Abstract
Purpose
Osteoarthritic pain is largely considered to be inflammatory pain. Sensory nerve fibers innervating the knee have been shown to be significantly damaged in rat models of knee osteoarthritis (OA) in which the subchondral bone junction is destroyed, and this induces neuropathic pain (NP). Pregabalin was developed as a pain killer for NP; however, there are no reports on pregabalin use in OA patients. The purpose of this study was to investigate the efficacy of pregabalin for pain in OA patients.
Materials and Methods
Eighty-nine knee OA patients were evaluated in this randomized prospective study. Patients were divided into meloxicam, pregabalin, and meloxicam+pregabalin groups. Pain scores were evaluated before and 4 weeks after drug application using a visual analogue scale (VAS), and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). Pain scales among groups were compared using a Kruskal-Wallis test.
Results
Before drug application, there was no significant difference in VAS and WOMAC scores among the three groups (p>0.05). Significant pain relief was seen in the meloxicam+pregabalin group in VAS at 1, 2, and 4 weeks, and WOMAC score at 4 weeks, compared with the other groups (p<0.05). No significant pain relief was seen in the meloxicam only group in VAS during 4 weeks and WOMAC score at 4 weeks compared with the pregabalin only group (p>0.05).
Conclusion
Meloxicam+pregabalin was effective for pain in OA patients. This finding suggests that OA pain is a combination of inflammatory and NP.
Keywords: Pain, osteoarthritis, knee, nerve, pregabalin, inflammatory, neuropathic
INTRODUCTION
Knee osteoarthritis (OA) is a common and progressive joint disease. With an estimated incidence rate of 240 per 100000 person-years, it is a major public health problem in the United States and often results in early retirement and joint replacement.1
Chronic pain can be classified as inflammatory or neuropathic. Inflammatory pain, found in conditions such as rheumatoid arthritis, is the result of sustained stimulation of nociceptors. By contrast, neuropathic pain is the result of damage to or dysfunction of nerves. Principal causes of neuropathic pain (NP) include diabetes, lumbar or cervical radiculopathies, and spinal cord injury.2,3 OA of the knee is generally considered to result in inflammatory pain.
Intra-articular injection of monoiodoacetate into the femorotibial joint space of rodents induces a pathology with temporal similarities to OA, and this model of OA is now used for investigating the pathogenesis of knee pain.4 In the early phase of the rat model pathology, the level of inflammatory neuropeptides in the sensory nerves innervating the knee increases, and this is believed to be a stage of inflammatory pain.5 By contrast, because the subchondral bone is densely innervated, subchondral bone pathology may result in neuropathy after destruction of the chondral structure in late phases of OA. In the late phase of the pathology in the rat model of OA, markers of nerve injury in sensory nerves innervating the knee are significantly increased compared with controls, and this is thought to be a NP stage.6 The origin of the pain would be clarified by assessing whether nerve damage or neuropathy underlies the lack of pharmacological response to celecoxib or diclofenac, but not to morphine as observed later in the temporal sequence of the pathology.7,8 These observations suggest that the pain of knee OA is both inflammatory pain and NP.
Patients with NP are challenging to manage. Available randomized clinical trials typically evaluated chronic NP of moderate to severe intensity. The trials concluded that first-line treatments could include certain antidepressants (i.e., tricyclic antidepressants and dual reuptake inhibitors of both serotonin and norepinephrine), calcium channel α2-δ ligands (i.e., gabapentin and pregabalin), and topical lidocaine.9 Pregabalin was developed for management of NP; however, there have been no reports of the clinical use of pregabalin for OA pain in patients.
Our hypothesis is that there is an inflammatory and a NP component to knee OA pain. Thus, the purpose of current study was to evaluate the efficacy of pregabalin for knee OA pain in patients using a prospective randomized trial.
