Abstract
OBJECTIVE
Our aim was to compare good candidates for trial of labor after cesarean (TOLAC) who underwent repeat cesarean to those who chose TOLAC.
STUDY DESIGN
Data for all deliveries at 14 regional hospitals over an 8-year period were reviewed. Women with a primary cesarean and 1 subsequent delivery in the dataset were included. The choice of elective repeat cesarean vs TOLAC was assessed in the first delivery following the primary cesarean. Women with ≥70% chance of successful vaginal birth after cesarean as calculated by a published nomogram were considered good candidates for TOLAC. Good candidates who chose an elective repeat cesarean were compared to those who chose TOLAC. Women who were delivered at 2 preselected tertiary centers by a general obstetrician-gynecologist practice were subanalyzed to determine whether there was an effect of physician group.
RESULTS
In all, 5445 women had a primary cesarean and a subsequent delivery. A total of 3120 women were calculated to be good TOLAC candidates. Of this group, 925 (29.7%) chose TOLAC. Women managed by a family practitioner or who were obese were less likely to choose TOLAC while women who were managed by a midwife or had a prior vaginal delivery were more likely to choose TOLAC. At the 2 tertiary centers, 1 general obstetrician-gynecologist group had significantly more patients who chose TOLAC compared to the other obstetrician-gynecologist physician groups (P < .001), with 63% of their patients choosing TOLAC.
CONCLUSION
Less than one-third of the good candidates for TOLAC chose TOLAC. Managing provider influences this decision.
Keywords: cesarean, patient characteristics, trial of labor after cesarean section, vaginal birth after cesarean
Over the past 20 years, the rate of vaginal birth after cesarean (VBAC) has continued to decline. The rate of attempted VBAC in the United States decreased from approximately 28% in 1996 to 8% in 2006.1,2 The most recent Practice Bulletin from the American College of Obstetricians and Gynecologists on VBAC recommends that trial of labor after cesarean (TOLAC) be offered to most women with a history of 1 prior low transverse cesarean delivery.3 However, there are barriers to offering and acceptance of TOLAC including patient preference, a lack of facilities that offer TOLAC, and unwillingness of physicians to offer TOLAC due to concerns regarding liability.3
Women who have a successful VBAC are less likely to suffer morbidity than women undergoing an elective repeat cesarean. However, women undergoing elective repeat cesarean have lower morbidity rates than those undergoing an intrapartum repeat cesarean for failed TOLAC. Prediction models have therefore been developed to identify women who are good candidates for TOLAC based on demographic characteristics that have been associated with successful VBAC.4-12 These models are intended for physician use in counseling women with a history of cesarean regarding their likelihood of successful VBAC. However, the characteristics of women who are calculated to be good candidates for TOLAC but ultimately undergo elective repeat cesarean have not been investigated. We sought to determine if there are certain demographic characteristics, or individual physicians, associated with an increased likelihood of a patient choosing to have an elective repeat cesarean among women who have ≥70% chance of successful VBAC.
MATERIALS AND METHODS
This was a retrospective cohort study of all women delivering a singleton pregnancy at 14 Intermountain Healthcare hospitals from July 2000 through July 2008. Patients who had a primary cesarean delivery and their subsequent delivery in one of our facilities were included. Only the delivery immediately following the primary cesarean was used for analysis. Women with an anomalous fetus or stillbirth were excluded. Women who underwent a tubal ligation at the time of their repeat cesarean were also excluded from the analysis as their desire for permanent sterilization likely greatly influenced their mode of delivery.
The nomogram published by Grobman et al4 for use at the first prenatal visit to predict the likelihood of successful VBAC was then utilized to select women who would have been considered good candidates for TOLAC. Women who were calculated to have a likelihood of successful VBAC ≥70% were included in the final study population. This cutoff was thought to be a clinically useful level at which patients would have a high likelihood of success and was selected a priori.
Resident physicians assisted with the cesareans and were involved with labor management at 2 of the sites, but did not provide counseling regarding the mode of delivery. The study size was dictated by the available cohort for the years of collected data. This study was approved by the Intermountain Healthcare Institutional Review Board.
