Abstract
Low socioeconomic status (low SES), as defined by income or educational attainment, has been associated with obesity in industrialized nations. Low SES persons have limited resources and may experience food insecurity that increases food reinforcement. Food reinforcement has been positively related to energy intake and weight status, and increased food reinforcement may explain the higher prevalence of obesity among low SES individuals who have restricted access to low-energy-dense foods and non-food reinforcers. We measured annual household income, highest education level completed and food reinforcement in 166 adults of varying body mass index (BMI, kg/m2). Multivariate linear regression analyses controlling for age, sex, minority status, session hunger and the reinforcing value of non-food alternatives showed that household income was related to food reinforcement (p = 0.048) and BMI (p = 0.019), and that food reinforcement was related to BMI (p = 0.0017). Path analyses revealed a significant indirect effect of household income on BMI through food reinforcement, suggesting that the relationship between lower household income and greater BMI was mediated in part by increased food reinforcement. A similar pattern of results was observed when education level was used as the proxy for SES. These findings support the hypothesis that deprivation and restricted food choice associated with low SES enhance food reinforcement, increasing the risk for obesity.
Introduction
Low socioeconomic status (low SES), as defined by income or educational attainment, has been associated with obesity in industrialized nations (1). While there have been steady increases in the prevalence of overweight across all socioeconomic classes, the highest proportions are still found amongst the most disadvantaged groups (2). The mechanism of association between low SES and obesity has yet to be elucidated, but a potential explanation is that low SES environments increase food reinforcement and promotes excessive energy intake. Understanding this pathway could help inform public policy directed at eliminating social disparities in obesity prevalence.
Reinforcement refers to the capacity of a stimulus to increase the frequency of a preceding behavior, and can be quantified by the amount of effort participants would expend for access to the stimulus. Disparate stimuli vary in reinforcement, and these differences are thought to shape choice among concurrently available alternatives (3). Food is a powerful reinforcer, and elevated food reinforcement has been associated with greater energy intake (4) and weight status (5). Thus, food reinforcement could guide decisions on when, what and how much to eat. Food reinforcement may be influenced by several life circumstances associated with low SES. In particular, low SES individuals may experience enhanced food reinforcement stemming from restricted access to or concerns about acquiring nutritionally adequate amounts of food, or food insecurity (6). Both actual and perceived deprivation increases food reinforcement (7). In addition, while acute deprivation increases food reinforcement for the next eating bout (8), chronic deprivation leads to neurochemical changes that increases food reinforcement even when food later becomes plentiful (9). These findings are in accordance with studies demonstrating that food insecurity is associated with obesity (6), and that childhood exposure to poverty is associated with assignment of psychological significance to food, binge eating, and obesity (10).
Furthermore, low SES people may experience greater food reinforcement because they have limited access to non-food reinforcers. Low SES neighborhoods have fewer physical activity facilities, and those that are available are often not safe to use (11). Many structured recreational activities (e.g. receiving music lessons) that are less compatible with eating are also more costly than sedentary activities (e.g. watching television) that tend to be accompanied by snacking behavior (12). Eating represents a choice among many behaviors, and when non-food reinforcers are harder to obtain than food reinforcers, preferences may be shifted toward eating (3). In support of this argument, low SES has been related to overweight through increased sedentary behaviors (13), and increased frequency of sedentary behaviors have been associated with greater energy intake (14).
Moreover, low SES neighborhoods often have fewer supermarkets and are primarily supplied by non-chain convenience stores poorly stocked in fruits and vegetables (15). Food at these locations are frequently more expensive than the same food at chained supermarkets (15), encouraging patrons to purchase and consume high-energy-dense, nutrient-poor foods that are typically more affordable than low-energy-dense, nutrient-rich foods (16). Consistent with these observations, the prevalence of obesity is lower in areas with supermarkets and higher in areas with small grocery stores or fast-food restaurants (17), and low SES people consume more fat as well as fewer fruits and vegetables than high SES peers (18). Notably, research suggests that regular consumption of palatable foods high in sugar and fat increases food reinforcement (19).
