al., 2006), and CM produces the largest effect sizes compared to cognitive-behavioral, relapse prevention, and other psychosocial treatments (Dutra et al., 2008).
Although the evidence base supporting CM’s effectiveness builds, community substance abuse treatment providers endorse many perceived barriers to the adoption and implementation of CM (Kirby et al., 2006; Rash et al., 2012). Many providers are concerned about CM’s generalizability and whether it will be effective for their particular patient population, with specific comorbidities or demographic characteristics. Related to the latter, providers frequently question whether CM will be effective across patients with heterogeneous income levels (Rash et al., 2009), as the overall amount of reinforcement provided is often low. Strong-Kinnamen et al. (2007) found that income was not related to the amount of reinforcement received for patients in CM conditions. We (Rash et al., 2009) found that CM’s effectiveness was not impacted by self-reported income level in a sample of primarily low-income cocaine abusing patients, and Secades-Villa et al. (2013) replicated this effect in a higher income European sample.
However, all three studies (Rash et al., 2009; Secades-Villa et al., 2013; Strong-Kinnamen et al., 2007) used estimates based on income earned prior to treatment entry. Substance abusers’ incomes can be highly variable, especially during periods of transition, and incomes are often low at treatment entry (Metsch et al., 2003; Oggins et al., 2001; Wickizer et al., 2000). During treatment, patients may decrease income-generating illegal activity, have more disposable income due to not buying drugs or alcohol, gain access to benefits and services, or gain or lose employment. Thus, pre-treatment income may reflect past economic resources and may not accurately represent resources available during substance abuse treatment. Income received during the treatment period may provide a more precise estimate of the impact of personal resources on CM’s effectiveness and whether or not higher income patients benefit from CM interventions, especially those providing relatively low magnitudes of reinforcers. In the present study, we first examined if income differed significantly before and after treatment entry. We then examined the impact of during-treatment income on the effectiveness of CM compared to standard treatment. This income estimate reflects the economic resources available at the time patients earned reinforcement if they were randomized to a CM condition, and it provides a more thorough assessment of the impact of patients’ income on response to CM.
2. METHOD
2.1 Participants
Data were collected as part of a randomized trial (Petry et al., 2012) to reduce substance use among cocaine dependent patients in community substance abuse programs. Participants were adult, English-speaking, cocaine dependent patients initiating outpatient substance abuse treatment between 2003 and 2007. Exclusion criteria included: 1) inability to understand the study, 2) uncontrolled psychotic symptoms, 3) active suicidality, or 4) in recovery for pathological gambling. The university’s Institutional Review Board approved study procedures, and all participants provided written informed consent. Of 442 participants randomized in Petry et al. (2012), we excluded 24 participants who did not have any financial data available during the treatment period. Analyses reported herein focused on the 418 remaining participants.
2.2 Measures/Procedures
At baseline, research assistants administered a variety of questionnaires to assess demographic characteristics and substance use diagnoses. Included among these questionnaires was the Service Utilization Form (SUF; Rosenheck and Lam, 1997), which is a comprehensive assessment of medical and mental health service utilization, employment, and financial resources. We assessed the following income sources: earned income, social security benefits (e.g., disability, supplemental), need-based assistance (e.g., rent supplements, food stamps), unemployment and worker’s compensation, vocational training, retirement funds, alimony and child support, other support from family and friends, illegal sources, and gambling wins. The SUF was re-administered one month following the start of treatment and again at the end of the 12-week treatment.
The baseline SUF income estimate represented past year income. At each subsequent time point (i.e., Week 4, Week 12), research assistants inquired about income received since the prior administration of the SUF. For patients who missed the week 4 evaluation, the week 12 evaluation assessed income received since treatment initiation. We excluded those with no income data during active treatment (analyses restricted to N = 418 of 442). Eighty nine percent of the analyzed sample (n = 372 of 418) had financial data for both during-treatment assessment time points. For individuals with missing income data at one of the two assessments (n = 46), we used data from the available time point to estimate income for the full 12-week treatment period (e.g., if the patient did not attend the later assessment, we estimated income based on income reported at the week 4 assessment).
2.3 Treatments
The primary trial (Petry et al., 2012) included two study arms, one for patients with cocaine negative urine samples at treatment initiation, and the second for patients with cocaine positive samples at baseline. For patients in the initially cocaine-negative arm, research assistants randomized participants to one of three conditions: a) standard care, b) abstinence-based CM ($250 average maximum available), or c) attendance-based CM ($250 average maximum available). Participants in the initially cocaine-positive arm were randomized to one of the following conditions: a) standard care, b) abstinence-based CM ($250 average maximum available), or c) abstinence-based CM ($560 average maximum available). Treatment conditions are described briefly below; for details, see Petry et al. (2012).
2.3.1 Standard treatment
All participants received intensive-outpatient group therapy. For up to 6 weeks, services were available for up to 4 hours per day, 5 days per week. Treatment frequency then decreased per the needs of the patient. Aftercare groups (1 per week) were available for up to 1 year. The content and structure of the standard services were similar for all study participants.