Women who were good candidates for TOLAC who had an elective repeat cesarean were compared to women electing TOLAC. Those with a failed TOLAC were considered in the same group as women with a successful VBAC for the purposes of this analysis. TOLAC patients were identified as such by having a patient TOLAC request documented by the labor and delivery nurse at admission, the use of oxytocin, intrauterine pressure catheter placement, vaginal delivery, arrest of dilation or descent as the indication for a second cesarean, or a billing code for failed TOLAC. All other women were classified as an elective repeat cesarean. To evaluate whether women were classified appropriately (TOLAC or elective repeat cesarean), 10% of the charts were chosen randomly and assessed by manual chart review.
Demographic and obstetric data were abstracted from the participants’ electronic medical records. Recorded demographic variables included maternal age, parity, self-reported race, marital status, prepregnancy body mass index, history of vaginal birth, indication for primary cesarean, and insurance status.
Women who chose an elective repeat cesarean were compared to those who chose TOLAC. Given that patients were nested, or clustered, within hospital, for univariate comparisons of the 2 groups, a mixed-effects logistic regression was used for binary categorical variables, and a mixed-effects multinomial regression was used for unordered categorical variables with ≥3 categories. This mixed-effects approach was utilized to account for the potential lack of independence between study subjects delivered at the same hospital. Variables that have previously been identified to be predictive of successful VBAC were candidates for inclusion in the multivariable model.4-12 These included: provider type (family practice, maternal-fetal medicine, general obstetrician-gynecologist, or certified nurse midwife), self-reported race, payer status (Medicaid, private insurance, or uninsured), marital status, maternal age >35 years, recurrent indication for primary cesarean (defined as arrest of dilation or descent), history of a vaginal delivery, and obesity. Obesity was defined according to the Institute of Medicine guidelines as a body mass index ≥30.13
Using interactive backwards elimination variable selection, a mixed-effects multivariable logistic regression model was then used to determine which variables were independently associated with a decision to have an elective repeat cesarean. In the mixed-effects model, patients were nested within facility. Variables included in the initial model, before backwards variable selection, were the variables found to be different between groups in univariate analysis with a P < .20.
Women who were delivered at 2 preselected tertiary centers by a general obstetrician-gynecologist practice were subanalyzed to determine whether there was an effect of physician group. These hospitals were selected because they have a close geographic proximity and presumably draw from a similar patient population. Of note, these data regarding managing provider were only available for the last 3 years of the dataset (from August 2005 through July 2008). Women with missing data for delivering provider (ie, delivered prior to August 2005) were excluded from this portion of the analysis. If a general obstetrician-gynecologist practice delivered <5 women in the allotted time period, they were excluded from the analysis. All patients delivered by a perinatologist, certified nurse midwife, or family practitioner were also excluded from this portion of the analysis. A comparison was made between each general obstetrician-gynecologist practice and the remainder of the groups as a set using a χ2 test. A mixed-effects approach was not needed for this analysis, as the providers were from different hospitals and so the hospital effect was essentially modeled by the provider variable in the χ2 analysis. The reported P values were then adjusted for multiple comparisons using the Hochberg procedure.14,15
A 2-sided P value < .05 was defined as statistically significant. The statistical software package STATA 11.0 (StataCorp, College Station, TX) was used for all analyses.