Collectively, these data suggest that low SES environments enhance food reinforcement and increase obesity risk. SES is a multidimensional construct that has been difficult to conceptualize in health research (20), but income and education level are two commonly-used indices of SES that have each been inversely associated with obesity (1). As an initial test of our hypothesis that greater food reinforcement may explain the relationship between low SES and obesity, we examined whether food reinforcement statistically mediated the effects of income or education level on BMI in 166 adults of varying body mass index (BMI, kg/m2).
Methods and Procedures
Participants
Full details of the study design have been reported elsewhere (4) and are summarized below. Participants were recruited for a study of genetic factors associated with food reinforcement from an existing family database, newspaper ads, flyers posted around the University at Buffalo campuses and in community settings, web-based sources (e.g. ads on Craig’s list and on the department’s website), and direct mailings targeted to community residents between the ages of 18–50. Exclusion criteria included medications influencing appetite, tobacco use, diabetes, current or past history of an eating disorder or a psychiatric disorder (e.g. anxiety, depression, attention deficit hyperactivity disorder), allergies to the study foods, current dieting, pregnancy, or low liking of more than two of the six study foods (<4 on a 9-point Likert-type scale). Of the 1387 individuals who were screened, 273 were eligible and agreed to participate. The analytic sample consisted of 166 of the 273 participants who were studied (47 non-obese females, 32 non-obese males, 37 obese females, 51 obese males). Participants with missing income (n = 2) or session hunger (n = 1) data were excluded from analysis. Current students (n = 94) and homemakers (n = 10) were also excluded from analysis, since their income or education level may not accurately reflect their SES (21). The study was approved by the University at Buffalo Health Sciences Institutional Review Board. Participant characteristics are shown in Table 1.
Table 1.
Participant characteristics.a
| Overall | |
|---|---|
| N | 166 |
| Age (years) | 39.7 ± 8.3 |
| Body Mass Index (kg/m2) | 31.6 ± 7.8 |
| Sex (M/F) | 82/84 |
| Highest Education Level Completed | |
| Attended high school | 2 |
| Completed high school | 25 |
| Some college/vocational training | 32 |
| Completed 2-year college | 36 |
| Completed 4-year college | 46 |
| Completed graduate/professional school | 25 |
| Self-reported Minority Status | |
| Minority (non-Caucasian)b | 41 |
| Non-minority (Caucasian) | 125 |
| Total Household Income (USD) | |
| <$40,000 | 41 |
| $40,000 – $79,999 | 65 |
| ≥$80,000 | 60 |
| Reinforcing Value of Foodc | 546.1 ± 1190.4 |
| Reinforcing Value of Non-Food Alternativesd | 879.9 ± 1295.7 |
| Total Time Spent Responding for Food (minutes) | 3.26 ± 5.10 |
| Total Time Spent Responding for Non-Food Alternatives (minutes) | 4.74 ± 6.22 |
Plus-minus values are means ± SD.
Of the 41 non-Caucasian participants, 1 self-identified as “Asian/Pacific Islander”, 31 as “Black/African American”, 4 as “Hispanic” and 7 as “More than one race”.
Reinforcing value of food (food reinforcement) was measured by the total number of responses participants made for food in a computerized choice task.
Reinforcing value of non-food alternatives was measured by the total number of responses participants made for reinforcers other than food in a computerized choice task.
Procedures
Participants visited the laboratory for two sessions. They first completed an ad libitum snack-eating task to identify their favorite high-energy-dense snack food, and then a computerized choice task 2–3 weeks later to measure their food reinforcement. Prior to both sessions, participants were asked to refrain from consuming anything other than water for ≥ 3 hours and to not consume the experimental foods for ≥24 hours. Upon arrival at the laboratory, participants completed multi-pass dietary recalls to verify adherence to study protocol. Participants were then provided a choice of three isocaloric (150 kcal) energy bar preloads to standardize homeostatic hunger and increase the ability to demonstrate individual differences in food reinforcement (22). Demographic information and anthropometrics were obtained at the end of the ad libitum eating session.