Participants in the study also submitted up to 21 urine and breath samples on a tapering frequency schedule that corresponded to reductions in clinical care (i.e., 3 sample submissions per week in weeks 1–3, 2 sample submissions per week in weeks 4–6, 1 sample submission per week in weeks 7–12). Breathalyzers (Intoximeters, St. Louis, MO) tested breath samples for recent alcohol use, and OnTrak TesTstiks (Varian Inc., Walnut Creek, CA) tested urine samples for cocaine and opioids.
2.3.2 Standard treatment plus CM
Participants randomly assigned to the CM conditions received the same standard treatment and sample monitoring as described above. In addition, CM participants earned prizes for meeting target behaviors (abstinence or attendance). Of the four CM conditions, one condition (abstinence-based CM, $250 average maximum available) from each arm was identical. Participants in this condition earned chances to win prizes for each sample submitted that tested negative for alcohol, cocaine, and opioids. The abstinence-based $560 condition was similar, but increased the average maximum available reinforcement from $250 to $560 for participants who submitted all negative samples during the treatment period. In the attendance-based CM condition ($250 average maximum available), participants earned chances to win prizes for attending treatment groups. Urine and breath samples were monitored according to the same frequency outlined above, but the results were not reinforced, in this attendance-based condition.
For the present analyses, we collapsed the four CM conditions and the two standard treatment conditions to increase the power to detect an impact of income on treatment outcomes. Table 1 presents comparisons between the participants assigned to a CM condition and those assigned to standard treatment. No differences were noted between the CM and standard treatment groups on demographic or baseline characteristics.
Table 1.
Baseline characteristics by treatment condition.
| Baseline Variables | Standard Care (n = 134) | Standard Care + CM (n = 284) | Statistic | p |
|---|---|---|---|---|
| Study Arm (%) | Χ2(1) = 0.01 | .94 | ||
| Initially cocaine negative | 25 | 24 | ||
| Initially cocaine positive | 75 | 76 | ||
| % Female | 53 | 56 | Χ2(1) = 0.41 | .52 |
| Race (%) | Χ2(2) = 0.46 | .79 | ||
| Caucasian | 48 | 51 | ||
| African American | 37 | 36 | ||
| Other | 15 | 13 | ||
| % Employed (full or part-time) | 47 | 45 | Χ2(1) = 0.14 | .71 |
| % Married, cohabitating, or remarried | 14 | 12 | Χ2(1) = 0.40 | .53 |
| Age | 36.79 (9.04) | 37.18 (8.98) | t(416) = −0.42 | .68 |
| Years of education | 11.65 (2.23) | 11.99 (1.91) | t(416) = −1.61 | .11 |
| Years of cocaine use | 11.52 (8.37) | 10.62 (7.63) | t(416) = 1.09 | .28 |
Notes. Values are means (SD) unless otherwise noted. CM = Contingency Management.
2.4 Data Analysis
We converted all monetary amounts to 2008 dollars using the Consumer Price Index. We first examined whether income estimates differed for the pretreatment to during-treatment periods. Because the baseline measure of income reflected past year income, we divided the 12-month estimates by 4 to derive 3-month estimates comparable to the 3-month period for during-treatment income. Table 2 lists the percent of participants endorsing each income source and median (IQR) dollars for those reporting income from that source before treatment and during the 12-week treatment period. Income sources are displayed for categories with 5 or more participants endorsing the source; however, all sources (even those not listed in the table) factored into total income. We assessed change in total income from baseline to the during-treatment period using paired t-tests, followed by comparisons of individual income sources. We reported parametric test results given a large sample size and better distribution properties of the difference distribution, but we repeated analyses using the nonparametric test equivalent with the same set of variables reaching significance (data not shown). However, in Table 2 we reported median and IQRs given that the information displayed represents the individual income distributions and not the difference distribution. Additionally, we calculated the medians (IQR) solely for those participants receiving income from a given source to more clearly see why income changes for the full sample (e.g., if mean earned income decreases in the full sample, is it because fewer people are working, or because those who are working are earning lower wages, or both?).
Table 2.
Self-reported income by source for pretreatment and during-treatment periods.