RESULTS
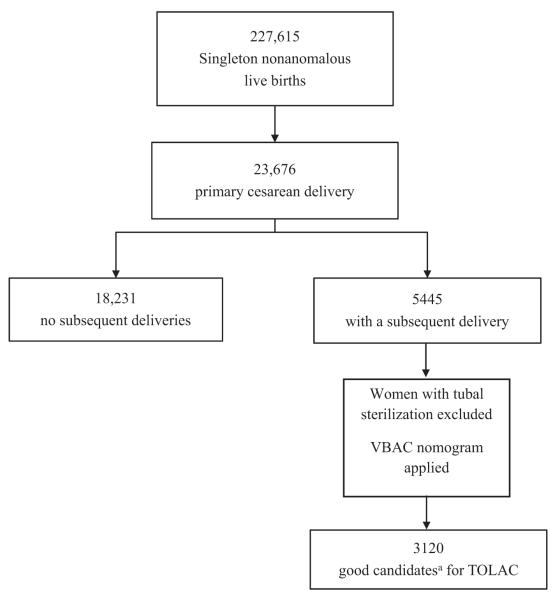
There were 227,615 singleton nonanomalous live births over the 8-year study period (Figure). A total of 5445 women had a primary cesarean and a subsequent delivery. Of these, 503 women had a bilateral tubal ligation at the time of cesarean and were excluded. The remaining 4942 women met inclusion criteria. Of these women, 3120 (63.1%) were calculated to be good TOLAC candidates (≥70% likelihood of success based on VBAC nomogram by Grobman et al4) in their delivery immediately following their primary cesarean. Of note, there were no women who underwent a tubal ligation following successful VBAC. The final study group comprised 2195 (70.4%) women who underwent elective repeat cesarean and 925 (29.7%) who chose TOLAC. The rate of successful VBAC among the women choosing TOLAC was 85%. Upon manual chart review, women were classified accurately as TOLAC or elective repeat cesarean 98.7% of the time.
FIGURE. Study population.
TOLAC, trial of labor after cesarean; VBAC, vaginal birth after cesarean.
aWomen were considered good candidates for TOLAC if their calculated likelihood of successful VBAC was ≥70% based on the prediction model by Grobman et al.4
The demographics of the study population and univariate comparisons between groups are detailed in Table 1. Factors found with univariate analysis to be different between groups were payer status, advanced maternal age, history of vaginal delivery, body mass index, and managing provider. These variables were included in a mixed-effects logistic regression analysis with patients nested in facility, to determine which factors were independently associated with choosing TOLAC.
TABLE 1.
Characteristics of women who are good candidates for trial of labor after cesarean
| Demographic variable | Chose elective repeat cesarean (n = 2195) |
Chose trial of labor after cesarean (n = 925) |
P value |
|---|---|---|---|
| Race, n (%) | .59 | ||
| Caucasian | 2077 (94.6) | 869 (93.9) | |
| Hispanic | 56 (2.6.2) | 24 (2.6) | |
| African American | 4 (0.2) | 3 (0.3) | |
| Other | 58 (2.6) | 29 (3.1) | |
| Payer status, n (%) | .04 | ||
| Private | 1705 (77.7) | 720 (77.8) | |
| Medicaid/Medicare | 456 (20.8) | 180 (19.4) | |
| Uninsured | 34 (1.5) | 26 (2.8) | |
| Maternal age >35 y, n (%) | 107 (4.9) | 65 (7.0) | .01 |
| Marital status, n (%) | |||
| Married | 2015 (91.8) | 868 (93.8) | .13 |
| Primary cesarean for recurring indication, n (%) |
85 (3.9) | 26 (2.8) | .21 |
| History of vaginal delivery, n (%) | 418 (19.0) | 352 (38.1) | <.001 |
| Obese, body mass index >30, n (%) |
243 (11.1) | 73 (7.9) | .007 |
| Delivery at tertiary hospital, n (%) | 992 (45.2) | 387 (41.8) | .83 |
| Managing provider, n (%) | <.001 | ||
| General obstetriciang- ynecologist |
1167 (53.2) | 438 (47.4) | |
| MFM | 30 (1.4) | 8 (0.9) | |
| Certified nurse midwife | 19 (0.9) | 30 (3.2) | |
| Family practice | 109 (5.0) | 35 (3.8) | |
| Unknowna | 870 (39.6) | 414 (44.8) |
MFM, maternal-fetal medicine.
Data on managing provider were not available until 2005.
In a mixed logistic regression, with facility included as a random effect, the facility explained a significant amount of variability in the outcome (intraclass correlation coefficient, 0.05; 95% confidence interval, 0.02–0.12; P < .001), indicating that the decisions about repeat cesarean vs TOLAC within the same facility were more alike than between facilities. All regression models accounted for this lack of independence of study participants delivered at the same hospital.