Session hunger
Subjective ratings of hunger during the food reinforcement task were collected before and after consumption of the preload using a Likert-type scale, with 1 indicating not at all hungry and 10 indicating extremely hungry. In all analyses, session hunger refers to the self-reported hunger scores following consumption of the preload.
Ad libitum snack-eating task
The ad libitum snack-eating task was presented as a taste test (4). Participants were provided 210–305 kcal (42–60 g) servings of six high-energy-dense snack foods (amount of food presented (g) and energy density (kcal/g) shown in parentheses): Wavy Lay’s Potato Chips (57 g, 5.4); Cooler Ranch Doritos (56 g, 5.4); M&M’s (60 g, 5.0);Twix (48 g, 5.0); Kit Kat (42 g, 5.0); and Butterfinger (57 g, 4.5). Water was provided ad libitum. Participants were told that they could eat as much or as little as they wanted, but to at least try the foods so that they could accurately rate them on various characteristics (pleasantness, sweetness, blandness, flavorfulness, and bitterness) using 9-point Likert-type scales. After rating the foods, participants were given several dietary habits questionnaires to complete. They were also told that the foods will be discarded after the session, so they were free to continue eating. When participants indicated that they were finished, they were asked to identify their favorite food among the six items available and told that it would be used in the food reinforcement test session.
Food reinforcement task
The food reinforcement task was implemented as a computer game with two stations. Participants responded by pressing a mouse button, and earned a point each time they met the schedule requirement (i.e. 4, 8, 16, 32, 64 responses and etc.). The reinforcing value of food (food reinforcement) and non-food alternatives were assessed by measuring the total number of responses participants made for each type of reinforcer on concurrent, progressive fixed-ratio schedules of reinforcement. At one station, participants received a 70–101 kcal portion of their favorite high-energy-dense snack food for every five points earned. At the other station, participants received 2 minutes of time to spend toward alternative activities (reading Time/Newsweek magazines or completing crossword puzzles/word searches) for every five points earned. The non-food alternatives were provided to reduce the likelihood that participants responded for food due to constrained choice, and were intended to be activities that: 1) are not novel to the participants, 2) are not so highly salient such that people do not respond for food in a concurrent choice scenario, 3) do not directly influence energy balance (e.g. physical activity) and 4) are not frequently associated with eating (e.g. television-watching). Participants were instructed to perform one activity at a time (i.e. play the computer game, eat or work on the alternative activities), and were told that the session would end whenever they no longer wished to earn points for food or for time to spend toward the alternative activities. Water was available ad libitum, and participants were given unlimited time to complete each response schedule. The test-retest reliability of the food reinforcement task has been previously demonstrated (5).
Body Mass Index
The participant’s weight and height were measured using a digital scale (TANITA Corporation of America Inc, Arlington Heights, IL) and a digital stadiometer (Measurement Concepts & Quick Medical, North Bend, WA). Body mass index (BMI) was then calculated according to the following formula: BMI = kg/m2.
Demographics
Information about annual household income in USD (available categories: ≤$9,999; $10,000 – $29,999; $30,000 – $49,999; $50,000 – $69,999; $70,000 – $89,999; $90,000 – $109,999; $110,000 – $139,999; $140,000 – $179,999 and $180,000 – $199,999, ≥$200,000), highest education level completed (available categories: Less than seventh grade; Junior high/9th grade; Some high school/10th or 11th grade; High School; Some college or vocational training; Completed a 2-year college degree; Completed a 4-year college degree; Completed graduate degree) and minority status (Caucasian/non-Caucasian) was collected using a standardized questionnaire.