MATERIALS AND METHODS
The ethics committee of our institution approved the protocol for the human procedures used in this study. In addition, the protocol and publication of the study were approved by our institutional review board and informed consent was obtained from each participant. Participants were selected from outpatients who attended our hospital for knee pain treatment. Eighty-nine patients were selected from 130 knee pain patients who matched the following criteria: presence of knee pain for more than one month, and observation of OA of the knee joint on examination of an anterior-posterior X-ray image. Exclusion criteria were a history of knee surgery, infection, or rheumatoid arthritis. The patients completed a self-administered questionnaire regarding sociodemographic factors (age and sex) and duration of knee symptoms.
Pain scores
All patients completed a visual analogue scale evaluation of pain at movement (VAS: before, 1, 2, and 4 weeks), the Western Ontario and McMaster Universities Osteoarthritis Index questionnaire (WOMAC: before and 4 weeks), and painDETECT screening (before).10,11 The WOMAC questionnaire consists of subsections for pain, stiffness, and physical function. The painDETECT questionnaire is patient-based and consists of seven weighted sensory descriptor items and two items relating to the temporal and spatial (radiating) characteristics of the patient's pain pattern. The painDETECT score ranges from 0 to 38. Patients were divided into three groups: likely (score ≥19), possible (score ≥13 to ≤18), and unlikely (score ≤12) neuropathic pain. VAS was evaluated at 3 time points. VAS at entry point, of severest pain during 4 weeks, and of average pain during 4 weeks were evaluated for all patients.
Radiographic evaluation
An anterior-posterior view X-ray examination was performed in all the patients and the Kellgren-Lawrence (KL) grading system was used. The KL system is a validated method to classify joints into one of five grades, with 0 representing normal and 4 representing the most severe radiographic disease.12 Evaluation was performed by five blinded observers. If three or more of the observers concurred, the score was used to define the KL grade.
Randomization and medication
Eighty-nine knee OA patients were evaluated in the current randomized prospective study. The patients were randomized according to the minimization method for three groups.13 We employed gender and age as stratification factors. Patients were divided into three groups: meloxicam group (10 mg meloxicam 30 minutes after breakfast), pregabalin group (25 mg pregabalin before sleep), and meloxicam+pregabalin group (10 mg meloxicam 30 min after breakfast and 25 mg pregabalin before sleep). Medication was administered every day over 4 weeks. Other drugs and injection into knee were not allowed in any patient.
Adverse events
All adverse events were reported together with an assessment of their severity (mild, moderate, severe) and the investigator's opinion of their relationship to treatment with each drug (none, unlikely, possible, or probable). Antiemetics were not used in any patient.
Statistical analysis
Data were compared using a Kruskal-Wallis test to compare pain scales between the three groups, a one way ANOVA with post hoc comparisons for age, symptom duration, and follow-up, and Fisher's test for dichotomous/categorical variables. p<0.05 was considered statistically significant.
RESULTS
No patients dropped out of the current study. Table 1 shows demographic characteristics for patients. Eighty-nine patients (63 female, 26 male) with a mean age of 70.0±8.0 (mean±SEM) years were admitted into the study. The average duration of symptoms was 35.5±8.0 (mean±SEM) months. The patients suffered from knee pain, originating from OA, for at least one month. Pain using VAS and WOMAC scores was not significantly different among the three groups (p>0.05).
Table 1.