| Pretreatment 3-month income | During-treatment 3-month income | Statistics | |||
|---|---|---|---|---|---|
|
| |||||
| Income source | % Endorsing of total sample (N = 418) | Median (IQR) for participants endorsing income source | % Endorsing of total sample (N = 418) | Median (IQR) for participants endorsing income source | Paired t-test for full sample, p- value |
| Total income from all sources | 99% (n = 412) | $2,820 ($1,130–5,030) | 96% (n = 403) | $2,160 ($880–3,430) | t(416) = −5.39, p <.001 |
| Earned income from jobs | 55% (n = 230) | $1,900 ($580–4,270) | 45% (n = 189) | $1,200 ($540–2,930) | t(416) = −5.70, p <.001 |
| Illegal income | 28% (n = 117) | $1,070 ($250–4,000) | 9% (n = 36) | $600 ($110–1,720) | t(417) = −3.33, p <.001 |
| Public assistance sources | |||||
| Food stamps | 57% (n = 239) | $260 ($110–480) | 59% (n = 247) | $440 ($230–500) | t(417) = 4.77, p <.001 |
| Rent supplements | 11% (n = 46) | $960 ($270–1,950) | 11% (n = 48) | $1,210 ($540–1,800) | t(417) = 0.20, p =.84 |
| Supplemental security | 13% (n = 54) | $1900 ($1,360–2,040) | 16% (n = 67) | $1750 ($1,100–2,040) | t(417) = 1.35, p =.18 |
| Social security disability | 10% (n = 40) | $2,050 ($1,820–2,400) | 12% (n = 51) | $1,740 ($790–2,330) | t(417) = 0.09, p =.93 |
| Other social welfare | 21% (n = 88) | $450 ($160–990) | 19% (n = 79) | $620 ($230–1,010) | t(417) = 0.38, p =.70 |
| Unemployment/worker’s comp/vocational | 8% (n = 33) | $580 ($150–1,380) | 5% (n = 21) | $1,280 ($610–2,130) | t(417) = 0.47, p = .64 |
| Other sources | |||||
| Alimony and child support | 5% (n = 22) | $430 ($270–1,200) | 4% (n = 17) | $410 ($210–1,260) | t(417) = 0.66, p = .51 |
| Support from family/friends | 53% (n = 223) | $160 ($50–650) | 42% (n = 177) | $210 ($70–520) | t(417) = −3.12, p = .002 |
| Gambling wins | 10% (n = 40) | $50 ($10–130) | 6% (n = 27) | $60 ($10–270) | t(417) = −0.27, p = .79 |
Notes. All monetary values are reported in 2008 dollars and rounded to nearest $10. Individual sources are reported only when n > 5, but all sources are included in the total income. During-treatment income is income reported during the 3-month treatment period. Pretreatment income is a 3-month estimate of income calculated from self-reported past year income at study intake. Earned income includes under the table jobs, seasonal positions, and salaried or benefited positions. Medians are reported only for those individuals reporting income from a given source, whereas the t-tests reflect the full sample (including those with $0 income from a given source). IQR = interquartile range.
The remaining analyses focus exclusively on income received during the treatment period. We examined the impact of during-treatment income on treatment outcome using a series of three regression models. The first model began with the primary variables of interest, and each subsequent model included additional explanatory variables to assess the stability of the coefficients of interest. Model 1 included 1) treatment condition (standard treatment = 0, CM = 1), mean-centered overall during-treatment income, and the interaction of these two terms.
To further characterize the impact of income on treatment outcome, we categorized participants’ income by type. Earned income and illegal income were coded as individual dichotomous dummy codes. Earned income was defined as all wages for working including (but not limited to) under the table and day labor income. Illegal income (e.g., drug sales, prostitution) did not include illegal gambling wins or income from under the table work. A third dichotomous code represented public assistance sources, which included food stamps, rent supplements, supplemental security income, disability income, other social welfare sources (e.g., state or county-level aid), unemployment, worker’s compensation, and assistance from vocational programs. Participants could be categorized in some, all, or none of the income source categories.
Model 2 included these three dichotomous indicators of income source as well as the predictors from Model 1. We anticipated that earned income may have a positive impact on treatment outcomes, and that public assistance and illegal sources may have negative associations with treatment outcomes given that these income sources might reflect home environments that pose higher risk for relapse (e.g., economic instability or stress, high-risk neighborhood).
Model 3 built on the prior model and also assessed the impact of controlling for individual characteristics on coefficient stability. Categorical variables included: 1) married, cohabitating, or remarried (versus other marital status), 2) female gender, and 3) treatment arm (cocaine positive or negative sample at treatment initiation). Years of education and lifetime years of cocaine use were entered as continuous predictors. We opted to include years of cocaine use, but not age, in the regression models given substantial overlap, r (N = 418)= 0.50, p < .001, between the two variables.
For all three models, we selected the longest duration of abstinence achieved (LDA) during treatment as the dependent variable for our regression analyses. We chose LDA because it is among the best predictors of posttreatment functioning (Higgins et al., 2000a b; Petry et al., 2005, 2006, 2007) and it was available for 100% of randomized participants. LDA ranges 0–12 weeks and quantifies the longest sustained period of samples negative from alcohol, cocaine, and opioids submitted during treatment. Samples positive for one or more of the three targeted substances, refused samples, and unexcused missed samples interrupted the duration of abstinence.
Both income and LDA were non-normally distributed. We repeated the base model using log-transformed variables, then with two adjusted income variations to curtail the impact of positive skew. The first adjusted income variable replaced the top 5 highest incomes with incremental values increasing by $100. The second adjusted income variable followed the same procedure with the 10 highest incomes. In all iterations, the pattern of results was similar. We present the least adulterated models below, using mean-centered during-treatment income.
3. RESULTS
3.1 Comparison of pretreatment and during-treatment income
Within-subject comparisons of patients’ incomes indicated a significant decrease pretreatment to during-treatment in total 3-month income (mean decrease of $1,488 for the full sample). Table 2 provides a more nuanced view of changes in total income beyond the overall mean change. Relative to the pre-treatment period, an additional 3% of the sample (n =9) reported no income during treatment and, among those reporting income, the amount decreased from pretreatment levels (from a median of $2,820 to $2,160).