Analytic Plan
The goals of the analyses were to assess whether income or education level was related to BMI and whether food reinforcement mediated these relationships. Category midpoints were used to create a continuous measure of income. Education level was coded as a five-category ordinal variable (high school or less; some college or vocational training; completed 2-year college degree; completed 4-year college degree; completed graduate degree). Mediation models were tested using multivariate linear regression, controlling for age, sex, minority status, session hunger and the reinforcing value of non-food alternatives as covariates. The relationship between income and BMI was first evaluated. If there were a significant total effect of income on BMI, the size and significance of the indirect effect of income on BMI through food reinforcement was then estimated by the product of the regression coefficients of the predictive variables from the income → food reinforcement and the food reinforcement → BMI paths (23). Confidence intervals were constructed from 10,000 bootstrap resamples of the data (of the same size as the original study population, with replacement) and implemented via a macro developed by Preacher and Hayes (23). We present three ways to interpret the indirect effect of the independent variable (income or education level) on the dependent variable (BMI) through the mediator variable (food reinforcement). First, the indirect effect is significant if the bootstrapped 95% confidence interval does not contain zero. Second, the magnitude of the indirect effect reflects the estimated change in the dependent variable through effects of the mediator variable per a unit change of the independent variable (24). Third, the proportion of the total effect explained by the indirect effect will be quantified by the effect ratio (indirect effect divided by the total effect) (25). An analogous set of analyses was conducted using education level as the proxy for SES. The bivariate relationships among household income, education level, session hunger and the reinforcing value of non-food alternatives were evaluated using Pearson product-moment correlations. Data were analyzed using SYSTAT 11 (Systat Software, 2004) and SAS 9.2 (SAS Institute Inc., 2008).
Results
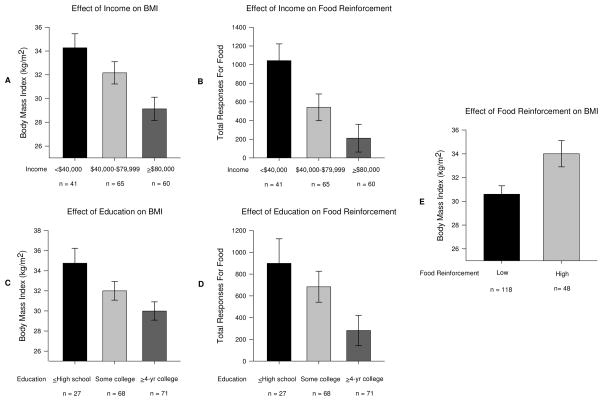
Multivariate linear regression analyses controlling for age, sex, minority status, session hunger and the reinforcing value of non-food alternatives showed that income was related to BMI (b = −0.37, p = 0.019, Figure 1A) and food reinforcement (b = −46.32, p = 0.048, Figure 1B), and that food reinforcement was related to BMI (b = 0.0041, p < 0.001, Figure 1E). Path analyses revealed a significant indirect effect of income on BMI through food reinforcement (estimate = −0.068, 95% CI = −0.23, −0.0017), suggesting that food reinforcement is a partial mediator of the relationship between income and BMI (Table 2). Specifically, BMI is expected to decrease by 0.068 units for every $10,000 increase in annual household income, if only the indirect effect through food reinforcement were considered. Based on the effect ratio, food reinforcement explained 19% of the association between income and BMI.
Figure 1.
Relationships among household income, highest education level completed, food reinforcement and BMI. Multivariate linear regression analyses controlling for the effects of age, sex, minority status, session hunger and the reinforcing value of non-food alternatives revealed that income predicted BMI (b = −0.37, p = 0.019, Figure 1A) and food reinforcement (b = −46.32, p = 0.048, Figure 1B), education level predicted BMI(b = −0.94, p = 0.041, Figure 1C) and food reinforcement (b = −137.07, p = 0.049, Figure 1D), as well as that food reinforcement predicted BMI (b = 0.0016, p = 0.0017, Figure 1E). To graph the relationships, income and education level were categorized by tertiles while food reinforcement was dichotomized by a median split. Group differences were then assessed using one-way analysis of variance.