Women who were managed by a certified nurse midwife or had a history of vaginal delivery were more likely to choose TOLAC (Table 2). Women who were managed by a family practitioner or were obese were less likely to choose TOLAC (Table 2).
TABLE 2.
Mixed-effects logistic regression model for choosing trial of labor after cesarean
| Variable | OR for choosing TOLAC (95% CI) |
|---|---|
| Managed by certified nurse midwife |
5.02 (2.69–9.38) |
| Managed by family practitioner |
0.58 (0.38–0.87) |
| History of vaginal delivery |
2.99 (2.49–3.59) |
| Obese | 0.46 (0.34–0.62) |
Mixed-effects logistic regression accounting for facility where participant was delivered.
CI, confidence interval; OR, odds ratio; TOLAC, trial of labor after cesarean.
There were 10 different general obstetrician-gynecologist practices that performed deliveries at 2 tertiary centers over a predefined 3-year period. Only 1 of these practice groups differed from the rest of the groups combined with regard to TOLAC rate with only 36.7% of their good candidates for TOLAC undergoing an elective repeat cesarean (adjusted P < .001) (Table 3).
TABLE 3.
Comparison of women by general obstetrician-gynecologist practice
| Physician group | Elective repeat cesarean, n (%) |
TOLAC, n (%) | Unadjusted P value |
Adjusted P value |
|---|---|---|---|---|
| 1 | 34 (70.8) | 14 (29.2) | .642 | .958 |
| 2 | 19 (76.0) | 6 (24.0) | .370 | .958 |
| 3 | 18 (36.7) | 31 (63.3) | < .001 | < .001 |
| 4 | 6 (85.7) | 1 (14.3) | .308 | .958 |
| 5 | 27 (67.5) | 13 (32.5) | .958 | .958 |
| 6 | 12 (63.2) | 7 (36.8) | .653 | .958 |
| 7 | 9 (75.0) | 3 (25.0) | .592 | .958 |
| 8 | 9 (100.0) | 0 (0.0) | .037 | .296 |
| 9 | 16 (69.6) | 7 (30.4) | .858 | .958 |
| 10 | 7 (100.0) | 0 (0.0) | .067 | .469 |
Reported P values represent comparison of that particular physician group to all other groups combined. P values were adjusted for multiplicity using Hochberg procedure.
TOLAC, trial of labor after cesarean.
COMMENT
Our data demonstrate that women who are good candidates for TOLAC but undergo an elective repeat cesarean differ from those who choose TOLAC. Demographic characteristics, prior patient experience, and physician counseling all play a role in whether patients choose TOLAC.
In our study population, only 30% of women who were good candidates for TOLAC chose to undertake a trial of labor. Despite the low percentage of women choosing TOLAC, our rate still exceeds the national rates of TOLAC. In 2000, the rate of VBAC attempt (per 100 women with 1 prior cesarean) was 20.6%, and declined subsequently to a rate of 7.6% in 2006.2
In our cohort, women who were obese were more likely to undergo repeat cesarean. We speculate that obesity influences physician counseling of patients regarding TOLAC. Physicians may perceive that an intrapartum urgent cesarean would be more difficult in obese women, with an increased risk of intraoperative injury and perinatal morbidity. They may counsel these women to have a repeat cesarean delivery knowing that they are more likely to have a dysfunctional labor16 and have a decreased chance of successful VBAC.4 Given the retrospective nature of the study design,we can only speculate regarding the counseling that was given to individual patients.
As expected, women with a history of vaginal birth and women who were cared for by a certified nurse midwife were more likely to choose TOLAC. This is likely a self-selected population with a strong desire for vaginal birth, and with lower rates of confounding maternal and fetal complications. However, all women in our cohort who were cared for by certified nurse midwives delivered in a hospital with physician backup. These data also suggest that comanagement of women undergoing TOLAC between a midwife and physician may increase the chances of a vaginal delivery, compared to having care by an obstetrician-gynecologist alone.