Follow-up comparisons of individual income sources suggest that the overall change in income was driven by a limited number of income types. Significant decreases were observed in earned and illegal income. For earned income (see Table 2), an additional 10% of the sample (n = 41) no longer reported any earned income during treatment compared to pretreatment, and the amount of wages decreased among those still working (from a median of $1,900 to $1,200). Fewer individuals (n = 81, 19%) reported illegal income, and median illegal income for those reporting this source decreased (from a median of $1,070 to $600). The number of individuals reporting support from family and friends decreased by 11% (n = 46), resulting in a net decrease in the sample mean average for this source for the entire sample; however, among those receiving monies from this source, the median amount rose slightly (from $160 to $210). Receipt of food stamps increased significantly; 8 additional participants (2%) began receiving food stamps after treatment entry and the 3-month average food stamp amount per person rose ($260 to $440).
3.2 Predictors of Treatment Outcome
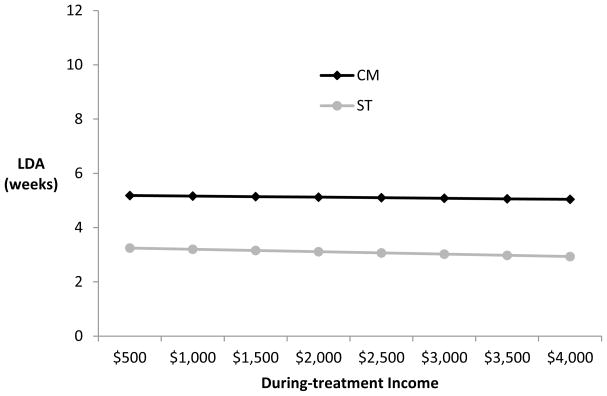
Table 3 lists the unstandardized coefficients and p-values for each of the three models. Model 1, which included the primary predictors of interest, was significant and accounted for 4% of the variance, F (3, 414) = 6.77, p < .001. Treatment condition was the only significant predictor (p < .001). During-treatment income was not significantly associated with LDA as a main effect (p = .54). Also, the interaction between income and treatment condition was not significant (p = .75) suggesting that the association of income and treatment outcome does not differ for those randomized to CM compared to standard treatment. Figure 1 displays predicted LDA for selected values of during-treatment income by treatment condition. Participants in the CM conditions achieve about 2 additional weeks of continuous abstinence compared to those in the standard treatment conditions, regardless of income.
Table 3.
Unstandardized regression coefficients and p-values for Models 1–3.
| Predictors | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| B | p | Beta | p | Beta | p | |
| CM (vs. standard treatment) | 1.91 | <.001 | 1.94 | <.001 | 1.75 | <.001 |
| Income during treatment period | −0.09 | .54 | −0.15 | .33 | −0.19 | .18 |
| Interaction: treatment condition x income | 0.05 | .75 | 0.13 | .42 | 0.20 | .21 |
| Income type | ||||||
| Earned | - | - | 0.56 | .18 | 0.03 | .94 |
| Public assistance | - | - | 1.22 | .007 | 1.77 | <.001 |
| Illegal | - | - | −1.98 | .007 | −1.66 | .02 |
| Married, cohabitating, or remarried (vs. other) | - | - | - | - | 0.64 | .26 |
| Caucasian (vs. other) | - | - | - | - | −0.15 | .71 |
| Female | - | - | - | - | −0.70 | .07 |
| Cocaine positive sample at treatment initiation | - | - | - | - | −2.97 | <.001 |
| Years of education | - | - | - | - | 0.28 | .004 |
| Years of cocaine use | - | - | - | - | −0.04 | .17 |
|
| ||||||
| Adjusted R2 | 0.04 | 0.07 | 0.17 | |||
Note. CM = contingency management.
Figure 1.
Predicted longest durations of abstinence (LDA; weeks) for selected income values for participants randomized to standard treatment (ST) or contingency management (CM) conditions. No significant effect of income on treatment outcome is present. The income estimate includes all sources of income (e.g., earned, public assistance, illegal) during the 12-week treatment period. Predicted values were calculated using Model 1 coefficients. Model 1 included the primary variables of interest: treatment condition (CM versus standard treatment), mean centered during-treatment income, and the interaction of these terms.
Model 2 examined the added value of income source codes in the prediction of LDA, F (6, 411) = 6.27, p < .001 (adjusted R2 = 0.07). CM remained significantly associated with improved outcomes (p < .001). Neither income, nor the income by treatment condition interaction, were significant predictors (ps = .33 and .42, respectively). Of the income source predictors, income from illegal sources was negatively associated with treatment outcomes (p = .007). Income from public assistance (e.g., food stamps, state aid programs) was positively associated with treatment outcome (p = .007). The presence of earned income was not significantly associated with LDA (p = .18).