Table 2.
Summary of simple mediation models assessing the indirect effect of food reinforcement on the relationship between socioeconomic status and BMI.
| SES Proxy | Effect of SES on BMI (Total Effect)a | Effect of SES on FR (Path A)a | Effect of FR on BMI (Path B)a | SES on BMI through FR (Indirect Effect)b | Bca 95% CIc
|
Effect Ratiod | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Income | −0.37 | −46.32 | 0.0015 | −0.068 | −0.23 | −0.0017 | 0.19 |
| Education | −0.94 | −137.07 | 0.0015 | −0.097 | −0.35 | −0.0052 | 0.10 |
Standardized regression coefficients.
The magnitude of the indirect effect is estimated by the product of the regression coefficients of the predictive variables from Path A and Path B.
BCa = bias-corrected and accelerated 95% confidence intervals obtained from 10,000 bootstrap resamples. Confidence intervals not containing zero suggest that the indirect effect is significant at the 0.95 level.
Effect ratio = indirect effect/total effect. The effect ratio quantifies the proportion of the total effect explained by the indirect effect.
Education level was also related to BMI (b = −0.94, p = 0.041, Figure 1C) and food reinforcement (b = −137.07, p = 0.049, Figure 1D). Path analyses revealed a significant indirect effect of education level on BMI through food reinforcement (estimate = −0.21, 95% CI = −0.71, −0.010), such that BMI is expected to decrease by −0.097 units per year increase in education level, if only the indirect effect through food reinforcement were considered (Table 2). Based on the effect ratio, food reinforcement explained 10% of the association between education level and BMI.
Income was related to education level (r = 0.41, p < 0.001). Neither income nor education level was related to session hunger or the reinforcing value of non-food alternatives. Session hunger was not related to the reinforcing value of non-food alternatives.
Discussion
We have shown for the first time that SES, as defined by income or educational attainment, is inversely related to food reinforcement, and that elevated food reinforcement partially mediates the association between lower SES and greater BMI. These results provide a novel theoretical approach for understanding the relationship between low SES and obesity. Low SES persons with limited financial resources may experience greater food reinforcement due to food insecurity (7–9) and lack of non-food reinforcers (11). Reduced access to low-energy-dense foods (17) then predisposes them to binge on high-energy-dense foods whenever they have the means, further enhancing food reinforcement (19). Since low SES individuals have tight budget constraints, bingeing now exacerbates food insecurity later, perpetuating a feast-famine cycle associated with greater liking of high-energy-dense foods, increased adiposity, decreased lean muscle mass and poor glycemic control.(26) In our sample, participants with the lowest household income were expected to be 1.05 BMI units heavier than participants with the highest household income, while the lowest-educated participants were expected to be 0.92 BMI units heavier than the highest-educated participants, if only the indirect effects of these factors on BMI through food reinforcement were considered. These differences would be equivalent to a 3.7–4.2% change in an individual with a BMI of 25. Given that moderate weight loss (5–10% of current body weight) has been shown to improve metabolic indicators and to reduce the risk of cardiovascular events in overweight individuals (27), attenuating the effect of SES on food reinforcement could have clinically significant implications.