Demographic Characteristics
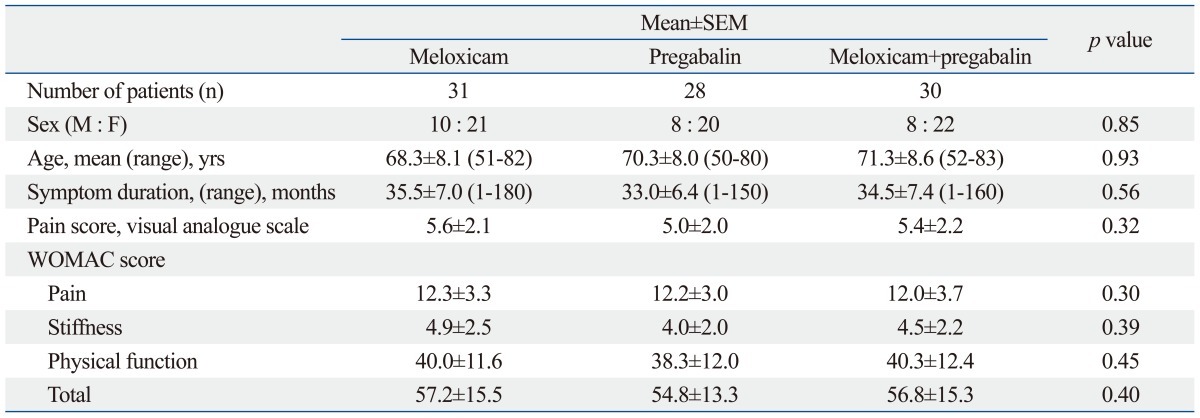
Table 2 shows the painDETECT score before medication, indicating likely NP (score ≥19), possible NP (score ≥13 to ≤18), and unlikely NP (score ≤12). Within this study population, 6 (6.7%) were classified as likely NP, 16 (17.8%) as possible NP, and 67 (75.3%) as unlikely NP. The NP scores were not significantly different among the three groups (p>0.05).
Table 2.
PainDETECT Score before Medication
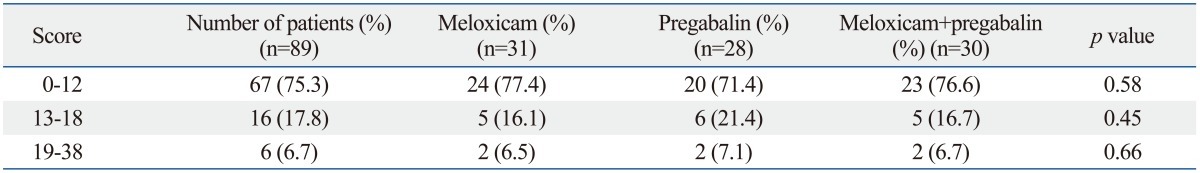
The painDETECT score was distributed from 0 to 38. Patients were divided into three groups: neuropathic pain is likely (score ≥19), possible (score ≥13 to ≤18), and unlikely (score ≤12).
Table 3 shows evaluation of KL grade. There was no patient with KL0, and all patients were distributed from KL1 to KL4. Twenty-two (24.7%) patients were classified into KL1, 24 (27.0) into KL2, 31 (34.8%) into KL3, and 12 (13.5%) into KL4. The percentage and number of each KL grade were not significantly different among the three groups (p>0.05).
Table 3.
X-Ray Evaluation
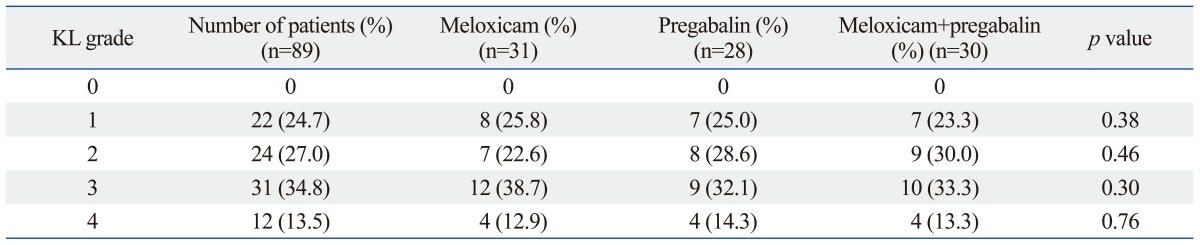
KL, Kellgren-Lawrence.
Table 4 shows pain during medication. Overall, medication improved the pain score in the three groups compared with before medication. There was significant pain relief in the meloxicam+pregabalin group as assessed by VAS score at 1, 2, and 4 weeks, and WOMAC score at 4 weeks, compared with the meloxicam or pregabalin only groups (p<0.05). No significant pain relief was seen in the meloxicam only group as assessed by VAS score during 4 weeks or WOMAC score at 4 weeks compared with the pregabalin only group (p>0.05).