Model 3, accounting for 17% of the variance in LDA, assessed the stability of the coefficients of interest while controlling for demographic and baseline characteristics, F (12, 405) = 8.32, p < .001. Treatment condition and the illegal and public assistance income source codes remained significant predictors. Neither income, nor the income by treatment condition interaction, were significantly associated with LDA. Among the demographic and baseline characteristics, years of education was positively associated, and a cocaine-positive sample at treatment entry was negatively associated, with LDA.
4. DISCUSSION
This study addressed a common question among providers regarding whether CM will be as effective with patients of greater financial means compared to those with less resources. Results suggested that CM is effective for substance abuse treatment-seekers regardless of income level, and these results remained stable after controlling for other variables that may impact the association between income and treatment outcome. The present analyses extend those of previous studies (Rash et al., 2009; Secades-Villa et al., 2013) by using income received during the active treatment phase. During-treatment income is a more proximal estimate of economic resources and is consistent with the period that monetary-based reinforcers are available for patients randomized to these conditions. Income decreased during treatment from pretreatment levels, and these decreases were driven largely by less earned income, less illegal income, and less support from family and friends. For example, we noted that fewer individuals reported earned income during treatment, but we also found lower earnings among those who continued to report this type of income.
Income was not related to treatment response for patients in the standard treatment or CM conditions. These findings, as well as others (Littlejohn, 2006; Rash et al., 2009; Secades-Villa et al., 2013), suggest that treatment-seeking substance abusers respond equally well to substance abuse treatment across income levels. However, some studies (Gregoire and Snively, 2001; Richmond et al., 1995; Roffman et al., 1993; Stephens et al., 1993; Walton et al., 2003) suggest that economic stability is positively related to treatment and posttreatment outcomes, with economic stability often defined more broadly than solely income as done in this study (e.g., housing, ability to pay bills, employment status, education level). Further, we note that income may be associated with treatment entry, such that lower income individuals may be more likely to receive treatment (Ilgen et al., 2011).
In contrast to our prior study (Rash et al., 2009), the specific sources of income were important correlates of treatment outcome. In this study, income from public assistance sources had a beneficial impact on treatment outcome, and illegal income was negatively associated with LDA. Related to the latter, illegal activity may serve as a proxy for continued involvement in drug culture that presents challenges for achieving sobriety. Another study (Petry et al., 2011a) suggests that any legal related difficulties, including involvement in income-producing illegal activities, are associated with poor treatment response. McLellan et al. (1981) found methadone maintained patients who relied primarily on public assistance support did not significantly reduce their drug use while in treatment, but decreases in drug use were noted for those reporting illegal and employment income. In another sample, Kosten et al. (1987) found that methadone patients made improvements in outcomes, regardless of their primary form of financial support, but the types of improvements depended on income sources. Relative to those who worked for pay or obtained income illegally, those who relied on public assistance made relatively little improvement in legal and employment domains, but they exhibited the greatest reductions in psychiatric, medical, and family problems (Kosten et al., 1987). Oggins et al. (2001) note that public assistance may provide an avenue for individuals with substance abuse disorders to remain in treatment, and treatment exposure is positively associated with outcomes (e.g., Metsch et al., 2003).
Cocaine positive samples at intake were associated with shorter durations of abstinence. This finding is not surprising as a positive sample at treatment initiation is a consistent and strong indicator of treatment response (Alterman et al., 1996, 1997; Petry et al., 2004, 2006; Preston et al., 1998; Stitzer et al., 2007a b). Years of education was the only other demographic or baseline characteristic significantly associated with LDA. Education is another commonly used index of socio-economic status and its relation to substance abuse treatment outcomes is mixed. McKay et al. (2005) found that years of education did not predict cocaine use at any time point up to 36 months posttreatment in crack cocaine users, but this same predictor was negatively associated with posttreatment alcohol use at one time point among alcohol users when controlling for current use. Other studies (Rash et al., 2009; Roffman et al., 1993) find no relation between education and treatment outcomes. Future studies are needed to clarify this relationship, as well as whether other socio-economic status indicators (e.g., housing, ability to pay bills) provide disparate results compared to relying solely on income.
This study used a large, representative sample of cocaine dependent treatment seekers recruited from community intensive outpatient programs. These findings may be limited to treatment-seeking substance abusers, as their income is substantially lower than the general population in the US, and the question of whether these results would replicate in other substance using samples (e.g., cigarette smokers) remains unaddressed. The incomes in this sample are, however, representative of treatment-seeking substance abusers. In the National Survey on Drug Use and Health (2008) survey, 45% of adults with an outpatient treatment episode for alcohol, drugs, or both in the past year reported a yearly income of less $10,000, 68% reported incomes of less than $20,000, and 84% reported incomes of less than $30,000. In this sample, 45% reported less than $10,000 income in the year prior to intake, 75% reported incomes less than $20,000, and 85% reported incomes of less than $30,000.