Food reinforcement may explain why current nutritional assistance programs have not improved dietary quality and may actually have increased obesity risk among low SES populations (28). Behavioral choice theory conceptualizes that food choice depends on the absolute reinforcing value of the food (i.e. the sensory and psychological properties of the food that motivate people to eat) and the accessibility of other foods (3). Nutritional assistance benefits improve access to healthier low-energy-dense options, but people tend to find high-energy-dense foods more reinforcing (29), and chronic deprivation characterized by food insecurity may enhance this preference (8). Food subsidies have been shown to increase purchasing of both high-energy-dense and low-energy-dense foods in laboratory studies (30). Thus, interventions that simultaneously make high-energy-dense foods less accessible and low-energy-dense foods more accessible, such as a combination of taxes and subsidies (30) may be necessary to promote healthier food choices. In addition, since food reinforcement is influenced by the availability of non-food reinforcers, and a considerable proportion high of-energy-dense snack foods are consumed during sedentary activities (12), another promising approach could involve reducing access to sedentary behaviors while increasing access to physical activity (31). Strategies that lower the energy content of foods without influencing their palatability or enhance the sensory characteristics of low-energy-dense foods may complement these efforts (32). Furthermore, though we are unaware of any systematic research that has successfully modified the absolute reinforcing value of food in humans, we speculate that methods of reducing drug craving – such as extinguishing cue-reinforcer memories (33) – may be adapted to lower food reinforcement in obese individuals.
Our study had several limitations. First, information on family size and sources of income was not collected. However, failing to adjust household income for family size and/or receipt of nutrition assistance should only bias associations toward the null; participants would appear to have greater disposable income than they otherwise would. Second, the sample was not recruited to balance the percentage of participants from each educational level, and did not include people from the lowest education levels (all participants graduated from secondary school and 42.7% of participants completed 4-year college). The restricted variance in education level may have led to underestimation of the relationships among education level, food reinforcement and BMI. Third, food reinforcement was not assessed in the context of a wide variety of non-food alternatives. People find different activities reinforcing, and the non-food alternatives provided in this study (reading Time/Newsweek magazines or completing crossword puzzles/word searches) may not reliably substitute for eating in some persons. In the current study, participants worked harder for non-food alternatives than for food, suggesting that these activities were salient reinforcers. Moreover, the choice of non-food reinforcers was unlikely to have influenced the pattern of results observed, as the reinforcing value of reading was not related to household income or education level and was entered as a covariate in all analyses. However, providing a variety of non-food reinforcers (e.g. access to social media, music, videos and entertainment magazines) may improve the external validity of the food reinforcement measure and should be considered in subsequent studies. Fourth, other constructs related to eating, such as hedonic hunger (34), were not examined. It would be interesting to determine whether other eating behavior phenotypes may also mediate the relationship between SES and BMI. Lastly, while we hypothesized that low SES individuals have restricted access to healthier foods and non-food reinforcers, we did not directly evaluate access to chained supermarkets and physical activity resources. Further inquiry into whether the built environment influences food reinforcement is warranted.
In summary, we argue that the ecological and economic circumstances experienced by low SES individuals – including restricted access to low-energy-dense foods, lack of alternatives to eating, and chronic deprivation – augments food reinforcement while promoting unhealthy food choices. Greater food reinforcement then leads to positive energy balance and weight gain. Future research should verify the proposed pathway and identify other factors related to low SES that may interact with food reinforcement to increase obesity risk. Implementing interventions that target food reinforcement or its moderators to promote healthy eating behavior in an obesogenic low SES environment would be a true innovation in weight control and health disparities research.
Acknowledgments
This research was funded in part by a grant from the National Institute of Drug Abuse, R01DA024883 awarded to Dr. Epstein. The funding agency was not involved in analysis or interpretation of the data.
This trial was registered at clinicaltrials.gov as NCT00962117. Appreciation is expressed to Lora G. Roba, Vida Rostami, Lauren Angelucci, Nicole Gens and Caitlin Hart for data collection and data entry and assisting in the implementation of protocol. This research was funded in part by a grant from the National Institute of Drug Abuse, R01DA024883 awarded to Dr. Epstein.
Footnotes
Disclosure
The authors declare no conflict of interest.
