Abstract
Oral focal mucinosis (OFM) is a rare soft tissue lesion of unknown etiology. Clinically, it is most commonly found on the gingiva and presents as a painless, sessile or pedunculated mass of the same colour as the surrounding mucosa. Histologically, it is characterized by focal myxoid degeneration of connective tissue. OFM occurs predominantly in adults during the fourth and fifth decade of life, although it has been reported infrequently in children and adolescents. Its diagnosis mainly relies on histological analysis and the treatment involves complete surgical excision. Its recurrence is unreported. The aim of this report of two cases is to describe the clinical and histological presentation and subsequent management of OFM. The cause of OFM remains unknown. The cases presented in this report bring OFM to the attention of anatomical pathologists while considering the differential diagnosis of myxoid lesions of the oral cavity.
Keywords: Oral focal mucinosis, Soft tissue lesions, Gingival lesions
Introduction
Oral Focal Mucinosis (OFM) is an oral counterpart of dermal lesion known as coetaneous focal mucinosis (CFM) or cutaneous myxiod cyst which is misdiagnosed as intraoral myxoma(1). OFM is presented as an innocuous swelling that may be pedunculated or sessile. The gingiva was confirmed as the most common site for OFM, with predominance in females. It has an unknown etiology, possibly from overproduction of hyaluronic acid by fibroblasts (2). Clinically, the lesion appears as asymptomatic round elevations, which are histologically characterized by a localized area of myxomatous connective tissue containing mucinous material surrounded by relatively dense collagenous connective tissues(3).
Histopathologically, fibroblast-like cells and foamy cells diffusely increased in a well-localized area of myxoid matrix, surrounded by collagenous fibrous connective tissue. Histochemically, fibroblast-like cells, foamy cells and myxoid matrix were revealed on metachromasia with toluidine blue at pH4.1 and pH 7.0 (3,4 It was first described in 1974 by). Tomich who reported 8 cases as oral counterpart of cutaneous focal mucinosis. He stated that most lesions, if not all, diagnosed as oral soft tissue myxomas are in reality lesion of this entity (5).
These two cases are significant clinically as well as histopathologically. The mucosa directly overlying bone appears to be particularly vulnerable. The lesions generally show no colour change (3, 6). The lesions are difficult to diagnose clinically as there are no clinical distinctive features. They are most commonly diagnosed as fibroma or granuloma. Thus, the histopathological diagnosis becomes important in these conditions (7).
Description of the Cases
Case 1
A 26 years old male patient was reported with a chief complaint of enlargement of gums in in relation to upper anterior teeth, with a history of trauma one year back when he noticed a swelling which grew to the present size. On examination, well-demarcated, reddish, pedunculated, partly smooth and shiny with pebbeled surface, blanching, bleeding, pinpoints, ovoid growth measuring about 15mmx 15mm in its greatest dimension was noted on the left side of the anterior teeth in relation to 22 and 23 extending up to mucogingival junction. An excisional biopsy was performed with scalpel to excise the tissue which was stored in 10% formalin and sent for histopathological examination.
Case 2
A 36-year-old female reported a chief complaint of an asymptomatic enlargement on the gingiva labial to 21. The swelling was initially small which gradually attained the present size. The lesion was approximately 8mm × 7mm in diameter and round in shape, firm, sessile and non-tender to palpation. The overlying mucosal surface was smooth, not ulcerated and showed no colour change. The lesion was extending from distal aspect of 21 medially to mesial aspect of 11. Excisional biopsy was performed with diode laser (320nm).
Histopathological findings
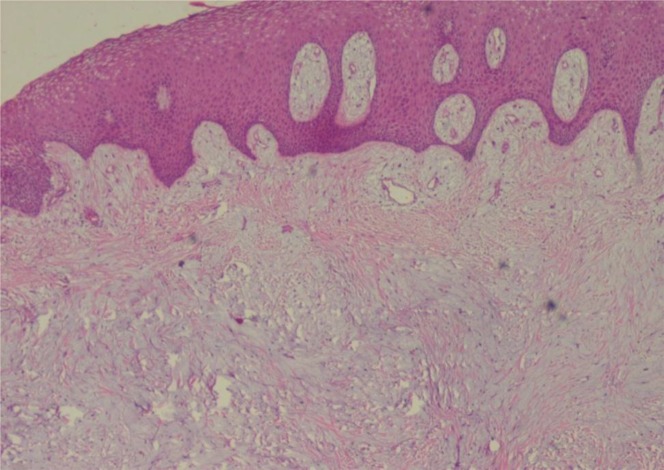
Hematoxylin and eosin stained microscopic slides of both cases revealed a stratified squamous hyper-parakeratinized epithelium and the underlying connective tissue stroma was composed of loose fibro-myxoid stroma with stellate shaped fibroblasts. Deeper stroma showed spindle shaped fibroblasts interspersed between thin collagen fiber bundles and numerous small blood capillaries.
Clinical Course
The patients were observed regularly; both cases healed satisfactorily with no complications or recurrence in last 8 months and 6 months respectively.
Discussion
OFM is a rare clinico-pathologic condition considered to be the microscopic counterpart of the cutaneous focal mucinosis or cutaneous myxoid cyst (1, 5).Three-fourths of all cases occur on the gingiva and the hard palate and presents as a sessile, soft, painless nodule with normal surface coloration, sometimes with a somewhat pale appearance (8).