To better understand the role of individual physicians in the decision to proceed with TOLAC, we subanalyzed the general obstetrician-gynecologist groups delivering at 2 tertiary centers in our database. This information was not available in the electronic medical record until 2005. These centers were chosen for their proximity of geographic location and similarity of patient population. Both facilities have adequate resources and personnel to support TOLAC (inhouse anesthesia and an in-house obstetrician at all times). Within this subset of 10 practices, there was only 1 general obstetrician-gynecologist group with <60% of their patients opting for an elective repeat cesarean. This group differed substantially from the other physician groups, as only 37% of their patients with a prior cesarean chose an elective repeat cesarean. This difference between groups indicates that physician counseling/preference likely plays a strong role in whether a woman opts for TOLAC. We could not evaluate this fully with a retrospective study. This particular practice is unique from the others in that it is comprised entirely of women, all of whom completed residency training in the last 10 years, are employed by the health system, and have an office 1 floor directly above labor and delivery. They offer TOLAC to all patients with a history of 1 prior low transverse cesarean. This counseling is performed by one of the physicians during routine office visits. They do not provide any preprinted handouts. The counseling is simply a discussion between the physician and her patient. These data suggest that a consistent effort within a practice to offer TOLAC has the potential to greatly increase the number of women attempting TOLAC.
One strength of our study is that it includes both community and tertiary centers. Our data are complete with the exception of information regarding the managing provider, which was not available until 2005. All of the analyzed women had both their primary cesarean and subsequent delivery within our system. This eliminates patient recall bias with respect to the indications for their previous surgery and allows us to more accurately calculate the chance of success in the subsequent pregnancy.
It should be noted that our population is relatively homogeneous (largely Caucasian, insured, and not obese), with an overall high likelihood of VBAC success. Although the selection of an inclusion cutoff of ≥70% likelihood of TOLAC success is somewhat arbitrary, it is thought to be a clinically meaningful cut point by the practitioners involved in the design of the study. Importantly, this was chosen a priori.
The largest assumption in this study is that women undergoing an elective repeat cesarean were offered TOLAC and still preferred an elective repeat cesarean. TOLAC can be offered at all of the hospitals included in our database. However, we have no way of knowing whether and how patients were counseled regarding TOLAC. Also, there are likely women in our cohort who planned TOLAC, but had clinical circumstances such as malpresentation or previa that prompted a repeat cesarean.
Our study is limited by its retrospective nature. The determination of women undergoing TOLAC was made by strict logic based on database entry by trained labor and delivery nurses in a standardized electronic medical record. This may have underestimated the women with a failed TOLAC. However, the classification of women into TOLAC vs elective repeat cesarean corresponded 98.7% of the time when a random sampling of medical records was reviewed manually.
Our results raise several questions regarding the decision of a woman with a history of 1 prior cesarean to proceed with repeat cesarean or TOLAC. If all the women who were good candidates for TOLAC who chose an elective repeat cesarean attempted TOLAC instead, we could have reduced the rate of cesarean in our study cohort from 70.4% to 25.5% (assuming a 70% chance of VBAC success).
Using these data, we can only speculate about patient decision-making, which is highly influenced by personal experience and physician counseling. To better understand patients’ considerations in deciding whether to proceed with TOLAC, we plan to survey women prospectively at the time of admission regarding the factors that influenced their decision to proceed with either an elective repeat cesarean or TOLAC. This may help us identify areas of patient concern or physician preference that inhibit good candidates from pursuing TOLAC. These areas could then be targeted to increase the number of women undergoing TOLAC, thereby reducing the rising cesarean rate and the costs and morbidities associated with multiple repeat cesareans.
Acknowledgments
This research was supported by the University of Utah Study Design and Biostatistics Center, with funding in part from National Institutes of Health research grant number 8UL1TR000105 (National Center for Research Resources and the National Center for Advancing Translational Sciences).
Footnotes
The authors report no conflict of interest.