Table 4.
Pain during Medication
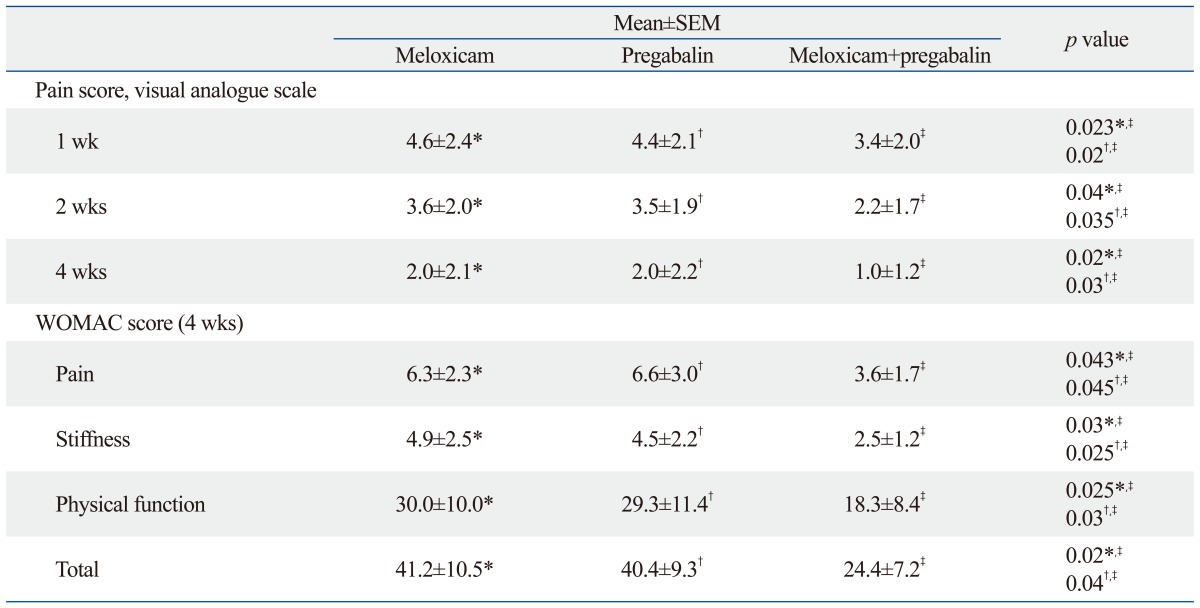
There was significant difference in all scores in the meloxicam+pregabalin group compared with the meloxicam or pregabalin only groups.
*,‡p<0.05.
†,‡p<0.05.
No significant difference in all scores was seen in the meloxicam only group compared with the pregabalin only group (*,†p>0.05).
Adverse events
There was no adverse event such as gastritis, nausea, dizziness, and somnolence in any patient.
DISCUSSION
In the current study, we investigated the efficacy of pregabalin for OA pain in OA patients. A combination of meloxicam+ pregabalin was more effective than meloxicam or pregabalin alone for pain in OA patients. This finding suggests that OA pain is a combination of inflammatory and neuropathic pain components.
The origin of OA pain is widely considered to be inflammatory, but our study identified at least 6.7% of our OA patients as likely to have NP and 17.8% as possibly having NP. Hochman, et al.14 used a list of NP descriptors from five validated questionnaires to evaluate knee OA pain. To distinguish inflammatory pain from NP in people with other chronic pain conditions, five items were commonly identified. These investigators reported that 34% of patients with OA of the knee described their pain in a way suggestive of NP.14 Some patients with severe pain and related disability may have a NP component in the pain of their knee OA.