References
- 1.Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic disparities in health in the United States: what the patterns tell us. American Journal of Public Health. 2010;100 (Suppl 1):S186–96. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schoenborn CA, Adams PF, Barnes PM. Body weight status of adults: United States, 1997–98. Advance Data. 2002:1–15. [PubMed] [Google Scholar]
- 3.Epstein LH, Leddy JJ, Temple JL, Faith MS. Food reinforcement and eating: a multilevel analysis. Psychological Bulletin. 2007;133:884–906. doi: 10.1037/0033-2909.133.5.884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Epstein LH, Carr KA, Lin H, Fletcher KD. Food reinforcement, energy intake, and macronutrient choice. American Journal of Clinical Nutrition. 2011;94:12–8. doi: 10.3945/ajcn.110.010314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Epstein LH, Temple JL, Neaderhiser BJ, Salis RJ, Erbe RW, Leddy JJ. Food reinforcement, the dopamine D2 receptor genotype, and energy intake in obese and nonobese humans. Behavioral Neuroscience. 2007;121:877–86. doi: 10.1037/0735-7044.121.5.877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Townsend MS, Peerson J, Love B, Achterberg C, Murphy SP. Food insecurity is positively related to overweight in women. Journal of Nutrition. 2001;131:1738–45. doi: 10.1093/jn/131.6.1738. [DOI] [PubMed] [Google Scholar]
- 7.Lowe MR, Butryn ML. Hedonic hunger: a new dimension of appetite? Physiology & Behavior. 2007;91:432–9. doi: 10.1016/j.physbeh.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 8.Raynor HA, Epstein LH. The relative-reinforcing value of food under differing levels of food deprivation and restriction. Appetite. 2003;40:15–24. doi: 10.1016/s0195-6663(02)00161-7. [DOI] [PubMed] [Google Scholar]
- 9.Carr KD. Feeding, drug abuse, and the sensitization of reward by metabolic need. Neurochemical Research. 1996;21:1455–67. doi: 10.1007/BF02532386. [DOI] [PubMed] [Google Scholar]
- 10.Olson CM, Bove CF, Miller EO. Growing up poor: Long-term implications for eating patterns and body weight. Appetite. 2007;49:198–207. doi: 10.1016/j.appet.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 11.Estabrooks PA, Lee RE, Gyurcsik NC. Resources for physical activity participation: Does availability and accessibility differ by neighborhood socioeconomic status? Annals of Behavioral Medicine. 2003;25:100–4. doi: 10.1207/S15324796ABM2502_05. [DOI] [PubMed] [Google Scholar]
- 12.Chaput JP, Klingenberg L, Astrup A, Sjodin AM. Modern sedentary activities promote overconsumption of food in our current obesogenic environment. Obesity Reviews. 2011;12:e12–20. doi: 10.1111/j.1467-789X.2010.00772.x. [DOI] [PubMed] [Google Scholar]
- 13.Lioret S, Maire B, Volatier JL, Charles MA. Child overweight in France and its relationship with physical activity, sedentary behaviour and socioeconomic status. European Journal of Clinical Nutrition. 2007;61:509–16. doi: 10.1038/sj.ejcn.1602538. [DOI] [PubMed] [Google Scholar]
- 14.Field M, Santarcangelo M, Sumnall H, Goudie A, Cole J. Delay discounting and the behavioural economics of cigarette purchases in smokers: the effects of nicotine deprivation. Psychopharmacology. 2006;186:255–63. doi: 10.1007/s00213-006-0385-4. [DOI] [PubMed] [Google Scholar]
- 15.Baker EA, Schootman M, Barnidge E, Kelly C. The role of race and poverty in access to foods that enable individuals to adhere to dietary guidelines. Preventing Chronic Disease. 2006;3:A76. [PMC free article] [PubMed] [Google Scholar]
- 16.Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. American Journal of Clinical Nutrition. 2005;82:265S–73S. doi: 10.1093/ajcn/82.1.265S. [DOI] [PubMed] [Google Scholar]
- 17.Morland KB, Evenson KR. Obesity prevalence and the local food environment. Health & Place. 2009;15:491–5. doi: 10.1016/j.healthplace.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Giskes K, Avendano M, Brug J, Kunst AE. A systematic review of studies on socioeconomic inequalities in dietary intakes associated with weight gain and overweight/obesity conducted among European adults. Obesity Reviews. 2010;11:413–29. doi: 10.1111/j.1467-789X.2009.00658.x. [DOI] [PubMed] [Google Scholar]