REFERENCES
- 1.Menacker F. Trends in cesarean rates for first births and repeat cesarean rates for low-risk women: United States, 1990-2003. Natl Vital Stat Rep. 2005;54:1–8. [PubMed] [Google Scholar]
- 2.Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2006. Natl Vital Stat Rep. 2009;57:1–102. [PubMed] [Google Scholar]
- 3.American College of Obstetricians and Gynecologists ACOG practice bulletin no. 115: vaginal birth after previous cesarean delivery. Obstet Gynecol. 2010;116:450–63. doi: 10.1097/AOG.0b013e3181eeb251. [DOI] [PubMed] [Google Scholar]
- 4.Grobman WA, Lai Y, Landon MB, et al. Development of a nomogram for prediction of vaginal birth after cesarean delivery. Obstet Gynecol. 2007;109:806–12. doi: 10.1097/01.AOG.0000259312.36053.02. [DOI] [PubMed] [Google Scholar]
- 5.Weinstein D, Benshushan A, Tanos V, et al. Predictive score for vaginal birth after cesarean section. Am J Obstet Gynecol. 1996;174:192–8. doi: 10.1016/s0002-9378(96)70393-9. [DOI] [PubMed] [Google Scholar]
- 6.Pickhardt MG, Martin JN, Jr, Meydrech EF, et al. Vaginal birth after cesarean delivery: are there useful and valid predictors of success or failure? Am J Obstet Gynecol. 1992;166:1811–9. doi: 10.1016/0002-9378(92)91572-r. [DOI] [PubMed] [Google Scholar]
- 7.Flamm BL, Geiger AM. Vaginal birth after cesarean delivery: an admission scoring system. Obstet Gynecol. 1997;90:907–10. doi: 10.1016/s0029-7844(97)00531-0. [DOI] [PubMed] [Google Scholar]
- 8.Gonen R, Tamir A, Degani S, et al. Variables associated with successful vaginal birth after one cesarean section: a proposed vaginal birth after cesarean score. Am J Perinatol. 2004;21:447–53. doi: 10.1055/s-2004-835961. [DOI] [PubMed] [Google Scholar]
- 9.Grobman WA, Lai Y, Landon MB, et al. Does information available at admission for delivery improve prediction of vaginal birth after cesarean? Am J Perinatol. 2009;26:693–701. doi: 10.1055/s-0029-1239494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith GCS, White IR, Pell JP, et al. Predicting cesarean section and uterine rupture among women attempting vaginal birth after prior cesarean section. PLoS Med. 2005;2:871–8. doi: 10.1371/journal.pmed.0020252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Srinivas SK, Stamilio DM, Stevens EJ, et al. Predicting failure of a vaginal birth attempt after cesarean delivery. Obstet Gynecol. 2007;109:800–5. doi: 10.1097/01.AOG.0000259313.46842.71. [DOI] [PubMed] [Google Scholar]
- 12.Hashima JN, Guise JM. Vaginal birth after cesarean: a prenatal scoring tool. Am J Obstet Gynecol. 2007;196:e22–3. doi: 10.1016/j.ajog.2006.10.884. [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine [Accessed Oct. 23, 2011];Resource sheet. Weight gain during pregnancy: reexamining the guidelines. 2009 May; Available at: http://www.iom.edu.
- 14.Sankoh AJ. Hugue MF, Dubey SD. Some comments on frequently used multiple endpoint adjustment methods in clinical trials. Stat Med. 1997;16:2529–42. doi: 10.1002/(sici)1097-0258(19971130)16:22<2529::aid-sim692>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 15.Wright SP. Adjusted P values for simultaneous inference. Biometrics. 1992;48:1005–13. [Google Scholar]
- 16.Nuthulapaty FS, Rouse DJ, Owen J. The association of maternal weight with cesarean risk, labor duration, and cervical dilation rate during labor induction. Obstet Gynecol. 2004;103:452–6. doi: 10.1097/01.AOG.0000102706.84063.C7. [DOI] [PubMed] [Google Scholar]