A strength of this study was the focus on during-treatment income, which provides a more precise estimate of economic resources at the time that CM is in effect. Substance abusers’ incomes can shift substantially during treatment episodes (Metsch et al., 2003; Oggins et al., 2001; Wickizer et al., 2000) and this pattern was evident in this sample who had lower incomes during the treatment compared to the pretreatment period. Income restrictions associated with entry into substance abuse treatment may have important clinical and policy implications, and increasing patient engagement in vocational skills and training programs may be an avenue to aid patients’ return to higher socioeconomic resource levels. These programs may yield broad effects on patient outcomes beyond economic improvement. For example, Petry et al. (in press) found that substance abuse outpatients in a CM program who engaged in 2 or more job-related activities (e.g., resume building, submitting applications) had greater reductions in employment-related problems, improved quality of life, better treatment retention, and longer periods of sustained abstinence compared to those who engaged in 1 or fewer job-related activities.
Limitations of this study include the use of self-reported income and the reliance on income as a primary indicator of economic stability. In addition, this study used different time frames for assessing income at baseline and the during-treatment periods, which may impact reliability or validity of the reports. Substance abusers reliably report income (Johnson et al., 1999), but reliable reports may still contain bias or error and therefore may not be entirely valid. For example, Aiken (1986) found that treatment-seeking substance abusers exhibit a positive self-presentation bias in their self-report of income. Moore et al. (1997) suggest that income reported during shorter periods (i.e., monthly) may be more biased than reports of yearly income and that reports of earned income are more reliable than reports of other sources, such as public assistance, which are more prone to error.
Despite these limitations, the results of this study suggest that CM is effective across income levels in cocaine dependent treatment-seekers. Participants benefited from CM in terms of longer durations of sustained abstinence regardless of whether they reported relatively low or high income during the treatment period. This study adds to the growing literature supporting CM’s effectiveness across a range of demographic (Barry et al., 2009; Rash et al., 2009; Secades-Villa et al., 2013), clinical (Rash et al., 2008a; Petry et al., 2011a b), and psychiatric (Alessi et al., 2011; Rash et al., 2008b; Weinstock et al., 2007) characteristics.
Acknowledgments
Role of funding source
Support for this research and manuscript preparation was provided by the National Institutes of Health grants R21-DA031897, P30-DA023918, P50-DA009241, T32-AA007290, R01-DA027615, P60-AA03510, R01-HD075630, and M01-RR06192. NIH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Footnotes
Contributors
All authors contributed to this manuscript. Dr. Petry designed the study and research protocol. Dr. Rash conducted the analyses and wrote the first draft. Drs. Petry and Andrade contributed to subsequent manuscript drafts. All authors have read and approved the final manuscript.
Conflicts of Interest
All authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Carla J. Rash, Email: Rashc@uchc.edu, Calhoun Cardiology Center, Department of Medicine, University of Connecticut Health Center MC-3944, 263 Farmington Avenue, Farmington, CT 06030-3944, (860) 679-4689, Fax: (860) 679-1312.
Leonardo F. Andrade, Department of Psychiatry, University of Connecticut Health Center, 263 Farmington Avenue, Farmington, CT 06030-3944.
Nancy M. Petry, Calhoun Cardiology Center – Behavioral Health, University of Connecticut Health Center, 263 Farmington Avenue, Farmington, CT 06030-3944.
References
- Aiken LS. Retrospective self-reports by clients differ from original reports: implications for the evaluation of drug treatment programs. Int J Addict. 1986;21:767–788. doi: 10.3109/10826088609027391. [DOI] [PubMed] [Google Scholar]
- Alessi SM, Rash C, Petry NM. Contingency management is efficacious and improves outcomes in cocaine patients with pretreatment marijuana use. Drug Alcohol Depend. 2011;118:62–67. doi: 10.1016/j.drugalcdep.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alterman AI, Kampman K, Boardman CR, Cacciola JS, Rutherford MJ, McKay JR, Maany I. A cocaine-positive baseline urine predicts outpatient treatment attrition and failure to attain initial abstinence. Drug Alcohol Depend. 1997;46:79–85. doi: 10.1016/s0376-8716(97)00049-5. [DOI] [PubMed] [Google Scholar]
- Alterman AI, McKay JR, Mulvaney FD, McLellan AT. Prediction of attrition from day hospital treatment in lower socioeconomic cocaine-dependent men. Drug Alcohol Depend. 1996;40:227–33. doi: 10.1016/0376-8716(95)01212-5. [DOI] [PubMed] [Google Scholar]