Oral focal mucinosis consists of a submucosal, well-localized but non-encapsulated nidus of very loose, myxomatous or "mucinous" connective tissue. More superficial lesions may produce atrophy and loss of rete ridges of the overlying squamous epithelium. Fibroblasts are seen in minimal within the mucinous area, often demonstrating delicate, fibrillar processes. The mucinous zone is much less vascular than the surrounding connective tissues, and inflammatory cells are not associated with the lesion except as a perivascular infiltrate of lymphocytic T-cells at the periphery (9).
A slight similarity is also seen between mucinosis and the nerve sheath myxoma, a variant of neurofibroma which rarely affects mucosa of the upper aerodigestive tract. The nerve sheath myxoma is more circumscribed, has fibrous septa between multiple myxoid nodules, and has more plump stromal cells (10).
Oral focal mucinosis is treated by conservative surgical removal. It does not recur with gingival excision.
In the first case, there is well-demarcated, reddish, pedunculated, partly smooth and shiny with peddled surface near 23, ovoid growth measuring about 15mm× 15mm in its greatest dimension. The second case occurred as a sessile gingival mass, measuring about 8mmx 6mm with smooth non ulcerated soft to firm mass.
OFM has no distinctive clinical features and most often thought to be clinically as fibroma, pyogenic granuloma, mucocele or similar lesions. Traumatic fibroma, pyogenic granuloma and minor salivary gland tumor were the differential diagnosis (7). A review of all reported cases show that it was never diagnosed clinically as ‘oral focal mucinosis’ (4, 7).The histological features are always the basis for the diagnosis. Microscopic examination of both cases showed a well-localized but non-encapsulated area of loose, myxomatous connective tissue stroma surrounded by dense, normal thin collagen bundles. The sub-epithelial pale eosinophilic myxoid stromas representing an overproduction of hyaluronic acid with stellate shaped fibroblasts were noted. Deeper stroma showed spindle fibroblasts, thin bundles of collagen fibers and numerous small blood capillaries along with diffuse infiltration of mixed inflammatory cells consisting of mainly lymphocytes and plasma cells. All these features were suggestive of oral focal mucinosis (10).
It must be emphasized that in many focal gingival lesions, clinically preoperative diagnosis is impossible due to their rarity. However, OFM should be considered in the differential diagnosis of soft tissue lesion in adults. The histopathological evaluation is always the basis of diagnosis. Out of 52 cases reported, 33 cases have been noted on the gingiva, 10 cases on the hard palate and 3 cases each on alveolar mucosa, buccal mucosa, and tongue; and 2 cases on lips. Oral focal mucinosis rarely recurs after surgical excision.
Figure 1.

Preoperative view of the lesion
Figure 2.

Surgically excised tissue
Figure 3.
Post operative view of lesion after 8 months
Figure 4.
Preoperative view of lesion wrt 11, 21
Figure 5.
Post operative view of lesion after 6months
Figure 6.
Histopathological picture of lesion
References
- 1.Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillo facial pathology. 2nd ed. Philadelphia, Pennsylvania: Elsevier; 2002. [Google Scholar]
- 2.Buchner A, Merrell PW, Leider AS, Hansen LS. Oral focal mucinosis. Int J Oral Maxillofac Surg. 1990;19:337–340. doi: 10.1016/s0901-5027(05)80076-1. [DOI] [PubMed] [Google Scholar]
- 3.Madhusudhan AS, Nagarajappa D, Manjunatha BS, Saawarn Swati, Charan Babu HS. Oral focal mucinosis: report of two cases. Rev Odonto Cienc. 2010;25:310–313. [Google Scholar]
- 4.Lima AAS, Machado MAN, Martins WD, Grégio AMT, Dirschnabel AJ, 3, Mattioli TMF, et al. Oral focal mucinosis. Quintessence Int. 2008;39:611–615. [PubMed] [Google Scholar]
- 5.Tomich CE. Oral focal mucinosis: A clinic pathologic and histochemical 4. Study of eight cases. Oral Surg. 1974;38:714–724. doi: 10.1016/0030-4220(74)90392-2. [DOI] [PubMed] [Google Scholar]
- 6.Saito I, Ide F, Enomoto T, Kudo I. Oral focal mucinosis. J Oral Maxillofac Surg. 1985;43(5):372–374. doi: 10.1016/0278-2391(85)90259-9. [DOI] [PubMed] [Google Scholar]
- 7.Aldred MJ, Talacko AA, Ruljancich K, Story RD, Newland S, Chen ST, 7, et al. Oral focal mucinosis: report of 15 cases and review of the literature. Pathology. 2003;35:393–396. doi: 10.1080/00313020310001602639. [DOI] [PubMed] [Google Scholar]
- 8.Reed RJ, Clark WH, Mihm MC. The cutaneous mucinosis. Hum Pathol 6. 1973;4:201–207. doi: 10.1016/s0046-8177(73)80007-3. [DOI] [PubMed] [Google Scholar]
- 9.Green TL, Leighty SM, Walters R. Immunohistochemical evaluation of oral myxoid lesions. Oral Surg Oral Med Oral Pathol. 1992;73:469–471. doi: 10.1016/0030-4220(92)90327-m. [DOI] [PubMed] [Google Scholar]
- 10.Wilk M, Schmoeckel C. Cutaneous focal mucinosis: A histopathological and immunohistochemical analysis of 11 cases. J Cutan Pathol. 1994;21:446–452. doi: 10.1111/j.1600-0560.1994.tb00287.x. [DOI] [PubMed] [Google Scholar]