Other investigators have reported that joint pain arises mainly from free nerve endings that exist in the capsule or in the synovium.15-17 By contrast, yet others have reported innervation of the osteochondral junction in human knee OA samples and suggested a contribution of the subchondral area to the pain of OA knees.18,19 We hypothesize that NP occurs in association with damage to nerves innervating subchondral bone because of its weight-bearing surface in late stage OA. Approximately 60-80% of OA patients achieve pain relief after local anesthetic treatment or surgical replacement of the affected joint, indicating that peripheral mechanisms drive the pain, although central mechanisms are also thought to play a role in some patients, and dysfunction of diffuse noxious inhibitory controls has been described as an alternative hypothesis.20-22 In an animal model of OA, the gradual proliferation of microglia related to neuropathic pain in the dorsal horn of the spinal cord demonstrated progressive nerve injury, which suggests the gradual initiation of a neuropathic pain state along with an inflammatory pain state in OA.23 These central mechanisms may overlap with those of other pain states including neuropathy.
Pregabalin was developed for management of NP; however, there has been no report of its use for pain in OA patients. Rahman, et al.24 reported that in an animal model of OA, pregabalin is useful for pain derived from knee OA, and they showed an altered physiology of deep dorsal horn wide dynamic range neurons in their model of knee OA, indicating a link between increased neuronal activity and hypersensitive behavioral responses in these animals.24 However, hypersensitivity was suppressed by antinociceptive actions of pregabalin, suggesting descending facilitation.24 In this regard, unraveling the cellular and molecular mechanisms underlying the OA pain state is of major clinical importance in the development of more clinically effective drugs such as pregabalin.
There are some limitations to the current study. First, we used only one drug dose in the three groups. In particular, we used 25 mg pregabalin for pain in patients in this study. Generally, 150 mg of pregabalin is recommended for the treatment of NP in patients with peripheral nerve injury and diabetic neuropathy. We believe that 150 mg is excessive for OA patients and were concerned about adverse events. Therefore, we selected 25 mg pregabalin for the current study. Second, we used 30 patients in each group. This number is not sufficient for a power analysis. Further study using different dosages and a larger number of patients is needed to clarify these points.
In conclusion, a combination of meloxicam plus pregabalin was effective for OA pain in OA patients. This finding, furthermore, suggests that OA pain is a combination of inflammatory and neuropathic pain components.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Paxton EW, Furnes O, Namba RS, Inacio MC, Fenstad AM, Havelin LI. Comparison of the Norwegian knee arthroplasty register and a United States arthroplasty registry. J Bone Joint Surg Am. 2011;93(Suppl 3):20–30. doi: 10.2106/JBJS.K.01045. [DOI] [PubMed] [Google Scholar]
- 2.Daousi C, MacFarlane IA, Woodward A, Nurmikko TJ, Bundred PE, Benbow SJ. Chronic painful peripheral neuropathy in an urban community: a controlled comparison of people with and without diabetes. Diabet Med. 2004;21:976–982. doi: 10.1111/j.1464-5491.2004.01271.x. [DOI] [PubMed] [Google Scholar]
- 3.Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003;103:249–257. doi: 10.1016/S0304-3959(02)00452-9. [DOI] [PubMed] [Google Scholar]
- 4.van der Kraan PM, Vitters EL, van de Putte LB, van den Berg WB. Development of osteoarthritic lesions in mice by "metabolic" and "mechanical" alterations in the knee joints. Am J Pathol. 1989;135:1001–1014. [PMC free article] [PubMed] [Google Scholar]