- Barry D, Sullivan B, Petry NM. Comparable efficacy of contingency management for cocaine dependence among African American, Hispanic, and White methadone maintenance clients. Psychol Addict Behav. 2009;23:168–174. doi: 10.1037/a0014575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry. 2008;165:179–187. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- Gregoire TK, Snively CA. The relationship of social support and economic self-sufficiency to substance abuse outcomes in a long-term recovery program for women. J Drug Educ. 2001;31:221–237. doi: 10.2190/3T8L-AGY5-KBV6-3TRQ. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Badger GJ, Budney AJ. Initial abstinence and success in achieving longer-term cocaine abstinence. Exp Clin Psychopharmacol. 2000a;8:377–386. doi: 10.1037//1064-1297.8.3.377. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Wong CJ, Badger GJ, Haug Ogden DE, Dantona RL. Contingent reinforcement increases cocaine abstinence during outpatient treatment and 1 year follow-up. J Consult Clin Psychol. 2000b;68:64–72. doi: 10.1037//0022-006x.68.1.64. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Price AM, Burnett-Zeigler I, Perron B, Islam K, Bohnert AS, Zivin K. Longitudinal predictors of addictions treatment utilization in treatment-naïve adults with alcohol use disorders. Drug Alcohol Depend. 2011;113:215–221. doi: 10.1016/j.drugalcdep.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson ME, Fisher DG, Reynolds G. Reliability of drug users’ self-report of economic variables. Addict Res Theory. 1999;7:227–238. [Google Scholar]
- Kirby KC, Benishek LA, Dugosh KL, Kerwin ME. Substance abuse treatment providers’ beliefs and objections regarding contingency management: implications for dissemination. Drug Alcohol Depend. 2006;85:19–27. doi: 10.1016/j.drugalcdep.2006.03.010. [DOI] [PubMed] [Google Scholar]
- Kosten TR, Rounsaville BJ, Kleber HD. Predictors of 2.5-year outcome in opioid addicts: pretreatment source of income. Am J Drug Alcohol Abuse. 1987;13:19–32. doi: 10.3109/00952998709001498. [DOI] [PubMed] [Google Scholar]
- Littlejohn C. Does socio-economic status influence the acceptability of, attendance for, and outcome of, screening and brief interventions for alcohol misuse: a review. Alcohol Alcohol. 2006;41:540–545. doi: 10.1093/alcalc/agl053. [DOI] [PubMed] [Google Scholar]
- Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- McKay JR, Foltz C, Stephens RC, Leahy PJ, Crowley EM, Kissin W. Predictors of alcohol and crack cocaine use outcomes over a 3-year follow-up in treatment seekers. J Subst Abuse Treat. 2005;28:S73–82. doi: 10.1016/j.jsat.2004.10.010. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Ball JC, Rosen L, O’Brien CP. Pretreatment source of income and response to methadone maintenance: a follow-up study. Am J Psychiatry. 1981;138:785–789. doi: 10.1176/ajp.138.6.785. [DOI] [PubMed] [Google Scholar]
- Metsch LR, Pereyra M, Miles CC, McCoy CB. Welfare and work outcomes after substance abuse treatment. Soc Serv Rev. 2003;77:237–254. [Google Scholar]
- Moore JC, Stinson LL, Welniak EJ. Income Measurement Error in Surveys: A Review. US Census Bureau; 1997. downloaded 03/17/13 from www.census.gov.edgekey.net/srd/papers/pdf/sm97-05.pdf. [Google Scholar]
- Oggins J, Guydish J, Delucchi K. Gender differences in incomes after substance abuse treatment. J Subst Abuse Treat. 2001;20:215–224. doi: 10.1016/s0740-5472(01)00163-5. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Carroll KM, Hanson T, MacKinnon S, Rounsaville B, Sierra S. Contingency management treatments: reinforcing abstinence versus adherence with goal-related activities. J Consult Clin Psychol. 2006;74:592–601. doi: 10.1037/0022-006X.74.3.592. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Hanson T, Sierra S. Randomized trial of contingent prizes versus vouchers in cocaine-using methadone patients. J Consult Clin Psychol. 2007;75:983–991. doi: 10.1037/0022-006X.75.6.983. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Marx J, Austin M, Tardiff M. Vouchers versus prizes: contingency management treatment of substance abusers in community settings. J Consult Clin Psychol. 2005;73:1005–1014. doi: 10.1037/0022-006X.73.6.1005. [DOI] [PubMed] [Google Scholar]
- Petry NM, Andrade LF, Rash CJ, Cherniack MG. Reinforcing job-related activities reduces employment problems and improves quality of life in substance abusing patients. Psychol Addict Behav. doi: 10.1037/a0032264. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Barry D, Alessi SM, Rounsaville BJ, Carroll KM. A randomized trial adapting contingency management targets based on initial abstinence status of cocaine-dependent patients. J Consult Clin Psychol. 2012;80:276–285. doi: 10.1037/a0026883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Ford JD, Barry D. Contingency management is especially efficacious in engendering long durations of abstinence in patients with sexual abuse histories. Psychol Addict Behav. 2011b;25:293–300. doi: 10.1037/a0022632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Rash CJ, Easton CJ. Contingency management treatment in substance abusers with and without legal problems. J Am Acad Psychiatry Law. 2011a;39:370–378. [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Tedford J, Austin M, Nich C, Carroll KM, Rounsaville BJ. Prize reinforcement contingency management for treatment of cocaine abusers: How low can we go, and with whom? Addiction. 2004;99:349–360. doi: 10.1111/j.1360-0443.2003.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prendergast M, Podus D, Finney J, Greenwell L, Roll J. Contingency management for treatment of substance use disorders: a meta-analysis. Addiction. 2006;101:1546–1560. doi: 10.1111/j.1360-0443.2006.01581.x. [DOI] [PubMed] [Google Scholar]