- 19.Clark EN, Dewey AM, Temple JL. Effects of daily snack food intake on food reinforcement depend on body mass index and energy density. American Journal of Clinical Nutrition. 2010;91:300–8. doi: 10.3945/ajcn.2009.28632. [DOI] [PubMed] [Google Scholar]
- 20.Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research - One size does not fit all. J Am Med Assoc. 2005;294:2879–88. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 21.Poulton R, Caspi A, Milne BJ, et al. Association between children’s experience of socioeconomic disadvantage and adult health: a life-course study. Lancet. 2002;360:1640–5. doi: 10.1016/S0140-6736(02)11602-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reiss S, Havercamp S. The sensitivity theory of motivation: implications for psychopathology. Behaviour Research and Therapy. 1996;34:621–32. doi: 10.1016/0005-7967(96)00041-1. [DOI] [PubMed] [Google Scholar]
- 23.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36:717–31. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 24.Preacher KJ, Kelley K. Effect size measures for mediation models: quantitative strategies for communicating indirect effects. Psychological Methods. 2011;16:93–115. doi: 10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- 25.Ezzati M, Vander Hoorn S, Lawes CMM, et al. Rethinking the “diseases of affluence” paradigm: Global patterns of nutritional risks in relation to economic development. Plos Med. 2005;2:404–12. doi: 10.1371/journal.pmed.0020133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dinour LM, Bergen D, Yeh MC. The food insecurity-obesity paradox: A review of the literature and the role food stamps may play. Journal of the American Dietetic Association. 2007;107:1952–61. doi: 10.1016/j.jada.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 27.VanGaal LF, Wauters MA, DeLeeuw IH. The beneficial effects of modest weight loss on cardiovascular risk factors. International Journal of Obesity. 1997;21:S5–S9. [PubMed] [Google Scholar]
- 28.Leung CW, Willett WC, Ding EL. Low-income Supplemental Nutrition Assistance Program participation is related to adiposity and metabolic risk factors. American Journal of Clinical Nutrition. 2012;95:17–24. doi: 10.3945/ajcn.111.012294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Giesen JC, Havermans RC, Douven A, Tekelenburg M, Jansen A. Will work for snack food: the association of BMI and snack reinforcement. Obesity. 2010;18:966–70. doi: 10.1038/oby.2010.20. [DOI] [PubMed] [Google Scholar]
- 30.Epstein LH, Dearing KK, Roba LG, Finkelstein E. The Influence of Taxes and Subsidies on Energy Purchased in an Experimental Purchasing Study. Psychological Science. 2010;21:406–14. doi: 10.1177/0956797610361446. [DOI] [PubMed] [Google Scholar]
- 31.Epstein LH, Paluch RA, Gordy CC, Dorn J. Decreasing sedentary behaviors in treating pediatric obesity. Arch Pediat Adol Med. 2000;154:220–6. doi: 10.1001/archpedi.154.3.220. [DOI] [PubMed] [Google Scholar]
- 32.Blatt AD, Roe LS, Rolls BJ. Hidden vegetables: an effective strategy to reduce energy intake and increase vegetable intake in adults. American Journal of Clinical Nutrition. 2011;93:756–63. doi: 10.3945/ajcn.110.009332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Epstein LH, Truesdale R, Wojcik A, Paluch RA, Raynor HA. Effects of deprivation on hedonics and reinforcing value of food. Physiology & Behavior. 2003;78:221–7. doi: 10.1016/s0031-9384(02)00978-2. [DOI] [PubMed] [Google Scholar]
- 34.Lowe MR, Butryn ML, Didie ER, et al. The Power of Food Scale. A new measure of the psychological influence of the food environment. Appetite. 2009;53:114–8. doi: 10.1016/j.appet.2009.05.016. [DOI] [PubMed] [Google Scholar]