- 5.Ochiai N, Ohtori S, Sasho T, Nakagawa K, Takahashi K, Takahashi N, et al. Extracorporeal shock wave therapy improves motor dysfunction and pain originating from knee osteoarthritis in rats. Osteoarthritis Cartilage. 2007;15:1093–1096. doi: 10.1016/j.joca.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 6.Ivanavicius SP, Ball AD, Heapy CG, Westwood FR, Murray F, Read SJ. Structural pathology in a rodent model of osteoarthritis is associated with neuropathic pain: increased expression of ATF-3 and pharmacological characterisation. Pain. 2007;128:272–282. doi: 10.1016/j.pain.2006.12.022. [DOI] [PubMed] [Google Scholar]
- 7.Fernihough J, Gentry C, Malcangio M, Fox A, Rediske J, Pellas T, et al. Pain related behaviour in two models of osteoarthritis in the rat knee. Pain. 2004;112:83–93. doi: 10.1016/j.pain.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 8.Pomonis JD, Boulet JM, Gottshall SL, Phillips S, Sellers R, Bunton T, et al. Development and pharmacological characterization of a rat model of osteoarthritis pain. Pain. 2005;114:339–346. doi: 10.1016/j.pain.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 9.Dworkin RH, O'Connor AB, Backonja M, Farrar JT, Finnerup NB, Jensen TS, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain. 2007;132:237–251. doi: 10.1016/j.pain.2007.08.033. [DOI] [PubMed] [Google Scholar]
- 10.Freynhagen R, Baron R, Gockel U, Tölle TR. painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin. 2006;22:1911–1920. doi: 10.1185/030079906X132488. [DOI] [PubMed] [Google Scholar]
- 11.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 12.Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957;16:494–501. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pocock SJ, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics. 1975;31:103–115. [PubMed] [Google Scholar]
- 14.Hochman JR, French MR, Bermingham SL, Hawker GA. The nerve of osteoarthritis pain. Arthritis Care Res (Hoboken) 2010;62:1019–1023. doi: 10.1002/acr.20142. [DOI] [PubMed] [Google Scholar]
- 15.Grönblad M, Korkala O, Liesi P, Karaharju E. Innervation of synovial membrane and meniscus. Acta Orthop Scand. 1985;56:484–486. doi: 10.3109/17453678508993040. [DOI] [PubMed] [Google Scholar]
- 16.Fortier LA, Nixon AJ. Distributional changes in substance P nociceptive fiber patterns in naturally osteoarthritic articulations. J Rheumatol. 1997;24:524–530. [PubMed] [Google Scholar]
- 17.Saito T, Koshino T. Distribution of neuropeptides in synovium of the knee with osteoarthritis. Clin Orthop Relat Res. 2000:172–182. doi: 10.1097/00003086-200007000-00024. [DOI] [PubMed] [Google Scholar]
- 18.Suri S, Gill SE, Massena de Camin S, Wilson D, McWilliams DF, Walsh DA. Neurovascular invasion at the osteochondral junction and in osteophytes in osteoarthritis. Ann Rheum Dis. 2007;66:1423–1428. doi: 10.1136/ard.2006.063354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ogino S, Sasho T, Nakagawa K, Suzuki M, Yamaguchi S, Higashi M, et al. Detection of pain-related molecules in the subchondral bone of osteoarthritic knees. Clin Rheumatol. 2009;28:1395–1402. doi: 10.1007/s10067-009-1258-0. [DOI] [PubMed] [Google Scholar]
- 20.Creamer P, Hunt M, Dieppe P. Pain mechanisms in osteoarthritis of the knee: effect of intraarticular anesthetic. J Rheumatol. 1996;23:1031–1036. [PubMed] [Google Scholar]
- 21.Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86-A:963–974. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Kosek E, Ordeberg G. Lack of pressure pain modulation by heterotopic noxious conditioning stimulation in patients with painful osteoarthritis before, but not following, surgical pain relief. Pain. 2000;88:69–78. doi: 10.1016/S0304-3959(00)00310-9. [DOI] [PubMed] [Google Scholar]
- 23.Orita S, Ishikawa T, Miyagi M, Ochiai N, Inoue G, Eguchi Y, et al. Pain-related sensory innervation in monoiodoacetate-induced osteoarthritis in rat knees that gradually develops neuronal injury in addition to inflammatory pain. BMC Musculoskelet Disord. 2011;12:134. doi: 10.1186/1471-2474-12-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rahman W, Bauer CS, Bannister K, Vonsy JL, Dolphin AC, Dickenson AH. Descending serotonergic facilitation and the antinociceptive effects of pregabalin in a rat model of osteoarthritic pain. Mol Pain. 2009;5:45. doi: 10.1186/1744-8069-5-45. [DOI] [PMC free article] [PubMed] [Google Scholar]