- Preston KL, Silverman K, Higgins ST, Brooner RK, Montoya I, Schuster CR, Cone EJ. Cocaine use early in treatment predicts outcome in a behavioral treatment program. J Consult Clin Psychol. 1998;66:691–696. doi: 10.1037//0022-006x.66.4.691. [DOI] [PubMed] [Google Scholar]
- Rash CJ, Alessi SM, Petry NM. Cocaine abusers with and without alcohol dependence respond equally well to contingency management treatments. Exp Clin Psychopharmacol. 2008b;16:275–281. doi: 10.1037/a0012787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rash CJ, Alessi SM, Petry NM. Contingency management is efficacious for cocaine abusers with prior treatment attempts. Exp Clin Psychopharmacol. 2008a;16:547–554. doi: 10.1037/a0014042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rash CJ, Olmstead TA, Petry NM. Income does not affect response to contingency management treatments among substance abuse treatment-seekers. Drug Alcohol Depend. 2009;104:249–253. doi: 10.1016/j.drugalcdep.2009.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rash CJ, Petry NM, Kirby KC, Martino S, Roll J, Stitzer ML. Identifying provider beliefs related to contingency management adoption using the contingency management beliefs questionnaire. Drug Alcohol Depend. 2012;1:121–212. doi: 10.1016/j.drugalcdep.2011.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richmond R, Heather N, Wodak A, Kehoe L, Webster I. Controlled evaluation of a general practice-based brief intervention for excessive drinking. Addiction. 1995;90:119–132. doi: 10.1046/j.1360-0443.1995.90111915.x. [DOI] [PubMed] [Google Scholar]
- Roffman RA, Klepsch R, Wertz JS, Simpson EE, Stephens RS. Predictors of attrition from an outpatient marijuana-dependence counseling program. Addict Behav. 1993;18:553–566. doi: 10.1016/0306-4603(93)90071-g. [DOI] [PubMed] [Google Scholar]
- Rosenheck R, Lam JA. Individual and community-level variation in intensity and diversity of service utilization by homeless persons with serious mental illness. J Nerv Ment Dis. 1997;185:633–638. doi: 10.1097/00005053-199710000-00007. [DOI] [PubMed] [Google Scholar]
- Secades-Villa R, Garcia-Fernandez G, Pena-Suares E, Garcia-Rodriguez O, Sanchez-Hervas E, Fernandez-Hermida J. Contingency management is effective across cocaine-dependent outpatients with different socioeconomic status. J Subst Abuse Treat. 2013;44:349–354. doi: 10.1016/j.jsat.2012.08.018. [DOI] [PubMed] [Google Scholar]
- Stephens RS, Wertz JS, Roffman RA. Predictors of marijuana treatment outcomes: the role of self-efficacy. J Subst Abuse. 1993;5:341–353. doi: 10.1016/0899-3289(93)90003-t. [DOI] [PubMed] [Google Scholar]
- Stitzer ML, Peirce J, Petry NM, Kirby K, Roll J, Krasnansky J, Cohen A, Blaine J, Vandrey R, Kolodner K, Li R. Abstinence-based incentives in methadone maintenance: interaction with intake stimulant test results. Exp Clin Psychopharmacol. 2007;15:344–50. doi: 10.1037/1064-1297.15.4.344. [DOI] [PubMed] [Google Scholar]
- Stitzer ML, Petry N, Peirce J, Kirby K, Killeen T, Roll J, Hamilton J, Stabile PQ, Sterling R, Brown C, Kolodner K, Li R. Effectiveness of abstinence-based incentives: interaction with intake stimulant test results. J Consult Clin Psychol. 2007;75:805–11. doi: 10.1037/0022-006X.75.5.805. [DOI] [PubMed] [Google Scholar]
- Strong-Kinnamen JE, Slade E, Bennett ME, Bellack AS. Examination of contingency payments to dually-diagnosed patients in a multi-faceted behavioral treatment. Addict Behav. 2007;32:1480–1485. doi: 10.1016/j.addbeh.2006.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. Office of Applied Studies, National Survey on Drug Use and Health. ICPSR26701-v3. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor]; 2008. 2012-12-10. [DOI] [Google Scholar]
- Walton MA, Blow FC, Bingham CR, Chermack ST. Individual and social/environmental predictors of alcohol and drug use 2 years following substance abuse treatment. Addict Behav. 2003;28:627–642. doi: 10.1016/s0306-4603(01)00284-2. [DOI] [PubMed] [Google Scholar]
- Weinstock J, Alessi SM, Petry NM. Regardless of psychiatric severity the addition of contingency management to standard treatment improves retention and drug use outcomes. Drug Alcohol Depend. 2007;87:288–296. doi: 10.1016/j.drugalcdep.2006.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickizer TM, Campbell K, Krupski A, Stark K. Employment outcomes among AFDC recipients treated for substance abuse in Washington State. Milbank Q. 2000;78:585–608. doi: 10.1111/1468-0009.00186. [DOI] [PMC free article] [PubMed] [Google Scholar]